Abstract
Background and objective
Stress is an environmental cue, which may lead to increased alcohol craving, and vulnerability to relapse. Heart rate variability (HRV) biofeedback, a supplement standard for inpatient rehabilitation, has been applied for treatment and has been shown to effectively reduce craving and anxiety, increase HRV, and improve vasomotor function, among patients who have alcohol dependence problems. Therefore, the purpose of this study was to investigate the impact of HRV biofeedback and the Phramongkutklao model (PMK model) as an intensive inpatient rehabilitation program concerning stress and craving reduction of inpatients with alcohol use disorder. The findings could benefit treatment design to increase the effectiveness regarding stress and craving reduction among patients with alcohol use disorder and may also reduce rehabilitation costs.
Methods
We conducted this study as a randomized controlled intervention trial, which was also performed single blinded. In all, 35 patients with alcohol use disorder were recruited and randomly assigned in two groups. Patients in the intervention group (n=17) were treated under the PMK model and underwent 16 sessions of the HRV biofeedback program, which included 30 minute long sessions, 4 days per week, for 4 weeks continuously. Patients in the control group (n=18) received PMK model treatment only. Participants were asked to complete a Stress Test (ST-5) and the Penn Alcohol-Craving Scale at baseline, after completing treatment, and at one month afterward (follow-up).
Results
The study showed decreased stress and craving in the intervention group immediately after treatment and at one-month follow-up, whereas the control group had reduced stress and craving only immediately after treatment. Furthermore, we found a significant effect concerning stress and craving between baseline and at one-month follow-up that showed the intervention group exhibited higher difference of scores than the control group.
Conclusion
The study results showed that applying HRV biofeedback may be considered beneficial for standard rehabilitation inpatients to reduce stress and craving for patients with alcohol use disorder.
Keywords: HRV biofeedback, PMK model, alcohol use disorder, stress, craving
Background
According to WHO’s most current alcohol consumption report, Thailand has the highest alcohol consumption in Southeast Asia and is above the worldwide average in 2015 of 6.3 L of pure alcohol per person aged 15 or older.1 A large amount of alcohol for a long time effect every part of the body, deteriorates vasomotor and cardiac autonomic nerve fiber, causing an imbalance in the autonomic nervous system (ANS). This, in turn, leads to neurovascular and cardiac dysfunction and reducing heart rate variability (HRV) that is indicative of an imbalance between the sympathetic and the parasympathetic nervous system. This cardiac autonomic imbalance is linked to increased alcohol craving.2,3 In addition, consuming large amounts of alcohol not only affects the prefrontal cortex concerning executive function skills making it more difficult to resist the urge to drink4,5 and creating hypersensitivity to environmental cues such as stress, which may in turn lead to increased alcohol craving and vulnerability to relapse6 Thus, governments and other public health organizations focus in particular on the impacts of alcohol consumption, and many kinds of treatment can be considered.
HRV biofeedback has been applied to treat many diseases and was shown to effectively reduce various symptoms. A recent investigation of HRV biofeedback with patients with alcohol use disorder showed a trend toward higher rates of one year abstinence although without significance.7 Interestingly, effectively reducing craving, anxiety, increasing HRV, and improving vasomotor function in patients was possible for those exhibiting alcohol dependence problems being a supplement standard for inpatient rehabilitation.2 HRV biofeedback was designed as a window to HRV that involves a direct link to the ANS. This as well provides a reliable measure of ANS dynamics that are especially sensitive to fluctuations in the psychophysiological state by paced breathing at resonance frequency approximately six breaths per minute. This also comprises an instrument that connects emotional regulation and information about a physiological function with feedback learning by visualizing on a screen, so that patients understand their training progress.8 Moreover, the positive result encourages them leading to better direction results9 as an adjunct to manage stress especially among patients with alcohol use disorder and potentially leading to reduced alcohol craving2 Therefore, this research aimed to compare stress and alcohol craving among patients with alcohol use disorder by adding HRV biofeedback practice along with the Phramongkutklao model (PMK model) developed by Saengcharnchai, an intensive inpatient rehabilitation program. The key approaches for modifying a patient’s behavior comprise Motivational Style and Spirituality Rehabilitation & Buddhism the 12 Steps.10 Findings could benefit treatment designs to increasing effectiveness in reducing stress and craving among patients with alcohol use disorder and may reduce costs for rehabilitation.
