Abstract
Background:
The comorbidity of depressed mood and college student drinking causes consequences for both the individual and society. Aspects of parenting have been shown to be important for college students’ well-being. While some interventions are beginning to address this population, few studies have examined how parental monitoring impacts the relationship between depressed mood, alcohol use, and related consequences. The present study examined whether perceived parental monitoring moderated the relationship between depressed mood and alcohol use and related problems.
Methods:
Students (N = 796) completed a survey during the fall semester of their first two years of college at a large, public university assessing drinking and related negative consequences, maternal and paternal monitoring, and depressed mood.
Results:
Results revealed that maternal and paternal monitoring moderated the relationship between depressed mood and typical weekly drinking, and depressed mood and consequences (i.e., self-perception, self-care, blackouts).
Conclusions:
Interventions should be tailored to parents based on considerations of both student mental health and alcohol use.
Keywords: college students, parental monitoring, drinking, alcohol-related consequences, depressed mood
College student drinking and related consequences have been well-studied. Heavy episodic drinking is common, with 35% to 39% of students reporting 5+ drinks on an occasion in the past 2–4 weeks (Johnston, O’Malley, Bachman, & Schulenberg, 2013; Substance Abuse and Mental Health Services Administration [SAMHSA], 2013). Such drinking leads to numerous negative consequences, including regretted decisions, academic problems, unprotected sex, accidental injuries, and death (American College Health Association [ACHA], 2014; Hingson, Zha, & Weitzman, 2009).
In addition to alcohol use, college students experience depressed mood at alarming rates (Dawson, Grant, Stinson & Chou, 2005; Gallagher, 2009; Geisner, Larimer, & Neighbors, 2005; Geisner, Mallett, & Kilmer, 2012; Kitzrow, 2003). Academic, social, and other stressors lead students to experience high rates of sadness, hopelessness, and can lead to clinical depression, self-harm, and suicidality. In fact, of college students surveyed over past 12 months, 83.3% felt exhausted (not from physical activity), 37.5% felt very sad, 67.3% felt very lonely, 52.7% felt things were hopeless, 39.1% felt so depressed it was difficult to function (ACHA, 2014). Furthermore, there are high rates of comorbidity of depression and substance use on college campuses (SAMHSA, 2008). Students who are depressed are much more likely to have higher alcohol use and related consequences (Geisner et al., 2004; Ross, 2004; Weitzman, 2004) than those without. This increased risk has been conceptualized in part through the self-medication hypothesis (Khantzian, 1985; 2003). Further, the motivational model of alcohol use suggests individuals are motivated to use alcohol to help regulate affect (Cooper, Frone, Russell, & Mudar, 1995; Miles Cox & Klinger, 1988). Studies have shown support for this theory showing that people may drink both to increase positive affect and to decrease negative affect (Kuntsche et al., 2014; Gottfredson & Hussong, 2013). Drinking to regulate affect may particularly salient for individuals with more depressive symptoms. Additionally, the physiological effects of alcohol, including lowered inhibitions, coupled with lack of healthy coping options that is common with depression, may place these students at higher risk for experiencing alcohol-related consequences. Likewise, those with alcohol use disorder are twice as likely to have a mental health disorder than those without (Dawson, Grant, Stinson, & Chou, 2005).
Several approaches have been shown to be effective in addressing drinking directly with students (NIAAA, 2002; 2015). Recently, several studies have also evaluated interventions targeting students with both alcohol or substance use and depression (Geisner, Neighbors, Lee, & Larimer, 2007; Geisner, Varvil-Weld, Mittmann, Mallett, & Turrisi, 2015; Kay-Lambkin, Baker, Lewin, & Carr, 2009). These studies indicate interventions targeting this comorbidity can lead to some reductions in alcohol use, related consequences, and depressed mood symptoms.
Parental monitoring shown to relate to lower drinking and consequences
In addition to individual interventions directly targeting students with depressed mood and high-risk drinking, parenting interventions have been shown to be effective in reducing drinking and related problems by college students (Ichiyama et al., 2009; Turrisi et al. 2009). While parenting evolves from adolescence to emerging adulthood, with young adults taking on more autonomy, research from the past 15 years has indicated parents have a continued and lasting effect on student behavior even as these parenting roles change (Kaynak et al., 2013; Turner, Chandler, & Heffer, 2009; Turrisi, Ray, & Abar, 2010). For example, parental monitoring for college students may not include a much of a physical presence as in adolescence. However, parents remain a source of information and support for their young adult children and their attitude and monitoring sends both direct and indirect messages to their students (Turrisi, Ray, & Abar, 2010). By continuing to communicate and ask questions, parents will be more aware of their student’s behaviors and can reinforce health behavior while discussing risks. When parents monitor their college student’s behavior, they are also conveying their care and concern and are still responsible for knowing their child’s activities. In turn, their students may then act in a manner more in line with family values and continue to have the respect and trust from the parents. Research has supported that parental monitoring remains important for college students. Students with higher parental monitoring of alcohol use report both decreased drinking (Arria et al., 2008; Beck, Boyle, & Boekeloo, 2004; Carroll, et al., 2016) as well as decreases in other risky behaviors (Barnes, Farrell, & Banerjee, 1994; Bohnert, Anthony, & Breslau, 2012; Branstetter & Furman, 2013; Fletcher, 2004; Fors, Crepaz, & Hayes, 1999; Griffin, Botvin, Scheier, Diaz, & Miller, 2000). These findings suggest that higher parental monitoring may be protective against increases in alcohol use over time among students with depressed mood.
Parental monitoring and depression
Research has also shown that the relationship with parents is important in the adjustment and continuation through college (Mattanah, 2016; Patock-Peckham, & Morgan-Lopez, 2009; Brack, Gay, & Matheny 1993). For example, those who maintain a more secure relationship experience less distress when transitioning to college (Kenny & Donaldson, 1991). Langhinrichsen-Rohling, Larsen, and Jacobs (1997) found that adolescents with more cohesion to parents had smoother transitions to college and had an easier time developing new relationships. On the other hand, “helicopter parenting” (i.e. parents who take an overprotective or excessive interest in their kids’ lives) has been associated with increased depression (Schiffrin et al., 2014).
