Abstract
Introduction:
False beliefs about sleep can persist despite contradicting scientific evidence, potentially impairing population health. Identifying commonly held false beliefs lacking an evidence base (‘myths’) can inform efforts to promote population sleep health.
Method:
We compiled a list of potential myths using internet searches of popular press and scientific literature. We utilized a Delphi process with sleep experts (n=10) from the fields of sleep medicine and research. Selection and refinement of myths by sleep experts proceeded in three phases, including: focus groups (Phase 1); email-based feedback to edit, add, or remove myths (Phase 2); and closed-ended questionnaires (Phase 3) where experts rated myths on two dimensions: falseness and public health significance using 5-point Likert scale from 1 (“not at all”) to 5 (“extremely false”).
Results:
The current study identified 20 sleep myths. Mean expert ratings of falseness ranged from 5.00 (s.d.=0.00) for the statement “during sleep the brain is not active” to 2.50 (s.d.=1.07) for the statement “sleeping in during the weekends is a good way to ensure you get adequate sleep.” Mean responses to public health significance ranged from 4.63 (s.d.=0.74) for the statement “many adults need only 5 or less hours of sleep for general health” to 1.71 (s.d.=0.49) for the statement “remembering your dreams is a sign of a good night’s sleep.”
Conclusion:
The current study identified commonly held sleep myths that have a limited or questionable evidence base. Ratings provided by experts suggest areas that may benefit from public health education to correct myths and promote healthy sleep.
Keywords: Population health, sleep health, sleep medicine, social psychology, myths
Introduction
Sleep is increasingly recognized as fundamental to overall health, as reflected in position statements and reports by leading scientific, clinical, and governmental organizations in the U.S. and internationally.1–6 In addition, research has examined genetic,7,8 physiologic,9,10 and environmental factors11 that play a critical role in sleep-wake regulation. Despite these advances in knowledge, little attention has been paid to widely-held beliefs about sleep in the public arena and whether these beliefs are consistent with the scientific evidence pertaining to how sleep actually impacts health and functioning. While some widely-held beliefs may promote behaviors that improve population health, those that are inconsistent with the evidence may actually degrade population-level sleep health.
Beliefs can take many different forms. According to the Health Belief Model, health behaviors can be predicted by beliefs associated with risk susceptibility, risk severity, benefits to action, barriers to action, self-efficacy, and cues to action.12 While this prevailing framework predicts beliefs that are associated with health behavior, beliefs that lack an evidence base (‘myths’) can be perpetuated in our daily lives through various sources, such as peer- or media-related influences.13 Prior research has identified the potential adverse public health consequences of myths regarding obesity,14 cancer risk,15 and smoking.16 To our knowledge, no prior study has systematically ascertain potential myths about sleep.
Sleep deficiency (defined as inadequate sleep duration and/or poor sleep quality) is a public health issue.17 Approximately one third of adults in the U.S. report sleeping less than the recommended 7 hours nightly.18 Further, approximately 30% of adults in the U.S. endorse insomnia symptoms and 10% have received a clinical diagnosis.19–21 Insufficient sleep duration and sleep difficulties carry economic burden, estimated to be over $40 billion annually.22 In sleep medicine, little attention has been paid to sleep myths that may persist in the population despite availability of scientific evidence to the contrary. In order to understand the impact of sleep myths on the population, we first need to identify commonly-held beliefs that are not supported by scientific evidence. The goal of this study was to identify myths about sleep.
Methods
We conducted internet searches to identify articles in the popular press about potential sleep myths. Then, we engaged experts using the Delphi method23 to identify those myths. We defined a myth as a belief held by individuals that lacks a strong evidence base or is contradicted by existing scientific evidence.24 The Delphi method is a systematic protocol for collecting opinions from experts in a certain domain.23 Using this method, experts were recruited and then engaged in a series of open-ended discussions, followed by use of closed-ended questionnaires.25
Participants and procedure
A convenience sample of experts was identified using PubMed searches. To qualify as an expert for this study, each expert needed 20 articles published and cited in 20 or more other peer-reviewed publications with at least one of the following Medical Subject Headings (MeSH): “sleep” and either “circadian rhythms;” “neuroscience;” or “psychiatry.” Twenty individuals who met these criteria were contacted. Among the experts contacted, 10 participated in the study (co-authors MG, SY, WT, OB, KK, SP, LH, DB, GJL, CC).
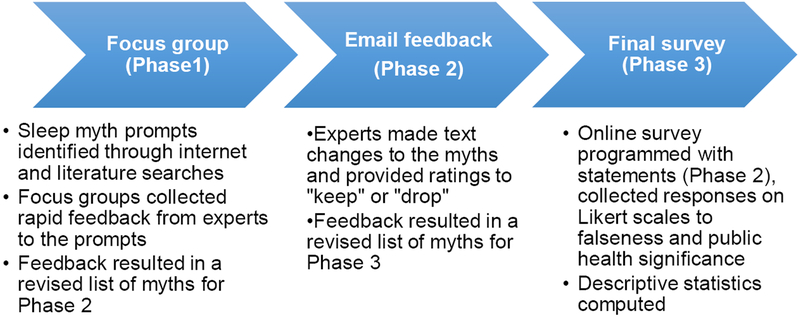
Procedures for the current study included three phases (Figure 1). Before the Delphi procedures, a search was conducted on a large online search engine in September 2016 using the terms: “sleep” AND (“myth” OR “misconception” OR “misperception”). From this search activity, the search engine identified over 8,000 websites. We used search tools to return 50 websites per page. We analyzed results on the first 5 pages (250 pages of content) to identify the most common sleep myths. Specifically, a research assistant downloaded the text from each article into a single document. Two independent coders reviewed this word document to categorize myths into categories (e.g., myths about sleep hygiene, sleep duration, and bedroom environment). Then, the first and last authors reviewed this list and consolidated the myths to a shorter list of the 50 most common myths about sleep. We used this list for the first phase of the Delphi method.
Figure 1.
Flow chart describing the Delphi phases to identify sleep myths.
The first phase of the Delphi method included focus groups where experts were asked to provide rapid-fire feedback to the list of potential myths identified in the online searches. Experts were asked to provide feedback and reactions for each potential myth based on two criteria: 1) falseness, or the perceived strength of existing contradictory evidence to refute the myth statement, and 2) public health significance, or the degree to which myths would be problematic to public health if allowed to go unchallenged. This phase resulted in 20 pages of focus group data that were transcribed and analyzed using the constant comparative method of qualitative analysis, whereby transcripts were read critically several times to identify primary themes in available responses.26 If a majority of experts (>50%, or >5 experts) agreed that a statement was true, and therefore not a myth, the statement was dropped. These activities resulted in a shorter list of 22 statements judged by most experts to be untrue, or “myths.”
In the second phase of the Delphi process, experts were provided the revised list of 22 potential myths. Experts were instructed to make edits to the statements for clarity. In addition, experts were asked to vote “keep” or “drop” for each potential myth using the two definitional criteria: 1) falseness, and 2) public health significance. Myths that received a “drop” rating by the majority of experts (>50%, >5) were dropped at this stage. Results from this phase were also analyzed using the constant comparative method of qualitative analysis.26 Potential myths that were marked “drop” by a majority of experts were eliminated from the analysis. In addition, all clarifications proposed for potential myths from experts were incorporated. Disagreement on edits was rare and resolved by the experts and first author via email. At this stage, experts identified two new potential myths believed to be missing from the initial list, resulting in a revised list of 24 potential myths.
