Abstract
Introduction
Approximately 3% of osteoporotic vertebral fractures develop osteoporotic vertebral collapse (OVC) with neurological deficits, and such patients are recommended to be treated surgically. However, a proximal junctional fracture (PJFr) following surgery for OVC can be a serious concern. Therefore, the aim of this study is to identify the incidence and risk factors of PJFr following fusion surgery for OVC.
Methods
This study retrospectively analyzed registry data collected from facilities belonging to the Japan Association of Spine Surgeons with Ambition (JASA) in 2016. We retrospectively analyzed 403 patients who suffered neurological deficits due to OVC below T10 and underwent corrective surgery; only those followed up for ≥2 years were included. Potential risk factors related to the PJFr and their cut-off values were calculated using multivariate logistic regression analysis and receiver operating characteristic (ROC) analysis.
Results
Sixty-three patients (15.6%) suffered PJFr during the follow-up (mean 45.7 months). In multivariate analysis, the grade of osteoporosis (grade 2, 3: adjusted odds ratio (aOR) 2.92; p=0.001) and lower instrumented vertebra (LIV) level (sacrum: aOR 6.75; p=0.003) were independent factors. ROC analysis demonstrated that lumbar bone mineral density (BMD) was a predictive factor (area under curve: 0.72, p=0.035) with optimal cut-off value of 0.61 g/cm2 (sensitivity, 76.5%; specificity, 58.3%), but that of the hip was not (p=0.228).
Conclusions
PJFr was found in 16% cases within 4 years after surgery; independent risk factors were severe osteoporosis and extended fusion to the sacrum. The lumbar BMD with cut-off value 0.61 g/cm2 may potentially predict PJFr. Our findings can help surgeons select perioperative adjuvant therapy, as well as a surgical strategy to prevent PJFr following surgery.
Keywords: Osteoporosis, vertebral fracture, proximal junctional fracture, corrective surgery, proximal junctional kyphosis
Introduction
Osteoporosis is a disorder characterized by low bone quantity, as well as the deterioration of bone quality, both of which increase the risk of fracture1). The disorder has become a major public health concern due to the high prevalence and high healthcare costs associated with it. Osteoporotic vertebral fracture is the most common osteoporotic fracture, accounting for nearly 50% of all osteoporotic fractures2). In addition, the incidence of osteoporotic vertebral fracture is increasing as the population ages, regardless of ethnicity3). Most cases of osteoporotic vertebral fracture can be managed conservatively; however, approximately 3% develop osteoporotic vertebral collapse (OVC) with neurological deficits, which severely affects not only the activities of daily living, but also the quality of life4,5). Multiple studies have shown that spinal fusion and vertebral column reconstruction using various surgical techniques could improve the neurological deficits from OVC6-10). Thus, it is widely accepted that such patients should be treated surgically to allow patients an early return to daily life activities.
Proximal junctional kyphosis (PJK) due to the proximal junctional fracture (PJFr) is a major concern after corrective surgery for adult spinal deformity (ASD)11,12). Its incidence is about 30% within 2 years11) and osteoporosis severity is a strong risk factor12). In OVC surgery, surgeons need to correct the kyphotic deformity from OVC and fix the spinal column rigidly with multilevel instrumentation6,7). Therefore, PJFr following surgery for OVC can also be a serious concern, in ways similar to surgery for ASD. However, to the best of our knowledge, the potential risk factors, as well as the incidence of PJFr following surgery for OVC, have yet to be fully defined. Based on this, the aim of current study was to identify the incidence and independent risk factors of PJFr, following surgically treated OVC.
Materials and Methods
Study design
This study retrospectively analyzed registry data collected from facilities belonging to the Japan Association of Spine Surgeons with Ambition (JASA) in 2016. The institutional review board of all institutions reviewed and approved this study. We included patients who suffered osteoporotic vertebral fracture below T10 and had neurological deficit due to delayed OVC. Other inclusion criteria were corrective surgery for the neurological deficit, a follow-up of at least 2 years after primary surgery, and an agreement to participate in our study. Patients underwent decompression without fusion surgery, while those in whom perioperative information could not be completely determined were excluded in this study. Thus, 405 patients were registered for this multicenter survey. From this database, two patients were excluded, due to being treated with vertebroplasty without any instrumentation. A final total of 403 patients were enrolled in this study.
