Abstract
Introduction
Although there has been a dramatic improvement in the outcomes of conservative treatment to achieve bony healing due to advances in diagnostic and therapeutic tools, in some patients, the results continue to be unfavorable. The purpose of this study was to investigate the outcomes of conservative treatment in pediatric patients with stress fractures occurring in the lamina that are discontinuous due to a contralateral pars defect or spina bifida occulta (SBO).
Methods
The medical records at our outpatient clinic for 103 consecutive patients (83 boys, 20 girls) with lumbar spondylolysis (LS) were reviewed to identify those who had presented with a stress fracture and a contralateral pars defect or with SBO at the affected lamina level.
Results
Twelve patients (11 boys, 1 girl) of mean age 12.3 (range 8-16) years were identified. Except for 1 stress structure that occurred at L4, all the stress fractures occurred at L5. Six patients had a pars defect, 5 had SBO, and 1 had both. Two of the 6 patients with a contralateral pars defect had early LS, 3 had progressive LS, and 1 had a pedicle fracture. The fracture healed in 1 (50%) of the 2 patients with early LS and in the patient with the pedicle fracture, but did not heal in any of the patients with progressive LS. Two of the 5 patients with SBO at the affected lamina level had early LS and 3 had progressive LS. The bony healing rate was 100% in the 2 patients with early LS and 66.7% in the 3 patients with progressive LS. The fracture healed in the patient with progressive LS and both a pars defect and SBO at the affected lamina.
Conclusions
Contralateral pars defect remains an unfavorable factor for bony healing discontinuous laminar stress fractures.
Keywords: conservative treatment, low back pain, lumbar spine, pediatric, spondylolysis, stress fracture
Introduction
The term lumbar spondylolysis (LS) is used to describe a stress fracture of the pars interarticularis1). Conservative treatment, including the cessation of sports activity and wearing a brace is recommended for bony healing in patients with LS. There is a strong association between early diagnosis and a favorable outcome of conservative treatment in terms of bony healing2-6).The diagnostic tools available for the detection of LS have improved in the last 20 years with the advent of magnetic resonance imaging (MRI) and computed tomography (CT) and there has been improvement in the therapeutic strategies available, including braces5,7). Consequently, there has been a dramatic improvement in the outcomes of conservative treatment in terms of bony healing2-4,8).
The literature identifies several factors that affect bony healing in patients with LS, including the stage of the fracture at the first presentation2-4), the spinal level affected6), and the condition of the contralateral pars interarticularis3). For example, Sairyo et al. reported that a unilateral pars defect could increase the risk of a stress fracture at the contralateral pedicle and pars interarticularis9). There have also been several reports of an association between LS and spina bifida occulta (SBO)10). In a study by Sakai et al., more than 90% of a cohort of elementary school-aged children with LS at L5 had sacral SBO and approximately 60% had SBO involving both the affected lamina and sacrum11).
The aim of this study was to investigate the outcomes of conservative treatment in patients with discontinuity of the lamina due to pseudoarthrosis (pars defect, terminal spondylolysis) on the contralateral side or SBO at the affected level and to determine their impact on the likelihood of successful fracture healing.
Patients and Methods
Patient data
Medical records from January 2012 to September 2017 at our outpatient clinic for 103 consecutive patients (83 boys, 20 girls) with a diagnosis of LS were reviewed to identify those who had presented initially with a stress fracture of the pars interarticularis and a contralateral pars defect or terminal LS or with SBO at the affected lamina level. The database was accumulated to include previously published data from January 2012 to December 20152).
Institutional review board exemption was obtained for this study in view of the study design, which involved a retrospective review of anonymized imaging studies.
Diagnostic imaging
LS was diagnosed on the basis of findings on plain radiographs, multidetector CT scans (Optima CT 660, GE Healthcare, Little Chalfont, UK), and MRI scans (1.5 T Achieva, Philips Healthcare, Amsterdam, The Netherlands). The fracture line or bony defect was classified as early, progressive, or terminal on CT using the system devised by Fujii et al.3), whereby a hairline fracture is visible in the early stage, progresses to a gap in the progressive stage, and manifests as pseudoarthrosis in the terminal stage.
Conservative protocol for bony healing
All the patients received conservative treatment that included rest, the cessation of sports activity, and the use of a thoracolumbosacral trunk brace4). Follow-up MRI scans were obtained monthly after the first presentation until high signal changes on the pedicle adjacent to the stress fracture were resolved on short tau inversion recovery (STIR) images12). Multidetector CT scans were also acquired at the first presentation for the staging of the stress fracture and at final follow-up to confirm if successful bony union had occurred. The pseudoarthrosis was defined if the defect was wide and sclerosis was observed on the final follow-up CT scan with resolution of the high signal changes on the pedicle on STIR images3,4). Patients with radiologic evidence of bony healing were allowed to remove the brace and return to playing sport provided that there were no clinical findings of tenderness or pain during motion.
