Abstract
Objective:
The aim of the study was to compare the effect of previously used contraceptive methods on women’s short- and long-term fecundity. Use of hormonal contraception (HC) was compared with use of a contraceptive mobile application (app).
Methods:
This real-life prospective observational study comprised 2874 women who were attempting to become pregnant using the Natural Cycles mobile app to monitor their fertility. The women registered to use the app between August 2014 and June 2016 with the intention of planning a pregnancy, and had previously either used the same app to prevent pregnancy or had recently discontinued HC use. We calculated the average time to pregnancy (TTP) for all women who became pregnant during the study, and performed Kaplan–Meier life-table analysis to examine the cumulative probabilities of pregnancy for all women in the study.
Results:
The average TTP was 2.3 (95% confidence interval [CI] 2.1, 2.4) and 3.7 (95% CI 3.4, 3.9) cycles for women who had previously used Natural Cycles and HC, respectively. The time to reach 30% pregnancy probability for women previously on HC was 1.6 (95% CI 1.5, 1.8) times longer than for women previously using Natural Cycles. There was no significant difference in 13 cycle cumulated pregnancy probability between the two groups.
Conclusion:
The results show that fertility awareness-based methods of contraception increase short-term pregnancy rates relative to HC, but have no effect on long-term pregnancy rates.
Keywords: Conception rate, contraceptive, mobile application, subfertility, time to pregnancy
Introduction
The probability of conception, the time to conceive and the factors that affect these quantities are of great interest in measuring human fertility and improving the management of infertility. Prospective studies have analysed attempts to become pregnant among different populations [1–7], retrospective studies have focused on women’s post-conception estimates of time to pregnancy (TTP) [8–14], and theoretical studies have reported methods [8–10] and statistical models [11] for describing fertility and conception. Various factors such as age [12–14], body mass index (BMI) [5,15–18], menstrual cycle characteristics [19,20] and lifestyle factors such as smoking [21] and alcohol consumption [22] have all been shown to affect female fertility.
Particular interest has focused on the possible impact of previous use of hormonal contraception (HC) on conception rates and TTP. Several studies [3,23–28] show that HC negatively affects conception rates in the initial cycles after discontinuation. Many studies, however, indicate that HC use does not affect 1 year pregnancy rates [28,29]. Recent research into the side effects of HC [30–33], along with the known delay of conception, constitutes strong motivation for research into how other contraceptives compare in this regard.
A few studies have investigated the effect of using fertility awareness-based (FAB) methods to improve fertility [34], so far mainly focusing on symptothermal or Billings-type methods [4,35,36] in which women through fairly simple self-diagnosis of menstruation days and cervical mucus quality are able to predict their ovulation date and fertile days. Pregnancy rates have been shown to be significantly higher when couples time intercourse for the days of highest predicted fertility [36], which is especially helpful for couples who cannot or do not want to follow the proposal of Wilcox et al. [37] to have intercourse two to three times per week. A recent study showed that the conception rates for couples with known subfertility could be significantly improved through dedicated use of FAB methods [38].
The aim of this study was to investigate the conception rates of women who discontinued contraception just prior to attempting pregnancy. In particular, we aimed to compare the pregnancy probability of women who used HC to that of women who used a FAB method for contraception. Specifically, we analysed data from users of the fertility monitoring device Natural Cycles. The great advantage of prospectively studying such user data is that it presents an opportunity to gain insight into the reproductive behaviour of women in a real-life environment, independently of potential bias arising from clinical settings or interactions with health care professionals.
Methods
Digital fertility monitor
This study was conducted among users of the mobile application (app) Natural Cycles (NaturalCycles Nordic, Stockholm, Sweden). The app requires user input of basal body temperature recordings and dates of menstruation. Optionally, users may also enter urinary luteinising hormone (LH) test results. The fertility-related data are entered into devices such as smartphones, tablets or laptops.
The underlying technology is a statistical algorithm [39] that calculates a fertility status for each day depending on the estimated probability of conception on that day. Peak fertility is normally given on the day before estimated ovulation [40], and the other days on which fertility is indicated belong to the fertile window associated with the days immediately preceding this day, as well as the ovulation day itself [37,41]. The algorithm can identify the ovulation day with a precision comparable to that of clinical methods of ovulation detection such as ultrasound [42]. In addition to ovulation day, the algorithm computes the following variables and their uncertainties: luteal phase length, follicular phase length and cycle length, as well as average body temperature during the different phases. The app also calculates the rate of anovulatory cycles. Women indicate in their profile setting whether they are using the app to prevent or to plan a pregnancy. A study conducted in 2016 showed that the typical use failure rate of the Natural Cycles app when used as a contraceptive is 7.0 pregnancies per 100 woman-years [43].
