Abstract
Introduction
Vertebral fractures associated with ankylosing spinal disorders pose significant diagnostic and therapeutic challenges. Notably, the ankylosed spine remains in ankylosis after fracture treatment, and the underlying susceptibility to further fractures still remains. Nevertheless, information is scarce in the literature concerning patients with ankylosing spinal disorders who have multiple episodes of vertebral fractures.
Case Report
Case 1 involves an 83-year-old male patient with diffuse idiopathic skeletal hyperostosis (ankylosis from C2 to L4) who had three episodes of vertebral fractures. The first episode involved a C5-C6 extension-type fracture, which was treated with posterior segmental screw instrumentation. Five years later, the patient sustained a three-column fracture at the L1 vertebra following another fall. The fracture was managed with percutaneous segmental screw instrumentation. One year and two months postoperatively, the patient fell again and had a refracture of the healed L1 fracture. The patient was treated with a hard brace, and the fracture healed. Case 2 involves a 76-year-old female patient with ankylosing spondylitis (ankylosis from C7 to L2) who had two episodes. At the first episode, she suffered paraplegia due to a T8 vertebra fracture. The patient was treated with laminectomy and posterior segmental screw instrumentation. The patient recovered well and had all the hardware removed at 10 months postoperatively. Five years later, she had another fall and suffered a three-column fracture at L1. The patient underwent percutaneous segmental screw instrumentation. The patient required revision surgery with L1 laminectomy and L1 right pediclectomy for persistent right inguinal pain. At one-year follow-up, the patient recovered well, and the fracture healed.
Conclusions
The abovementioned cases show that an age older than 75 years and a long spinal ankylosis from the cervical spine to the lumbar spine may serve as risk factors for the repetition of vertebral fractures associated with ankylosed spinal disorders.
Keywords: Ankylosing spinal disorder, Diffuse idiopathic skeletal hyperostosis, Ankylosing spondylitis, Fracture
Introduction
Ankylosing spinal disorders (ASDs) represent a group of conditions where multilevel spinal columns are contiguously fused by either inflammatory (e.g., ankylosing spondylitis (AS)) or noninflammatory (e.g., diffuse idiopathic skeletal hyperostosis (DISH)) etiologies1-3). The clinical significance of an ankylosed spine includes reduced mobility and deformity of the trunk; however, more critical importance resides in its underlying susceptibility to unstable fractures3,4). Given their unusual (noncompression type) fracture configuration, preexisting pathologic osseous changes, and severe instability caused by long lever arms, vertebral fractures associated with ASD pose significant diagnostic and therapeutic challenges1,2,5-10). A delay in diagnosis was found to occur in approximately 20% of patients with ASD1,2). Complication rates are as high as 84% in the literature, with a one-year mortality of 32%2). Furthermore, the ankylosed spine remains in ankylosis after fracture treatment, and the underlying susceptibility to further fractures still remains. To date, information is scarce in the literature concerning patients with ASD who have multiple episodes of vertebral fractures11).
Case Report
Case 1
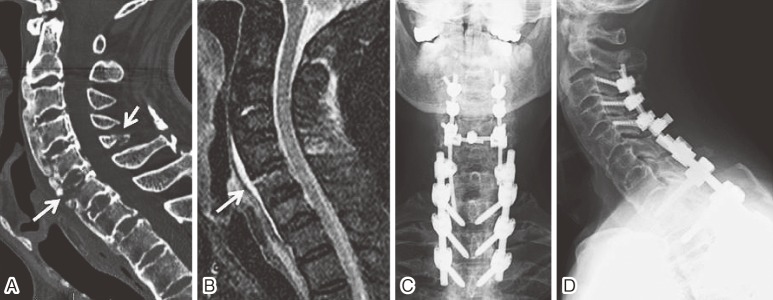
An 83-year-old male was presented to the clinic following a ground-level fall with severe neck pain. Physical examination revealed no motor weakness or sensory disturbance. Cervical computed tomography (CT) scans showed ossification of the anterior longitudinal ligament (ALL), which was fractured along the C6 vertebral body to the C5 spinal process (Fig. 1A). The ossification of ALL was shown to continue from C2 to L4 to form an ankylosed spine, whereas bilateral sacroiliac (SI) joints and facet joints remain unfused, thus indicating DISH. Short T1 inversion recovery (STIR) MR images showed high signal in the C6 vertebra contagious to the prevertebral space; this finding is consistent with hemorrhage in an extension injury (Fig. 1B). The patient was admitted and underwent posterior segmental screw instrumentation and an autologous iliac bone graft from C3 to T3 on the second day after admission (Fig. 1C, 1D). The postoperative course was uneventful.