The patients with PJFr
In the current study, to assure enough number of the patients for reliable statistical analysis, PJFr was defined to include a fracture of an upper instrumented vertebra and a proximal adjacent vertebra to the instrumented vertebra. PJFr was detected by the senior spine surgeons using plain radiography or computed tomography at the regular check-up after surgery, or when the patients complained of back pain.
Potential risk factors
Data for potential risk factors relating to PJFr were evaluated. Patient factor such as age, sex, patients body mass index (BMI), osteoporosis severity, and the level of the original vertebral fracture, as well as operative factors such as surgical approach, number of fused segments, level of upper instrumented vertebra (UIV), and level of lower instrumented vertebra (LIV) were collected from medical records. Osteoporosis severity was evaluated using preoperative lateral lumbar plain radiography. Classification was applied to all patients using the 4-grade scale as follows: Grade 0: presence of dense vertical and horizontal trabecular bone; Grade I: presence of clear vertical trabecular bone, but unclear horizontal one; Grade II: presence of rough vertical trabecular bone; Grade III: presence of unclear vertical trabecular bone. In addition, preoperative data on bone mineral density (BMD) evaluated by dual-energy x-ray absorptiometry (DXA) from the hip and/or lumbar regions were collected. The operative approach was divided into the following three types: anterior, posterior, and combined. The operative approach, procedure, length of fusion, and indication of surgery were decided according to the individual strategy of the physician's institution.
Clinical outcomes
All patients were evaluated for surgical outcomes before surgery and at the final follow-up, using the Frankel performance grade. To evaluate the severity of paralysis due to OVC, the Frankel performance grade was assessed as follows: Grade A: complete neurological injury; Grade B: preserved sensation only; Grade C: Preserved motor but nonfunctional; Grade D: Preserved motor, functional; Grade E: Normal motor function13).
Statistical analysis
Chi-square tests or Fisher's exact test (as appropriate) for categorical variables, and Mann-Whitney U tests for continuous variables were used to compare patients with and without PJFr on univariate analysis. Additionally, the residual analysis was performed following the chi-square test. The result of residual analysis was described as p < 0.05 when the adjusted |r| of variables was > 1.96, according to the Haberman's method14). To calculate independent predictive factors for PJFr, variables such as age, osteoporosis severity, level of UIV, level of LIV, number of fused segments, and surgical approach were included in the multivariate logistic regression model. In this analysis, patients with PJFr were set as a dependent variable. Adjusted odds ratio (aOR) and 95% confident intervals (CI) of the dependent variables were calculated. Finally, as sub-analysis using the patients with DXA data, the receiver operating characteristic (ROC) curves were plotted to investigate the cut-off values of BMD to predict PJFr. The area under the curve (AUC) and 95% CI were calculated. An AUC of 0.5 indicates chance performance, 0.5 to 0.6 indicates bad predictive ability, 0.6 to 0.7 indicates sufficient predictive ability, 0.7 to 0.8 indicates good predictive ability, and 0.8 to 1.0 indicates excellent predictive ability15). The cut-off value was defined as the point corresponding to the maximum sum of the sensitivity and specificity. All analyses were performed using SPSS computer software (version 23; SPSS, Chicago, IL, USA). A p < 0.05 was considered statistically significant.
Results
Upon assessment of the 402 patients, 63 patients (15.6%) experienced PJFr, 38 patients showed fracture of an UIV, and 25 patients showed proximal adjacent vertebra to the instrumented vertebra within a mean follow-up term of 45.7 months. The mean age of the patients was 73.8 years; 331 patients (82.1%) were women, (Table 1).
Table 1.
