Abstract
Members of several different virus families cause equine viral encephalitis, the majority of which are arthropod-borne viruses (arboviruses) with zoonotic potential. The clinical signs caused are rarely pathognomonic; therefore, a clinical diagnosis is usually presumptive according to the geographical region. However, recent decades have seen expansion of the geographical range and emergence in new regions of numerous viral diseases. In this context, this review presents an overview of the prevalence and distribution of the main viral causes of equine encephalitis and discusses their impact and potential approaches to limit their spread.
Keywords: arbovirus, vector, vaccination, mathematical modeling
Introduction
Viral encephalitis is one of the most common infections of the central nervous system (CNS) in horses worldwide.1 Clinical signs can include mild fever, dullness, sleepiness, listlessness, ataxia, inability to rise trembling, skin twitching, difficulty in urination and defecation, facial paralysis, blindness, seizures, coma, and other non-neurological signs.1,2 The combination, severity, and duration of these clinical signs can vary depending on the etiological agent and its virulence; infection can be fatal. As clinical signs are usually very similar among the different diseases, which specific pathogen is considered depends on geographical areas. This review focuses on the main neurotropic viruses that cause encephalitis in equids and not viruses that can cause other neurological diseases such as equine herpes myeloencephalopathy. Other viruses that cause encephalitis in horses less frequently or affecting a smaller region are listed in Table 1.
Table 1.
Other equine encephalitic viruses
| Family | Genus | Virus | Geographical distribution | Reservoir host | Other hosts | Vector borne | Zoonotic potential | Reference |
|---|---|---|---|---|---|---|---|---|
| Togaviridae | Alphavirus | Highlands J | North America | Birds | Equids | Y | Y | 84,85 |
| Ross River | Australia | Marsupials Horses Birds |
Human | Y | Y | 86,87 | ||
| Middleburg | Africa | Birds | Equids Ruminants Human |
Y | Y | 88–90 | ||
| Sindbis | Africa, Eurasia Australia | Birds | Equids Human | Y | Y | 91 | ||
| Flaviviridae | Flavivirus | Murray valley | Australia New Guinea |
Birds | Equids Cattle Marsupials Fox | Y | Y | 92 |
| Kunjin | Australia | Birds | Equids Human | Y | Y | 92 | ||
| St. Louis encephalitis | North America | Birds | Equids Human | Y | Y | 93 | ||
| Usutu | Africa Europe |
Birds | Human Ruminants Equids |
Y | Y | 90 | ||
| Louping ill | Spain Portugal UK |
Sheep Grouse | Equids Human | Y | Y | 94 | ||
| Powassan | North America Russia | Lagomorphs Rodents Skunks Dogs Birds |
Equids Human | Y | Y | 95 | ||
| Tick-borne encephalitis | Asia Europe Finland Russia |
Small rodents | Equids Human Primates Dogs Ruminants |
Y | Y | 96–98 | ||
| Bunyaviridae | Orthobunyaviridae | California Serogroup (California encephalitis, Jamestown Canyon, La Crosse, Snowshoe hare) |
North America | Rodents Lagomorphs | Equids Human | Y | Y | 99 |
| Shuni Virus | Africa | Ruminants | Equids Human | Y | Y | 100 | ||
| Reoviridae | Orbivirus | African horse sickness | Africa | Equids | - | Y | N | 101 |
| Equine encephalosis | Africa | Equids Elephants |
- | Y | N | 102 |
Prevalence and distribution
Alphaviruses
Encephalitic alphaviruses belonging to the family Togaviridae cause neurological signs in equids and humans on the American continent.3 The most common equine encephalitic viruses are Eastern equine encephalitis (EEE), Western equine encephalitis (WEE), and Venezuelan equine encephalitis (VEE). Collectively known as the equine encephalitides, they are transmitted by mosquitoes and wild birds are the main reservoir host. Horses and humans are considered dead-end hosts for EEE and WEE viruses because they do not generate enough viremia to infect mosquitoes and perpetuate the transmission cycle. On the other hand, equids are the key reservoir host for VEE virus because they develop high titer viremia that can act as source of infection for subsequent feeding mosquitoes.2,4
EEE virus
In North America, EEE has been considered endemic for decades.5 This disease is more prevalent in the Southeastern region of the United States with a high fatality rate. However, since 2005, the geographic range of the virus has spread northwards,6,7 and 8.7% seroprevalence was reported in horses in southern Quebec in 2012.8 Madariaga virus (MADV) is the new species designation for the South American isolates of EEE virus (previously referred to as EEE lineages II, III, and IV) to reflect the different pathogenesis and ecology and genetic divergence from North American strains.9 In Central and South America, small outbreaks of MADV with low fatality rate have been reported between the1930s and 1990s.5 More recently, larger outbreaks of higher morbidity and mortality have occurred.10–12 In Brazil, high fatality rate outbreaks were reported between 2008 and 2009 with 229 horses affected.13 In 2010, seroprevalence of MADV in horses was reported to be 26.3% in Panama and 9.9% in Brazil.11,14
WEE virus
In North America, the WEE virus has traditionally affected states west of the Mississippi river, with the largest outbreaks registered in the 1930s and 1940s in Canada and the United States affecting hundreds of thousands of equids.2 However, no cases have been reported in North America since 1998 and the last time the virus was detected in mosquito pools was in 2008.15
In South and Central America, the last confirmed equine outbreak was reported in Brazil in 2007 and a prevalence of 36.4% has been reported in non-vaccinated horses in the Pantanal region of Brazil in 2010 and 0.4% in 2015.14 The disease is suspected but has not been confirmed in other countries such as Bolivia and Costa Rica. In Uruguay, a fatal human case in 2009 associated with WEE virus encephalitis in a child led to a seroprevalence survey in this country, which revealed a low prevalence of this virus in horses ranging from 3% to 4%.16,17
WEE virus is an example of an apparently declining equine and human pathogen probably caused by a reduction in genetic diversity of circulating lineages, which contrasts with the recent emergence of other arboviruses.15,18
VEE virus
Generally, only the epizootic strains 1-AB and 1-AC of VEE virus produce encephalomyelitis in horses, with a fatality rate close to 90%.19,20 Outbreaks of this disease started in South America and spread northward via Central America up to Mexico and southern Texas affecting hundreds of thousands of horses.21 In Mexico, a high equine seroprevalence has been reported ranging from 17% to 80% in different states between 2003 and 2010.22
Flaviviruses
The family Flaviviridae contains the largest number of viral species that may cause encephalitis in horses. All are zoonotic and transmitted by mosquitoes or ticks (Table 1). The most significant are West Nile virus (WNV) and Japanese encephalitis virus (JEV).1
West Nile virus
West Nile virus is the flavivirus with the widest distribution, which includes all continents (Table 2). In affected regions, WNV is maintained in an enzootic cycle between mosquitoes and birds.23 Horses and humans are considered dead-end hosts because of the low viremia developed, which is not sufficient to transmit the virus back to mosquitoes.3 Experimental studies have demonstrated that only 10% of the infected horses develop neurological signs, but they can be lethal.24 WNV was first isolated in Africa in 1937 and spread to Eurasia and Australia where sporadic outbreaks occurred.25 Since the 1990s, more frequent outbreaks have occurred in the Mediterranean Basin and WNV appeared for the first time in North America in 1999, subsequently spreading across the continent.25,26 Since 2008, a re-emergence of WNV in Central and Southeastern Europe has been observed, with both lineage 1 and lineage 2 WNV involved in outbreaks.27 In Australia, WNV was named Kunjin virus, which was endemic in northern Australia but has caused recent outbreaks of encephalitis in horses in the southeast probably because of enhanced vector transmission.28,29
Table 2.