Figure 1.
(A) A sagittal reconstruction image of the CT scans showing ossification of the ALL, which was fractured along the C6 vertebral body, as part of the discovertebral three-column fracture throughout the C5 spinal process (arrows).
(B) A STIR MR image showing high signal in the C6 vertebra contagious to the prevertebral space; this image is consistent with hemorrhage in an extension injury (arrow).
(C) Anterior-posterior and (D) lateral radiograph status postposterior segmental screw instrumentation and autologous bone graft from C3 to T3 (C3-C5: lateral mass screws; T1-T3: pedicle screws).
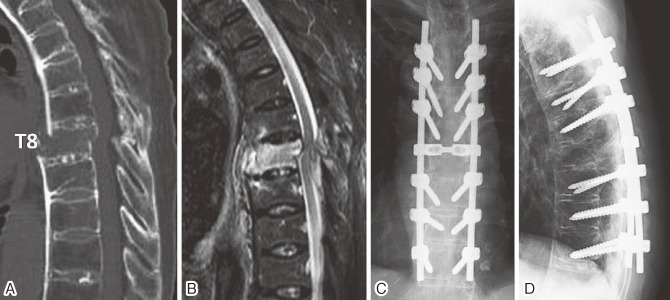
Five years later, the patient (88 years old) slipped from a chair and was brought to the emergency room with severe back pain. Upon physical examination, the patient was neurologically intact. CT scans revealed a three-column fracture of the L1 vertebra (Fig. 2A, 2B). Conservative treatment with a hard brace failed to control his back pain. Percutaneous segmental screw instrumentation was performed from T10 to L4 (Fig. 2C, 2D). CT scans at seven months postoperatively showed the formation of bridging callus over the anterior wall of the L1 vertebral body.
Figure 2.
(A) A sagittal reconstruction image of the CT scans showing the ossification of ALL throughout the thoracolumbar spine (T1 to L4).
(B) A magnified CT scan image of the L1 vertebra showing a fracture line (arrows).
(C) Anterior-posterior and (D) lateral radiograph status postpercutaneous segmental screw instrumentation from T10 to L4.
One year and two months postoperatively, the patient (89 years old) had another fall. CT scans and MR images demonstrated a refracture of the L1 vertebral body. The fracture line was located lower in the vertebral body than the initial fracture. There was no screw loosening or rod breakage. The patient was treated with a hard brace, and the L1 fracture healed.
Case 2
A 76-year-old female who sustained a T8 vertebral fracture after a ground-level fall was transferred to our hospital because of newly developed numbness and weakness in the lower extremities at the 16th day after the injury. Physical examination revealed an incomplete paraplegia (American Spinal Injury Association Impairment Scale C). CT scans showed ankylosis of the spine from C7 to L2 with ossification of ALL and fusion of the facet joints. Furthermore, the right SI joint was also fused, thus indicating AS. There was a three-column vertebral fracture of T8 (Fig. 3A). MR images showed compression of the spinal cord (Fig. 3B). On the second day after the transfer, the patient underwent laminectomy from T7 to T9, posterior segmental screw instrumentation, and an autologous iliac bone graft from T5 to T10 (Fig. 3C, 3D). The patient recovered from paraplegia and was discharged with no assistive devices. Ten months postoperatively, she requested hardware removal because of persistent back pain due to metal irritation. Given that the CT scans showed that the fracture had healed, all the hardware was removed.
Figure 3.
(A) A sagittal image of CT scans showing the ankylosed spine and a displaced fracture of the T8 vertebra.
(B) A STIR MR image showing the compression of the spinal cord at the fracture level.
(C) Anterior-posterior and (D) lateral radiograph status postlaminectomy from T7 to T9, posterior segmental screw instrumentation, and autologous bone graft from T5 to T10.