Methods
Study design
The study was conducted as a randomized controlled intervention trial, performed single blinded where the investigator was blinded to the group allocated to collect data. Data were collected by the research assistant who was a clinical psychologist and analyzed by the researcher. Because the PMK model was employed in an open inpatient rehabilitation setting, the researcher used simple randomization for both groups by computer-generated random number tables.
Materials and procedures
Participants
In all, 35 patients between 20 and 59 years of age were randomly assigned to two groups, 17 patients in the intervention and 18 patients in the control group involving those under the PMK model program at Phramongkutklao Hospital over six months. Participants were eligible to participate in the study if they were 20 years or older, diagnosed as patients with alcohol use disorder determined by the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition criteria (DSM-V) for alcohol dependence. A psychiatrist used the Structured Clinical Interview, while subjects completed alcohol detoxification around 14 days, and completed benzodiazepine washout period at least 7 days before. To avoid confounding by comorbidities, this study excluded participants with serious current physical, mental health problems or cognitive impairments.
General demographic questionnaire
At baseline, participants completed the general demographic questionnaire including age, sex, marital status, education, religious affiliation, occupation, income, chronic illness history, chronic illness, alcohol consumption period, and stressor.
Stress test (ST-5)
Participants completed a questionnaire developed by the Department of Mental Health, Ministry of Public Health of Thailand11 comprising five items: sleep problem, decreased concentration, irritability, boredom, and social isolation. Participants were required to rate their experience of symptoms over the past two to four weeks on a 4-point Likert scale (0–3). The proposed cut off scores in three groups comprised no stress (0–4), might have stress (5–7), and have a problem (≥8). The ST-5 had acceptable concurrent validity. While the scale demonstrated good internal consistency (α=0.80).12
The Penn alcohol-Craving Scale (PACS)
Participants completed a questionnaire developed by Flannery, Volpicelli & Pettinati in 1999.13 It comprised a five-item self-administered, single-factor scale tool that could be conducted easily and quickly. The first three questions revolved around frequency, intensity, and duration of thoughts about drinking within the past week. The questions used indicators embedded with rating numbers from 0 to 6. The Thai-version was translated by Chenchujit in 2010 and tested for content validity by three Thai/English-speaking psychiatrists and was back-translated to English to determine correctness of the content.14 The scale of PACS showed high internal consistency (α=0.92), meaning it could indicate good predictive validity.15,16
Standard rehabilitation care
All participants received the PMK Model at Phramongkutklao Hospital for 28 days, comprising group therapy for 4 hrs daily, 5 days weekly. Cognitive behavior learning and group processes were the main strategies.
HRV biofeedback
Participants in the intervention group received treatment as usual and 16 sessions of the HRV biofeedback program where each session lasted between 30 mins, 4 days weekly, for four weeks continuously.
Procedure
Participants were asked to complete the ST-5 and PACS at three time points, before beginning the first HRV biofeedback session (baseline), after completing the last HRV biofeedback session, and one month after the last HRV biofeedback session (follow-up).
At the beginning of the study, participants in the intervention group were introduced to the settings, device and basic procedures of biofeedback, developed by Helicor, Inc and explained the method of using the StressEraser as; describe below. First, subjects inserted their left index finger in the pulse rate sensor clip on the top of the device. Then, they inhaled slowly while viewing the waves on the screen and exhaled slowly while counting slowly from one to five and watching for a triangle to appear above the wave. Finally, they inhaled again as the next wave began to rise (Figure 1).
Figure 1.
Participants were asked to slowdown their breathing rhythm to a particular rate by inhaling until the wave reached the highest mark on the device and exhale slowly while counting from 1 to 5 and watching for a triangle to appear above the wave, and start to inhale again as the next wave began to rise.
