Abstract
Objective:
Behavioral economic theory suggests that a reduction in alcohol use is most likely when there is an increase in rewarding substance-free activities. Anxiety has also been linked to heavy drinking, and strategies to reduce anxiety may enhance alcohol interventions. The goal of this two-site randomized controlled clinical trial was to evaluate the efficacy of a brief alcohol intervention that was supplemented with either a behavioral economic Substance-Free Activity Session (SFAS) or a relaxation training (RT) session.
Method:
Participants were 393 college students (61% female, Mean age = 18.77 years) who reported two or more past-month heavy drinking episodes. Participants were randomized to one of three conditions: 1) assessment, 2) alcohol brief motivational intervention (BMI) plus SFAS or 3) BMI plus RT. Both treatment conditions included two in-person sessions plus a phone booster session. Outcomes were evaluated 1, 6, 12, and 16 months post-intervention.
Results:
Generalized linear mixed models indicated that the combination of a BMI plus either the SFAS or RT was associated with significant reductions in alcohol use and problems across the 16-month follow-up compared to assessment only. There were no significant differences between the two active treatment conditions. Changes in proportional reinforcement from substance-related activities, and protective behavioral strategies mediated treatment effects.
Conclusion:
Two-session (plus booster) interventions that combine BMI and either substance-free activity enhancement or RT can result in enduring reductions in alcohol misuse among college drinkers.
Keywords: alcohol, behavioral economics, binge drinking, college, motivational interventions, substance-free reinforcement
Approximately 37% of college students report at least one heavy drinking episode (4/5 or more drinks in one occasion for a woman/man) in the past month (Hingson, Zha, & Smyth, 2017), and each year approximately 16% of college students drive under the influence of alcohol and 20% meet criteria for Alcohol Use Disorder (AUD). Heavy drinkers are also less engaged in academics during college, finish with lower grades, and are more likely to drop out than lighter drinkers (Jennison, 2004; Latvala et al., 2014; Singleton, 2007).
Brief Motivational Interventions (BMI) for College Drinking
BMIs have demonstrated success in reducing drinking across numerous clinical trials (Scott-Sheldon, Carey, Elliott, Garey, & Carey, 2014) and are identified as a Tier 1 prevention approach by the National Institute of Alcohol Abuse and Alcoholism (NIAAA, 2015). BMIs are delivered in a motivational interviewing style (Miller & Rollnick, 2013) and typically include peer-normative comparisons, personalized feedback on drinking patterns and associated risks, and goal-setting related to reducing drinking or associated harm (i.e., protective behavioral strategies; PBS). Although BMIs have been widely disseminated, several recent meta-analyses suggest that drinking and alcohol problem reductions are generally small to moderate and are often not maintained beyond 1-year follow-ups (Foxcroft et al., 2016; Tanner-Smith & Lipsey, 2015), leading to calls for new intervention elements to enhance response (Huh et al., 2015).
The modest overall response to BMI may be due in part to the limited focus of most BMIs, which generally target motivation to reduce drinking without addressing the underlying reasons for drinking (e.g., boredom, social facilitation, stress, lack of academic goals or future orientation), or providing alternative means of socializing or experiencing reward. Predictors of poor response to BMI include low levels of substance-free reinforcement (Murphy, Correia, Colby, & Vuchinich, 2005), poor self-regulation/impulsivity (Carey, Henson, Carey, & Maisto, 2007; Soltis et al., 2018), low future time orientation (Murphy et al., 2012a), elevated alcohol reinforcing efficacy (Murphy et al., 2015), and anxiety or depressive symptoms (Merrill, Reid, Carey, & Carey, 2014).
Behavioral Economic Supplement to Improve College Drinking Interventions
Given the promise, and limitations, of BMI there has been surprisingly little research aimed at enhancing these interventions with novel content to address the underlying factors that contribute to elevated motivation to drink (DeMartini, Fucito, & O’Malley, 2015; Turrisi et al., 2013). Behavioral economic research has demonstrated that substance use increases in contexts that are devoid of substance-free sources of reinforcement, and conversely, that substance use generally decreases if access to alternative reinforcers is increased (Bickel, Johnson, Koffarnus, MacKillop, & Murphy, 2014). Further, studies with teens and young adults have shown that reward deprivation is uniquely associated with alcohol use disorder symptoms (Joyner et al., 2016) and predicts poor response to brief alcohol interventions (Murphy et al., 2005).
Young adult heavy drinkers may under-engage in constructive alternatives to drinking because the benefits of activities such as studying or attending classes/internships may not be experienced until months or years into the future (e.g., graduating college, lucrative employment) (Murphy & Dennhardt, 2016). In contrast, alcohol use is associated with immediate reinforcement (e.g., stress reduction, social facilitation), particularly in the college environment where drinking is often a central element of socializing. Delay discounting refers to the extent to which delayed rewards lose value relative to immediate rewards, and individual differences in delay discounting and related measures of future orientation or self-regulation have shown consistent associations with substance abuse (Bickel et al., 2014; MacKillop et al., 2011; Murphy & Dockray, 2018), and predict poor treatment response (MacKillop & Kahler, 2009; Murphy, et al., 2012a). Laboratory research suggests that delay discounting may also be malleable and can be reduced by enhancing the salience of future rewards (Bickel et al., 2014; Daniel, Stanton, & Epstein, 2013) and providing feedback that helps individuals view the sum of their discrete choices as larger “molar” behavior patterns that are associated with delayed outcomes (Hofmeyr, Ainslie, Charlton, & Ross, 2011), yet translational research is needed to determine the clinical utility of these approaches to reduce delay discounting over time and in ways that stimulate salutary behavior change (Rung & Madden, 2018).
