Abstract
Background:
Older adults purchase and use over-the-counter (OTC) medications with potentially significant adverse effects. Some OTC medications, such as those with anticholinergic effects, are relatively contraindicated for use by older adults due to evidence of impaired cognition and other adverse effects.
Objective:
To inform the design of future OTC medication safety interventions for older adults, this study investigated consumers’ decision making and behavior related to OTC medication purchasing and use, with a focus on OTC anticholinergic medications.
Methods:
The study had a cross-sectional design with multiple methods. A total of 84 adults participated in qualitative research interviews (n = 24), in-store shopper observations (n = 39), and laboratory-based simulated OTC shopping tasks (n = 21). Simulated shopping participants also rank-ordered eight factors on their importance for OTC decision making.
Results:
Findings revealed that many participants had concerns about medication adverse effects, generally, but were not aware of age-related risk associated with the use of anticholinergic medications. Analyses produced a map of the workflow of OTC-related behavior and decision making as well as related barriers such as difficulty locating medications or comparing them to an alternative. Participants reported effectiveness, adverse effects or health risks, and price as most important to their OTC medication purchase and use decisions. A persona analysis identified two types of consumers: the habit follower, who frequently purchased OTC medications and considered them safe; and the deliberator, who was more likely to weigh their options and consider alternatives to OTC medications.
Conclusion:
A conceptual model of OTC medication purchase and use is presented. Drawing on study findings and behavioral theories, the model depicts dual processes for OTC medication decision making – habit-based and deliberation-based – as well as the antecedents and consequences of decision making. This model suggests several design directions for consumer-oriented interventions to promote OTC medication safety.
Keywords: Over-the-counter medication, Anticholinergic medications, Elderly, Mixed methods, User-centered design, Decision making
1. Understanding older adults’ over-the-counter medication decision making and behavior
The National Academy of Medicine report on Cognitive Aging calls attention to the short- and long-term adverse cognitive effects of anticholinergic medication use by older adults.1 Multiple studies of older adults show an association between the use of anticholinergics and brain atrophy, cognitive decline, hospitalizations, incidence of delirium or dementia, and mortality.2–15 In fact, systematic reviews reveal that up to 93% of all human studies systematically measuring anticholinergic activity and adverse cognitive outcomes report an association between the two.13,16 The prolonged use of anticholinergic medications by older adults is also associated with adverse outcomes such as dry mouth, visual impairment, and constipation.17 The American Geriatrics Society lists anticholinergics on its 2015 Beers list of potentially inappropriate medications for older adults.18 Despite this, as many as 1 in every 2 older Americans uses an anticholinergic medication.7,13 Similar exposure rates among older adults have been reported elsewhere, for example in large cohorts in the UK (47%)8 and New Zealand (23–51%).19 In addition to prescription anticholinergics, older adults commonly use over-the-counter (OTC) anticholinergics, particularly first-generation antihistamines such as diphenhydramine, doxylamine, and dimenhydrinate.20,21 Older adults in the US may purchase and use OTC medications with these ingredients, including popular products such as Benadryl® and nighttime or “PM” products, at high rates and for prolonged periods to treat allergies, sleeplessness, cold and cough, motion sickness, and other acute or chronic conditions.20,22
Despite several inpatient and outpatient-based interventions, no changes have been documented in the prevalence of anticholinergic medication prescribing or use over the past two decades.23,24 A promising but underutilized strategy to reduce older adults’ use of anticholinergics or other potentially unsafe prescription and OTC medications is to introduce consumer-oriented interventions that inform decision making and encourage behavior change.25 Research with older adults aiming to reduce other types of unsafe prescription or OTC medication use has reported success with patient-empowering booklets26 and consumer-facing educational software.27 Other studies have developed educational board games,28 OTC product labeling,29 and consumer-facing interventions in OTC retail stores.30 A key aspect of medication-related consumer-oriented interventions is not only changing behavior, but also influencing upstream consumer factors such as awareness, perceptions, education, and empowerment.26,28,31
To design a consumer-oriented intervention to reduce anticholinergic medication use, it is imperative to understand the product’s future end-users, how they currently make medication-related decisions, and how upstream factors influence ultimate decisions and behavior.32,33 Known by the axiom “know thy user,” obtaining this understanding is an industry best-practice for designing effective, usable, satisfying user-centered solutions.34 In practice, attaining an appropriately broad and deep understanding of a healthcare consumer, their perceptions, abilities, tasks, tools, and contexts requires multiple methods.35 Survey and interview studies of OTC medication perceptions provide some insight toward such understanding—for example, that consumers are influenced by brand familiarity32,36 and often treat OTC medications as safe or “not real” medications.32,37 However, there is a further need for research in natural and simulated OTC shopping settings, through which decision making and behavior can be studied prospectively and under realistic circumstances.38
This study investigated consumer decision making and behavior related to OTC medication purchasing and use, with a focus on anticholinergic medications. This formative, multimethod research phase of user-centered design was intended to produce: 1) an understanding of OTC-related cognition and behavior and 2) requirements and implications for person-centered intervention design. A sub-goal of this study was to develop a conceptual model to bridge study findings and potential future interventions. The model, presented in the discussion, follows Blalock’s recommendation to leverage existing behavioral theories when seeking to influence medication-related health behavior.39 This study addresses gaps in in situ or simulation studies and conceptual models of older adults’ OTC medication decision making and behavior, particularly related to anticholinergic medications.
2. Method
The cross-sectional study was conducted January–September 2016 and employed multiple methods with a new sample for each (total N = 84): interviews (N = 24); in-store shopper observations with and without ad-hoc probes (N = 39); and a laboratory-based simulated OTC shopping task with concurrent think-aloud (N = 21). Interviews were approved by the Indiana University Institutional Review Board (IRB) and remaining study components were deemed exempt by the IRB as not meeting the definition of human subjects research.
