Abstract
Objective
Transfer from hospital to hospital for cardiac surgery represents a large portion of some clinical practices. Previous literature in other surgical fields has shown worse outcomes for patients transferred. We hypothesized that transferred patients would be higher risk and demonstrate worse outcomes than those admitted through the emergency department.
Methods
All patients undergoing cardiac operations with a Society of Thoracic Surgeons (STS) Predicted Risk of Mortality (PROM) were evaluated from a multicenter, statewide STS database. Only patients requiring admission prior to surgery were included. Patients were stratified by admission through the emergency department or in transfer. Transfers were further stratified by the cardiothoracic surgery capabilities at the referring center.
Results
A total of 13,094 patients met the inclusion criteria of admission prior to surgery. This included 7,582 (57.9%) transfers, of which 502 (6.6%) were referred from cardiac centers. Compared to emergency department admissions, transfers had increased hospital costs despite lower operative risk (PROM 1.5% vs. 1.6%, p<0.01) and equivalent postoperative morbidity (15.6% vs. 15.3% p=0.63). In risk adjusted analysis, transfer status was not independently associated with worse outcomes. Patients transferred from centers that perform cardiac surgery are higher risk than general transfers (PROM 2.5% vs. 1.5, p<0.01), but specialized care results in excellent risk adjusted outcomes (O/E: Mortality 0.81; Morbidity or Mortality 0.90).
Conclusions
Transfer patients have similar rates of postoperative complications but increased resource utilization compared to patients admitted through the emergency department. Importantly, patients transferred from centers that perform cardiac surgery represent a particularly high-risk subgroup.
Graphical Abstract
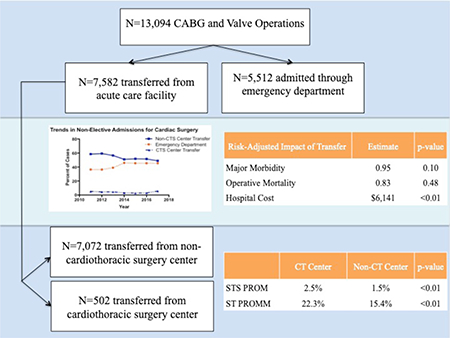
Central Picture Legend
Graphical abstract demonstrating the study populations, surgical outcomes, resource utilization and trends in non-elective admissions. (CABG: Coronary Artery Bypass Grafting; Non-CTS Center: Non-Cardiothoracic Surgery Center; CT Center: Cardiothoracic Surgery Center; OR: Odds-Ratio)
Central Message
Patients transferred for cardiac surgery have increased resource utilization despite a lower clinical risk than those admitted through the emergency department.
Central Picture
Graphical abstract demonstrating the study populations, surgical outcomes, resource utilization and trends in non-elective admissions. Although there is no significant risk-adjusted impact of transfers on clinical outcomes, transferred patients incur increased risk-adjusted hospital costs than patients admitted through the emergency department. Among transferred patients, there is a higher risk cohort, existing in large part due to referral bias, which includes patients transferred from one CTS center to another. (CABG: Coronary Artery Bypass Grafting; CT Center: Cardiothoracic Surgery Center; Non-CTS Center: Non-Cardiothoracic Surgery Center; OR: Odds-Ratio; STS PROM: Society of Thoracic Surgeons Predicted Risk of Mortality; STS PROMM: Society of Thoracic Surgeons Predicted Risk of Morbidity or Mortality)
Introduction
Patients require hospital to hospital transfer when local expertise or resources are insufficient to provide appropriate care to patients.1 Patients that are transferred for a wide range of medical and surgical conditions have been shown to have more severe comorbid conditions and advanced disease processes.2–4 As a result, there has been concern that facilities may be disincentivized to accept transfers because of higher rates of adverse outcomes and an increase in resource utilization.5,6
Due to the resources and expertise required to establish and maintain cardiac surgery programs, inter hospital transfer is a means to facilitate access to specialty care. However, associated with the transfer process itself is the potential for delays in care, longer hospitalizations, and increased patient and healthcare costs.6,7 Prior work in the study of transfer networks within cardiac surgery has been limited. More commonly, transfer studies in cardiovascular disease have focused on the emergent situation such as in the management of ST segment myocardial infarction or aortic emergencies.8-12 Overall, patients in need of cardiac surgery generally require prompt, and occasionally, emergent evaluation. Concern has been raised regarding the potential adverse effects of prolonged preoperative hospitalization in patients transferred for cardiac surgery.13
Given the complexities surrounding patients that are transferred prior to cardiac surgery, we sought to better understand the outcomes in non-elective patients transferred from a referral hospital to the operative hospital compared to patients admitted through the emergency department at the operative facility. We hypothesized patients transferred from another hospital prior to their operation would have worse outcomes and greater resource utilization than those admitted directly through the emergency department.