Murphy and colleagues (2012b) developed a one-session supplement to a standard alcohol BMI for college student heavy drinkers called the Substance-Free Activity Session (SFAS) using a sequential approach in which investigators drafted a manual and then modified it based on feedback from focus groups and an open series of pilot cases with heavy drinking college students (see Murphy et al., 2012b). The SFAS uses MI and personalized feedback to target the behavioral economic mechanisms of substance-free reinforcement and future orientation. Specifically, the SFAS attempts to increase the student’s commitment to patterns of substance-free activities and general degree of future orientation by asking about their goals for college and beyond, making the long-term benefits of those goals tangible, and by discussing the congruence between their recent patterns of time allocation to drinking versus other activity categories with those long-term goals. Depression and anxiety can interfere with goal-pursuit and increase the reinforcing value of alcohol so students with anxiety or depressive symptoms are provided with coping strategies.
A pilot trial (N = 82) administered a 50-minute SFAS session 1-week after a 50-minute alcohol BMI and found that participants in the BMI+SFAS condition reported larger reductions in alcohol-related problems compared to a BMI+Relaxation Training (RT) comparison condition matched for duration (2 sessions) and individual modality (Murphy et al., 2012a). Changes in alcohol problems were mediated by changes in PBS and self-regulation (Soltis et al., 2018). A second pilot trial (N = 97) reduced the length of the SFAS to 30 minutes so that it could be administered immediately after an abbreviated 30-minute BMI in a single 60-minute meeting (Yurasek, Dennhardt, & Murphy, 2015). The compressed BMI+SFAS session was associated with significant reductions in drinking and problems, but there were no significant differences relative to the active control condition (BMI+ alcohol and drug education).
The Current Study
The pilot studies reviewed above demonstrate the potential benefits of supplementing BMI with a session that targets behavioral economic mechanisms. Both pilot trials compared BMI+SFAS to BMI plus an active control (either alcohol and drug education or RT) to determine the extent to which the SFAS can enhance BMI, but there is a need to evaluate the SFAS with a larger sample and a longer follow-up period to establish efficacy above and beyond the standard BMI session plus an active control (RT). There is also a need to evaluate the BMI+SFAS relative to an assessment-only control condition to describe the treatment effects of the combined intervention above and beyond assessment reactivity, given that many universities do not offer BMI and might be interested in the absolute effects of BMI+SFAS. Thus, the current study randomly assigned participants to one of three conditions: 1) assessment, 2) BMI+RT or 3) BMI+SFAS in a two-site clinical trial that included 1, 6, 12, and 16-month follow-ups. We used the 50-minute BMI and SFAS sessions that were included in the first pilot project rather than the abbreviated 30-minute sessions of the second pilot due to observations by the clinicians and patterns of results that suggested that 30 minutes may not be adequate time to cover all components of the interventions. Based on previous research supporting the efficacy of BMIs, we hypothesized that both active interventions (BMI+SFAS and BMI+RT) would be associated with reductions in drinks per week and alcohol-related problems relative to assessment only. Consistent with the findings of Murphy et al. (2012a), we hypothesized that BMI+SFAS would be associated with greater treatment effects relative to BMI+RT. Finally, we investigated change in secondary intervention outcomes and potential mediators targeted by the BMI+SFAS (self-regulation, delay discounting, and proportion of reinforcement derived from substances) and by both the BMI+SFAS and BMI+RT (depression, anxiety, PBS).
Methods
Participants
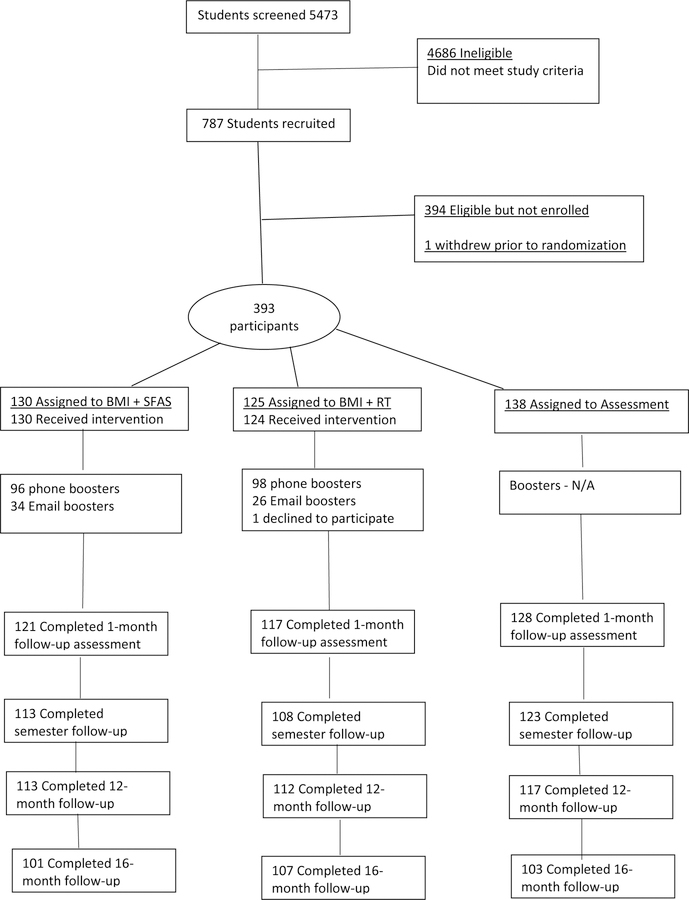
Participants were 393 undergraduate students from two large public universities in the United States who were recruited through classes and university-wide email solicitations. University one was located in a metropolitan area and university two was located in a smaller college town. The inclusion of the two sites resulted in a more heterogeneous and diverse sample of student drinkers. Students were eligible to participate if they were full-time first or second-year students, reported two or more past-month heavy drinking episodes (≥ 5/4 drinks on one occasion for men/women), and worked fewer than 20 hours per week. The limited employment criterion was included to select for “typical” college students who have time for potential increases in academic/extra-curricular activities. Seven hundred and eighty-seven students were eligible and 393 (50%) agreed to participate (See Figure 1). Of the 393 participants (61% women; Mean age = 18.77, SD = 1.06), 85.2% self-identified as White/European American, 10.9% as Black/African-American, 5.9% as Hispanic/Latino, 1.8% as Asian, and 1.8% as Native American. Participants drank an average of 16.76 (SD = 11.97) drinks per week and reported experiencing 13.05 (SD = 7.89) alcohol-related problems at baseline. Participants received $25 for completing the baseline assessment, $25 for completing the intervention sessions, $25 for completing each of the first two follow-up assessments and $40 for completing each of the last two follow-up assessments. Reports were provided yearly to the Data Safety and Monitoring Board established for this study; no adverse events were reported. This study is registered with clinicaltrials.gov.