Univariate Analysis of Patient Characteristics.
| Overall | PJF (+) | PJF (−) | p-value# | |
|---|---|---|---|---|
| Number of patients | 403 | 63 | 340 | |
| Age | 73.8±7.8 | 74.9±8.1 | 73.6±7.8 | 0.238† |
| Sex | 0.724‡ | |||
| Women | 331 (82.1%) | 53 (84.1%) | 278 (81.8%) | |
| Men | 72 (17.9%) | 10 (15.9%) | 62 (18.2%) | |
| BMI | 22.6±4.4 | 22.5±3.9 | 22.6±4.5 | 0.872† |
| Follow up (months) | 45.7±20.7 | 45.0±20.1 | 45.8±20.8 | 0.772† |
| Osteoporosis grade | 0.019‡ | |||
| 0 | 25 (6.2%) | 2 (3.2%) | 23 (6.8%) | |
| I | 153 (38.1%) | 15 (23.8%) | 138 (40.6%) | <0.05* |
| II | 170 (42.3%) | 37 (58.7%) | 133 (39.1%) | <0.05* |
| III | 53 (13.2%) | 9 (14.3%) | 44 (12.9%) | |
| OVC level | 0.002‡ | |||
| T10 | 16 (4.0%) | 0 (0%) | 16 (4.7%) | |
| T11-L2 | 311 (77.2%) | 42 (66.7%) | 269 (79.1%) | <0.05* |
| L3-L5 | 76 (18.9%) | 21 (33.3%) | 55 (16.2%) | <0.05* |
#: p-value calculated by the comparison between groups with and without PJF
†: t-test, ‡: Chi-square test, *: post-hoc residual analysis
PJF: proximal junctional fracture, BMI: body mass index, OVF: osteoporotic vertebral collapse
Comparison of patient characteristics
There were no significant differences between patients with and without PJFr, mean age (p=0.238), proportion of men and women (p=0.724), BMI (p=0.872), and follow-up period (p=0.772, Table 1). Osteoporosis severity was significantly higher in patients with PJFr than without PJFr (p=0.019); there were significantly more patients without PJFr in grade I (23.8% vs 40.6%, p < 0.05), while patients with PJFr were significantly higher in number in grade II (58.7% vs 39.1%, p < 0.05) upon residual analysis. Likewise, the OVC level showed a significant difference between the two groups (p=0.002). The number of fractures at the thoracolumbar junction level was significantly low and the number of fractures at the lower lumbar level was significantly high in patients with PJFr, compared to that in patients without PJFr (p < 0.05, respectively).
Comparison of surgical factors
Use of the posterior approach had the highest rate in patients both with and without PJFr, and there were no significant differences in surgical approach between the groups (p=0.338, Table 2). Likewise, the number of fused segments showed no significant differences (p=0.312). In terms of the level of instrumented vertebra, UIV levels showed no significant differences between two groups (p=0.128). Meanwhile, LIV levels were significantly different (p=0.004): the patients with PJFr showed a significantly higher number of LIV extended to the sacrum and significantly lower in the thoracolumbar junction (p < 0.05, respectively).
Table 2.
Univariate Analysis of Surgical Factors.
| PJF (+) n=63 |
PJF (−) n=340 |
p-value | |
|---|---|---|---|
| Surgical approach | 0.338‡ | ||
| Anterior | 1 (1.6%) | 18 (5.3%) | |
| Posterior | 58 (92.1%) | 292 (85.9%) | |
| Combined | 4 (6.3%) | 30 (8.8%) | |
| Number of fused segments | 3.7±1.4 | 3.9±1.8 | 0.312† |
| UIV | 0.128‡ | ||
| Thoracic (-T10) | 23 (36.5%) | 172 (50.1%) | |
| Thoracolumbar (T11-L2) | 34 (54.0%) | 149 (43.8%) | |
| Lumbar (T3-L5) | 6 (9.5%) | 21 (6.2%) | |
| LIV | 0.004‡ | ||
| Thoracolumbar (T11-L2) | 22 (34.9%) | 170 (50.0%) | <0.05* |
| Lumbar (T3-L5) | 33 (52.4%) | 155 (45.6%) | |
| Pelvis (S1-) | 8 (12.7%) | 13 (3.8%) | <0.05* |
†: t-test, ‡: Chi-square test, *: post-hoc residual analysis
PJF: proximal junctional fracture, UIV: upper instrumented vertebra, LIV: lower instrumented vertebra
Comparison of clinical outcomes using Frankel grade
Regarding the Frankel grade, in patients with PJFr, one patient (1.6%) deteriorated, 29 patients (46.8%) showed the same grade, and 33 patients (52.4%) improved; while in the group without PJFr, seven patients (2.1%) deteriorated, 156 patients (46.4%) showed the same grade and 175 patients (52.1%) improved. There was no significant difference between two groups (p=0.848, Table 3).