The algorithm improves its predictions using previously recorded cycles from the same woman and can provide predictions of the fertility status, ovulation and menstruation days for up to five cycles in advance. In addition to menstruation, basal body temperature and LH test results, the user may enter information about pregnancy test results and sexual activity as well as personal notes. The user is encouraged to take a pregnancy test and register the results in the app if the data indicate a possible pregnancy.
Study design
This prospective observational analysis studied women aged 20 years and older from an international population, the majority (~90%) of whom were from Sweden. The general sociodemographic characteristics of the participants are presented in Table 1. There were no significant differences between the HC and Natural Cycles groups with respect to age, BMI or country of residence. Recruitment was performed by means of conventional end-consumer marketing techniques. Every user who registered for the app agreed to share data anonymously for subsequent research. Women included in the study registered with the Natural Cycles app for the purpose of planning a pregnancy at the earliest on 1 August 2014 and at the latest 90 days before the conclusion of the study on 5 September 2016. Participants had to enter data for at least 10 days in total, of which at least 1 day included basal body temperature. Each daily data point could be any combination of menstruation, basal body temperature or LH test results, pregnancy test result, sexual activity or a personal note for a specific date. All cycles entered in the pregnancy planning mode, including anovulatory cycles, were considered in the study. At registration, users were asked questions related to their individual cycle, previous contraception and date of birth, as well as self-reported height and weight before starting to use the fertility monitor. The study protocol was reviewed and approved on 1 December 2016 by the Stockholm regional ethics committee (no. 2016/2037–31/2). All participants provided informed consent through the online app.
Table 1.
Sociodemographic characteristics of all women in the study and subdivided into the two cohorts.
| Characteristic | NC, prevent mode | HC | All users |
|---|---|---|---|
| No. of users | 1284 | 1590 | 2874 |
| Age,a years | 28.4±3.7 | 27.8±4.0 | 28.1±3.9 |
| BMI,b kg/m2 | 23.5±3.9 | 23.8±4.3 | 23.7±4.2 |
| Country of residence, % | |||
| Sweden | 84.1 | 87.9 | 86.2 |
| Norway | 5.0 | 3.8 | 4.3 |
| USA | 4.2 | 2.0 | 3.0 |
| Other | 6.7 | 6.3 | 6.5 |
Values for age and BMI are given as means ± 1 SD.
The three largest nationalities (Sweden, Norway and the USA) were the largest groups in both cohorts.
Age at which the user started attempting to become pregnant.
For 213 women information about height was lacking, and BMI could thus not be calculated.
NC, Natural Cycles.
Previous contraception
Users were considered for this study only if they fulfilled either of the following criteria: (1) they had previously used HC and had discontinued use less than 2 months prior to signing up for Natural Cycles; (2) they had used Natural Cycles in the ‘prevent pregnancies’ mode prior to deciding to become pregnant. To be considered for this category the user was required to have added at least 60 days of data while using Natural Cycles for pregnancy prevention.
Data analysis
In addition to determining the TTP for users who became pregnant, life-table analysis was used to calculate the cumulative probability of pregnancy. This analysis included users who did not achieve pregnancy, thus yielding a better measure of the fecundity of the entire investigated sample. The Kaplan–Meier estimate [44] is useful for studies where a high dropout rate is expected, since it prevents artificially overestimating fertility because of early dropout of women who did not conceive [4].
Two particularities of our sample meant standard methods based on the assumption of proportional hazards (e.g. Cox regression [45]) were not appropriate for comparing the two categories: (1) we expected the women who had previously used HC to experience a shorter period of hormone-induced lowered fertility, which would subside with time; and (2) the expected fertility increase [36] resulting from the app itself was likely to affect the two categories differently, as one group had already used it for some time.
