Abstract
Community Health Centers (CHCs) target medically underserved communities and expanded by 70% in the last decade. We know little, however, about mental health services at CHCs. We analyzed data from 2006 to 2015 and determined county-level drivers of these services. Mental health patients at CHCs fall from 2006 to 2007 but then rise consistently from 2007 to 2015. Counties with fewer physicians, greater percent insured and greater percent white population show faster growth in mental health services. Increases in mental health services at CHCs outpace general CHC growth and reflect federal efforts to integrate behavioral health care into primary care.
Keywords: Community Health Centers, mental health services, Affordable Care Act, Medicaid, medically underserved communities
Introduction
Federally Qualified Health Centers provide primary health care to low-income, historically disadvantaged communities and serve all patients regardless of ability to pay (Druss et al., 2006). These centers, referred to as Community Health Centers (CHCs), currently serve over 27 million Americans and act as a key safety net provider (HRSA, 2018a). The patient population at CHCs consists primarily of persons with Medicaid (38.5% of total) or no health insurance (37.5% of total) (HRSA, 2010). The reach of CHCs has expanded by an unprecedented 70% in the last decade (Lo Sasso & Byck, 2010) (Rosenbaum et al., 2017). In addition, several provisions of the Affordable Care Act (ACA), as well as generous federal funding, intended to further increase the scope and reach of CHCs.
Mental disorders account for a large share of the overall global burden of disease (Murray et al., 2015) but often remain untreated. A disproportionate fraction of the 43 million Americans with diagnosable mental disorder use either Medicaid or have no health insurance (NIMH, 2017). However, only one in five uninsured persons with a serious mental disorder seek mental health care (Garfield, Zuvekas, Lave, & Donohue, 2011).
CHC expansion in medically underserved areas over the last decade holds the potential to increase help-seeking for primary mental health care. Over three-quarters of CHCs provide mental health services (HRSA, 2018). This circumstance raises the possibility that Medicaid or uninsured persons will seek these services in their local area. Geographic proximity to sources of care serves as an important but overlooked determinant of receiving mental health care (Allard, Tolman, & Rosen, 2003; Fortney, Rost, Zhang, & Warren, 1999; Lindrooth, Lo Sasso, & Lurie, 2006). Distance increases travel time and transportation difficulties, as well as increasing feelings of estrangement and of being unwelcome in places farther removed from one’s local environment. For this reason, the creation of new CHCs, and the expansion of current CHCs to include mental health care, may increase the volume of patients seeking primary care mental health services.
The literature includes no recent report of trends in primary care mental health services provided at CHCs (Druss et al., 2006; Wells, Morrissey, Lee, & Radford, 2010). An updated report on CHCs should interest policy scholars for two reasons. First, since 2011 CHCs received over $11 billion in federal funds. This large financial outlay warrants evaluation by health policy scholars. Second, retrieval of primary mental health care data in specific regions could inform subsequent research on whether increases in supply of primary care benefit the overall system of care—including costly but often unnecessary psychiatric emergency department (ED) visits. Initial evaluations from 2006 to 2011, for instance, indicate that expansion of care provided at CHCs corresponds with fewer psychiatric-related ED visits (Bruckner, Singh, Yoon, Chakravarthy & Snowden, in press), as well as a reduced risk of psychiatric-related revisits to the ED (Singh, Chakravarthy, Yoon, Snowden, & Bruckner, in press). Researchers, therefore, may benefit from a comprehensive assessment of the evolution over time of mental health services provided at CHCs.
We describe trends in mental health services offered at over 1,300 CHCs. We examine 2006 to 2015, a dynamic period which spans the Mental Health Parity and Addiction Equity Act (MHPAEA) and the Affordable Care Act (ACA). In addition to describing overall trends, we aggregate mental health visits by county and examine whether county-level demographic and health care factors correspond with growth in mental health services offered at CHCs.
Methods
Variables and Data:
We retrieved, via a Freedom of Information Act Request (#17F167), data on all CHCs from 2006 to 2015 from the Uniform Data System (UDS) (HRSA, 2018b). 2015 represents the last year with CHC data available at the time of our request. The federal government requires UDS reports as a condition of receiving federal funding. The UDS includes patient and encounter-level summaries of the volume and type of mental health services offered, by each CHC that receives primary care grant funding from section 330 of the Public Health Service Act (Consolidated Health Centers Act, 2018). UDS uses consistent methodology and forms over this ten year period in collecting the mental health variables of interest.