However, research to date has not examined how the relationship between depression and alcohol use and consequences may differ based on specific parenting practices. Parents can reduce risk and intervene not only with alcohol use, but perhaps especially if their college son/daughter is struggling with depressive issues. As both drinking and depression have increased prevalence in this population, and we know that those suffering with depression experience more alcohol-related negative consequences even at given drinking levels, parental monitoring may have an especially important protective impact for this vulnerable population. Parents with increased monitoring may have more knowledge of the struggles their son or daughter is dealing with. Additionally, since research shows college students continue to rely on their parents for health information (Vader, Walters, Roudsari, & Nguyen, 2011), parents who continue monitoring their children in college may be able to direct them to services or self-care practices needed to address their depressive symptoms. Thus, the current paper explores how students’ perceptions of parental monitoring moderate the relationship between self-reported depressive symptoms and later drinking and specific drinking-related consequences during college. We hypothesized students with depressive symptoms at baseline who perceived higher parental monitoring would report less drinking and fewer drinking-related consequences at one-year follow-up compared to their peers who reported lower levels of parental monitoring. Students subjectively rate some consequences as more negative than others (Mallett, Bachrach, & Turrisi, 2008; Merrill, Read, & Colder, 2013) and parents may also have certain consequences they would like their children to avoid. Thus, the analysis on which if any consequences would be impacted was left as exploratory.
Method
Participants
The sample consisted of 796 students enrolled in a large public university in the northwestern United States. Students were eligible to participate if they were in their first year of college, enrolled full-time, and between the ages of 18–19. Participants were on average 18.19 (SD = .39) years old at T1 (fall semester of the first year). The majority identified as female (60.2%) and Caucasian (55.8%). Other races represented in the sample were Asian (27.3%,), African American (2.1%), Native Hawaiian or Pacific Islander (1.5%), American Indian or Alaskan Native (0.9%), multi-racial (7.7%), and other (3.5%).
Procedures
Students who met inclusion criteria were randomly selected from the university registrar’s database and invited to participate (N=1799). Each participant was mailed an invitation letter conveying the general purpose and procedures of the study, compensation ($30 for each assessment), and a URL and Personal Identification Number (PIN) to access the questionnaire. This information was also provided in an e-mail and participants received up to six e-mailed reminders to complete the survey. Invitations and reminders were emailed to continuing participants during the fall semester of their second year (T2). The university’s local institutional review boards approved all study procedures.
Of the 1799 invited students, 796 (44.3%) completed the questionnaire at T1, and 692 completed at T2 (86.9% retention rate). Chi-square and t-test analyses revealed participants who were lost to attrition were not significantly different from participants who were retained on demographics (i.e., gender, race), depressed mood or typical weekly drinking at T1 (all p’s > .05).
Measures
To examine the aims of the current study, outcomes (drinking and alcohol-related consequences) were measured at T2. Depressed mood and parental monitoring were assessed at T1. Means and standard deviations for each of the measured variables, as well as the bivariate correlations between these variables are provided in Table 1.
Table 1.
Means (M), Standard Deviations (SD) and Bivariate Correlations for Continuous Predictors and Outcome Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | M(SD) | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Depressed Mood (T1) | --- | --- | --- | --- | --- | --- | --- | --- | --- | --- | 1.76 (3.03) |
| 2. Maternal Monitoring (T1) | −.09** | --- | --- | --- | --- | --- | --- | --- | --- | --- | 0.63 (1.00) |
| 3. Paternal Monitoring (T1) | −.11** | .60*** | --- | --- | --- | --- | --- | --- | --- | --- | 0.20 (1.02) |
| 4. Typical Weekly Drinking (T2) | .002 | −.09** | −.11** | --- | --- | --- | --- | --- | --- | --- | 5.24 (7.62) |
| 5. Negative Self-perceptions (T2) | .42*** | −.06` | −.11** | .42*** | --- | --- | --- | --- | --- | --- | 1.01 (2.15) |
| 6. Poor Self-care (T2) | .62*** | −.09* | −.11** | .62*** | .72*** | --- | --- | --- | --- | --- | 3.40 (6.48) |
| 7. Blackouts (T2) | .75*** | −.11*** | −.13*** | .75*** | .58*** | .75*** | --- | --- | --- | --- | 4.44 (6.86) |
| 8. Social-Interpersonal (T2) | .64*** | −.10** | −.14*** | .64*** | .68*** | .71*** | .72*** | --- | --- | --- | 2.54 (3.93) |
| 9. Academic-Occupational (T2) | .56*** | −.09* | −.08* | .56*** | .65*** | .76*** | .67*** | .64*** | --- | --- | 1.13 (2.47) |
| 10. Sexual (T2) | .41*** | −.10** | −.04 | .41*** | .40*** | .49*** | .52*** | .51*** | .45*** | --- | 0.32 (0.94) |
p < .10
p < .05
p < .01
p < .001
Typical weekly drinking.
Participants reported the number of alcoholic beverages they consumed on each day of a typical week during the past month using the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985). An alcoholic beverage was defined for participants as 12 oz. beer, 10 oz. wine cooler, 4 oz. wine, or 1 oz. 100 proof (1 ¼ oz. 80 proof) liquor. Items were summed to calculate an index score of typical weekly alcohol consumption (α = .82).
Negative drinking consequences.
Alcohol-related consequences were assessed with 27 items from the Young Adult Alcohol Consequences Questionnaire (YAACQ; Read, Kahler, Strong, & Colder, 2006) and two items from the Young Adult Alcohol Problems Screening Test (YAAPST; Abar et. al., 2009; Hurlbut & Sher, 1992; Larimer et al., 1999). Participants were asked to indicate the number of times they experienced each consequence (No or not in the past year = 0 to Eleven or more times in the past year = 6). Each of these items was endorsed by at least 5% of participants. Items were summed to form subscales of consequences. Items from the YAACQ measured social-interpersonal consequences (5 items, α = .84; e.g., While drinking, I have said or done embarrassing things.), negative self-perceptions (3 items, α = .86; e.g., I have felt badly about myself because of drinking.), poor self-care (8 items, α = .92; e.g., Because of my drinking, I have not eaten properly.), blackouts (7 items, α = .93; e.g., I have woken up in an unexpected place after heavy drinking.), and academic/occupational consequences (4 items, α = .87; e.g., The quality of my work or school work has suffered because of drinking.). These subscales are consistent with those described in Read et al (2006). Items from the YAAPST were used to assess sexual consequences (e.g., I had sex when I didn’t really want to because of drinking. and I have had sex with someone I wouldn’t ordinarily have sex with because of drinking.; α = .91).
Depressed mood.
Participants completed the depression subscale of the Depression, Anxiety and Stress Scale (DASS-21; Anthony, Biedling, Cox, Enns, & Swinson, 1998). The subscale consisted of seven items. Sample items included: I couldn’t seem to experience any positive feeling at all, and I found it difficult to work up the initiative to do things. Participants rated how much each item applied to them over the past week (never = 0 to almost always = 3). Items from each subscale were summed to create composite variable for depression (α = .88).
Perceived parental monitoring.