To compare the cumulative probability of pregnancy of the two categories of women, we calculated the time at which a group of women exposed to a certain risk factor reached a given cumulative probability of pregnancy, divided by the comparable time for a control subset. We denoted this ratio as the Kaplan–Meier ratio (KMR). The threshold for the study was 30%, as this was low enough to ensure good statistical accuracy while at the same time high enough not to introduce uncertainties related to interpolation. In order to understand the long-term effects on fecundity, we also compared the 13 cycle pregnancy probabilities.
Results are presented with their associated 95% confidence intervals (CIs); a two-sided p-value represents the probability that the ratio is consistent with 1. A p-value of 0.05 or lower was considered statistically significant.
Results
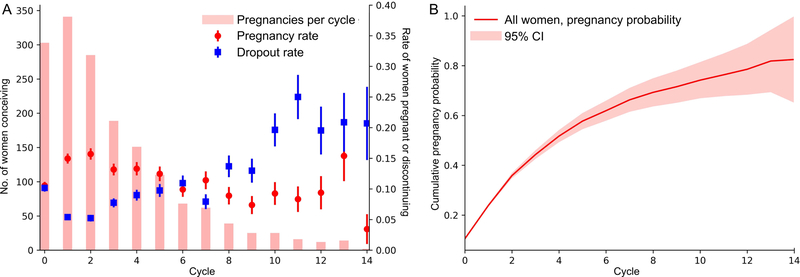
A total of 2934 women were included in the study. The total number of cycles observed was 10,409. The 13 cycle pregnancy probability for the entire group was 78.6% (95% CI 68.3%, 88.9%). A total of 1656 participants registered a positive pregnancy test on the app. The average time from beginning to use the app for planning a pregnancy until entering the first positive pregnancy test was 120 days. As the participants could start using the app at any point in their cycle, the starting cycle is denoted as cycle 0 to distinguish it from subsequent full cycles. Using this definition, conception occurred on average in cycle 3.02±3.07 (1 standard deviation [SD]). Hereafter, and in the abstract, for simplicity we report the average TTP as x cycles instead of in cycle x. The maximum number of observations was 24 cycles, and the last cycle with a pregnancy occurrence was cycle 20. Figure 1 shows in which cycle pregnancy occurred for women who became pregnant in the first 15 cycles, along with the pregnancy probability (including women who did not become pregnant in these cycles) and dropout rate in that cycle. Many users pay their usage fees annually, leading to an expected peak in the discontinuation rate at around 12 months (cycles 11–12 in Figure 1). The cumulative probability of pregnancy and 95% CIs are shown in Figure 1. The results presented in this section are summarised in Table 2.
Figure 1.
(A) Conceptions per cycle (bars, left axis), pregnancy rates per cycle (red) and dropout rate per cycle (blue). Error bars indicate one standard deviation. (B) Kaplan-Meier estimate of cumulative pregnancy rate and 95% Confidence Interval per cycle. The observed peak in dropout rates around cycle 11–12 corresponds to the 1-year renewal of subscriptions.
Table 2.
Summary of results of all women in the study and subdivided into the two cohorts.
| Variable | NC, prevent mode | HC | All users |
|---|---|---|---|
| No. of users | 1284 | 1590 | 2874 |
| No. of pregnancies | 738 | 918 | 1656 |
| Average TTPa | 2.25 (2.07, 2.43) | 3.65 (3.43, 3.87) | 3.02 (2.90, 3.14) |
| Time to 30% pregnancy probabilitya | 1.11 (1.05, 1.25) | 1.81 (1.77, 1.95) | 1.48 (1.46, 1.60) |
Average TTP and time to 30% pregnancy probability are given as no. of cycles with 95% CIs in parentheses.
NC, Natural Cycles.