Methods
Patient Data
The Virginia Cardiac Services Quality Initiative (VCSQI) includes 19 hospitals and surgical groups in the region. Data recorded from the registry includes 99% of all adult cardiac surgery in the region and methodologies for clinical data acquisition and cost data methodology have been described previously.14,15,16,17 Institutional STS data is compiled from individual centers and standard STS definitions were used for all variables. Charges are captured with International Classification of Disease, ninth revision revenue codes and Uniform Billing-04/92 files are matched to STS data with a success rate of 99%. Institutional charges are then converted to estimated costs with cost-to-charge ratios submitted by each hospital to Centers for Medicare & Medicaid Services. Finally, costs are adjusted to 2017 dollars accounting for medical-specific inflation using Centers for Medicare & Medicaid Services inpatient prospective payment system multipliers. This study was exempt from review by the University of Virginia Institutional Review Board due to the de-identified nature of the quality database.
All patients who underwent coronary artery bypass grafting (CABG) and/or valve operations with a Society of Thoracic Surgeons (STS) Predicted Risk of Mortality (PROM) score between July 2011 and June 2017 were extracted from the VCSQI database. Patients were excluded if they were admitted electively for their operation. Patients were stratified by emergency department (ED) admission or transfer admission. A subgroup analysis of all transfer patients was performed with stratification by cardiothoracic surgery availability at the transferring center (Cardiothoracic Surgery [CTS] center vs. non-Cardiothoracic Surgery [non-CTS] center). The primary outcome of interest was risk-adjusted odds of postoperative adverse events in transferred patients. Secondary outcomes included pre- and post-operative length of stay, hospital costs and rates of discharge to facilities.
Statistical Analysis
Continuous variables with skewed distributions are presented as median [interquartile range (IQR)], normally distributed continuous variables as mean ± standard deviation, and categorical variables as count (percentage). Wilcoxon rank sum test was used for skewed continuous variables, independent t test for normally distributed continuous variables and the Chi-Square test was utilized for categorical variables. Hierarchical logistic regression with a generalized linear regression model was used to analyze operative mortality and major morbidity with adjustment using the appropriate log transformed STS risk score, insurance status, and year of operation while accounting for center level clustering with hospital as a random effect. Linear regression modeling was used to assess risk-adjusted hospital costs and length of stay using STS risk scores, insurance status and year of operation. SAS version 9.4 (SAS Institute, Cary, NC) statistical software was used for analysis with a statistical threshold 0.05 set for significance.
Results
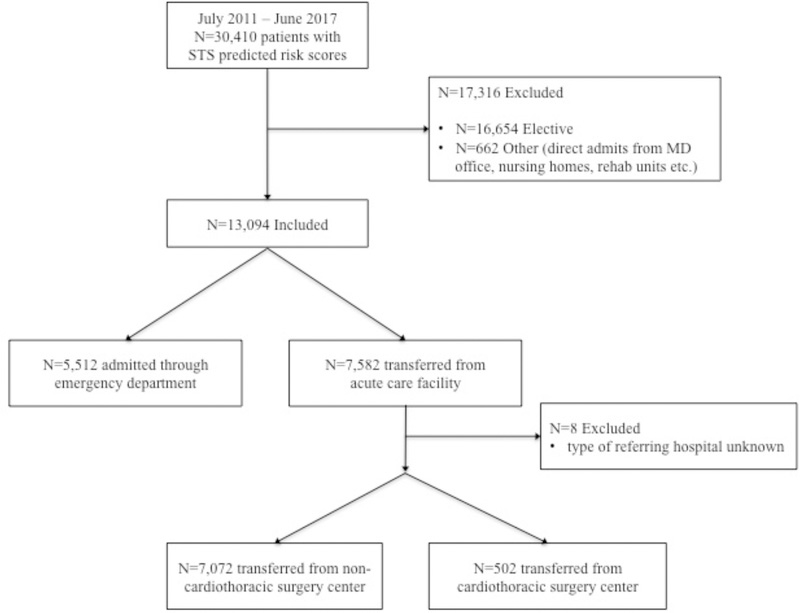
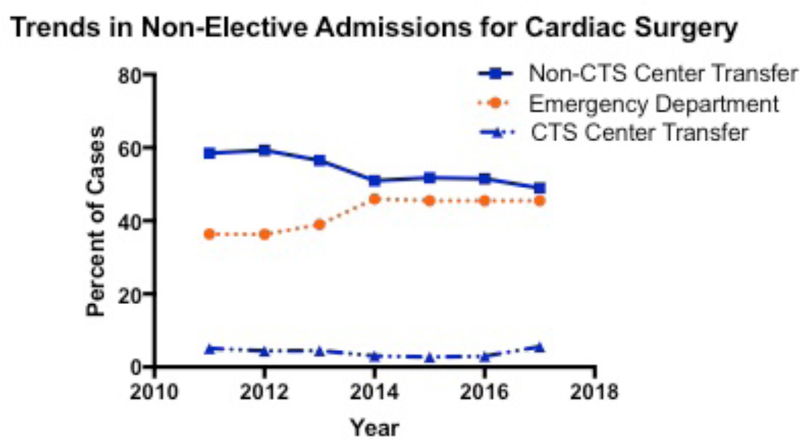
A total of 30,410 patients underwent qualified procedures and had STS risk scores available. Of these, 13,094 (44%) met the inclusion criteria of admission prior to surgery. This included 7,582 (57.9%) transfers, of which 502 (6.6%) were transferred from CTS capable centers (Figure 1). During the study period, there was a decrease in the percentage of patients transferred from 64% in the first year of the study to 55% in the most recent period (p<0.001) (Figure 2).
