Abstract
Fear of cancer recurrence (FCR) is a common problem among cancer survivors and evidence- based interventions grounded in theoretical models are needed. Mindfulness-Based Cognitive Therapy (MBCT) is an evidence-based intervention for reducing health anxiety that could be useful to apply to FCR. However, there has only been one study of MBCT for FCR to date, and the theoretical rationale and practical application of MBCT for FCR has not been described. The purpose of this paper is to offer an evidence-based rationale for MBCT to treat FCR based on a health anxiety model; describe the process of adapting MBCT to target FCR; and present a case study of the adapted protocol for treating FCR in a young adult breast cancer survivor to illustrate its delivery, feasibility, acceptability, and associated changes in outcomes. Clinical implications and directions for future research are discussed.
Keywords: cancer, fear of recurrence, health anxiety, mindfulness, mindfulness-based cognitive therapy
The number of people who survive cancer is increasing as early detection and treatments improve. One of the greatest unmet needs among this growing population is a lack of skills for coping with fear of cancer recurrence (FCR), which involves anxiety about the realistic possibility that cancer will return or progress (Koch, Jansen, Brenner, & Arndt, 2013; Stanton, Rowland, & Ganz, 2015; Thewes et al., 2014). FCR is associated with poorer outcomes for survivors and their caregivers, and many oncology mental health providers find it difficult to treat (Kim, Carver, Spillers, Love-Ghaffari, & Kaw, 2012; Lebel, Tomei, Feldstain, Beattie, & McCallum, 2013; Hall, Mishel, & Germino, 2014; Armes et al., 2009; Thewes et al., 2014).
One approach with evidence to improve FCR is mindfulness training. Mindfulness is derived from Eastern meditation traditions and involves the self-regulation of attention toward present moment experiences with an attitude of openness and acceptance (Bishop et al., 2004). Mindfulness can be practiced formally during mindfulness meditation practices (e.g., the body scan, awareness of breath meditation) and informally by bringing mindful awareness to everyday activities (e.g., eating, walking). Mindfulness is different from meditation, which refers to a broad collection of mental training practices (Walsh & Shapiro, 2006). Mindfulness skills and cognitive-behavioral therapy (CBT) skills are the two most common approaches that show efficacy for treating FCR (Hall et al., 2018). Although several mindfulness interventions have been developed for cancer survivors (e.g., see Shaw, Sherman, Fitness, & Elder, 2018), Mindfulness-Based Cognitive Therapy (MBCT; Segal, Williams, & Teasale, 2012) may be uniquely beneficial because it is the only evidence-based, manualized protocol that explicitly integrates CBT and mindfulness training to help individuals change their relationship to the uncomfortable thoughts and physical symptoms that often accompany survivorship. There have been a handful of studies of MBCT in cancer but only one trial of MBCT for FCR, which supported the utility of MBCT as compared to usual care (Cillessen et al., 2018; Compen et al., 2018).
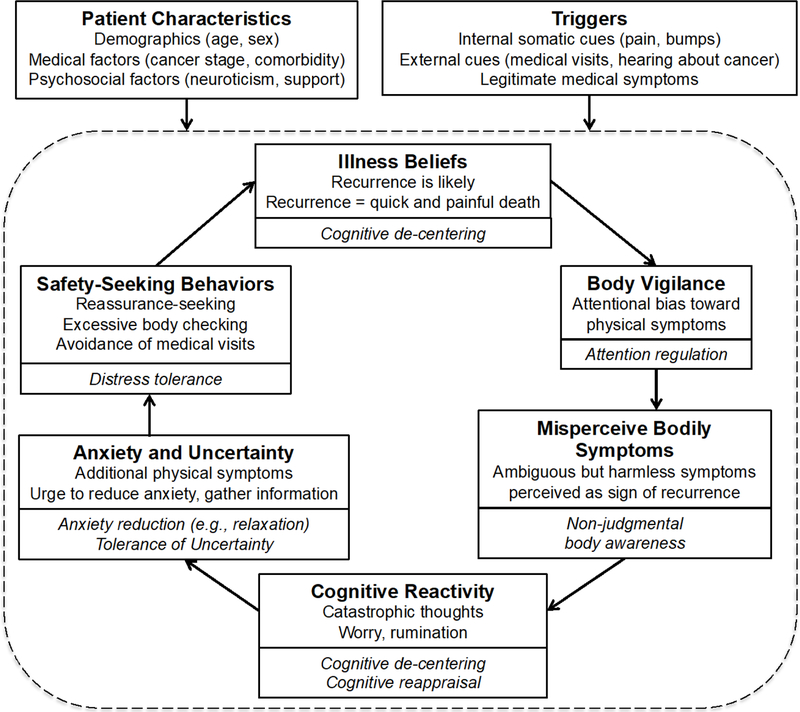
In addition, no research has detailed a rationale for why MBCT could treat FCR. The lack of a theoretical framework is a limitation in much of the research on mindfulness interventions in cancer (Hall et al., 2018; Shaw et al., 2018). Research on mindfulness and health anxiety might be leveraged to fill this theoretical gap (Fardell et al., 2016). Health anxiety involves a preoccupation with fears of having or acquiring an illness, which can occur among individuals with or without medical problems (e.g., hypochondriasis in DSM-IV, illness anxiety disorder in DSM-5; Asmundson, Abramowitz, Richter, & Whedon, 2010; Salkovskis, Rimes, Warwick, & Clark, 2002). Health anxiety and FCR share symptom overlap and are both conceptualized from a cognitive-behavioral perspective wherein interpretations of thoughts, physical sensations, and external events (e.g., news of cancer in the media) lead to anxiety and reassurance-seeking behaviors (e.g., medical visits, body-checking; Simonelli, Segal, & Duffey, 2017; Salkovskis & Warwick, 1986). Reassurance-seeking behaviors are negatively reinforced because they temporarily reduce anxiety symptoms, and thus perpetuate distress in the long- term. MBCT has evidence to treat health anxiety and theoretical models suggest that it does so by promoting non-judgmental awareness of body sensations and anxious thoughts, which minimizes reassurance-seeking behaviors (Surawy, McManus, Muse, & Williams, 2015; Lovas & Barsky, 2010; McManus, Suraway, Muse, Vazquez-Montes, & Williams, 2012). A model by Abramowitz, Deacon, and Valentiner (2007a) details health anxiety processes that are impacted by mindfulness training. This model is consistent with and integrates key components of FCR conceptualizations (Curran, Sharpe, & Butow, 2017; Simonelli et al., 2017), and thus may offer a rationale and testable hypotheses for the efficacy and mechanisms of MBCT for FCR. Figure 1 depicts this model with our adaptations for FCR and mindfulness treatment targets.