Ethics considerations
The study was approved by the Institutional Review Board at Mahidol University (IRB number: MU-CIRB 2017/099.3105) and Phramongkutklao Hospital (IRB number: Q013h/60) was conducted in accordance with the Declaration of Helsinki, and written informed consent was obtained from all participants.
Statistics
Statistical analyses were performed using SPSS Software, Version 21 (IBM). All data were represented as frequency, percentage, means, and standard deviation (SD). Chi-square or Fisher’s exact test analyses were conducted to investigate similarity among patient characteristics in the two groups. The Paired t-test was used to analyze the differences at baseline, post-intervention and follow-up session in the same group. The independent t-test was employed to analyze the differences between the two groups. Differences in the two groups were considered statistically significant at p-value ≤0.05.
Results
The average age in the intervention group was 41.1 years and 44.5 years in the control group. Most were male, 88.2% and 94.4% in the intervention and the control groups, respectively, and they were mostly married, 47.1 in the intervention and 55.6 in the control groups. Both intervention and control groups mostly had obtained lower than bachelor’s degree educational level at 76.5% and 72.2%, respectively. Most were Buddhist, 94.1 in the intervention and 94.4% in the control groups. The majority in both groups worked as government officers, accounting for 70.6 in the intervention and 60% in the control groups. In addition, the average monthly income of the intervention group was lower than 15,000 THB at 29.4%, whereas in the control group lower than 15,000 THB and between 20,001 and 30,000 THB totaled 27.8%. The health data indicated most in the intervention group, 58.8%, had no any chronic illness while the control group had the same number of people with and without chronic illness. Among those who had chronic illness in the intervention group, most had diabetes and liver disease, 23.5%, whereas those in the control group had liver disease at 27.8%. Between the intervention and control groups, no differences in baseline characteristics were found including age, sex, religious affiliation, marital status, education, occupation, income, and chronic illness history as shown in Table 1.
Table 1.
Demographic characteristics (n=35)
| Variables/characteristics | Intervention group | Control group | p-Value | ||
|---|---|---|---|---|---|
| Age (Mean ± SD) | 41.1±7.3 | 44.5±10 | 1.00 | ||
| Frequency | Percentage | Frequency | Percentage | ||
| Sex | |||||
| Male | 15 | 88.2 | 17 | 94.4 | 0.60 |
| Female | 2 | 11.8 | 1 | 5.6 | |
| Marital status | |||||
| Single | 5 | 29.4 | 4 | 22.2 | 0.95 |
| Married | 8 | 47.1 | 10 | 55.6 | |
| Divorced/Widowed | 4 | 23.5 | 4 | 22.2 | |
| Education | |||||
| Below Bachelor Degree | 13 | 76.5 | 13 | 72.2 | 0.74 |
| Bachelor Degree | 3 | 17.6 | 2 | 11.1 | |
| Upper Bachelor Degree | 1 | 5.9 | 3 | 16.7 | |
| Religious affiliation | |||||
| Buddhist | 16 | 94.1 | 17 | 94.4 | 1.00 |
| Christianity | 1 | 6.3 | 1 | 5.6 | |
| Occupation | |||||
| Employee | 4 | 23.5 | 6 | 33.3 | 0.43 |
| Business | 1 | 5.9 | 3 | 16.7 | |
| Government officer | 12 | 70.6 | 9 | 50 | |
| Income | |||||
| <15,000 baht | 5 | 29.4 | 5 | 27.8 | 1.00 |
| 15,000–20,000 baht | 4 | 23.5 | 4 | 22.2 | |
| 20,001–30,000 baht | 4 | 23.5 | 5 | 27.8 | |
| >30,000 baht | 4 | 23.5 | 4 | 22.2 | |
| Chronic illness history | |||||
| No | 10 | 58.8 | 9 | 50 | 0.60 |
| Yes | 7 | 41.2 | 9 | 50 | |
| Chronic illness | |||||
| Diabetes | 4 | 23.5 | 1 | 5.6 | 1.00 |
| Hypertension | 3 | 17.6 | 4 | 22.2 | 1.00 |
| Liver disease | 4 | 23.5 | 5 | 27.8 | 1.00 |
| Gastritis | 1 | 5.9 | 1 | 5.6 | 1.00 |
| Hypercholesterolemia | 1 | 5.9 | 1 | 5.6 | 1.00 |
As for alcohol consumption data, the alcohol consumption period of both groups was 20– 30 years, accounting for 58.8% and 61.1%, respectively. Interesting, stress was the most common reason stated for drinking in both groups at 94.1% and 77.8%; followed by festivals and parties at 70.6% and 72.2%. The stressors of the intervention group were mostly expenses, debts, and responsibilities and burdens toward work at 35.5%, whereas stressors in the control group were responsibilities and burdens toward work, 38.9% as shown in Table 2.