Figure 1.
Flow chart illustrating recruitment, intervention assignment, and follow-up assessment.
Primary Drinking Measures
Participants estimated the total number of standard drinks they consumed each day during a typical week in the past month using the Daily Drinking Questionnaire (DDQ; Collins, Parks, & Marlatt, 1985). The DDQ is used frequently with college students and is a reliable measure that is highly correlated with self-monitored drinking reports (Kivlahan, Marlatt, Fromme, Coppel, & Williams, 1990). The Young Adult Alcohol Consequences Questionnaire (YAACQ; Read, Merrill, Kahler, & Strong, 2007) asks participants to indicate whether or not they have experienced problems related to their alcohol use in the past 6 months using a list of 48 statements (e.g., “While drinking, I have said or done embarrassing things”; “I have neglected my obligations to family, work, or school because of drinking.”). The YAACQ has demonstrated good internal consistency (α=.90 in the current study) and predictive validity (Read et al., 2007).
Secondary Outcome Measures and Mediators
Depression, Anxiety, and Stress Scales (DASS).
The DASS (Lovibond & Lovibond, 1995) is a self-report survey designed to measure symptoms of depression, anxiety and stress. Each of the three DASS scales contains 7 items and participants are asked to use 4-point scales to rate the extent to which they have experienced each emotional state over the past week; scores for depression, anxiety and stress are calculated by summing the scores. We examined change in Depression (α=.89) and Anxiety (α =.73) scales as secondary outcomes.
Adolescent Reinforcement Survey-Substance Use Version (ARSS-SUV).
The ARSS-SUV (Murphy et al., 2005) is a measure of reinforcement from 45 substance-related and substance-free activities in the previous month (e.g., socializing with friends, relaxing at home). For each activity, the participant makes separate frequency and enjoyment rating for times they participated in the activity with and without the use of alcohol or drugs. Frequency and enjoyment ratings are made with 5-point Likert scales (0–4); frequency ratings range from 0 (zero times per week) to 4 (more than once per day), and enjoyment ratings range from 0 (unpleasant or neutral) to 4 (extremely pleasant). Cross-product scores that reflect reinforcement derived from the substance-erelated or substance free activity are created by multiplying the frequency and enjoyment ratings. We examined the reinforcement ratio score, i.e., substance-related total / (substance-free total + substance-related total), which measures the proportion of total reinforcement related to substance use. The reinforcement ratio demonstrates good reliability and validity among college student drinkers (Hallgren, Greenfield, & Ladd, 2016).
Delay Discounting Task (DDT).
Delayed reward discounting was assessed using a 60-item version of the DDT (Amlung & MacKillop, 2011). Participants are asked to choose between a series of hypothetical smaller, immediate versus larger, delayed rewards (e.g. Would you prefer $30 today, or $100 in 6 months?). The items featured varying amounts and delays, with each choice contributing to the participant’s overall discounting rate parameter (k). This parameter was computed using a Graphpad Prism macro that fit the participant choices to a hyperbolic equation. Higher k values reflect a greater proportion of choices for the smaller immediate monetary amounts. Hypothetical money choices provide reliable and valid estimates of discounting rates (Madden, Begotka, Raiff, & Kastern, 2003).
Short Self-Regulation Questionnaire (SSRQ).
Participants rate statements related to self-regulation (e.g. “I feel bad when I don’t meet my goals” and “I enjoy a routine and like things to stay the same,”) on a 5-point Likert-type scale ranging from 1 (strongly disagree) to 5 (strongly agree). Scores for each item are summed to create a total self-regulation score (α=.93) with higher scores indicating better self-regulation (Carey, Neal, & Collins, 2004). The SSRQ has demonstrated strong construct validity among young adult drinkers (Carey et al., 2004).
The Protective Behavioral Strategies Scale
(PBSS; Martens, Pedersen, LaBrie, Ferrier, & Cimini, 2007). Participants indicate how often they use each protective strategy when drinking alcohol using a 6-point scale ranging from 1 (never) to 6 (always). Examples of strategies include “use a designated driver,” and “avoid drinking games.” The PBSS has strong convergent and incremental validity (Martens et al., 2007) and internal consistency (α=.82 in this sample).
Procedure
All procedures were approved by the University Institutional Review Boards. All sessions occurred in a private, on-campus laboratory space. All assessment and intervention sessions occurred during weeks 4 – 10 over four consecutive fall semesters; this timing ensured that the baseline assessment did not include the summer and that the 1-month follow-up was completed prior to final exams. After providing informed consent participants were randomized to one of three conditions: 1) assessment-only, 2) BMI+RT or 3) BMI+SFAS, stratified by site, gender, and year in school. At the conclusion of the baseline assessment (approximately 50 minutes) participants assigned to conditions 2 or 3 completed a 50-minute individual BMI session. One week later, the participants completed a 50-minute individual RT or SFAS session with the same clinician. Clinicians were blind to the second session to which the participant had been assigned until after they completed the BMI. Participants completed in-person follow-up assessments one-month post-intervention, and the booster session was completed in January immediately prior to the spring semester. The 6, 12, and 16-month follow-ups occurred at the same point in the semester as the baseline assessment session so that outcomes were not influenced by the academic calendar (Del Boca, Darkes, Greenbaum, & Goldman, 2004). Additionally, the baseline assessments were conducted at least 4 weeks into the semester and the follow-up questionnaires asked about past-month use alcohol use and problems. Thus, the assessment windows excluded winter and summer break alcohol use, which can be uncharacteristic (Del Boca et al., 2004). Follow-up assessments were conducted by an RA who was blind to treatment condition.