In the third and final phase, experts rated potential myths using a closed-ended survey. Specifically, experts rated the potential myths on their degree of falseness and public health significance. In the case of truth/falseness, experts marked their response to the question “How false is each statement” on a scale from “Not at all false” (1), “A moderate amount false” (3), to “A great deal false” (5). In the case of public health significance, experts rated its importance, from a public health standpoint, on a scale from “Not at all” (1), “A moderate amount” (3) to “A great deal” (5). Descriptive statistics, including mean and standard deviation of expert ratings, were tabulated using SPSS (version 24.0, Armonk, NY: IBM Corporation). Mean expert rating above the scale midpoint on falseness (a mean response above 3, or neutral, which indicated agreement with falseness of the statement) was used as the threshold for establishing consensus that a statement or assertion was a myth.
Results
Delphi procedures resulted in classification of 20 of the statements as myths. Myths were categorized in the following domains: (1) sleep duration; (2) sleep timing; (3) behaviors during sleep; (4) daytime behaviors that relate to sleep; (5) pre-sleep behaviors; and (6) brain function and sleep. Expert ratings as well as a summary of the evidence regarding the myths are outlined below. Myths are rank-ordered within each domain on ratings of falseness (from high falseness to low).
(1) Sleep Duration
Myth: Being able to fall asleep “anytime, anywhere” is a sign of a healthy sleep system
Experts provided a rating of falseness for this myth “A great deal” (4.75 ± 0.46) and a rating of public health significance “A lot” (4.00 ± 0.93). Excessive daytime sleepiness, or the ability to fall asleep ‘anytime, anywhere’ can result from sleep deficiency.27 In other words, rather than being characteristic of “a good sleeper,” being able to fall asleep “anytime, anywhere” may be indicative of a chronically sleep-deprived state. Excessive daytime sleepiness can also be one of the primary symptoms of obstructive sleep apnea (OSA).28Individuals who report OSA symptoms (e.g., sleepiness) and are not treated for OSA are at high risk for adverse consequences, such as motor vehicle crashes.29 Strong evidence refutes the myth that ability to fall asleep “anytime, anywhere” is a sign of healthy sleep, but is instead likely a sign of an underlying sleep problem.
Myth: Many adults need only 5 or fewer hours of sleep for general health
Experts provided a rating of falseness for this myth “A great deal” (4.63 ± 0.52) and a rating of public health significance “A great deal” (4.63 ± 0.74). Habitual insufficient sleep (5 or fewer hours) is associated with adverse outcomes related to cardiovascular, metabolic, mental, and immunological health.1–3 Although preliminary evidence suggests there may be a short sleeper phenotype30 or some individuals who can function well with less than the recommended 7 hours (e.g., 5 hours) without adverse impact, these individuals represent a minority. Evidence of elevated chronic disease risk with short sleep duration supports a recommendation of 7 hours for most adults1–3 and refutes this myth.
Myth: Your brain and body can learn to function just as well with less sleep
Experts provided a rating of falseness for this myth “A great deal” (4.63 ± 1.06) and a rating of public health significance “A lot” (4.14 ± 0.90). When sleep is restricted, self-reported levels of sleepiness increase for the first several days before starting to plateau, but objective measures of a person’s inability to stay awake show a steady increase over time.31 Several studies show that even after weeks of observation and tracking, reducing sleep leads to sustained decrements in performance.32 Further, night shift-workers, who habitually sleep fewer hours than day-workers, face higher morbidity due to breast cancer and all-cause mortality than day-workers.33 Overall, individuals might “adjust” to consistent sleep debt and/or circadian misalignment, but do so at the risk of serious health consequences.33 Consequently, evidence refutes the statement that the brain and body can adapt to function on less sleep.
Myth: Adults sleep more as they get older
Experts provided a rating of falseness for this myth “A great deal” (4.63 ± 0.52) and a rating of public health significance “A lot” (4.00 ± 0.93). Sleep duration varies across the lifespan.34 A meta-analysis demonstrates that older adults get less sleep than younger adults.35 The decline in sleep duration among older adults may be at least in part due to medical comorbidities.36,37 Further, it is not evident whether older adults in general need less sleep than do younger adults, only that they get less. Thus, evidence refutes the statement that healthy older adults get more sleep with age.
Myth: If you can get it, more sleep is always better
Experts provided a rating of falseness for this myth “A moderate amount” (3.25 ± 1.28) and a rating of public health significance “A moderate amount” (2.86 ± 0.90). Associations between mortality and long sleep (defined as ≥ 8 hours in several studies; longer in others),38–40 and prospective cohort research has shown higher mortality among long sleepers, even among individuals with good health status when first assessed.41 However, because of a lack of experimental evidence of detrimental effects of long sleep duration, it has been argued that habitual long sleep may be a marker of other unreported chronic conditions rather than causally linked to ill health or early mortality.1
As noted in consensus reports, obtaining extra sleep is important for those recovering from sleep loss or healing from a medical condition; evidently, children need longer sleep for optimal behavioral development.1,2 However, in contrast with short sleep, there is not clear experimental evidence that long sleep is related to health and mortality and there is no consensus about habitual long sleep.1,2 Earlier field experiments and more recent laboratory experiments42–44 have generated conflicting results regarding positive and negative effects of long sleep on mood and cognition. Other laboratory studies have shown, when provided with the opportunity for long sleep, participants sleep longer and eventually asymptotically experience longer than habitual sleep duration (>8 hours) and demonstrate more alertness than individuals on shorter sleep schedules.45,46 Also, performance enhancements are observed among individuals instructed to sleep longer (>8 hours).47 However, for individuals with insomnia, trying to compensate for lack of sleep by staying in bed longer can lead to a vicious cycle of further sleep fragmentation and more time lying awake struggling to stay asleep. Conversely, restriction of time in bed is one of the most effective behavioral treatments for insomnia. Thus, low ratings from experts on falseness reflect the conflicting evidence in the field regarding long sleep duration and belie the myth that obtaining more sleep is always better.
Myth: One night of sleep deprivation will have lasting negative health consequences
Experts provided a rating of falseness for this myth “A moderate amount” (3.25 ± 1.04) and a rating of public health significance “A moderate amount” (2.29 ± 0.76). One night of sleep deprivation has some short-term adverse effects, though they likely resolve with recovery sleep. Meta-analysis has found sleep deprivation (e.g., lack of sleep for at least 24 hours) leads to worse performance in several cognitive domains (e.g., lapses in simple attention).48 Another review examined the effects of sleep deprivation on cardiovascular and metabolic domains, demonstrating sleep deprivation causes increased cardiovascular mortality.49 Also, sleep deprivation can cause an increase in resting blood pressure.49,50 However, experimental research shows performance on a cognitive task declines among individuals subjected to two nights of sleep deprivation, yet performance returns to pre-deprivation levels with sufficient sleep recovery.51 Thus, evidence of adverse outcomes associated with sleep deprivation is strong. However, evidence from cognitive and performance measures suggests that sleep recovery following brief periods of sleep deprivation can return to baseline levels.
