Abstract
Patient: Male, 56
Final Diagnosis: Right heart failure due to pulmonary embolism
Symptoms: Syncope
Medication: —
Clinical Procedure: —
Specialty: Cardiology
Objective:
Unusual clinical course
Background:
Sildenafil is a pulmonary vasodilator and its efficacy has been well established in patients with group 1 pulmonary hypertension. There are no established guidelines regarding its use in acute right ventricle failure. In our experience, it can be used as an adjunctive therapy in acute right ventricle failure due to pulmonary embolism, to reduce right ventricle afterload and hence improve size and function of the right ventricle.
Case Report:
This is a case report where sildenafil was used as a rescue agent to achieve improvement in the right ventricle size and function in a case of acute onset massive pulmonary embolism with acute right ventricle failure in the scenario where systemic thrombolytic therapy was contraindicated.
Conclusions:
Improvement of right ventricle size and function was achieved using phosphodiesterase-5 Inhibitors in a case of acute right ventricle failure due to acute massive pulmonary embolism. There are no established guidelines regarding this clinical approach, however, given its efficacy in this case as adjunctive therapy in treatment of acute right ventricle, larger studies are needed to further establish its utility.
MeSH Keywords: Phosphodiesterase Inhibitors; Pulmonary Embolism; Ventricular Dysfunction, Right
Background
Phosphodiesterase-5 (PDE5) inhibitors are potent pulmonary vasodilators and are used frequently in patients with group 1 pulmonary hypertension [1]. They inhibit the metabolism of cyclic guanosine monophosphate (cGMP) and potentiate vasodilatory effects of natriuretic peptides and nitric oxide. Their role is well established in hypertrophied right ventricles but there are no established guidelines regarding their use in new onset acute right ventricle failure [2,3]. We present a case of saddle pulmonary embolism with acute right ventricle failure in a patient who underwent surgery recently and thus could not receive thrombolytic therapy. Sildenafil (a PDE inhibitor) was used as a rescue agent to achieve improvement of right ventricular size and function.
Case Report
A 56-year-old male presented to the emergency department of our hospital due to sudden onset shortness of breath and an episode of syncope while walking around inside his house. He underwent robotic assisted laparoscopic prostatectomy for prostate carcinoma, 5 days prior to his presentation to the Emergency Department. His post-operative course in the hospital was uneventful. In the emergency department, his blood pressure was 94/54 mmHg, heart rate 121 beats per minute, respiratory rate 20 breathes per minute, he was afebrile, and his oxygen saturation was 92% on 6 L per minute of oxygen via nasal cannula. Cardiac examination revealed S1S2, regular, tachycardic, no murmur/gallops/rubs. Respiratory examination revealed normal vesicular breath sounds bilaterally. He was noted to have asymmetrical left lower extremity edema. Electrocardiogram (ECG) revealed sinus tachycardia, no ST-T wave changes (Figure 1). Troponin was mildly elevated at 0.120 ng/mL (reference range: 0 to 0.020). Computed tomography angiography (CTA) of chest showed extensive bilateral pulmonary emboli, with a large clot burden in both main pulmonary arteries, evidence of acute right ventricular failure (Figure 2). Duplex venous scan showed acute left infra-popliteal deep vein thrombosis. Echocardiogram showed normal left ventricular ejection fraction of 60% to 65%, abnormal septal motion and flattening of interventricular septum, right ventricular systolic pressure of 49.7 mmHg, moderately dilated right ventricle, decreased right ventricle function, Tricuspid annular plane systolic excursion of 12.1 mm (normal 15 to 20 mm) (Figure 3A, 3B). As the majority of the clot burden was distal, it was not deemed amenable to surgical extraction as recent surgery was a major contraindication for thrombolysis. The patient was started on a heparin drip and inhaled nitric oxide at 20 ppm along with oral sildenafil 40 mg every 8 hours. The next day, the patient was stable hemodynamically and his inhaled nitric oxide was tapered off. Repeat echocardiogram 48 hours from initial presentation showed improved right ventricle size and function (Figure 4A, 4B). His right ventricular systolic pressure decreased to 22.4 mmHg and his tricuspid annular plane systolic excursion improved to 17.8 mm. We recommended that he continue sildenafil for the next month after discharge along with oral anticoagulation with a plan to follow-up as an outpatient. The patient gave written consent to treatment during his hospitalization. The patient and his family members were well-informed regarding the entire plan of care, and they were in agreement with the care plan.
Figure 1.

Electrocardiogram showing sinus tachycardia and left ventricular hypertrophy.
Figure 2.

Computed tomography (CT) angiogram of the chest showing bilateral pulmonary embolism.