Figure 1.
Theoretical rationale for MBCT to reduce FCR symptoms.
Note. FCR components are indicated at the top of each box and mindfulness-related improvements are indicated at the bottom of each box (in italics). There is evidence to support that mindfulness training can improve attentional bias (Vago & Nakamura, 2011), body awareness (Silverstein, Brown, Roth, & Britton, 2011), cognitive decentering and cognitive reappraisal (Garland, Gaylord, & Fredrickson, 2011; Bieling et al., 2012), and tolerance of negative affective states (Lotan, Tanay, & Bernstein, 2013).
Although FCR and health anxiety share similarities, there are also important distinctions. FCR is specific to individuals with a cancer history while health anxiety can occur among individuals with or without a medical problem. In FCR, the fears are therefore realistic because individuals have a true, often serious, medical illness with the real possibility of recurrence, whereas in illness anxiety disorder, fears are often unrealistic and relate to medical conditions the individual does not actually have (Dinkel, Kremsreiter, Marten-Mittag, & Lahmann, 2014). In addition, cancer survivors are continually re-exposed to external triggers as a result of their ongoing care (e.g., follow-up scans and medical visits). In illness anxiety disorder, patients often do not need to undergo medical care that will trigger their symptoms. Physical symptoms resulting from cancer treatment further serve as internal triggers for cancer survivors. A study of over 300 cancer patients found that FCR was indeed distinct from health anxiety disorders, with a subgroup of patients who had pure, clinically significant FCR without a comorbid anxiety disorder (13%), fewer who had both (7%), and none with a health anxiety disorder only (Dinkel et al., 2014).
MBCT interventions for FCR treatments should therefore be adapted to target these unique aspects of survivorship, and these adaptations should be clearly described and justified (Shaw et al., 2018). For example, FCR treatments should consider that techniques for working with less realistic health anxieties, such as challenging the veracity of fearful cognitions (e.g., cognitive restructuring), may not be successful for survivors whose concerns are realistic and for whom a recurrence may indeed have elevated probability. MBCT teaches new ways of relating to thoughts rather than challenging the content of thoughts and thus may offer utility, though these techniques could be further targeted specifically to cancer-related concerns. MBCT should also focus on teaching patients skills for coping effectively with upcoming medical visits that are likely to be triggering, and emphasize skills for living a meaningful life despite the potential for cancer recurrence.
As a first step to guide future research and clinical work, we next discuss how we adapted MBCT to target FCR based on these considerations. We also include a case study to illustrate the delivery of the adapted intervention, since there are currently no practical guidelines for session-by-session delivery of MBCT to treat FCR and because detailed descriptions of intervention delivery are needed to promote replication in mindfulness research (Shaw et al., 2018).
Case Illustration
Adapted Intervention
The intervention was based on the Mindful Way Workbook (Teasdale, Williams, & Segal, 2014), an accompaniment to the original MBCT manualized protocol (Segal et al., 2002) that outlines the same treatment as the standard group intervention in a format appropriate for individual use. In its standard form, MBCT is an 8-week group program with 2-hour weekly sessions. MBCT includes a variety of formal mindfulness practices: the body scan, awareness of breath meditation, 3-minute breathing space, mindful yoga, and sitting meditation (i.e., awareness of the breath, body, sounds, and thoughts, including difficult thoughts; Segal et al.,2012). The instructions for these meditation practices are to notice the intended object of awareness with openness, noting when the mind wanders and gently guiding it back. Thus, these practices all provide training in focused attention, open awareness, and loving kindness (Germer, Siegal, & Fulton, 2013) using a variety of attentional strategies including focused, sustained, selective, and alternating attention (Sears, Tirch, & Denton, 2011). MBCT also emphasizes informal mindfulness practices and traditional CBT skills. These details are further described in the case illustration section below.
We took several steps to adapt the MBCT protocol to target FCR. Following the intake, the case was presented at the hospital’s Behavioral Medicine Program peer clinical supervision meeting to develop a treatment plan. We obtained input from clinical psychologists with expertise in psycho-oncology to inform the types of adaptations that were needed. We outlined these suggestions alongside an outline of the MBCT protocol and our theoretical model to determine how and where to integrate each suggestion. We ensured that the adapted components had empirical evidence of efficacy and addressed the unique aspects of FCR described above.
This process resulted in several adaptations. First, we expanded the psychoeducation component of MBCT by including psychoeducation about FCR, based on expert suggestions that this could help promote insight into FCR processes and build motivation for treatment. Psychoeducation was targeted for FCR rather than health anxiety by using the theoretical model depicted in Figure 1, which we adapted to include cancer-specific examples of illness beliefs, triggers, and the possibility of identifying legitimate concerns of recurrence. We included this information in Session 2 to because the traditional MBCT protocol includes psychoeducation about emotions in this session.
Second, we incorporated motivational interviewing techniques to reduce maladaptive reassurance-seeking behaviors (e.g., unnecessary medical visits, excessive body-checking). This adaptation was guided by our theoretical model, expert clinical recommendations, and empirical evidence for motivational interviewing to promote behavior change for cancer patients (Spencer & Wheeler, 2016). We included this content early (Session 3) to build motivation for learning and applying skills taught in later sessions. We also included a discussion of how these behaviors differ from the care team’s recommendations and how to communicate with providers to help promote the patient’s active engagement in her healthcare.
Third, we targeted existing MBCT cognitive techniques to FCR by working with the patient to identify feared thoughts about cancer and recurrence specifically. MBCT teaches patients how to relate differently to their thoughts (i.e., cognitive decentering) rather than change the content of thoughts directly (cognitive restructuring). We focused on applying mindfulness skills to cancer-specific thoughts and generating feared thoughts about recurrence to use during sitting meditation practices. To promote effective coping with triggers, we also planned for how to apply mindfulness and cognitive de-centering skills during moments of increased anxiety (e.g.,follow-up visits and scans, physical symptoms).