2.1. Interviews (n = 24)
Interviews were performed with 24 older adult primary care patients of a large urban safety net health system in the Midwest US. Participants were selected from an electronic database of anticholinergic medication users in the health system. Of 44 contact attempts, 24 (54.5%) agreed to participate, 10 (22.7%) declined, and 10 (22.7%) could not be reached or requested a call-back. Interviews were performed in patients’ homes. Two members from a group of four staff research assistants and one research manager met the patient in their home and obtained written consent. The staff received training individually and in groups on conducting qualitative interviews for this study. One staff member conducted the interviews. There were 11 interview questions that covered four topics: participants’ (i) knowledge and use of medications with anticholinergic properties, (ii) decision making and information seeking regarding using prescription and OTC medications, (iii) involvement of physicians in taking medications with or without anticholinergic properties; and (iv) medication use and management practices, broadly. Some questions were open-ended and encouraged a narrative response (e.g., “What drug information did you seek prior to taking it?”) whereas others were closed-ended with opportunity to explain further (e.g., “Do you understand what each of your medications is for?”). Interviews were audio-recorded with participant permission. In addition to notes on interview responses, staff collected notes on the home environment and performed an inventory of prescription and OTC medications. Interview participants received a $25 gift card.
2.2. In-store observations (n = 39)
Two staff design researchers first performed unobtrusive observations over approximately 9 h with 34 adults of varying ages. These observations were conducted in the OTC aisles of five major pharmacy retail shops in a large urban US city, chosen among those located in a 10-mile radius of the above-referenced Midwestern safety net hospital. Observations were distributed over various weekdays at popular shopping times, as indicated by Google analytics for each listed retail location. Staff recorded overt behaviors such as examining products and asking for assistance. The observations were an exploratory process intended to inform researchers of the practices generally followed by adults during OTC medication shopping, particularly those behaviors that might otherwise be taken for granted by the research team, for example, needing glasses to read a product label. However, they were uncontrolled and did not provide insight into difficult to observe phenomena such as decision making and information seeking.
Therefore, following unstructured observations, the two design researchers conducted contextual inquiry observations with five additional shoppers estimated by the researcher as aged 65 or older. Contextual inquiry is a naturalistic method used by designers wherein observations of natural behavior are supplemented by ad-hoc opportunistic probes to elicit additional information on observed behaviors.40 Scripted and ad-hoc probes asked shoppers about what they were thinking of as they were making their selection and prior experience with the purchase and use of similar OTC products.
For both observation methods, researchers positioned themselves at aisle-ends that shelved sleep, pain, cold and flu medications. Shoppers’ demographic data were not collected. Participants were not paid.
2.3. Shopping simulations (n = 21)
Shopping simulations were performed with older adults in a private conference room of a senior living center or in a university research laboratory. The simulation was performed using a mock-up of a retail OTC aisle using actual medication packages, contents, and pricing labels obtained from a retail store. We used both generic and brand name medications for pain, sleep, and combination (“PM”) products, some containing anticholinergic ingredients. The shelving was created with cardboard so it could be taken apart and easily transported. For illustration of this setup, we present a photograph of a participant performing the simulated shopping task in Fig. 1.
Fig. 1.

A participant performs the simulated shopping task. Participant is seen comparing packages of two over-the-counter (OTC) medications.
Participants were 21 English-speaking older adults with adequate vision and prior OTC medication shopping experience recruited from three urban senior living centers. Participants were screened for absence of terminal illness and cognitive impairment using a six-item screener.41 Participation occurred in either the senior living center or research laboratory per participants’ travel preference. Each session was video-recorded with the participant’s permission.
The simulation session followed a published protocol for OTC shopping research from a similar study that was conducted in retail pharmacies.30,38 Per that protocol, participants were instructed to select one or more medications to treat hypothetical sleep disturbance and pain symptoms. While participants made their selections, they were instructed to think-aloud, meaning to articulate their thoughts contemporaneously.42 Researchers occasionally probed participants to articulate their thoughts during the task, for instance, asking “why did you pick this medicine?” Instructions and probes encouraged participants to verbalize their thoughts and decision making process. After making a decision, researchers performed a debrief interview during which they further probed about any other factors involved in participants’ decisions, whether they had purchased the selected medication in the past, and how they typically make purchase decisions of this type. These questions were in part based on findings from preceding interviews and in-store observations.
Following the simulated shopping task, each participant completed a paper-based survey about their OTC medication shopping history. Of present relevance, participants completed a rank-ordering of factors they considered while purchasing OTC medications. They were instructed to order by importance the following eight factors: price, effectiveness, health risk/adverse (“side”) effects, ingredients, unit dosage, quantity, habit, brand.
Shopping simulation participants received a $25 gift card.
2.4. Data analysis
Transcribed data were analyzed as follows. For interviews and observations, descriptive qualitative content analysis43 was used to discern general patterns of awareness, decision making, and shopping behavior. Interview responses were coded in 11 categories such as adverse effects, alternative options, following instructions, decisions about medications, and access and adherence. The percent of respondents mentioning an identified theme and sub-theme (e.g., patient-driven, physician-driven, vs. shared decision making) were calculated for descriptive purposes.
Commonly observed themes and patterns from interview and instore observation data analysis were then visualized in a flow diagram44 of OTC medication purchasing and use. Flow diagraming is a data synthesis and visualization technique of contextual design, wherein key tasks and processes are plotted in sequence and annotated with barriers.40,44
Interviews and observations were also analyzed using the qualitative personas development method, a design technique in which data from a sample are grouped by similarity to form a small number of personas or user types.45 A persona represents patterns of behavior performed by similar people under similar circumstances and therefore captures a combination of person, process, and context factors.45 Personas provide intervention designers an understanding of the various user types who will need to be accommodated by the designed product or service.46
Simulated shopping task recordings were analyzed for medication choice and verbalized decision criteria. Participants’ written rankings of the eight decision criteria (from the survey administered during the shopping simulations) were analyzed by computing each criterion’s prevalence among participants’ top-three and bottom-three rankings.
Lastly, findings from the above analyses were synthesized and interpreted through the lens of prevailing social-psychological theories of human behavior, to formulate a conceptual model of OTC anticholinergic medication purchase and use behavior. This conceptual model is presented and discussed in the Discussion section.
3. Results
3.1. Participants
Table 1 reports the characteristics of participants from each research method.
Table 1.