Figure 1:
Consort diagram showing the derivation of the study cohort. Of the 39,051 CABG/valve operations in the database over a 6-year period, 22% were excluded because STS risk scores were unavailable for the given procedure. From these 30,410 patients, 17,316 were excluded, with the majority of these due to elective admission status. Of the 13,094 patients admitted preoperatively for a qualified operation, over half were transferred from another institution. (CABG: Coronary Artery Bypass Grafting; STS: Society of Thoracic Surgeons; MD: Medical Doctor)
Figure 2:
Trends in Non-Elective Admissions Source for Cardiac Surgery Over Study Period. The solid blue line represents transfers from non-cardiothoracic surgery centers. Although decreasing during the study period, this remains the predominant admission source for non-electively admitted patients. (CTS Center: Cardiothoracic Surgery Center; Non-CTS Center: Non-Cardiothoracic Surgery Center)
Patient demographics, comorbid diseases and operations performed were generally similar between ED admissions and transfers, with ED admissions having a higher prevalence of smoking history, peripheral arterial disease, and previous myocardial infarction (Table 1). Transferred patients were more likely to have government insurance (58% vs. 54%, p<0.001) than those admitted through the ED. Consistent with baseline risk factors, transfer patients had lower median STS Risks than those admitted through the ED (PROM 1.5% [0.74–3.63] vs. 1.6% [0.76–3.95], p=0.0041, Predicted Risk of Morbidity or Mortality [PROMM], 15.7% [9.8–27.5] vs. 16.5% [9.9 – 28.4], p=0.0057).
Table 1:
Baseline Characteristics of Patients Admitted as Transfers vs. Through the Emergency Department
| Transfer | Emergency Department | p-value | ||
|---|---|---|---|---|
| N | 57.9 (7582) | 42.1 (5512) | ||
| Patient Age | 64.1 ± 10.9 | 64.2 ± 11.1 | 0.6742 | |
| Sex (F) | 29.1 (2206) | 30.6 (1689) | 0.0559 | |
| Ejection Fraction | 55 [40–60] | 53 [40– 60] | 0.2613 | |
| Procedure | 0.0866 | |||
| Isolated CABG | 84.5 (6408) | 83.5 (4600) | ||
| Isolated Valve | 7.4 (559) | 8.4 (464) | ||
| CABG/Valve | 8.1 (615) | 8.1 (448) | ||
| Smoking History | 29.4 (2222) | 33.4 (1831) | <.0001 | |
| Hypertension | 85.6 (6480) | 85.6 (4715) | 0.9200 | |
| Diabetes | 48.8 (3701) | 47.3 (2606) | 0.0882 | |
| Peripheral Artery Disease | 13.4 (1015) | 14.8 (816) | 0.0239 | |
| Prior Myocardial Infarction | 68.3 (5171) | 71.9 (3950) | <.0001 | |
| Heart Failure | 33.1 (2509) | 31.7 (1746) | 0.0906 | |
| Previous Cardiac Intervention | 28.6 (2167) | 34.3 (1891) | <.0001 | |
| Reoperation | 4.1 (312) | 4.1 (227) | 0.9926 | |
| Preoperative Length of Stay | 4 [2,6] | 4 [2,6] | <.0001 | |
| Urgency | 0.1169 | |||
| Elective | 3 (227) | 3.3 (182) | ||
| Urgent | 90.7 (6876) | 89.9 (4947) | ||
| Emergent | 6.2 (467) | 6.5 (359) | ||
| Salvage | 0.2 (11) | 0.3 (17) | ||
| Insurance | <.0001 | |||
| HMO | 4.3 (322) | 5.8 (319) | ||
| Commercial | 24.7 (1865) | 26.2 (1439) | ||
| Government | 58.3 (4406) | 54 (2963) | ||
| Self | 12.8 (965) | 14 (768) | ||
| Cardiopulmonary Bypass Time | 97 [76–123] | 100 [78–129] | <.0001 | |
| Cross Clamp Time | 71 [54–91] | 74 [55–95] | <.0001 | |
| PROMM | 15.7% [9.8–27.5] | 16.5% [9.9–28.4] | 0.0057 | |
| PROM | 1.5% [0.74–3.63] | 1.6% [0.76–3.95] | 0.0014 | |