Recently published seroprevalence of West Nile virus in some countries
| Country | Seroprevalence | Year | Test used | Reference |
|---|---|---|---|---|
| Algeria | 17.4% (26.8% horses, 14.4% donkeys) |
2014 | ELISA confirmed with WB and VNT | 103 |
| Argentina | 16.2% | 2008 | PRNT | 104 |
| Australia (KUNV) | 4.8% | 2011 | cELISA confirmed by PRNT | 105 |
| Brazil | 1.46% | 2004–2009 | ELISA and VNT | 104 |
| Canada | 16.5% | 2012–2014 | ELISA confirmed by PRNT | 106 |
| Chad | 97% | 2003–2004 | 107 | |
| Cote d’Ivoire | 28% | 2003–2005 | 107 | |
| Croatia | 3.43% | 2010–2011 | ELISA confirmed with VNT and PRNT | 108 |
| France | 35% | 2003 | ELISA and VNT | 109 |
| Gabon | 3% | 2004 | 107 | |
| Greece | 33% | 2010 | cELISA | 110 |
| Israel | 84.6% | 2014 | cELISA and VNT | 111 |
| Italy | 39.1% | 2008 | - | 112 |
| Mexico | 26% 45% |
2006 2007 |
cELISA | 113 |
| Morocco | 31% | 2011 | ELISA and VNT | 114 |
| Pakistan | 65% | 2012–2013 | cELISA (anti-pr-E IgG) | 115 |
| Palestine | 48.6% | 2014 | cELISA | 111 |
| Poland | 15.08% | 2012–2013 | VNT | 116 |
| Romania | 58.5% 15.2% |
2010 2006–2008 |
cELISA | 111 |
| Saudi Arabia | 17.3–55.6% (depending on region) |
2013–2015 | ELISA and VNT | 117 |
| Senegal | 92% | 2002–2003 | ELISA confirmed with PRNT | 107 |
| Slovak Republic | 6.9% | 2013 | cELISA and NT | 118 |
| Spain | 7.1% (CI 95% 5.4–11.2%) | 2010 | cELISA and VNT | 119 |
| Tunisia | 28% (95% CI 22–34%) | 2009 | ELISA and VNT | 120 |
| Turkey | 4.9–30.6% (depending on regions) |
2011–2013 | PRNT | 121 |
| Ukraine | 13.5% | 2010–2011 | ELISA and PRNT | 122 |
| USA | 19% (feral horses)a 7.2% (feral horses) |
2008 2009 |
ELISA confirmed by PRNT | 123 |
| Venezuela | 4.3% | 2004–2006 | ELISA confirmed with PRNT | 124 |
Notes: aWidespread vaccination in horses in this country precludes performing seroprevalence studies.
Abbreviations: cELISA, competition ELISA; ELISA, enzyme-linked immunosorbent assay; PRNT, plaque reduction neutralization test; VNT, virus neutralization test.
Japanese encephalitis virus
Japanese encephalitis virus most commonly circulates amongst birds and mosquitoes.30 Pigs are referred to as a virus-amplifying host because they develop high viremia.31 As for EEE virus and WEE virus, horses and humans are dead-end hosts for JEV.32 The virus is endemic in southern areas of Asia and some Pacific countries, such as Malaysia, Indonesia, Singapore, New Guinea and Australia where sporadic outbreaks are observed.33 Whereas in northern Asiatic areas such as Korea, Nepal, China, Taiwan, Japan, northern parts of Vietnam, India or Thailand; seasonal epidemics develop.33 In Korea, around half of 989 horses tested between 2005 and 2007 were antibody positive.34 In India, 10.5% of 637 horses screened between 2006 and 2010 had antibodies against JEV.35
Mononegavirales
Viruses in the order Mononegavirales are large enveloped viruses with a single-stranded negative-sense RNA genome. Several families in the order (Rhabdoviridae, Orthobornaviridae, and Paramyxoviridae) include viruses that can produce encephalitis in animals and humans.36
Rabies virus
Rabies virus, a neurotropic virus in the genus Lyssavirus (family Rhabdoviridae), is one of the deadliest zoonoses worldwide.37 European countries, Iceland, Greenland, New Zealand, and Australia are considered free of this disease, but it is present on the American, African, and Asian continents.38 All mammals are susceptible, but canids and bats are the major vectors. Transmission is via saliva, mainly when a rabid animal bites another animal. Rabies infection is relatively rare in horses; only 23 rabid equids were reported in the United States in 2016 and 13 in 2017.39 Nevertheless, in some African countries, large numbers of rabies cases occur in equids, including donkeys, and there may occasionally be transmission to people.40
Borna disease virus
Borna disease virus-1 (BoDV-1) is a neurotropic pathogen in the genus Orthobornavirus (family Bornaviridae) that causes mononuclear encephalomyelitis in horses.41 This disease is endemic in certain areas in central Europe including Germany, Switzerland, Liechtenstein, and Austria and is usually fatal. The reservoir host of this virus is the bicolored white-toothed shrew (Crocidura leucodon), but natural infection can occur occasionally in equids and other animals such as sheep, cattle, llamas, cats, dogs, and ostriches.42 A landscape modeling study conducted in an endemic area suggested that horses come into contact with shrews in dry habitats such as grasslands and stables.43 In Germany, close to the town of Borna, large numbers of horses died in the late 1800s.42,44 In the 1990s, the incidence was much lower, around 100 horses per year in the endemic area.45 Recently, a new endemic area in Austria was reported after confirmation of lethal disease in horses.46 One case has been reported in the United Kingdom in a horse imported from Germany.47 Antibodies against Bornaviruses have been detected in equids in non-endemic areas of Europe, Iceland, Turkey, Israel, Japan, China, Iran, Australia, and United States.48–53 However, it is not considered proof of infection due to the cross-reactivity with avian Bornaviruses.46 There are sporadic reports of confirmed human BoDV-1 infection including a recent fatal encephalitis case,54 but it is unclear whether these represent interspecies transmission from horses or other hosts. An association between BoDV-1 infection and human neuropsychiatric disease was first reported in 1985,55 although this remains controversial.