Mental health diagnoses contained in the UDS reports include depression and other mood disorders, anxiety disorders including posttraumatic stress disorder, attention deficit and disruptive behavior disorders, and other mental disorders excluding drug or alcohol dependence. For each CHC from 2006 to 2011, we summed the patients with these primary diagnoses to arrive at the total number of patients seen for a mental disorder. In addition, we summed encounters with these primary diagnoses to yield the total number of visits for mental disorder at that CHC. Next, we aggregated these values to the county level to permit linkage (by county ID and year) to socio-demographic and health care supply variables in other datasets.
Beginning in 2012, the UDS reports include all mental health diagnoses even if they do not reflect the primary diagnosis of the patient (Bureau of Primary Health Care, 2012). Given this coding change, the number of mental health patients from 2012 to 2015 appears inflated relative to 2011 figures. For this reason, we cannot directly compare the number of mental health patients seen before 2012 to those seen from 2012 through 2015. We therefore analyzed these two periods separately.
We linked county-year data from five additional sources. We used population estimates from the US Census to derive two measures of CHC mental health service penetration: mental health patients seen per 1,000 county population, and mental health visits per 1,000 county population (United States Census Bureau, 2016; United States Census Bureau, 2018). The US Census also contains annual estimates of race/ethnicity composition. We retrieved from the US Census the percent of the county population that identifies as white, non-Hispanic African American, and Hispanic (United States Census Bureau, 2016; United States Census Bureau, 2018).
Given that CHCs tend to serve economically disadvantaged communities, we included as an independent variable the percent of the population living below the poverty line. The Small Area Income and Poverty Estimates Program provides this dataset (SAIPE, 2018). In addition, relatively low health care supply may influence CHC expansion. To gauge supply, we retrieved physician concentration information from the Area Health Resource Files (AHRF, 2018). We also acquired information on the percent of the population without health insurance from the Small Area Health Insurance Estimates Program (SAHIE, 2018). Lastly, we included an indicator variable for metropolitan county (vs. nonmetropolitan) using the National Center for Health Statistics 2013 classification scheme (NCHS, 2017). We reasoned that the pace of CHC growth may occur unevenly across rural (nonmetropolitan) and urban (metropolitan) counties.
Analysis
We first plotted the annual percent change in mental health patients and overall patients seen at CHCs over time. We also ranked counties based on the rate of increase (from 2006 to 2015) and in the absolute level of increase in mental health service capacity. Next, we performed a longitudinal linear mixed effects regression analysis of county-level CHC growth. We specified total mental health visits at. CHCs per 1,000 population in a county as the dependent We analyzed continuous outcomes using ordinary-least-squares (OLS) mixed effect regression. Independent variables at the county level included percent white, percent non-Hispanic African American, percent Hispanic, percent with health insurance, percent in poverty, physicians per 1,000 population, and metropolitan designation (with nonmetropolitan designation as referent) (NCHS, 2017).
For our exploration, the mixed effects model estimates the parameters of interest from variation both across counties (within a year) and across years (within a county). The mixed model also flexibly allows each county to have their own starting level of CHC mental health resources (i.e., random intercept). In addition, we included year “fixed effects” to control for trends over time in CHC growth that occur across the entire nation. We did not include random slope as likelihood ratio tests indicated no significant difference in results upon adding random slope to the simpler model with random intercept only. We specified the “cluster” option of standard errors (SE) given the strong correlation of annual observations within each county. Previous literature in mental health services uses this approach (Cook, Zuvekas, Chen, Progovac, & Lincoln, 2017; Bower et al., 2013). As noted earlier, the UDS coding shift in mental health diagnoses in 2012 necessitates separate analyses for the periods 2006–11 and 2012–15. The latter time period occurs after the enactment of ACA, which allows us to assess whether the ACA Affected county-level drivers of mental health services offered at CHCs. We performed all statistical analyses in Stata SE 14.2 (Statacorp, 2015).