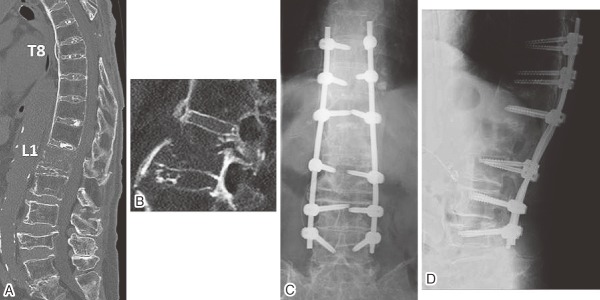
Five years later, the patient (81 years old) fell again and was transferred to our hospital with severe back pain and right inguinal pain. Physical examination disclosed no motor or sensory loss. CT scans revealed a healed T8 fracture postlaminectomy and hardware removal (Fig. 4A). In addition to these fractures, the patient had a three-column extension-type fracture of the L1 vertebra (Fig. 4B). We performed percutaneous segmental screw instrumentation from T10 to L4 (Fig. 4C, 4D). Her back pain improved postoperatively. However, her right inguinal pain remained unchanged. Imaging studies revealed the compression of the right L1 root by the displaced pedicle and lamina. Two weeks postoperatively, we performed revision surgery including L1 laminectomy and L1 right pediclectomy. Her right inguinal pain improved following the surgery. At the one-year follow-up, the patient walked with a cane. X-rays showed no hardware problems.
Figure 4.
(A) A CT scan image showing a healed T8 fracture status postlaminectomy and hardware removal.
(B) A magnified CT scan image showing a three-column extension-type fracture of the L1 vertebra.
(C) Anterior-posterior and (D) lateral radiograph status postpercutaneous segmental screw instrumentation from T10 to L4.
Discussion
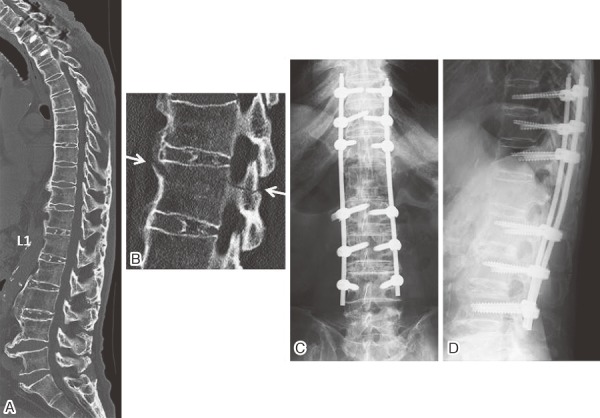
In this report, we presented two patients with ASD who suffered multiple episodes of vertebral fractures. Samartzis et al11) reported an 81-year-old male with AS who also sustained two episodes of vertebral fractures. To the best of our knowledge, there are no other reports of repetitive fractures of the ankylosed spine. The present two cases and the reported case share some clinical features, including an age older than 75 years old and ankylosis of the spine from the cervical spine to the lumbar spine (Table 1). These features may represent risk factors for the repetition of vertebral fractures associated with ASD.
Table 1.
| First episode | Second episode | Third episode | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Diagnosis | Age | Location | Instrumentation | Age | Location | Instrumentation | Age | Location | Treatment | |||
| case 1 | M | DISH (C2-L4) * |
83 | C5-C6 | C3-T2 | 88 | L1 | T11-L3 | 89 | L1 | Brace | ||
| case 2 | F | AS (C7-L2) | 76 | T8 | T6-T10 | 82 | L1 | T11-L3 | |||||
| Reference | M | AS (C2-L4) | 81 | T11-T12 | T8-L2 | 83 | C6-C7, L2-L3 | C3-T3, T8-L5 | |||||
*Parenthesis indicates area of ankylosed spine
In the literature, the mean age at the time of vertebral fracture is 59-62 years old in patients with AS and 68-70 years old in patients with DISH2,7). Although information is lacking in the literature regarding the number of ankylosed segments in patients with vertebral fracture without repetition, a long ankylosed spine (19 segments on average) seems to be a prerequisite for the development of a second fracture in the ankylosed spine.
The present two patients recovered well eventually. By contrast, the case reported by Samartzis et al11) had simultaneous fractures at C6-C7 and L2-L3 at the second episode, and the patient died following the fractures. The devastating outcome for this patient is likely more attributed to “the simultaneous double” nature of the spine fracture rather than “the repetitive” nature, as reported by Yagi et al12).