Unadjusted, postoperative complication rates were similar between ED admissions and transfers including all STS major morbidities and pneumonia (2.6% vs. 3.2%, p=0.0705) (Table 2). However, operative mortality was lower in overall transfers than ED admissions (2.6% vs. 3.3%, p=0.0235) with better than expected mortality for transferred patients (Observed/Expected [O/E]=0.78, p=0.0112) and similar to expected for ED patients (O/E=0.89, p=0.2754). Despite being lower risk, having similar rates of adverse events, and shorter intensive care unit stays, transferred patients had a longer unadjusted post-operative length of stay (6 [5,9] vs. 6 [4,8], p<0.0001) and higher hospital costs incurred at the operating hospital ($46,290 [$34,573 - $72,165] vs. $43,592 [$34,747 - $60,795], p<0.0001; $55,382 ± $43,461 vs. $50,756 ± $36,3665). Transferred patients were slightly less likely to discharge to a facility (24.1% vs. 25.8% vs. p=0.0312) than those admitted through the ED. In regression analysis of all patients admitted prior to their operation, transfer status itself did not confer an increased risk of morbidity or mortality (Table 3). However, there was a risk-adjusted $6,141,65 (95% CI: $5,405 - $6,878, p<0.0001) and 0.352 day (95% CI: 0.232–0.472, p=0.0034) increase in hospital cost and postoperative length of stay, respectively.
Table 2:
Unadjusted Outcomes of Patients Admitted as Transfers vs. Through the Emergency Department
| Transfer | Emergency Department | p-value | |
|---|---|---|---|
| Operative Mortality | 2.61 (198) | 3.28 (181) | 0.0235 |
| Major Morbidity | 15.6 (1183) | 15.3 (843) | 0.6295 |
| Prolonged Ventilation | 12.4 (943) | 12.3 (678) | 0.8143 |
| Renal Failure | 3(225) | 3(163) | 0.9718 |
| Permanent Stroke | 1.5 (115) | 1.6 (87) | 0.7773 |
| Need for Reoperation | 2.7 (208) | 3(166) | 0.3629 |
| Deep Sternal Wound Infection | 0.1 (5) | 0.1 (3) | 0.7936 |
| Hospital Cost | $46,290 [34,573–72,165] | 43,592 [34,747–60,795] | <0.0001 |
| Postoperative Length of Stay | 6 [5,9] | 6 [4,8] | <.0001 |
Table 3:
Logistic and Linear Regression for Relative Risk of Transfer Admissions vs. Emergency Department Admissions
| Risk-Adjusted Odds Ratioa | 95% Confidence Interval | p-value | C statistic | |
|---|---|---|---|---|
| Operative Mortality | 0.830 | 0.662 – 1.041 | 0.1074 | 0.798 |
| Major Morbidity | 0.959 | 0.855 – 1.077 | 0.4802 | 0.771 |
| Prolonged Ventilation (>24H) | 0.933 | 0.820–1.060 | 0.2854 | 0.798 |
| Renal Failure | 0.990 | 0.784 – 1.251 | 0.9349 | 0.823 |
| Permanent Stroke | 0.943 | 0.701 – 1.267 | 0.696 | 0.691 |
| Surgical Reoperation | 0.879 | 0.701 – 1.101 | 0.2611 | 0.673 |
| Parameter Estimatea | 95% Confidence Interval | p-value | R2 | |
| Hospital Cost | $6,141.65 | $5,405 - $6,878 | 736.41 | .1397 |
| Postoperative Length of stay | 0.352 | 0.232 – 0.472 | 0.0034 | .1270 |
Adjusted-Odds Ratio and Parameter Estimate Referenced to Emergency Department Admission
On subgroup analysis of all transfer patients, those that transferred from CTS centers had more complex cardiovascular disease compared to patients transferred from non-CTS centers (Table 4), including a higher likelihood of heart failure (46.8% vs. 32.2%, p<0.0001) and previous cardiac surgery (13% vs. 3.5%, p<0.0001). These factors translated into higher median STS predicted risks (PROM 2.5% [1.13–6.55] vs. 1.5% [0.73–3.47] and PROMM 22.3% [12.2–37.7] vs. 15.4% [9.6–26.8], both p<0.0001). Consistent with their STS risk scores, patients transferred from CTS centers had worse unadjusted outcomes than those from non-CTS centers with statistically significant increased rates of three out of five STS major morbidities and higher operative mortality (4.2% vs. 2.5%, p =0.0226) (Table 5). Overall, the increased morbidity and mortality was accounted for by patient factors, with O/E ratios for CTS transfers of 0.81 (p=0.5501) for mortality and 0.90 (p=0.3502) for morbidity. Moreover, in logistic regression analysis evaluating only transfers, transfer from a CTS center was not associated with increased risk-adjusted odds of mortality or major morbidity (Table 6).
