Abstract
Introduction:
Food supplements utilization is showing increasing trend among healthy as well as chronic disease population. Diabetes as a pandemic disease is treated by different interventions and traditional pharmacological treatment, but also utilization of natural products and food supplements (FS) are becoming important. Role of the pharmacist in diabetes management includes different interventions like counseling and recommendation of FS.
Aim:
To explore current trends in dietary supplements utilization among diabetic patients from the pharmacists’ perspective, pharmacists’ attitudes and knowledge about this group of products and suggest future directions related to this issue.
Methods:
We have analyzed pharmacists’ perception of FS utilization for diabetes and its complication treatment by conducting online survey. The survey was developed by authors based on research aim and published literature.
Results:
It has been found that 72% of patients with diabetes are purchasing different FS and that they are willing to pay between 5,0-15,0 EUR per visit for this products. Even in majority of cases pharmacists proactively advice patients about FS selection they identify need for specific education in this field in order to strengthen their competencies and competitiveness. Pharmacists also identified need for FS specially formulated and intended for blood glucose controls and most often diabetes complications and related conditions.
Conclusion:
This is the first study in this field conducted in Bosnia and Herzegovina suggesting further activities and research of this topic.
Keywords: dietary supplements, diabetes, pharmacists, complementary therapies
1. INTRODUCTION
Diabetes mellitus (DM) is pandemic disease recording continuous increase in patient population. IDF Diabetes Atlas estimated that in 2017 there were 451 million people with diabetes worldwide and it is expected that this number will increase to 693 million by 2045 (1). It is estimated by the diabetes associations in Bosnia and Herzegovina (B&H) that more than 220.000 people or 5,1% of population suffer from diabetes and majority are patients with type 2 diabetes (2). The main goal of diabetes treatment is to prevent or delay complications and maintain quality of life as stated in the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Consensus Report published in 2018 (3). This report is especially concerned with prevention of cardiovascular complications which are the major cause of mortality among patients with diabetes (4) but also other micro vascular complications including neuropathy, nephropathy, and retinopathy are life-threatening and negatively impacting quality of life (5). Patient centric care is a core of successful treatment and improvements of long term outcomes in chronic disease like diabetes. It is mainly reflected as partnership relation between patient and health care providers.
Community pharmacists are considered to be the most accessible health care professionals, as no appointments are required to see them, and to have the highest level of patient contact. As such, they are well placed to play a significant role in the care of patients with diabetes. There is significant evidence to support the role of pharmacists in providing a range of extended diabetes care services, from the screening to ongoing disease state management (6).
Diabetes treatment is multifactorial as a disease itself and includes non-pharmacological approach like physical activity, dietary restrictions and life-style changes as well as pharmacological approach. There are a numerous pharmacological treatment options for diabetes (7).
Food or dietary supplements are becoming more and more used over past 20 years and it becomes a matter of consumer interest (8-10). In the EU, food supplements are regulated as foods. They are intended to correct nutritional deficiencies, maintain an adequate intake of certain nutrients, or to support specific physiological functions. They are not medicinal products and as such cannot exert a pharmacological, immunological or metabolic action. Therefore their use is not intended to treat or prevent diseases in humans or to modify physiological functions (11).
Numerous food supplements have been used to treat diabetes and associated complications (12). Common reasons that food supplements are used include lowering blood glucose, lowering blood pressure, improving cholesterol, insulin resistance, neuropathy, and prevention of other diabetes-related complications. Food supplement use has been found to be relatively prevalent among patients with diabetes, with just over half reporting use (13). Patients with diabetes are more likely to use dietary supplements than people without diabetes (14) and some reports found that 22% to 67% patients with diabetes use food supplements (12).
It is important for health care practitioners not only to be aware of what dietary supplements their patients are taking, but also to understand how these supplements work and their possible side effects (15). Pharmacists can help patients to make informed and safe choices of dietary supplements.
2. AIM
Objective of our study was to assess pharmacists` attitudes on food supplements used among diabetes patients and experiences from everyday practice related to patients` preferences and consumption as well as pharmacists` recommendation and identified needs.