Two items assessed participants’ perception of parental monitoring: My father/mother tries to know where I go at night and My father/mother tries to know what I do during my free time. These items were adapted from Abar and Turrisi (2008) and Wood, Read, Mitchell, and Brand (2004) (also, see Varvil-Weld, Mallett, Turrisi, & Abar, 2012; Varvil-Weld, Turrisi, Hospital, Mallett, & Bamaca-Colbert, 2015). Participants were asked to rate each item twice, once for each parent. Ratings were on a 5-point Likert scale (strongly disagree = −2 to strongly agree = 2). Items were averaged to create a composite variable for maternal (α = .85) and paternal (α = .83) monitoring.
Covariates.
Students reported their sex (Males = 0; Females =1) and race. Race was dummy coded into three groups: Caucasians (reference group), Asians, and other (African American, Native Hawaiian or Pacific Islander, American Indian or Alaskan Native, multi-racial, and other).
Data Analytic Plan
To address missing data, we used the Expectation-Maximization (EM) algorithm in SPSS version 24 to impute missing data values for continuous variables. This allowed us to use data for participants who reported both sex and race (n = 786). Missingness on continuous predictors and outcomes ranged from 2.4% (depression) to 14.7% (paternal monitoring). According to Little’s missing completely at random (MCAR) test, data were MCAR (χ2(118) = 122.79, p = .36) (see Little & Rubin, 2002). Using the imputed data set, all predictors were mean-centered prior to conducting analyses.
Moderated linear regression was conducted in SPSS to examine the interactive effects of depression symptoms and parental monitoring on typical weekly drinking and alcohol-related consequence subscales. Separate regression models were conducted for each parent (i.e., maternal, paternal) and for each outcome. For example, typical weekly drinking was regressed onto maternal monitoring, depression, the product of maternal monitoring and depression, and the covariates (sex and race). In a separate analysis, typical weekly drinking was regressed onto paternal monitoring, depression, the product of paternal monitoring and depression, and the covariates. A second set of regression models repeated these analyses with each subtype of consequences as the outcome variable (i.e., negative self-perceptions, poor self-care, blackouts, social-interpersonal, academic/occupational, sexual).
To address any non-normality in the distribution of the outcomes, the models were estimated using bootstrapped samples (bootstrap N = 2000) to produce asymmetrical 95% confidence intervals around the parameter estimates. Effects were determined to be significant at p < .05 if the upper and lower limits of the confidence intervals (CI) did not contain zero.
Tukey’s HSD tests were conducted to determine the nature of the significant moderator effects. Each outcome (i.e., drinking and consequences) was examined across 3 levels (e.g., average; +1SD above average; −1SD below average) of each predictor variable (i.e., depressed mood and parental monitoring) (Jaccard & Turrisi, 2003).
Results
Tables 2 and 3 contain all estimates, standard errors and confidence intervals for main and interaction effects. Since the interaction of symptoms of depressed mood and perceived parental monitoring is the primary focus of this paper, only the main effects associated with instances of a significant interaction are reported in text. These effects and post hoc test results are discussed below.
Table 2.
Estimates, Standard Errors and Confidence Intervals for Main and Interaction Effects (Maternal Monitoring)
| Predictors |
Typical Drinking |
Negative
Self- perceptions |
Poor Self-care |
Blackout |
Social- Interpersonal |
Academic /
Occupational |
Sexual |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI | |
| Depression | −0.02 (0.08) | −0.16, 0.14 | 0.08 (0.03) | 0.03, 0.14* | 0.21 (0.08) | 0.06, 0.38* | 0.08 (0.08) | −0.07, 0.24 | 0.07 (0.04) | −0.01, 0.16* | 0.05 (0.03) | −0.003, 0.12 | 0.03 (0.02) | 0.002, 0.08* |
| Maternal-Monitoring | −0.36 (0.27) | −0.89, 0.18 | −0.13 (0.07) | −0.28, 0.02 | −0.49 (0.24) | −0.96, −0.04* | −0.59 (0.28) | −1.15, −0.03* | −0.38 (0.16) | −0.70, −0.08* | −0.20 (0.09) | −0.37, −0.03* | −0.08 (0.05) | −0.18, 0.01 |
| Sex | ||||||||||||||
| Female | −2.53 (0.61) | −3.72, −1.36* | 0.24 (0.15) | −0.05, 0.51 | 0.18 (0.48) | −0.75, 1.13 | −0.62 (0.53) | −1.74, 0.38 | 0.23 (0.28) | −0.31, 0.78 | −0.01 (0.18) | −0.38, 0.34 | −0.05 (0.07) | −0.19, 0.08 |
| Male (ref) | ||||||||||||||
| Race | ||||||||||||||
| Asian | −3.44 (0.55) | −4.51, −2.33* | −0.45 (0.14) | −0.72, −0.19* | −2.21 (0.47) | −3.19, −1.31* | −2.78 (0.49) | −3.73 −1.84* | −1.12 (0.27) | −1.64, −0.60* | −0.46 (0.20) | −0.85, −0.07* | −0.16 (0.08) | −0.31, 0.01 |
| Other | −0.97 (0.73) | −2.39, 0.49 | 0.41 (0.29) | −0.11, 0.99 | −0.56 (0.65) | −1.81, 0.79 | −0.40 (0.68) | −1.69, 0.95 | 0.27 0.45) | −0.60, 1.20 | −0.07 (0.25) | −0.55, 0.47 | 0.00 (0.10) | −0.18, 0.21 |
| White (ref) | ||||||||||||||
| Depression x Monitoring | −0.16 (0.08) | −0.31, −0.01* | −0.08 (0.03) | −0.14, −0.03* | −0.24 (0.09) | −0.43, −0.07* | −0.24 (0.11) | −0.45, −0.04* | −0.07 (0.05) | −0.16, 0.02 | −0.04 (0.03) | −0.11, 0.004 | −0.05 (0.03) | −0.10, 0.0001 |
p < .05.
Notes: B, unstandardized regression coefficient; SE, unstandardized standard error; CI, confidence interval; Female = 1, Male = 0; Caucasian is the reference group for race; Other includes participants who indicated African American, Native Hawaiian or Pacific Islander, American Indian or Alaskan Native, multi-racial, and other.
Table 3.
