Abstract
Although adult spinal deformity (ASD) has become a global health problem, the classification system and optimal surgical treatment for ASD is yet to be standardized worldwide. A significant part of the population, as high as 10%, in industrialized societies will be aged above 65 years within the next 10 years. Herein, a systematic review of the scientific literature related to the classification and treatment of ASD was conducted wherein historical to the most recent classifications of ASD were reviewed. By discussing the benefits and limitations of the previous classification systems and considering the factors affecting the clinical outcomes of surgical treatment of ASD, this article would like to propose future directions for the development of a new classification system for ASD.
Keywords: Adult spinal deformity, classification, adult scoliosis, review
Introduction
Adult scoliosis is defined as a spinal deformity in a skeletally mature patient with a coronal Cobb angle of more than 10°1,2). Prevalence of deformity in adults is reported between 2% and 32% in the previous reports. One recent paper reported the prevalence to be more than 60% in elderly volunteers3-7). With an increase in the longevity globally, the number of adult patients with deformity is increasing and is higher than that of the adolescent patients with spinal deformity seeking medical treatment8). While a widely accepted classification system is available for adolescent idiopathic scoliosis (AIS)9), the same cannot be extrapolated to adult spinal deformity (ASD). In adults with spinal deformity, treatment approaches are guided by several factors including symptoms of pain and disability, patient's general health, age, bone quality, and patient's expectations unlike the skeletal age and predicted progression of deformity, which is important in AIS management10,11). This study aims to discuss the benefits and limitations of the present classification systems for ASD and propose future directions for the development of globally acceptable classification for ASD.
Classification systems in spine deformity play a crucial role in accurately characterizing specific disorders, in order to guide treatment and decision-making and to form a basis for the uniform reporting of results of treatment that may lead to the evidence based approach to the treatment12). Management strategies for ASD are variable across the globe. This can be partially explained by varied clinical presentation and an abundance of comorbidities affecting the treatment strategy decisions in the elderly; however, it is also due to the lack of evidence based approach to ASD. Development of a new comprehensive classification system is required to establish an evidence-based medical approach to ASD.
Methods
A literature review was conducted through web search on PubMed with the following key words; adult scoliosis, scoliosis prognosis, adult spinal deformity (ASD) classification, ASD complications, spinopelvic parameters, spine sagittal and coronal balance, and scoliosis diagnostic imaging. Scientific papers written in English, from January 1950 to September 2017, describing the classification, surgical complications, and prognosis for ASD, were also included in the review process. PubMed search with the keywords “adult spinal deformity classification” between January 1950 and September 2017, revealed 571 articles, which were thoroughly reviewed by all the authors. Of these, 12 scientific articles describing a new classification system for Adware included in this study2,8,9,12-14,17,18,21,22,32,33). Combination of keywords namely “adult spinal deformity complications” and “scoliosis prognosis” searched on PubMed revealed 422 results, out of which 14 scientific articles describing the complications relevant to the disadvantages of previously described classification systems, were included in this study34-47). Scientific papers on global coronal and sagittal balance and spinopelvic parameters published in the literature, pertinent to the ASD classification, were included in the study. In addition, future directions on how to develop a new comprehensive and globally acceptable ASD classification system are discussed in this article.
History of Adult Spinal Deformity Classification
In 2001, Simmons described two types of deformities seen in adults with spinal deformity, of which one is degenerative lumbar scoliosis with no or minimal rotational deformity (Type I) and the other is degenerative scoliosis often superimposed on a preexisting scoliosis with greater rotational deformity and greater loss of lordosis(Type II)13). Instrumentation and correction techniques differ for these two types of deformities, with shorter instrumentation procedures usually considered for Type I deformity and longer instrumentation with sagittal plane reconstruction necessary for Type II deformity.
In 2005, Aebi et al. classified ASD in three types based on etiology (Table 1)8). The type 1 scoliosis is defined as the primary degenerative scoliosis (“de novo” scoliosis). This curve also termed as “discogenic curve” is basically the result of an asymmetric degenerative change in the intervertebral disc with the consecutive development of a frontal deviation and concomitant rotation with the facet joints on one side as a pivot. Spinal stenosis is more often seen in primary degenerative scoliosis than in secondary degenerated idiopathic curves1). Type 2 scoliosis is defined as progressive idiopathic scoliosis in adult life. Idiopathic curves and curves with other etiology of secondary degeneration present themselves in several forms, depending on the type of treatment given previously14). The degenerated idiopathic scoliosis mostly in the lumbar and/or thoracolumbar spine treated surgically, is quite frequently associated with the increased Modic changes in the adjacent lower segments with lower functional scores and worse Oswestry disability index (ODI) scores after Harrington instrumentation when compared to age and sex matched control group15).
Table 1.
Aebiclassification of Adult Scoliosis8).
| Type | Description | Etiology |
|---|---|---|
| I | Primary degenerative scoliosis (“denovo” scoliosis) | Asymmetric disc and facet joint degeneration |
| II | Progressive idiopathic scoliosis of the lumbar and/or thoracolumbar spine | Idiopathic scoliosis present since adolescence, progression due to mechanical reasons or bony and/or degenerative changes |
| III (a) | Secondary adult scoliosis mostly thoracolumbar or lumbosacral | Secondary to an adjacent thoracic or thoracolumbar curve of idiopathic, neuromuscular or congenital origin Obliquity of pelvis due to leg length discrepancy orhip pathology with secondary spinal curve Lumbosacral transitional anomaly |
| III (b) | Deformity progressing mostly due to bone weakness, for example, osteoporotic fracture with secondary deformity | Metabolic bone disease, osteoporosis |
In 2005, Schwab et al. proposed a radiographic classification system based on the degree of lordosis (L1-S1) and frontal plane obliquity of L3 on standing radiographs (Table 2)2). A total of 98 adult patients with scoliosis with a 2-year minimum follow-up, were included. Curve patterns included thoracic/thoracolumbar/lumbar/thoracic and lumbar (mean Cobb angle 30°, standard deviation 19°). Cobb angle revealed no correlation to the visual analog pain score (VAS) or general health (36-Item Short-Form Health Survey)16). Significant correlation between endplate obliquity of L3, L1-S1 lordosis, and VAS was noted (P< 0.05). Mean pain scores of patients were: type I, VAS = 27.7; type II, VAS = 43.3; and type III, VAS = 47.1 (type I vs. III, P< 0.05). Surgical rates (failed minimum 3-month conservative care, including bracing, physical therapy, and pharmacological treatment) by group were: type I, 0%; type II, 9%; and type III, 22.7% (P=0.002).