Table 3.
Clinical Outcomes Using the Frankel Classification.
| PJF (+) group, n=63 | PJF (−) group, n=340 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Final FU | Final FU | |||||||||||
| A | B | C | D | E | A | B | C | D | E | |||
| Preoperative | A | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | |
| B | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 3 | 2 | 1 | ||
| C | 0 | 0 | 5 | 23 | 1 | 2 | 2 | 10 | 102 | 15 | ||
| D | 0 | 0 | 1 | 20 | 9 | 0 | 1 | 3 | 115 | 52 | ||
| E | 0 | 0 | 0 | 0 | 4 | 0 | 0 | 0 | 0 | 30 | ||
Darker gray indicates patients who deteriorated in grade in at final follow up.
Middle gray indicates patients with a stable grade at final follow up.
Blighter gray indicates patients improved grade at final follow up.
PJF: proximal junctional fracture, FU: follow up
Risk factors for PJFr
Multivariate logistic regression analysis revealed that the grade of osteoporosis (grade 0 or I: reference, grade II or III: aOR 2.92, p=0.001), LIV levels (thoracolumbar junction: reference, sacrum: aOR 6.75, p=0.003) were significant independent factors for PJFr (Table 4). Age, UIV level, surgical approach, and the number of fused segments were not significant independent factors.
Table 4.
Multivariate Logistic Regression Analysis.
| Variables | Adjusted OR | p-value | 95%CI | |
|---|---|---|---|---|
| Age | 75< | Reference | ||
| 75≥ | 1.16 | 0.614 | 0.66-2.04 | |
| Osteoporosis | Grade 0 or I | Reference | ||
| Grade II or III | 2.92 | 0.001 | 1.54-5.51 | |
| UIV | Thoracic (-T10) | Reference | ||
| TL Junction (T11-L2) | 1.22 | 0.618 | 0.56-2.69 | |
| Lumbar (L3-) | 0.83 | 0.807 | 0.19-3.73 | |
| LIV | TL Junction (T11-L2) | Reference | ||
| Lumbar (L3-L5) | 1.81 | 0.108 | 0.88-3.75 | |
| Sacrum (S1-) | 6.75 | 0.003 | 1.93-23.65 | |
| Approach | Posterior | Reference | ||
| Anterior | 0.30 | 0.268 | 0.03-2.56 | |
| Combined | 0.52 | 0.265 | 0.17-1.63 | |
| Fused segments | 1, 2 | Reference | ||
| 3, 4 | 1.18 | 0.695 | 0.51-2.76 | |
| ≥5 | 0.71 | 0.566 | 0.22-2.28 | |
Dependent variable was set as the patients with proximal junctional fracture.
OR: odds ratio, CI: confidential interval, UIV: upper instrumented vertebra, LIV: lower instrumented vertebra, TL: thoracolumbar
Cut-off value of DXA (sub-analysis)
The result of hip DXA was collected from 151 patients (27 patients with PJFr), while lumbar DXA results were collected from 56 patients (9 patients with PJFr). ROC analysis demonstrated that lumbar BMD was a significant factor with good predictive ability (AUC=0.72, 95%CI: 0.57-0.88, p=0.035, Fig. 1), but that of the hip was not a significant factor (AUC=0.59, 95%CI: 0.49-0.69, p=0.228, Fig. 2). The optimal cut-off value for predicting PJFr after primary surgery was 0.61 g/cm2 lumbar BMD (sensitivity, 76.5%; specificity, 58.3%).