Table 2.
Alcohol-related consumption (n=35)
| Variables Alcohol-related Consumption |
Intervention group | Control group | p-Value | ||
|---|---|---|---|---|---|
| Frequency | Percentage | Frequency | Percentage | ||
| Alcohol consumption period | 10 | 58.8 | 11 | 61.1 | 1.00 |
| 20–30 years | |||||
| Higher than 30 years | 2 | 11.8 | 3 | 16.7 | |
| The reason for drinking | |||||
| Festivals and parties | 12 | 70.6 | 13 | 72.2 | 0.92 |
| Invitation from peers | 8 | 47.1 | 10 | 55.6 | 0.62 |
| Advertisement | 1 | 5.9 | 2 | 11.1 | 1.00 |
| Nearby shop | 5 | 29.4 | 7 | 38.9 | 0.56 |
| Stress | 16 | 94.1 | 14 | 77.8 | 0.34 |
| Want to try | 2 | 11.8 | 3 | 16.7 | 1.00 |
| Stressor | |||||
| Relationship with family members | 4 | 23.5 | 4 | 22.2 | 1.00 |
| Family’s expectant | 3 | 17.6 | 3 | 16.7 | 1.00 |
| Family responsibilities and burdens | 3 | 17.6 | 3 | 16.7 | 1.00 |
| Relationship with colleagues | 4 | 23.5 | 5 | 27.8 | 1.00 |
| Work responsibilities and burdens | 6 | 35.3 | 7 | 38.9 | 0.83 |
| Career advancement | 2 | 11.8 | 2 | 11.1 | 1.00 |
| Lack of acceptance from superiors and colleagues | 3 | 17.6 | 1 | 5.6 | 0.34 |
| Expenses and debts | 6 | 35.5 | 6 | 33.3 | 0.90 |
Stress scores
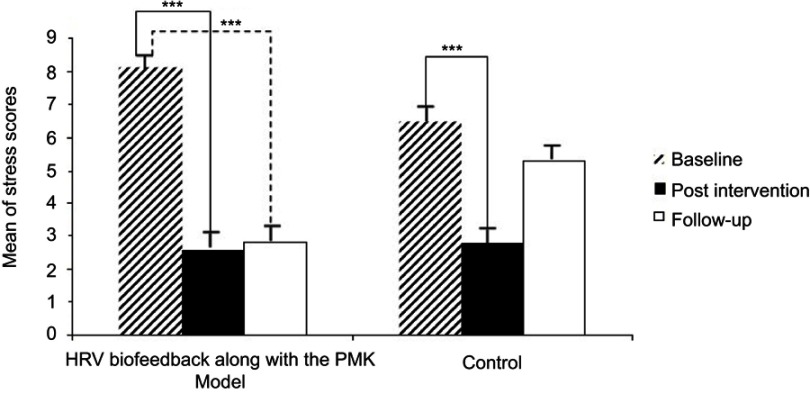
The intervention group reported lower stress scores after using HRV biofeedback along with the PMK model (t=5.487, p=0.000***) and at one-month follow-up (t=5.642, p=0.000***). The control group also reported lower stress scores after receiving only the PMK model (t=5.642, p=0.000***) but this reduction did not occur at one-month follow-up (t=1.555, p=0.138). At one-month follow-up, the stress was higher in both groups when compared with after the intervention, but the HRV biofeedback along with the PMK model group tended toward less stress than the control group receiving only the PMK model (Figure 2).