Participant characteristics.
| Characteristic | Interviews | In-store observations |
Shopping simulations |
|---|---|---|---|
| Sample size | 24 | 39 | 21 |
| Mean age (SD, range) | 72.6 (4.78, 65–85) | – | 73.5 (5.59, 65–83) |
| Sex, n (%) | |||
| Male | 6 (25%) | – | 4 (19.0%) |
| Female | 18 (75%) | 17 (81.0%) | |
| Race, n (%) | |||
| White | 10 (41.7%) | – | 4 (19.0%) |
| African American | 14 (58.3%) | 14 (66.7%) | |
| Asian | 1 (4.8%) | ||
| Native Hawaiian | 1 (4.8%) | ||
| Multiple races | 1 (4.8%) | ||
| Mean years of education | – | – | 13.6 |
Blank cells indicate data were not recorded.
3.2. Interview findings
Most of the 24 interview participants stated having an awareness of medication-related adverse effects (67%) and 69% of those individuals had concerns or prior experiences with adverse effects. Two participants who were aware of adverse effects specifically stated that treating their symptoms was a more important consideration than potential adverse effects. Although all participants were using prescription or OTC anticholinergic medications, none mentioned adverse effects specific to anticholinergic medications, when asked. Participants were generally unaware of which medications had anticholinergic effects and did not voice concerns about using anticholinergic medications. About a third of all participants were willing to consider alternatives to current medications (29%), though often only with the consultation or recommendation of a clinician. Indeed, for both prescribed and OTC medications, 83% said they consulted a physician and nearly as many (75%) considered their physician the chief decision maker about medications. When asked specifically about OTC medications, participants reported how symptoms such as pain led to using an OTC medication already available at home. In contrast, purchasing new OTC medications created challenges including getting to the store and communicating their needs to a proxy shopper (e.g., adult child).
3.3. In-store observation findings
In-store observations identified several purchases of “combination” medications—ones treating multiple symptoms. These medications generally contained added anticholinergic ingredients, for instance, diphenhydramine added to a pain or cold medication and branded as a “PM/nighttime” product. Participants used aisle labels as way-finding mechanisms to locate OTC medications based on symptoms. Further, shoppers appeared to scan the shelves for packaging information that would help make a selection, for example, pillow or moon imagery to identify medications for sleep. Most shoppers knew what medication they wanted to purchase when entering the store, indicated by shoppers who went directly to the location of the purchased product; this strategy was confirmed by contextual inquiry participants. If what they sought could not be found, shoppers either asked store staff or sought alternative medications. Nine (26%) shoppers sought help from someone in the store: four approached someone in the pharmacy with questions about choosing a medication and the other five approached front-store staff for help retrieving a medication off the shelf. Three shoppers brought empty OTC medication boxes to help find similar products at the store. Observations also showed that individuals frequently examined the front and, to a lesser extent, back or sides of product packaging.
Probes during in-store contextual inquiry revealed that shoppers sought information about price, quantity, effectiveness, familiarity, and adverse effects or health risks. They also attempted to identify and compare alternatives by combining several decision criteria, for example: “I am looking for Bayer, but I don’t see it here. So let’s see, this aisle says pain … let me look at the other ones here … Aspirin … and … Advil. I don’t know … both says pain reliever … I know my doctor said I can take Aspirin … so I will probably pick the cheap brand of Aspirin.” During these information-processing cycles, many participants weighed the pros and cons of: 1) purchasing medication based on familiarity and past experiences vs. 2) price, for example: “I am not supposed to take Ibuprofen or Aspirin, I can take Tylenol. So I would take this generic brand here since it is cheap”. When asked why this participant chose a product labeled “PM”, she responded, “Oh I didn’t see that. I did see night-time relief, which is good, I can sleep well at night.” Generally, even if participants were aware of certain ingredients relatively contraindicated for them, they did not demonstrate awareness or concern about anticholinergic ingredients.
3.4. Laboratory-based simulated shopping findings
During the simulated shopping sessions with think-aloud, 30% of participants chose sleep medications and 20% pain medications with anticholinergic ingredients, potentially risky decisions in this older adult sample. All participants preferred a medication they perceived was effective and inexpensive. Participants preferred familiar medications. They attended to marketing text such as “Pain reliever” and “nighttime sleep aid,” but failed to read all the ingredients. Most participants were observed paying attention to warnings and usage instructions on the medication box.
When asked to rank OTC medication decision criteria by importance, participants tended to rank effectiveness, health risks/adverse (“side”) effects, and price toward the top and quantity, habit, and brand toward the bottom (Table 2). However, about a third of participants also highly ranked habit and brand, consistent with above observations.
Table 2.
Percentage of participants ranking the importance of OTC medication decision criteria in their top 3, middle, and bottom 3.
| Decision criteria | Participant rankings of importance of each decision criterion |
||
|---|---|---|---|
| Top 3 | Middle | Bottom 3 | |
| Effectiveness | 62% | 14% | 24% |
| Health risk/adverse (“side”) | 48% | 38% | 14% |
| effects | |||
| Price | 38% | 29% | 33% |
| Dosage | 24% | 38% | 38% |
| Ingredients | 29% | 38% | 33% |
| Quantity | 38% | 14% | 48% |
| Habit | 33% | 14% | 52% |
| Brand | 29% | 14% | 57% |
Values ≥ 33% are bolded
3.5. Flow and personas analyses of OTC medication purchase and use
Findings from in-store observations and contextual inquiry coupled with simulated shopping sessions were combined to identify the workflow and cognitive processes involved in OTC purchase and use behavior, depicted in Fig. 2. The flow diagram also indicates the goals and barriers related to these processes (Fig. 2). Barriers included transportation and in-store navigation challenges, lack of familiarity with medications, difficulty reading or understanding packaging, and the inaccessibility of staff in the store.
Fig. 2.