Estimates, Standard Errors and Confidence Intervals for Main and Interaction Effects (Paternal Monitoring)
| Predictors |
Typical Drinking |
Negative
Self- perceptions |
Poor Self-care |
Blackout |
Social- Interpersonal |
Academic /
Occupational |
Sexual |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI |
B (SE) |
CI | |
| Depression | −0.01 (0.07) | −0.15, 0.14 | 0.08 (0.03) | 0.03, 0.14* | 0.21 (0.08) | 0.07, 0.40* | 0.09 (0.08) | −0.05, 0.28 | 0.07 (0.04) | −0.01, 0.16 | 0.05 (0.03) | −0.002, 0.12 | 0.03 (0.02) | 0.001, 0.08* |
| Paternal-Monitoring | −0.63 (0.28) | −1.17, −0.07* | −0.22 (0.08) | −0.38, −0.06* | −0.62 (0.23) | −1.07, −0.18* | −0.67 (0.27) | −1.22, −0.10* | −0.50 (0.16) | −0.81, −0.21* | −0.18 (0.09) | −0.35, −0.02* | −0.03 (0.04) | −0.10, 0.06 |
| Sex | ||||||||||||||
| Female | −2.59 (0.58) | −3.74, −1.51* | 0.22 (0.14) | −0.06, 0.51 | 0.09 (0.46) | −0.85, 1.00 | −0.73 (0.50) | −1.72, 0.24 | 0.16 (0.28) | −0.38, 0.68 | −0.05 (0.18) | −0.42, 0.31 | −0.06 (0.07) | −0.20, 0.07 |
| Male (ref) | ||||||||||||||
| Race | ||||||||||||||
| Asian | −3.35 (0.54) | −4.42, −2.25* | −0.42 (0.13) | −0.70, −0.16* | −2.16 (0.47) | −3.06, −1.23* | −2.75 (0.50) | −3.71, −1.77* | −1.08 (0.28) | −1.61, −0.53* | −0.47 (0.20) | −0.85, −0.07* | −0.18 (0.08) | −0.33, −0.01* |
| Other | −0.89 (0.73) | −2.29, 0.58 | 0.44 (0.28) | −0.09, 1.01 | −0.51 (0.65) | −1.72, 0.82 | −0.36 (0.70) | −1.73, 1.02 | 0.32 (0.47) | −0.58, 1.30 | −0.07 (0.26) | −0.55, 0.49 | −0.01 (0.10) | −0.19, 0.19 |
| White (ref) | ||||||||||||||
| Depression x Monitoring | −0.13 (0.08) | −0.29, 0.02 | −0.08 (0.03) | −0.13, −0.02* | −0.24 (0.08) | −0.42, −0.10* | −0.19 (0.10) | −0.41, −0.01* | −0.06 (0.05) | −0.15, 0.03 | −0.03 (0.03) | −0.08, 0.02 | −0.03 (0.02) | −0.08, 0.001 |
p < .05
Notes: B, unstandardized regression coefficient; SE, unstandardized standard error; CI, confidence interval; Female = 1, Male = 0; Caucasian is the reference group for race; Other includes participants who indicated African American, Native Hawaiian or Pacific Islander, American Indian or Alaskan Native, multi-racial, and other.
Maternal Monitoring as a Moderator
Typical weekly drinking.
The main effect for depressed mood on drinking was not significant (b = −.02, SE = .08, 95% CI [−.16, .14]). A non-significant association was also detected between maternal monitoring and drinking (b = −.36, SE = .27, 95% CI [−.89, .18]). Examination of the product term revealed a significant interaction effect (b = −.16, SE = .08, 95% CI [−.31, −.01]). However, post hoc analysis did not reveal for whom drinking differed (see Table 4).1
Table 4.
Typical Weekly Drinking Means for Perceived Parent Monitoring (columns) and Depressive Symptoms (rows).
| Typical Weekly Drinking | |||
|---|---|---|---|
| Predictors | Maternal Monitoring | ||
| Depression | Below-Average | Average | Above-Average |
| Below-Average | 7.72 | 7.86 | 7.99 |
| Average | 8.21 | 7.86 | 7.52 |
| Above-Average | 8.69 | 7.87 | 7.04 |
| Mean Difference | 0.97 | 0.01 | 0.95 |
Note: Means that are significantly different are bolded.
Indicates that mean difference exceeds Tukey’s HSD critical difference, p < .05.
Negative self-perception consequences.
The main effect for depression on negative self-perceptions consequences was significant (b = .08, SE = .03, 95% CI [.03, .14]); as depression increased, negative self-perceptions related to drinking increased. The effect of maternal monitoring on negative self-perceptions resulting from drinking was not significant (b = −.13, SE = .07, 95% CI [−.28, .02]). A significant interaction effect was detected (b = −.08, SE = .03, 95% CI [−.14, −.03]). Post-hoc analysis revealed a significant difference in negative self-perception consequences between below average and above-average levels of depression for students who were below average on perceived maternal monitoring (p < .05; see Table 5). This suggests that as depressive symptoms increased, students with below average levels of maternal monitoring reported a greater number of negative self-perception consequences (see Figure 2).
Table 5.
Drinking-related Consequences (Negative Self-perceptions, Poor Self-care, and Blackout Drinking) Means for Perceived Parent Monitoring (columns) and Depressive Symptoms (rows).
| Negative Self-Perception | Poorer Self-Care | Blackout Drinking | |||||||
| Predictors | Maternal Monitoring | Maternal Monitoring | Maternal Monitoring | ||||||
| Depression | Below-Average | Average | Above-Average | Below-Average | Average | Above-Average | Below-Average | Average | Above-Average |
| Below-Average | 0.52 | 0.65 | 0.78 | 2.99 | 3.26 | 3.52 | 5.14 | 5.29 | 5.44 |
| Average | 1.05 | 0.92 | 0.80 | 4.44 | 3.98 | 3.51 | 6.20 | 5.63 | 5.06 |
| Above-Average | 1.57 | 1.20 | 0.82 | 5.89 | 4.69 | 3.50 | 7.27 | 5.98 | 4.69 |
| Mean Difference | 1.05* | 0.55 | 0.04 | 2.90* | 1.43 | 0.02 | 2.13* | 0.69 | 0.75 |
| Predictors | Paternal Monitoring | Paternal Monitoring | Paternal Monitoring | ||||||
| Depression | Below-Average | Average | Above-Average | Below-Average | Average | Above-Average | Below-Average | Average | Above-Average |
| Below-Average | 0.63 | 0.64 | 0.65 | 3.10 | 3.24 | 3.37 | 5.38 | 5.31 | 5.24 |
| Average | 1.16 | 0.94 | 0.72 | 4.65 | 4.05 | 3.45 | 6.38 | 5.72 | 5.06 |
| Above-Average | 1.69 | 1.23 | 0.79 | 6.21 | 4.87 | 3.52 | 7.39 | 6.13 | 4.88 |
| Mean Difference | 1.06* | 0.59 | 0.14 | 3.11* | 1.63 | 0.15 | 2.01* | 0.82 | 0.36 |
Note: Means that are significantly different are bolded.
Indicates that mean difference exceeds Tukey’s HSD critical difference, p < .05.
Figure 2.
