Abstract
Hyperbaric oxygen therapy shares many characteristics with negative pressure wound therapy (NPWT) from mechanisms of action that are primary, but also adjunctive. Both modalities share parallel challenges as advanced wound management strategies.
Introduction
Wound healing methodologies can remain classically driven, but also have evolved with advances over time. One of the ongoing sea changing currents is the use of negative pressure wound therapies. In many ways negative pressure wound therapies and all their variants share similar mechanisms of active and challenges to their usages as we see in hyperbaric oxygen therapies.
Serendipity
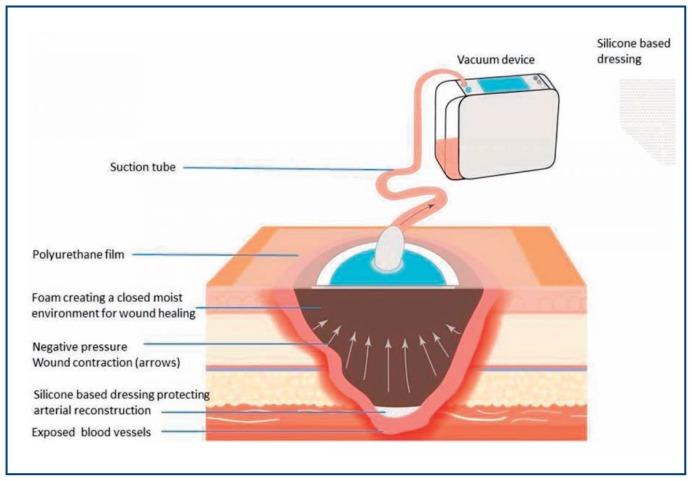
Many physical forces might be exploited to close a wound defect and promote healing. From the simple, classical such as mechanical tension with sutures to the more exotic like chemokines and even electricity in galvanotaxis. Negative pressure wound therapy can be seen in its beginnings as utilizing yet another physical force, vacuum, to close wounds. See Figure 1. However, very earlier on negative pressure wound therapy or vacuum assisted closure was also appreciated to have other helpful effects that went well beyond just pulling wound edges and walls together.1,2 As negative pressure methods began to be studied more findings suggesting more proposed mechanisms of action were found and put forth. From the cleansing action of pulling wound fluid through and out the wound,3 to generating helpful local neo-angiogenesis and cellular stimulation.4 There is always a bit of push and tug between what is believed to be at work, what is really known about what is at work, and what is just being discovered or disproven about various mechanisms of action. This parallels hyperbaric oxygen in many ways. Hyperbaric oxygen attempts to use a very special physical phenomena—pressure changes how oxygen is absorbed and distributed throughout the body. It achieves this—but like the effects of vacuum forces moving tissue planes only begin to describe the effects of negative pressure—hyperbaric oxygen also has other effects.
Figure 1.
Negative Pressure Wound Therapy
Source: Annals of Vascular Surgery
Organizing Selected Parallels Between NPWT and HBO2
Both NPWT and HBO2 have direct effects on tissues and both effect tissue flows in and out of the tissue beds being targeted by the modality. For example, both NPWT and HBO2 improve local flows through diminishing local edema resistance to enhanced flow and driving more perfusing flow into a targeted area.5,6
Both NPWT and HBO2 stimulate neoangiogenesis that can be seen on exam with better quality granulation tissue in the wounds.7 Both have a variety of mechanisms that are being studied to see why that granulation tissue and neoangiogenesis forms and how to optimize it from the specific microdeformation character of the negative pressure transmission medium to the timing and cycling of hyperbaric with periods of hyperoxemia and hypoxia.8 9
Both NPWT and HBO2 share some common practice pre-requisites for good use in wound healing. Similar to HBO2 negative pressure wound therapy has several guidelines exist for its use from focused topics such as for DFUs.10 to overall reviews.11 Akin to HBO2 its usages continue to evolve and now include topical applications for incisions. Similar to HBO2 these recommendations include good practice habits such as to clean and debride the wound of necrotic debris before using negative pressure. Both have specific precautions due to their mechanisms of action such as protecting underlying structures for NPWT or managing hypoglycemia in HBO2 This is true for HBO2 to be effective and especially true if both NPWT and HBO2 are to be combined for synergistic effects. Any infections should be controlled—even though both HBO2 and NPWT may have their own contributions to assist the body in clearing local tissue infections.
Both HBO2 and NPWT have prerequisites for safe uses. For negative pressure that means addressing if any suction force is being applied near bowel or vascular structures. For HBO2 the patient needs to be stabilized to tolerate effects of negative pressure and any risk factors such as diabetes mellitus or seizures are well controlled. Although both may have anti-infective properties, infection and necrosis should be brought under control with surgery and antibiotics. However, both modalities, especially with more negative pressure being combined with irrigation or direct drug delivery, may have more promise in treating active infections than originally thought.