3. METHODS
We have designed survey containing sixteen questions regarding pharmacist practice and experience, pharmacy location, impressions and attitudes regarding use of food supplements among diabetes patients in everyday practice. The survey has been distributed to the e-mail addresses of 100 pharmacists at Public Institution Apoteke Sarajevo, as one of the biggest pharmacy chains in a country. Survey was distributed online by Microsoft Forms in October 2018 and was open for 15 days for answers collection. Collected results have been analyzed in MS Excel.
4. RESULTS
Out of 100 distributed 88 provided fully answered surveys. In regards to pharmacy location 33% are located in densely populated urban area, 26% in less inhabited suburban area, 21% in central pedestrian zone and 20% of respondents are working in a watchdog pharmacy.
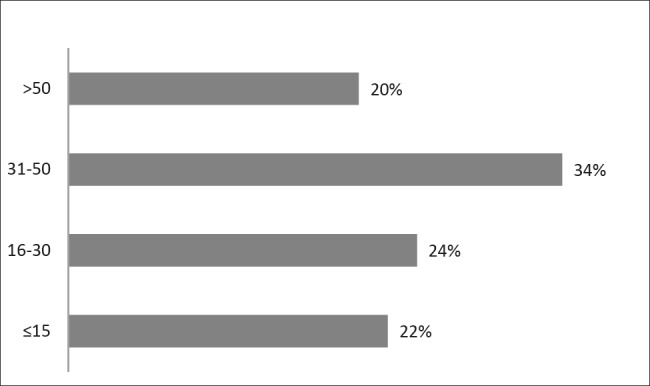
When it comes to pharmacy service users and visitors respondents stated that 1% are unemployed persons, 8% employed, 30% are pensioners and majority (30%) respond that mostly common users are mix of the first three categories. In majority of pharmacies number of patients/customers per day was between 100 and 200 and in majority of them 10 to 30 diabetes patients visit the pharmacy. Detailed overview of number of patients per day and diabetes patients are show in Figure 1 and Figure 2.
Figure 1. Number of patients visiting pharmacy per day.
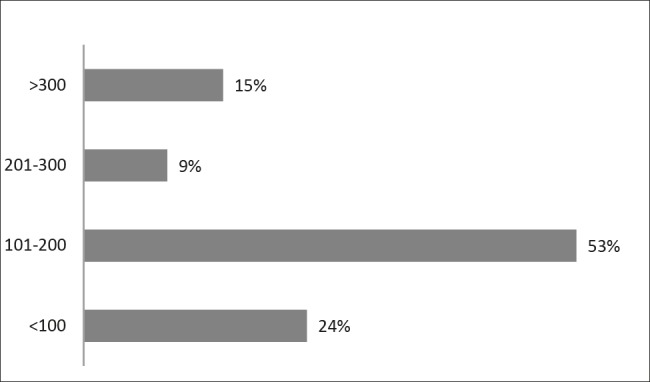
Figure 2. Number of patiets with diabetes per day.
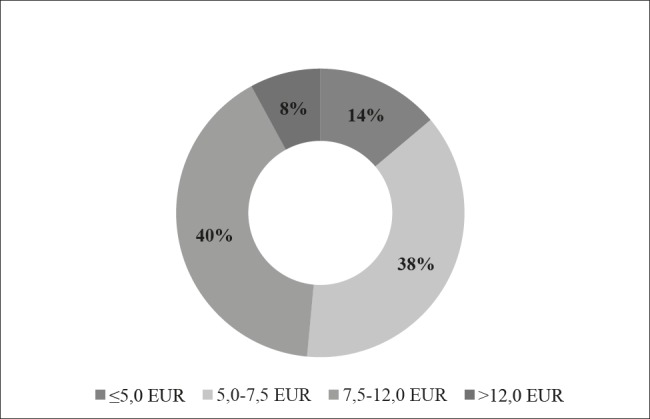
Based on experience of the pharmacist 73% of patients/consumers are spending between 5,0-15,0 EUR on food supplements per visit, 20% of them are spending up to 5,0 EUR and 9% spend more than 15,0 EUR for out of pocket purchasing of food supplements. These figures are corresponding to pharmacists` opinion about optimal prices of food supplements ranging between 5,0–15,0 EUR per pack as showed in Figure 3 in more details.