Lastly, grounded in a motivational interviewing and Acceptance and Commitment Therapy (ACT) approach, we incorporated values clarification exercises. The purpose of this adaptation was to help the patient emphasize meaning and purpose in life despite realistic concerns about potential recurrence. Values clarification work is not a standard part of MBCT but has been used effectively in ACT interventions for cancer survivors (Arch & Mitchell, 2015). We used the identified values to develop a behavioral plan for promoting well-being during survivorship, which included both valued living activities and guidelines for healthy lifestyle behaviors (e.g., exercise, diet). These were incorporated in Session 7 because this is the session of MBCT that focuses directly on behavioral interventions. Loving kindness meditation practices were also suggested for home practice in this session as a way to further build positive emotions and self-care in the context of the possibility of cancer recurrence.
Table 1 shows a summary of the adapted protocol. The intervention was delivered over eight weekly 50-minute sessions to align with the structure of standard outpatient individual therapy visits. Although the treatment was individualized and flexible, the protocol was outlined at the start of treatment and followed consistently throughout. Each session followed a consecutive chapter of the workbook. Sessions began with a 10-minute review of the previous week and homework, including problem-solving, clarification of key concepts, and discussion of mindfulness practice, followed by new didactic material and skills training. The only modification made to formal mindfulness practices was that mindfulness of thoughts was targeted to cancer- related worries. Following mindfulness teacher training guidelines (Crane, Kuyken, Hastings, Rothwell, & Williams, 2010), the therapist (CML) drew from a ten-year personal mindfulness practice, formal MBCT training experiences (including multiple workshops and direct supervised experience co-leading 10+ MBCT groups), and clinical experience delivering individual and group MBCT and CBT.
Table 1.
Treatment Outline of MBCT Adapted for FCR
| Session | Theme | Content | HW assigned |
|---|---|---|---|
| Intake 1 | -- | • Discussion of cancer experience • Psychosocial and medical history |
• Online web-link to begin mindfulness practice • Recommendation for the Mindful Way Workbook |
| Intake 2 | -- | • diagnostic interviewing and case formulation | • Online web-link for mindfulness practices |
| 1 (Ch. 5) | Automatic pilot | • psychoeducation • Mindfulness of external object |
Pages 21–25 (doing vs. being) • Mindful eating • Body scan • Routine activities |
| 2 (Ch. 6) | Another way of knowing | • “Walking down the street” exercise • CBT model of FCR • Mindfulness rationale |
• Body scan • Brief mindful breathing • Routine activities • Pleasant events calendar |
| 3 (Ch. 7) | Gathering the scattered mind | • Consequences of safety behaviors • Communicating with providers • Relating to unhelpful thoughts • 3-minute breathing space, regular |
• Mindful stretching • Mindful movement • 3-minute breathing space, regular • Unpleasant events calendar |
| 4 (Ch. 8) | Recognizing aversion | • Mindfully sitting with difficulties (exposure) • 3-minute breathing space, responsive |
• Sitting meditation or mindful movement • 3-minute breathing space regular and responsive • Mindful walking |
| 5 (Ch. 9) | Allowing | • Top 10 difficult thoughts or sensations • Mindfully sitting with difficulties (exposure) |
• Sitting with difficulties meditation • 3-minute breathing space regular and responsive |
| 6 (Ch. 10) | Seeing thoughts as thoughts | • Cognitive de-centering psychoeducation • Mindfulness of thoughts with cognitive de- centering (cancer-specific thoughts) |
• Mindfulness of thoughts • 3-minute breathing space, regular and responsive • Early warning system |
| 7 (Ch. 11) | Kindness in action | • Nourishing/draining exercise • Values identification • Healthy behaviors: valued action, coping strategies, survivorship lifestyle guidelines |
Loving kindness meditation practice • Sustainable mindfulness practice • 3m breathing space regular and responsive • Prepare action plan |
| 8 | Looking ahead | • Progress review • Lessons learned • Relapse prevention planning |
• Continued mindfulness practice of choice • Relapse prevention plan |
Note. Workbook chapters used for each session are specified in parentheses; adaptations made for FCR are italicized. Home practice recommendations followed workbook guidelines and typically consisted of 30-minutes of home practice per day using the audio recordings provided in the workbook. Two additional follow-up sessions (not shown here) focused on progress review and maintenance planning.
Patient Characteristics
The patient’s identifying information has been altered to protect confidentiality. “Hannah” was a breast cancer survivor in her early 30’s. She had been diagnosed with early stage, localized breast cancer and completed cancer treatment (double mastectomy, chemotherapy, radiation) approximately two years prior to seeking psychological treatment. She was married, highly educated, employed, and had a high level of social support. Hannah had no history of premorbid psychiatric problems or treatment. She denied a family history of known psychiatric problems but described her father as being anxious about health concerns (e.g., scanning his body for changes daily). She was referred to the behavioral medicine service in the outpatient psychiatry department at a large academic medical center by her primary care provider for anxiety about cancer recurrence. Specific presenting problems, which caused significant distress for Hannah and created tension in her relationships, included fearful beliefs about recurrence disproportionate to her actual risk (e.g., the chance of recurrence is 50/50); persistent worry about cancer recurrence and catastrophic interpretations of physical symptoms (e.g., changes in breathing reflect lung metastasis); and several reassurance-seeking behaviors including excessive body-checking (up to 20 times/day), asking for reassurance from her partner (2–3 times/week), and reading about breast cancer recurrence and treatment in medical journals (2–3 times/week).
Assessments
General hospital intake.
During the initial evaluation session, Hannah completed a general hospital intake, which provided an opportunity to discuss her cancer experience and provide additional background information in terms of her psychosocial and medical history. The Mindful Way Workbook was recommended at this intake session, and Hannah was provided with a web-link to begin practicing mindfulness using free online guided recordings in preparation for beginning the treatment protocol (Sears, 2018). Hannah used these recordings approximately once per day for one week after the first intake session; she then obtained a copy of the Mindful Way Workbook and began using audio CD included with the workbook for the remainder of treatment according to the home practice guidelines recommended for each week.
MINI International Neuropsychiatric Interview (MINI).
In a second evaluation session, Hannah completed a thorough diagnostic interview using the MINI International Neuropsychiatric Interview (Sheehan et al., 1998). The MINI assessed for DSM-IV current and past major depressive disorder, dysthymia, bipolar disorder, panic disorder, agoraphobia, social anxiety disorder, obsessive compulsive disorder, post-traumatic stress disorder, and generalized anxiety disorder. Diagnostic questioning was used to assess for hypochondriasis based on DSM-IV criteria, and illness anxiety disorder and somatic symptom disorder based on DSM-5 criteria. Hannah’s symptoms met DSM-IV criteria for hypochondriasis and were congruent with DSM-5 diagnostic criteria for Illness Anxiety Disorder, though Hannah did not clearly fit into care-seeking or care-avoidant DSM-5 subtypes, suggesting that hypochondriasis was the most appropriate diagnosis. Hannah did not meet criteria for any other psychological disorder.