Table 4:
Baseline Characteristics of Transfers by Type of Referring Center
| Transfer from CTS Center | Transfer from Non-CTS Center | p-value | ||
|---|---|---|---|---|
| N | 6.6 (502) | 93.4 (7072) | ||
| Patient Age | 64.8 ± 12.4 | 64.1 ± 10.8 | 0.1927 | |
| Sex (F) | 29.9 (150) | 29 (2053) | 0.6852 | |
| Ejection Fraction | 50 [35 – 60] | 55 [43 – 60] | 0.0032 | |
| Procedure | <.0001 | |||
| Isolated CABG | 66.9 (336) | 85.8 (6065) | ||
| Isolated Valve | 18.7 (94) | 7.4 (520) | ||
| CABG/Valve | 14.3 (72) | 6.9 (487) | ||
| Smoking History | 25.3 (127) | 29.7 (2093) | 0.0388 | |
| Hypertension | 82.5 (414) | 85.8 (6058) | 0.0429 | |
| Diabetes | 45 (226) | 49.1 (3471) | 0.0766 | |
| Peripheral Artery Disease | 13.4 (943) | 14.4 (72) | 0.5304 | |
| Prior Myocardial Infarction | 68.4 (4833) | 66.3 (333) | 0.3372 | |
| Heart Failure | 46.8 (235) | 32.2 (2271) | <.0001 | |
| Previous Cardiac Intervention | 36.1 (181) | 28.1 (1984) | 0.0001 | |
| Reoperation | 13 (65) | 3.5 (247) | <.0001 | |
| Preoperative Length of Stay | 4 [2–6] | 4 [2–6] | 0.1003 | |
| Urgency | 0.0002 | |||
| Elective | 6.2 (31) | 2.8 (195) | ||
| Urgent | 87.9 (441) | 90.9 (6428) | ||
| Emergent | 6 (30) | 6.2 (437) | ||
| Salvage | 0 (0) | 0.2 (11) | ||
| Cardiopulmonary Bypass Time | 101[80–129] | 96 [75–122] | 0.0072 | |
| Cross Clamp Time | 73 [57–95] | 70 [54–90] | 0.0139 | |
| PROMM | 22.3% [12.2–37.7] | 15.4% [9.6–26.8] | <0.001 | |
| PROM | 2.5% [1.13–6.55] | 1.5% [0.73–3.47] | <.0001 | |
Table 5:
Unadjusted Outcomes of Transfers by Type of Referring Center
| Transfer from CTS Center | Transfer from Non-CTS Center | p-value | |
|---|---|---|---|
| Operative Mortality | 4.2 (21) | 2.5 (177) | 0.0226 |
| Major Morbidity | 23.9 (120) | 15 (1062) | <.0001 |
| Prolonged Ventilation | 18.9 (95) | 12 (847) | <.0001 |
| Renal Failure | 4.8 (24) | 2.8 (200) | 0.0126 |
| Permanent Stroke | 1.6 (8) | 1.5 (107) | 0.8868 |
| Need for Reoperation | 4.6 (23) | 2.6 (185) | 0.0092 |
Table 6:
Logistic Regression for Relative Risk of Transfers from Cardiothoracic Surgery Centers vs. Transfers from Non-Cardiothoracic Surgery Centers
| Risk-Adjusted Odds Ratiob | 95% Confidence Interval | p-value | C-statistic | |
|---|---|---|---|---|
| Operative Mortality | 1.177 | 0.708 – 1.957 | 0.5305 | 0.812 |
| Major Morbidity | 1.262 | 0.984–1.618 | 0.0667 | 0.768 |
Adjusted-Odds Ratio Referenced to Transfer from Non Cardiothoracic Surgery Center
Discussion
In the present analysis of all non-elective admissions prior to cardiac surgery within a regional consortium, just over half were admitted as transfers. Overall, transfers had a marginally lower risk profile and fared no worse in terms of postoperative complications than those admitted through the ED. Despite their favorable clinical outcomes, their admissions were associated with higher costs, which seemed to be concentrated in the post-operative non-critical care setting (Central Picture). Within the transfer population, there is a particularly high-risk subset, those transferred from centers that have the ability to perform cardiac surgery. This group’s increased risk is related to the complexity of their cardiovascular disease, and there is a notable referral bias, with the highest risk patients the most likely to be transferred from one CT center to another.