Figure 1.
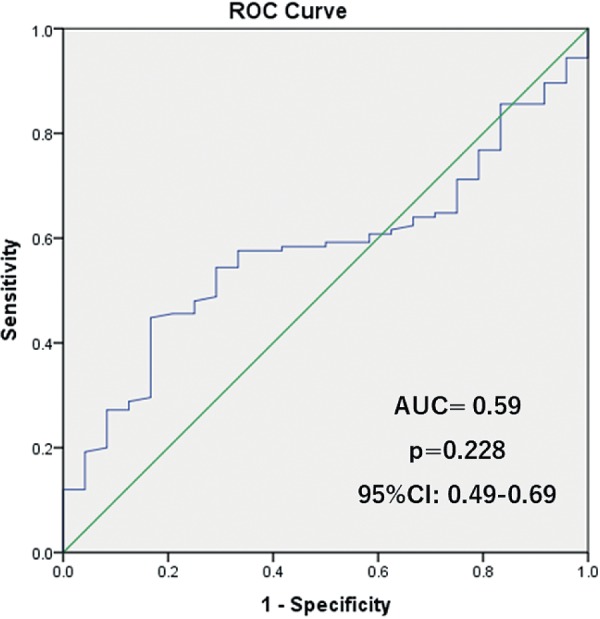
ROC analysis of the PJFr and BMD of femur.
Figure 2.
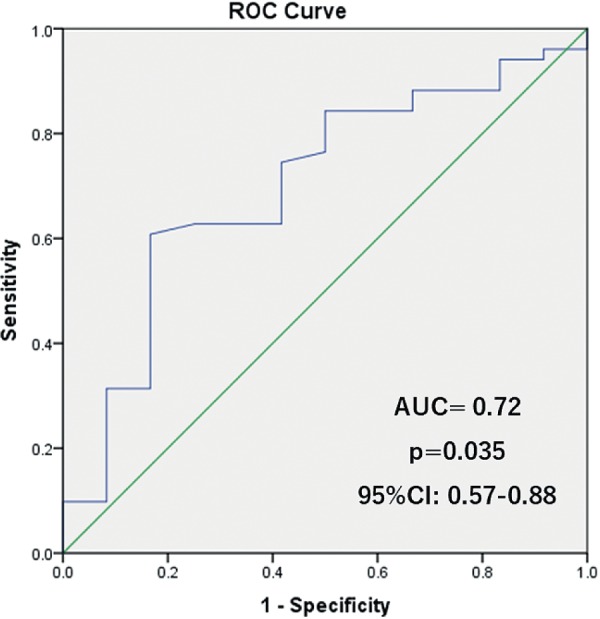
ROC analysis of the PJFr and BMD of lumbar.
Discussion
The current study shows that PJFrs following surgery for delayed neurological deficits due to OVC were found in 15.6% of cases within 45.7 months of follow-up. Independent risk factors for PJFr were severe osteoporosis and fusion to sacrum, but not age, UIV revel, surgical approach, or number of fused segments. Furthermore, we demonstrated that lumbar DXA, but not hip DXA, might predict PJFr.
Osteoporosis is one of the greatest health concerns globally, because of the progression of aging in the world's population. In the United States, it is estimated that more than 9.9 million Americans have osteoporosis and an additional 43.1 million have low bone density16). In addition, about one out of every two Caucasian women will experience a fracture due to osteoporosis at some point in their lifetime17). Furthermore, the cost of osteoporosis management is expected to rise to $25.3 billion by 202518). A similar trend was reported in Europe19), Latin America20), the Middle East21), Africa21), and Asia22). Regarding osteoporotic vertebral fracture, a 50-year-old woman has a 16% chance of experiencing a vertebral fracture over her lifetime23), while a person experiencing one vertebral fracture has a one in four chance of having another fracture over 5 years24). Surprisingly, Taneichi et al. have reported that 30% of all osteoporotic vertebral fracture progress to a collapse, 13% to nonunion, and 3% to OVC with neurological deficits5). Although the incidence of OVC with neurological deficits is relatively low, the huge number of patients with osteoporotic vertebral fractures also leads to a huge number of OVCs. Therefore, elucidating the incidence and risk factors of specific complications following OVC surgery, aids the surgeon in planning the surgical strategy and deciding the preoperative and postoperative adjuvant therapies.