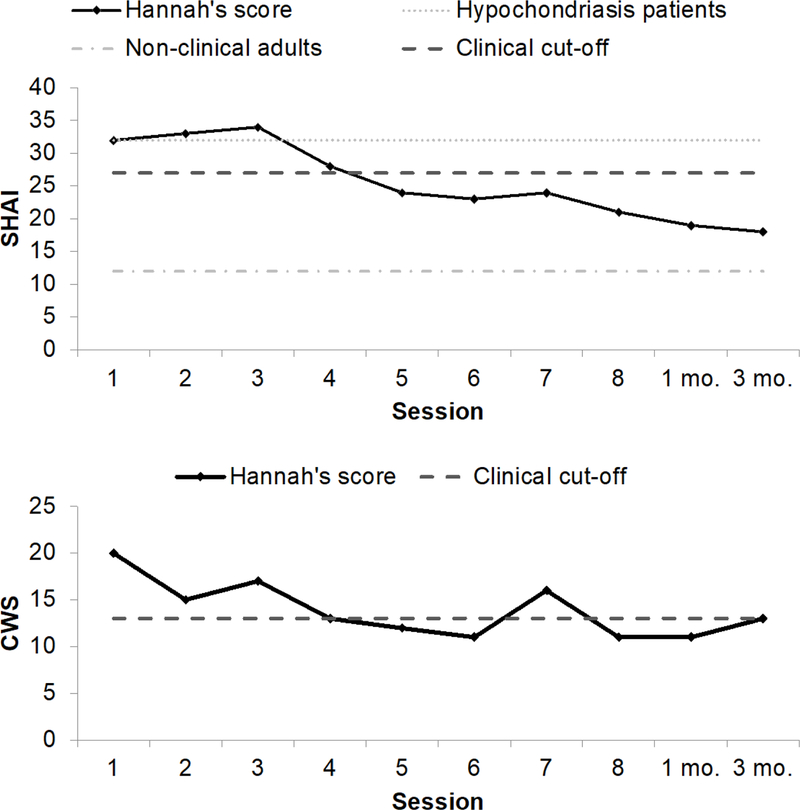
Short Health Anxiety Inventory (SHAI).
Hannah completed this measure at the beginning of each treatment session to assess her progress over time. The SHAI is an 18-item self-report measure of health anxiety symptoms (Salkovskis et al., 2002). Respondents select one of four statements on a scale of 0 to 3 that reflect varying degrees of health anxiety (e.g., 0 = “I do not worry about my health” to 3 = “I spend most of my time worrying about my health”). Scores range from 0 to 54, with higher scores indicating more severe symptoms. The SHAI demonstrates good reliability and validity, and discriminates between individuals with and without hypochondriasis (Abramowitz, Deacon, & Valentiner, 2007b; Alberts, Hadjistavropoulos, Jones, & Sharpe, 2013; Salkovskis et al., 2002). Hannah’s scores on the full 18-item measure were compared to norms for non-clinical students (M = 12.41, SD = 6.81), clinical hypochondriasis populations (M = 32.53, SD = 9.57), and an established clinical cut-off of 27 (Alberts et al., 2013).
Cancer Worry Scale (CWS).
Hannah also completed the 8-item CWS at the beginning of each session, which worry about cancer recurrence and the functional impact of these worries (Douma et al., 2010). The 8-item version of this scale is based on the original measure developed by Lerman et al. (1991), and includes additional items related to fears of needing surgery (again) and fears of family members getting cancer. Items are rated on a 4-point scale (1 = never to 4 = almost always) where higher scores indicate greater worry. It shows good internal consistency and convergent and discriminant validity, and discriminates between individuals with and without clinically significant FCR (clinical cut-off score of 13; Custers et al., 2014). This clinical cut-off score was used to characterize Hannah’s functioning and progress throughout therapy.
Treatment Delivery
The first treatment session focused on introducing the concept and practice of mindfulness as contrasted to “automatic pilot” (i.e., rushing through life without paying attention). Mindfulness of an external object (i.e., a rock) was practiced, wherein Hannah was asked to explore the object with different senses, observing experiences without judgment and returning attention to the object whenever it wandered off. Post-processing of this exercise followed the MBCT mindful inquiry process: (1) “What did you notice?”; (2) “How is this way of noticing different from how you typically notice your experiences?”; and (3) “How might this different way of noticing be helpful for reducing your anxiety?” Hannah discussed that her mind often wandered to neutral topics during the exercise and she was able to bring it back to the rock when guided. She considered how mindfulness might reduce automatic pilot by helping her to slow down. She also noted that the use of mindfulness skills might replace her tendency to critically focus on her body for signs of recurrence with a more open and accepting self-focus that prevents anxiety from escalating.
The focus of Session 2 was psychoeducation about cognitive-behavioral theory and mindfulness. An imagery exercise was used to teach the idea that thoughts are not facts but can impact emotions and behavior. Here, Hannah was asked to imagine that she was walking down the street and waved at a friend who did not wave back, and to consider what thoughts and feelings she would have in this situation. The CBT 3-component model was also taught (i.e., interrelated thoughts, physical sensations, behaviors) to further reinforce these ideas. Lastly, the proposed fear of recurrence model was presented (Figure 1) and Hannah was asked to personalize this model to her own experience. She reported that this model was an accurate depiction of her symptoms, and she considered the ways in which mindfulness could break down this cycle, noting that open body awareness could prevent catastrophic thoughts, and attentional control could prevent selectively focusing on certain areas.
In Session 3, Hannah was asked to complete a handout of long- and short-term pros and cons of safety-seeking behaviors. She discussed that these behaviors sometimes temporarily decreased anxiety in the short-term, and that they were likely to increase anxiety and reduce her quality of life in the long-term. She also reflected on the fact that none of these behaviors were recommended by her cancer care team. This session also introduced cognitive- decentering. Hannah was provided with a handout describing common unhelpful thinking patterns (i.e., “cognitive distortions” in traditional CBT), with a suggestion to approach these thoughts mindfully by noticing them, labeling them as unhelpful thoughts, and intentionally letting them go by redirecting her attention toward other aspects of the present moment. Strategies for changing the thought or generating alternate thoughts were not discussed. The 3- minute breathing space was practiced and taught as a way for Hannah to ground herself and gain information about her experience before choosing how to respond to unhelpful thoughts; the instruction was to begin practicing this exercise at three scheduled points throughout the day.