Hendra and Nipah virus
The name of in the genus Henipavirus (family Paramyxoviridae) is an amalgamation of Hendra and Nipah. Both species are emerging zoonotic pathogens for which flying foxes (bats in the genus Pteropus) are the reservoir host. Hendra virus (HeV) causes respiratory and often fatal neurological disease in horses and people. It emerged in Brisbane in 1994 and is restricted to Australia.56 Prevalence is low as most cases occur as spillover events to individual horses. There is a risk of human transmission during the preclinical stages of the disease and all infected people had close direct contact with body fluids from infected horses.57
Nipah virus (NiV), which has circulated in Malaysia and Singapore since the late 1990s, has spread to Thailand, India, and Bangladesh.58 It mainly affects domestic pigs and people but can occasionally affect horses producing encephalitis and meningitis.59
Prevention and control
The majority of equine encephalitic viruses are limited to specific geographical areas. Spread to disease-free areas of the world can have catastrophic consequences on equine welfare and industry including mortality, loss of earnings, increased costs (due to veterinary treatment and hospitalization, and preventive measures such as vaccination), as well as public health consequences. For example, outbreaks of African horse sickness in the past have caused 300,000 equine deaths in a short time. It was estimated that the economic cost of such an outbreak in the Netherlands could be more than 500 million Euros.60 In another recent study, it was estimated that the cost of a WNV epidemic in Belgium would be over 30 million euros for equine patients and over 45 million euros for human patients.61
Viral outbreaks are not completely avoidable, but preventative strategies can help restrict their occurrence. Management strategies can also be used in an attempt to eradicate a pathogen from a population or limit its impact. Particularly due to its zoonotic potential, an outbreak of HeV led to the re-evaluation of infection control and equine management practices in Queensland, Australia. Horses can also be used as epidemiological sentinels for human surveillance.2 For example, although horses are not believed to be an amplifying host of EEE virus epidemics, they tend to be the first to show clinical signs, therefore providing the first indication that the virus is circulating.4 Thus, illness detection in horses can trigger measures to prevent associated outbreaks in humans. Viruses can be spread through many different mechanisms, therefore warranting different control strategies.62 New equine encephalitic viruses are still being discovered, for example, HeV and NiV were both first identified in the 1990s,63 and there are likely to be more that remain undiscovered. Control of future emerging virus outbreaks may rely on identifying appropriate strategies already applied to related known diseases. Mathematical modeling can provide an understanding of mechanisms driving disease outbreaks. However, it is important to consider how reliable the values assigned to parameters are (“parameter identifiability”) before mathematical models are used to guide interventions.
Diagnostic techniques
The increasing threat of vector-borne diseases emphasizes the importance of vector surveillance systems and diagnostic tests for early detection of pathogens.64 Early identification of the virus causing equine encephalitis will improve the effectiveness of many disease control measures. As previously mentioned, clinical diagnosis of equine encephalitic viruses is often unreliable due to overlap in the clinical signs seen; therefore, laboratory testing is usually necessary to confirm the etiology of the disease. The OIE (World Organisation for Animal Health) Manual of Diagnostic Tests and Vaccines for Terrestrial Animals describes internationally agreed diagnostic tests for each of the virus species presented in this review with the exception of BoDV-1. The preferred diagnostic test varies for the different viruses and the purpose for which it is being performed, which can include confirmation of a clinical case, surveillance, demonstrating freedom from infection of an individual animal or population and monitoring the response to vaccination. Virus isolation can be time-consuming and for many of the viruses described requires high levels of laboratory containment, but the OIE recommends it as a definitive diagnostic of VEE virus. Polymerase chain reaction (PCR)-based techniques are widely used for virus detection as they offer the advantages of being specific and rapid to perform. However, for some viruses, particularly the flaviviruses, the transient nature of viremia means that RT-PCR tests frequently return false-negative results. Therefore, serological confirmation is necessary. Enzyme-linked immune-sorbent assays (ELISA) are increasingly popular as a relatively inexpensive and rapid diagnostic test. However, cross-reactivity between closely related co-circulating viruses complicates serological testing, particularly for flaviviruses.6 Therefore, confirmatory testing using a virus-neutralizing test such as the plaque-reduction neutralization test is often required. Disease surveillance often includes random testing of animals in order to observe whether a pathogen is present within a population,62 which also requires cost-effective and accurate assays to be developed.
Vaccination
Vaccines are currently available for many of the viruses that cause equine encephalitis (Table 3). An equine vaccine for JEV is notably missing although human vaccines are available and are sometimes administered to horses (eg, in Japan). In contrast, although there are equine vaccines against WNV, there is no human WNV vaccine. Although live-attenuated and inactivated virus vaccines have successfully prevented disease for many decades, these vaccines have some limitations. For example, inactivated virus vaccines typically induce short-lived protective antibody responses and there is a risk of reversion to virulence with inactivated virus vaccines. This has led to the development of second-generation vaccines, such as the live-vectored and DNA vaccines available for WNV. These vaccines often enable a “differentiation of infected from vaccinated animals” (DIVA) approach to be taken whereby diagnostic tests are used that detect antibodies against proteins not generated in response to the vaccine. This can be critical in controlling an emerging virus outbreak as it enables authorities to determine when an outbreak is over by screening for antibodies that only develop in infected animals.
Table 3.
Vaccines licensed for use in horses to protect against viruses that cause encephalitis
| Virus | Vaccine type |
|---|---|
| Eastern equine encephalitis | Inactivated whole virus |
| Western equine encephalitis | Inactivated whole virus |
| Venezuelan equine encephalitis (VEE) | Inactivated whole virus A conditionally available modified live virus (MLV) VEE vaccine has been released during previous outbreaks |
| West Nile | Inactivated whole virus Modified live (canarypox vector expressing prM and E proteins) DNA vaccine |
| Rabies | Inactivated whole virus |
| Hendra | Subunit (recombinant glycoprotein) |
Abbreviations: prM, membrane, E, envelope.
Vaccination coverage is often determined by factors such as economic and logistic issues in developing countries and motivational and legislative issues in developed countries.65 Mass vaccination is not likely to be cost-effective; focusing on high-risk groups would most likely be more appropriate.64 Furthermore, it is not always necessary to vaccinate every individual for a population to be protected. The basic reproduction number, , is the expected number of new infectious cases generated from an individual host during their infectious period. When this value is larger than one (>1), we expect the number of infected individuals to increase, and if is less than one, we expect the disease to die out of the population. Considering this, it is possible to approximate the proportion of a population that require vaccination in order to stop the pathogen circulating, therefore reducing to below unity. By vaccinating a proportion () of the population, the is decreased to . This allows derivation of a condition for this proportion; as must be less than one, we have
This shows that it is not necessary to vaccinate the whole population, as unvaccinated horses will be protected from the vaccination of others, known as herd immunity.65 Empirical studies have confirmed this theoretical idea.66 Vaccination has led to the global eradication of smallpox and rinderpest virus. However, herd immunity and disease eradication are more difficult to achieve for viruses with reservoir host species or insect vectors.
Control of exposure to viral vectors and reservoir hosts
Reducing exposure of horses to wildlife that transmit equine encephalitic viruses can be difficult to achieve. Population control methods such as vaccination and/or sterilization of wild or feral canids have been widely employed to reduce human transmission of rabies.67 However, this approach can cause ethical debate, for example, where poisoning of bats has been used to control rabies in South America.