Table 2.
Schwab, a Lumbar Classification of Scoliosis in the Adult2).
| Type | Lumbar lordosis | L3 obliquity |
|---|---|---|
| I | >55° | <15° |
| II | 35°-55° | 15°-25° |
| III | <35° | >25° |
The higher parameter determines the type (i.e., lordosis>55° and L3 obliquity 18° is type II).
In 2006, Schwab et al. proposed a new classification system, based on the previously established “high impact clinically significant radiographic parameters” through a prospective study of 947 patients with ASD17). In 2007, the classification system was modified to account for patients with deformity in the sagittal plane alone through the addition of a sixth group18). In addition, a global balance modifier was included (Table 3).
Table 3.
| Type: location of deformity (apical level of major curve OR sagittal plane only) |
| Type I: thoracic only scoliosis (no thoracolumbar or lumbar component) |
| Type II: upper thoracic major, apex T4-T8 (with thoracolumbar or lumbar curve) |
| Type III: lower thoracic major, apex T9-T10 (with thoracolumbar or lumbar curve) |
| Type IV: thoracolumbar major curve, apex T11-L1 (with any other minor curve) |
| Type V: lumbar major curve, apex L2-L4 (with any other minor curve) |
| Type K: Deformity in sagittal plane only |
| Lordosis modifier: Sagittal Cobb angle from T12-S1 |
| A: marked lordosis>40° |
| B: moderate lordosis 0°-40° |
| C: no lordosis Cobb<0° |
| Subluxation modifier: frontal or sagittal plane (anterior or posterior), maximum value |
| 0: no subluxation |
| +: subluxation 1-6mm |
| ++: subluxation>6mm |
| Global balance modifier: sagittal plane C7 offset from posterior superior corner of S1 |
| N: normal (0-4cm) |
| P: positive (4-9.5cm) |
| VP: very positive (>9.5cm) |
Loss of lumbar lordosis and presence of intervertebral subluxation significantly impacted the outcome scores like Scoliosis Research Society-22 (SRS-22) and ODI only in type IV and V curves19,20). As lumbar lordosis is lost, the surgical rate increases significantly (group A, 37%, group C, 51%; P< 0.05). With increasing subluxation (0-++), the operative rate increases from 35 to 52% (P < 0.05). Similarly, as the sagittal balance increases from N to P to VP, the surgical rate significantly increases by 39, 46, and 58%, respectively (N vs. VP; P= 0.02). Loss of lumbar lordosis, lordosis modifiers B and C, and marked subluxation (modifier ++) were associated with more circumferential surgery. Sagittal imbalance was associated with higher rates of dorsal-only surgery. Osteotomies were also used more frequently in cases of sagittal imbalance and increasing loss of lumbar lordosis. Higher rates of fixation to the sacrum were found to be associated with loss of lumbar lordosis (groups B and C) and with increasing positive sagittal balance (P = 0.0006).
In 2006, the Scoliosis Research Society (SRS) introduced a classification system (Table 4) with an intent of accurately categorizing adults with similar deformities, and providing framework that will help in developing evidence based approach to ASD management21). The SRS system was evaluated for interobserver variability through the analysis of 14 expert surgeons' choice of classification of 25 radiographic cases. There was a good interobserver reliability for primary curve type (κ = 0.64), regional sagittal modifier (κ = 0.73), degenerative lumbar modifier (κ = 0.65), and global balance modifier (κ = 0.92). These surgeons were also queried regarding the selection of fusion levels for operative intervention. Although there was good agreement on the selection of the caudal level (κ = 0.77), there was a significantly higher variability in the choice of cephalad level (κ =0.56).
Table 4.
SRS Classification of Adult Spinal Deformity21).
| Primary curve types |
| Single thoracic (ST) |
| Double thoracic (DT) |
| Double major (DM) |
| Triple major (TM) |
| Thoracolumbar (TL) |
| Lumbar “denovo”/idiopathic (L) |
| Primary sagittal plane deformity (SP) |
| Adult spinal deformity modifiers |
| Regional sagittal modifier (include only if outside normal range as listed) |
| • (PT) Proximal thoracic (T2-T5): ≥+20° |
| • (MT) Main thoracic (T5-T12): ≥+50° |
| • (TL) Thoracolumbar (T10-L2): ≥+20° |
| • (L) Lumbar (T12-S1): ≥ −40° |
| Lumbar degenerative modifier (include only if present) |
| • (DDD) 2 disc height and facet arthropathy based on X-ray includelowest involved level between L1 and S1 |
| • (LIS) Listhesis (rotational, lateral antero, retro) ≥3 mm includelowest level between L1 and L5 |
| • (JCT) Junctional L5-S1 curve ≥10° (intersection angle superiorendplates L5 and S1) |
| Global balance modifier (include only if imbalance present) |
| • (SB) Sagittal C7 plumb ≥5 cm anterior or posterior to sacral promontory |
| • (CB) Coronal C7 plumb ≥3 cm right or left of CSVL |
| SRS definition of regions |
| • Thoracic: apex T2-T11-T12 disc |
| • Thoracolumbar: apex T12-L1 |
| • Lumbar: apex L1-L2 disc-L4 |
| Criteria for specific major curve types |
| 1. Thoracic curves |
| • Curve ≥40° |
| • Apical vertebral body lateral to C7 plumbline |
| • T1 rib or clavicle angle ≥10° upper thoracic curves |
| 2. Thoracolumbar and lumbar curves |
| • Curve ≥30° |
| • Apical vertebral body lateral to CSVL |
| 3. Primary sagittal plane deformity |
| • No major coronal curve |
| • One or more regional sagittal measurements (PT, MT, TL, L) outside |
In 2008, Charles Kuntz IV et.al, proposed a classification for ASD based on Neutral Upright Spinal Alignment (NUSA) in asymptomatic volunteers (Table 5)22). Fromthe literature review, 17 angles and displacements were selected to depict the neutral upright coronal and axial spinal alignment, and 21 angles and displacements were selected to depict the neutral upright sagittal spinal alignment. Pooled estimates of the mean and variance were calculated for the angles and displacements from the articles that met the inclusion criteria. Classification of spinal deformity was then developed based on age-dependent NUSA; spinal abnormality; deformity curve location, pattern, magnitude, and flexibility; and global spinal alignment. Based on findings of the literature review, the authors emphasize that, despite a wide variation in the regional curves from occiput to pelvis in asymptomatic volunteers, global spinal alignment is maintained at a narrow range for the preservation of horizontal gaze and balance of the spine over pelvis and femoral heads.