Session 4 introduced emotional exposure exercises in the form of a “sitting with difficulties” meditation. To first reinforce motivation for the exposure, psychoeducation was provided about the anxiety-avoidance cycle, with a focus on negative consequences of avoidance and benefits of emotional willingness. Hannah was asked to identify a difficult cancer-related thought or image to focus on during a sitting meditation, and to generate predictions about what this exercise would be. She was then guided through the meditation, which involved mindfulness of the breath, body sensations, and sounds before attempting to maintain attention on the chosen difficulty. Hannah was asked to openly notice any thoughts or body sensations that came up while focused on the difficulty, and to gently return her attention to the difficulty when it wandered off. Post-processing focused on the inaccuracies of her initial predictions, the difficulty of staying focused on the thought/image, and the overall lack of emotional reaction to the experience. Hannah noted that attempting to “embrace” anxiety symptoms might reduce their negative impact. The “responsive” application of the 3-minute breathing space was discussed, which encourages applying the practice to cope during moments of increased symptoms.
Session 5 was used to further practice emotional exposure. Hannah first generated a list of top ten feared thoughts or physical sensations. In reviewing this list, the therapist considered which symptoms, if any, could lend themselves to traditional CBT interoceptive exposure exercises as a way to enhance the effects of the exposure. Hannah identified breathlessness as a feared symptom, and was willing to participate in a voluntary hyperventilation exercise as part of the meditation (i.e., over-breathing along with an online metronome at a rate of 60 beats per minute). Hannah reported noticing anxious thoughts and distress throughout the exercise and that she was able to stay present in these experiences and allow them to naturally change and pass on their own. She agreed to practice exposing herself to the other fears on her list for homework, either by intentionally bringing mindful awareness to the symptom as it naturally occurred, or by bringing the fear to mind or body during a sitting with difficulties meditation.
The focus of Session 6 was cognitive de-centering. Cognitive de-centering was defined as the ability to view thoughts as transient mental events that are separate from the self and do not necessarily need to be believed or acted upon. Psychoeducation was provided regarding the ability to enhance cognitive de-centering through repeated mindfulness practice, with an emphasis on mindfulness of thoughts. Visual imagery strategies for supporting mindfulness of thoughts practiced were offered, such as imagining oneself sitting by a stream and, each time a thought occurs, placing the thought on a leaf and watching it float down the stream. This exercise was then practiced in session and Hannah generated her own mental imagery to use. She reported initial difficulty noticing any thoughts, and post-processing focused on the ways in which allowing anxious thoughts might paradoxically help to reduce them.
In Session 7, Hannah reported having a difficult week due to anxiety about a small bump that appeared on her chest. She described being able to disengage from this anxiety and pull herself out of a potential spiral sooner than she would have in the past. The session focused on teaching behavioral self-care and coping strategies. Hannah was asked to rate how much she values different life domains and the extent to which she currently engages in behaviors within each domain (e.g., relationships, education) in order to help clarify her values. She generated a list of her typical activities on an average day and indicated whether each activity was nourishing or draining, nourishing activities further sub-divided into those that were pleasurable or produced a sense of mastery. Lastly, Hannah was provided with a list of health behaviors derived from cancer survivor lifestyle guidelines. Together, insights gained from these interventions were used to generate a list of behaviors Hannah could engage in to cope with moments of increased anxiety, and promote self-care and valued living.
Session 8 was the final treatment session. Hannah developed a relapse prevention plan that included lessons to remember (e.g., anxiety passes on its own, reassurance behaviors maintain anxiety); behaviors to engage in regularly to maintain improvements (e.g., daily 10- minute meditation practice, getting enough sleep); and behavioral strategies for coping in moments of distress (e.g., 3-minute breathing space, nourishing activities). Hannah also considered ways in which her partner could support this plan and agreed to share the plan with him for his support. She returned approximately one month later for a follow-up booster session and reported that she had been able to enact her plan effectively, continuing to practice mindfulness daily, and had no worries about recurrence over the past month; in fact, this session was largely spent discussing ways to apply mindfulness skills to stressors unrelated to cancer. At her second and final booster session, Hannah reported that she recently began endocrine therapy and noticed temporary increases in anxiety during these medical visits, but was able to effectively manage the feelings and prevent anxious thoughts from escalating. She added that she continued to practice mindfulness exercises 20 minutes daily and, other than during medical visits, she did not worry about recurrence.
Results
Feasibility and Acceptability
The intervention appeared to be feasible and acceptable for this patient. Hannah attended each session on time and consistently completed each homework assignment. She did not cancel or miss any of her scheduled appointments. Hannah was actively engaged during sessions, asking questions and reporting observations from her mindfulness practice. She reported using mindfulness skills regularly throughout her daily life as a way to regulate emotions and prevent anxiety from “spiraling.” Hannah also reported that the format and content of the workbook were clear and helpful. She indicated that she had “gotten a lot” out of treatment and planned to complete the workbook a second time with a focus on a different problem (i.e., work stress). Hannah reported that the 3-minute breathing space was particularly valuable for use throughout the day, and longer practices were important to complete during evenings to build and maintain mindfulness skills. From the therapist’s perspective, mindful sitting with difficulties was a key component for helping Hannah develop distress tolerance and non-reactivity skills to prevent reassurance-seeking behaviors and minimize FCR symptoms.
Treatment Effects
Subjective reports of fear of recurrence reduction.
Session 8 included a review of treatment during which Hannah was explicitly ask to share her perspective on any changes she noticed as a result of practicing mindfulness skills. Hannah stated that she became less anxious and worried about recurrence, less stressed, and more calm as a result of treatment. She reported decreased attentional bias toward body sensations and greater acceptance of physical sensations, stating that she worried and focused less on physical symptoms. Hannah also described improvements in her ability to de-center from anxious, reporting that catastrophic thoughts about physical symptoms would “dissolve” on their own without any effort to alter or suppress them, which enabled her to refrain from acting on these thoughts via reassurance- seeking behaviors and, instead, allow the thoughts to arise and pass. Improvements in distress tolerance were reported, as Hannah indicated that she learned “there is a place within [herself]” that is able to breathe and stay calm during discomfort. In addition, Hannah reported that she experienced “unintended” improvements in work, relationships, and sleep.