A PJFr that introduces PJK is also a major concern in the surgery for ASD. The risk factors are well-established such as older age, preoperative comorbidities, global imbalance, marked correction, low BMD, posterior approach rigid fixation, and fusion to sacrum12,25). Compared to surgery for ASD, surgery for OVC generally requires relatively short segment fusions. However, all patients with OVC have osteoporosis as a comorbidity, which has been supposed to be a strong risk factor of PJFr. In the current study, the incidence of PJFr was 15.6% within a follow-up term of 45.7 months.
We demonstrated that the result of lumbar DXA may predict PJFr, but that of hip DXA could not. Eckstein et al. reported that the mechanical competence in the elderly is governed by strong regional variation26), which was validated by several another studies25,27). Thus, the regional variation of DXA could be a key for the differences in the ability to predict fracture between hip and lumbar DXAs. However, valid application of our findings to the clinical setting has one caveat: patients with osteoporotic vertebral fracture tend to have one or more old vertebral fractures in their lumbar region, which introduces a falsely high BMD measurement. To overcome this limitation, it is recommended to measure the BMD of the vertebrae that are planned for UIV using a new technique, such as peripheral quantitative computer tomography, that can evaluate the BMD of specific trabecular bone28).
Multiple studies reported that the use of teriparatide is effective for prevention of postoperative adjacent vertebral fractures not only in vertebroplasty29), but also in surgery of OVC30). In addition, Yagi et al. reported that prophylactic teriparatide therapy improved volumetric BMD and fine bone structure at a vertebra adjacent to UIV after long fusion surgery31). Seki et al. demonstrated that the perioperative teriparatide therapy prevented adjacent vertebral fracture of UIV significantly more than bisphosphonates therapy after surgery for ASD32). These studies suggested the potential benefit of teriparatide as adjuvant therapy to prevent PJFr after OVC surgery. However, teriparatide therapy has a high cost, often $50,000 to $100,000 per year33). Therefore, though the current study did not include the data of postoperative teriparatide use, risk factors for PJFr following surgery for OVC and its cut-off value can be important data to select patients needing adjuvant therapy.
Although our results can provide beneficial information for surgeons and patients, this study has some limitations. First, the retrospective design did not allow elimination of certain bias such as selection bias. Important factors such as surgical indication, selection of surgical method, and the postoperative therapy, including the use of medicine for osteoporosis, can be affected by the retrospective nature of this study. In addition, as this study was conducted with data from multiple centers, the surgical procedure, surgical indication, and postsurgical therapy were inconsistent. Secondly, we did not include the global alignment, which is considered as a key factor related to PJK in ASD. Thirdly, though the total number was enough to provide reliable results, the number of patients with DXA data was relatively small. In particular, the small number of lumbar DXA (n=56) might not be representative of the whole sample of 403 patients. Finally, the clinical outcomes did not include the patient-oriented score, which makes it difficult to identify the impact of PJFr on the patient's health-related quality of life. Therefore, large-scale, prospective studies with solid strategies and surgical procedures are important to validate our findings.