At the equine premises level, exposure to insect vectors can be reduced by using fly rugs and insect repellents, and stabling horses during peak vector activity (eg, at dusk).62 Other localized methods of vector control include mass trapping and blocking breeding sites by obstructing water surfaces with polystyrene balls.68 Control measures also include reducing mosquito populations.25 The use of pesticides to control vector-borne viruses raises environmental and health concerns and mosquito populations are developing resistance to conventional control agents. There has been an increased interest in the development of biopesticides68 and the creation of genetically modified mosquitoes that cannot transmit pathogens.69–71 Mathematical modeling has predicted that if the abundance of mosquitoes could be reduced such that becomes then WNV would die out.72 Wonham et al (2004) predicted that if the initial size of the New York mosquito population was 40–70% smaller, the outbreak of WNV in 2000 could have been prevented.73 In contrast, reducing the bird population increases the chance of an outbreak as it increases the ratio of mosquitoes to birds making virus transmission more likely, as long as the population is not reduced to the extent that the mosquito population is not maintained. Although mosquitoes are the most common insect vector of equine encephalitic viruses, ticks (eg, Powassan virus74 and louping ill virus) and midges (eg, African horse sickness viruses) can also act as vectors.3
Control of disease spread through international movement of horses
Increased globalization has led to a greater potential for the spread of infectious diseases. Most international equine movements are for competition purposes. The number of prestigious international competition events has increased in the last 10–15 years. There has also been an increase in the number of stallions being transported between the northern and southern hemispheres for breeding; this number rose from 7 in 1989 to over 100 in 2000.63 In addition, horses may be transported as a result of change of ownership or slaughter in the meat industry. Countries often have different strategies of restricting pathogens from entering, including testing and quarantine of imported animals. They may also place restrictions on importation from specific countries to prevent introduction of certain pathogens. However, this can have an impact on the equine industry given the frequent international movement of some horse populations.62 Quarantine, disinfection, pathogen screening, and transport restrictions are useful tools in infection control and biosecurity systems; however, these require optimization for maximum impact.62
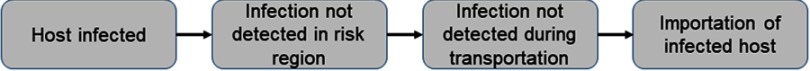
It is not possible to predict when a new virus (either a newly identified pathogen or a known pathogen in a new geographical area) will emerge. However, models to assess the risk of a virus entering a population and changes in risk over time can be developed. There are also models for the risk of disease introduction through host movement.76,77 Countries can be characterized as high risk (virus circulating), low risk (previous outbreaks and/or main vector present), and very low risk. If different host species or reasons for travel are associated with different risk levels then these can be further subdivided into groups. Risk pathways can then be constructed for the steps required for incursion (Figure 1). From these pathways, stochastic risk models that quantify the risk that importation of different groups of animals can be developed. These methods allow us to assess control strategies such as quarantine and their effectiveness on different risk groups.
Figure 1.
Pathway of the steps required for the incursion of a virus due to importation of infected host.
In the case of vector-borne viruses, seasonal prevalence and vector abundance in endemic regions and regions at risk of disease introduction can be taken into account.
Vector-borne diseases are often restricted to temperate climates due to the range of the insects.62 However, with climate change, the areas inhabited by virus-transmitting insects are changing.78,79 The spread of vector-borne viruses is strongly influenced by temperature. Temperature has an effect on the life cycle of the insects, as well as the extrinsic incubation period (the time between a vector acquiring an infectious agent and becoming infectious). The average global temperature is predicted to increase between 1°C and 4.6°C during this century.75 Increased temperatures and altered rainfall patterns are likely to affect the range and behavior of insect vectors.63 Access to breeding sites also has an effect on the distribution of mosquitoes; an increased transmission of EEE virus has been associated with the freshwater hardwood swamps in the Atlantic and Gulf Coast states and the Great Lakes region (USA).4 This is important to consider in the case of vector-borne diseases, as even if an infected host enters a naïve population, the virus cannot spread without the presence of its vector. The main species of vector, geographical distribution, and zoonotic potential vary between equine encephalitic viruses.4 Geographic Information System-based spatial models for predicting locations with high risk have been developed;68,80–82 these use predictor variables such as temperature, rainfall, and landscape/vegetation.25
Whereas some regions may be able to support the vector life cycle throughout the year, viruses may overwinter in unidentified hosts or be re-introduced (eg, by importation or migratory birds) in some climates. Some viruses, such as WNV, are transmitted vertically (from adults to eggs) within mosquito populations; this provides a mechanism for the viruses to be maintained within the population.64 Vector-borne diseases can spread when vectors are carried by the wind. Incursions of JEV into northeastern Queensland are thought to be most likely due to infected mosquitoes blown by the wind from Papua New Guinea.63
International horse movements are not only a threat to naïve populations into which a new pathogen is introduced; the imported equine is also at risk of acquiring disease. An example of this occurred in horses imported to Korea from Ireland, New Zealand, and Australia in 1996 that became infected with JEV.63,83 This highlights the importance of vaccinating horses against viruses they may come into contact before they travel, for example, horses that travel from the United Kingdom may be vaccinated against WNV.63
Conclusion
There is an apparent general increase in viral emergence and re-emergence, particularly of arboviruses. This trend includes viruses that cause potentially devastating encephalitic disease in horses. As a result, there is increasing awareness of the need to monitor disease trends in equine populations, particularly of viruses with zoonotic potential, and to formulate approaches to prevent or control disease outbreaks.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Long MT. West nile virus and equine encephalitis viruses. Vet Clin North Am Equine Pract. 2014;30:523–542. doi: 10.1016/j.cveq.2014.08.001 [DOI] [PubMed] [Google Scholar]