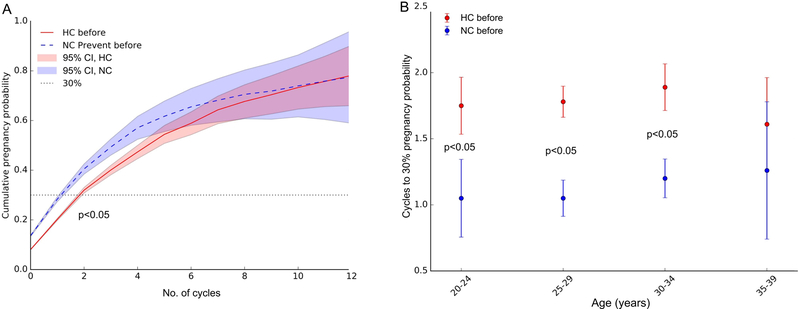
A total of 1590 women had self-reported previous use of HC during the last 2 months of starting to try to conceive, while 1284 women had logged at least 60 days using Natural Cycles to prevent pregnancy prior to switching to the pregnancy planning mode. Women who had previously used Natural Cycles had an average TTP of 2.25 (95% CI 2.07, 2.43) cycles, and women who had previously used HC had an average TTP of 3.65 (95% CI 3.43, 3.87) cycles. Women who had previously used HC took on average 146 days to become pregnant after starting to use the app, while women who had previously used Natural Cycles to prevent pregnancy took on average 85 days to become pregnant. The KMR when using the women on HC as the control group was 1.62 (95% CI 1.45, 1.78), which showed significantly lower conception rates for women who had recently used HC. Figure 2 shows the survival curves for the two groups. The figure also illustrates that after five cycles there was no longer a significant difference between the total pregnancy probabilities of the two groups. The rate of anovulatory cycles was 3.5%, with no significant difference between the two groups.
Figure 2.
(A) Kaplan-Meier pregnancy probabilities for previous use of HC (red line) and NC prevent (blue dashed line). In this figure linear interpolation is performed between the cycle estimates. A dotted line indicating 30% cumulative pregnancy probability is added for reference.
The KMR when using the women on HC as the control group was 1.62 (95% CI 1.45, 1.78), which showed significantly lower conception rates for women who had recently used HC. (p<0.05)
(B) The time to reach 30% pregnancy probability for different age groups. For all of the three younger age categories, in women with previous use of Natural Cycles to prevent pregnancy the time to reach the 30% pregnancy probability was significantly shorter compared with the HC group. (p<0.05)
We further stratified the participants according to their age at the start of the measurements: 20–24, 25–29, 30–34 and 35–39 years. The KMR was calculated separately for these four age categories. The results are presented in Figure 2. For all of the three younger age categories, in women with previous use of Natural Cycles to prevent pregnancy the time to reach the 30% pregnancy probability was significantly shorter compared with the HC group.
Discussion
Findings and interpretation
We analysed 1656 women who used the Natural Cycles app to become pregnant and found an average TTP of 3.02 cycles, with a 95% CI between 2.90 and 3.14 cycles. The total 1 year pregnancy rate was 78.6%, which is lower than the pregnancy rate (79–94%) reported by similar studies [4,27,46]. We believe this may be attributable in part to fertile early dropouts, including women leaving the study after conceiving without reporting the pregnancy. Furthermore our life-table analysis, including all 2934 women in the study, showed that previous use of HC yielded lower early conception rates when compared with previous use of Natural Cycles prevent pregnancy.
On average, women who had used HC required more TTP compared with women who had previously used Natural Cycles to prevent pregnancy, but after cycle 4 the per-cycle pregnancy probability for the HC group became higher. As we found the ovulation rates of the two groups to be comparable, this finding did not appear to be due to inhibition of ovulation in the HC group. As mentioned in the introduction, previous studies [3,23–28] have shown that HC affects conception rates in the first cycles after stopping, but has no effect on 1 year pregnancy rates [28,29]. Our results confirm both these findings. It should be noted that the conclusions of the study regarding HC are valid only for the comparison with women who had previously used Natural Cycles to prevent pregnancy. The lack of knowledge in this study regarding concomitant medication is, however, a possible bias when assessing the effect of HC. For some women, previous use of HC might have masked underlying conditions that affect fecundity.
Our study also showed that knowledge and experience of an FAB method as a contraceptive may help women conceive faster. The results indicate that women timing intercourse to their known fertile window increased their conception rates, which is consistent with previous findings [34–36].
Typical use contraceptive efficacy with combined oral contraceptives reported in recent reviews [47, 48] is comparable to that with use of the Natural Cycles app, as well as for other comparable modern FAB methods [43,49–51]. Thus, the results presented in this paper provide useful information for women who are seeking a contraceptive method, yet plan to become pregnant in the near future.
Strengths and weaknesses of the study
This prospective observational study comprised a large set of real-life data. Analysing data that users enter directly into the app on a daily basis allows an insight into their fertility without affecting their everyday behaviour.