(2) Sleep Timing
Myth: In terms of your health, it does not matter what time of day you sleep
Experts provided a rating of falseness for this myth “A great deal” (4.63 ± 0.74) and a rating of public health significance “A lot” (3.57 ± 1.13). Research on night shift-workers (individuals who work at night and sleep during the day), provides evidence regarding the implications of sleep timing for health. Night shift workers, who experience circadian desynchronization, report less sleep and lower sleep quality than day-workers,52 and are also at higher risk for long-term adverse health outcomes including depression,53 diabetes,54 and breast cancer.33 Although it could be argued that sleep during the day is better than no sleep at all, the evidence from shift-workers suggests that sleep timing is related to health, thereby refuting this myth.
(3) Behaviors During Sleep
Myth: Lying in bed with your eyes closed is almost as good as sleeping
Experts provided a rating of falseness for this myth “A great deal” (4.63 ± 0.74) and a rating of public health significance “A lot” (3.86 ± 1.07). Endocrine, cardiovascular, metabolic, and cognition is markedly different during wakefulness than non-rapid eye movement (REM) sleep. Cognition is a prime example, as brain activity during sleep takes on a very different pattern compared with activity in the awake brain.55–57 Sleep and arousal regulatory centers in the brain function as a sort of “on-off” switch, whereby one is either sleeping or awake with little overlap.58 Also, a sharp nocturnal “dip” in core body temperature is much larger when individuals are asleep compared to when they lie quietly awake in bed, providing further evidence that sleep differs from lying down with eyes closed.59 Thus, available evidence showing cognitive activity when a person is sleeping is distinctly different from wake with eyes closed refutes this myth.
Myth: If you have difficulty falling asleep, it is best to stay in bed and try to fall back to sleep
Experts provided a rating of falseness for this myth “A great deal” (4.63 ± 0.74) and a rating of public health significance “A moderate amount” (3.14 ± 0.90). Individuals who experience difficulty falling asleep are instructed to follow what is termed ‘stimulus control therapy.’60 Although it seems counter-intuitive, in stimulus control therapy individuals experiencing difficulty falling asleep are instructed to leave their bed, avoid blue light, and return to bed only when they are tired. Individuals who follow these instructions demonstrate significant improvements, such as lower time to fall asleep.61 Meta-analysis also shows stimulus control therapy improves one’s ability to fall asleep and overall sleep quality.62 Thus, available evidence and high ratings on falseness from experts refutes this myth.
Myth: Although annoying for bed partners, loud snoring is mostly harmless
Experts provided a rating of falseness for this myth “A lot” (4.25 ± 0.89) and a rating of public health significance “A lot” (4.25 ± 0.89). Snoring is caused by turbulent airflow due to partial obstruction of the upper airway during sleep. One large, cross-sectional study of US adults found 52.8% reported snoring, and that snoring was associated with adverse health outcomes in its own right.63 Furthermore, snoring is a primary symptom of OSA that, when untreated, places individuals at elevated risk for adverse cardiovascular events.5 Thus, loud or bothersome snoring may be an indication that one needs to consult with a healthcare provider.
Myth: A sound sleeper rarely moves at night
Experts provided a rating of falseness for this myth “A lot” (3.88 ± 0.64) and a rating of public health significance “A little” (1.83 ± 0.41). Occasional movement has been documented as a normal part of sleep.64 The number of movements during sleep vary across the lifespan, with the fewest occurring during sleep among those between ages 18 to 30.9 However, unless prolonged and chronic, small movements and cortical arousals during sleep may be a part of normal sleep.
(4) Daytime Behaviors that Relate to Sleep
Myth: Hitting the snooze when you wake up is better than getting up when the alarm first goes off
Experts provided a rating of falseness for this myth “A lot” (3.75 ± 1.04) and a rating of public health significance “A moderate amount” (2.75 ± 1.04). While little research has directly examined effects of alarms in interrupting sleep, and the role of “snoozing” in between alarm sounds, sleep disruptions are not optimal. Sleep fragmentations, such as those caused by a snooze bar, are associated with adverse outcomes, including decreased mental flexibility and subjective mood.65 Thus, evidence suggests it may be best to set the alarm when one needs to get up instead of setting multiple alarms that might interrupt sleep.
Myth: If you are having difficulties sleeping at night, taking a nap in the afternoon is a good way to get adequate sleep
Experts provided a rating of falseness for this myth “A moderate amount” (3.13 ± 1.13) and a rating of public health significance “A moderate amount” (3.14 ± 1.07). Research shows a ‘siesta,’ or mid-afternoon nap, is common in some cultures.66,67 Napping can also be used to supplement insufficient nocturnal sleep. However, habitual napping can be associated with adverse health outcomes.68 Napping is discouraged among those with insomnia, as it may reduce homeostatic sleep drive and perpetuate nighttime insomnia and presents health consequences.57,67 The evidence that napping can perpetuate insomnia along with expert scores casts doubt on a recommendation that individuals who experience difficulty sleeping at night should nap.
(5) Pre-Sleep Behaviors
Myth: Alcohol before bed will improve your sleep
Experts provided a rating of falseness for this myth “A lot” (4.13 ± 0.35) and a rating of public health significance “A lot” (4.00 ± 0.76). Folklore makes reference to a ‘nightcap’ or serving of alcohol consumed as part of the bedtime routine.70 The literature on sleep and alcohol shows alcohol consumed close to bedtime reduces sleep latency, but subsequently causes sleep disturbances in the second half of the night. Across a number of different studies and doses, overall alcohol has a negative overall impact on sleep, delaying the onset of REM sleep.71 Alcohol consumption has also been found to worsen sleep apnea symptoms.72 Thus, evidence is relatively strong to refute this myth.
Myths: For sleeping, it is better to have a warmer bedroom than a cooler bedroom
Experts provided a rating of falseness for this myth “A lot” (3.88 ± 1.13) and a rating of public health significance “A moderate amount” (2.75 ± 1.04). Cross-sectional evidence showed a warm environment (specifically, a reported “hot and stuffy” bedroom) is associated with poor sleep.73 Another cross-sectional study of self-reported environmental barriers to sleep showed “too high a temperature” was a limiting factor for sleep health.74 Consequently, a temperature between 65 and 70 degrees Fahrenheit is often recommended for sleep.75 Taken together, there is moderate evidence to refute this myth.
Myth: Boredom can make you sleepy even if you got adequate sleep before
Experts provided a rating of falseness for this myth “A lot” (3.75 ± 1.04) and a rating of public health significance “A moderate amount” (2.71 ± 1.11). It is sometimes said that boring activities, such as a dry lecture or meeting, could induce sleepiness. However, participants who underwent 60 hours of forced bed rest, arguably total boredom, slept longer than 7 hours in a given 24-hour cycle, but did not sleep the entire time.45,46,76 Other evidence from cross-sectional surveys among older adults shows individuals with hobbies and lower reported boredom have better sleep quality.77 Thus, boredom may reveal underlying sleepiness, but boredom alone does not cause sleepiness.