Results
Twelve patients (11 male, 1 female) of mean age 12.3 (range 8-16) years were diagnosed with stress fracture of the lamina, including the pars interarticularis and pedicle with pseudoarthrosis (pars defect, terminal spondylolysis) on the contralateral side or SBO at the affected lamina level on their first presentation. Except for1 stress structure that occurred at L4, all the stress fractures occurred at L5. Six of the 12 patients had terminal LS, 5 had SBO, and1 patient had both (Table 1). All the patients completed their treatment and none were lost to follow-up.
Table 1.
Bony Healing Rate in Each Group.
| Patients with terminal spondylolysis (n = 6) | |||
| Stage at first presentation | Early (n = 2) | Progressive (n = 3) | Pedicle fracture (n = 1) |
| Bony healing (n) | 1 | 0 | 1 |
| Bony healing rate (%) | 50.0 | 0 | 100 |
| Patients with spina bifida occulta (n = 5) | |||
| Stage at first presentation | Early (n = 2) | Progressive (n = 3) | |
| Bony healing (n) | 2 | 2 | |
| Bony healing rate (%) | 100 | 66.7 | |
| Patients with terminal spondylolysis and spina bifida occulta (n = 1) | |||
| Stage at first presentation | Progressive (n = 1) | ||
| Bony healing (n) | 1 | ||
| Bony healing rate (%) | 100 | ||
Patients with terminal contralateral spondylolysis
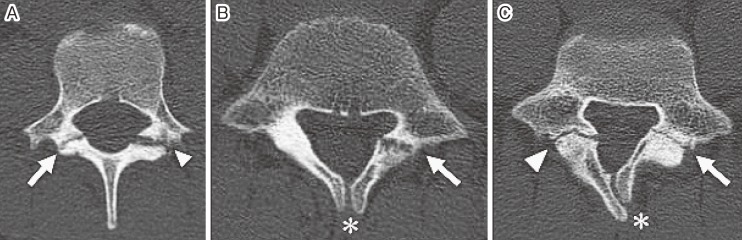
Two of the 6 patients with terminal LS on the contralateral side had a hairline fracture (early LS), 3 had an obvious fracture (progressive LS), and 1 had a pedicle fracture. Successful bony healing was achieved in 1 (50%) of the 2 patients with early LS, in none of the 3 patients with progressive LS, and in the patient with the pedicle fracture (Fig. 1A).
Figure 1.
Oblique axial views on computed tomographic scans showing (A) progressive LS (arrow) with terminal LS (arrow head) on the contralateral side, (B) progressive LS (arrow) with SBO (asterisk) at the affected lamina, and (C) progressive LS (arrow) with both terminal LS (arrow head) on the contralateral side and SBO (asterisk) at the affected lamina level.
LS, lumbar spondylolysis; SBO, spina bifida occulta
Patients with spina bifida occulta at the affected lamina level
Two of the 5 patients with SBO had early spondylolysis and 3 had progressive spondylolysis. The bony healing rate was 100% in the 2 patients with early spondylolysis and 66.7% in the 3 patients with progressive spondylolysis (Fig. 1B).
Patient with both defects
Bony healing was achieved in the patient with progressive LS who had both terminal LS on the contralateral side and SBO at the affected lamina level (Fig. 1C).
Discussion
Lumbar spondylolysis (LS) is a stress fracture at the pars interarticularis, and frequently occurs in adolescent athletes. If LS is detected before the fracture line becomes complete, the bone is able to heal without surgical intervention. MRI is often used to make an early diagnosis5,6,12). High signal change at the pedicle adjacent to the fracture site is a reliable diagnostic sign. This high signal change is also known to be an indicator of the potential for bony healing. Treatment for LS changed after several biomechanics studies showed that spondylolysis was initiated as a stress fracture from the ventral aspect because of the higher concentration of stress at the site during movements of the lumbar spine, such as extension and rotation. It has been established theoretically that a hard trunk brace can restrict those movements.
The above-mentioned advances in conservative treatment have achieved better outcomes in terms of bony healing. According to recent reports regarding the outcomes of conservative treatment in pediatric patients with LS, bony healing rates of more than 90% for early LS and 60%-80% for progressive LS have been obtained2,4).
Fujii et al. identified several factors that affected bony union following conservative treatment in 134 children; these factors were similar to those in our study. The stage of the contralateral defect most affected did not affect bony healing3). Approximately 20 years have passed since that study, and diagnostic and treatment methods have improved considerably. In the past, LS could only be diagnosed on plain radiographs and limited-gantry CT scans and was treated using a Damen corset. Recent advances in MRI and multidetector CT have allowed accurate early diagnosis of LS, which is usually treated nowadays with a thoracolumbosacral trunk brace. However, the results of this study suggest that despite the advances in the diagnostic and treatment methods, the ability of the bone to heal is adversely affected if terminal spondylolysis is present on the contralateral side but not if SBO is present at the affected lamina level. Even in 2 patients with early LS, 1 (50%) patient was refractory to the conservative treatment although total bony healing rates for early LS was more than 90% in the recent report2,4).
There have been two recent reports of favorable results using low-intensity pulsed ultrasound in patients with progressive LS13) and in those with early LS14). Those reports indicate that a higher bony healing rate and a shorter treatment period could be expected in the future if this treatment modality could be approved for use in patients with LS.