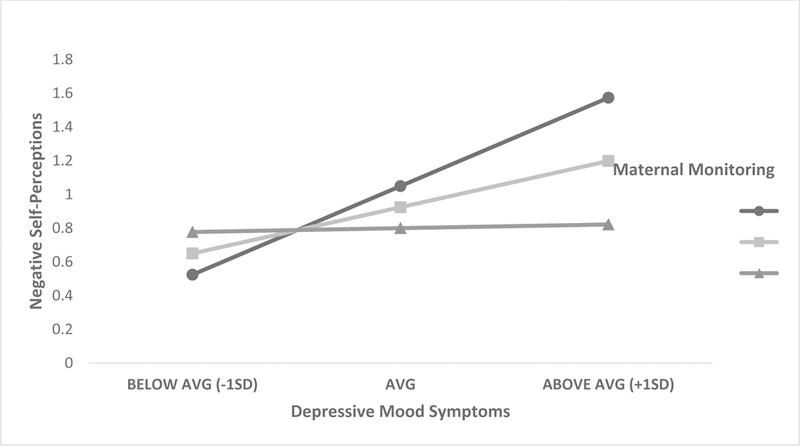
Interaction between Depressive Symptoms and Perceived Maternal Monitoring on Negative Self-Perceptions Consequences.
Poor self-care consequences.
The association between depressed mood and poor self-care consequences was significant (b = .21, SE = .08, 95% CI [.06, .38]); as depression increased, poorer self-care consequences of drinking increased. The effect of maternal monitoring on poor self-care was also significant (b = −.49, SE = .24, 95% CI [−.96, −04]); as perceptions of maternal monitoring increased, poor self-care drinking consequences decreased. A significant interaction effect was also detected (b = −.24, SE = .09, 95% CI [−.43, −.07]). Post-hoc analysis showed a significant difference in self-care consequences between below average and above-average levels of depression for students who were below average on perceived maternal monitoring (p < .05; see Table 5). This suggests that as depressive symptoms increased, students with below average levels of maternal monitoring reported a greater number of poor self-care consequences (see Figure 3).
Figure 3.
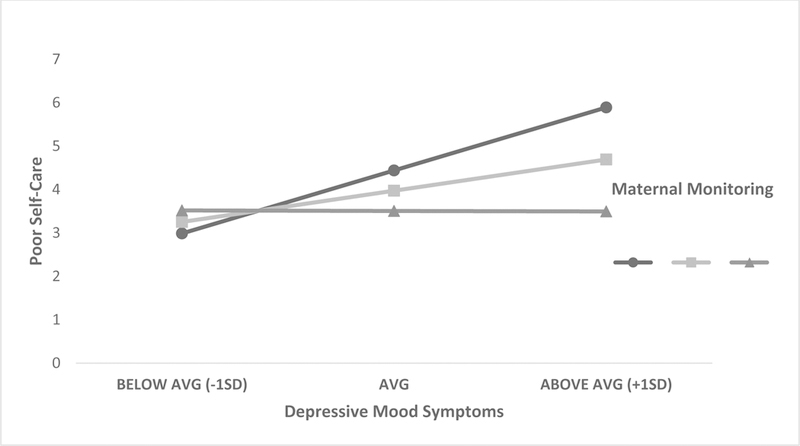
Interaction between Depressive Symptoms and Perceived Maternal Monitoring on Poor Self-Care Consequences.
Blackout consequences.
The main effect for depression on blackout consequences was not significant (b = .08, SE = .08, 95% CI [−.07, .24]). The effect of maternal monitoring on blackout was significant (b = −.59, SE = .28, 95% CI [−1.15, −03]); as perceptions of maternal monitoring increased, the number of blackout consequences reported decreased. The interaction effect was also significant (b = −.24, SE = .09, 95% CI [−.43, −.07]). Post-hoc analysis revealed a significant difference in blackout consequences between below average and above-average levels of depression for students who were below average on perceived maternal monitoring (p < .05; see Table 5). This suggests that as depressive symptoms increased, students with below average levels of maternal monitoring reported a greater number of blackouts (see Figure 4).
Figure 4.
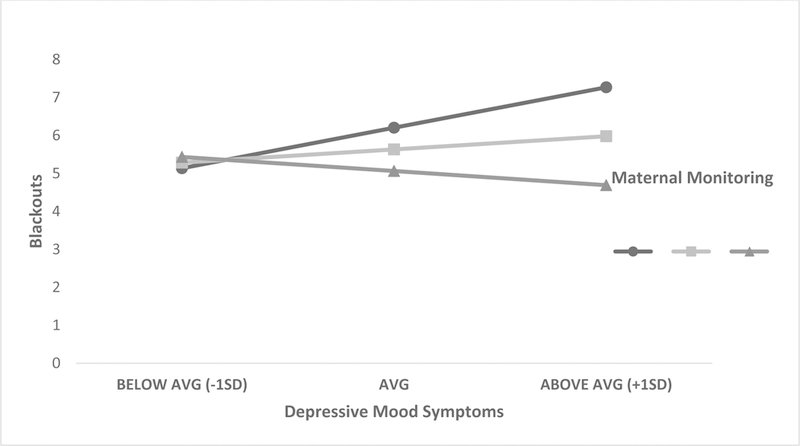
Interaction between Depressive Symptoms and Perceived Maternal Monitoring on Blackout Consequences.
Paternal Monitoring as a Moderator
Table 2 lists all results for analyses that included perceptions of paternal monitoring. Moderator effects were similar to those reported for mothers. That is, perceived paternal monitoring moderated the effects of depressed mood on negative self-perceptions, poor self-care, and blackout consequences (see Table 5). No other significant moderation effects were detected between depressed mood symptoms and perceived paternal monitoring. Further discussion and implications are provided below.
Exploratory Analyses
Since some students’ will increase their drinking habits from the first year of college to second year, a set of exploratory analyses were conducted to determine if the moderation effects of parental monitoring held in students whose drinking increased. The previous set of analyses were repeated with only students who increased their typical weekly drinking (N=284). Results revealed that the effects of depressed mood x maternal monitoring on negative self-perceptions and on poor self-care were significant (b = −.14, SE = .01, 95% CI [−.25, −.01], b = −.35, SE = .01, 95% CI [−.82, −.004], respectively). The interaction between depressed mood and paternal monitoring on poor self-care was also significant (b = −.29, SE = .02, 95% CI [−.74, −.03]). These results suggest that monitoring reduced the effect of depression on these two consequences even among students who increased their drinking. For the remaining analyses, the results did not show a significant buffering effect.
Discussion
The current study was designed to evaluate the extent to which the relationship between depressed mood and negative drinking outcomes (use and consequences) is moderated by perceived parental monitoring. Overall, results reveal that student perceptions of maternal and paternal monitoring interact with their reported depressive symptoms to influence negative self-perceptions, poor self-care, and blackout consequences of drinking. Specifically, students with higher levels of depressive symptoms who perceived lower monitoring had more of these consequences than did depressed students who perceived higher maternal monitoring. This may be related to the specifics of depressive symptoms such as low self-esteem and motivation to care for oneself which may be exacerbated when there is the perception that nobody is looking out for the student. Additionally, while research indicates that students rely on the parents for health information (Vader, Walters, Roudsari, & Nguyen, 2011), this may occur less for students with low perceived parental monitoring and these students may not get support for self-care or directed to professional help from their parents. Instead, these students may aim to reduce their negative affect by self-medicating with alcohol, which may lead to increases in these specific alcohol-related consequences.