Myth: Watching television in bed is a good way to relax before sleep
Experts provided a rating of falseness for this myth “A moderate amount” (3.50 ± 0.93) and a rating of public health significance “A moderate amount” (3.14 ± 1.35). Routines before bed can include television watching, as one survey of adults in the U.S. found 50% of respondents reported television watching in the 30-minutes period leading up to bedtime.72 Time-use data from U.S. adults also revealed late-night television watching to be more common among short sleepers.79 Also, experimental evidence shows pre-sleep arousal mediates the relationship between television viewing and sleep difficulties.80 Thus, television viewing may not be an optimal pre-bed activity for relaxation before bed.
Myth: Exercising within 4 hours of bedtime will disturb your sleep
Experts provided a rating of falseness for this myth “A moderate amount” (3.25 ± 1.04) and a rating of public health significance “A moderate amount” (2.43 ± 0.53). Exercise and sleep appear to be mutually beneficial, as one meta-analysis showed small to moderate improvements in sleep-related variables with consistent physical activity.81 According to survey data from US adults, nighttime exercise was not associated with sleep disturbance for the majority of individuals.82 Other experimental evidence shows no impairment in sleep following vigorous nighttime exercise.81,83,84 Thus, low ratings of falseness and conflicting evidence preclude a definitive conclusion that this statement is indeed a myth.
(6) Brain Function and Sleep
Myth: During sleep, the brain is not active
Experts provided a rating of falseness for this myth “A great deal” (5.00 ± 0.00) and a rating of public health significance “A little” (2.00 ± 1.19). Although it may appear to an observer that the brain is passive during sleep, research indicates otherwise. The characteristic neuronal activity in the thalamus and brainstem of the awake EEG begins to slow and brain waves become larger in amplitude.58 Then, sleep is periodically marked during REM sleep by activity, including eye movement, loss of muscle tone, and rapid firing of neurons.85,86 Finally, sleep plays an important role in clearance of neurotoxic waste from the brain.87 Thus, strong evidence refutes the myth that the brain is passive during sleep.
Myth: Remembering your dreams is a sign of a good night’s sleep
Experts provided a rating of falseness for this myth “A lot” (3.63 ± 1.190) and a rating of public health significance “A little” (1.71 ± 0.49). Diaries comparing sleep duration and dream recall show an association between sleep duration and dreaming.88 This research suggests that longer sleep duration, which would provide opportunity for more and longer REM episodes, is a marker of a good night’s sleep. However, dream recall in sleep research can be conducted with dream diaries, but also by awakening participants from REM sleep when the majority of dreaming takes place.89,90 Thus, the challenges associated with dream research (e.g., awakening from REM and dream diaries) and the minimal number of studies examining the relationship between sleep health and dreaming, refute this myth.
Statements not classified as myths
Four statements identified in the Delphi approach as potential myths were dropped in the final phase of the procedure because they did not meet definitional criteria for falseness. The average expert rating of falseness to the statement “Sleeping in on weekends is a good way to ensure you get adequate sleep” was 2.50 ± 1.07. Second, regarding the statement “Waking up in the middle of the night is a sign of poor sleep” the average rating of falseness was 3.00 ± 1.07. Third, the statement “Sleeping with a pet is comforting and improves sleep quality” received an average expert rating of 2.63 ± 1.19. Finally, the statement “It is better to sleep in, compared to getting up and exercising” received an average falseness rating of 3.00 ± 0.76.
Discussion
Myths about sleep that go unaddressed at the population level may result in maladaptive health behavior patterns. Dominant theories of behavior change posit that beliefs are important, for they predict behavioral intentions, which in turn predict health-related behaviors.91 Utilizing the Delphi approach, we engaged experts to develop a list of beliefs about sleep that are promulgated in the media, which represent sleep myths, or statements and suggestions that are not supported by scientific evidence. Our findings offer utility to educational efforts to improve sleep health in the population.
Myths about sleep identified in this study span conceptual domains, including sleep behavior (e.g., “Lying in bed with your eyes closed is almost as good as sleeping”), as well as sleep timing, sleep duration, behaviors relating to sleep, behaviors close to bedtime, and brain function. It is important to note that every myth with the exception of one (“During sleep, the brain is not active”) yielded some uncertainty about falseness among experts (e.g., ratings below the scale mid-point).
The disagreement about falseness of each statement between experts in the current study is intriguing. The disagreement among experts in our study could have been due to the different areas of knowledge and expertise among the experts, which may lend different perspectives on the topics addressed by the myths in this study. Alternatively, the disagreement could suggest the need for more research on the topics relating to the myths that received more varied expert responses. In this manner, the myths that received varied responses from experts may represent an agenda for additional future research to confirm or refute each myth.
Several myths identified suggest there may be beliefs in the general population that human beings can adapt to insufficient sleep. For instance, consider the myth “Many adults need only 5 hours or less of sleep for general health” and “Your brain and body can learn to function just as well with less sleep.” These beliefs could be perpetuated through a variety of sources, ranging from media to social influences. No matter their source, if believed to be true, perceptions that sleep is not important may have adverse effects on individual intention to obtain recommended sleep. Also, several beliefs suggest important targets for sleep health education campaigns and other communication-based efforts to change unfounded beliefs. For instance, the belief “if you have difficulty falling asleep, it is best to stay in bed and try to fall back asleep,” could be altered with an educational campaign or initiative to promote awareness about stimulus control therapy or leaving the bedroom during periods of sleep onset difficulty, avoiding blue light exposure, and returning to the bed when tired.
Experts in the fields of sleep, circadian rhythms, and neuroscience offered judgments regarding the myths that potentially hinder population health. Further, experts indicated the public health significance of myths, and in so doing set an agenda for future research that may seek to promote evidence-based beliefs and ultimately, evidence-based population sleep health practices.
Limitations
The sample of experts identified was based on convenience sampling based on peer-reviewed publications from PubMed searches. A larger sample of experts in the fields of sleep medicine, circadian rhythms, and related fields of neuroscience and psychiatry may have yielded somewhat different results. In addition, the evidence to refute the myths varied in ‘strength,’ so that some myths could be refuted by meta-analyses or clinical trials. Other myths had less available data or weaker level of evidence such as cross-sectional survey data. Other myths may have been tangentially addressed in the scientific literature. In addition, although this study utilized rigorous procedures to engage experts in identifying sleep myths, many of the statements were qualified by at least one expert disagreeing regarding its falseness. The vague statements and unqualified/under-specified lay language lend themselves to a variety of interpretations. Thus, it should be noted that the classification as a myth is qualified by varied ratings across the experts of a variety of statements that could be better crafted to be more clearly myth, or clearly evidence-based statements on that general topic. Further, a number of sleep myths may have not been identified in a search using “Myth,” but instead additional statements may exist that lack supporting scientific evidence may instead be promulgated as truth. Finally, the Delphi method presents a limitation in that once myths are selected through the various steps outlined in this method, they are difficult to amend. Certainly, a larger panel of experts may have afforded the design of a broader array of myths or linguistic changes to improve comprehensibility of the myths articulated in this study. Obtaining expert input on statements that lack evidence (myths) is the first step before future research may examine actual prevalence of myths in the population or associations with health outcomes.