We acknowledge that there are several limitations to this study, mainly arising from its retrospective design and the inclusion of a limited number of subjects. However, all the patients completed their treatment and none were lost to follow-up. Furthermore, the study had some important strengths, in that all the patients were treated using the same protocol in a single outpatient clinic by the same clinician. The main factor in our ability to obtain 100% follow-up data was that our clinic is located on a small island covering an area of approximately 600 km2.
In conclusion, although there has been a dramatic improvement in the fracture healing rate in patients with LS due to advances in the methods used to diagnose and treat this condition, a bony defect (terminal spondylolysis) on the contralateral side still heralds unfavorable outcomes in terms of bony healing in patients with LS.
Conflicts of Interest: The authors declare that there are no relevant conflicts of interest.
Sources of Funding: This work was partly supported by JSPS KAKENHI Grant Number 16K10825.
Author Contributions: Toshinori Sakai and Tsuyoshi Goto conceived and designed the study. Kosuke Sugiura, Hiroaki Manabe, Fumitake Tezuka, Kazuta Yamashita, Yoichiro Takata, gathered and analyzed the data. Toshinori Sakai and Tsuyoshi Goto drafted the paper. Takashi Chikawa and Koichi Sairyo significantly revised the drafted paper. All the authors gave final approval of the version to be published.
Acknowledgement
We would like to thank all the staff members at Suiho Daiichi Hospital for helping to generate the records used in this study.
References
- 1.Wiltse LL, Widell EH Jr, Jackson DW. Fatigue fracture: the basic lesion is isthmic spondylolisthesis. J Bone Joint Surg Am. 1975;57(1):17-22. [PubMed] [Google Scholar]
- 2.Sakai T, Tezuka F, Yamashita K, et al. Conservative treatment for bony healing in pediatric lumbar spondylolysis. Spine (Phila Pa 1976). 2017;42(12):E716-20. [DOI] [PubMed] [Google Scholar]
- 3.Fujii K, Katoh S, Sairyo K, et al. Union of defects in the pars interarticularis of the lumbar spine in children and adolescents. The radiological outcome after conservative treatment. J Bone Joint Surg Br. 2004;86(2):225-31. [DOI] [PubMed] [Google Scholar]
- 4.Sairyo K, Sakai T, Yasui N, et al. Conservative treatment for pediatric lumbar spondylolysis to achieve bone healing using a hard brace: what type and how long?: Clinical article. J Neurosurg Spine. 2012;16(6):610-4. [DOI] [PubMed] [Google Scholar]
- 5.Sairyo K, Katoh S, Takata Y, et al. MRI signal changes of the pedicle as an indicator for early diagnosis of spondylolysis in children and adolescents: a clinical and biomechanical study. Spine (Phila Pa 1976). 2006;31(2):206-11. [DOI] [PubMed] [Google Scholar]
- 6.Goda Y, Sakai T, Sakamaki T, et al. Analysis of MRI signal changes in the adjacent pedicle of adolescent patients with fresh lumbar spondylolysis. Eur Spine J. 2014;23(9):1892-5. [DOI] [PubMed] [Google Scholar]
- 7.Terai T, Sairyo K, Goel VK, et al. Spondylolysis originates in the ventral aspect of the pars interarticularis: a clinical and biomechanical study. J Bone Joint Surg Br. 2010;92(8):1123-7. [DOI] [PubMed] [Google Scholar]
- 8.Morita T, Ikata T, Katoh S, et al. Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br. 1995;77(4); 620-5. [PubMed] [Google Scholar]
- 9.Sairyo K, Katoh S, Sasa T, et al. Athletes with unilateral spondylolysis are at risk of stress fracture at the contralateral pedicle and pars interarticularis: a clinical and biomechanical study. Am J Sports Med. 2005;33(4):583-90. [DOI] [PubMed] [Google Scholar]
- 10.Sakai T, Sairyo K, Takao S, et al. Incidence of lumbar spondylolysis in the general population in Japan based on multidetector computed tomography scans from two thousand subjects. Spine (Phila Pa 1976). 2009;34(21):2346-50. [DOI] [PubMed] [Google Scholar]
- 11.Sakai T, Goda Y, Tezuka F, et al. Characteristics of lumbar spondylolysis in elementary school age children. Eur Spine J. 2016;25(2):602-6. [DOI] [PubMed] [Google Scholar]
- 12.Sakai T, Sairyo K, Mima S, et al. Significance of magnetic resonance imaging signal change in the pedicle in the management of pediatric lumbar spondylolysis. Spine (Phila Pa 1976). 2010;35(14):E641-5. [DOI] [PubMed] [Google Scholar]
- 13.Arima H, Suzuki Y, Togawa D, et al. Low-intensity pulsed ultrasound is effective for progressive-stage lumbar spondylolysis with MRI high-signal change. Eur Spine J. 2017;26(12):3122-8. [DOI] [PubMed] [Google Scholar]
- 14.Tsukada M, Takiuchi T, Watanabe K. Low-intensity pulsed ultrasound for early-stage lumbar spondylolysis in young athletes. Clin J Sport Med. 2017. doi: 10.1097/JSM.0000000000000531. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]