Figure 3. Optimal price of food supplement by pharmacists` opinion.
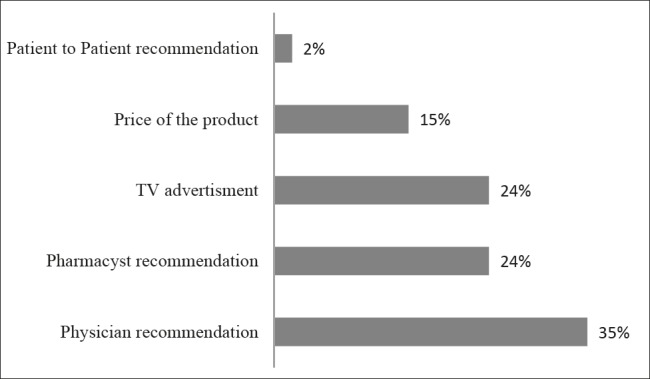
Pharmacists stated that 72% of patients with diabetes are buying different food supplements during the visit and 98% stated that they proactively advice and offer food supplements to diabetes patients, while only 2% of them reactively response to patient requests for purchasing food supplements. Majority of pharmacist stated that physician recommendation (35%) but also pharmacist recommendation (24%) have the major impact on selection and patients` willingness to use food supplements. Factors and level of influence on patients` choice of food supplements are presented in Figure 4.
Figure 4. Factors influencing patients` willingness to pruchase food supplements.
When asked if additional specialized education for pharmacists in the field of diabetes and use of food supplements is needed, 60% of pharmacists answered positively and 55% think that this would significantly increase competitiveness of the pharmacy they work in, while 27% are not sure if this would contribute to better pharmacy recognition.
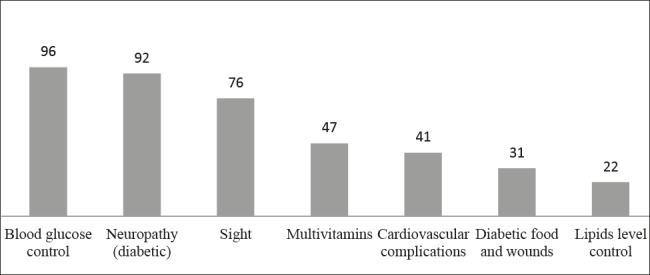
Analyzing pharmacists` attitude about which specially formulated food supplements for diabetes and its complications would be mostly recommended, highest frequency is found for products aimed to support blood glucose control, neuropathy and sight problems as presented in Figure 5.
Figure 5. Pharmacists` opinion about mostly needed food suplmenents for common diabetes related conditions.
5. DISCUSSION
Use of food supplements among healthy but also population with different chronic disease is growing trend (16). Results of a study conducted by Owen-Smit AA et al showed that 56.3% of respondents with chronic diseases reported daily use of food supplements (17). Numerous food supplements are used in diabetes and some of the reasons are a desire to avoid adverse effects of pharmaceuticals, the belief that supplements are “natural,” the realization that traditional treatments are unable to “cure” diseases, and the powerful suggestions of friends, family members, or coworkers (18, 19). In a study conducted by Odegard PS at all it has been found that patients with diabetes type 2 use food supplements twice more than patients with diabetes type 1 and that HbA1c was lower among those who use food supplements comparing to non-users (20). It has been found that patients with diabetes were 1,6 times more likely to use food supplements and alternative medicines compared to the general population (21). In our study this trend is recorded as well since two-thirds of diabetes patients are using or requesting food supplements during pharmacy visits. It has been also identified that willingness to pay for food supplements is relatively high representing 3% of average salary in Bosnia and Herzegovina.