There are several implications for interventions based on these findings. First, findings suggest parent-based interventions designed to increase monitoring may help to dampen the effects of depression on certain negative drinking consequences (i.e., negative self-perceptions, lack of self-care). Parental monitoring may serve to remind the student of the presence of one or more caring adults in their life, which may contribute to their ability to alternative coping strategies rather than drinking. Increased monitoring may also allow parents to recognize signs and symptoms of depression in their son or daughter and help support them in getting appropriate care. Parent interventions emphasizing effective monitoring techniques and providing support for the protective role of monitoring into the college years could be an important avenue for administrators.
These findings also illustrate the potential importance of treating depressed mood symptoms in order to reduce alcohol related consequences in college populations. Despite the high prevalence of socially-motivated and celebratory drinking on college campuses, drinking to cope with negative affect is relevant for a significant minority of students in these settings (Colder, 2001; Cooper, Frone, M.R., Russell, M. & Mudar, 1995; Kuntsche, Knibbe, Gmel, & Engels, 2005). Providing alternative coping strategies and other brief interventions to reduce depressed mood has shown potential to improve both depression and drinking outcomes (Geisner et al., 2015; Merrill, Reid, Carey, Carey, 2014; Murphy et al., 2012).
The current study has several strengths, including a relatively large sample, as well as a longitudinal design with good retention across a one-year follow-up period and use of well-validated measures of predictor and outcome variables. One limitation is that all data, including alcohol and depressed mood variables as well as parental monitoring, were based on self-report from the perspective of the student alone, rather than including parent reports. Nonetheless, research has consistently indicated that confidential self-reports of alcohol and mental health symptoms in non-treatment-seeking samples of young adults are generally both reliable and valid as long as established measures are used and there are no consequences (i.e., punishment) for accurate reporting (Kypri, et al., 2016; LaForge, Borsari, & Baer, 2005; Simons, Wills, Emery, & Marks, 2015). Similarly, our own and other research has demonstrated that student reports correlate well with parent reports of monitoring behaviors in this population (Varvil-Weld, Turrisi, Scaglione, Mallett, Ray, 2013). Another limitation is that the lack of certain measures (such as those measuring parenting style, e.g. “helicopter parenting”) preclude finer analysis on cause and effect between parenting style and how it is related to increased depression. It is possible that parents of depressed children may hover more to protect them from increased risks. Assessing other covariates, such as socio-economic status, major, athletic participation and the like would further shed light on these relationships. Finally, we analyzed parents separate as literature has found mothers and fathers differed on parenting constructs and drinking outcomes (e.g., Patock-Peckham, Cheong, Balhom, & Nagoshi, 2001; Patock-Peckham & Morgan-Lopez, 2007, 2010).
Despite limitations, the current research adds to the literature on the relation between depressed mood, alcohol use and consequences, and parenting behaviors in a college population, and provide support for the importance of including parents in efforts to reduce alcohol use and consequences among students suffering from elevated depressive symptoms. Future research is needed to further examine mechanisms through which parental monitoring impacts alcohol use and consequences among depressed students, as well as to further test parenting interventions to address alcohol and depression comorbidity in this population.
Figure 1.
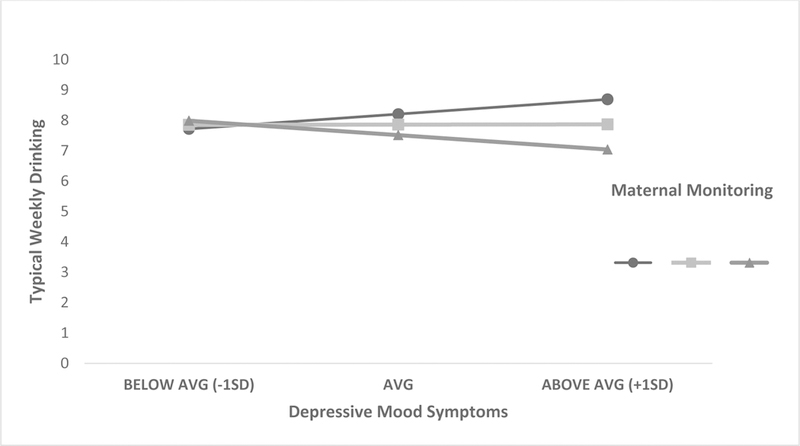
Interaction between Depressive Symptoms and Perceived Maternal Monitoring on Typical Weekly Drinking.
Acknowledgement:
This research was supported by NIAAA R01AA012529 awarded to Rob Turrisi. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIAAA or the National Institutes of Health.
Footnotes
Analyses were also conducted using peak drinking as an outcome (i.e., students reported the maximum number of drinks consumed on an occasion within the past 30 days; Dimeff et al., 1999; Marlatt et al., 1998). Results were similar to those reported for typical weekly.