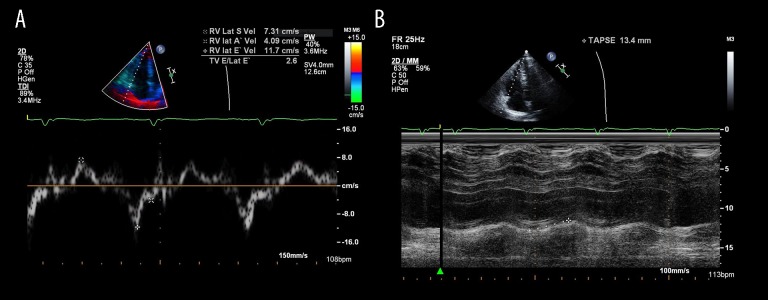
Figure 3.
(A) Tissue Doppler images of the right ventricle showing decreased right ventricular function. (B) Echocardiogram showing tricuspid annular plan systolic excursion of 13.4 mm reflecting decreased right ventricle function.
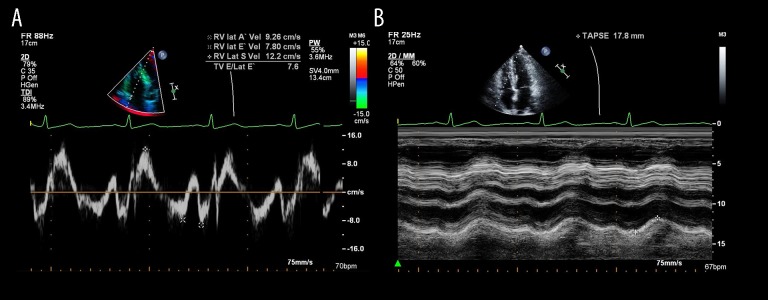
Figure 4.
(A) Tissue Doppler images of the right ventricle showing decreased right ventricular function. (B) Follow-up Transthoracic echocardiogram showing tricuspid annular plane systolic excursion of 17.8 mm reflecting improved right ventricle function.
Discussion
Acute pulmonary embolism is a potentially fatal condition and timely therapy is warranted to prevent recurrence and mortality [4]. Pulmonary embolism with sustained hypotension (systolic blood pressure <90 mmHg) for more than 15 minutes or evidence of shock is termed as massive pulmonary embolism while those with right ventricle dysfunction and borderline blood pressure are termed as sub-massive pulmonary embolism. Hemodynamically unstable/massive pulmonary embolism is an indication for systemic or catheter-based thrombolysis. Patients with sub-massive pulmonary embolism with a large clot burden, significant right ventricle enlargement and dysfunction; high requirement of oxygen, and persistent severe tachycardia can also be candidates for thrombolytic therapy [5]. In our case, the patient was not a candidate for thrombolytic therapy due to surgery just 5 days prior to presentation with pulmonary embolism. Risk of major bleeding is more than 50% in patients receiving thrombolysis within a week of surgery while it is up to 20% within 1 to 2 weeks after surgery [6]. Although surgical embolectomy is an alternative treatment modality in patients in whom thrombolytic have failed or contraindicated, the distal nature of the thrombus is not amenable to surgery, [7], and hence, it was not contemplated in our patient.
Right ventricle failure can occur due to increased preload, increased afterload, or reduced myocardial contractility. Sudden increase in right ventricle afterload is the primary cause of right ventricle failure in acute pulmonary embolism with a large clot burden [2]. Hence, measures to decrease afterload are the most effective strategies to improve right ventricle function and size. PDE5 inhibitors like sildenafil are well known to reduce pulmonary vascular resistance leading to better right ventricle contractility in patients with pulmonary hypertension [2]. In a study which included surgical specimens of 9 patients, it was concluded that PDE5 is not expressed in normal human right ventricles tissue but by virtue of upregulated mRNA and protein, contractility is increased in hypertrophied right ventricles. The role of increased cGMP and a decrease in right ventricle afterload was also been seen in cases of only hypertrophied right ventricles [3]. In another study, contrasting results were obtained in terms of favorable hemodynamic changes in anesthetized dogs (n=3) and rats with isolated perfused lung preparation. Intravenous sildenafil at a dose of 0.25 mg/kg or 1 mg/kg were found to reduce mean pulmonary artery pressure by 8 to 16 mmHg (P<0.05) in normal preexisting right ventricles [8]. In a case series (n=20) of patients with acute pulmonary embolism and right ventricle failure that were treated with sildenafil at 25 mg, 3 times a day as an adjunct to oral anticoagulation, it was found that there was no mortality in the median 9-month follow-up; and 65.2% of patients had no evidence of right heart strain after a median 101 days follow-up [9]. There have also been case reports describing improvement in hemodynamics with sildenafil in acute pulmonary embolism who had failed to improve with systemic or catheter directed thrombolytic therapy [10–12].