The literature in cardiac surgery evaluating hospital-to-hospital transfer is scarce. To our knowledge, Prabhu et. al. conducted one of the only studies to analyze the impact of inpatient transfers in a general cardiothoracic surgery population.13 In their analysis they observed an increased rate of postoperative nosocomial infections in transferred patients compared to other non-elective admissions (21% vs. 5%), which they concluded was a result of exposure to a longer preoperative hospitalization (11 vs. 6 days). Due to the limitations of our data, we were unable to calculate the preoperative length of stay at the hospital initiating transfer, but we observed a similar duration of pre-operative hospitalization at the operative hospital. Despite this similarity, our results did not support their findings, with no significant differences noted in rates of STS captured infections – pneumonia and deep sternal wound infection. Although their study compared similar patient groups as ours, a number of notable differences between their methodology and the present analysis could explain these discrepancies. Their analysis included a small patient sample size, with only 87 patients in the transfer group, few hospitals contributing data, and all transferred patients were initially admitted at a single institution. All of these factors expose their conclusions to significant bias from individual hospital practices and patient factors. In addition, there was no attempt to reduce these biases with risk-adjustment. Based on the present data, although transferred patients spend more time hospitalized in the preoperative phase, this does not translate to increased rates of hospital-acquired infections.
We found a generally lower risk profile for transferred patients compared to those admitted through the operative hospital’s ED, with outcomes that correspond to those expectations. Given the higher risk nature of transfer patients in other surgical fields, this finding in itself is surprising. However, distinguishing the relative impact that patient risk and the transfer process itself have on outcomes is challenging, yet vitally important. Other surgical fields have struggled with this question. In 2017, three separate studies of patients requiring colorectal surgery, all using data from the American College of Surgeons National Surgical Quality Improvement Program came to conflicting conclusions regarding the contributions of patient factors and transfer status.2,18,19 All three found that patients transferred had worse outcomes, but there was no consensus across studies on the primary cause of these findings. The present analysis is uniquely positioned to add perspective to this uncertainty. In our adjusted analysis of over 7,000 transferred patients there was no increased risk inherent to the process itself. This suggests that the correlation between adverse outcomes and transfer status seen in other fields may be predominantly related to differential patient risks. In fact, the observed morbidity and mortality rates for transfers were less than those predicted by STS risk scores, supporting the conclusion that patients are being appropriately selected for transfer to centers best equipped to manage them. One must note, when applying our findings broadly, this is in the context of a single regional transfer network where communication and inter-facility efficiencies may be different than other regions.
Although there is debate about the causal factors, consistent among the majority of studies on surgical transfer is an observed increase in resource utilization for patients transferred for surgical care.6,7 Much of this has been attributed to a delay in the time to definitive care associated with an increased pre-intervention hospitalization time. In our study, the preoperative length of stay at the operating facility was incrementally shorter in transfer patients compared to those admitted through the ED, with a median time to surgery of four days in both groups. This does not take in to account the initial hospitalization prior to transfer, and if also considered, the overall time from admission to operation may be longer for transferred patients. In addition to the increased overall length of stay, the cost of care to the operating facility was over 5% higher for transferred patients compared to those admitted through the ED. Similar to the interpretation of the preoperative length of stay, one could imagine this cost difference would also be significantly higher if the services rendered at the admitting hospital were included in these calculations.
Given the similarities in complication rates and preoperative stays between transfer and ED admissions, from where might the increased cost arise? The difference is likely attributable to a delay in discharge, which is known to increase hospital costs.20,21 In general, transferred patients had longer postoperative lengths of stay without other discernable reasons since complications rates were similar, and intensive care times shorter. Providers are likely to find more challenges in the coordination of post acute care, while formulating a more conservative discharge plan for patients whose immediate care systems are removed from the operating facility.22 This notion is further supported by data that show a higher likelihood of discharge delays for patients that had unexpected admissions in vascular surgery, demonstrating how preoperative non-clinical factors may influence the discharge process.21 As we observed in this analysis, fewer patients are discharged to rehabilitative facilities, indicating further challenges in the transition from acute care to home. In the future, transfers can be identified as high risk for discharge delays and targeted programs created to help smooth their movement through different phases of care.