- 2.Kumar B, Manuja A, Gulati B, Virmani N, Tripathi BN. Zoonotic viral diseases of equines and their impact on human and animal health. TOVJ. 2018;12:80–98. doi: 10.2174/1874357901812010080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chapman GE, Baylis M, Archer D, Daly JM. The challenges posed by equine arboviruses. Equine Vet J. 2018;50:436–445. doi: 10.1111/evj.12829 [DOI] [PubMed] [Google Scholar]
- 4.Zacks MA, Paessler S. Encephalitic alphaviruses. Vet Microbiol. 2010;140(3–4):281–286. doi: 10.1016/j.vetmic.2009.08.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brault AC, Powers AM, Villarreal Chavez CL, et al. Genetic and antigenic diversity among eastern equine encephalitis viruses from North, Central, and South America. Am J Trop Med Hyg. 1999;61:579–586. doi: 10.4269/ajtmh.1999.61.579 [DOI] [PubMed] [Google Scholar]
- 6.Graham AC, Ledermann JP, Saxton-Shaw KD, et al. The first outbreak of Eastern equine encephalitis in Vermont: outbreak description and phylogenetic relationships of the virus isolate. PLoS One. 2015;10:e0128712. doi: 10.1371/journal.pone.0128712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rocheleau JP, Arsenault J, Ogden NH, Lindsay LR, Drebot M, Michel P. Characterizing areas of potential human exposure to eastern equine encephalitis virus using serological and clinical data from horses. Epidemiol Infect. 2017;145:667–677. doi: 10.1017/S0950268817000668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rocheleau J-P, Arsenault J, Lindsay LR, et al. Eastern equine encephalitis virus: high seroprevalence in horses from Southern Quebec, Canada, 2012. Vector Borne Zoonotic Dis. 2013;13:712–718. doi: 10.1089/vbz.2012.0964 [DOI] [PubMed] [Google Scholar]
- 9.Riet-Correa F, Nogueira ML, VMK M, et al. Isolation and characterization of madariaga virus from a Horse in Paraíba State, Brazil. Transbound Emerg Dis. 2015;64:990–993. doi: 10.1111/tbed.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aguilar PV, Robich RM, Turell MJ, et al. Endemic eastern equine encephalitis in the Amazon region of Peru. Am J Trop Med Hyg. 2007;76:293–298. doi: 10.4269/ajtmh.2007.76.293 [DOI] [PubMed] [Google Scholar]
- 11.Carrera J-P, Forrester N, Wang E, et al. Eastern equine encephalitis in Latin America. New Engl J Med. 2013;369:732–744. doi: 10.1056/NEJMoa1212628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.de Novaes Oliveira R, Iamamoto K, Silva MLCR, et al. Eastern equine encephalitis cases among horses in Brazil between 2005 and 2009. Arch Virol. 2014;159:2615–2620. doi: 10.1007/s00705-014-2121-4 [DOI] [PubMed] [Google Scholar]
- 13.Silva MLCR, Galiza GJN, Dantas AFM, et al. Outbreaks of eastern equine encephalitis in northeastern Brazil. J Vet Diagn Invest. 2011;23:570–575. doi: 10.1177/1040638711403414 [DOI] [PubMed] [Google Scholar]
- 14.Pauvolid-Corrêa A, Soares Juliano R, Campos Z, Velez J, Nogueira RMR, Komar N. Neutralising antibodies for mayaro virus in Pantanal, Brazil. Mem Inst Oswaldo Cruz. 2015;110:125–133. doi: 10.1590/0074-02760140383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Negi SS, Braun WA, Auguste AJ, Bergren NA, Forrester NL, Weaver SC. Western equine encephalitis virus: evolutionary analysis of a declining alphavirus based on complete genome sequences. J Virol. 2014;88:9260–9267. doi: 10.1128/JVI.01463-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Burgueño A, Frabasile S, Díaz LA, et al. Genomic characterization and seroprevalence studies on alphaviruses in Uruguay. Am J Trop Med Hyg. 2018;98:1811–1818. doi: 10.4269/ajtmh.17-0980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Delfaro A, Burgueño A, Morel N, et al. Fatal human case of Western Equine Encephalitis, Uruguay. Emerg Infect Dis. 2011;17:952–954. doi: 10.3201/eid1701.100876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kading RC, Hartman DA, Bergren NA, et al. Continued evidence of decline in the enzootic activity of western equine encephalitis virus in Colorado. J Med Entomol. 2018;1987:1–5. [DOI] [PubMed] [Google Scholar]
- 19.Estrada-Franco JG, Carrara A-S, Aronson JF, Weaver SC, Gonzalez D. Equine amplification and virulence of subtype IE venezuelan equine encephalitis viruses isolated during the 1993 and 1996 Mexican Epizootics. Emerg Infect Dis. 2012;9:162–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forrester NL, Wertheim JO, Dugan VG, et al. Evolution and spread of Venezuelan equine encephalitis complex alphavirus in the Americas. PLoS Negl Trop Dis. 2017;11:1–19. doi: 10.1371/journal.pntd.0005693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Navarro-Lopez R, Clements T, Freier JE, et al. Venezuelan equine encephalitis virus, Southern Mexico. Emerg Infect Dis. 2012;10:2113–2121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adams AP, Navarro-Lopez R, Ramirez-Aguilar FJ, et al. Venezuelan equine encephalitis virus activity in the Gulf Coast region of Mexico, 2003-2010. PLoS Negl Trop Dis. 2012;6:2003–2010. doi: 10.1371/journal.pntd.0001875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.David S, Abraham AM. Epidemiological and clinical aspects on West Nile virus, a globally emerging pathogen. Infect Dis (Lond). 2016;48:571–586. doi: 10.3109/23744235.2016.1164890 [DOI] [PubMed] [Google Scholar]
- 24.Bunning ML, Bowen RA, Cropp CB, et al. Experimental infection of horses with West Nile virus. Emerg Infect Dis. 2002;8:380–386. doi: 10.3201/eid0804.010239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kramer LD, Styer LM, Ebel GD. A global perspective on the epidemiology of West Nile virus. Annu Rev Entomol. 2008;53:61–81. [DOI] [PubMed] [Google Scholar]
- 26.Hofmeister EK. West Nile virus: north American experience. Integr Zool. 2011;6:279–289. doi: 10.1111/j.1749-4877.2011.00251.x [DOI] [PubMed] [Google Scholar]
- 27.Bakonyi T, Ivanics E, Erdelyi K, et al. Lineage 1 and 2 strains of encephalitic West Nile virus, central Europe. Emerg Infect Dis. 2006;12:618–623. doi: 10.3201/eid1204.051379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.van den Hurk AF, Hall-Mendelin S, Webb CE, et al. Role of enhanced vector transmission of a new West Nile virus strain in an outbreak of equine disease in Australia in 2011. Parasit Vectors. 2014;7:586. doi: 10.1186/1756-3305-7-23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prow NA, Edmonds JH, Williams DT, et al. Virulence and evolution of West Nile Virus, Australia, 1960-2012. Emerg Infect Dis. 2016;22:1353–1362. doi: 10.3201/eid2208.151719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kumar K, Arshad SS, Selvarajah GT, et al. Prevalence and risk factors of Japanese encephalitis virus (JEV) in livestock and companion animal in high-risk areas in Malaysia. Trop Anim Health Prod. 2018;50:741–752. doi: 10.1007/s11250-017-1490-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ricklin ME, Garcia-Nicolas O, Brechbuhl D, et al. Japanese encephalitis virus tropism in experimentally infected pigs. Vet Res. 2016;47:34. doi: 10.1186/s13567-016-0319-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mansfield KL, Hernandez-Triana LM, Banyard AC, Fooks AR, Johnson N. Japanese encephalitis virus infection, diagnosis and control in domestic animals. Vet Microbiol. 2017;201:85–92. doi: 10.1016/j.vetmic.2017.01.014 [DOI] [PubMed] [Google Scholar]