The number of women studied and the amount of data logged made this study larger than many similar previous studies, producing more precise estimates. However, the low threshold for entering and leaving the study led to a higher dropout rate and lower logging frequency and thus introduced a higher risk of bias compared with comparable prospective studies [1–7]. Right censoring due to dropouts may lower the reported cumulative possibility of pregnancy, but as long as dropouts do not correlate with any specific covariate, the comparisons of different sub-cohorts should not be affected.
While the result in this study is relevant in its own right, additional research is needed to establish the magnitude of the effect of using FAB methods for contraception on subsequent conception rates when compared with women who recently used other non-hormonal forms of contraception.
Finally, we note that the study population only comprised women who had decided to use an app for fertility monitoring, which may lead to a selection bias compared with the average population.
Conclusion
We have shown that the previous use of contraception has a significant impact on short-term conception rates, and that women who had previously used HC had a significantly lower probability of conceiving early compared with women who had previously used the Natural Cycles app to prevent pregnancy. Long-term conception rates were not, however, affected.
The result should not be seen as unique to this specific app and is likely widely applicable to women who use FAB methods prior to planning a pregnancy. It highlights the benefits to women of knowing their ovulation day when planning a pregnancy. The results presented in this study may be of interest to women who plan to become pregnant in the near future as well as to health care professionals counselling women on contraception and fertility.
Acknowledgements
We sincerely thank all the women who participated in the study. Furthermore, we would like to thank J. Sellberg for help with the methodology and O. Scheibelreiter for proofreading the manuscript.
Funding
The study was funded by NaturalCycles Nordic AB. Partial support was provided by an infrastructure grant for population research from the Eunice Kennedy Shriver National Institute of Health P2C HD047879 (JT).
Footnotes
Disclosure statement
EBS and RS are the scientists behind the Natural Cycles app and the founders of the company with stock ownership. OL and SPR is employed by NaturalCycles Nordic AB. KGD and HKK serve on the medical advisory board of NaturalCycles and have received honoraria for participating in advisory boards and/or giving presentations on matters related to contraception and fertility regulation for MSD/Merck, Bayer AG, Gedeon Richter, Exeltis, Actavis, Ferring (KGD), Exelgyn (KGD), HRA-Pharma (KGD) and Mithra (KGD). JH is on the medical advisory board of NaturalCycles, serves on the international advisory board of Finox, and has received honoraria for giving presentations related to infertility treatments in meetings arranged by MSD, Merck and Ferring. JT declares explicitly that there are no conflicts of interest in connection with this article.
References
- 1.Wise LA, Mikkelsen EM, Rothman KJ, et al. A prospective cohort study of menstrual characteristics and time to pregnancy. Am J Epidemiol 2011;174:701–709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wang X, Chen C, Wang L, et al. Conception, early pregnancy loss, and time to clinical pregnancy: a population-based prospective study. Fertil Steril 2003;79:577–584. [DOI] [PubMed] [Google Scholar]
- 3.Mikkelsen EM, Riis AH, Wise LA, et al. Pre-gravid oral contraceptive use and time to pregnancy: a Danish prospective cohort study. Hum Reprod 2013;28:1398–1405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gnoth C, Godehardt D, Godehardt E, et al. Time to pregnancy: results of the German prospective study and impact on the management of infertility. Hum Reprod 2003;18:1959–1966. [DOI] [PubMed] [Google Scholar]