Table 5.
CKIV Classification of ASD22).
| Patient age (yr) |
|---|
| Infantile 0-2 |
| Juvenile 3-9 |
| Adolescent 10-18 |
| Adult 19-60 |
| Geriatric>60 |
| Spinal abnormality |
| Scoliotic, kyphotic, lordotic, scoliokyphotic, scoliolordotic deformity curves |
| Major structural deformity curve standing deformity curve with greatest deviation from age-appropriate NUSA for 98.5% of asymptomatic population (a spinal deformity has only one major structural deformity curve) |
| Scoliotic deformity curves |
| Scoliotic major structural deformity curve>age-appropriate NUSA for 98.5% of the population |
| Minor structural scoliotic curves remain>25 degrees on side-bending radiographs |
| Scoliotic curves named for curve apex in spinal zones |
| Occipitocervical (OC) O-C2 |
| Cervical (C) C2/C3 disc-C6/C7 disc |
| Cervicothoracic (CT) C7-T1 |
| Proximal thoracic (PT) T1/T2 disc-T5 |
| Main thoracic (MT) T5/T6 disc-T11/T12 disc |
| Thoracolumbar (TL) T12-L1 |
| Lumbar (L) L1/L2 disc-L4/L5 disc |
| Lumbosacral (LS) L5-S1 (remain>10 degrees on side-bending radiographs) |
| Kyphotic and lordotic deformity curves |
| Kyphotic major structural deformity curve>age-appropriate NUSA mean+2.5 SD (98.5% of population) |
| Lordotic major structural deformity curve<age-appropriate NUSA mean−2.5 SD (98.5% of population) |
| Minor structural kyphotic curves remain>adult NUSA mean+1 SD on extension radiographs |
| Minor structural lordotic curves remain<adult NUSA mean−1 SD on flexion radiographs |
| Kyphotic and lordotic curves named for Sagittal angle in spinal zones |
| Occipitocervical (OC) O-C2 |
| Cervical (C) C2-C7 |
| Cervicothoracic (CT) C6-T2 |
| Proximal thoracic (PT) T1-T5 |
| Main thoracic (MT) T4-T12 |
| Thoracolumbar (TL) T10-L2 |
| Lumbar (L) L1-L5 |
| Lumbosacral (LS) L4-S1 |
| Scoliokyphotic and scoliolordotic deformity curves |
| Structural scoliotic curve+structural kyphoticcurve in the same spinal zone |
| Structural scoliotic curve+structurallordotic curve in the same spinal zone |
| Global spinal alignment, horizontal gaze, balance |
| Coronal imbalance (IPA)>age-appropriate NUSA mean+2.5 SD |
| Sagittal imbalance (CBVA)>or<age-appropriate NUSA mean±2.5 SD |
| Spinal balance, balance |
| ±coronal imbalance (C7-S1 CVA)>or<age-appropriate NUSA mean 2.5 SD |
| ±sagittal imbalance (C7-S1 SVA)>or<age-appropriate NUSA mean 2.5 SD |
| Pelvic alignment, neutral |
| Coronal rotation (PO)>adult NUSA mean+2.5 SD |
| Sagittal rotation (PT)>or<adult NUSA mean±2.5 SD |
aNUSA, neutral upright spinal alignment; SD, standard deviation; IPA, interpupillary angle; CBVA, chin-brow to vertical angle; CVA, coronal vertical axis; SVA, sagittalvertical axis; PO, pelvic obliquity; PT, pelvic tilt
bSpinal deformity is classified based on the patient age; spinal abnormality; deformity curve location, pattern, magnitude, and flexibility; and global spinal alignment.
Standard imaging for ASD comprises 36” full-cassette standing anteroposterior (AP) and lateral free-standing radiographs, which include visualization from the external auditory canal to the femoral heads. Cobb's angle, C7 plumb line, central sacral vertical line (CSVL), apical vertebral translation, and apical vertebral rotation (AVR)23) are important parameters on AP radiograph (Fig. 1). Classical parameters can be measured on a lateral X-ray, such as thoracic kyphosis and LL; different plumb lines and offsets have been described on lateral projection to evaluate the global spinal alignment (Fig. 2, 3)24-26).
Figure 1.
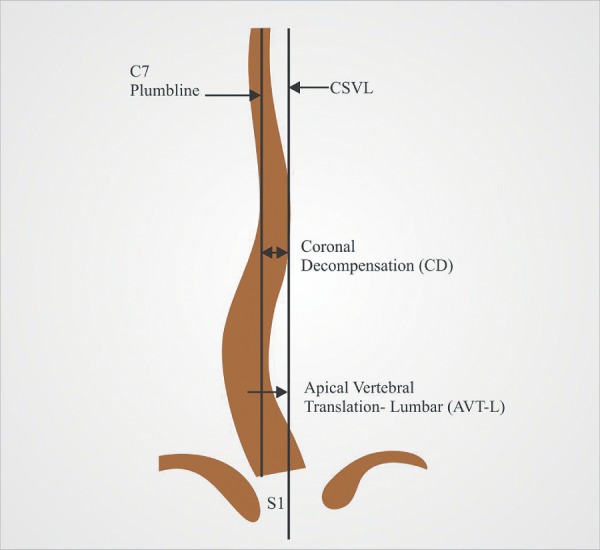
Coronal spinal radiographic parameters.