Implications
Beliefs are associated with behaviors. Thus, altering health-related beliefs that are untrue is one promising strategy for promoting population health.14 Beliefs are cognitive constructs and are prone to change over time through experience and influence from peers and news sources.13 Public health campaigns can reach a large number of individuals to promote awareness about health practices and change beliefs and behaviors.
Public health campaigns have been undertaken in domains such as smoking cessation and highway safety.92,93 The statements identified by experts in the current study represent potential future directions for public health campaigns and efforts that seek to address untrue beliefs about sleep, promote awareness of the importance of sleep, and bolster intentions in the population to engage in healthful sleep practices.
Results of the current study also have implications in family contexts. For instance, a snoring bed partner could disrupt a partner’s sleep or other individuals in the household. In addition, promoting awareness about problematic snoring among spouses and the need to seek treatment for potential sleep apnea could be a potentially promising direction for future interventions.
The myths about sleep identified in the current study represent a sampling of the potentially numerous untrue beliefs in the population regarding sleep health. Although we recruited and engaged sleep experts in identifying sleep health beliefs, future work could engage the general public to explore the prevalence of identified myths at the population level. In so doing, future research may develop an agenda for public health communication and education that seeks to change population-level beliefs that are not supported by scientific evidence regarding sleep health.
Conclusion
Beliefs may be broadly categorized as those that promote or those that degrade healthful sleep practices. In this study, we focused on potential myths, one category of beliefs that have potential adverse effects on population sleep health. We utilized a systematic method for engaging experts in iterative rounds of open-ended, followed by closed-ended, feedback. We identified a list of 20 myths categorized into six dimensions of sleep. The results provide a working framework for public health research and practice to address sleep beliefs that are not substantiated by scientific evidence, in the hope of ultimately promoting healthful sleep practices.
Table 1.
Statements classified as myths displayed by conceptual domains with corresponding expert ratings on falseness and public health significance on scales from 1 (not at all) to 5 (extremely, n=10).
| Degree of Falseness | Public Health | |||
|---|---|---|---|---|
| Statement | M | S.D. | M | S.D. |
| 1) Sleep Duration | ||||
| 1 Being able to fall asleep “anytime, anywhere” is a sign of a healthy sleep system | 4.75 | 0.46 | 4.00 | 0.93 |
| 2 Many adults need only 5 or less hours of sleep for general health | 4.63 | 0.52 | 4.63 | 0.74 |
| 3 Your brain and body can learn to function just as well with less sleep | 4.63 | 1.06 | 4.14 | 0.90 |
| 4 Adults sleep more as they get older | 4.13 | 0.99 | 2.29 | 0.76 |
| 5 If you can get it, more sleep is always better | 3.25 | 1.28 | 2.86 | 0.90 |
| 6 One night of sleep deprivation will have lasting negative health consequences | 3.25 | 1.04 | 2.29 | 0.76 |
| 2) Sleep Timing | ||||
| 7 In terms of your health, it does not matter what time of day you sleep | 4.63 | 0.74 | 3.57 | 1.13 |
| 3) Behaviors During Sleep | ||||
| 8 Lying in bed with your eyes closed is almost as good as sleeping | 4.63 | 0.74 | 3.86 | 1.07 |
| 9 If you have difficulty falling asleep, it is best to stay in bed and try to fall back to sleep | 4.63 | 0.74 | 3.14 | 0.90 |
| 10 Although annoying for bed partners, loud snoring is mostly harmless | 4.25 | 0.89 | 4.25 | 0.89 |
| 11 A sound sleeper rarely moves at night | 3.88 | 0.64 | 1.83 | 0.41 |
| 4) Daytime Behaviors that Relate to Sleep | ||||
| 12 Hitting the snooze when you wake up is better than getting up when the alarm first goes off | 3.75 | 1.04 | 2.75 | 1.04 |
| 13 If you are having difficulties sleeping, taking a nap in the afternoon is a good way to get adequate sleep | 3.13 | 1.13 | 3.14 | 1.07 |
| 5) Pre-Sleep Behaviors | ||||
| 14 Alcohol before bed will improve your sleep | 4.13 | 0.35 | 4.00 | 0.76 |
| 15 For sleeping, it is better to have a warmer bedroom than a cooler bedroom | 3.88 | 1.13 | 2.75 | 1.04 |
| 16 Boredom can make you sleepy even if you got adequate sleep before | 3.75 | 1.04 | 2.71 | 1.11 |
| 17 Watching television in bed is a good way to relax before sleep | 3.50 | 0.93 | 3.14 | 1.35 |
| 18 Exercising within 4 hours of bedtime will disturb your sleep | 3.25 | 1.04 | 2.43 | 0.53 |
| 6) Brain Function and Sleep | ||||
| 19 During sleep, the brain is not active | 5.00 | 0.00 | 2.00 | 1.00 |
| 20 Remembering your dreams is a sign of a good night’s sleep | 3.63 | 1.19 | 1.71 | 0.49 |
Table 2.
Statements not classified as myths with corresponding expert ratings of falseness and public health significance on scales from 1 (not at all) to 5 (extremely, n=10).