Even there are still insufficient evidence to draw definitive conclusions about the efficacy of individual herbs and supplements for diabetes; however, they appear to be generally safe. Some of the products for blood glucose control are well examined with documented efficacy and safety like Coccinia indica, chromium and Gymnema sylvestre (22). One of the reasons for insufficient evidence is milder legislation comparing to the traditional medicines. This is especially important to be familiar with recent studies and evidences since majority of the pharmacist consider that products for blood glucose control are highly needed, followed by treatment of most common symptomatic conditions like diabetic neuropathy and visual impairment. Health care professionals dealing with diabetes or treating patients should be familiar with these products and provide evidence-based information to their patients, but they must also caution patients that long-term safety information is not available (23).
Pharmacists, as most accessible healthcare provider on primary level are well positioned to encourage patients to communicate openly about their use of dietary supplements, provide safety and efficacy information about supplements, and discourage use of dangerous or ineffective products (24). Considering our findings, it is obvious that almost 25%-50% of patients (visitors) to the pharmacies are patients with diabetes, presenting huge population for pharmacist proper intervention like counseling and medication management. Even some studies reported lack of open discussion and patient provision of information regarding food supplement use, in our sample this is not the case since patients are requesting such products and these are proactively suggested from the pharmacists` side. This could be the results of more traditional design of pharmacies with counter presence and lack of modern self-service pharmacies shops that can be found in Western countries.
Kwan D et al reported that majority of consumers and pharmacists agreed that pharmacists should be knowledgeable about natural products, such as food supplements, and felt that pharmacists should be able to manage interactions as well as identify and evaluate the variety of information available to help consumers make informed decisions (25). It is interesting that pharmacists in our sample found that physicians have higher impact on patients regarding food supplements use and selection, and made their suggestion equal to the effects of the media advertising. This could be the cultural reflection, since similar results are found in a study conducted by Catic T et al among patients reporting that 61.74% responders would consult doctor first, 20.33% would consult pharmacist in case that they do not have access to doctor due to schedule and long waiting and only 17.58% consider pharmacist as first choice for medical advice (26). There are a lot of possible community pharmacist interventions and services in order to improve diabetes treatment outcomes published in developed, but also developing countries (6). The findings from systematic review conducted by Pousinho S et al clearly support the involvement of pharmacists as members of health care teams in the management of patients with type 2 diabetes (27). Beside treatment outcomes, overall positive impact on diabetes management and health care system are recognized especially in case of systematically educated pharmacists who could perform group education for diabetes patients (28). In order to provide full service to the diabetes patients, pharmacist should be well educated and familiar with disease course, available treatment options and provide evidence-based information about food supplements products to the patients. As stated by the respondents, additional special education regarding diabetes of the community pharmacists is needed. Lack of pharmacists` sufficient knowledge about food supplements has been recognized globally as reported in one systematic review (29), especially taking into the consideration that proper and precise information about effectiveness, safety and potential interactions should be provided by the pharmacists. There is also and ethical issue rose about knowledge to provide accurate information and counseling service to the patients as well as issues concerning pharmacist influence on consumer preferences and profit driven sales (30).
The major lack of our study could be the small sample, but taking into the consideration that Sarajevo is a capital that can reflect overall attitudes among pharmacists, we found these results interesting as a screenshot of the current practices and basic for further research on this topic.
6. CONCLUSION
This is the first study conducted on food supplements attitudes in Bosnia and Herzegovina specially focusing on diabetes. Our findings suggest that there is a growing trend in food supplements utilization among patients with diabetes but also in other health conditions and that patient are willing to use such products as supplement to the traditional pharmacological treatments willing to spend substantial amount of out of pocket money. We also found that pharmacist are aware of existence of such products but found important to have specially designed products for blood glucose reduction and supplementary treatment of mostly common diabetic complications. Additional education specially designed for diabetes treatment options and food supplements should be provided to the pharmacists in order to increase their competencies and services provided to this population.
Author’s contribution:
Each author gave substantial contributions to the conception or design of the work in acquisition, analysis, or interpretation of data for the work. Each author had a part in article preparing for drafting or revising it critically for important intellectual content, and each author gave final approval of the version to be published and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflicts of interest:
There are no conflicts of interest.