Behavioral changes.
Hannah reported improvements in each reassurance-seeking behavior. She reportedly stopped asking her husband for reassurance about her health, obsessively scanning her body for signs of recurrence, and reading medical journal articles about cancer. She also reported that she would intentionally use neutral physical symptoms as opportunities to practice resisting behavioral urges (e.g., practicing noticing an itch without automatically scratching).
Objective scores.
See Figure 2 for SHAI and CWS scores over time. Scores on each measure decreased from before to after treatment and tended to change similarly with each other. Changes on both measures were clinically significant, as evidenced by an overall pre- post decrease of 44% on the SHAI and 35% on the CWS, both surpassing the standard 20% decrease indicative of responder status (Behar & Borkove, 2003); a statistically significant reliable change index (RCI) score of 6.54 on the SHAI and 6.40 on the CWS (ps < .01; Jacobson, Roberts, Berns, & McGlinchey, 1999); and a final SHAI score below the clinical cut- off, and CWS score at the clinical cut-off. By the end of treatment, Hannah did not meet any DSM criteria for any health anxiety-related disorder or other psychological disorder.
Figure 2.
SHAI and CWS scores at the start of each session. 1 mo. and 3 mo. refer to follow-up visits.
Discussion
The purpose of this paper was to build on identified shortcomings of the mindfulness for cancer literature (e.g., Shaw et al., 2018) by offering a theoretical model of MBCT for FCR, describing an MBCT protocol adapted for FCR, and illustrating the delivery of this protocol in an individual therapy setting. Results are one step toward providing preliminary support that MBCT may be useful for FCR by targeting theoretically-grounded psychobehavioral processes. The patient indicated that the proposed theoretical model (Figure 1) accurately reflected her symptoms at baseline and she described improvements in model components and mindfulness skills as her FCR decreased. Consistent with recent FCR theories (Butow et al., 2013; Fardell et al., 2016; Segal et al., 2002; Simonelli et al., 2017), this model may help clarify specific attentional, perceptual, cognitive, affective, and behavioral micro-processes upon which mindfulness training may intervene, offering a theoretically-grounded rationale and empirically- supported and testable mechanistic hypotheses for future research.
We hope the proposed model motivates further exploration of the overlap between health anxiety and FCR. Given that FCR is not itself a diagnostic disorder yet is distinct from anxiety disorders (Dinkel et al., 2014), research is needed to better understand the new DSM-5 health anxiety-related disorders and how they may relate to cancer survivors (Bailer et al., 2016; see Simonelli et al., 2017 for a review of FCR and psychiatric diagnoses). The current patient met full DSM-IV criteria for hypochondriasis and each of the main symptoms of DSM-5 illness anxiety disorder, but she did not clearly fit into the care-seeking or care-avoidant illness anxiety disorder subtypes. This may be because these new diagnostic groups are less valid classifications of health anxiety than hypochondriasis was (Bailer et al., 2016) or because the care-avoidant subtype requires further consideration for cancer survivors who are likely to be adherent to medical visits as part of their follow-up care (DiMatteo, 2004). Adjustment Disorders may ultimately be the most appropriate diagnoses for patients with FCR.
The case study results also support the potential benefits of MBCT for FCR in individual therapy outpatient hospital settings. The patient reported clinically significant improvements on validated measures of health anxiety and cancer worry; her final score on the CWS may also be an over-estimate because it was taken the day of a medical visit (McGinty, Small, Laronga, & Jacobsen, 2016). It is worth noting that there was a temporary increase in cancer worry at session 7 due to the appearance of small bump on the patient’s body. Triggers for FCR are ubiquitous (e.g., medical visits, cancer in the media) and the aim of MBCT is to learn skills to manage increased distress and prevent symptoms from escalating to relapse. For Hannah, her CWS scores returned to and were maintained at non-clinical levels at session 8 and throughout the 3-month follow-up, consistent with her subjective reports of maintained improvements, reflecting a pattern of change consistent with improvement in an MBCT approach.
This is the first study we are aware of to describe the application of the MBCT workbook to individual therapy and how to adapt this protocol to target FCR. There is little research on how to deliver MBCT in individual therapy settings and the efficacy of an individual MBCT approach. One of the few studies of individual MBCT to date happens to focus on FCR and the results demonstrated significant symptom reductions as compared to usual care, but methodological weaknesses limit the ability to isolate the effects of the individual format (i.e., individual telehealth delivery was compared to group in-person delivery; Cillesen et al., 2018; Compen et al., 2018). For cancer patients, exploring individual MBCT is important given that individual therapy is the common treatment option in many academic medical center outpatient psychiatry departments, and group interventions can be logistically challenging and thus not easily available or they may not be appropriate for some patients (e.g., due to differences in disease severity). Other mindfulness-based interventions (e.g., Mindfulness-Based Stress Reduction [Kabat-Zinn, 1982], Mindfulness-Based Cancer Recovery [Carlson & Speca, 2011]) also show efficacy for improving emotional outcomes for cancer survivors (Lengacher et al., 2011; Lengacher et al., 2009; Lengacher et al., 2014), although these programs do not take an exlicit CBT approach.
Limitations to the current study are worth noting and point to directions for future research. First, as a single case study, the results cannot generalize to other survivors. The patient was very motivated, highly educated, and engaged in care, and she had early stage disease and a good prognosis. Certain modifications made for this patient may or may not be necessary for others (e.g., communication with the medical team). Research in larger and more diverse samples is needed, particularly RCTs that explore the efficacy of MBCT as compared to active, evidence-based interventions. Much of the mindfulness intervention research also focuses on WEIRD samples (i.e., white, educated, industrialized, rich, democratic; Goldberg et al., 2018), though research on vulnerable and low-income populations is increasing (e.g., Smith, Metzker, Waite, & Gerrity, 2015), reflecting a need for continued research among diverse groups. Second, although the patient’s subjective reports and improvements were consistent with the proposed theoretical model, this model was not directly tested due to the added burden of measuring every variable as part of standard clinical care. Similarly, we did not collect a formal satisfaction measure as this assessment is not part of our standard care. Future studies should examine the relationships between model constructs (e.g., distress tolerance, attentional bias) and FCR. Future research could also explore the application of the proposed model to other patient populations with fears of disease recurrence (e.g., recurrent cardiac events, stroke).