Figure 2.
The bar graph shows the results of stress scores in the same group between the control and intervention group at baseline (striped bars), post-intervention (black bars) and follow-up (white bars).
Note: ***P<0.001.
Abbreviations: HRV, heart rate variability; PMK model, Phramongkutklao model.
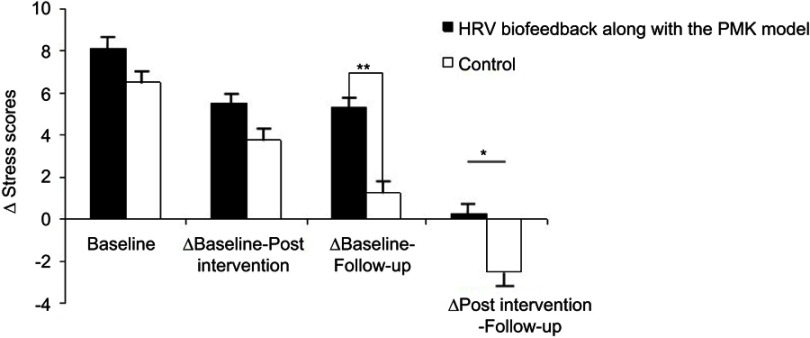
Furthermore, no significant difference was found in the groups between baseline and post-intervention (t=−1.321, p=0.196). However, between baseline and one-month follow-up the intervention group revealed significantly higher difference of scores than those in the control group (t= −3.341, p=0.002**) (Figure 3).
Figure 3.
The bar graph shows the difference of stress scores among two group samples who received HRV biofeedback along with the PMK model (black bars) and the group who received only the PMK model (white bars) that were separately displayed at baseline, ∆Baseline-Post-intervention, ∆Baseline-Follow-up and ∆Post-intervention-Follow-up. e
Notes: **P>0.01; *P<0.05. ∆Stress scores, differences of stress scores; ∆Baseline-Post-intervention, differences of stress scores between baseline and post-intervention; ∆Baseline-Follow-up, differences of stress scores between baseline and follow-up; ∆Post-intervention-Follow-up; differences of stress scores between post-intervention and follow-up.
Abbreviations: HRV, heart rate variability; PMK model, Phramongkutklaomodel.
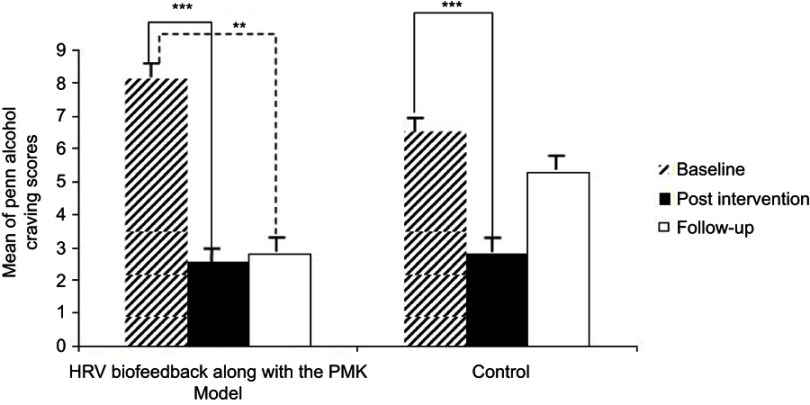
Penn alcohol-craving scores
As expected, the intervention group had a significant decrease in craving after using HRV biofeedback along with the PMK model (t=5.768, p=0.000***) and at one-month follow-up (t=4.014, p=0.001**). The control group also exhibited decreased craving after receiving only the PMK model (t=4.950, p=0.000***) but without significant changes in craving at one-month follow-up (t=0.524, p=0.607). However, both groups tended toward higher craving at one-month follow-up compared with post-intervention, but no significant increase was observed in the intervention group (Figure 4).
Figure 4.
The bar graph shows the result of craving scores in the same group between the control and intervention group at baseline (striped bars), post-intervention (black bars) and follow-up (white bars).