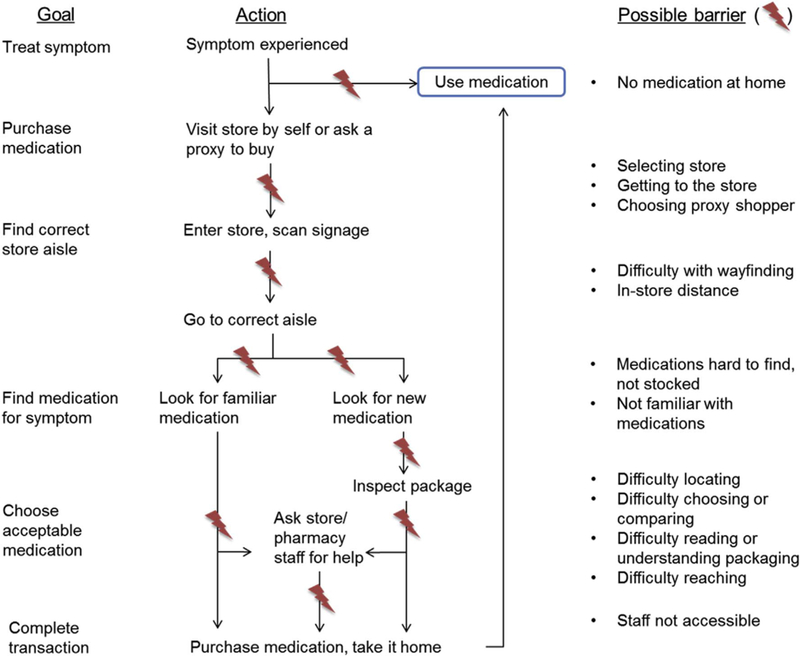
Flow of OTC medication purchase and use and barriers therein. Components of this figure were identified from in-store observations, and reported by participants during contextual inquiry and simulated shopping sessions.
Separate from the flow analysis, personas analysis was used to identify distinct consumer types, based on interviews, observations, and simulation sessions. These personas represented not only different individuals, but also typical actions and contextual circumstances. We identified two personas. The first was the habit follower. Habit followers were frequent OTC medication purchasers who trusted these medications to be clinically tested, perceived the medications that they used repeatedly were safe, and followed the instructions listed on medication packaging. The second persona type was the deliberator. Deliberators were less frequent OTC medication purchasers and more likely to examine their choices and try non-pharmacological remedies before or in combination with OTC medications. Participants representing both personas reported medication price as a significant factor influencing their decisions.
4. Discussion
Using mixed methods for data collection and analysis taken from user-centered design methodology, this study described the perceptions, workflow, decision making processes, and personas related to OTC medication purchase and use behavior. Although to our knowledge ours is the first study to formally map the process of OTC medication decision making and behavior, we acknowledge future work is needed, including more detailed workflow analysis, as demonstrated in other studies of medication management.47,48 In addition, because the present study focused on pain and sleep aids containing anticholinergic agents known to increase risk in older adults, additional research is needed before generalizing our conclusions to other medications and age groups.
4.1. Factors associated with OTC medication decision making and behavior
Consistent with prior studies of OTC medications, participants attended to effectiveness and health risks or adverse effects.36 For example, in a Nielsen study of 1194 households, the top five most important factors for OTC medication decisions included two efficacy and two safety factors.49 This finding also parallels the typical finding that older adult prescription medication adherence is chiefly influenced by the consumer’s weighing of costs (e.g., risk of harm, effort) to benefits (e.g., efficacy).50 However, like studies of OTC analgesics,51,52 we also noted participants lacked awareness or had difficulty fully understanding the age-related safety implications of OTC medications with anticholinergic effects, which may under-represent the true impact of safety in the decision making process. This lack of awareness and understanding indicates the need for further research on what consumers do or do not know regarding OTC medications with anticholinergic effects, how they obtain and process safety information about these medications, and what interventions such as education or product labeling could improve awareness and understanding.
Our observations of in-store and simulated shopping revealed that individuals sought effectiveness and safety information primarily, if ever, from product packaging and more rarely (10% of in-store shoppers) from a pharmacist. In other studies, older adults were more likely than younger counterparts to seek advice from healthcare professionals,53 and consumers provided with an ask-the-pharmacist service demonstrated a high rate of questions for pharmacists regarding effectiveness and safety.54 Furthermore, a national survey (n = 1009) study reported 80% of Americans would purchase an OTC medication if advised by their pharmacist and 82% would avoid an advised-against medication.55 This raises the possibility that observed shoppers in our in-store observations would have sought advice from pharmacists but may not have perceived pharmacists as available, approachable, or accessible. Other explanations include the potential time required to consult a pharmacist, not knowing that a pharmacist can assist with OTC medication decisions, or not trusting the pharmacist compared to physicians.
The physician is another potential source of advice for OTC medication decisions. Interview participants often regarded the physician as a trusted source of medication advice, although our question did not distinguish between prescription and OTC medication advice. However, two other studies reported low rates of consumers consulting with healthcare providers about OTC medications.51,56 A more recent study found that 86% believed their physician was aware of their OTC medications but only 46% actually reported OTC medication use to physicians and this rate was even lower among those who were younger, African Americans, less educated, less health literate, and patients in a safety net hospital.57
Other reasons for OTC medication decisions included price, quantity, and habit. Price and quantity were unimportant to some but very important to others, indicating the socioeconomic nature of OTC medication purchasing in our study population. The implication is safety interventions focusing on educating individuals about adverse effects or effectiveness may not be sufficient if cost factors are not considered, or that cost factors can be used to enhance safety intervention effectiveness. For example, the price of allergy medication with anticholinergic ingredients (diphenhydramine) differs from the price of those without (e.g., fexofenadine, loratadine, cetirizine). Habit was another factor that some ranked as highly important whereas others ranked it as less important. Hannah and Hughes36 found that 79.1% of survey respondents agreed or strongly agreed that their OTC medication choices were influenced by name and brand, leading the authors to conclude:
“Over time, people may build up their own ‘OTC formulary’ of products … If a patient has used a cough medicine and deems it to be effective, hearing about the evidence-base of the product (or alternative products) will seem irrelevant when they want to purchase the product again.”36
However, for those who ranked habit as relatively unimportant, at least three possibilities exist: 1) some individuals’ purchasing behavior is less habit-driven than others’; 2) individuals may switch to a more deliberative decision making process when prompted, for example, in a simulated shopping research session; 3) or participants were indeed influenced by habit but reported otherwise, for example, because they were not fully aware of the reasons for their behavior or wished to give a socially desirable answer.