Clinician training and supervision.
Clinicians were graduate students in clinical/counseling psychology who completed over 20 hours of training in MI that included readings, training DVDs, and role-plays. Clinicians completed similar training in the SFAS and RT sessions and received supervision (and regular coding/review of session tapes) by study investigators.
BMI.
The BMI session was modeled after the Brief Alcohol Screening and Intervention for College Students model (BASICS; Dimeff, 1999; Murphy et al., 2012a). It included an alcohol use decisional balance exercise and the following personalized alcohol-related feedback: (a) normative feedback on drinking beliefs and weekly drinking compared to gender-specific national norms, (b) an estimate of the student’s peak blood alcohol content (BAC) in the past month, (c) a list of the alcohol-related problems that the student reported experiencing in the past month, (d) money spent on alcohol, and (e) calories consumed from alcohol. Participants also received information on PBS. Clinicians utilized MI style to discuss the feedback and to encourage the student to set specific goals related to drinking or PBS based on their interest (Miller & Rollnick, 2013).
SFAS.
The SFAS is designed to increase the salience of the student’s academic and career goals, to highlight the connection between their current patterns of behavior (e.g., drinking, attending class) and the attainment of these goals, and to increase future orientation and engagement in rewarding alternatives to substance use (Murphy, et al., 2012a; Murphy, et al., 2012b). The session is conducted in MI style and begins with an open-ended discussion of the students’ college and career goals, motives for pursuing stated goals, and how alcohol could interfere with successful goal completion. The clinician presents information on average income differences for those earning a high school diploma versus a 4-year college degree, a graph illustrating predicted future income differences based on college GPA, and a graph showing that average college GPA decreases as a function of time spent drinking, and increases with more time spent attending class and studying. Personalized feedback elements include: a) the requirements (grades, internships, graduate school) for the student’s major and/or intended career or information on how to choose a major or career, b) a list of extracurricular and community activities/internships tailored to the student’s goals, c) a graph of the amount of time the student spent engaged in various activities (e.g. studying, exercise, drinking/drug use) in the past month, d) for students reporting anxiety, stress, or depressive symptoms (which can interfere with reward pursuit), information on these symptoms and possible adaptive coping responses, and e) a list of substance-free recreational or leisure activities that the student reported enjoying currently and/or those activities they thought they would enjoy. Participants also completed an exercise where they rated the current and future value of their common activities (e.g., going to a party with friends or attending classes) and graphed those values to illustrate that many activities with low current value have high future value. Finally, students used a goal-setting worksheet to set both academic/professional and personal goals, received a planner to assist with time management (along with suggestions for similar smart-phone apps), and a list of tips for enhancing self-regulation and for succeeding in college.
Relaxation training (RT) session.
Individual RT was chosen to control for clinician contact time associated with the SFAS and because it is a common alcohol treatment element and general wellness strategy (Klajner, Hartman, & Sobell, 1984; Murphy et al., 2012a). The same clinician who conducted the BMI during the week prior conducted the RT session and established the credibility of the session by providing the student with the rationale that drinking is often used to relieve stress related to college, and this session would provide them with skills to manage stress. The clinician led the student through a diaphragmatic breathing exercise, followed by a progressive muscle RT protocol, and a discussion of stress management strategies. Students were then asked about their reaction to the relaxation techniques and were provided with RT handouts.
Booster sessions.
Students in the BMI+SFAS and BMI+RT conditions completed a 10–15-minute booster phone call one week prior to the start of the next semester after their intervention (i.e., the spring semester). Across both conditions, if students were unable to complete the booster via phone, the booster content was sent via email. During the SFAS booster session, the clinician reviewed the goals the student had set at the end of the SFAS session and asked about their progress and plan to achieve these goals going forward. If a student reported a change in their interests, the student set new goals and clinician sent updated SFAS feedback with information specific to the major and/or career. In the RT booster session, the clinician reviewed the stress management techniques discussed in the initial session, the student’s progress in implementing these strategies, addressed barriers to use, and provided additional stress management strategies.
Data Analysis Plan
All variables were checked for outliers prior to analysis. Outliers greater than 3.29 SDs above or below the mean were recoded to one unit above or below the highest or lowest non-outlier value (Tabachnick & Fidell, 2012). We used generalized linear mixed models with a negative binomial distribution and log link function to evaluate change in the primary drinking outcomes (drinks per week and alcohol-related problems) due to the data being skewed and zero-inflated and general linear mixed models with a normal distribution and identify link function to evaluate change in secondary outcomes (depression, anxiety, protective behavioral strategies, self-regulation, delay discounting, and reinforcement ratio) across the four follow-up time points (1, 6, 12, and 16-month follow-ups) as a function of time and treatment condition. Time was centered at the 1-month follow-up (time=0 at 1-month follow-up) and baseline levels of the outcome were included as a covariate. Random slope effects (i.e., time-by-treatment interactions) were not significant and eliminated from the final reported models. Thus, final models were estimated using a compound symmetry covariance matrix with random intercepts and linear effects of time. Gender, ethnicity, and Greek status were included as covariates due to their association with drinking level and the possibility of differential treatment response (Huh et al., 2015). Site was also included as a covariate to control for differences in student characteristics and response rates across sites. Models were run with the following planned contrasts: Active treatment versus assessment, BMI+SFAS versus assessment, BMI+RT versus assessment, and BMI+SFAS versus BMI+RT.