| Degree of Falseness | Public Health | |||
|---|---|---|---|---|
| Statement | M | S.D. | M | S.D. |
| 1 Waking up in the middle of the night is a sign of poor sleep | 3.00 | 1.07 | 2.71 | 0.95 |
| 2 It is better to get up and exercise than sleep, even if it means cutting your sleep short | 3.00 | 0.76 | 2.57 | 0.53 |
| 3 Sleeping with a pet is comforting and improves sleep quality | 2.63 | 1.19 | 2.14 | 0.90 |
| 4 Sleeping in on weekends is a good way to ensure you get adequate sleep | 2.50 | 1.07 | 3.14 | 0.69 |
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Watson NF, Badr MS, Belenky G, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. J Clin Sleep Med. 2015;11(06):591–592. doi: 10.5664/jcsm.4758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Watson NF, Badr MS, Belenky G, et al. Recommended Amount of Sleep for a Healthy Adult: A Joint Consensus Statement of the American Academy of Sleep Medicine and Sleep Research Society. Sleep. 2015;38(6):843–844. doi: 10.5665/sleep.4716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health J Natl Sleep Found. 2015;1(1):40–43. doi: 10.1016/j.sleh.2014.12.010 [DOI] [PubMed] [Google Scholar]
- 4.Britt LD, Sachdeva AK, Healy GB, Whalen TV, Blair PG. Resident duty hours in surgery for ensuring patient safety, providing optimum resident education and training, and promoting resident well-being: A response from the American College of Surgeons to the Report of the Institute of Medicine, “Resident Duty Hours: Enhancing Sleep, Supervision, and Safety”. Surgery. 2009;146(3):398–409. doi: 10.1016/j.surg.2009.07.002 [DOI] [PubMed] [Google Scholar]
- 5.Somers VK, White DP, Amin R, et al. Sleep apnea and cardiovascular disease: An american heart association/american college of cardiology foundation scientific statement from the american heart association council for high blood pressure research professional education committee, council on clinical cardiology, stroke council, and council on cardiovascular nursing in collaboration with the national heart, lung, and blood institute national center on sleep disorders research (national institutes of health). J Am Coll Cardiol. 2008;52(8):686–717. [DOI] [PubMed] [Google Scholar]
- 6.Strohl KP, Brown DB, Collop N, et al. An official American Thoracic Society Clinical Practice Guideline: sleep apnea, sleepiness, and driving risk in noncommercial drivers. An update of a 1994 Statement. Am J Respir Crit Care Med. 2013;187(11):1259–1266. doi: 10.1164/rccm.201304-0726ST [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dudley KA, Patel SR. Disparities and genetic risk factors in obstructive sleep apnea. Sleep Med. 2016;18:96–102. doi: 10.1016/j.sleep.2015.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Varvarigou V, Dahabreh IJ, Malhotra A, Kales SN. A review of genetic association studies of obstructive sleep apnea: field synopsis and meta-analysis. Sleep. 2011;34(11):1461–1468. doi: 10.5665/sleep.1376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bonnet MH, Burton GG, Arand DL. Physiological and medical findings in insomnia: Implications for diagnosis and care. Sleep Med Rev. 2014;18(2):111–122. doi: 10.1016/j.smrv.2013.02.003 [DOI] [PubMed] [Google Scholar]
- 10.Driscoll TR, Grunstein RR, Rogers NL. A systematic review of the neurobehavioural and physiological effects of shiftwork systems. Sleep Med Rev. 2007;11(3):179–194. doi: 10.1016/j.smrv.2006.11.001 [DOI] [PubMed] [Google Scholar]
- 11.Desantis AS, Diez Roux AV, Moore K, Baron KG, Mujahid MS, Nieto FJ. Associations of neighborhood characteristics with sleep timing and quality: the Multi-Ethnic Study Of Atherosclerosis. Sleep. 2013;36(10):1543–1551. doi: 10.5665/sleep.3054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Becker MH. The health belief model and personal health behavior. Health Educ Monogr. 1974;2:324–473. [Google Scholar]
- 13.Katz E, Lazarsfeld PF. Personal Influence. Glencoe, IL: Free Press; 1955. [Google Scholar]
- 14.Casazza K, Fontaine KR, Astrup A, et al. Myths, presumptions, and facts about obesity. N Engl J Med. 2013;368(5):446–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chavez LR, Hubbell FA, McMullin JM, Martinez RG, Mishra SI. Understanding Knowledge and Attitudes About Breast Cancer: A Cultural Analysis. Arch Fam Med. 1995;4(2):145. doi: 10.1001/archfami.1995.01850270069016 [DOI] [PubMed] [Google Scholar]
- 16.Leventhal H, Glynn K, Fleming R. Is the Smoking Decision an “Informed Choice”?: Effect of Smoking Risk Factors on Smoking Beliefs. JAMA. 1987;257(24):3373–3376. doi: 10.1001/jama.1987.03390240079027 [DOI] [PubMed] [Google Scholar]
- 17.Buysse DJ. Sleep health: Can we define it? Does it matter? SLEEP. 2014;37(1):9–17. doi: 10.5665/sleep.3298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of Healthy Sleep Duration among Adults — United States, 2014. MMWR Morb Mortal Wkly Rep. 2016;65(6):137–141. doi: 10.15585/mmwr.mm6506a1 [DOI] [PubMed] [Google Scholar]
- 19.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6(2):97–111. doi: 10.1053/smrv.2002.0186 [DOI] [PubMed] [Google Scholar]
- 20.Morin CM, Jarrin DC. Epidemiology of Insomnia. Sleep Med Clin. 2013;8(3):281–297. doi: 10.1016/j.jsmc.2013.05.002 [DOI] [PubMed] [Google Scholar]
- 21.Morin CM, Bootzin RR, Buysse DJ, Edinger JD, Espie CA, Lichstein KL. Psychological and behavioral treatment of insomnia:update of the recent evidence (1998–2004). Sleep. 2006;29(11):1398–1414. [DOI] [PubMed] [Google Scholar]
- 22.Hafner M, Stepanek M, Taylor J, Troxel WM, Van Stolk C. Why sleep matters — the economic costs of insufficient sleep. https://www.rand.org/pubs/research_reports/RR1791.html. Published 2016 Accessed August 17, 2017. [PMC free article] [PubMed] [Google Scholar]
- 23.Dalkey N, Helmer O. An experimental application of the Delphi method to the use of experts. Manag Sci. 1963;9(3):458–467. [Google Scholar]
- 24.Merriam-Webster. Myth. Merriam-Webster.com. www.merriam-webster.com. Published; 2016. Accessed March 1, 2016. [Google Scholar]
- 25.Schmidt RC. Managing Delphi Surveys Using Nonparametric Statistical Techniques*. Decis Sci. 1997;28(3):763–774. doi: 10.1111/j.1540-5915.1997.tb01330.x [DOI] [Google Scholar]
- 26.Charmaz K Constructing Grounded Theory: A Practical Guide through Qualitative Analysis. London, UK: Sage Publications Ltd; 2006. [Google Scholar]
- 27.Ohayon MM. From wakefulness to excessive sleepiness: what we know and still need to know. Sleep Med Rev. 2008;12(2):129–141. doi: 10.1016/j.smrv.2008.01.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bixler EO, Vgontzas AN, Lin H-M, Calhoun SL, Vela-Bueno A, Kales A. Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab. 2005;90(8):4510–4515. doi: 10.1210/jc.2005-0035 [DOI] [PubMed] [Google Scholar]