To further understand the nature of transfer patients, the type of center they arrived from was used to further stratify transfers. We observed that individuals who are transferred from one cardiac surgery center to another are a particularly high-risk subpopulation. They have elevated operative risk, as a result of their baseline comorbidities and complex cardiovascular diseases. This drives a referral bias such that only the sickest, highest risk patients are transferred from one CT center to another. As a result of this appropriate triage, patients are referred to specialized centers best equipped to manage these patients. In these situations, a cardiac surgeon evaluated the patient, and based on their assessment felt a patient would be best treated at an institution with higher specialization. This highlights the long accepted, but difficult to prove, value of expert evaluation to provide meaningful risk assessment.23 Perhaps, they have a sense of the patient’s frailty or cognitive ability, which may ultimately influence their outcome.24-26 These patients are also likely those with marginal coronary targets, borderline left ventricular viability or difficult to manage valvular abnormalities. Although many of the factors contributing to this risk are measured, commonly used risk stratification tools may not completely capture the relative challenge these patients pose. Irrespective of the trigger to transfer, accepting physicians and hospital administrators must be aware of this high-risk referral bias and support this practice to provide optimal patient care.
This study has a number of limitations including the retrospective methodology that expose the results to bias in patient selection. In addition, transfers of patients for cardiac evaluation who did not ultimately require surgery were not captured in this data set. Incremental differences in outcomes resulted in statistically significant differences, though the clinical importance varies. Finally, this analysis only included patients with calculable STS PROM. While a number of patients with complex concomitant procedures were excluded for this reason, it allowed for proper risk adjustment and better evaluation of the risk imposed by transferring patients.
Conclusions
In conclusion, appropriate regional triage leads to excellent clinical outcomes albeit at the expense of increased healthcare costs. With the knowledge of the costs associated with escalation of care for the most complex patients, alternative reimbursement schemes may be required in order to appropriately reimburse safety net hospitals that accept a large percentage of transfers. Better understanding of, and preparation for complex discharges of transferred patients could help ameliorate some aspects of this problem. In the context of patients admitted prior to their operation, there is no increased risk associated with the transfer process itself, and these referrals allow for patients to be treated at centers best equipped to manage complex disease processes.
Perspective Statement.
Patients transferred for cardiac surgery represent a significant proportion of some surgical practices. This study is the first to analyze cardiac surgery transfers on a large scale and outline unique characteristics related to their care. In addition, we identify a high-risk subpopulation, those transferred from a center that can perform cardiac surgery.
Acknowledgments
Funding: This work was supported by the National Heart, Lung, and Blood Institute (grant T32 HL007849)
Glossary
- CTS
Cardiothoracic Surgery
- CABG
Coronary Artery Bypass Grafting
- ED
Emergency Department
- non-CTS
Non-Cardiothoracic Surgery
- O/E
Observed/Expected
- PROM
Predicted Risk of Mortality
- PROMM
Predicted Risk of Morbidity or Mortality
- STS
Society of Thoracic Surgeons
- VCSQI
Virginia Cardiac Services Quality Initiative
Footnotes
Conflict of Interest: Dr. Ailawadi is a consultant for Abbott, Edwards, Medtronic, and Cephea.
References
- 1.Kummerow Broman K, Ward MJ, Poulose BK, Schwarze ML. Surgical Transfer Decision Making: How Regional Resources are Allocated in a Regional Transfer Network. Jt Comm J QualPatient Saf. 2018;44(1):33–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sharp SP, Schuster DJ, Ata A, et al. Impact of Interhospital Transfer on Outcomes in Non-emergency Colorectal Surgery. World J Surg. 2017. [DOI] [PubMed] [Google Scholar]
- 3.Hsu BS, Schimelpfenig M, Lakhani S. Comparison of Transferred Versus Nontransferred Pediatric Patients Admitted for Sepsis. Air Med J. 2016;35(1):43–45. [DOI] [PubMed] [Google Scholar]
- 4.Kudlow P, Burns KE, Adhikari NK, et al. Inter-hospital transfers and outcomes of critically ill patients with severe acute kidney injury: a multicenter cohort study. Crit Care. 2014;18(5):513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gordon HS, Rosenthal GE. Impact of interhospital transfers on outcomes in an academic medical center. Implications for profiling hospital quality. Med Care. 1996;34(4):295–309. [DOI] [PubMed] [Google Scholar]