Results
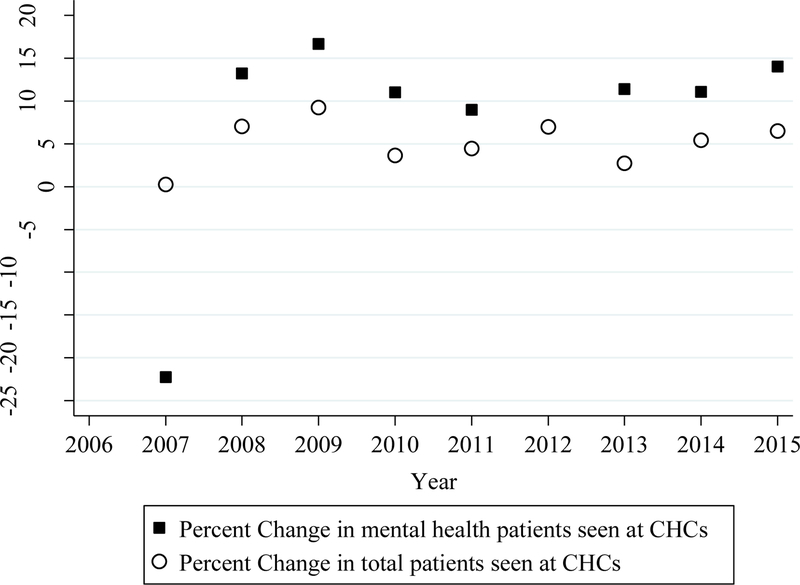
From 2006 to 2015, the total number of patients seen at CHCs rises from 17.8 to 27.8 million. The annual increase in overall patients seen ranges from 0.02% to 9.2% (Figure 1), with a mean of 5.1%. Among patients seen at CHCs with a mental disorder diagnosis, visits fall from 2006 to 2007 but then rise between 8 to 14% per year from 2007 to 2015 (note that we omit 2012 due to the change in UDS coding of mental health diagnoses in 2012). The average annual percent increase in mental health patients outpaces the general growth in overall patients at CHCs.
Figure 1.
Annual percent change in patients seen at Community Health Centers, 2006 to 2015. Total patients shown with hollow circles; mental health patients shown in shaded squares. Footnote: 2012 data for change in mental health visits are unavailable due to coding differences between 2011 and 2012 mental health visit data.
The rise in mental health visits at CHCs occurs via two mechanisms. First, counties with no CHCs receive funding for the creation of new centers. Whereas 835 counties in 2006 offered mental health services at CHCs, the number of counties with such services grew to 995 in 2015. Second, CHCs initially offering mental health services dramatically expand their capacity. Table 1 lists ten counties with the largest absolute gains in mental health visits at FHQCs from 2006 to 2015. Heavily populated counties tend to show the largest absolute gains, although Santa Fe County, New Mexico and Manatee County, Florida serve as two exceptions. Table 2 lists ten counties with the largest percent increase over time in mental health visits at CHCs, among counties reporting at least 100 mental health visits in 2006. These counties range dramatically in socioeconomic characteristics, with some showing relatively greater affluence (e.g., Clackamas County, Oregon and Marathon County, Wisconsin).
Table 1.
Descriptive Characteristics of the ten counties with the largest absolute gains in mental health visits at Community Health Centers, 2006 to 2015.
| State | County | Total population (2015) | Percent insured (2015) | Percent poverty (2015) | Difference in mental health visits (2015–2006) |
|---|---|---|---|---|---|
| California | Los Angeles County | 10,112,255 | 87.5 | 16.7 | 382,447 |
| New York | New York County | 1,641,168 | 92.1 | 17.6 | 348,285 |
| California | San Diego County | 3,290,245 | 90.5 | 13.9 | 309,453 |
| Florida | Hillsborough County | 1,347,077 | 85.3 | 15.8 | 264,402 |
| Washington | King County | 2,114,256 | 93.5 | 9.8 | 258,410 |
| New York | Bronx County | 1,449,196 | 88.9 | 30.3 | 241,769 |
| New Mexico | Santa Fe County | 147,708 | 85.1 | 13.1 | 230,955 |
| Florida | Miami-Dade County | 2,692,593 | 78.8 | 20.0 | 215,283 |
| Florida | Manatee County | 363,110 | 81.9 | 14.8 | 196,468 |
| Massachusetts | Suffolk County | 776,688 | 95.4 | 19.8 | 192,239 |
Table 2.