Challenges for both NPWT and HBO2
However, although both modalities may be used on their own, there may be more benefits in using them together in synergy. But if high quality clinical data is lacking for randomized, prospective, well controlled and adequately powered studies for each of them in isolation—combining them compounds that problem. The question remains how much synergy is really reached in any combination and can these additional costs of treatment be justified in an increasingly data driven and value based medical economy?12
That said, many wound care practices attempt to take the available data and develop practice habits that introduce increasingly more sophisticated (and therefore expensive) advanced wound care treatments to either heal a higher percentage of wounds and ulcerations with fewer complications. If advanced modalities such as HBO2 or NPWT are not good matches for the patient’s problems, then this may also assist patients and clinicians to also consider more palliative care regimens that are safe and acceptable to the patient. Both NPWT and hyperbaric oxygen therapy can be brought to bear in this manner. NPWT can be continued throughout a patient’s HBO2 treatment regimen so long as the actual dressing is protected and that no component, such as an electrical based pump or any other flammable items, enter the chamber according to the practice requirements for that chamber.
It is ironic that medical care now exists in a sea of deceptively extensive EMR-based clinical data. It is deceptive in that although much more data is available—most EMR platforms focusing on compliance, documentation and capturing billing more effectively—aren’t easy to use to capture and organize clinical data for meaningful evidence based conclusions. So the day to day clinical experiential data is all there for anyone to analyze, but it still takes considerable human effort to capture it without omissions or duplications and organize it in a way such that biases can be controlled and meaningful evidence based conclusions can be reached in a way that are more generalizable for more clinicians to accept.
Conclusion
Both hyperbaric oxygen and NPWT have become advanced wound care methods with varying levels of evidence that deserve further study. Clinicians can incorporate them into their practices to better manage difficult wounds either alone or in combinations trying to capitalize upon synergy between them. However, ongoing clinical research is needed to better delineate who gets the most value out of these advanced modalities safely and effectively and in manners that merely increase the cost of care for patients. The costs for patients may also be logistical and may also help patients realize that such treatments are not a good match for their particular situation such that other treatment regimens can be pursued. Over time it is hoped that clinical data registries growing out of evolving EMRs will help all make more evidence-based decisions for utilizing both hyperbaric oxygen treatment and negative pressure and continue to explore how they might be used together.
Footnotes
John P. Kirby MD, FACS, is the Director of Wound Healing Programs, Associate Professor of Surgery, Section of Acute and Critical Care Surgery, at Washington University School of Medicine, Barnes-Jewish Hospital, in St. Louis, Missouri.
Contact: kirbyj@wustl.edu
Disclosure
None reported.
References
- 1.Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997;38:553–562. doi: 10.1097/00000637-199706000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997;38:563–577. [PubMed] [Google Scholar]
- 3.Stannard JP, Volgas D, Stewart R, McGwin G, Alonso JE. Negative pressure wound therapy after severe open fractures: a prospective randomized study. J Orthop Trauma. 2009;23:552–557. doi: 10.1097/BOT.0b013e3181a2e2b6. [DOI] [PubMed] [Google Scholar]
- 4.Birke-Sorensen H, Malmsjo M, Rome P, et al. Evidence-based recommendations for negative pressure wound therapy: treatment variables (pressure levels, wound filler and contact layer): steps towards an international consensus. J Plast Reconstr Aesthet Surg. 2011;64:S1–16. doi: 10.1016/j.bjps.2011.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Vig S, Dowsett C, Berg L, et al. Evidence-based recommendations for the use of negative pressure wound therapy in chronic wounds: steps towards an international. 614:73–80. doi: 10.1016/j.jtv.2011.07.002. [DOI] [PubMed] [Google Scholar]; J Tissue Viability. 2011;20(Suppl 1):S1–18. doi: 10.1016/j.jtv.2011.07.002. [DOI] [PubMed] [Google Scholar]
- 6.Hunt TK, Aslam RS, Jussain Z, Beckert S. Lactate, with oxygen, incities angiogenesis. Ado Exp Med Biol. 2008 doi: 10.1007/978-0-387-74911-2_9. [DOI] [PubMed] [Google Scholar]
- 7.Huang C, Leavitt T, Bayer LR, Orgill DP. Effect of negative pressure wound therapy on wound healing. Curr Probl Surg. 2014;51:301–31. doi: 10.1067/j.cpsurg.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 8.Erba P, Ogawa R, Ackermann M, et al. Angiogenesis in wounds treated by microdeformational wound therapy. Ann Surg. 2011;253:402–409. doi: 10.1097/SLA.0b013e31820563a8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hopf HW, Gibson JJ, Angeles AP, et al. Hyperoxia and angiogenesis. Wound Rep Regen. 2005;13(6):558–564. doi: 10.1111/j.1524-475X.2005.00078.x. [DOI] [PubMed] [Google Scholar]
- 10.Andros P, Armstrong D, Attinger C, Boulton A. Consensus Statement on Negative Pressure Wound Therapy for the Management of Diabetic Foot Wounds, Wounds, June 2006 Supplement. [PubMed] [Google Scholar]
- 11.Huang Chenyu, Leavitt Tripp, Bayer Lauren R, Orgill Dennis P. Impact of NPWT on Wound Healing surent problems in Surgery. 2014 Jul;51(7) doi: 10.1067/j.cpsurg.2014.04.001. [DOI] [PubMed] [Google Scholar]
- 12.Mouës CM, Heule F, Hovius SE. A review of topical negative pressure therapy in wound healing: sufficient evidence? Am J Surg. 2011;201:544–556. doi: 10.1016/j.amjsurg.2010.04.029. [DOI] [PubMed] [Google Scholar]