The influence of habit vs. deliberation about factors such as effectiveness and safety was central to the two consumer types identified by our personas analysis. That analysis proposed two general categories of OTC medication decision makers: the habit follower and the deliberator. We note that each persona is a “hypothetical archetype of actual users,”58 and necessarily an oversimplification of reality. The habit follower and deliberator personas are empirically based but require validation.59,60 Holden and colleagues offer one quantitative method for forming and evaluating healthcare consumer personas.46
4.2. A conceptual model of OTC medication decision making and behavior
A landmark 2014 report from a national summit on OTC medication safety for older adults25 states:
“We know surprisingly little about the ways older adults select OTC medications and decide when to start or stop use, how older people actually use the medications, or how involved clinicians and family members are in older adult OTC behavior. This effort is critical for developing interventions to help ensure safe and appropriate OTC use.”25
The reports calls for research, like ours, exploring the basis for OTC medication-related behavior, as well as the development of interventions to increase the safety of this behavior for older adults. We therefore present a conceptual model based on a combination of our mixed-method study findings and the social-psychological literature on decision making and health behavior.39,61 To build this model, we first restate some of our findings:
Individuals differed on various dimensions such as familiarity with OTC medications, prior knowledge, and beliefs (e.g., regarding adverse effects), and these differences corresponded to differences in decision making and behavior.
System factors62,63 were also important and were related to the physical environment (e.g., store layout), task (e.g., time pressure), tools and artifacts (e.g., product packaging), and socio-organizational context (e.g., availability of staff to assist, product costs).
A third and variable form of input into decision making and behavior comes from pharmacists and physicians.
Some individuals appear to be habit followers, whereas others are deliberators. These appear to be discrete consumer types.
The conceptual model in Fig. 3 synthesizes and builds on these findings. In the model, individual characteristics, system factors, and other individuals serve as input for consumer OTC medication decision making. Examples of each input are given based on present findings and related literature (e.g., showing that family members can influence OTC decisions36), but further research is needed to fully specify them. The model distinguishes between two decision making pathways, based on the two identified personas. The first path is a habit-based, more intuitive, and relatively low-effort or “autopilot” route called System 1 in the literature.64 The second is a more deliberative reasoning-based process called System 2,64 in which effort is invested to compare multiple options based on important factors such as price, prior effectiveness, and awareness of adverse effects. The distinction between the two pathways is described in the literature on human behavior as dual-process theories of reasoning.65 Our initial findings were highly consistent with these theories but further research would be needed to more fully understand whether and how System 1 and System 2 processes play a role in OTC medication decision making. We further note that each process can be specified by referring to social-psychological theories applicable to medication use behavior,39 such as the Theory of Planned Behavior66 or Health Belief Model,67 which explain the decision making factors involved in deliberation-based processes. For example, the Health Belief Model might depict deliberation-based anticholinergic OTC medication use as a product of: the perceived personal threat of medication-related cognitive impairment; perceived benefits vs. barriers of avoiding anticholinergic medication use; and specific cues to action such as medication labels, instructions, or alternative medications. Further research is required to formally specify and test specific deliberation-based models for OTC medication-related behavior, as has been done for prescription medication use.68,69 Another research question not addressed by our findings is: under which circumstances is an individual’s decision process habit-vs. deliberation-based?
Fig. 3.
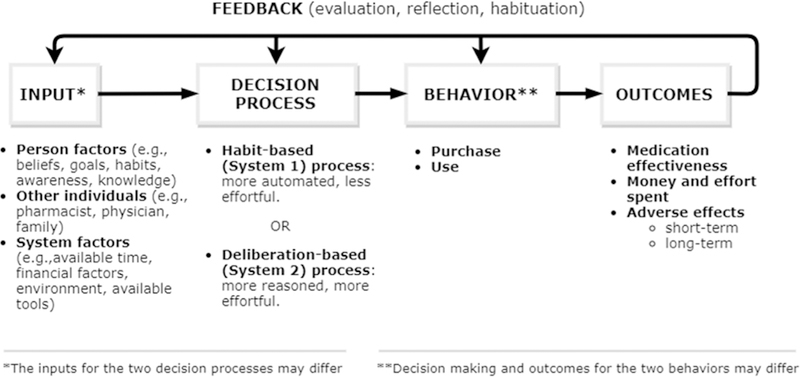
Conceptual model of OTC medication decision making and behavior.
The model depicts purchase and use behavior as the output of both System 1 and System 2 based decision making. This then results in outcomes, not observed in this study, but commonly reported in the literature, such as the actual effectiveness of the medication, adverse effects, and money or effort expended in completing the behavior. The last element of the model is a set of feedback loops representing: 1) an individual’s evaluation of the outcomes of their OTC medication-related behavior and reflection on whether it met his or her goals; and 2) the progressive habituation of behavior and thus the automation of future decisions. Although this temporal feedback phenomenon was not observed in the present cross-sectional study, it is a hallmark feature of human learning, behavior, and performance.62,70,71
4.3. Practical implications
The model in Fig. 3 suggests four design directions for consumer interventions related to OTC medication use and safety. First, interventions targeting habit-based decision making could support safer habits for older adults. This would be accomplished generally by replacing an existing routine with another, such that the same cues will trigger safer but equally rewarding responses.72 Interventions of this kind would involve introducing nudges or simple alternatives at critical times (e.g., when a symptom is experienced or upon entering an aisle) and consistent rewarding of desired behaviors. Second, interventions could instead encourage deliberation. For instance, interventions could prompt shoppers to pause and reflect in retail aisles or send reminders to their phones. This approach could include awareness-raising campaigns, for example distributing multimedia materials on websites and social media platforms.
A third approach would be to support decision making with education, product labeling, or decision aids using personalized, just-in-time information. Personalization could involve tailoring information to the individual’s personal risk, symptoms, knowledge, or importance placed on factors such as cost, safety, and effectiveness. The decision aid would provide data on the decision criteria described above, direct consumers’ attention to safety-relevant label information and away from marketing elements, and provide easy directions for identifying potentially harmful medications and choosing safer alternatives. The decision aid could facilitate other useful decision-relevant actions such as documenting consumers’ brand preferences, storing coupons, or communicating with pharmacists. The Indiana University (IU) Brain Health Patient Safety Laboratory is currently developing and testing both digital and analog mobile decision aids of this kind including the Brain Buddy App and paper-based Brain Safe decision aid.