Repetitive vertebral fractures in patients with ASD may be more common than those reported in the literature. Attention needs to be payed to prevent subsequent vertebral fractures, particularly in patients who are older than 75 years old and have long spinal ankylosis from the cervical spine to the lumbar spine. For the prevention of the second fracture, it is important to be aware that a simple fall can cause fractures of the ankylosed spine. Therefore, fall precautions and fall prevention programs can help. Furthermore, despite the lack of guidelines for the screening and treatment of osteoporosis in ASD, medications such as teriparatide, which has recently been reported to be effective in the treatment of a vertebral fracture with ASD13), may also be beneficial for the prevention of subsequent vertebral fractures.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: Ryunosuke Fukushi, MD; Article drafting, Satoshi Kawaguchi, MD, PhD; Conception and design, Goichi Watanabe, MD, PhD; Data acquisition and analysis, Keiko Horigome, MD, PhD; Article revision, Hideki Yajima, MD; Data acquisition and analysis, Toshihiko Yamashita, MD, PhD; Final approval of the article to be submitted.
References
- 1.Westerveld LA, Verlaan JJ, Oner FC. Spinal fractures in patients with ankylosing spinal disorders: a systematic review of the literature on treatment, neurological status and complications. Eur Spine J. 2009;18(2):145-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caron T, Bransford R, Nguyen Q, et al. Spine fractures in patients with ankylosing spinal disorders. Spine (Phila Pa 1976). 2010;35(11):E458-64. [DOI] [PubMed] [Google Scholar]
- 3.Chaudhary BR, Fehlings MG. Ankylosing spinal disorders--falls, flawed flexibility, and fixations. World Neurosurg. 2015;83(5):724-6. [DOI] [PubMed] [Google Scholar]
- 4.Prieto-Alhambra D, Munoz-Ortego J, De Vries F, et al. Ankylosing spondylitis confers substantially increased risk of clinical spine fractures: a nationwide case-control study. Osteoporos Int. 2015;26(1):85-91. [DOI] [PubMed] [Google Scholar]
- 5.Lukasiewicz AM, Bohl DD, Varthi AG, et al. Spinal Fracture in Patients With Ankylosing Spondylitis: Cohort Definition, Distribution of Injuries, and Hospital Outcomes. Spine (Phila Pa 1976). 2016;41(3):191-6. [DOI] [PubMed] [Google Scholar]
- 6.Choi D. Fractures in Ankylosing Disorders of the Spine: Easy to Miss and High Risk of Deterioration. World Neurosurg. 2015;83(6):1029-31. [DOI] [PubMed] [Google Scholar]
- 7.Westerveld LA, van Bemmel JC, Dhert WJ, et al. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J. 2014;14(5):729-40. [DOI] [PubMed] [Google Scholar]
- 8.Mahajan R, Srivastava A, Patel N, et al. A novel technique for reduction of unreducible lumbar fractures in ankylosing spondylitis. Eur Spine J. 2014;23(7):1568-72. [DOI] [PubMed] [Google Scholar]
- 9.Balling H, Weckbach A. Hyperextension injuries of the thoracolumbar spine in diffuse idiopathic skeletal hyperostosis. Spine (Phila Pa 1976). 2015;40(2):E61-7. [DOI] [PubMed] [Google Scholar]
- 10.Rustagi T, Drazin D, Oner C, et al. Fractures in Spinal Ankylosing Disorders: A Narrative Review of Disease and Injury Types, Treatment Techniques, and Outcomes. J Orthop Trauma. 2017;31 Suppl 4:S57-S74. [DOI] [PubMed] [Google Scholar]
- 11.Samartzis D, Anderson DG, Shen FH. Multiple and simultaneous spine fractures in ankylosing spondylitis: case report. Spine (Phila Pa 1976). 2005;30(23):E711-5. [DOI] [PubMed] [Google Scholar]
- 12.Yagi M, Sato S, Miyake A, et al. Traumatic Death due to Simultaneous Double Spine Fractures in Patient with Ankylosing Spondylitis. Case Rep Orthop. 2015;2015:590935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Matsumoto T, Ando M, Sasaki S. Effective treatment of delayed union of a lumbar vertebral fracture with daily administration of teriparatide in a patient with diffuse idiopathic skeletal hyperostosis. Eur Spine J. 2015;24 Suppl 4:S573-6. [DOI] [PubMed] [Google Scholar]