- 33.Wang H, Liang G. Epidemiology of Japanese encephalitis: past, present, and future prospects. Ther Clin Risk Manag. 2015;11:435–448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yang DK, Kim BH, Kweon CH, et al. Serosurveillance for Japanese encephalitis, Akabane, and Aino viruses for Thoroughbred horses in Korea. J Vet Sci. 2008;9:381–385. doi: 10.4142/jvs.2008.9.4.381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gulati BR, Singha H, Singh BK, Virmani N, Kumar S, Singh RK. Isolation and genetic characterization of Japanese encephalitis virus from equines in India. J Vet Sci. 2012;13:111–118. doi: 10.4142/jvs.2012.13.2.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ebihara H, Tomonaga K, Calisher CH, et al. Taxonomy of the order Mononegavirales: update 2017. Arch Virol. 2017;162:2493–2504. doi: 10.1007/s00705-017-3383-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Barecha CB, Girzaw F, Kandi RV, Pal M. Epidemiology and Public Health Significance of Rabies. Perspect Clin Res. 2017;5:55–67. [Google Scholar]
- 38.Rupprecht CE, Willoughby R, Slate D. Current and future trends in the prevention, treatment and control of rabies. Expert Rev Anti Infect Ther. 2006;4:1021–1038. doi: 10.1586/14787210.4.6.1021 [DOI] [PubMed] [Google Scholar]
- 39.Ma X, Monroe B, Cleaton J, Orciary L, Li Y, Al. E. Rabies surveillance in the United States during 2017. J Am Vet Med Assoc. 2018;253:1555–1568. doi: 10.2460/javma.253.8.980 [DOI] [PubMed] [Google Scholar]
- 40.Jemberu WT, Molla W, Almaw G, Alemu S. Incidence of rabies in humans and domestic animals and people’s awareness in North Gondar Zone, Ethiopia. PLoS Negl Trop Dis. 2013;7:e2216–e2216. doi: 10.1371/journal.pntd.0002216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tizard I, Ball J, Stoica G, Payne S. The pathogenesis of bornaviral diseases in mammals. Anim Health Res Rev. 2016;17:92–109. doi: 10.1017/S1466252316000062 [DOI] [PubMed] [Google Scholar]
- 42.Lipkin WI, Briese T, Hornig M. Borna disease virus - Fact and fantasy. Virus Res. 2011;162:162–172. doi: 10.1016/j.virusres.2011.09.036 [DOI] [PubMed] [Google Scholar]
- 43.Hermes N, Eickmann M, Encarnação JA, Herzog S, Becker NI, Herden C. Landscape features and reservoir occurrence affecting the risk for equine infection with Borna disease virus. J Wildl Dis. 2013;49:860–868. doi: 10.7589/2012-10-262 [DOI] [PubMed] [Google Scholar]
- 44.Ludwig H, Bode L. Borna disease virus: new aspects on infection, disease, diagnosis and epidemiology Introduction and historical development. Rev Sci Tech. 2000;19:259–288. [DOI] [PubMed] [Google Scholar]
- 45.Staeheli P, Sauder C, Hausmann J, Schwemmle M, Ehrensperger F. Epidemiology of Borna disease virus. J Gen Virol. 2000;81:2123–2135. doi: 10.1099/0022-1317-81-9-2123 [DOI] [PubMed] [Google Scholar]
- 46.Weissenböck H, Bagó Z, Kolodziejek J, et al. Infections of horses and shrews with Bornaviruses in Upper Austria: A novel endemic area of Borna disease. Emerg Microbes Infect. 2017;6:1–9. doi: 10.1038/emi.2017.36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Priestnall SL, Schoniger S, Ivens PAS, et al. Borna disease virus infection of a horse in Great Britain. Vet Rec. 2011;168:380. doi: 10.1136/vr.c6405 [DOI] [PubMed] [Google Scholar]
- 48.Björnsdóttir S, Agustsdóttir E-L, Blomström A-L, et al. Serological markers of Bornavirus infection found in horses in Iceland. Acta Vet Scand. 2013;55:77. doi: 10.1186/1751-0147-55-77 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Inoue Y, Yamaguchi K, Sawada T, Rivero JC, Horii Y. Demonstration of continuously seropositive population against Borna disease virus in Misaki Feral horses, a japanese strain: a four-year follow-up study from 1998 to 2001. J Vet Med Sci. 2002;64:445–448. doi: 10.1292/jvms.64.445 [DOI] [PubMed] [Google Scholar]
- 50.Kinnunen PM, Billich C, Ek-Kommonen C, et al. Serological evidence for Borna disease virus infection in humans, wild rodents and other vertebrates in Finland. J Clin Virol. 2007;38:64–69. doi: 10.1016/j.jcv.2006.10.003 [DOI] [PubMed] [Google Scholar]
- 51.Pisoni G, Nativi D, Bronzo V, Codazza D. Sero-epidemiological study of Borna disease virus infection in the Italian equine population. Vet Res Comm. 2007;31:245–248. doi: 10.1007/s11259-007-0016-5 [DOI] [PubMed] [Google Scholar]
- 52.Zhang L, Wang X, Zhan Q, et al. Evidence for natural Borna disease virus infection in healthy domestic animals in three areas of western China. Arch Virol. 2014;159:1941–1949. doi: 10.1007/s00705-013-1971-5 [DOI] [PubMed] [Google Scholar]
- 53.Dauphin G, Legay V, Pitel P, Zientara S. Borna disease: current knowledge and virus detection in France. Vet Res. 2002;33:127–138. doi: 10.1051/vetres:2002002 [DOI] [PubMed] [Google Scholar]
- 54.Korn K, Coras R, Bobinger T, et al. Fatal encephalitis associated with Borna disease virus 1. New Engl J Med. 2018;379:1375–1377. doi: 10.1056/NEJMc1800724 [DOI] [PubMed] [Google Scholar]
- 55.Rott R, Herzog S, Fleischer B, et al. Detection of serum antibodies to Borna disease virus in patients with psychiatric disorders. Science. 1985;228:755–756. doi: 10.1126/science.3922055 [DOI] [PubMed] [Google Scholar]
- 56.Middleton D. Hendra virus. Vet Clin North Am Eq Pract. 2014;30:579–589. doi: 10.1016/j.cveq.2014.08.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marsh G, Haining J, Hancock TJ, et al. Experimental infection of horses with Hendra virus/Australia/horse/2008/Redlands. Emerg Infect Dis. 2011;17:2232–2238. doi: 10.3201/eid1712.111162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Daszak P, Plowright RK, Epstein JH, et al. The emergence of Nipah and Hendra virus: pathogen dynamics across a wildlife-livestock-human continuum In: Collinge SK, Ray C, editors. Disease Ecology: Community Structure and Pathogen Dynamics. Oxford: Oxford University Press; 2006:186–201. [Google Scholar]
- 59.Hooper P, Zaki S, Daniels P, Middleton D. Comparative pathology of the diseases caused by Hendra and Nipah viruses. Microbes Infect. 2001;3:315–322. [DOI] [PubMed] [Google Scholar]
- 60.Robin M, Page P, Archer D, Baylis M. African horse sickness: the potential for an outbreak in disease-free regions and current disease control and elimination techniques. Equine Vet J. 2016;48:659–669. doi: 10.1111/evj.12600 [DOI] [PubMed] [Google Scholar]