Fourth, interventions can support evaluative feedback on post-purchase or post-use outcomes, for example, using a diary for symptom resolution or side-effects.
4.4. Methods strengths and limitations
This study had a number of strengths and limitations. Strengths included the mixed method design, which permitted gathering complementary perspectives on consumer characteristics and behavior. Further, the use of user-centered design methods was consistent with best practices for consumer interventions, which are needed to empower patients73 and complement largely professional-oriented deprescribing interventions.74 The development of a conceptual model to frame future research and practice is a further strength of the study.39,75 Limitations include the use of convenience sampling and therefore the risks of sampling bias and restriction of range. Furthermore, each method had specific limitations that we attempted to balance by using multiple methods. Interviews had limitations related to self-report. Unobtrusive in-store observations offered better insight into actual behavior but permitted no control over shoppers demographics or medication needs, resulting in potential sampling bias. Simulating shopping allowed insight into the cognitive processes involved in decision making, to the extent that these could be verbalized by participants, but had lower ecological validity compared to natural shopping. Paradoxically, using scenarios to study naturalistic decision making may have produced framing effects that influenced participants’ decisions and behaviors.76 Lastly, the design of the study to generate rather than test a model of decision making and behavior requires further research to validate and further specify the conceptual model presented above.
5. Conclusion
Understanding the way older consumers decide to purchase and use OTC medications with or without anticholinergic effects offers important insight for the user-centered design of consumer-oriented OTC medication safety interventions. An important insight for future research and practice is the dual-process nature of naturalistic decision making: habit-based and deliberation-based. The model depicting this dual-process decision making, its antecedents, and outcomes suggests several design directions for consumer interventions to promote OTC medication safety as well as other future medication safety interventions.
Acknowledgments
We thank the participants in the study and the research sites for assistance recruiting. We thank reviewers for helpful feedback. This study was supported by grantP30 HS024384–01 (Callahan, PI) from the Agency for Healthcare Research and Quality (AHRQ). The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ.
Footnotes
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.sapharm.2018.03.002.
References
- 1.Institute of Medicine. Cognitive Aging: Progress in Understanding and Opportunities for Action Washington, DC: National Academies Press; 2015. [PubMed] [Google Scholar]
- 2.Han L, Agostini JV, Allore HG. Cumulative anticholinergic exposure is associated with poor memory and executive function in older men. J Am Geriatr Soc. 2008;56(12):2203–2210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katz IR. What should we do about undertreatment of late life psychiatric disorders in primary care? J Am Geriatr Soc. 1998;46(12):1573–1575 published Online First: 1998/12/16. [DOI] [PubMed] [Google Scholar]
- 4.Turner C, Handford AD, Nicholson AN. Sedation and memory: studies with a histamine H-1 receptor antagonist. J PsychopharmacoL 2006;20(4):506–517. 10.1177/0269881106059804 published Online First: 2006/01/13. [DOI] [PubMed] [Google Scholar]
- 5.Kay G, Crook T, Rekeda L, et al. Differential effects of the antimuscarinic agents darifenacin and oxybutynin ER on memory in older subjects. Eur UroL. 2006;50(2):317–326. http://dx.doi.org/10.10167j.eururo.2006.03.057 published Online First: 2006/05/12. [DOI] [PubMed] [Google Scholar]
- 6.Sittironnarit G, Ames D, Bush AI, et al. Effects of anticholinergic drugs on cognitive function in older Australians: results from the AIBL study. Dement Geriatr Cognit Disord. 2011;31(3):173–178. 10.1159/000325171 published Online First: 2011/03/11. [DOI] [PubMed] [Google Scholar]
- 7.Campbell NL, Boustani MA, Lane KA, et al. Use of anticholinergics and the risk of cognitive impairment in an African American population. NeuroLogy. 2010;75(2):152–159. 10.1212/WNL.0b013e3181e7f2ab published Online First: 2010/07/14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fox C, Richardson K, Maidment ID, et al. Anticholinergic medication use and cognitive impairment in the older population: the medical research council cognitive function and ageing study. J Am Geriatr Soc. 2011;59(8):1477–1483. [DOI] [PubMed] [Google Scholar]
- 9.Borson S, Boustani MA, Buckwalter KC, et al. Report on milestones for care and support under the US national plan to address Alzheimer’s disease. Alzheimer’s Dementia. 2016;12(3):334–369. [DOI] [PubMed] [Google Scholar]
- 10.Koyama ASM, Ensrud K, Hillier TA, Yaffe K. Long-term cognitive and functional effects of potentially inappropriate medications in older women. J Gerontol A Biol Sci Med Sci. 2014;69(4):423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cai X, Campbell N, Khan B, et al. Long-term anticholinergic use and the aging brain. Alzheimer’s Dementia 2013;9(4):377–385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Risacher SL, McDonald BC, Tallman EF, et al. Association between anticholinergic medication use and cognition, brain metabolism, and brain atrophy in cognitively normal older adults. JAMA Neurol. 2016;73(6):721–732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Campbell N, Boustani M, Limbil T, et al. The cognitive impact of anticholinergics: a clinical review. Clin Interv Aging. 2009;4:225–233 [published Online First: 2009/06/26]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell N, Perkins A, Bradt P, et al. Association of anticholinergic burden with cognitive impairment and health care utilization among a diverse ambulatory older adult population. Pharmacotherapy. 2016;36(11):1123–1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chatterjee S, Bali V, Carnahan RM, et al. Risk of mortality associated with anticholinergic use in elderly nursing home residents with depression. Drugs Aging. 2017. 10.1007/s40266-017-0475-5. [DOI] [PubMed] [Google Scholar]
- 16.Fox C, Smith T, Maidment I, et al. Effect of medications with anti-cholinergic properties on cognitive function, delirium, physical function and mortality: a systematic review. Age Ageing. 2014;43(5):604–615. [DOI] [PubMed] [Google Scholar]
- 17.Feinberg M The problems of anticholinergic adverse effects in older patients. Drugs Aging. 1993;3(4):335–348 published Online First: 1993/07/01. [DOI] [PubMed] [Google Scholar]