- 5.Wise LA, Rothman KJ, Mikkelsen EM, et al. An internet-based prospective study of body size and time-to-pregnancy. Hum. Reprod 2010;25:253–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sapra KJ, McLain AC, Maisog JM, et al. Clustering of retrospectively reported and prospectively observed time-to-pregnancy. Ann Epidemiol 2015;25:959–963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wesselink AK, Wise LA, Hatch EE, et al. Menstrual cycle characteristics and fecundability in a North American preconception cohort. Ann Epidemiol 2016;26:482–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joffe M, Key J, Best N, et al. Studying time to pregnancy by use of a retrospective design. Am J Epidemiol 2005;162:115–124. [DOI] [PubMed] [Google Scholar]
- 9.Radin RG, Rothman KJ, Hatch EE, et al. Maternal recall error in retrospectively-reported time-to-pregnancy: an assessment and bias analysis. Paediatr Perinat Epidemiol 2015;29:576–588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bonde JP, Joffe M, Sallmén M, et al. Validity issues relating to time-to-pregnancy studies of fertility. Epidemiology 2006;17:347–349. [DOI] [PubMed] [Google Scholar]
- 11.Sozou PD, Hartsthorne GM. Time to pregnancy: a computational method for using the duration of non-conception for predicting conception. PloS One 2012;7:e46544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henry L Some data on natural fertility. Eugen Q 1961;8:81–91. [DOI] [PubMed] [Google Scholar]
- 13.Trussell J, Wilson C. Sterility in a population with natural fertility. Popul Stud 1985;39:269–286. [Google Scholar]
- 14.Dunson D, Colombo B, Baird DD. Changes with age in the level and duration of fertility in the menstrual cycle. Hum Reprod 2001;17:1399–1403. [DOI] [PubMed] [Google Scholar]
- 15.Grodstein F, Goldman MB, Cramer DW. Body mass index and ovulatory infertility. Epidemiology 1994;5:247–250. [DOI] [PubMed] [Google Scholar]
- 16.Rich-Edwards JW, Spiegelman D, Garland M, et al. Physical activity, body mass index and ovulatory disorder infertility. Epidemiology 2002;13:184–190. [DOI] [PubMed] [Google Scholar]
- 17.Wise LA, Palmer JR, Rosenberg L. Body size and time-to-pregnancy in black women. Hum Reprod 2013;28:2856–2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gesink Law DC, Maclehose RF, Longnecker MP. Obesity and time to pregnancy. Hum Reprod 2007;22:414–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Jensen TK, Scheike T, Keiding N, et al. Fecundability in relation to body mass and menstrual cycle patterns. Epidemiology 1999;10:422–428. [DOI] [PubMed] [Google Scholar]
- 20.Brodin T, Bergh T, Berglund L, et al. Menstrual cycle length is an age-independent marker of female fertility: results from 6271 treatment cycles of in vitro fertilization. Fertil Steril 2008;90:1656–1661. [DOI] [PubMed] [Google Scholar]
- 21.Curtis KM, Savitz DA, Arbuckle TE. Effects of cigarette smoking, caffeine consumption, and alcohol intake on fecundability. Am J Epidemiol 1997;146:32–41. [DOI] [PubMed] [Google Scholar]
- 22.Mikkelsen EM, Riis AH, Wise LA, et al. Alcohol consumption and fecundability: prospective Danish cohort study. BMJ 2016;354:i4262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Axmon A, Rylander L, Albin M, Hagmar L. Factors affecting time to pregnancy. Hum Reprod 2006;21:1279–1284. [DOI] [PubMed] [Google Scholar]
- 24.Hassan MA, Killick SR. Negative lifestyle is associated with a significant reduction in fecundity. Fertil Steril 2004;81:384–392. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan B, Nahum R, Yairi Y, et al. Use of various contraceptive methods and time of conception in a community-based population. Eur J Obstet Gynecol Reprod Biol 2005;123:72–76. [DOI] [PubMed] [Google Scholar]
- 26.Linn S, Schoenbaum SC, Monson RR, et al. Delay in conception for former ‘pill’ users. JAMA 1982;247:629–632. [PubMed] [Google Scholar]
- 27.Vessey MP, Wright NH, McPherson K, Wiggins P. Fertility after stopping different methods of contraception. Br Med J 1978;1:265–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Barnhart KT, Schreiber CA. Return to fertility following discontinuation of oral contraceptives. Fertil Steril 2009;91:659–663. [DOI] [PubMed] [Google Scholar]
- 29.Mansour D, Gemzell Danielsson K, Inki P, Jensen JT. Fertility after discontinuation of contraception: a comprehensive review of the literature. Contraception 2011;84:465–477. [DOI] [PubMed] [Google Scholar]