- 61.Humblet M, Vandeputte S, Fecher-Bourgeois F, et al. Estimating the economic impact of a possible equine and human epidemic of West Nile virus infection in Belgium. Euro Surveill. 2016;21(31):pii=30309. doi: 10.2807/1560-7917.ES.2016.21.31.30309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Weese JS. Infection control and biosecurity in equine disease control. Equine Vet J. 2014;46:654–660. doi: 10.1111/evj.12295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Timoney PJ. Factors influencing the international spread of equine diseases. Vet Clin North Am Equine Pract. 2000;16:537–551. [DOI] [PubMed] [Google Scholar]
- 64.Kaaijk P, Luytjes W. Are we prepared for emerging flaviviruses in Europe? Challenges for vaccination. Hum Vaccin Immunother. 2018;14:337–344. doi: 10.1080/21645515.2017.1389363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Nokes DJ, Anderson RM. The use of mathematical models in the epidemiological study of infectious diseases and in the design of mass immunization programmes. Epidemiol Infect. 1988;101:1–20. doi: 10.1017/s0950268800029186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Anderson RM, May RM. The invasion, persistence and spread of infectious diseases within animal and plant communities. Philos Trans R Soc Lond B Biol Sci. 1986;314:533–570. doi: 10.1098/rstb.1986.0072 [DOI] [PubMed] [Google Scholar]
- 67.Zinsstag J, Lechenne M, Laager M, et al. Vaccination of dogs in an African city interrupts rabies transmission and reduces human exposure. Sci Transl Med. 2017;9:eaaf6984. doi: 10.1126/scitranslmed.aaf6984 [DOI] [PubMed] [Google Scholar]
- 68.Curtis C. Insecticide-treated nets against malaria vectors and polystyrene beads against Culex larvae. Trends Parasitol. 2005;21:504–507. doi: 10.1016/j.pt.2005.08.025 [DOI] [PubMed] [Google Scholar]
- 69.Coutinho-Abreu IV, Zhu KY, Ramalho-Ortigao M. Transgenesis and paratransgenesis to control insect-borne diseases: current status and future challenges. Parasitol Int. 2010;59:1–8. doi: 10.1016/j.parint.2009.10.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lacey LA, Frutos R, Kaya HK, Vail P. Insect pathogens as biological control agents: do they have a future? Biol Control. 2001;21:230–248. doi: 10.1006/bcon.2001.0938 [DOI] [Google Scholar]
- 71.Sinkins SP, Gould F. Gene drive systems for insect disease vectors. Nature Rev Genet. 2006;7:427–435. doi: 10.1038/nrg1870 [DOI] [PubMed] [Google Scholar]
- 72.Bowman C, Gumel AB, van den Driessche P, Wu J, Zhu H. A mathematical model for assessing control strategies against West Nile virus. Bull Math Biol. 2005;67:1107–1133. doi: 10.1016/j.bulm.2005.01.002 [DOI] [PubMed] [Google Scholar]
- 73.Wonham MJ, de-Camino-Beck T, Lewis MA. An epidemiological model for West Nile virus: invasion analysis and control applications. Proc Biol Sci. 2004;271:501–507. doi: 10.1098/rspb.2003.2608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Keane DP, Little PB. Equine viral encephalomyelitis in Canada: a review of known and potential causes. Can Vet J. 1987;28:497–504. [PMC free article] [PubMed] [Google Scholar]
- 75.Ecology WB. How climate change alters rhythms of the wild. Science. 2000;287:793–795. doi: 10.1126/science.287.5454.793 [DOI] [PubMed] [Google Scholar]
- 76.de Vos CJ, Hoek CA, Nodelijk G. Risk of introducing African horse sickness virus into the Netherlands by international equine movements. Prev Vet Med. 2012;106(2):108–122. doi: 10.1016/j.prevetmed.2012.01.019 [DOI] [PubMed] [Google Scholar]
- 77.Faverjon C, Leblond A, Hendrikx P, et al. A spatiotemporal model to assess the introduction risk of African horse sickness by import of animals and vectors in France. BMC Vet Res. 2015;11:127. doi: 10.1186/s12917-015-0435-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Githeko AK, Lindsay SW, Confalonieri UE, Patz JA. Climate change and vector-borne diseases: a regional analysis. Bull WHO. 2000;78:1136–1147. [PMC free article] [PubMed] [Google Scholar]
- 79.Reiter P. Climate change and mosquito-borne disease: knowing the horse before hitching the cart. Rev Sci Tech. 2008;27:383–398. [PubMed] [Google Scholar]
- 80.Kelen PV, Downs JA, Unnasch T, Stark L. A risk index model for predicting eastern equine encephalitis virus transmission to horses in Florida. Appl Geog. 2014;48:79–86. doi: 10.1016/j.apgeog.2014.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Moncayo AC, Edman JD, Finn JT. Application of geographic information technology in determining risk of eastern equine encephalomyelitis virus transmission. AMCA. 2000;16:28–35. [PubMed] [Google Scholar]
- 82.Zou L, Miller SN, Schmidtmann ET. A GIS tool to estimate West Nile virus risk based on a degree-day model. Environ Monit Assess. 2007;129:413–420. doi: 10.1007/s10661-006-9373-8 [DOI] [PubMed] [Google Scholar]
- 83.University of Kentucky. Equine Disease. 1997. Available from: https://gluck.ca.uky.edu/sites/gluck.ca.uky.edu/files/q_oct_1997.pdf. Accessed July 8, 2019. [Google Scholar]
- 84.Borland EM, Ledermann JP, Powers AM. Culex Tarsalis Mosquitoes as Vectors of Highlands J Virus. Vector-Borne Zoonotic Dis. 2016;16:558–565. doi: 10.1089/vbz.2015.1907 [DOI] [PubMed] [Google Scholar]
- 85.Karabatsos N, Lewis AL, Calisher CH, Hunt AR, Roehrig JT. Identification of Highlands J virus from a Florida horse. Am J Trop Med Hyg. 1988;39:603–606. doi: 10.4269/ajtmh.1988.39.603 [DOI] [PubMed] [Google Scholar]
- 86.Gummow B, Tan RHH, Joice RK, Burgess G, Picard J. Seroprevalence and associated risk factors of mosquito-borne alphaviruses in horses in northern Queensland. Aust Vet J. 2018;96:243–251. doi: 10.1111/avj.12711 [DOI] [PubMed] [Google Scholar]
- 87.Stephenson EB, Peel AJ, Reid SA, Jansen CC, McCallum H. The non-human reservoirs of Ross River virus: A systematic review of the evidence. Parasit Vectors. 2018;11:1–13. doi: 10.1186/s13071-017-2573-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Attoui H, Sailleau C, Jaafar FM, et al. Complete nucleotide sequence of Middelburg virus, isolated from the spleen of a horse with severe clinical disease in Zimbabwe. J Gen Virol. 2007;88:3078–3088. doi: 10.1099/vir.0.83076-0 [DOI] [PubMed] [Google Scholar]
- 89.Burt FJ, Goedhals D, Mathengtheng L. Arboviruses in southern Africa: are we missing something? Future Virol. 2014;9:993–1008. doi: 10.2217/fvl.14.87 [DOI] [Google Scholar]
- 90.Venter M. Assessing the zoonotic potential of arboviruses of African origin. Curr Opin Virol. 2018;28:74–84. doi: 10.1016/j.coviro.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 91.Niekerk SV, Human S, Williams J, Wilpe EV, Pretorius M, Swanepoel R. Neurologic disease in horses, South Africa. Emerg Infect Dis. 2015;21:2225–2229. doi: 10.3201/eid2112.150132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Boyle DB, Dickerman RW, Marshall ID. Primary viraemia responses of herons to experimental infection with Murray Valley encephalitis, Kunjin and Japanese encephalitis viruses. Austr J Exp Biol Med Sci. 1983;61:655–664. doi: 10.1038/icb.1983.62 [DOI] [PubMed] [Google Scholar]
- 93.White GS, Symmes K, Sun P, et al. Reemergence of St. Louis encephalitis virus, California, 2015. Emerg Infect Dis. 2016;22:2185–2188. doi: 10.3201/eid2212.160805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Hyde J, Nettleton P, Marriott L, Willoughby K. Louping ill in horses. Vet Rec. 2007;160:532. doi: 10.1136/vr.160.4.105 [DOI] [PubMed] [Google Scholar]