Overall, the current results suggest that MBCT may be a useful treatment approach for FCR with a theoretically-grounded rationale and testable mechanistic components. Further research is needed to explore the utility of MBCT for FCR in larger and more diverse samples, using more rigorous methodological designs and direct tests of hypothesized mechanistic components.
Acknowledgments
Funding: This study was supported by funds from the National Center for Complementary and Integrative Health (XXXXX) and National Cancer Institute (XXXXX).
Footnotes
Compliance with Ethical Standards
Research involving human participants: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: This study was deemed exempt from IRB approval. The patient gave permission for her case to be described with anonymity.
Conflict of interest: The authors declare that they have no conflict of interest.
References
- Abramowitz JS, Deacon BJ,& Valentiner DP (2007a). The Short Health Anxiety Inventory: Psychometric properties and construct validity in a non-clinical sample. Cognitive Therapy and Research, 31, 871–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Abramowitz JS, Deacon BJ, & Valentiner DP (2007b). The short health anxiety inventory in an undergraduate sample: Implications for a cognitive-behavioral model of hypochondriasis. Cognitive Therapy and Research, 31, 887–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberts NM, Hadjistavropoulos HD, Jones SL, & Sharpe D (2013). The Short Health Anxiety Inventory: A systematic review and meta-analysis. Journal of Anxiety Disorders, 27, 68–78. [DOI] [PubMed] [Google Scholar]
- Arch JJ, & Mitchell JL (2015). An Acceptance and Commitment Therapy (ACT) group intervention for cancer survivors experiencing anxiety at re-entry. Psycho-Oncology, 25, 610–615. [DOI] [PubMed] [Google Scholar]
- Armes J, Crowe M, Colbourne L, Morgan H, Murrells T, Oakley C,…Richardson A (2009). Patients’ supportive care needs beyond the end of cancer treatment: A prospective, longitudinal survey. Journal of Clinical Oncology, 27, 6172–6179. [DOI] [PubMed] [Google Scholar]
- Asmundson GJ, Abramowitz JS, Richter AA, & Whedon M (2010). Health anxiety: Current perspectives and future directions. Current Psychiatry Reports, 12, 306–312. [DOI] [PubMed] [Google Scholar]
- Bailer J, Kerstner T, Witthöft M, Diener C, Mier D, & Rist F (2016). Health anxiety and hypochondriasis in the light of DSM-5. Anxiety, Stress, & Coping, 29, 219–239. [DOI] [PubMed] [Google Scholar]
- Behar ES, & Borkove TD (2003). Psychotherapy outcome research. In: Scinka JA, Velicer EF, eds. Handbook of Psychology: Research Methods in Psychology, 2, 213–240. [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J,…Devins G (2004). Mindfulness: A proposed operational definition. Clinical Psychology-Science and Practice, 11, 230–241. [Google Scholar]
- Butow PN, Bell ML, Smith AB, Fardell JE, Thewes B, Turner J, …Mihalopoulos C (2013). Conquer fear: Protocol of a randomised controlled trial of a psychological intervention to reduce fear of cancer recurrence. BMC Cancer, 13, 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carlson L, & Speca M (2011). Mindfulness-Based Cancer Recovery: A Step-by-step MBSR Approach to Help You Cope with Treatment and Reclaim Your Life Oakland, CA: New Harbinger Publications. [Google Scholar]
- Cillessen L, Schellekens MPJ, Van de Ven MOM, Donders ART, Compen FR, Bisseling EM,…Speckens AEM (2018). Consolidation and prediction of long-term treatment effect group and online mindfulness-based cognitive therapy for distressed cancer patients. Acta Oncologica, 22, 1–10. [DOI] [PubMed] [Google Scholar]
- Compen F, Bisseling E, Schellekens M, Donders R, Carlson L, van der Lee M, & Speckens A (2018). Face-to-Face and Internet-Based Mindfulness-Based Cognitive Therapy Compared With Treatment as Usual in Reducing Psychological Distress in Patients With Cancer: A Multicenter Randomized Controlled Trial. Journal of Clinical Oncology, 36, 2413–2421. [DOI] [PubMed] [Google Scholar]
- Crane RS, Kuyken W, Hastings RP, Rothwell N, & Williams JMG (2010). Training teachers to deliver mindfulness-based interventions: Learning from the UK experience. Mindfulness, 1, 74–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran L, Sharpe L, & Butow P (2017). Anxiety in the context of cancer: A systematic review and development of an integrated model. Clinical Psychology Review, 56, 40–54. [DOI] [PubMed] [Google Scholar]
- Custers JA, van den Berg SW, van Laarhoven HW, Bleiker EM, Gielissen MF, Prins JB (2014). The cancer worry scale: Detecting fear of recurrence in breast cancer survivors. Cancer Nursing, 37, E44–50. [DOI] [PubMed] [Google Scholar]
- DiMatteo MR (2004). Variations in patients’ adherence to medical recommendations: A quantitative review of 50 years of research. Medical Care, 42, 200–209. [DOI] [PubMed] [Google Scholar]
- Dinkel A, Kremsreiter K, Marten-Mittag., & Lahmann C (2014). Comorbidity of fear of progression and anxiety disorders in cancer patients. General Hospital Psychiatry, 36, 13–619. [DOI] [PubMed] [Google Scholar]
- Douma KF, Aaronson NK, Vasen HF, Gerrirsma MA, Gundy CM, Janssen EP,…Bleiker. (2010). Psychological distress and use of psychosocial support in familial adenomatous polyposis. Psycho‐Oncology, 19, 289–298. [DOI] [PubMed] [Google Scholar]
- Fardell JE, Thewes B, Turner J, Glichrist J, Sharpe L, Smith A,…Butow P (2016). Fear of cancer recurrence: A theoretical review and novel cognitive processing formulation. Journal Cancer Survivorship, 10, 663–673. [DOI] [PubMed] [Google Scholar]
- Germer C, Siegel RD, & Fulton PR (2013). Mindfulness and Psychotherapy (2nd ed.). New York, NY: Guilford Press. [Google Scholar]
- Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, & Simpson TL (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall DL, Luberto CM, Philpotss LL, Song R, Park ER, & Yeh GY (2018). Mind- body interventions for fear of cancer recurrence: A systematic review and meta- analysis. Psych-Oncology Advance online publication. doi: 10.1002/pon.4757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall DL, Mishel MH, & Germino BB (2014). Living with cancer-related uncertainty: Associations with fatigue, insomnia, and affect in younger breast cancer survivors. Supportive Care in Cancer, 22, 2489–2495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, & Oh D (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal Consulting and Clinical Psychology, 78, 169–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacobson NS, Roberts LJ, Berns SB, & McGlinchey JB (1999). Methods for defining and determining the clinical significance of treatment effects: Description, application, and alternatives. Journal Consulting and Clinical Psychology, 67, 300–307. [DOI] [PubMed] [Google Scholar]