Mediators were tested in separate models and included PBS, depression, anxiety, self-regulation, and reinforcement-ratio. These mediators were selected based on the fact that they are related to increased alcohol use and/or poor intervention response and are theoretically targeted in the SFAS intervention (Murphy et al., 2012). Multilevel (mixed) mediation models were estimated using the product of coefficients approach (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). This approach provides an estimate of the mediated effect by multiplying the regression of the mediator on the independent variable (the “a-path”), and the regression of the outcome on the mediator (the “b-path”), with the independent variable included in the model (MacKinnon, 2008). The 95% confidence intervals for the mediated effects were estimated using Rmediation (Tofighi & MacKinnon, 2011).
All models were estimated in Mplus version 8.1 (Muthén & Muthén, 1998–2018) with maximum likelihood estimation with robust standard errors to accommodate missing data. Missing not at random models were also estimated to determine whether the models were robust to the missing at random assumption of maximum likelihood estimation (Enders, 2011). The robust maximum likelihood estimator (MLR estimator in Mplus) was used to adjust the standard errors for clustering within clinician. For most outcomes, the effect of clinician explained less than 3% of the variance in outcomes.
Results
Evaluation of Internal Validity
Content integrity coding.
A random subset of BMI sessions (n = 12), SFAS sessions (n = 6), and RT sessions (n = 8) (5% of the total sessions in each category) were reviewed by one of four masters-level clinicians. Sessions were reviewed using an intervention adherence protocol used in several previous BMI studies (Murphy, et al., 2012a). Each of the components on the protocol was rated as a 1 “Did it poorly or didn’t do it but should have,” 2 “Meets expectations,” or 3 “Above Expectations”. For the 24 main components of the BMI protocol the mean rating was 1.94 (SD = .23, Mdn = 2.00), with 88% of the components rated as meeting or exceeding expectations. The SFAS session was rated for inclusion of the 23 key components. The average rating was 1.85 (SD = .42), Mdn = 2.00), with 87% of the components as rated as meeting or exceeding expectations. Although each component was covered, consistent with MI principles, the time spent on each section depended on the student’s interest level. The RT session was rated for inclusion of the 11 key components of the session. The average rating was 2.27 (SD = .47, Mdn = 2.00), with 99% of the components rated as meeting or exceeding expectations.
Motivational interviewing integrity.
Twenty-two recordings (14 BMI, 8 SFAS) were randomly selected and rated by two doctoral level expert raters to assess treatment integrity using the MI Treatment Integrity Coding Manual 4.2 (MITI: Moyers, Manuel, & Ernst, 2014). Four summary scores were examined: Technical global, Relational global, MI-adherent behavior count, and MI-nonadherent count. The technical global score describes the extent to which therapists engaged in techniques designed to strengthen change talk and soften sustain talk; the suggested threshold for good competence is four (range = 1–5). The relational global score describes the extent to which therapists worked with the client empathically and as equal partners; the suggested threshold for good competence is four (range = 1–5). The MI-adherent and MI-nonadherent counts describe how often therapists engaged in each type of behavior. A random sample (n = 9) of sessions were double-coded to establish interrater reliability; interrater reliability was determined using a two-way absolute single-measures intra-class correlation (ICC), which provides a conservative estimate of reliability that is generalizable to single- and double-coded sessions (Hallgren, Leifman, & Andreasson, 2012). All codes demonstrated acceptable reliability. Reliability ranged from fair for MI-nonadherent (ICC = .513) to excellent for Relational (ICC = .773) and MI-adherent (ICC = .826), with good reliability for Technical (ICC = 0.610; (Cicchetti & Nelson, 1994)). Overall, therapists demonstrated proficiency on the Relational (M = 4.3, SD = 0.7) and Technical (M = 4.5, SD = 0.8) components of MI. Therapists engaged in more MI-adherent behaviors (M = 2.8, SD = 2.4) than MI-nonadherent behaviors (M = 0.4, SD = 1.3).
Retention and Attrition.
All 255 participants randomized to an intervention condition completed both sessions, except for one who did not complete the relaxation session, and 99% (n = 253) completed the booster contact (77% completed via phone, 23% via email). Follow-up assessment rates were high: 1-month: (n = 366, 93% follow-up rate), 6-months (n =344, 88%), 12-months: (n =342, 87%) and 16-months (n =311, 79%). Although attrition was minimal, participants with missing data at the 12-month follow-up were more likely to be male (p = .047) and there were more missing data at 6-months and 16-months for participants recruited from Site 1 (ps = .027, .001). Missing data at 1-month follow-up was associated with typical drinking at the 16-month follow-up (mediated effect=-0.518 (0.202), p=0.005 (95% CI: −0.94, −.147). Given these findings, missing not at random models for typical drinking were conducted to evaluate whether there was evidence of systematic missingness. There were no substantive differences in model results.
Analysis of Drinking Outcomes.
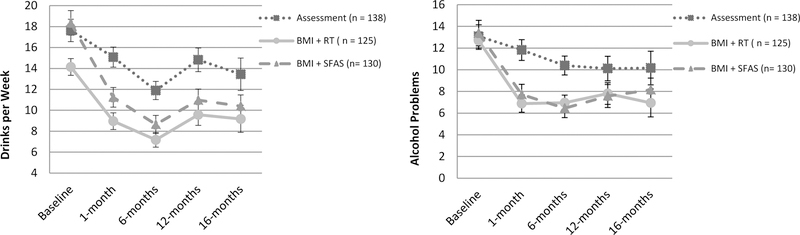
Table 1 shows baseline, one-month, six-month, 12-month and 16-month descriptive data on primary and secondary outcome measures, including the pre-post (within-group) effect sizes that accounted for the correlation between the timepoints (see also Figure 2). There was a significant between-conditions difference in typical weekly drinking at baseline (F (2, 390) = 4.58, p = .011). BMI+RT participants reported significantly less weekly drinking (M= 14.14, SD= 8.89) than those in the assessment (M= 17.63, SD= 12.55) or BMI+SFAS (M= 19.08, SD= 17.75) conditions. There were no other significant treatment group differences on baseline demographic or drinking measures. There were also no site by condition effects, condition by gender effects, or clinician effects for any of the outcomes. Generalized linear mixed models results are provided in Table 2.