C7 plumb line is a vertical reference line from center of C7 vertebra.
Central sacral vertebral line is a vertical reference line drawn through the center of S1 endplate.
Coronal decompensation is the distance between C7 plumb line and CSVL.
Figure 2.
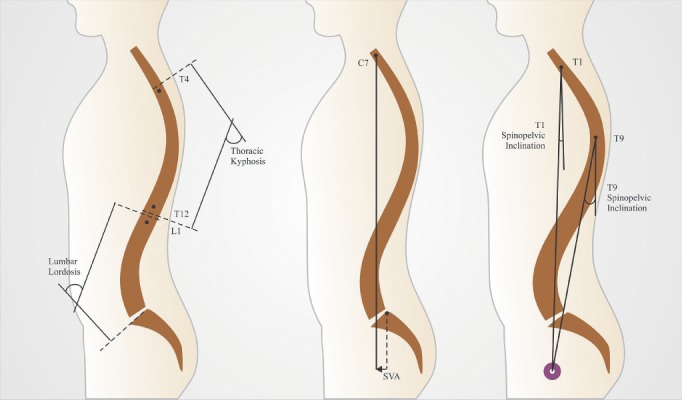
Sagittal spinal radiographic parameters.
Left: Thoracic Kyphosis measured from superior endplate of T4 to inferior endplate of T12 and lumbar lordosis measured from superior endplate of T12 to superior endplate of S1.
Center: SVA defined as horizontal offset from center of C7 vertebral body to posterosuperior corner of S1.
Right: T1 and T9 spino-pelvic angle, defined as an angle between the vertical plumb line and line joining the hip axis to the center of T1 or T9 vertebral body.
Figure 3.
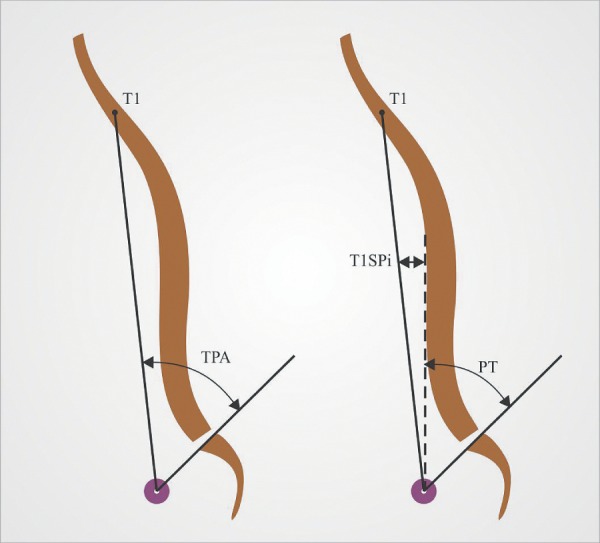
T1 pelvic angle (TPA).
TPA is defined as an angle between the line joining HA to the center of T1 vertebral body and the line joining HA to the center of sacral end plate.
Three main pelvic sagittal parameters have been described by Duval-Beaupere et al. namely pelvic incidence (PI), Pelvic tilt (PT), and sacral slope (SS; Fig. 4)27,28). Pelvic incidence is a relatively constant morphological parameter with slight changes throughout adulthood, in a subject; however, recent studies have reported that PI does change with age, specifically in females29). According to this study, birth experience could be one of the reasons for higher PI in females aged above 40 years. As PI increases, lumbar lordosis must increase in proportion to maintain the sagittal vertical balance. PT and SS are posturally dependent values, which change according to the pelvic rotation over hip axis. These three pelvic parameters are interrelated by the equation PI=PT+SS.
Figure 4.
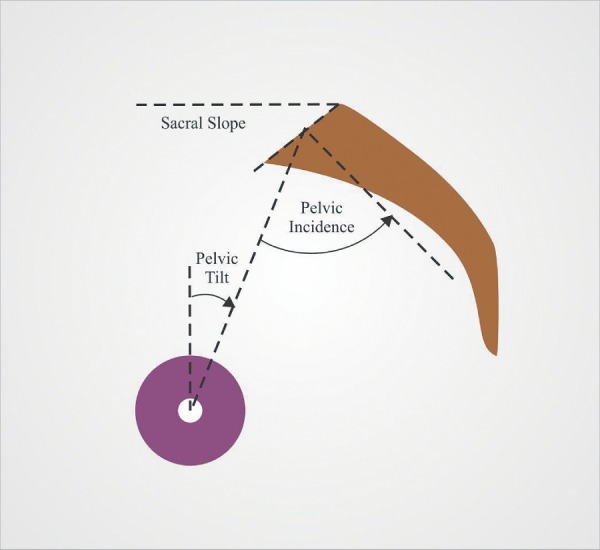
Pelvic parameters.
Sacral slope defined as an angle between the horizontal reference line and sacral slope.
Pelvic tilt defined as an angle between the vertical reference line through the hip axis and line joining the center of sacral endplate to hip axis.
Pelvic incidence defined as an angle between the line joining hip axis to the center of sacral endplate and perpendicular to the sacral endplate from its center.
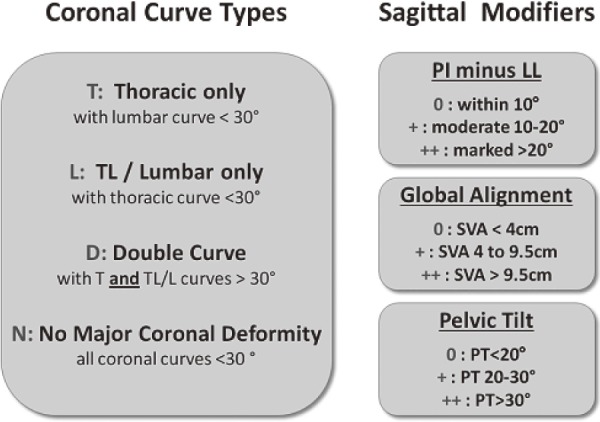
Considering observations in recent studies, the pelvic parameters have substantial correlation with health-related quality of life measures30-32); in 2012, the SRS Adult Deformity Committee revised a previously published classification to include the pelvic parameters33). The deformity is described by its main coronal curve pattern and its amplitude, using Cobb angle and three modifiers are applied: the relationship of PI and LL (PI-LL), pelvic tilt (PT), and sagittal vertical axis (SVA; Table 6).