- Kabat-Zin J (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. General Hospital Psychiatry, 4, 33–47. [DOI] [PubMed] [Google Scholar]
- Kim Y, Carver CS, Spillers RL, Love-Ghaffari M,& Kaw CK (2012). Dyadic effects of fear of recurrence on the quality of life of cancer survivors and their caregivers. Quality of Life Research, 21, 517–525. [DOI] [PubMed] [Google Scholar]
- Koch L, Jansen L, Brenner H, & Arndt V (2013). Fear of recurrence and disease progression in long‐term (≥ 5 years) cancer survivors—a systematic review of quantitative studies Psycho‐Oncology, 22, 1–11. [DOI] [PubMed] [Google Scholar]
- Lebel S, Tomei C, Feldstain A, Beattie S, & McCallum M (2013). Does fear of cancer recurrence predict cancer survivors’ health care use? Support Care Cancer, 21, 901–906. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Johnson-Mallard V, Barta M, Fitzgerald S, Moscoso MS, Post-White J, …Kip KE(2011). Feasibility of a mindfulness-based stress reduction program for early- stage breast cancer survivors. Journal of Holistic Nursing, 29, 107–117. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Johnson‐Mallard V, Post‐White J, Moscoso MS, Jacobsen PB, Klein TW, …Kip KE (2009). Randomized controlled trial of mindfulness‐based stress reduction (MBSR) for survivors of breast cancer. Psycho‐Oncology, 18, 1261–1272. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Shelton MM, Reich RR, Barta MK, Johnson-Mallard V, Moscoso ML,…Kip KE (2014). Mindfulness based stress reduction (MBSR (BC)) in breast cancer: Evaluating fear of recurrence (FOR) as a mediator of psychological and physical symptoms in a randomized control trial (RCT). Journal of Behavioral Medicine,37,185–195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lerman C, Track B, Rimer BK, Boyce A, Jepson C, & Engstrom PF (1991). Psychological and behavioral implications of abnormal mammograms. Annals of Internal Medicine, 114,657–661. [DOI] [PubMed] [Google Scholar]
- Lovas D,A, & Barsky AJ (2010). Mindfulness-based cognitive therapy for hypochondriasis, or severe health anxiety: A pilot study. Journal of Anxiety Disorders, 24, 931–935. [DOI] [PubMed] [Google Scholar]
- McGinty HL, Small BJ, Laronga C, & Jacobsen PB (2016). Predictors and patterns of fear of cancer recurrence in breast cancer survivors. Health Psychology, 35,1–9. [DOI] [PubMed] [Google Scholar]
- McManus F, Surawy C, Muse K, Vazquez-Montes M, & Williams JM (2012). A randomized clinical trial of mindfulness-based cognitive therapy versus unrestricted services for health anxiety (hypochondriasis). Journal of Consulting and Clinical Psychology, 80, 817–828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis PM, & Warwick H, M. (1986). Morbid preoccupations, health anxiety and reassurance: A cognitive-behavioural approach to hypochondriasis. Behaviour Research and Therapy, 25, 597–602. [DOI] [PubMed] [Google Scholar]
- Salkovskis PM, Rimes KA, Warwick HM, & Clark DM (2002). The Health Anxiety Inventory: Development and validation of scales for the measurement of health anxiety and hypochondriasis. Psychological Medicine, 32, 843–853. [DOI] [PubMed] [Google Scholar]
- Sears RW (2018). Mindfulness Audio Recordings, Retrieved from http://psych-insights.com/mindfulness-audio-recordings/ [Google Scholar]
- Sears RW, Tirch DD, & Denton RB (2011). Mindfulness in Clinical Practice Sarasota, FL: Professional Resource Exchange. [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2012). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse (2nd ed). New York: Guilford. [Google Scholar]
- Shaw LK, Sherman KA, Fitness J, & Elder E (2018). Factors associated with romantic relationship formation difficulties in women with breast cancer. Psycho-Oncology 27, 1270–1276. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, …Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychology, 20: 22–33, quiz 34–57. [PubMed] [Google Scholar]
- Simonelli LE, Siegel SD, & Duffy NM (2017). Fear of cancer recurrence: a theoretical review and its relevance for clinical presentation and management. Psycho-Oncology, 26, 1444–1454. [DOI] [PubMed] [Google Scholar]
- Smith B, Metzker K, Waite R, & Gerrity P (2015). Short-form mindfulness-based stress reduction reduces anxiety and improves health-related quality of life in an inner-city population. Holistic nursing Practice, 29, 70–77. [DOI] [PubMed] [Google Scholar]
- Spencer JC, & Wheeler SB (2016). A systematic review of Motivational Interviewing interventions in cancer patients and survivors. Patient Education and Counseling, 99, 1099–1105. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Rowland JH, & Ganz PA (2015). Life after diagnosis and treatment of cancer in adulthood: Contributions from psychosocial oncology research. American Psychologist, 70,159–174. [DOI] [PubMed] [Google Scholar]
- Surawy C, McManus F, Muse K, & Williams JMG (2015). Mindfulness-Based Cognitive Therapy (MBCT) for health anxiety (Hypochondriasis): Rationale, implementation and case illustration. Mindfulness, 6,382–392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teasdale JD, Williams JM, & Segal ZV (2014). The mindful way workbook: An 8-week program to free yourself from depression and emotional distress New York, NY: Guilford Press. [Google Scholar]
- Thewes B, Brebach R, Dzidowska M, Rhodes P, Sharpe L, & Butow P (2014). Current approaches to managing fear of cancer recurrence; A descriptive survey of psychosocial and clinical health professionals. Psycho‐Oncology, 23, 390–296. [DOI] [PubMed] [Google Scholar]
- Walsh R, & Sharpiro SL (2006). The meeting of meditative discoplines and western psychology: A mutually enriching dialogue. American Psychologist, 61, 227–239 [DOI] [PubMed] [Google Scholar]