Table 1.
Pre-Post Means (SD) and Effect Sizes for Drinking Variables and Secondary Outcomes
| Factor | Baseline (M/SD) | 1-month follow-up | Within-groups effect size (d) | 6-month follow-up | Within-groups effect size (d) | 1-year follow-up | Within-groups effect size (d) | 16-month follow-up | Within-groups effect size (d) |
|---|---|---|---|---|---|---|---|---|---|
| Drinking Variables | |||||||||
| Typical Drinks Per Week | |||||||||
| Assessment-only | 17.63 (12.55) | 15.08 (10.82) | .30 | 11.89 (9.67) | .51 | 14.82 (12.23) | .27 | 13.44 (15.76) | .29 |
| BMI+ RT | 14.14 (8.89) | 8.96 (8.64) | .78 | 7.18 (7.28) | .83 | 9.57 (10.64) | .47 | 9.18 (13.33) | .40 |
| BMI+ SFAS | 18.35 (13.50) | 11.24 (10.30) | .71 | 8.65 (9.11) | .93 | 10.97 (11.26) | .63 | 10.39 (10.86) | .64 |
| Alcohol-related consequences (0– 48) | |||||||||
| Assessment-only | 13.08 (8.19) | 11.82 (9.04) | .21 | 10.39 (8.45) | .35 | 10.11 (9.84) | .29 | 10.16 (10.31) | .36 |
| BMI + RT | 12.68 (7.61) | 6.88 (7.39) | .78 | 6.96 (7.82) | .67 | 7.81 (8.43) | .67 | 6.94 (8.40) | .61 |
| BMI + SFAS | 13.38 (7.85) | 7.72 (6.28) | .83 | 6.45 (7.18) | .83 | 7.58 (7.78) | .69 | 8.15 (9.08) | .64 |
| Secondary Outcomes | |||||||||
| Protective Behavioral Strategies (0 – 75) | |||||||||
| Assessment-only | 43.69 (12.35) | 44.17 (13.57) | .01 | 51.83 (13.61) | .68 | 52.84 (13.25) | .62 | 51.40 (13.20) | .53 |
| BMI + RT | 44.86 (14.73) | 51.32 (16.29) | .63 | 57.14 (14.16 | .97 | 57.34 (14.18) | .90 | 59.04 (15.03) | .98 |
| BMI + SFAS | 43.58 (13.18) | 49.26 (14.50) | .55 | 55.47 (14.89) | .88 | 54.21 (12.77) | .76 | 55.15 (13.61) | .76 |
| Depression (0 – 56) | |||||||||
| Assessment-only | 6.54 (8.09) | 5.32 (7.42) | .17 | 4.94 (7.28) | .23 | 6.14 (8.71) | .04 | 6.82 (9.74) | .04 |
| BMI+ RT | 8.01 (9.16) | 5.57 (8.67) | .35 | 4.84 (6.11) | .37 | 5.37 (8.18) | .24 | 5.52 (7.93) | .25 |
| BMI + SFAS | 7.80 (9.31) | 4.61 (6.75) | .45 | 4.73 (8.39) | .29 | 6.37 (9.59) | .14 | 4.28 (6.31) | .40 |
| Anxiety (0 – 56) | |||||||||
| Assessment-only | 5.03(6.35) | 4.68 (5.83) | .05 | 3.71 (4.56) | .26 | 5.31 (7.00) | .04 | 5.46 (7.44) | .02 |
| BMI + RT | 5.44 (6.57) | 4.53 (6.37) | .21 | 3.91 (5.49) | .26 | 3.42 (5.05) | .40 | 3.90 (5.59) | .21 |
| BMI + SFAS | 5.80 (6.80) | 3.10 (4.52) | .45 | 2.84 (5.81) | .45 | 4.34 (7.18) | .19 | 3.19 (5.01) | .42 |
| Anxiety (0 – 56) | |||||||||
| Assessment-only | 5.03(6.35) | 4.68 (5.83) | .05 | 3.71 (4.56) | .26 | 5.31 (7.00) | .04 | 5.46 (7.44) | .02 |
| BMI + RT | 5.44 (6.57) | 4.53 (6.37) | .21 | 3.91 (5.49) | .26 | 3.42 (5.05) | .40 | 3.90 (5.59) | .21 |
| BMI + SFAS | 5.80 (6.80) | 3.10 (4.52) | .45 | 2.84 (5.81) | .45 | 4.34 (7.18) | .19 | 3.19 (5.01) | .42 |
| Self-Regulation (31 –155) | |||||||||
| Assessment-only | 116.23 (15.59) | 116.38 (14.59) | .05 | 119.00 (14.26) | .18 | 117.09 (16.96) | .02 | 115.49 (16.14) | .10 |
| BMI + RT | 115.10 (17.85) | 117.84 (18.69) | .26 | 118.01 (17.63) | .15 | 119.57 (18.25) | .31 | 119.50 (17.46) | .29 |
| BMI + SFAS | 112.69 (16.30) | 116.47 (16.41) | .35 | 115.27 (17.59) | .21 | 115.59 (17.07) | .24 | 117.58 (18.09) | .39 |
| Delay Discounting (0 –1) | |||||||||
| Assessment-only | .038 (.079) | .043 (.081) | .06 | .039 (.081) | .05 | .042 (.084) | .00 | .030 (.072) | .10 |
| BMI + RT | .029 (.055) | .036 (.078) | .15 | .040 (.100) | .27 | .044 (.096) | .10 | .034 (.076) | .02 |
| BMI + SFAS | .039 (.078) | .040 (.069) | .07 | .048 (.088) | .12 | .044 (.102) | .16 | .049 (.100) | .14 |
| Reinforcement-Ratio (0–1) | |||||||||
| Assessment-only | .34 (.14) | .31 (.14) | .18 | .30 (.16) | .29 | .29 (.16) | .31 | .31 (.17) | .11 |
| BMI + RT | .34 (.16) | .25 (.18) | .61 | .26 (.19) | .51 | .23 (.17) | .63 | .26 (.17) | .46 |
| BMI + SFAS | .34 (.13) | .28 (.15) | .56 | .25 (.16) | .74 | .27 (.17) | .40 | .27 (.17) | .35 |
Means at each time point represent participants who completed that time point. Effect sizes were calculated accounting for correlation between baseline and follow-up timepoints.