- 18.American Geriatrics Society 2015. Beers criteria update expert panel. American Geriatrics society 2015 updated Beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63(11):2227–2246. 10.1111/jgs.13702. [DOI] [PubMed] [Google Scholar]
- 19.Salahudeen MS, Hilmer SN, Nishtala PS. Comparison of anticholinergic risk scales and associations with adverse health outcomes in older people. J Am Geriatr Soc. 2015;63(1):85–90. [DOI] [PubMed] [Google Scholar]
- 20.Albert SM, Roth T, Toscani M, et al. Sleep health and appropriate use of OTC sleep aids in older adults—recommendations of a gerontological society of America workgroup. Gerontol. 2015;57(2):163–170 gnv139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kaufman DW, Kelly JP, Rosenberg L, et al. Recent patterns of medication use in the ambulatory adult population of the United States: the Slone survey. JAMA. 2002;287(3):337–344. [DOI] [PubMed] [Google Scholar]
- 22.Kemper RF, Steiner V, Hicks B, et al. Anticholinergic medications: use among older adults with memory problems. J Gerontol Nurs. 2007;33(1):21–31. [DOI] [PubMed] [Google Scholar]
- 23.Felton M, Hanlon JT, Perera S, et al. Racial differences in anticholinergic use among community-dwelling elders. Consult Pharm. 2015;30(4):240–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sumukadas D, McMurdo ME, Mangoni AA, et al. Temporal trends in anticholinergic medication prescription in older people: repeated cross-sectional analysis of population prescribing data. Age Ageing. 2014;43(4):515–521. [DOI] [PubMed] [Google Scholar]
- 25.Albert SM, Bix L, Bridgeman MM, et al. Promoting safe and effective use of OTC medications: CHPA-GSA National Summit. Gerontol. 2014;54(6):909–918 gnu034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tannenbaum C, Martin P, Tamblyn R, et al. Reduction of inappropriate benzodiazepine prescriptions among older adults through direct patient education: the EMPOWER cluster randomized trial. JAMA Intern Med. 2014;174(6):890–898. [DOI] [PubMed] [Google Scholar]
- 27.Neafsey PJ, Strickler Z, Shellman J, et al. An interactive technology approach to educate older adults about drug interactions arising from over-the-counter self-medication practices. Publ Health Nurs. 2002;19(4):255–262. [DOI] [PubMed] [Google Scholar]
- 28.Burghardt KJ, Bowman MR, Hibino M, et al. Using educational games to promote the seeking of a pharmacist and to teach key medication use messages: results from an inner city health party. Res Soc Adm Pharm. 2013;9(5):542–552. [DOI] [PubMed] [Google Scholar]
- 29.King JP, Davis TC, Bailey SC, et al. Developing consumer-centered, nonprescription drug labeling: a study in acetaminophen. Am J Prev Med. 2011;40(6):593–598. [DOI] [PubMed] [Google Scholar]
- 30.Chui MA, Stone JA, Holden RJ. Improving over-the-counter medication safety for older adults: A study protocol for a demonstration and dissemination study. Res Soc AdmPharm 2017;13(5):930–937 10.1016/j.sapharm.2016.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kuntz JL, Safford MM, Singh JA, et al. Patient-centered interventions to improve medication management and adherence: a qualitative review of research findings. Patient Educ Counsel. 2014;97(3):310–326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.A spoonful of sugar. Understanding the Over-the-counter Medication Needs and Practices of Older Adults. 2013 7th International Conference on Pervasive Computing Technologies for Healthcare and Workshops IEEE; 2013. [Google Scholar]
- 33.Martin-Hammond AM, Abegaz T, Gilbert JE. Designing an over-the-counter consumer decision-making tool for older adults. J Biomed Inf. 2015;57:113–123. [DOI] [PubMed] [Google Scholar]
- 34.ISO Standard 9241–210. Ergonomics of Human-system Interaction – Part 210: Human-centred Design for Interactive Systems, 2010. 2010; 2010.
- 35.Valdez RS, Holden RJ, Novak LL, et al. Transforming consumer health informatics through a patient work framework: connecting patients to context. J Am Med Inf Assoc. 2015;22(1):2–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hanna L-A, Hughes CM. Public’s views on making decisions about over-the-counter medication and their attitudes towards evidence of effectiveness: a cross-sectional questionnaire study. Patient Educ Counsel. 2011;83(3):345–351. [DOI] [PubMed] [Google Scholar]
- 37.Eaves ER. “Just Advil”: harm reduction and identity construction in the consumption of over-the-counter medication for chronic pain. Soc Sci Med. 2015;146:147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stone JA, Lester CA, Aboneh EA, et al. A preliminary examination of over the counter medication misuse rates in older adults. Res Soc Adm Pharm. 2017;13(1):187–192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Blalock SJ. The theoretical basis for practice-relevant medication use research: patient-centered/behavioral theories. Res Soc Adm Pharm. 2011;7(4):317–329. [DOI] [PubMed] [Google Scholar]
- 40.Beyer H, Holtzblatt K. Contextual Design: Defining Customer-centered Systems. San Francisco: Morgan Kaufmann; 1998. [Google Scholar]
- 41.Callahan CM, Unverzagt FW, Hui SL, et al. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care. 2002;40(9):771–781. [DOI] [PubMed] [Google Scholar]
- 42.Ericsson KA, Simon HA. How to study thinking in everyday life: contrasting think-aloud protocols with descriptions and explanations of thinking. Mind Cult Activ. 1998;5(3):178–186. [Google Scholar]
- 43.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. QuaI Health Res. 2005;15:1277–1288. [DOI] [PubMed] [Google Scholar]
- 44.Holtzblatt K, Beyer H. Contextual Design: Evolved. San Rafael, CA: Morgan & Claypool; 2015. [Google Scholar]
- 45.Adlin T, Pruitt J. The Persona Lifecycle: Keeping People in Mind throughout Product Design. San Francisco: Morgan Kaufmann; 2010. [Google Scholar]
- 46.Holden RJ, Kulanthaivel A, Purkayastha S, et al. Know thy eHealth user: development of biopsychosocial personas from a study of older adults with heart failure. Int J Med Inf. 2017;108:158–167 10.1016/j.ijmedinf.2017.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bajcar J Task analysis of patients’ medication-taking practice and the role of making sense: a grounded theory study. Res Soc Adm Pharm. 2006;2(1):59–82. [DOI] [PubMed] [Google Scholar]
- 48.Mickelson RS, Unertl KM, Holden RJ. Medication management: the macrocognitive workflow of older adults with heart failure. JMIR Human Factors. 2016;3:e27 https://humanfactors.jmir.org/2016/2/e27/. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Consumer Healthcare Products Association. Understanding Trust in OTC Medicines: Consumer and Healthcare Provider Perspectives. 2013; 2013. http://www.yourhealthathand.org/images/uploads/CHPA_OTC_Trust_Survey_White_Paper.pdf.