- 95.Little PB, Thorsen J, Moore W, Weninger N. Powassan viral encephalitis: a review and experimental studies in the horse and rabbit. Vet Pathol. 1985;22:500–507. [DOI] [PubMed] [Google Scholar]
- 96.Rieille N, Klaus C, Hoffmann D, Péter O, Voordouw MJ. Goats as sentinel hosts for the detection of tick-borne encephalitis risk areas in the Canton of Valais, Switzerland. BMC Vet Res. 2017;13:1–13. doi: 10.1186/s12917-016-0931-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Rushton JO, Lecollinet S, Hubálek Z, Svobodová P, Lussy H, Nowotny N. Tick-borne encephalitis virus in horses, Austria, 2011. Emerg Infect Dis. 2013;19:635–637. doi: 10.3201/eid1904.121450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Yoshii K, Song JY, Park SB, Yang J, Schmitt HJ. Tick-borne encephalitis in Japan, Republic of Korea and China. Emerg Microbes Infect. 2017;6:e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Beaty BJ, Bishop DHL. Bunyavirus-vector interactions. Virus Res. 1988;10:289–301. [DOI] [PubMed] [Google Scholar]
- 100.van Eeden C, Williams JH, Gerdes TGH, et al. Shuni virus as cause of neurologic disease in horses. Emerg Infect Dis. 2012;18:318–321. doi: 10.3201/eid1802.111403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Carpenter S, Mellor PS, Fall AG, Garros C, Venter GJ. African horse sickness virus: history, transmission, and current status. Annu Rev Entomol. 2017;62:343–358. doi: 10.1146/annurev-ento-031616-035010 [DOI] [PubMed] [Google Scholar]
- 102.Dhama K, Pawaiya R, Karthik K, Chakraborty S, Tiwari R, Verna A. Equine encephalosis virus (EEV): a review. AJAVA. 2014;9:123–133. [Google Scholar]
- 103.Lafri I, Prat CM, Bitam I, et al. Seroprevalence of West Nile virus antibodies in equids in the North-East of Algeria and detection of virus circulation in 2014. Comp Immunol Microbiol Infect Dis. 2017;50:8–12. doi: 10.1016/j.cimid.2016.11.005 [DOI] [PubMed] [Google Scholar]
- 104.Silva JR, Medeiros LC, Reis VP, et al. Serologic survey of West Nile virus in horses from Central-West, Northeast and Southeast Brazil. Mem Inst Oswaldo Cruz. 2013;108:921–923. doi: 10.1590/S0074-02762013005000001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Prow NA, Tan CS, Wang W, et al. Natural exposure of horses to mosquito-borne flaviviruses in south-east Queensland, Australia. Int J Environ Res Public Health. 2013;10:4432–4443. doi: 10.3390/ijerph10094432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Rocheleau JP, Michel P, Lindsay LR, et al. Emerging arboviruses in Quebec, Canada: assessing public health risk by serology in humans, horses and pet dogs. Epidemiol Infect. 2017;145:2940–2948. doi: 10.1017/S0950268817002205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Cabre O, Grandadam M, Marie JL, et al. West Nile Virus in horses, sub-Saharan Africa. Emerg Infect Dis. 2006;12:1958–1960. doi: 10.3201/eid1212.060042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Barbic L, Listes E, Katic S, et al. Spreading of West Nile virus infection in Croatia. Vet Microbiol. 2012;159:504–508. doi: 10.1016/j.vetmic.2012.04.038 [DOI] [PubMed] [Google Scholar]
- 109.Durand B, Dauphin G, Zeller H, et al. Serosurvey for West Nile virus in horses in southern France. Vet Rec. 2005;157:711–713. doi: 10.1136/vr.157.22.711 [DOI] [PubMed] [Google Scholar]
- 110.Bouzalas IG, Diakakis N, Chaintoutis SC, et al. Emergence of equine west nile encephalitis in central Macedonia, Greece, 2010. Transbound Emerg Dis. 2016;63:e219–e227. doi: 10.1111/tbed.12334 [DOI] [PubMed] [Google Scholar]
- 111.Ludu Oslobanu EL, Mihu-Pintilie A, Anita D, Anita A, Lecollinet S, Savuta G. West Nile virus reemergence in Romania: a serologic survey in host species. Vector Borne Zoonotic Dis. 2014;14:330–337. doi: 10.1089/vbz.2013.1405 [DOI] [PubMed] [Google Scholar]
- 112.Calistri P, Giovannini A, Savini G, et al. West Nile virus transmission in 2008 in north-eastern Italy. Zoonoses Public Health. 2010;57:211–219. doi: 10.1111/j.1863-2378.2009.01303.x [DOI] [PubMed] [Google Scholar]
- 113.Ibarra-Juarez L, Eisen L, Bolling BG, et al. Detection of West Nile virus-specific antibodies and nucleic acid in horses and mosquitoes, respectively, in Nuevo Leon State, northern Mexico, 2006-2007. Med Vet Entomol. 2012;26:351–354. doi: 10.1111/j.1365-2915.2012.01014.x [DOI] [PubMed] [Google Scholar]
- 114.Benjelloun A, El Harrak M, Calistri P, et al. Seroprevalence of West Nile virus in horses in different Moroccan regions. Vet Med Sci. 2017;3:198–207. doi: 10.1002/vms3.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zohaib A, Saqib M, Beck C, et al. High prevalence of West Nile virus in equines from the two provinces of Pakistan. Epidemiol Infect. 2015;143:1931–1935. doi: 10.1017/S0950268814002878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Bazanow B, Jansen van Vuren P, Szymanski P, et al. A survey on West Nile and Usutu viruses in horses and birds in Poland. Viruses. 2018;10:E87. doi: 10.3390/v10020087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Hemida MG, Perera R, Chu DKW, Ko RLW, Alnaeem AA, Peiris M. West Nile virus infection in horses in Saudi Arabia (in 2013-2015). Zoonoses Public Health. 2019;66:248–253. doi: 10.1111/zph.12532 [DOI] [PubMed] [Google Scholar]
- 118.Csank T, Drzewniokova P, Korytar L, et al. A SEROSURVEY OF FLAVIVIRUS INFECTION IN HORSES AND BIRDS IN Slovakia. Vector Borne Zoonotic Dis. 2018;18:206–213. doi: 10.1089/vbz.2017.2216 [DOI] [PubMed] [Google Scholar]
- 119.Garcia-Bocanegra I, Arenas-Montes A, Napp S, et al. Seroprevalence and risk factors associated to West Nile virus in horses from Andalusia, Southern Spain. Vet Microbiol. 2012;160:341–346. doi: 10.1016/j.vetmic.2012.06.027 [DOI] [PubMed] [Google Scholar]
- 120.Bargaoui R, Lecollinet S, Lancelot R. Mapping the serological prevalence rate of West Nile fever in equids, Tunisia. Transbound Emerg Dis. 2015;62:55–66. doi: 10.1111/tbed.12077 [DOI] [PubMed] [Google Scholar]
- 121.Ergunay K, Gunay F, Erisoz Kasap O, et al. Serological, molecular and entomological surveillance demonstrates widespread circulation of West Nile virus in Turkey. PLoS Negl Trop Dis. 2014;8(7):e3028. doi: 10.1371/journal.pntd.0003028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Ziegler U, Skrypnyk A, Keller M, et al. West nile virus antibody prevalence in horses of Ukraine. Viruses. 2013;5:2469–2482. doi: 10.3390/v5102469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Franson JC, Hofmeister EK, Collins GH, Dusek RJ. Seroprevalence of West Nile virus in feral horses on Sheldon National Wildlife Refuge, Nevada, United States. Am J Trop Med Hyg. 2011;84:637–640. doi: 10.4269/ajtmh.2011.10-0467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Bosch I, Herrera F, Navarro JC, et al. West Nile virus, Venezuela. Emerg Infect Dis. 2007;13:651–653. doi: 10.3201/eid1304.061383 [DOI] [PMC free article] [PubMed] [Google Scholar]