Ns :(presented in the order Assessment, RT, SFAS) :
1-month outcomes – Typical Drinks ns: 128; 117; 121; Problems ns : 127; 117; 121 ; PBS ns 126; 117; 120; Depression ns: 126; 117; 121; Anxiety ns: 126;117; 120; Self-Regulation ns: 126; 117; 120; Reward Probability Index ns: 126; 117; 120; R-Ratio ns: 125; 114; 119.
Semester: Typical Drinks ns 123; 108; 113; Problems ns: 123; 108; 112; PBS ns 122; 106; 110; Depression ns: 123; 107; 112; Anxiety ns: 123; 107; 112; Self-Regulation ns: 121; 107; 111; Reward Probability Index ns: 122; 107; 109; R-Ratio ns: 120; 110; 106.
12-month: Typical Drinks ns:117; 112; 113; Problems ns:117; 113; 113; PBS ns 116; 112; 112; Depression ns: 116; 111; 113; Anxiety ns: 116; 111; 113; Self-Regulation ns: 116; 112; 112; Reward Probability Index ns: 116; 112; 112; R-Ratio ns: 116; 112; 113.
16-month: Typical Drinks ns: 103; 107; 101; Problems ns: 103; 107; 101; PBS ns 101; 103; 100; Depression ns: 103; 104; 101; Anxiety ns: 103; 105; 101; Self-Regulation ns: 101; 103; 100; Reward Probability Index ns: 101; 103; 100; R-Ratio ns: 102; 99; 95.
Figure 2.
Change in Typical Drinks per Week and Alcohol-Related Problems by Condition. Means (+/− 1 SEM) at each time point.
Table 2.
Results from Mixed Models Examining Drinking and Secondary Outcomes
| B (SE) | |
|---|---|
| Typical Drinks per Week | |
| Contrast 1: Active v. Assess | .12 (.02)* |
| Contrast 2: BMI + SFAS v. Assess | −.40 (.07)** |
| Contrast 3: BMI + SFAS v. BMI + RT | −.04 (.05) |
| Contrast 4: BMI + RT v. Assess | −1.07 (.25)*** |
| Time | −.007 (.004) |
| Baseline Typical Drinks per Week | .04 (.004)** |
| Treatment Site | .22 (.07)** |
| Gender (Female = 1) | −.27 (.07)** |
| Race (White = 1) | .24 (.09) |
| Greek (Greek = 1) | .12 (.07) |
| Alcohol-related Problems | |
| Contrast 1: Active v. Assess | .14(.03)** |
| Contrast 2: BMI + SFAS v. Assess | −.43 (.10)** |
| Contrast 3: BMI + SFAS v. BMI + RT | −.02 (.07) |
| Contrast 4: BMI + RT v. Assess | −3.12 (.70)*** |
| Time | −.01 (.005) |
| Baseline Alcohol-related Problems | .07 (.004)** |
| Treatment Site | .34 (.09)** |
| Gender (Female = 1) | −.23 (.09)** |
| Race (White = 1) | .02 (.09) |
| Greek (Greek = 1) | .17 (.07)* |
| Secondary Outcomes | B (SE) |
| Protective Behavioral Strategies | |
| Contrast 1: Active v. Assess | −1.51 (.39)** |
| Contrast 2: BMI + SFAS v. Assess | 3.78 (1.30)** |
| Contrast 3: BMI + SFAS v. BMI + RT | −0.77 (.54) |
| Contrast 4: BMI + RT v. Assess | 5.14 (1.26)*** |
| Time | 0.40 (.07) ** |
| Baseline Protective Behavioral Strategies | 0.62 (.04)** |
| Treatment Site | −2.95 (.86)** |
| Gender (Female = 1) | 3.49 (1.31)** |
| Race (White = 1) | −0.21 (1.17) |
| Greek (Greek = 1) | −3.36 (.98)** |
| Depression | |
| Contrast 1: Active v. Assess | .37 (.18)* |
| Contrast 2: BMI + SFAS v. Assess | −1.21 (.64) |
| Contrast 3: BMI + SFAS v. BMI + RT | −.13 (.33) |
| Contrast 4: BMI + RT v. Assess | −0.99 (.66) |
| Time | .05 (.02)* |
| Baseline Depression | .49 (.04)** |
| Treatment Site | .43 (.46) |
| Gender (Female = 1) | −.22 (.49) |
| Race (White = 1) | −1.22 (.69) |
| Greek (Greek = 1) | −.32 (.57) |
| Anxiety | |
| Contrast 1: Active v. Assess | .46 (.09 )** |
| Contrast 2: BMI + SFAS v. Assess | −1.72 (.36)** |
| Contrast 3: BMI + SFAS v. BMI + RT | −.36 (.21) |
| Contrast 4: BMI + RT v. Assess | −1.03 (.30)** |
| Time | .02 (.02) |
| Baseline Anxiety | .43 (.05)** |
| Treatment Site | −.13 (.40) |
| Gender (Female = 1) | .03 (.34) |
| Race (White = 1) | −.25 (.63) |
| Greek (Greek = 1) | −.17 (.46) |
| Self-Regulation | |
| Contrast 1: Active v. Assess | −.81 (.30)** |
| Contrast 2: BMI + SFAS v. Assess | 2.03 (1.22)† |
| Contrast 3: BMI + SFAS v. BMI + RT | −.23 (.66) |
| Contrast 4: BMI + RT v. Assess | 2.48 (1.04)* |
| Time | .06 (.04) |
| Baseline Self-regulation | .76 (.03)** |
| Treatment Site | −2.98 (1.03) ** |
| Gender (Female = 1) | 2.20 (.63)** |
| Race (White = 1) | .59 (1.41) |
| Greek (Greek = 1) | −1.39 (1.07) |
| Delay Discounting | |
| Contrast 1: Active v. Assess | −0.001 (.003) |
| Contrast 2: BMI + SFAS v. Assess | 0.006 (.01) |
| Contrast 3: BMI + SFAS v. BMI + RT | 0.003 (.003) |
| Contrast 4: BMI + RT v. Assess | 0.000 (.01) |
| Time | 0.00 (.00) |
| Baseline Delay Discounting | 0.63 (.08)** |
| Treatment Site | −0.02 (.01) |
| Gender (Female = 1) | 0.01 (.01) |
| Race (White = 1) | −0.03 (.02) |
| Greek (Greek = 1) | −0.003 (.01) |
| Time Spent Drinking | |
| Contrast 1: Active v. Assess | .34 (.10) ** |