Descriptive Characteristics of the ten counties with the largest percentage growth in mental health visits at Community Health Centers, 2006 to 2015.
| State | County | Total population (2015) | Percent insured (2015) | Percent poverty (2015) | Percent change in mental health visits [(2015–2006)/2006] |
|---|---|---|---|---|---|
| Louisiana | Jefferson Parish | 435,555 | 84.5 | 16.3 | 138.89 |
| Wisconsin | Marathon County | 135,782 | 93.8 | 9.5 | 136.04 |
| California | Yolo County | 212,202 | 92.5 | 17.5 | 115.80 |
| Oregon | Clackamas County | 401,150 | 93.8 | 9.4 | 113.42 |
| Oregon | Benton County | 88,271 | 92.9 | 18.3 | 103.17 |
| Ohio | Mahoning County | 231,767 | 92.4 | 16.8 | 70.46 |
| Ohio | Trumbull County | 203,631 | 91.6 | 17.6 | 70.46 |
| Tennessee | Loudon County | 50,978 | 86.5 | 13.5 | 48.53 |
| Tennessee | Monroe County | 45,677 | 85.7 | 18.6 | 48.53 |
| Florida | Brevard County | 567,934 | 86.5 | 13.4 | 43.67 |
Footnote: We analyzed only counties with at least 100 mental health visits in 2006 (N = 1,814).
Results from the mixed effects model indicate that, from 2006 to 2011, several county-level factors correspond with CHC growth in mental health visits (Table 3). Counties with fewer physicians per capita, as well as counties with a greater fraction white, show more rapid growth in mental health visits at CHCs. The coefficient for fraction poverty also indicates that high-poverty counties tend to show more rapid growth in mental health visits, although the result does not reach conventional levels of statistical detection. In addition, non-metropolitan counties experience greater growth in mental health visits at CHCs than do metropolitan (i.e., urban) counties.
Table 3.
County-level regression results for years 2006–11 & 2012–2015 predicting growth in mental health visits at Community Health Centers.
| 2006–2011 | 2012–2015 | |||
|---|---|---|---|---|
| Covariates | Coefficient | Standard Error | Coefficient | Standard Error |
| Percent white | 1.28** | 0.49 | 4 26*** | 1.55 |
| Percent African American | −20.18 | 54.97 | 248.19 | 174.19 |
| Percent Hispanic | 63.08 | 58.25 | 263.84 | 183.28 |
| Percent insured | −0.17 | 0.65 | 6.86*** | 2.06 |
| Percent in poverty | 1.15* | 0.69 | 6.68*** | 1.95 |
| Physicians per 1000 population | ‒8.31*** | 3.13 | −40.06*** | 9.56 |
| Metropolitan Area (reference = nonmetropolitan) | −74 54*** | 11.48 | −178.09*** | 35.09 |
| Year indicators (fixed effects) | ||||
| 2006 | Reference group | |||
| 2007 | −21.71*** | 4.48 | -- | -- |
| 2008 | 15.40*** | 4.43 | -- | -- |
| 2009 | −1.42 | 4.42 | -- | -- |
| 2010 | 4.22 | 4.52 | -- | -- |
| 2011 | 8.48* | 4.61 | -- | -- |
| 2012 | -- | -- | Reference group | |
| 2013 | -- | -- | 32.14*** | 8.02 |
| 2014 | -- | -- | 42 70*** | 10.73 |
| 2015 | -- | -- | 61.81*** | 14.84 |
p value < 0.1
p value < 0.05
p value < 0.01
Inference from the regression results for the period after ACA enactment (Table 3) coheres with that of 2006–11 save for two notable exceptions. First, the share of persons in a county with health insurance now moves positively with mental health visits (coef: 6.86, SE= 2.06, p =0.001). Second, the positive association between county-level poverty and mental health visits at CHCs reaches statistical detection (coef: 6.68, SE= 1.95, p< 0.001). For both time periods we do not observe an association between share of racial/ethnic minority population and mental health visits at CHCs.
To give the reader a sense of the magnitude of our results, we calculated (for 2012–2015 results) the number of mental health visits at CHCs statistically attributable to county-level increases in rates of health insurance coverage. A county’s level of health insurance coverage increased from 2012 to 2015 by over seven percent. Linear predictions from our mixed effects model (using Stata’s ‘margins’ command, all other covariates held constant at their means) suggest a gain of 690 mental health visits at CHCs (per 100,000 population) with every unit increase in the percentage of insured population from 2012 to 2015. Application of this increase to the base level of visits in 2012 and the total population of counties with a CHC indicates approximately 900,000 additional mental health visits in 2015 at CHCs statistically attributable to a seven percent rise in health insurance coverage.