References
- Abar C, & Turrisi R (2008). How important are parents during the college years? A longitudinal perspective of indirect influences parents yield on their college teens’ alcohol use. Addictive Behaviors, 33(10), 1360–1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American College Health Association (ACHA) (2003). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. Hanover, MD: American College Health Association. [Google Scholar]
- American College Health Association (ACHA) (2014). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2014. Hanover, MD: American College Health Association. [Google Scholar]
- Anthony MM, Bieling PJ, Cox BJ, Murray M, & Swinson RP (1998). Psychometric properties of the 42-item and 21 item version of the depression anxiety stress scales in clinical groups and a community sample. Psychological Assessment, 10(2), 176–181. [Google Scholar]
- Arria AM, Kuhn V, Caldeira KM, O’Grady KE, Vincent KB, & Wish ED (2008). High school drinking mediates the relationship between parental monitoring and college drinking: A longitudinal analysis. Substance Abuse Treatment, Prevention, and Policy, 3, 6. doi: 10.1186/1747-597X-3-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes GM, Farrell MP, & Banerjee S (1994). Family influences on alcohol abuse and other problem behaviors among black and white adolescents in a general population sample. Journal of Research on Adolescence, 4, 183–201. [Google Scholar]
- Barnes GM, Welte JW, Hoffman JH, & Dintcheff BA (2005). Shared predictors of youthful gambling, substance use, and delinquency. Psychology of Addictive Behaviors, 19, 165. [DOI] [PubMed] [Google Scholar]
- Beck KH, Boyle JR, & Boekeloo BO (2004). Parental monitoring and adolescent drinking: results of a 12-month follow-up. American Journal of Health Behavior, 28, 272–279. [DOI] [PubMed] [Google Scholar]
- Bohnert KM, Anthony JC, & Breslau N (2012). Parental monitoring at age 11 and subsequent onset of cannabis use up to age 17: Results from a prospective study. Journal of Studies on Alcohol and Drugs, 73(2), 173–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brack G, Gay MF, & Matheny KB (1993). Relationships between attachment and coping resources among late adolescents. Journal of College Student Development, 34, 212–215. [Google Scholar]
- Branstetter SA, & Furman W (2013). Buffering effect of parental monitoring knowledge and parent-adolescent relationships on consequences of adolescent substance use. Journal of Child and Family Studies, 22(2), 192–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll HA, Heleniak C, Witkiewitz K, Lewis M, Eakins D, Staples J, Andersson C, Berglund M, & Larimer M (2016). Effects of parental monitoring on alcohol use in the US and Sweden: A brief report. Addictive Behaviors, 63, 89–92, doi: 10.1016/j.addbeh.2016.07.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol consumption: the effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53, 189–200. doi: 10.1037/0022-006X.53.2.189 [DOI] [PubMed] [Google Scholar]
- Colder CR (2001). Life stress, physiological and subjective indexes of negative emotionality, and coping reasons for drinking: Is there evidence for a self-medication model of alcohol use? Psychology of Addictive Behaviors, 15, 237–245. doi: 10.1037/0893-164X.15.3.237 [DOI] [PubMed] [Google Scholar]
- Cooper M, Frone MR, Russell M & Mudar P (1995). Drinking to regulate positive and negative emotions: A motivational model of alcohol use. Journal of Personality & Social Psychology, 69, 990–1005. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Grant BF, Stinson FS, & Chou PS (2005). Psychopathology associated with drinking and alcohol use disorders in the college and general adult populations. Drug and Alcohol Dependence, 77, 139–150. doi: 10.1016/j.drugalcdep.2004.07.012 [DOI] [PubMed] [Google Scholar]
- Fletcher AC, Steinberg L, & Williams‐Wheeler M (2004). Parental influences on adolescent problem behavior: Revisiting Stattin and Kerr. Child Development, 75(3), 781–796. [DOI] [PubMed] [Google Scholar]
- Fors SW, Crepaz N, & Hayes DM (1999). Key factors that protect against health risks in youth: further evidence. American journal of health behavior, 23, 368–380. [Google Scholar]
- Gallagher RP (2009). National Survey of Counseling Center Directors, 2009 Monograph Series Number 8R. Alexandria, VA: The International Association of Counseling Services, Inc; http://www.education.pitt.edu/survey/nsccd/archive/2009/monograph.pdf. [Google Scholar]
- Geisner IM, Larimer ME, & Neighbors C (2004). The relationship between alcohol use, related problems, and psychological distress: Gender as a moderator in a college sample. Addictive Behaviors, 29, 843–848. doi: 10.1016/j.addbeh.2004.02.024 [DOI] [PubMed] [Google Scholar]
- Geisner IM, Mallett K, & Kilmer JR (2012). An examination of depressive symptoms and drinking patterns in first year college students. Issues in Mental Health Nursing, 33, 280–287. doi: 10.3109/01612840.2011.653036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner IM, Neighbors C, Lee CM, & Larimer ME (2007).Evaluating personal alcohol feedback as a selective prevention for college students with depressed mood. Addictive Behaviors, 32, 2776–2787. doi: 10.1016/j.addbeh.2007.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner IM, Varvil-Weld L, Mittmann A, Mallett K, & Turrisi R (2015). Brief web-based intervention for college students with comorbid risky alcohol use and depressed mood: Does it work and for whom? Addictive Behaviors, 42, 36–43. doi. 10.1016/j.addbeh.2014.10.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottfredson NC, & Hussong AM (2013). Drinking to dampen affect variability: Findings from a college student sample. Journal of Studies on Alcohol and Drugs, 74, 576–583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffin KW, Botvin GJ, Scheier LM, Diaz T, & Miller NL (2000). Parenting practices as predictors of substance use, delinquency, and aggression among urban minority youth: Moderating effects of family structure and gender. Psychology of Addictive Behaviors, 14, 174–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hingson RW, Zha W, & Weitzman ER (2009). Magnitude of and trends in alcohol-related mortality and morbidity among US college students ages 18–24, 1998–2005. Journal of Studies on Alcohol and Drugs, Supplement, (16), 12–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ichiyama MA, Fairlie AM, Wood MD, Turrisi R, Francis DP, Ray AE, & Stanger LA (2009). A randomized trial of a parent-based intervention on drinking behavior among incoming college freshmen. Journal of Studies on Alcohol and Drugs, Supplement 16, 67–76. [PMCID: PMC2701098] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaccard J, & Turrisi R. (2003). Interaction effects in multiple regression. 2nd ed. Sage: Newbury Park, CA. [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG, & Schulenberg JE (2013). Monitoring the Future national results on drug use: 2012 Overview, Key Findings on Adolescent Drug Use. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Kaynak Ö, Meyers K, Caldeira KM, Vincent KB, Winters KC, & Arria AM (2013). Relationships among parental monitoring and sensation seeking on the development of substance use disorder among college students. Addictive behaviors, 38(1), 1457–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kay-Lambkin FJ, Baker AL, Lewin TJ, & Carr VJ (2009). Computer-based psychological treatment for comorbid depression and problematic alcohol and/or cannabis use: a randomized controlled trial of clinical efficacy. Addiction, 104, 378–388. doi: 10.1111/j.1360-0443.2008.02444. [DOI] [PubMed] [Google Scholar]
- Kenny ME & Donaldson GA (1991). Contributions of Parental Attachment and Family Structure to the Social and Psychological Functioning of First-Year College Students. Journal of Counseling Psychology, 38, 479–86. [Google Scholar]