Conclusion
PJFr following fusion surgery for OVC was found in 15.6% cases with a mean follow-up term of 45.7 months, while the independent risk factors for PJFr were severe osteoporosis and extended fusion to the sacrum. In addition, the lumbar DXA cut-off value of 0.61 g/cm2 may potentially predict the PJFr, but the hip DXA was not predictive. Our findings could help surgeons to decide the perioperative adjuvant therapy as well as the surgical strategy to prevent PJFr following surgery.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
References
- 1.Sambrook P, Cooper C. Osteoporosis. Lancet. 2006;367(9527):2010-8. [DOI] [PubMed] [Google Scholar]
- 2.Lee YL, Yip KM. The osteoporotic spine. Clin Orthop Relat Res. 1996;(323):91-7. [DOI] [PubMed] [Google Scholar]
- 3.Bow CH, Cheung E, Cheung CL, et al. Ethnic difference of clinical vertebral fracture risk. Osteoporos Int. 2012;23(3):879-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kashii M, Yamazaki R, Yamashita T, et al. Factors affecting postoperative activities of daily living in patients with osteoporotic vertebral collapse with neurological deficits. J Bone Miner Metab. 2015;33(4):422-31. [DOI] [PubMed] [Google Scholar]
- 5.Taneichi H KK, Oguma T, Kokaji M. Risk factor analysis for osteoporotic vertebral collapse and pseudarthrosis. Rinsyo Seikeigeka. 2002;37:437-42. [Google Scholar]
- 6.Kashii M, Yamazaki R, Yamashita T, et al. Surgical treatment for osteoporotic vertebral collapse with neurological deficits: retrospective comparative study of three procedures--anterior surgery versus posterior spinal shorting osteotomy versus posterior spinal fusion using vertebroplasty. Eur Spine J. 2013;22(7):1633-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nakashima H, Imagama S, Yukawa Y, et al. Comparative study of 2 surgical procedures for osteoporotic delayed vertebral collapse: anterior and posterior combined surgery versus posterior spinal fusion with vertebroplasty. Spine (Phila Pa 1976). 201515;40(2):E120-6. [DOI] [PubMed] [Google Scholar]
- 8.Nakajima H, Uchida K, Honjoh K, et al. Surgical treatment of low lumbar osteoporotic vertebral collapse: a single-institution experience. J Neurosurg Spine. 2016;24(1):39-47. [DOI] [PubMed] [Google Scholar]
- 9.Kaneda K, Taneichi H, Abumi K, et al. Anterior decompression and stabilization with the Kaneda device for thoracolumbar burst fractures associated with neurological deficits. J Bone Joint Surg Am. 1997;79(1):69-83. [DOI] [PubMed] [Google Scholar]
- 10.Uchida K, Nakajima H, Yayama T, et al. Vertebroplasty-augmented short-segment posterior fixation of osteoporotic vertebral collapse with neurological deficit in the thoracolumbar spine: comparisons with posterior surgery without vertebroplasty and anterior surgery. J Neurosurg Spine. 2010;13(5):612-21. [DOI] [PubMed] [Google Scholar]
- 11.Scheer JK, Osorio JA, Smith JS, et al. Development of Validated Computer-based Preoperative Predictive Model for Proximal Junction Failure (PJF) or Clinically Significant PJK With 86% Accuracy Based on 510 ASD Patients With 2-year Follow-up. Spine (Phila Pa 1976). 201615;41(22):E1328-E35. [DOI] [PubMed] [Google Scholar]
- 12.Watanabe K, Lenke LG, Bridwell KH, et al. Proximal junctional vertebral fracture in adults after spinal deformity surgery using pedicle screw constructs: analysis of morphological features. Spine (Phila Pa 1976). 201015;35(2):138-45. [DOI] [PubMed] [Google Scholar]
- 13.Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. I. Paraplegia. 1969;7(3):179-92. [DOI] [PubMed] [Google Scholar]
- 14.Haberman SJ. The Analysis of Residuals in Cross-Classified Tables. Biometrics. 1973;29(1):205-20. [Google Scholar]
- 15.Simundic AM. [Diagnostic accuracy]. Acta Med Croatica. 2006;60(1):93-111. [PubMed] [Google Scholar]