Table 6.
SRS-Schwab Adult Spine Deformity Classification26).
Nine readers graded 21 premarked cases twice each, approximately 1 week apart and inter- and intrarater variability and agreement were determined for the curve type and each modifier separately. Interrater kappa for curve type was 0.80 and 0.87 for the two readings, respectively, with modifier kappas of 0.75 and 0.86, 0.97 and 0.98, and 0.96 and 0.96 for pelvic incidence minus lumbar lordosis (PI-LL), pelvic tilt (PT), and sagittal vertical axis (SVA), respectively. By the second reading, the curve type was identified by all readers consistently in 66.7%, PI-LL in 71.4%, PT in 95.2%, and SVA in 90.5% of cases. Intrarater kappa averaged 0.94 for curve type, 0.88 for PI-LL, 0.97 for PT, and 0.97 for SVA across all readers.
Benefits and Limitations of Previous Classification Systems
For several years, patients with ASD were treated conservatively due to high risk of major surgery considering their advanced age, lack of powerful instrumentation tools, and poor bone quality for a major corrective spinal surgery34,35). Progress in the surgical techniques and technology, supported by progress in anesthesia for spine surgery and diagnostic imaging has helped in advancement of surgical treatment for ASD patients. Even though the treatment protocols for ASD patients have evolved in the last two decades, the ongoing efforts to develop a widely accepted adult deformity classification system are testament to the difficulty and clinical variability that are inherent in treating the patient with ASD36).
The Aebi classification is uniquely helpful in understanding the natural history of adult deformity due to its etiological foundation8). This classification provides an alternate insight into adult/geriatric spinal deformity; however, it lacks in guiding surgical treatment of ASD. Frank J. Schwab and SRS have done a good amount of work on adult spinal deformity classification in the last decade. High impact clinically significant radiographic parameters, correlating with patient reported pain scores were used in the Schwab classification17). Furthermore, the reported surgical outcomes were closely related to the aforementioned radiographic parameters. The SRS classification system made a significant advancement in the classification of ASD by including coronal and sagittal plane deformity as well as global spinal alignment21). The advantage of SRS-Schwab classification33) is that it took spinopelvic parameters into account, which were not considered previously. All the modifiers described in SRS-Schwab classification system strongly correlate to the HRQoL scores30-32).
Despite the fact that present classification systems help in understanding the clinical impact of various radiographic parameters and their significance in guiding treatment protocols, a multitude of variables such as clinical comorbid conditions, patient's age, symptoms like claudication and radicular pain, osteoporosis, obesity, smoking are not considered in planning treatment for patients with ASD. Higher complication rates in ASD surgery are known to be associated with older age, higher American Society of Anesthesiologists (ASA) grades, several comorbidities, and higher number of three-column osteotomies, all of which are important variables to be considered in ASDclassification37,38).
The SRS-Schwab classification provides framework for defining spinopelvic malalignment and realignment targets for surgeons, using global spinal balance and spinopelvic parameters. Unfortunately, even when the ideal targets of radiological parameters as described in the SRS-Schwab classification are achieved, the rate of complications like proximal junctional failure (PJF) and revision surgery for the same, is higher in patients with significantly greater baseline deformity, and thus undergo greater correction during surgery39). Kim et al. found that patients who develop PJF had significantly greater correction in the SVA and greater postoperative LL40). It was presumed that, the ASD should be overcorrected to negate the effects of ongoing degeneration in the elderly; however, with time, several studies have revealed that, older age and overcorrection of SVA surgically are independent risk factors for proximal junctional kyphosis (PJK) and revision surgery41-44). Nevertheless, none of the present classification system considers patient's age and age specific alignment goals in establishing treatment guidelines.
Complication rates in ASD surgery are high. Various studies evaluating mortality and morbidity after these procedures, have reported complication rates ranging from 25 to 80%45,46). In a prospective multicenter assessment of perioperative and minimum 2-year postoperative complication rates associated with ASD surgery, Smith et al. identified substantially higher complication rate in 291 ASD patients who completed minimum 2-year follow up37). Overall, 469 complications (207 minor; 262 major) were documented, with 203 patients (69.8%) affected. Table 7 summarizes the perioperative and delayed complications reported in this multicenter study. Most common categories of complications were implant related, radiographic, and neurological. Most common implant and radiographic complications were rod breakage and PJK, respectively37). Higher complication rates were associated with older age (P= 0.009), greater body mass index (P≤ 0.031), increased comorbidities (P≤ 0.007), previous spine fusion (P= 0.029), and three-column osteotomies (P= 0.036). A secondary analysis of the data obtained from Scoli-RISK 1 study47) for predictors of health related quality of life after complex ASD surgery revealed old age, higher ASA grade, larger preoperative Cobb angle, higher number of three-column osteotomies, and the occurrence of both neurological and non-neurologic complications as factors predictive of lower 2-year HRQoL scores36). Systematic review of 3299 patients from 49 articles in available literature from 1950 to 2010, on ASD surgery outcomes and complications by Yadla et al., reported greater than 40% incidence of perioperative adverse events and 13% risk of pseudoarthrosis after ASD surgery46). Mortality and morbidity study after ASD surgery in patients older than 75 years revealed an overall perioperative complication rate of 62% with older age increasing the likelihood of complication45). Patients in this age group with a history of hypertension were 10 times more likely to develop major perioperative complication. Presently used classification systems based on global balance, regional deformity patterns, and pelvic parameters do not consider these variables associated with higher rate of complications while selecting patients for surgical intervention. These variables are essential in the classification system as some of these complications lead to unacceptable patient impairment and disability.