- 6.Crippen CJ, Hughes SJ, Chen S, Behrns KE. The impact of interhospital transfers on surgical quality metrics for academic medical centers. Am Surg. 2014;80(7):690–695. [PubMed] [Google Scholar]
- 7.Limmer AM, Edye MB. Interhospital transfer delays emergency abdominal surgery and prolongs stay. ANZ J Surg. 2017;87(11):867–872. [DOI] [PubMed] [Google Scholar]
- 8.Aggarwal B, Raymond C, Jacob J, et al. Transfer of patients with suspected acute aortic syndrome. Am J Cardiol. 2013;112(3):430–435. [DOI] [PubMed] [Google Scholar]
- 9.Kawecki D, Gierlotka M, Morawiec B, et al. Direct Admission Versus Interhospital Transfer for Primary Percutaneous Coronary Intervention in ST-Segment Elevation Myocardial Infarction. JACC Cardiovasc Interv. 2017;10(5):438–447. [DOI] [PubMed] [Google Scholar]
- 10.Nakatsuma K, Shiomi H, Morimoto T, et al. Inter-Facility Transfer vs. Direct Admission of Patients With ST-Segment Elevation Acute Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Circ J. 2016;80(8): 1764–1772. [DOI] [PubMed] [Google Scholar]
- 11.Ward MJ, Kripalani S, Storrow AB, et al. Timeliness of interfacility transfer for ED patients with ST-elevation myocardial infarction. Am JEmergMed. 2015;33(3):423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tarkin J, Malhotra A, Apps A, et al. Inter-hospital transfer for primary angioplasty: delays are often due to diagnostic uncertainty rather than systems failure and universal time metrics may not be appropriate. EuroIntervention. 2015;11(5):511–517. [DOI] [PubMed] [Google Scholar]
- 13.Prabhu S, Blusztein D, Jackson D, et al. The Effect of Treatment Delays Associated with Inpatient Inter-hospital Transfer from Peripheral to Tertiary Hospitals for the Surgical Treatment of Cardiology Patients. Heart Lung Circ. 2016;25(1):75–81. [DOI] [PubMed] [Google Scholar]
- 14.Ailawadi G, LaPar DJ, Speir AM, et al. Contemporary Costs Associated With Transcatheter Aortic Valve Replacement: A Propensity-Matched Cost Analysis. Ann Thorac Surg. 2016; 101(1): 154–160; discussion 160. [DOI] [PubMed] [Google Scholar]
- 15.Osnabrugge RL, Speir AM, Head SJ, et al. Costs for surgical aortic valve replacement according to preoperative risk categories. Ann Thorac Surg. 2013;96(2): 500–506. [DOI] [PubMed] [Google Scholar]
- 16.Hawkins RB, Downs EA, Johnston LE, et al. Impact of Transcatheter Technology on Surgical Aortic Valve Replacement Volume, Outcomes, and Cost. Ann Thorac Surg. 2017;103(6): 1815–1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hawkins RB, Mehaffey JH, Yount KW, et al. Coronary artery bypass grafting bundled payment proposal will have significant financial impact on hospitals. J Thorac Cardiovasc Surg. 2018;155(1):182–188. [DOI] [PubMed] [Google Scholar]
- 18.Sharp SP, Ata A, Valerian BT, Canete JJ, Chismark AD, Lee EC. Complications and surgical outcomes after interhospital transfer vs direct admission in colorectal surgery: A National Surgical Quality Improvement Program analysis. Am J Surg. 2017;213(6): 1031–1037. [DOI] [PubMed] [Google Scholar]
- 19.Chow CJ, Gaertner WB, Jensen CC, Sklow B, Madoff RD, Kwaan MR. Does Hospital Transfer Impact Outcomes After Colorectal Surgery? Dis Colon Rectum. 2017;60(2): 194–201. [DOI] [PubMed] [Google Scholar]
- 20.Landeiro F, Roberts K, Gray AM, Leal J. Delayed Hospital Discharges of Older Patients: A Systematic Review on Prevalence and Costs. Gerontologist. 2017. [DOI] [PubMed] [Google Scholar]
- 21.Houghton JS, Urriza Rodriguez D, Weale AR, Brooks MJ, Mitchell DC. Delayed discharges at a major arterial centre: a 4-month cross-sectional study at a single specialist vascular surgery ward. BMJOpen. 2016;6(9):e011193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mehaffey JH, Hawkins RB, Mullen MG, et al. Access to Quaternary Care Surgery: Implications for Accountable Care Organizations. JAm CollSurg. 2017;224(4): 525–529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pons JM, Borras JM, Espinas JA, Moreno V, Cardona M, Granados A. Subjective versus statistical model assessment of mortality risk in open heart surgical procedures. Ann Thorac Surg. 1999;67(3):635–640. [DOI] [PubMed] [Google Scholar]
- 24.Hawkins RB, Mehaffey JH, Charles EJ, et al. Psoas Muscle Size Predicts Risk-Adjusted Outcomes After Surgical Aortic Valve Replacement. Ann Thorac Surg. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baekelandt BM, Hjermstad MJ, Nordby T, et al. Preoperative cognitive function predicts survival in patients with resectable pancreatic ductal adenocarcinoma. HPB (Oxford). 2016;18(3):247–254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mukka S, Knutsson B, Krupic F, Sayed-Noor AS. The influence of cognitive status on outcome and walking ability after hemiarthroplasty for femoral neck fracture: a prospective cohort study. Eur J Orthop Surg Traumatol. 2017;27(5):653–658. [DOI] [PMC free article] [PubMed] [Google Scholar]