- 16.Wright NC, Looker AC, Saag KG, et al. The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cosman F, de Beur SJ, LeBoff MS, et al. Clinician's Guide to Prevention and Treatment of Osteoporosis. Osteoporos Int. 2014;25(10):2359-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burge R, Dawson-Hughes B, Solomon DH, et al. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465-75. [DOI] [PubMed] [Google Scholar]
- 19.Hernlund E, Svedbom A, Ivergard M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013;8:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnell O. The socioeconomic burden of fractures: today and in the 21st century. Am J Med. 1997;103(2A):S20-6. [DOI] [PubMed] [Google Scholar]
- 21.Baddoura R, Hoteit M, El-Hajj Fuleihan G. Osteoporotic fractures, DXA, and fracture risk assessment: meeting future challenges in the Eastern Mediterranean Region. J Clin Densitom. 2011;14(4):384-94. [DOI] [PubMed] [Google Scholar]
- 22.Iki M, Kagamimori S, Kagawa Y, et al. Bone mineral density of the spine, hip and distal forearm in representative samples of the Japanese female population: Japanese Population-Based Osteoporosis (JPOS) Study. Osteoporos Int. 2001;12(7):529-37. [DOI] [PubMed] [Google Scholar]
- 23.Melton LJ, 3rd, Chrischilles EA, Cooper C, et al. Perspective. How many women have osteoporosis? J Bone Miner Res. 1992;7(9):1005-10. [DOI] [PubMed] [Google Scholar]
- 24.Kaptoge S, Armbrecht G, Felsenberg D, et al. When should the doctor order a spine X-ray? Identifying vertebral fractures for osteoporosis care: results from the European Prospective Osteoporosis Study (EPOS). J Bone Miner Res. 2004;19(12):1982-93. [DOI] [PubMed] [Google Scholar]
- 25.Yagi M, King AB, Boachie-Adjei O. Incidence, risk factors, and natural course of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Minimum 5 years of follow-up. Spine (Phila Pa 1976). 2012;37(17):1479-89. [DOI] [PubMed] [Google Scholar]
- 26.Eckstein F, Lochmuller EM, Lill CA, et al. Bone strength at clinically relevant sites displays substantial heterogeneity and is best predicted from site-specific bone densitometry. J Bone Miner Res. 2002;17(1):162-71. [DOI] [PubMed] [Google Scholar]
- 27.Lochmuller EM, Burklein D, Kuhn V, et al. Mechanical strength of the thoracolumbar spine in the elderly: prediction from in situ dual-energy X-ray absorptiometry, quantitative computed tomography (QCT), upper and lower limb peripheral QCT, and quantitative ultrasound. Bone. 2002;31(1):77-84. [DOI] [PubMed] [Google Scholar]
- 28.Baum T, Grabeldinger M, Rath C, et al. Trabecular bone structure analysis of the spine using clinical MDCT: can it predict vertebral bone strength? J Bone Miner Metab. 2014;32(1):56-64. [DOI] [PubMed] [Google Scholar]
- 29.Tseng YY, Su CH, Lui TN, et al. Prospective comparison of the therapeutic effect of teriparatide with that of combined vertebroplasty with antiresorptive agents for the treatment of new-onset adjacent vertebral compression fracture after percutaneous vertebroplasty. Osteoporos Int. 2012;23(5):1613-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kanchiku T, Imajo Y, Suzuki H, et al. Operative methods for delayed paralysis after osteoporotic vertebral fracture. J Orthop Surg (Hong Kong). 2017;25(2):2309499017717194. [DOI] [PubMed] [Google Scholar]
- 31.Yagi M, Ohne H, Konomi T, et al. Teriparatide improves volumetric bone mineral density and fine bone structure in the UIV+1 vertebra, and reduces bone failure type PJK after surgery for adult spinal deformity. Osteoporos Int. 2016;27(12):3495-502. [DOI] [PubMed] [Google Scholar]
- 32.Seki S, Hirano N, Kawaguchi Y, et al. Teriparatide versus low-dose bisphosphonates before and after surgery for adult spinal deformity in female Japanese patients with osteoporosis. Eur Spine J. 2017;26(8):2121-7. [DOI] [PubMed] [Google Scholar]
- 33.Lee TH, Emanuel EJ. Tier 4 drugs and the fraying of the social compact. N Engl J Med. 2008;359(4):333-5. [DOI] [PubMed] [Google Scholar]