- 29.Garbarino S, Guglielmi O, Sanna A, Mancardi GL, Magnavita N. Risk of Occupational Accidents in Workers with Obstructive Sleep Apnea: Systematic Review and Meta-analysis. Sleep. 2016;39(6):1211–1218. doi: 10.5665/sleep.5834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.He Y, Jones CR, Fujiki N, et al. The Transcriptional Repressor DEC2 Regulates Sleep Length in Mammals. Science. 2009;325(5942):866–870. doi: 10.1126/science.1174443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Carskadon MA, Dement WC. Cumulative Effects of Sleep Restriction on Daytime Sleepiness. Psychophysiology. 1981;18(2):107–113. doi: 10.1111/j.1469-8986.1981.tb02921.x [DOI] [PubMed] [Google Scholar]
- 32.Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12(1):1–12. doi: 10.1046/j.1365-2869.2003.00337.x [DOI] [PubMed] [Google Scholar]
- 33.Lin X, Chen W, Wei F, Ying M, Wei W, Xie X. Night-shift work increases morbidity of breast cancer and all-cause mortality: a meta-analysis of 16 prospective cohort studies. Sleep Med. 2015;16(11):1381–1387. doi: 10.1016/j.sleep.2015.02.543 [DOI] [PubMed] [Google Scholar]
- 34.Miles LE, Dement WC. Sleep and aging. Sleep. 1980;3(2):1. [PubMed] [Google Scholar]
- 35.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-Analysis of Quantitative Sleep Parameters From Childhood to Old Age in Healthy Individuals: Developing Normative Sleep Values Across the Human Lifespan. Sleep. 2004;27(7):1255–1273. doi: 10.1093/sleep/27.7.1255 [DOI] [PubMed] [Google Scholar]
- 36.Jaussent I, Bouyer J, Ancelin M-L, et al. Excessive sleepiness is predictive of cognitive decline in the elderly. Sleep. 2012;35(9):1201–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ohayon MM, Vecchierini M-F. Normative sleep data, cognitive function and daily living activities in older adults in the community. Sleep. 2005;28(8):981–989. [PubMed] [Google Scholar]
- 38.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59(2):131–136. [DOI] [PubMed] [Google Scholar]
- 39.Patel SR, Ayas NT, Malhotra MR, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27(3):440–444. [DOI] [PubMed] [Google Scholar]
- 40.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. SLEEP. 2004;27(1):51–54. [PubMed] [Google Scholar]
- 41.Mesas AE, López-García E, León-Muñoz LM, Guallar-Castillón P, Rodríguez-Artalejo F. Sleep Duration and Mortality According to Health Status in Older Adults. J Am Geriatr Soc. 2010;58(10):1870–1877. doi: 10.1111/j.1532-5415.2010.03071.x [DOI] [PubMed] [Google Scholar]
- 42.Taub JM, Berger RJ. Performance and Mood Following Variations in the Length and Timing of Sleep. Psychophysiology. 1973;10(6):559–570. doi: 10.1111/j.1469-8986.1973.tb00805.x [DOI] [PubMed] [Google Scholar]
- 43.Youngstedt SD, Jean-Louis G. Long Sleep a Greater Mortality Risk Than Short Sleep in Older Adults. J Am Geriatr Soc. 2011;59(5):957–958. doi: 10.1111/j.1532-5415.2011.03396.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reynold AM, Bowles ER, Saxena A, Fayad R, Youngstedt SD. Negative Effects of Time in Bed Extension: A Pilot Study. J Sleep Med Disord. 2014;1(1). http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4217706/. Accessed February 24, 2016. [PMC free article] [PubMed] [Google Scholar]
- 45.Wehr TA, Moul DE, Barbato G, et al. Conservation of photoperiod-responsive mechanisms in humans. Am J Physiol. 1993;265(4 Pt 2):R846–857. doi: 10.1152/ajpregu.1993.265.4.R846 [DOI] [PubMed] [Google Scholar]
- 46.Klerman EB, Dijk D-J. Age-Related Reduction in the Maximal Capacity for Sleep—Implications for Insomnia. Curr Biol. 2008;18(15):1118–1123. doi: 10.1016/j.cub.2008.06.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mah CD, Mah KE, Kezirian EJ, Dement WC. The Effects of Sleep Extension on the Athletic Performance of Collegiate Basketball Players. Sleep. 2011;34(7):943–950. doi: 10.5665/SLEEP.1132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Lim J, Dinges DF. A Meta-Analysis of the Impact of Short-Term Sleep Deprivation on Cognitive Variables. Psychol Bull. 2010;136(3):375–389. doi: 10.1037/a0018883 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mullington JM, Haack M, Toth M, Serrador JM, Meier-Ewert HK. Cardiovascular, inflammatory, and metabolic consequences of sleep deprivation. Prog Cardiovasc Dis. 2009;51(4):294–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ogawa Y, Kanbayashi T, Saito Y, et al. Total sleep deprivation elevates blood pressure through arterial baroreflex resetting: a study with microneurographic technique. Sleep. 2003;26(8):986–989. [DOI] [PubMed] [Google Scholar]
- 51.Drummond SPA, Paulus MP, Tapert SF. Effects of two nights sleep deprivation and two nights recovery sleep on response inhibition. J Sleep Res. 2006;15(3):261–265. doi: 10.1111/j.1365-2869.2006.00535.x [DOI] [PubMed] [Google Scholar]
- 52.Akerstedt T Shift work and disturbed sleep/wakefulness. Occup Med. 2003;53(2):89–94. [DOI] [PubMed] [Google Scholar]
- 53.Angerer P, Schmook R, Elfantel I, Li J. Night Work and the Risk of Depression. Dtsch Arzteblatt Int. 2017;114(24):404–411. doi: 10.3238/arztebl.2017.0404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Leproult R, Holmbäck U, Van Cauter E. Circadian misalignment augments markers of insulin resistance and inflammation, independently of sleep loss. Diabetes. 2014;63(6):1860–1869. doi: 10.2337/db13-1546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Edley SM, Graybiel AM. The afferent and efferent connections of the feline nucleus tegmenti pedunculopontinus, pars compacta. J Comp Neurol. 1983;217(2):187–215. [DOI] [PubMed] [Google Scholar]
- 56.Rye DB, Saper CB, Lee HJ, Wainer BH. Pedunculopontine tegmental nucleus of the rat: cytoarchitecture, cytochemistry, and some extrapyramidal connections of the mesopontine tegmentum. J Comp Neurol. 1987;259(4):483–528. [DOI] [PubMed] [Google Scholar]
- 57.Saper CB. Staying awake for dinner: hypothalamic integration of sleep, feeding, and circadian rhythms. Prog Brain Res. 2006;153:243–252. [DOI] [PubMed] [Google Scholar]
- 58.Saper CB, Chou TC, Scammell TE. The sleep switch: hypothalamic control of sleep and wakefulness. Trends Neurosci. 2001;24(12):726–731. [DOI] [PubMed] [Google Scholar]
- 59.Barrett J, Lack L, Morris M. The sleep-evoked decrease of body temperature. Sleep. 1993;16(2):93–99. [PubMed] [Google Scholar]
- 60.Bootzin RR, Epstein D, Wood JM. Stimulus control instructions In: Case Studies in Insomnia. Springer; 1991:19–28. http://link.springer.com/chapter/10.1007/978-1-4757-9586-8_2. [Google Scholar]
- 61.Harris J, Lack L, Kemp K, Wright H, Bootzin R. A randomized controlled trial of intensive sleep retraining (ISR): a brief conditioning treatment for chronic insomnia. Sleep. 2012;35(1):49–60. doi: 10.5665/sleep.1584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Trauer JM, Qian MY, Doyle JS, Rajaratnam SMW, Cunnington D. Cognitive Behavioral Therapy for Chronic Insomnia: A Systematic Review and Meta-analysis. Ann Intern Med. 2015;163(3):191–204. doi: 10.7326/M14-2841 [DOI] [PubMed] [Google Scholar]