Table 7.
Rate of Complications in 291 Patients Surgically Treated for ASD39).
| Complication category | Minor/Major Complications (%) | ||
|---|---|---|---|
| Period (<6 weeks) | Delayed (>6 weeks) | Total | |
| Implant | 3/8 (3.8) | 11/59 (24.1) | 14/67 (27.8) |
| Radiographic | 4/10 (4.8) | 25/42 (23.0) | 29/52 (27.8) |
| Neurological | 21/24 (15.5) | 16/20 (12.4) | 37/44 (27.8) |
| Operative | 41/32 (25.1) | 0/1 (0.3) | 41/33 (25.4) |
| Cardiopulmonary | 31/20 (17.5) | 1/3 (1.4) | 32/33 (18.9) |
| Infection | 11/20 (10.7) | 5/7 (4.1) | 16/27 (14.8) |
| Gastrointestinal | 24/1 (8.6) | 0/0 (0) | 24/1 (8.6) |
| Wound (excluding infection) | 3/7 (3.4) | 0/5 (1.7) | 3/12 (5.2) |
| Vascular | 4/0 (1.4) | 1/0 (0.3) | 5/0 (1.7) |
| Musculoskeletal | 0/0 (0) | 3/0 (1.0) | 3/0 (1.0) |
| Renal | 1/2 (1.0) | 0/0 (0) | 2/1 (1.0) |
| Other | 2/1 (1.0) | 0/0 (0) | 2/1 (1.0) |
| Total (minor/major) | 270 (145/125) | 199 (62/137) | 469 (207/262) |
| Mean no. of complications/patient (minor/major) | 0.93 (0.50/0.43) | 0.68 (0.21/0.47) | 1.61 (0.71/0.90) |
| Number of patients affected | 152 (52.2) | 124 (42.6) | 203 (69.8) |
Future Directions to Establish a New Classification of ASD
Recent studies have found that normative values for both sagittal alignment and HRQoL scores vary with age29,48). Recently, a scientific paper from Japan describes normative data for parameters of sagittal spinal alignment in different age groups in healthy individuals29). This study included 626 asymptomatic volunteers, with minimum 50 subjects of each gender and each decade, i.e., from the 3rd to the 8th decade of life. According to them, advancing age caused an increase in PT and SVA, and a decrease in LL and thoracic kyphosis. A remarkable change in the spinopelvic sagittal alignment was seen from 7th decade to 8th decade. Incorporating this natural history of sagittal spinopelvic alignment in surgical planning of ASD patients is gaining immense importance as more and more patients of ASD are treated surgically. This has led to the development of concept of age-adjusted alignment goals in ASD patients49).
These studies report that, applying the same and strict alignment targets for all patients without considering age, clinical comorbidities, and trying to create a radiographically perfect looking spine in the elderly is doomed to fail in the long run. Age specific alignment goals will be critical in establishing the future ASD classification systems, with realistic radiographic realignment targets, for caring physicians.
Incorporating patient and surgical characteristics like older age, higher ASA grade, clinical comorbid conditions, obesity, larger preoperative Cobb angle, and requirement of increasing three-column osteotomies for ideal radiographic alignment that predict poorer outcomes after surgery into future classification systems, may allow the surgeons to target these specific variables to improve patient outcomes after ASD surgery. The Seattle spine team approach for adult spine deformity surgery has described three-pronged approach aimed to reduce perioperative complication rates and enhance patient safety in patients undergoing complex spinal reconstructions for ASD50,51). This group reported on the dual-attending surgeon approach, a live multidisciplinary preoperative screening conference, and the intraoperative protocol for the management of coagulopathy to mitigate perioperative complications in ASD surgery. Complication rates were significantly lower (16% vs. 52%; p<0.001) after the introduction of Seattle spine team approach in surgical management of ASD patients. Development of risk mitigating approaches, like Seattle spine team approach and sliding scale for selection for appropriate surgical procedure, after considering particular patients' overall ability to tolerate the level of morbidity of a surgical intervention will be effective in reducing the perioperative complication rates in ASD surgery50,51).
Furthermore, dividing patients according to the most preferred and beneficial treatment approach will help in establishing universal treatment guidelines for ASD management. A comprehensive classification, which considers variables discussed previously before categorizing patients into simple focal decompression, limited fusion, complete long fusion, or conservative management will have global applicability.
Conclusion
Last two decades have seen immense advancement in the classification and treatment approaches of ASD; however, the globally acceptable treatment guidelines with minimum possible complication rates for ASD surgery are not established. A comprehensive classification of ASD, which not only considers radiographic characteristics of ASD but also incorporates patient's symptoms like radicular pain, claudication, back pain, and clinical comorbid conditions like poor bone quality, obesity, smoking, and myriad of chronic medical conditions, which play a role in formulating the treatment strategy in this elderly population, will have a global appeal. Furthermore, patients should be divided into categories of simple focal decompression, limited fusion, complete long fusion, or conservative management.
Disclaimer: Manabu Ito is the Editor of Spine Surgery and Related Research and on the journal's Editorial Committee. He was not involved in the editorial evaluation or decision to accept this article for publication.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Author Contributions: Laxmikant Dagdia wrote and prepared the manuscript, and all the authors contributed in the preparation of manuscript. Manabu Ito revealed the primary idea and concepts to prepare the review article on the required topic. All authors have read, reviewed, and approved the article.