Discussion
A disproportionate share of persons with an untreated mental disorder lives in underserved counties where CHCs expanded. We set out to describe trends in the volume of mental health services provided at over 1,337 CHCs in 995 US counties. Our analyses reveal three novel findings. First, from 2007 to 2015, mental health service capacity at CHCs grows each year. Second, the rise in mental health service capacity outpaces the general rise in patients seen at CHCs. Third, both supply-side and sociodemographic factors at the county level correspond with CHC growth in mental health services. The county-level findings indicate that, especially after the ACA, an increase in Medicaid enrollments may have resulted in an influx of mental health visits at CHCs.
Given the lack of recent literature in this area, we did not have strong a priori expectations about the steady increase in CHC mental health services over this time period. We speculate that several factors contributed to this rapid rise. First, the US Health Resources and Services Administration provided Behavioral Health Integration grant awards to certain CHCs to expand access to mental health and substance abuse services (HRSA, 2014). Second, the Mental Health Parity and Addiction Equity Act (MHPAEA), passed in 2008, greatly enhanced the ability of persons with private health insurance plans to receive comprehensive mental health care (Frank, Beronio, & Glied, 2014). The ACA further required that MHPAEA apply to all plans offered in state-based insurance exchange programs, as well as to the newly Medicaid eligible adults with incomes up to 138% of the federal poverty line (Busch, 2012). To the extent that persons newly covered under these plans visited CHCs, these factors may have also contributed to the sustained rise in CHC mental health services.
Another factor that may contribute to the rise in mental health services involves CHCs’ increasing efforts to organizeactivities around the concept of the patient-centered medical home (Neuhausen, Grumbach, Bazemore, & Phillips, 2012). This concept created payment reform incentives (financially supported by state and federal Medicaid initiatives including the ACA) to treat chronic conditions comprehensively and to enhance coordination of care (Croft & Parish, 2013). The ACA specified that, in order for organizations to meet the payment incentive for designation as a “medical home,” they must provide care for at least one serious and persistent mental health condition (Kaiser Family Foundation, 2012). Given that Medicaid provides the largest source of financing for CHCs, new financial incentives to treat mental disorders among Medicaid patients may have accounted for the rise in CHC mental health services.
Results from the county-level regression analyses indicate that both supply-side and socio-demographic factors vary with mental health services growth at CHCs. The observation that low physician concentration correlates with growth in mental health services coheres with the notion that CHCs continue to focus on medically underserved communities. In addition, the association of fraction white with mental health visits at CHCs may reflect greater prevalence of help-seeking for mental health among white relative to Hispanic and African American populations. This observation may portend an exacerbation of racial/ethnic disparities in access to mental health care (Snowden, 2001). If others replicate our results, policymakers may want to consider novel strategies to expand mental health services and outreach to racial/ethnic minority populations in low-income communities.
Non-metropolitan counties exhibit substantially lower concentrations of psychiatrists, psychologists and psychiatric nurse practitioners relative to metropolitan areas (Andrilla, Patterson, Garberson, Coulthard, & Larson, 2018). Non-metropolitan areas also exhibit markedly higher rates of suicides compared to metropolitan regions (Kegler, Stone, & Holland, 2017). Rapid expansion of mental health services at CHCs may serve to reduce these regional disparities in mental health care supply as well as adverse health outcomes. We encourage future research to examine whether expansion of mental health services at CHCs corresponds with a decline in suicidal ideation, self-harm and suicide completion in rural geographies in the US.
After 2011, both county-level poverty and health insurance rates move positively with mental health services at CHCs. Expansion of Medicaid in low-income communities, following the ACA, may account for these findings. The ACA demonstrably reduced the percent uninsured and increased Medicaid enrollments among low-income Americans (Buchmueller, Levinson, Levy, & Wolfe, 2016; Vistnes & Cohen, 2016). Medicaid’s substantial financing for CHCs, combined with a variety of policy initiatives since 2010 (noted above), may contribute to the rise in CHC mental health services especially in counties which rapidly expanded Medicaid coverage. This speculative explanation requires further refinement and testing using other datasets with information on individual’s health insurance type and use of specific services at CHCs.
Our study permits estimation of associations between county variables but does not permit causal inference. We recommend future work to identify causes underlying the uneven regional growth in CHC mental health services especially after the ACA. In addition, we caution the reader against drawing inferences about individual help-seeking patterns from our county-level data. We, rather, view our work as informing policy efforts to redress regional disparities in access to mental health services. Use of the county as the geographic unit may also mask important local-area variation in terms of which communities access CHCs (Ko & Ponce, 2013).