- 50.Sirey JA, Weinberger MI, Greenfield A, et al. Medication beliefs and self-reported adherence among community-dwelling older adults. Clin Therapeut. 2013;35(2):153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wilcox CM, Cryer B, Triadafilopoulos G. Patterns of use and public perception of over-the-counter pain relievers: focus on nonsteroidal antiinflammatory drugs. J Rheumatol. 2005;32(11):2218–2224. [PubMed] [Google Scholar]
- 52.Ngo SN, Stupans I, Leong WS, et al. Appropriate use of non-prescription ibuprofen: a survey of patients’ perceptions and understanding. Int J Pharm Pract 2010;18(1):63–65. [DOI] [PubMed] [Google Scholar]
- 53.Stephens EC, Johnson MM. Dr. Mom and other influences on younger and older adults’ OTC medication purchases. J Appl Gerontol. 2000;19(4):441–459. [Google Scholar]
- 54.Jariangprasert CS, El-Ibiary SY, Tsourounis C, et al. What women want to know: an assessment of online questions asked by women using an ask-the-pharmacist service. J Pharm Technol. 2007;23(4):214–220. [Google Scholar]
- 55.National Council on Patient Information and Education. Uses and Attitudes about Taking Over-the-counter Medicines. 2003; 2003. http://www.bemedwise.org/docs/summarysurveyfindings.pdf.
- 56.Sleath B, Rubin RH, Campbell W, et al. Physician-patient communication about over-the-counter medications. Soc Sci Med. 2001;53(3):357–369. [DOI] [PubMed] [Google Scholar]
- 57.Serper M, McCarthy DM, Patzer RE, et al. What patients think doctors know: beliefs about provider knowledge as barriers to safe medication use. Patient Educ Counsel. 2013;93(2):306–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cooper A The Inmates Are Running the Asylum: Sams-Pearson 1999; 1999. [Google Scholar]
- 59.Cooper A, Reimann R, Cronin D, et al. About Face: the Essentials of Interaction Design. San Francisco, CA: Wiley; 2014. [Google Scholar]
- 60.Miaskiewicz T, Kozar K. Personas and user-centered design: how can personas benefit product design processes? Des Stud. 2011;2011(32):417–430. [Google Scholar]
- 61.Fishbein M A reasoned action approach to health promotion. Med Decis Making. 2008;28:834–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Holden RJ, Carayon P, Gurses AP, et al. SEIPS 2.0: a human factors framework for studying and improving the work of healthcare professionals and patients. Ergonomics. 2013;56(11):1669–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Holden RJ, Schubert CC, Mickelson RS. The patient work system: an analysis of self-care performance barriers among elderly heart failure patients and their informal caregivers. Appl Ergon. 2015;47:133–150. 10.1016/j.apergo.2014.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kahneman D Maps of bounded rationality: psychology for behavioral economics. Am Econ Rev. 2003;93(5):1449–1475. [Google Scholar]
- 65.Evans JSB. In two minds: dual-process accounts of reasoning. Trends Cognit Sci 2003;7(10):454–459. [DOI] [PubMed] [Google Scholar]
- 66.Ajzen I The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211. [Google Scholar]
- 67.Rosenstock IM. The health belief model and preventive health behavior. Health Educ Behav. 1974;2(4):354–386. [Google Scholar]
- 68.Young HN, Lipowski EE, Cline RJ. Using social cognitive theory to explain consumers’ behavioral intentions in response to direct-to-consumer prescription drug advertising. Res Soc Adm Pharm. 2005;1(2):270–288. [DOI] [PubMed] [Google Scholar]
- 69.Wu P, Liu N. Association between patients’ beliefs and oral antidiabetic medication adherence in a Chinese type 2 diabetic population. Patient Prefer Adherence. 2016;10:1161–1167. 10.2147/PPA.S105600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bandura A Social Foundations of Thought and Action. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- 71.Kluger AN, DeNisi A. The effects of feedback interventions on performance: a historical review, a meta-analysis, and a preliminary feedback intervention theory. Psychol Bull. 1996;119(2):254–284. [Google Scholar]
- 72.Wendel S Designing for Behavior Change: Applying Psychology and Behavioral Economics. O’Reilly Media; 2013. [Google Scholar]
- 73.Novak LL, Unertl KM, Holden RJ. Realizing the potential of patient engagement: designing IT to support health in everyday life. In: Ammenwerth E, Rigby M, eds. Evidence-based Health Informatics. IOS Press; 2016:237–247. [PMC free article] [PubMed] [Google Scholar]
- 74.Patterson SM, Hughes C, Kerse N, et al. Interventions to Improve the Appropriate Use of Polypharmacy for Older People. The Cochrane Library; 2012. [DOI] [PubMed] [Google Scholar]
- 75.Faiola A, Holden RJ. Consumer health informatics: empowering healthy-lifestyle-seekers through mHealth. Prog Cardiovasc Dis. 2017;59(5):479–486. [DOI] [PubMed] [Google Scholar]
- 76.Tversky A, Kahneman D. The framing of decisions and the psychology of choice. Science. 1981;211(4481):453–458. [DOI] [PubMed] [Google Scholar]