- 30.Lundin C, Gemzell Danielsson K, Bixo M, et al. Combined oral contraceptive use is associated with both improvement and worsening of mood in the different phases of the treatment cycle – a double-blind, placebo-controlled randomized trial. Psychoneuroendocrinology 2016;76:135–143. [DOI] [PubMed] [Google Scholar]
- 31.Zethraeus N, Dreber A, Ranehill E, et al. Combined oral contraceptives and sexual function in women – a double-blind, randomized, placebo controlled trial. J Clin Endocrinol Metab 2016; 101:4046–4053. [DOI] [PubMed] [Google Scholar]
- 32.Zethraeus N, Dreber A, Ranehill E, et al. A first-choice combined oral contraceptive influences general well-being in healthy women: a double-blind, randomized placebo-controlled trial. Fertil Steril 2017;107:1238–1245. [DOI] [PubMed] [Google Scholar]
- 33.Skovlund CW, Mørch LS, Kessing LV, Lidegaard Ø. Association of hormonal contraception with depression. JAMA Psychiatry 2016;73:1154–1162. [DOI] [PubMed] [Google Scholar]
- 34.Thijssen A, Meier A, Panis K, Ombelet W. ‘Fertility awareness-based methods’ and subfertility: a systematic review. Facts Views Vis Obgyn 2014;6:113–123. [PMC free article] [PubMed] [Google Scholar]
- 35.Scarpa B, Dunson D, Giacchi E. Bayesian selection of optimal rules for timing intercourse to conceive by using calendar and mucus. Fertil Steril 2007;88:915–924. [DOI] [PubMed] [Google Scholar]
- 36.Mu Q, Fehring R. Efficacy of achieving pregnancy with fertility-focused intercourse. MCN Am J Matern Child Nurs 2014;39:35–40. [DOI] [PubMed] [Google Scholar]
- 37.Wilcox AJ, Weinberg CR, Baird DD. Timing of sexual intercourse in relation to ovulation – effects on the probability of conception, survival of the pregnancy, and sex of the baby. N Engl J Med 1995;333:1517–1521. [DOI] [PubMed] [Google Scholar]
- 38.Frank-Herrmann P, Jacobs C, Jenetzky E, et al. Natural conception rates in subfertile couples following fertility awareness training. Arch Gynecol Obstet 2017;295:1015–1024. [DOI] [PubMed] [Google Scholar]
- 39.Berglund Scherwitzl E, Lindén Hirschberg A, Scherwitzl R. Identification and prediction of the fertile window using NaturalCycles. Eur J Contracept Reprod Health Care 2015;20:403–408. [DOI] [PubMed] [Google Scholar]
- 40.Dunson D, Baird DD, Wilcox AJ, Weinberg CR. Day-specific probabilities of clinical pregnancy based on two studies with imperfect measures of ovulation. Hum Reprod 1999;14:1835–1839. [DOI] [PubMed] [Google Scholar]
- 41.Wilcox AJ, Dunson D, Baird DD. The timing of the ‘fertile window’ in the menstrual cycle: day specific estimates from a prospective study. BMJ 2000;321:1259–1262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Behre HM, Kuhlage J, Gassner C, et al. Prediction of ovulation by urinary hormone measurements with the home use ClearPlan Fertility Monitor: comparison with transvaginal ultrasound scans and serum hormone measurements. Hum Reprod 2000;15:2478–2482. [DOI] [PubMed] [Google Scholar]
- 43.Berglund Scherwitzl E, Gemzell Danielsson K, Sellberg JA, Scherwitzl R. Fertility awareness-based mobile application for contraception. Eur J Contracept Reprod Health Care 2016;21:234–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1958;53:457–481. [Google Scholar]
- 45.Cox DR. Regression models and life-tables. J Roy Stat Soc Ser B Method 1972;34:187–220. [Google Scholar]
- 46.Sivin I, Stern J. Long-acting, more effective copper T IUDs: a summary of U.S. experience, 1970–75. Stud Fam Plann 1979;10:263–281. [PubMed] [Google Scholar]
- 47.Kost K, Singh S, Vaughan B, et al. Estimates of contraceptive failure from the 2002 National Survey of Family Growth. Contraception 2008;77:10–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Trussell J Contraceptive failure in the United States. Contraception 2011;83:397–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Arévalo M, Jennings V, Nikula M, Sinai I. Efficacy of the new TwoDay Method of family planning. Hum Reprod 2004;82:885–892. [DOI] [PubMed] [Google Scholar]
- 50.Arévalo M, Jennings V, Sinai I. Efficacy of a new method of family planning: the Standard Days Method. Contraception 2001;65:333–338. [DOI] [PubMed] [Google Scholar]
- 51.Frank-Herrmann P, Heil J, Gnoth C, et al. The effectiveness of a fertility awareness based method to avoid pregnancy in relation to a couple’s sexual behaviour during the fertile time: a prospective longitudinal study. Hum Reprod 2007;22:1310–1319. [DOI] [PubMed] [Google Scholar]