Garfield and colleagues in 2011 estimated that full implementation of the ACA would result in an additional 1.15 million new mental health service users (Garfield et al., 2011). They reasoned that most of these gains would occur through Medicaid expansion given that almost a quarter of nonelderly adult Medicaid enrollees have a mental disorder. Our results support this general prediction, although we caution against using the CHC data to directly estimate the total number of new patients. After 2011, the CHC data report mental health visits regardless of the nature of the primary diagnosis, such that persons with more than one mental health condition could be counted twice. For this reason, the CHC values after 2011 do not directly correspond with a total number of new mental health services users.
The literature finds that CHCs generally provide high-quality, low-cost care to medically underserved populations (Goldman, Chu, Tran, Romano, & Stafford, 2012; Laiteerapong et al., 2014; Regan, Schempf, Yoon, & Politzer, 2003; Starfield et al., 1994). CHC growth also corresponds with fewer psychiatric ED visits and lower risk of repeat ED visits (Bruckner, Singh, Yoon, Chakravarthy & Snowden, in press; Singh, Chakravarthy, Yoon, Snowden, & Bruckner, in press). We know of no work, however, which evaluates the quality of mental health care delivered at CHCs. Scholars note that shortages in access to subspecialty care may adversely affect CHCs’ ability to effectively deliver integrated care especially among persons with severe mental illness (Merikangas, Bromet, & Druss, 2017). Nevertheless, beginning in 2014, as a condition of receiving federal funding CHCs must report the proportion of patients screened for clinical depression who also have a documented follow-up plan (HRSA, 2018b). This quality improvement measure represents an initial attempt to assess the population-level impact of mental health services delivered at CHCs. We also encourage other investigations regarding the extent to which CHCs provide mental health screening for primary care visits listed as a “physical health” visit. Given the dramatic shift over time in the US in the provision of mental health services by primary care physicians (relative to psychiatrists), such research could evaluate the consequences of this shift on effective provision of mental health care (Olfson, Kroenke, Wang, & Blanco, 2014).
Acknowledgments
1. Competing interests: All authors declare: no support from any organisation for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
3. Funding: This research is supported by a grant from the National Institutes of Mental Health (1R21MH110815–01A1)
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Disclosures of Conflicts of Interest: None for any author.
Ethical approval: This article does not contain any studies with human participants or animals performed by any of the authors.
Data sharing: The county-level datasets used for the analysis and the statistical code are available from the corresponding author:
Data Integrity: All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
References
- Allard SW, Tolman RM, & Rosen D (2003). Proximity to service providers and service utilization among welfare recipients: the interaction of place and race. J Policy Anal Manage, 22(4), 599–613. doi: 10.1002/pam.10157 [DOI] [PubMed] [Google Scholar]
- Andrilla CHA, Patterson DG, Garberson LA, Coulthard C, & Larson EH (2018). Geographic variation in the supply of selected behavioral health providers. American journal of preventive medicine, 54(6), S199–S207. [DOI] [PubMed] [Google Scholar]
- Area Health Resource Files (AHRF). (2018). County Level Data. Health Resources & Services Administration. Retrieved from https://data.hrsa.gov/data/download [Google Scholar]
- Bower P, Kontopantelis E, Sutton A, Kendrick T, Richards DA, Gilbody S, … & Meyer B (2013). Influence of initial severity of depression on effectiveness of low intensity interventions: meta-analysis of individual patient data. BMJ, 346, f540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruckner TA, Singh P, Yoon J, Chakravarthy B, & Snowden L (In press). Psychiatric Emergency Department Visits after Regional Expansion of Community Health Centers. Psychiatric Services. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmueller TC, Levinson ZM, Levy HG, & Wolfe BL (2016). Effect of the Affordable Care Act on Racial and Ethnic Disparities in Health Insurance Coverage. Am J Public Health, 106(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bureau of Primary Health Care. (2012). UDS Reporting Instructions for Health Centers. Retrieved from https://bphc.hrsa.gov/datareporting/reporting/2012udsmanual.pdf