References
- 1.Aebi M. Correction of degenerative scoliosis of the lumbar spine. A preliminary report. ClinOrthopRelat Res. 1988 Jul;(232):80-6. [PubMed] [Google Scholar]
- 2.Schwab F, Benchick el-Fegoun A, Gamez L, et al. Lumbar classification of scoliosis in the adult patient: Preliminary approach. Spine (Phila Pa 1976). 2005;30(14):1670-3. [DOI] [PubMed] [Google Scholar]
- 3.Carter OD, Haynes SG. Prevalence rates for scoliosis in US adults: results from the first National Health and Nutrition Examination Survey. Int J Epidemiol. 1987;16(4):537-44. [DOI] [PubMed] [Google Scholar]
- 4.Perennou D, Marcelli C, Herisson C. Adult lumbar scoliosis: Epidemiologic aspects in a low-back pain population. Spine (Phila Pa 1976). 1994;19(2):123-8. [DOI] [PubMed] [Google Scholar]
- 5.Robin GC, Span Y, Steinberg R, et al. Scoliosis in the elderly: a follow-up study. Spine (Phila Pa 1976). 1982;7(4):355-9. [DOI] [PubMed] [Google Scholar]
- 6.Francis RS. Scoliosis screening of 3,000 college-aged women. The Utah Study-Phase 2. PhysTher. 1988;68(10):1513-6. [PubMed] [Google Scholar]
- 7.Schwab F, Dubey A, Gamez L, et al. Adult scoliosis. Prevalence, SF-36, and nutritional parameters in an elderly volunteer population. Spine (Phila Pa 1976). 2005;30(9):1082-5. [DOI] [PubMed] [Google Scholar]
- 8.Aebi M. The adult scoliosis. Eur Spine J. 2005;14(10):925-48. [DOI] [PubMed] [Google Scholar]
- 9.Lenke L, Edwards C, Bridwell K. The Lenke classification of adolescent Idiopathic scoliosis: How it organizes curve patterns as a template to perform selective fusions of the spine. Spine (Phila Pa 1976). 2003;28(20):S199-207. [DOI] [PubMed] [Google Scholar]
- 10.Albert TJ, Purtill J, Mesa J, et al. Study design: health outcome assessment before and after adult deformity surgery. A prospective study. Spine (Phila Pa 1976). 1995;20(18):2002-4; discussion p2005 [DOI] [PubMed] [Google Scholar]
- 11.Deyo RA, Cherkin DC, Loeser JD, et al Morbidity and mortality in association with operations on the lumbar spine. The influence of age, diagnosis, and procedure. J Bone Joint Surg Am. 1992;74(4):536-43. [PubMed] [Google Scholar]
- 12.Garbuz DS, Masri BS, Esdaile J, et al. Classification systems in orthopedics. J Am Acad Orthop Surg. 2002;10(4):290-7. [DOI] [PubMed] [Google Scholar]
- 13.Simmons ED. Surgical treatment of patients with lumbar spinal stenosis with associated scoliosis. Clin Orthop Relat Res. 2001;(384):45-53. [DOI] [PubMed] [Google Scholar]
- 14.Ogilvie JW (1992) Adult scoliosis: evaluation and nonsurgical treatment. Instr Course Lect. 1992;41:251-5. [PubMed] [Google Scholar]
- 15.Akazawa T, Kotoni T, Sakuma T, et al. Modic changes and disc degeneration of non-fused segments 27 to 45 years after Harrington instrumentation for adolescent idiopathic scoliosis: comparison to healthy controls. Spine (Phila Pa 1976). 2017. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Grevitt M, Khazim R, Webb J, et al. The short form 36 health survey questionnaire in spine surgery. J Bone Joint Surg Br. 1997;79(1):48-52. [DOI] [PubMed] [Google Scholar]
- 17.Schwab F, Farcy J, Bridwell K, et al. A clinical impact classification of scoliosis in the adult. Spine (Phila Pa 1976). 2006;31(18):2109-14. [DOI] [PubMed] [Google Scholar]
- 18.Schwab F, Lafage V, Farcy J, et al. Surgical rates and operative outcome analysis in thoracolumbar and lumbar major adult scoliosis, Application of the new adult deformity classification system Spine (Phila Pa 1976). 2007;32(24):2723-30. [DOI] [PubMed] [Google Scholar]
- 19.Bridwell K, Cats-BarilW, Harrast J, et al. The validity of the SRS-22 instrument in an adult spinal deformity population compared with the Oswestry and SF-12: a study of response distribution, concurrent validity, internal consistency, and reliability. Spine (Phila Pa 1976). 2005;30(4):455-61. [DOI] [PubMed] [Google Scholar]
- 20.Fairbank J, Pynsent P. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25(22):2940-52. [DOI] [PubMed] [Google Scholar]
- 21.Lowe T, Berven SH, Schwab FJ, et al. The SRS classification for adult spinal deformity. Building on the King/Moe and Lenke classification systems. Spine (Phila Pa 1976). 2006;31(19 Suppl):S119-25. [DOI] [PubMed] [Google Scholar]
- 22.Kuntz C 4th, Shaffrey C, Ondra S, et al. Spine deformity: a new classification derived from neutral upright spinal alignment measurements in asymptomatic juvenile, adolescent, adult, and geriatric individuals. Neurosurgery. 2008;63(3 Suppl):25-39. [DOI] [PubMed] [Google Scholar]
- 23.Nash CL Jr, Moe JH. A study of vertebral rotation. J Bone Joint Surg Am. 1969;51(2):223-9. [PubMed] [Google Scholar]
- 24.Lafage V, Schwab F, Patel A, et al. Pelvic tilt and truncal inclination: two key radiographic parameters in the setting of adults with spinal deformity. Spine (Phila Pa 1976). 2009;34:E599-606. [DOI] [PubMed] [Google Scholar]
- 25.Lafage V, Schwab F, Skalli W, et al. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976). 2008;33(14):1572-8. [DOI] [PubMed] [Google Scholar]
- 26.Protopsaltis TS, Schwab FJ, Bronsard N, et al. The t1 pelvic angle, a novel radiographic measure of global sagittal deformity, accounts for both spinal inclination and pelvic tilt and correlate with health-related quality of life. J Bone Joint Surg Am. 2014;96(19):1631-40. [DOI] [PubMed] [Google Scholar]
- 27.Duval-Beaupere G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng. 1992;20(4):451-62. [DOI] [PubMed] [Google Scholar]