Notes: ***P>0.001; **P>0.01.
Abbreviations: HRV, heart rate variability; PMK model, Phramongkutklao model.
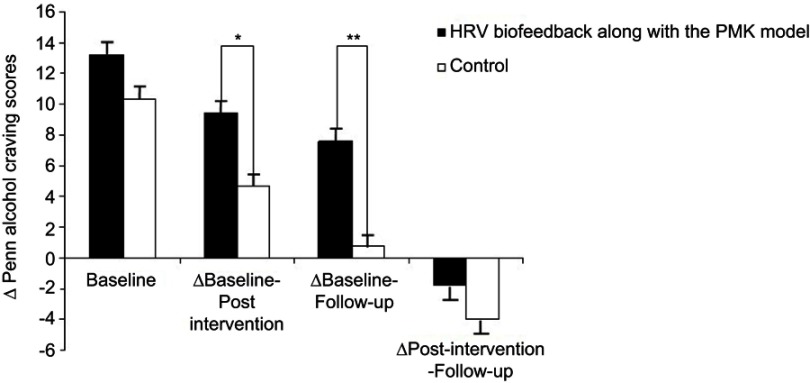
In addition, the intervention group reported higher difference of scores than those of the control group at baseline and post-intervention (t=−2.554, p=0.015*) and at baseline and one-month follow-up (t=−2.959, p=0.006**) (Figure 5).
Figure 5.
The bar graph showed the difference of craving scores among two group samples who received HRV biofeedback along with the PMK model (black bars) and the group who received only the PMK model (white bars) that were separately displayed at baseline, ∆Baseline-Post-intervention, ∆Baseline-Follow-up, and ∆Post-intervention- Follow-up.
Notes: **P>0.01; *P<0.05. ∆Penn alcohol-craving scores, differences of Penn alcohol-craving scores; ∆Baseline-Post-intervention, differences of Penn alcohol-craving scores between baseline and post-intervention; ∆Baseline-Follow-up, differences of the Penn alcohol-craving scores between baseline and follow-up; ∆Post-intervention-Follow-up; differences of the Penn alcohol-craving scores between post-intervention and follow-up.
Abbreviations: HRV, heart rate variability; PMK model, Phramongkutklao model.
Discussion
According to the results, a significant decrease in stress and craving scores was observed between before and after the intervention in both groups. The findings here supported other studies that found HRV biofeedback training had better effectiveness in reducing stress17,18 and craving.2,19 It could be explained from the related study showing that the PMK model could a significantly reduce or stop drinking among patients with alcohol use disorder to improve their quality of life such as their physical and mental health.20 The PMK model also involved the inpatient rehabilitation program to limit stimuli and external factors.21 Consequently, these might have affected the stress and craving scores after the intervention in both groups declined greatly. The intervention group also reported lower stress and craving scores at one-month follow-up compared with baseline whereas no significant was observed in the control group. Notably, differences in stress and craving scores in the intervention group at baseline and post-intervention were higher than those in the control group. This might be because the participants in the intervention group had practiced HRV biofeedback by breathing slowly, deeply, and regularly, to increase more efficiently; slowdown their breathing rhythm, leading to slower heart rate and breathing. It also increased their baroreflex sensitivity and the heartbeat fluctuation rate. Then, the parasympathetic nervous system responded to the body producing greater efficiency in rebalancing the ANS.21,22
Furthermore, HRV biofeedback is a stress management tool using deep breathing, visualization, and calming of their physiological arousal.23 This showed a graph on the monitor screen when the participants practiced breathing, and when they were relaxed, the graph showed wide and lengthy continuous waves. Because they could see the physiological data head in a better direction than before, it created feedback learning. This encouraged them to practice it more efficiently. Moreover, the participants repetitively used HRV biofeedback, so their body learned and became accustomed to it, so they could control their breathing by themselves without the need of biofeedback anymore. As a result, the participants in the intervention group had lower stress and craving at one-month follow-up. B.F. Skinner’s Operant Conditioning learning theory states that as long as the stimulus creates satisfaction, the reaction becomes positive; this is called positive reinforcement. This means when patients with alcohol use disorder practiced the breathing according to the graph on the monitor correctly and continuously, the biofeedback would show scores that positively reinforced the patients that they were breathing efficiently. When they repeatedly practiced until their body had learned and became used to it, they would be able to control their breathing without the need for the biofeedback anymore.9
Conclusion
The study found that HRV biofeedback along with the PMK model could significantly reduce stress and craving among patients with alcohol use disorder immediately after treatment and at one-month follow-up. However, no significant changes were found in the control group at one-month follow-up. Moreover, the intervention group also tended to exhibit less stress and craving than the control group. However, further studies should enroll a greater a number of participants and should be continuously followed up at three months and six months to measure the persistence of treatment. Furthermore, data in the follow-up phase should be collected while participants underwent inpatient rehabilitation to control other factors, which may have affected the results.