- Busch SH (2012). Implications of the Mental Health Parity and Addiction Equity Act. Am J Psychiatry, 169(1), 1–3. doi: 10.1176/appi.ajp.2011.11101543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consolidated Health Centers Act. (2018). Section 330 of the Public Health Service Act. Retrieved from http://www.nachc.org/wp-content/uploads/2018/05/Section-330-statute-as-of-March-2018-Clean.pdf
- Cook BL, Zuvekas SH, Chen J, Progovac A, & Lincoln AK (2017). Assessing the individual, neighborhood, and policy predictors of disparities in mental health care. Medical Care Research and Review, 74(4), 404–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croft B, & Parish SL (2013). Care integration in the Patient Protection and Affordable Care Act: implications for behavioral health. Adm Policy Ment Health, 40(4), 258–263. doi: 10.1007/s10488-012-0405-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss BG, Bornemann T, Fry-Johnson YW, McCombs HG, Politzer RM, & Rust G (2006). Trends in Mental Health and Substance Abuse Services at the Nation’s Community Health Centers: 1998–2003. Am J Public Health, 96(10), 1779–1784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortney J, Rost K, Zhang M, & Warren J (1999). The impact of geographic accessibility on the intensity and quality of depression treatment. Med Care, 37(9), 884–893. [DOI] [PubMed] [Google Scholar]
- Frank RG, Beronio K, & Glied SA (2014). Behavioral health parity and the Affordable Care Act. J Soc Work Disabil Rehabil, 13(1–2), 31–43. doi: 10.1080/1536710X.2013.870512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfield RL, Zuvekas SH, Lave JR, & Donohue JM (2011). The impact of national health care reform on adults with severe mental disorders. Am J Psychiatry, 168(5), 486–494. doi: 10.1176/appi.ajp.2010.10060792 [DOI] [PubMed] [Google Scholar]
- Goldman LE, Chu PW, Tran H, Romano MJ, & Stafford RS (2012). Federally qualified health centers and private practice performance on ambulatory care measures. Am J Prev Med, 43(2), 142–149. doi: 10.1016/j.amepre.2012.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Resources & Services Administration (HRSA). (2010). Table 4: Selected Patient characteristics. 2010 National Data. Retrieved From https://bphc.hrsa.gov/uds/socioeconomic.aspx?year=2010&state=
- Health Resources & Services Administration (HRSA). (2018). Behavioral Health and Primary Care Integration. Retrieved from https://bphc.hrsa.gov/qualityimprovement/clinicalquality/behavioralhealth/index.html
- Health Resources & Services Administration (HRSA). (2018a). Health Center Data & Reporting. Retrieved from https://bphc.hrsa.gov/datareporting/index.html
- Health Resources & Services Administration (HRSA). (2018b). Uniform Data System (UDS) Resources. Retrieved from https://bphc.hrsa.gov/datareporting/reporting/index.html
- Health Resources & Services Administration (HRSA, 2014). HRSA awards $51.3 million in Affordable Care Act funding to support mental health and substance abuse treatment. Retrieved from https://www.hrsa.gov/about/news/press-releases/2014-11-06-behavioral-health.html
- Kaiser Family foundation. 2012. States Getting a Jump Start on Health Reform’s Medicaid Expansion. Retrieved from https://www.kff.org/health-reform/issue-brief/states-getting-a-jump-start-on-health/
- Kegler SR, Stone DM, & Holland KM (2017). Trends in suicide by level of urbanization—United States, 1999–2015. MMWR. Morbidity and mortality weekly report, 66(10), 270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ko M, & Ponce NA (2013). Community residential segregation and the local supply of federally qualified health centers. Health Serv Res, 48(1), 253–270. doi: 10.1111/j.1475-6773.2012.01444.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laiteerapong N, Kirby J, Gao Y, Yu TC, Sharma R, Nocon R, … Huang ES (2014). Health care utilization and receipt of preventive care for patients seen at federally funded health centers compared to other sites of primary care. Health Serv Res, 49(5), 1498–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindrooth RC, Lo Sasso AT, & Lurie IZ (2006). The effect of distance to provider on employee response to changes in mental health benefits. Health Econ, 15(10), 1133–1141. doi: 10.1002/hec.1118 [DOI] [PubMed] [Google Scholar]