- 63.Bhattacharyya N. Sleep and health implications of snoring: a populational analysis. The Laryngoscope. 2015;125(10):2413–2416. [DOI] [PubMed] [Google Scholar]
- 64.Halász P, Kundra O, Rajna P, Pál I, Vargha M. Micro-arousals during nocturnal sleep. Acta Physiol Acad Sci Hung. 1979;54(1):1–12. [PubMed] [Google Scholar]
- 65.Martin SE, Engleman HM, Deary IJ, Douglas NJ. The effect of sleep fragmentation on daytime function. Am J Respir Crit Care Med. 1996;153(4):1328–1332. doi: 10.1164/ajrccm.153.4.8616562 [DOI] [PubMed] [Google Scholar]
- 66.Bursztyn M, Mekler J, Ben-Ishay D. The siesta and ambulatory blood pressure: is waking up the same in the morning and afternoon? J Hum Hypertens. 1996;10(5):287–292. [PubMed] [Google Scholar]
- 67.Naska A, Oikonomou E, Trichopoulou A, Psaltopoulou T, Trichopoulos D. Siesta in Healthy Adults and Coronary Mortality in the General Population. Arch Intern Med. 2007;167(3):296–301. doi: 10.1001/archinte.167.3.296 [DOI] [PubMed] [Google Scholar]
- 68.Mantua J, Spencer RMC. The interactive effects of nocturnal sleep and daytime naps in relation to serum C-reactive protein. Sleep Med. 2015;16(10):1213–1216. doi: 10.1016/j.sleep.2015.06.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Edinger JD, Wohlgemuth WK, Radtke RA, Marsh GR, Quillian RE. Cognitive Behavioral Therapy for Treatment of Chronic Primary Insomnia: A Randomized Controlled Trial. JAMA. 2001;285(14):1856–1864. doi: 10.1001/jama.285.14.1856 [DOI] [PubMed] [Google Scholar]
- 70.Gu F, Han J, Laden F, et al. Total and Cause-Specific Mortality of U.S. Nurses Working Rotating Night Shifts. Am J Prev Med. 2015;48(3):241–252. doi: 10.1016/j.amepre.2014.10.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ebrahim IO, Shapiro CM, Williams AJ, Fenwick PB. Alcohol and Sleep I: Effects on Normal Sleep. Alcohol Clin Exp Res. 2013;37(4):539–549. doi: 10.1111/acer.12006 [DOI] [PubMed] [Google Scholar]
- 72.Scanlan MF, Roebuck T, Little PJ, Redman JR, Naughton MT. Effect of moderate alcohol upon obstructive sleep apnoea. Eur Respir J. 2000;16(5):909–913. [DOI] [PubMed] [Google Scholar]
- 73.Ohayon MM. Prevalence and Correlates of Nonrestorative Sleep Complaints. Arch Intern Med. 2005;165(1):35–41. doi: 10.1001/archinte.165.1.35 [DOI] [PubMed] [Google Scholar]
- 74.Urponen H, Vuori I, Hasan J, Partinen M. Self-evaluations of factors promoting and disturbing sleep: An epidemiological survey in Finland. Soc Sci Med. 1988;26(4):443–450. doi: 10.1016/0277-9536(88)90313-9 [DOI] [PubMed] [Google Scholar]
- 75.National Sleep Foundation. Best Temperature for Sleep. Sleep.Org https://sleep.org/articles/temperature-for-sleep/ Accessed January 26, 2018. [Google Scholar]
- 76.Campbell SS. Duration and Placement of Sleep in a “Disentrained” Environment. Psychophysiology. 1984;21(1):106–113. doi: 10.1111/j.1469-8986.1984.tb02327.x [DOI] [PubMed] [Google Scholar]
- 77.Tanaka H, Shirakawa S. Sleep health, lifestyle and mental health in the Japanese elderly. J Psychosom Res. 2004;56(5):465–477. doi: 10.1016/j.jpsychores.2004.03.002 [DOI] [PubMed] [Google Scholar]
- 78.Basner M, Dinges DF. Dubious bargain: trading sleep for Leno and Letterman. Sleep. 2009;32(6):747–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Basner M, Spaeth AM, Dinges DF. Sociodemographic Characteristics and Waking Activities and their Role in the Timing and Duration of Sleep. Sleep. 2014;37(12):1889–1906. doi: 10.5665/sleep.4238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Exelmans L, Van den Bulck J. Binge Viewing, Sleep, and the Role of Pre-Sleep Arousal. J Clin Sleep Med. 2017;13(08):1001–1008. doi: 10.5664/jcsm.6704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Youngstedt SD, O’Connor PJ, Dishman RK. The effects of acute exercise on sleep: a quantitative synthesis. Sleep. 1997;20(3):203–214. [DOI] [PubMed] [Google Scholar]
- 82.Buman MP, Phillips BA, Youngstedt SD, Kline CE, Hirshkowitz M. Does nighttime exercise really disturb sleep? Results from the 2013 National Sleep Foundation Sleep in America Poll. Sleep Med. 2014;15(7):755–761. doi: 10.1016/j.sleep.2014.01.008 [DOI] [PubMed] [Google Scholar]
- 83.O’Connor PJ, Breus MJ, Youngstedt SD. Exercise-induced increase in core temperature does not disrupt a behavioral measure of sleep. Physiol Behav. 1998;64(3):213–217. [DOI] [PubMed] [Google Scholar]
- 84.Yoshida H, Ishikawa T, Shiraishi F, Kobayashi T. Effects of the timing of exercise on the night sleep. Psychiatry Clin Neurosci. 1998;52(2):139–140. doi: 10.1111/j.1440-1819.1998.tb00994.x [DOI] [PubMed] [Google Scholar]
- 85.Strecker RE, Morairty S, Thakkar MM, et al. Adenosinergic modulation of basal forebrain and preoptic/anterior hypothalamic neuronal activity in the control of behavioral state. Behav Brain Res. 2000;115(2):183–204. [DOI] [PubMed] [Google Scholar]
- 86.Thakkar J, Redfern J, Thiagalingam A, Chow CK. Patterns, predictors and effects of texting intervention on physical activity in CHD - insights from the TEXT ME randomized clinical trial. Eur J Prev Cardiol. 2016;23(17):1894–1902. doi: 10.1177/2047487316664190 [DOI] [PubMed] [Google Scholar]
- 87.Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373–377. doi: 10.1126/science.1241224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Schredl M, Reinhard I. Dream recall, dream length, and sleep duration: state or trait factor. Percept Mot Skills. 2008;106(2):633–636. doi: 10.2466/pms.106.2.633-636 [DOI] [PubMed] [Google Scholar]
- 89.Beaulieu-Prévost D, Zadra A. Absorption, psychological boundaries and attitude towards dreams as correlates of dream recall: two decades of research seen through a meta-analysis. J Sleep Res. 2007;16(1):51–59. doi: 10.1111/j.1365-2869.2007.00572.x [DOI] [PubMed] [Google Scholar]
- 90.Scarpelli S, Marzano C, D’Atri A, Gorgoni M, Ferrara M, De Gennaro L. State- or trait-like individual differences in dream recall: preliminary findings from a within-subjects study of multiple nap REM sleep awakenings. Front Psychol. 2015;6:928. doi: 10.3389/fpsyg.2015.00928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Fishbein M, Ajzen I. Predicting and Changing Behavior. New York, NY: Psychology Press; 2009. [Google Scholar]
- 92.Stevens MM, Olson AL, Gaffney CA, Tosteson TD, Mott LA, Starr P. A pediatric, practice-based, randomized trial of drinking and smoking prevention and bicycle helmet, gun, and seatbelt safety promotion. Pediatrics. 2002;109(3):490–497. [DOI] [PubMed] [Google Scholar]
- 93.Richardson AK, Green M, Xiao H, Sokol N, Vallone D. Evidence for truth®: the young adult response to a youth-focused anti-smoking media campaign. Am J Prev Med. 2010;39(6):500–506. doi: 10.1016/j.amepre.2010.08.007 [DOI] [PubMed] [Google Scholar]