- Khantzian EJ (1985). The self-medication hypothesis of addictive disorders: Focus on heroin and cocaine dependence. American Journal of Psychiatry, 142, 1259–1264. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ (2003) The Self-Medication Hypothesis Revisited: The Dually Diagnosed Patient. Primary Psychiatry 10, 47–48, 53–54. [Google Scholar]
- Kitzrow MA (2003). The mental health needs of today’s college students: Challenges and recommendations. National Association of Student Personnel Administrators (NASPA) Journal, 42(1), 167–181. [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, & Engels R (2005). Why do young people drink? A review of drinking motives. Clinical Psychology Review, 25, 841–61. [DOI] [PubMed] [Google Scholar]
- Kuntsche E, Nic Gabhainn S, Roberts C, Windlin B, Vieno A, Bendtsen P, Hublet A, Tynjälä J, Välimaa R, Dankulincová Z, Aasvee K, Demetrovics Z, Farkas J, van der Sluijs W, Gaspar de Matos M, Mazur J, & Wicki M (2014). Drinking motives and links to alcohol use in 13 European countries. Journal of Studies on Alcohol and Drugs, 75, 428–437. [DOI] [PubMed] [Google Scholar]
- Kypri K, Wilson A, Attia J, Sheeran P, Miller P, & McCambridge J (2016). Social Desirability Bias in the Reporting of Alcohol Consumption: A Randomized Trial. Journal of Studies on Alcohol and Drugs, 77, 526–531 (2016). [DOI] [PubMed] [Google Scholar]
- Laforge RG, Borsari B, & Baer JS (2005). The utility of collateral informant assessment in college alcohol research: Results from a longitudinal prevention trial. Journal of Studies on Alcohol, 66, 479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langhinrichsen‐Rohling J, Larsen A and Jacobs J 1997. Retrospective reports of the family of origin environment and the transition to college. Journal of College Student Development, 38, 49–61. [Google Scholar]
- Little RJA, & Rubin DB (2002). Statistical analysis with missing data: Second Edition New York: Wiley. [Google Scholar]
- Mattanah JF (2016). College Student Psychological Adjustment: Exploring Relational Dynamics That Predict Success. Momentum Press; NYC, NY. [Google Scholar]
- Mallett KA, Bachrach RL, Turrisi R (2008). Are all negative consequences truly negative? Assessing variations mong college students’ perceptions of alcohol related consequences. Addictive Behaviors, 33, 1375–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill JE, Reid AE, Carey MP, & Carey KB (2014). Gender and depression moderate response to brief motivational intervention for alcohol misuse among college students. Journal of Consulting and Clinical Psychology, doi: 10.1037/a0037039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merrill, Read JP, & Colder CR (2013). Normative perceptions and past year consequences as predictors of subjective evaluations and weekly drinking behavior. Addictive Behaviors, 38, 2625–2634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miles Cox W, & Klinger E (1988). A motivational model of alcohol use. Journal of Abnormal Psychology, 97, 168–180. [DOI] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, & Martens MP (2012). A randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology, 80(5), 876–886. doi: 10.1037/a0028763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patock-Peckham JA, Cheong J, Balhorn ME and Nagoshi CT (2001). A social learning perspective: A model of parenting styles, self-regulation, perceived drinking control, and alcohol use and problems. Alcoholism: Clinical and Experimental Research, 25, 1284–1292. [PubMed] [Google Scholar]
- Patock-Peckham JA, & Morgan-Lopez AA (2009). College drinking behaviors: Meditational likes between parental bonds, depression, and alcohol problems. Psychology of Addictive Behaviors, 21(3), 297–306. [DOI] [PubMed] [Google Scholar]
- Patock-Peckham JA, & Morgan-Lopez AA (2010). Direct and mediational links between parental bonds and neglect, antisocial personality, reasons for drinking, alcohol use, and alcohol problems. Journal of Studies on Alcohol and Drugs, 71(1), 95–104. [DOI] [PubMed] [Google Scholar]
- Read JP, Kahler CW, Strong DR, & Colder CR (2006). Development and preliminary validation of the young adult alcohol consequences questionnaire. J Stud Alcohol 67:169–177. [DOI] [PubMed] [Google Scholar]
- Ross V (2004). Depression, anxiety, and alcohol or other drug use among college students. Retrieved from Education Development Center, Inc; website: www.edc.org. [Google Scholar]
- Schiffrin HH, Liss M, Miles-McLean H, Geary KA, Erchull MJ, Tashner T (2014). Helping or Hovering? The Effects of Helicopter Parenting on College Students’ Well-Being. Journal of Child and Family Studies, 23, 548–557. [Google Scholar]
- Simons JS, Wills TA, Emery NN, & Marks RM (2015). Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addictive Behaviors, 50, 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA), U.S. Department of Health and Human Services. (2008). Results from the 2007 National Survey on Drug Use and Health: National Findings (Report No. NSDUH Series H-34, DHHS Publication No. SMA 08–4343). Office of Applied Statistics: Rockville, MD. [Google Scholar]
- Tabachnick BG, & Fidell LS (2012). Using multivariate statistics (5th edition). New York, NY: Pearson. [Google Scholar]
- Turner EA, Chandler M, & Heffer RW (2009). The influence of parenting styles, achievement motivation, and self-efficacy on academic performance in college students. Journal of College Student Development, 50(3), 337–346. [Google Scholar]
- Turrisi R, Larimer ME, Mallett K, Kilmer JR, Ray A, Mastroleo N, Geisner IM, Grossbard J, Tollison S, Lostutter T, & Montoya H (2009). A randomized clinical trial evaluating a combined intervention for high-risk students. Journal of Studies on Alcohol and Drugs, 70, 555–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrisi R, Ray A, & Abar C (2010). When is parenting over? Examining parental monitoring and high-risk alcohol consumption in young adult college students In Guilamo-Ramos V, Jaccard J, & Dittus P (Eds.), Parental monitoring of adolescents: Current perspectives for researchers and practitioners. NY: Columbia University Press, pp. 124–146. [Google Scholar]
- Vader AM, Walters ST, Roudsari B, & Nguyen N (2011). Where do college students get health information? Believability and use of health information sources. Health promotion practice, 12(5), 713–722. [DOI] [PubMed] [Google Scholar]
- Varvil-Weld L, Turrisi R, Hospital MM, Mallett KA, & Bámaca-Colbert MY (2014). Maternal and peer influences on drinking among Latino college students. Addictive Behavior, 39, 246–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varvil-Weld L, Turrisi R, Scaglione N, Mallett KA, Ray AE (2013). Parents’ and students’ reports of parenting: Which are more reliably associated with college student drinking? Addictive Behaviors, 38, 1699–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varvil-Weld L, Mallett KA, Turrisi R, & Abar CC (2012). Using parental profiles to predict membership in a subset of college students experiencing excessive alcohol consequences: findings from a longitudinal study. Journal of Studies on Alcohol and Drugs, 73(3), 434–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzman E (2004). Poor mental health, depression, and associations with alcohol consumption, harm, and abuse in a national sample of young adults in college. Journal of Nervous and Mental Disease, 192, 269–277. doi: 10.1097/01.nmd.0000120885.17362.94 [DOI] [PubMed] [Google Scholar]
- Wetherill RR, Schnyer DM, & Fromme K (2012). Acute Alcohol Effects on Contextual Memory BOLD Response: Differences Based on Fragmentary Blackout History. Alcoholism Clinical and Experimental Research, 36, 1108–1115. doi: 10.1111/j.1530-0277.2011.01702.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wood MD, Read JP, Mitchell RE, & Brand NH (2004). Do parents still matter? Parent and peer influences on alcohol involvement among recent high school graduates. Psychology of Addictive Behaviors, 18, 19–30. [DOI] [PubMed] [Google Scholar]