Acknowledgments
The researchers would like to express gratitude for the funding for graduate students from the Center for Alcoholic Studies, partial funding from the Graduate Studies of Mahidol University Alumni Association, partial publication funding from Phramongkutklao College of Medicine and also to personnel from the Department of Psychiatry and Neurology, Phramongkutklao Hospital, the participants, and all those involved in this study, who provided great collaboration and support.
Disclosure
Pichita Teeravisutkul reports grants from the Center for Alcoholic Studies, The Graduate Studies of Mahidol University Alumni Association and Phramongkutklao College of Medicine, outside the submitted work. The authors report no other conflicts of interest in this work.
References
- 1.World Health Organization. The Global Status Report on Alcohol and Health 2011 [Internet] Geneva: WHO; 2011. [cited September 28, 2016] Available from: http://www.who.int/substance_abuse/publications/global_alcohol_report/msbgsruprofiles.pdf. Accessed July15, 2019. [Google Scholar]
- 2.Penzlin AI, Siepmann T, Illigens BM, Weidner K, Siepmann M. Heart rate variability biofeedback in patients with alcohol dependence: a randomized controlled study. Neuropsychiatry Dis Treat. 2015;9(11):2619–2627. PMID: 26557753. doi: 10.2147/NDT.S84798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thayer JF, Friedman BH. Stop that! Inhibition, sensitization, and their neurovascular concomitants. Scand J Psychol. 2002;43(2):123–130. PMID: 12004949. [DOI] [PubMed] [Google Scholar]
- 4.Moselhy HF, Georgiou G, Kahn A. Frontal lobe changes in alcoholism: a review of the literature. Alcohol Alcohol. 2001;36:357–368. PMID: 11524299. doi: 10.1093/alcalc/36.5.357 [DOI] [PubMed] [Google Scholar]
- 5.Oscar-Berman M. Neuropsychological vulnerabilities in chronic alcoholism. In: Noronha A, Eckardt M, Warren K, editors Review of NIAAA’s Neuroscience and Behavioral Research Portfolio: NIAAA Research Mono-Graph No. 34. Bethesda (MD): U.S. Department of Health and Human Services, Public Health Service, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism; 2000:437–471. [Google Scholar]
- 6.Fox HC, Bergguist KL, Hong KL, Sinha R. Stress-induced and alcohol cue-induced craving in recently abstinent alcohol-dependent individuals. Alcohol Clin Exp Res. 2007;31(3):395–403. PMID: 17295723. doi: 10.1111/j.1530-0277.2006.00320.x [DOI] [PubMed] [Google Scholar]
- 7.Penzlin AI, Barlinn K, Illigens BM, Weidner K, Siepmann M, Siepmann T. Effect of short-term heart rate variability biofeedback on long-term abstinence in alcohol dependent patients – a one-year follow-up. BMC Psychiatry. 2017;17(1):325. doi: 10.1186/s12888-017-1489-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hassett AL, Radvanski DC, Vaschillo EG, et al. A pilot study of the efficacy of heart rate variability(HRV)biofeedback in patients with fibromyalgia. Appl Psychophysiol Biofeedback. 2007;32(1):1–10. PMID: 17219062. doi: 10.1007/s10484-006-9028-0 [DOI] [PubMed] [Google Scholar]
- 9.Frank DL, Khorshid L, Kiffer JF, Moravec CS, McKee MG. Biofeedback in medicine: who, when, why and how? Ment Health Fam Med. 2010;7(2):85–91. PMID: 22477926. [PMC free article] [PubMed] [Google Scholar]
- 10.Saengcharnchai P. Alcoholics Anonymous in Hospital Setting. Bangkok: Department of Psychiatry and Neurology Phramongkutlao Hospital; 2003. [Google Scholar]
- 11.Thailand Ministry of Public Health. [Department of Mental Health screening test for stress 5 (ST-5)]; 2009. [cited April 20, 2019]. Available from: http://www.dmh.go.th/test/qtest5/asheet.asp?qid=1. Accessed July 26, 2019. Thai.