Our patient was not given any thrombolytic agent that would immediately dissolve the thrombus. He was given a heparin drip which helped to prevent further expansion, propagation, and recurrence of thrombus. We did use inhaled nitric oxide, a short-acting potent vasodilator, which has been shown to unload right ventricles in a critical care setting. It has been shown to improve pulmonary pressure and right ventricle contractility in acute right ventricle failure [13]. But we tapered off the inhaled nitric oxide rapidly in less than 24 hours, and it is known to have an extremely short half-life to have any kind of sustained effect. The only agent that was used continuously to reduce afterload was sildenafil. However, we should consider the very brief use of inhaled nitric oxide and possibly natural fibrinolysis as limiting factors. We did not consider using endothelin receptor inhibitors or the soluble guanylate cyclase stimulator riociguat, as they have not been proven to be safe in acute right ventricle dysfunction [2].
Conclusions
Sildenafil, a PDE5 inhibitor, is a potent pulmonary vasodilator and its efficacy has been well established in patients with group 1 pulmonary hypertension. In our experience, it can be used as an adjunctive therapy in acute right ventricle failure due to pulmonary embolism to reduce right ventricle after-load, and hence improve size and function of the right ventricle. There are animal studies, case series, and isolated case reports regarding the use of sildenafil in acute pulmonary embolism. Larger systematic studies are needed to further establish its role in acute right ventricle failure.
Footnotes
Conflict of interest
None.
References:
- 1.Pepke-Zaba J, Gilbert C, Collings L, Brown MC. Sildenafil improves health-related quality of life in patients with pulmonary arterial hypertension. Chest. 2008;133(1):183–89. doi: 10.1378/chest.07-0592. [DOI] [PubMed] [Google Scholar]
- 2.Ventetuolo CE, Klinger JR. Management of acute right ventricular failure in the intensive care unit. Ann Am Thorac Soc. 2014;11(5):811–22. doi: 10.1513/AnnalsATS.201312-446FR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagendran J, Archer SL, Soliman D, et al. Phosphodiesterase type 5 is highly expressed in the hypertrophied human right ventricle, and acute inhibition of phosphodiesterase type 5 improves contractility. Circulation. 2007;116:238–48. doi: 10.1161/CIRCULATIONAHA.106.655266. [DOI] [PubMed] [Google Scholar]
- 4.Tapson VF. Acute pulmonary embolism. N Engl J Med. 2008;358(10):1037–52. doi: 10.1056/NEJMra072753. [DOI] [PubMed] [Google Scholar]
- 5.Kearon C, Akl EA, Comerota AJ, Prandoni P. Antithrombotic therapy for VTE disease: Antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl.):e419S. doi: 10.1378/chest.11-2301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Condliffe R, Elliot CA, Hughes RJ, et al. Management dilemmas in acute pulmonary embolism. Thorax. 2014;69:174–80. doi: 10.1136/thoraxjnl-2013-204667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keeling WB, Leshnower BG, Lasajanak Y, et al. Midterm benefits of surgical pulmonary embolectomy for acute pulmonary embolus on right ventricular function. J Thorac Cardiovasc Surg. 2016;152(3):872–78. doi: 10.1016/j.jtcvs.2015.11.042. [DOI] [PubMed] [Google Scholar]
- 8.Dias-Junior CA, Souza-Costa DC, Zerbini T, et al. The effect of sildenafil on pulmonary embolism-induced oxidative stress and pulmonaryhypertension. Anesth Analg. 2005;101(1):115–20. doi: 10.1213/01.ANE.0000153499.10558.F3. [DOI] [PubMed] [Google Scholar]
- 9.Hall H, Orton C, Morza R, et al. Exploring the role of sildenafil in acute pulmonary embolism. Clin Surg. 2018;3:1963. [Google Scholar]
- 10.Ganiere V, Felhi F, Tagan D. Dramatic beneficial effects of sildenafil in recurrent massive pulmonary embolism. Intensive Care Med. 2006;32(3):452–54. doi: 10.1007/s00134-005-0058-5. [DOI] [PubMed] [Google Scholar]
- 11.Lewis GD, Bloch KD, Semigran MJ. Pulmonary thromboembolism superimposed on a congenital ventricular septal defect in a 50-year-old man inhaled nitric oxide and sildenafil to the rescue. Cardiol Rev. 2004;12(4):188–90. doi: 10.1097/01.crd.0000122635.12743.57. [DOI] [PubMed] [Google Scholar]
- 12.Galea M, Quiney N. Sildenafil in acute pulmonary embolism: Case report and review of the literature. Jornal of Intensive Care Society. 2009;10(1):44–45. [Google Scholar]
- 13.Bhorade S, Christenson J, O’Connor M, et al. Response to inhaled nitric oxide in patients with acute right heart syndrome. Am J Respir Crit Care Med. 1999;159:571–79. doi: 10.1164/ajrccm.159.2.9804127. [DOI] [PubMed] [Google Scholar]