- 28.Legaye J, Duval-Beaupere G, Hecquet J, et al. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J. 1998;7(2):99-103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yukawa Y, Kato F, Suda K, et al. Normative data for parameters of sagittal spinal alignment in healthy subjects: an analysis of gender specific differences and changes with aging in 626 asymptomatic individuals. Eur Spine J. 2016. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 30.Glassman SD, Bridwell K, Dimar JR, et al. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 2005;30(18):2024-9. [DOI] [PubMed] [Google Scholar]
- 31.Kim YJ, Bridwell KH, Lance LG, et al. An analysis of sagittal spinal alignment following long adult lumbar instrumentation and fusion to L5 or S1: can we predict ideal lumbar lordosis? Spine (Phila Pa 1976). 2006;31(20):2343-52. [DOI] [PubMed] [Google Scholar]
- 32.Schwab FJ, Smith VA, Biserni M, et al. Adult scoliosis: a quantitative radiographic and clinical analysis. Spine (Phila Pa 1976). 2002;27(4):387-92. [DOI] [PubMed] [Google Scholar]
- 33.Schwab F, Ungar B, Blondel B, et al. SRS-Schwab adult spinal deformity classification: a validation study. Spine. 2012;37(12):1077-82. [DOI] [PubMed] [Google Scholar]
- 34.Ascani E, Bartolozzi P, Logroscino CA, et al. Natural history of untreated idiopathic scoliosis after skeletal maturity. Spine (Phila Pa 1976). 1986;11(8):784-9. [DOI] [PubMed] [Google Scholar]
- 35.Briard JL, Jegou D, Cauchoix J. Adult lumbar scoliosis. Spine (Phila Pa 1976). 1979;4(6):526-32. [DOI] [PubMed] [Google Scholar]
- 36.Bridwell KH, Berven S, Edwards C 2nd, et al. The problems and limitations of applying evidence-based medicine to primary surgical treatment of adult spinal deformity. Spine (Phila Pa 1976). 2007;32(19 Suppl):S135-9. [DOI] [PubMed] [Google Scholar]
- 37.Smith JS KE, Virginie L, Shaffrey CI, et al. International Spine Study Group. Prospective multicenter assessment of perioperative and minimum two-year postoperative complication rates associated with adult spinal deformity surgery. J Neurosurg Spine. 2016;25(1):1-14. [DOI] [PubMed] [Google Scholar]
- 38.Carreon LY, Glassman SD, Shaffrey CI, et al. Predictors of health-related quality-of-life after complex adult spinal deformity surgery: a Scoli-RISK-1 secondary analysis. Spine Deform. 2017;5(2):139-44. [DOI] [PubMed] [Google Scholar]
- 39.Yagi M, Akilah KB, Boachie-Adjei O. Incidence, risk factors and classification of proximal junctional kyphosis: surgical outcomes review of adult idiopathic scoliosis. Spine (Phila Pa 1976). 2011;36(1):E60-8. [DOI] [PubMed] [Google Scholar]
- 40.Kim HJ, Bridwell KH, Lenke LG, et al. Patients with proximal junctional kyphosis requiring revision surgery have higher postoperative lumbar lordosis and larger sagittal balance corrections. Spine (Phila Pa 1976). 2014;39(9):E576-80. [DOI] [PubMed] [Google Scholar]
- 41.Kim YJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis in adult spinal deformity after segmental posterior spinal instrumentation and fusion: minimum five-year follow-up. Spine (Phila Pa 1976). 2008;33(20):2179-84. [DOI] [PubMed] [Google Scholar]
- 42.LauD, Clark AJ, Scheer JK, et al. Proximal junctional kyphosis and failure following spinal deformity surgery: a systematic review of the literature as a background to classification development. Spine (Phila Pa 1976). 2014;39(25):2093-102. [DOI] [PubMed] [Google Scholar]
- 43.Kim HJ, Bridwell KH, Lenke LG, et al. Proximal junctional kyphosis results in inferior SRS pain subscores in adult deformity patients. Spine (Phila Pa 1976). 2013;38(11):896-901. [DOI] [PubMed] [Google Scholar]
- 44.Kim HJ, Lenke LG, Shaffrey CI, et al. Proximal junctional kyphosis as a distinct form of adjacent segment pathology after spinal deformity surgery. Spine (Phila Pa 1976). 2012;37(22 Suppl):S144-64. [DOI] [PubMed] [Google Scholar]
- 45.Acosta FL Jr, McClendon J Jr, O'Shaughnessy BA, et al. Morbidity and mortality after spinal deformity surgery in patients 75 years and older: complications and predictive factors: clinical article. J Neurosurg Spine. 2011;15(6):667-74. [DOI] [PubMed] [Google Scholar]
- 46.Yadla S, Maltenfort MG, Ratliff JK, et al. Adult scoliosis surgery outcomes: a systematic review. Neurosurg Focus. 2010;28(3):E3. [DOI] [PubMed] [Google Scholar]
- 47.Lenke LG, Fehlings MG, Shaffrey CI, et al. Neurologic outcomes of complex adult spinal deformity surgery: results of the prospective, multicenter Scoli-Risk-1 study. Spine (Phila Pa 1976). 2016;41(3):204-12. [DOI] [PubMed] [Google Scholar]
- 48.Lafage R, Schwab F, Challier V, et al. Defining spino-pelvic alignment thresholds: should operative goals in adult spinal deformity surgery account for age? Spine (Phila Pa 1976). 2016;41(1):62-8. [DOI] [PubMed] [Google Scholar]
- 49.Lafage R, Schwab F, Glassman S, et al. Age-Adjusted Alignment Goals Have the Potential to Reduce PJK. Spine (Phila Pa 1976). 2017;42(17):1275-282. [DOI] [PubMed] [Google Scholar]
- 50.Sethi RK, Pong RP, Leveque JC, et al. The Seattle spine team approach to adult deformity surgery: a systems-based approach to perioperative care and subsequent reduction in perioperative complication rates. Spine Deform. 2014;2(2):95-103. [DOI] [PubMed] [Google Scholar]
- 51.Buchlak QD, Yanamadala V, Leveque JC, et al. Complication avoidance with pre-operative screening: insights from the Seattle spine team.Curr Rev Musculoskelet Med. 2016;9(3):316-26. [DOI] [PMC free article] [PubMed] [Google Scholar]