- 12.Silpakit O. Srithanya Stress Scale. J Ment Health. 2008;26(3):177–185. [Google Scholar]
- 13.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Center for the study of addictions. Alcohol Clin Exp Res. 1999;23(8):1289–1295. PMID: 10470970. doi: 10.1111/j.1530-0277.1999.tb04349.x [DOI] [PubMed] [Google Scholar]
- 14.Maneesang W, Verachai V, Kalayasiri R. Effects of video cues on inhalants craving in individuals receiving inhalants substance- dependency treatment. Chula Med J. 2012;56(2):147–161. [Google Scholar]
- 15.Kim MJ, Kim SG, Kim HJ, et al. A study of the reliability and validity of the korean version of the penn alcohol craving scale for alcohol-dependent patients. Psychiatry Investig. 2008;5(3):175–178. doi: 10.4306/pi.2008.5.3.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Yoon G, Kim SW, Thuras P, Grant JE, Westermeyer J. Alcohol craving in outpatients with alcohol dependence: rate and clinical correlates. J Stud Alcohol. 2006;67(5):770–777. [DOI] [PubMed] [Google Scholar]
- 17.Ratanasiripong P, Park JF, Ratanasiripong N, Kathalae D. Stress and anxiety management in nursing students: biofeedback and mindfulness meditation. J Nurs Educ. 2015;54(9):520–524. PMID: 26334339. doi: 10.3928/01484834-20150814-07 [DOI] [PubMed] [Google Scholar]
- 18.Siepmann M, Hennig UD, Siepmann T, et al. The effects of HRV biofeedback in patients with preterm labour. Appl Psychophysiol Biofeedback. 2014;39(1):24–35. PMID: 24271650. doi: 10.1007/s10484-013-9238-1 [DOI] [PubMed] [Google Scholar]
- 19.Meule A, Freund R, Skirde AK, Vögele C, Kübler A. Heart rate variability biofeedback reduces food cravings in high food cravers. Appl Psychophysiol Biofeedback. 2012;37(4):241–251. PMID: 22688890. doi: 10.1007/s10484-012-9197-y [DOI] [PubMed] [Google Scholar]
- 20.Daengthoen L, Saengcharnchai P, Yingwiwattanapong J, Pernparn U. Effects of the PMK model on alcohol-dependent patient: a randomized controlled trial. J Subst Use. 2014;19(1–2):81–88. doi: 10.3109/14659891.2012.734543 [DOI] [Google Scholar]
- 21.Eddie D, Vaschillo E, Vaschillo B, Lehrer P. HRV biofeedback: theoretical basis, delivery, and its potential for the treatment of substance use disorders. Addict Res Theory. 2015;23(4):266–272. doi: 10.3109/16066359.2015.1011625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lehrer P, Vaschillo E, Vaschillo B, et al. Resonant frequency biofeedback training to increase cardiac variability: rationale and manual for training. Appl Psychophysiol Biofeedback. 2000;25(3):177–191. PMID: 10999236. [DOI] [PubMed] [Google Scholar]
- 23.Scott E. Biofeedback and Stress Relief. Stress Management [Internet] Verywell; 2017. [cited October 4, 2016] Available from: https://www.verywell.com/biofeedback-and-stress-relief-3144924. Accessed July15, 2019. [Google Scholar]