- Lo Sasso AT, & Byck GR (2010). Funding growth drives community health center services. Health Aff (Millwood), 29(2), 289–296. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, Bromet EJ, & Druss BG (2017). Future Surveillance of Mental Disorders in the United States: Count People, Not Disorders. JAMA Psychiatry, 74(5), 431–432. doi: 10.1001/jamapsychiatry.2017.0109 [DOI] [PubMed] [Google Scholar]
- Murray CJ, Barber RM, Foreman KJ, Ozgoren AA, Abd-Allah F, Abera SF, … & Abu-Rmeileh NM (2015). Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. The Lancet, 386(10009), 2145–2191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Health Statistics (NCHS). (2017). 2013 Urban-Rural Classification Scheme for Counties. Retrieved from https://www.cdc.gov/nchs/data_access/urban_rural.htm
- National Institute of Mental Health (NIMH). (2017). Mental Health Information- Statistics. Retrieved from https://www.nimh.nih.gov/health/statistics/mental-illness.shtml
- Neuhausen K, Grumbach K, Bazemore A, & Phillips RL (2012). Integrating community health centers into organized delivery systems can improve access to subspecialty care. Health Aff (Millwood), 31(8), 1708–1716. doi: 10.1377/hlthaff.2011.1261 [DOI] [PubMed] [Google Scholar]
- Olfson M, Kroenke K, Wang S, & Blanco C (2014). Trends in office-based mental health care provided by psychiatrists and primary care physicians. J Clin Psychiatry, 75(3), 247–253. doi: 10.4088/JCP.13m08834 [DOI] [PubMed] [Google Scholar]
- Regan J, Schempf AH, Yoon J, & Politzer RM (2003). The role of federally funded health centers in serving the rural population. J Rural Health, 19(2), 117–124; discussion 115–116. [DOI] [PubMed] [Google Scholar]
- Rosenbaum S, Paradise J, Markus AR, Sharac J, Tran C, Reynolds D, & Shin P (2017). Community health centers: recent growth and the role of the ACA. Kaiser Family Foundation. Retrieved from https://hsrc.himmelfarb.gwu.edu/sphhs_policy_ggrchn/60/ [Google Scholar]
- Shin P, Rosenbaum S, & Paradise J (2012). Community Health Centers: The challenge of growing to meet the need for primary care in medically underserved communities. The Henry J. Kaiser Family Foundation. Retrieved from https://hsrc.himmelfarb.gwu.edu/cgi/viewcontent.cgi?referer=https://scholar.google.com/&httpsredir=1&article=1048&context=sphhspolicyggrchn [Google Scholar]
- Singh P, Chakravarthy B, Yoon J, Snowden L, & Bruckner TA (In press). Psychiatric-Related Revisits to the Emergency Department Following Rapid Expansion of Community Mental Health Services. Academic Emergency Medicine. [DOI] [PubMed] [Google Scholar]
- Small Area Health Insurance Estimates (SAHIE) Program. (2018). SAHIE Datasets. US Census Bureau. Retrieved from https://www.census.gov/programs-surveys/sahie/data/datasets.html
- Small Area Income and Poverty Estimates (SAIPE) Program. (2018). SAIPE Datasets. US Census Bureau. Retrieved from https://www.census.gov/programs-surveys/saipe/data/datasets.html
- Snowden LR (2001). Barriers to effective mental health services for African Americans. Ment Health Serv Res, 3(4), 181–187. [DOI] [PubMed] [Google Scholar]
- Starfield B, Powe NR, Weiner JR, Stuart M, Steinwachs D, Scholle SH, & Gerstenberger A (1994). Costs vs quality in different types of primary care settings. Jama, 272(24), 1903–1908. [PubMed] [Google Scholar]
- StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- United States Census Bureau. (2016). Intercensal Estimates of the Resident Population by Five-Year Age Groups, Sex, Race, and Hispanic Origin for Counties: April 1, 2000 to July 1, 2010. Retrieved from https://www.census.gov/data/datasets/time-series/demo/popest/intercensal-2000-2010-counties.html
- United States Census Bureau. (2018). Annual County Resident Population Estimates by Age, Sex, Race, and Hispanic Origin: April 1, 2010 to July 1, 2017. Retrieved from https://www.census.gov/data/datasets/2017/demo/popest/counties-detail.html
- Vistnes JP, & Cohen JW (2016). Gaining Coverage In 2014: New Estimates Of Marketplace And Medicaid Transitions. Health Aff (Millwood), 35(10), 1825–1829. [DOI] [PubMed] [Google Scholar]
- Wells R, Morrissey JP, Lee IH, & Radford A (2010). Trends in behavioral health care service provision by community health centers, 1998–2007. Psychiatr Serv, 61(8), 759–764. doi: 10.1176/ps.2010.61.8.759 [DOI] [PMC free article] [PubMed] [Google Scholar]