Declaration of patient consent:
The authors certify that they have obtained all appropriate patient consent forms
Financial support and sponsorship:
Nil.
REFERENCES
- 1.Cho NH, Shaw JE, Karuranga S, Huang Y, da Rocha Fernandes JD, Ohlrogge AW, Malanda B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–281. doi: 10.1016/j.diabres.2018.02.023. [DOI] [PubMed] [Google Scholar]
- 2.Catic T, Lekic L, Zah V, Tabakovic V. Budget Impact of Introducing Linagliptin into Bosnia and Herzegovina Health Insurance Drug Reimbursement List in 2016-2018. Mater Sociomed. 2017 Sep;29(3):176–181. doi: 10.5455/msm.2017.29.176-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of Hyperglycemia in Type 2 Diabetes, 2018. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2018;41(12):2669–2701. doi: 10.2337/dci18-0033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leon BM, Maddox TM. Diabetes and cardiovascular disease: Epidemiology, biological mechanisms, treatment recommendations and future research. World J Diabetes. 2015;6(13):1246–1258. doi: 10.4239/wjd.v6.i13.1246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Papatheodorou K, Banach M, Bekiari E, Rizzo M, Edmonds M. Complications of Diabetes 2017. J Diabetes Res. 2018;2018:3086167. doi: 10.1155/2018/3086167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hughes JD, Wibowo Y, Sunderland B, Hoti K. The role of the pharmacist in the management of type 2 diabetes: current insights and future directions. Integr Pharm Res Pract. 2017;6:15–27. doi: 10.2147/IPRP.S103783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chamberlain JJ, Herman WH, Leal S, Rhinehart AS, Shubrook JH, Skolnik N, et al. Pharmacologic Therapy for Type 2 Diabetes: Synopsis of the 2017 American Diabetes Association Standards of Medical Care in Diabetes. Ann Intern Med. 2017;166:572–578. doi: 10.7326/M16-2937. [DOI] [PubMed] [Google Scholar]
- 8.Sirico F, Miressi S, Castaldo C, Spera R, Montagnani S, Di Meglio F, et al. Habits and beliefs related to food supplements: Results of a survey among Italian students of different education fields and levels. PLoS One. 2018;13(1):e0191424. doi: 10.1371/journal.pone.0191424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.O’Brien SK, Malacova E, Sherriff JL, Black LJ. The Prevalence and Predictors of Dietary Supplement Use in the Australian Population. Nutrients. 2017;9(10):1154. doi: 10.3390/nu9101154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kantor ED, Rehm CD, Du M, White E, Giovannucci EL. Trends in dietary supplement use among US adults from 1999-2012. JAMA Intern. Med. 2016;316:1464–1474. doi: 10.1001/jama.2016.14403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.European Food Safety Authority. [01 January 2019]. https://www.efsa.europa.eu/en/topics/topic/food-supplements/
- 12.Shane-McWhorter L. Dietary supplements for diabetes are decidedly popular: Help your patients decide. Diabetes Spectr. 2013;26(4):259–266. [Google Scholar]
- 13.Zablocka-Slowinska K, Dzielska E, Gryszkin I, Grajeta H. Dietary supplements during diabetes therapy and the potential risk of interactions. Adv Clin Exp Med. 2014;23(6):939–946. doi: 10.17219/acem/37348. [DOI] [PubMed] [Google Scholar]
- 14.American Diabetes Association. Herbs, supplements and alternative medicines. [01 January 2019]. www.diabetes.org/living-with-diabetes/treatment-and-care/medication/other-treatments/herbs-supplements-and-alternative-medicines/
- 15.Campbell AP. Diabetes and Dietary Supplements. Clinical Diabetes. 2010;28(1):35–39. [Google Scholar]
- 16.CRN. 2017 CRN Consumer Survey on Dietary Supplements. [03 January 2019]. https://www.crnusa.org/newsroom/dietary-supplement-usage-increases-says-new-survey.
- 17.Owen-Smith AA, Rand C, Smith DH, Tom JO, Laws R, Waterbury A, Vollmer WM. Use of select dietary supplements among individuals with diabetes or atherosclerotic cardiovascular disease. J Altern Complem Med. 2014;19(2):55–63. [Google Scholar]
- 18.Nahin RL, Byrd-Clark D, Stussman BJ, Kalyanaraman N. Disease severity is associated with the use of complementary medicine to treat or manage type-2 diabetes: data from the 2002 and 2007 National Health Interview Survey. BMC Complement Altern Med. 2012;12:193. doi: 10.1186/1472-6882-12-193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bin YS, Kiat H. Prevalence of dietary supplement use in patients with proven or suspected cardiovascular disease. Evid Based Complement Alternat Med. 2010;2011:632829. doi: 10.1155/2011/632829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Odegard PS, Janci MM, Foeppel MP, Beach JR, Trence DL. Prevalence and Correlates of Dietary Supplement Use in Individuals With Diabetes Mellitus at an Academic Diabetes Care Clinic. The Diabetes Educator. 2011;37(3):419–425. doi: 10.1177/0145721711401668. [DOI] [PubMed] [Google Scholar]
- 21.Egede LE, Ye X, Zheng D, Silverstein MD. The prevalence and pattern of complementary and alternative medicine use in individuals with diabetes. Diabetes Care. 2002 Feb;25(2):324–329. doi: 10.2337/diacare.25.2.324. [DOI] [PubMed] [Google Scholar]
- 22.Yeh GY, Eisenberg DM, Kaptchuk TJ, Phillips RS. Systematic Review of Herbs and Dietary Supplements for Glycemic Control in Diabetes. Diabetes Care. 2003;26(4):1277–1212. doi: 10.2337/diacare.26.4.1277. [DOI] [PubMed] [Google Scholar]
- 23.Shane-McWhorter L. Dietary Supplements for Diabetes Are Decidedly Popular: Help Your Patients Decide. Diabetes Spectrum. 2013;26(4):259–266. [Google Scholar]
- 24.Geil P, Shane-McWhorter L. Dietary Supplements in the Management of Diabetes: Potential Risks and Benefits. Journal of the Academy of Nutrition and Dietetics. 2008;108(4):S59–S65. doi: 10.1016/j.jada.2008.01.020. [DOI] [PubMed] [Google Scholar]
- 25.Kwan D, Boon HS, Hirschkorn K, et al. Exploring consumer and pharmacist views on the professional role of the pharmacist with respect to natural health products: a study of focus groups. BMC Complement Altern Med. 2008;8:40. doi: 10.1186/1472-6882-8-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Catic T, Jusufovic FI, Tabakovic V. Patients perception of community pharmacist in Bosnia and Herzegovina. Mater Sociomed. 2013;25(3):206–209. doi: 10.5455/msm.2013.25.206-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Pousinho S, Morgado M, Falcão A, Alves G. Pharmacist Interventions in the Management of Type 2 Diabetes Mellitus: A Systematic Review of Randomized Controlled Trials. J Manag Care Spec Pharm. 2016;22(5):493–515. doi: 10.18553/jmcp.2016.22.5.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Berg J, Dodd SA, Dodd S. The role of a community pharmacist in diabetes education. JEMDSA. 2009;14(3):148–150. [Google Scholar]
- 29.Waddington F, Naunton M, Kyle G, Thomas J, Cooper G, Waddington A. A systematic review of community pharmacist therapeutic knowledge of dietary supplements. Int J Clin Pharm. 2015;37(3):439–446. doi: 10.1007/s11096-015-0092-5. [DOI] [PubMed] [Google Scholar]
- 30.Boon H, Hirschkorn K, Griener G, Cali M. The ethics of dietary supplements and natural health products in pharmacy practice: a systematic documentary analysis. Int J Pharm Pract. 2009;17(1):31–38. doi: 10.1211/ijpp.17.1.0005. [DOI] [PMC free article] [PubMed] [Google Scholar]