| Contrast 2: BMI + SFAS v. Assess | −.93 (.42)* |
| Contrast 3: BMI + SFAS v. BMI + RT | .08 (.15) |
| Contrast 4: BMI + RT v. Assess | −1.07 (.25)** |
| Time | −.05 (.02)** |
| Baseline Time Spent Drinking | .44 (.03)** |
| Treatment Site | 1.11 (.28)** |
| Gender (Female = 1) | −1.13 (.28)*** |
| Race (White = 1) | 0.41 (.26) |
| Greek (Greek = 1) | .60 (.28)* |
| Reinforcement Ratio | |
| Contrast 1: Active v. Assess | .02 (.004) ** |
| Contrast 2: BMI + SFAS v. Assess | −.04 (.01)** |
| Contrast 3: BMI + SFAS v. BMI + RT | .01 (.01) |
| Contrast 4: BMI + RT v. Assess | −0.05 (.01)*** |
| Time | .00 (.00) |
| Baseline Reinforcement Ratio | .58 (.04)** |
| Treatment Site | .02 (.01) |
| Gender (Female = 1) | −.05 (.01)** |
| Race (White = 1) | .01 (.02) |
| Greek (Greek = 1) | .02 (.01)* |
Abbreviations: B, unstandardized regression coefficient; β, standardized regression coefficient in general linear mixed models.
Bs presented for the covariates come from the model containing contrast 1 and 2. Contrasts 3 & 4 were run in separate models
Contrast 1 was coded with Active treatment as −1 and Assessment as +2; contrast 2 was coded with Assessment as −1 and BMI + SFAS as +1; contrast 3 was coded with BMI + RT as −1 and BMI + SFAS as +1, and contrast 4 was coded with Assessment as −1 and BMI + SFAS as +1.
p < .05
p < .01
p = .065
Change in Drinks Per Week.
The contrast that compared active treatment [BMI+SFAS or BMI+RT] versus assessment-only was significant, as were the individual contrasts that compared BMI+SFAS and BMI+RT to assessment. There was no difference between BMI+SFAS and BMI+ RT1. As indicated in Table 1 and Figure 2, the greatest reductions occurred over the first 6 months (with large within group effect sizes for both active treatments) and diminished slightly at the 1-year and 16-month follow-ups. Assessment-only participants reduced their drinking by an average of 4.2 drinks per week at the 16-month follow-up (dw = .29), compared to a 5.0 drink reduction by BMI+ RT participants (dw = .40) and an 8.0 drink reduction by BMI+SFAS participants (dw = .64). Men and students from university two reported significantly more drinks per week across all time-points.
Change in Alcohol Problems.
The contrast that compared active treatment [BMI+SFAS or BMI+RT] versus assessment-only was significant, as were the individual contrasts that compared BMI+SFAS and BMI+RT to assessment. There was no difference between BMI+SFAS and BMI+RT. Both active treatments were associated with large reductions in alcohol problems at 1-month follow-up that were generally maintained over 16-months. Assessment-only participants showed a small gradual decline in alcohol problems over the one and 6-month follow-ups. Assessment-only participants reduced their alcohol problems by 2.9 at the 16-month follow-up (dw = .36), compared to a 5.7 reduction by BMI+RT participants (dw = .61) and a 5.2 reduction by BMI +SFAS participants (dw = .64). Men, Greek members, and students from university two reported more alcohol problems across all time-points.
Evaluation of Secondary Intervention Outcomes and Mediation
Change in secondary intervention outcomes.
General linear mixed models were used to examine treatment-related change in secondary outcomes at follow-up (see Tables 1 & 2). There were significant main effects indicating that individuals in either of the active treatment conditions reported greater self-regulation and PBS, as well as less depression, anxiety, and reinforcement-ratio values than those in the assessment-only condition. The contrasts examining BMI+SFAS versus assessment and BMI+RT versus assessment showed that individuals who received a BMI+SFAS or a BMI+RT had less anxiety, greater PBS, lower reinforcement-ratio values, and greater self-regulation (trend level effect for BMI + SFAS) than those in the assessment-only condition. There were no differences in these proximal intervention outcomes between those in the BMI+SFAS condition and those in the BMI+RT condition. Covariate analyses indicated that students at university two reported significantly lower self-regulation across all time-points. Females reported greater self-regulation and PBS, and lower reinforcement-ratio scores, and Greek membership predicted fewer PBS and greater reinforcement-ratio outcomes.
Mediation analysis.
We conducted multilevel mediation analyses to determine if change in several secondary outcome variables across the entire follow-up period (depression, anxiety, PBS, self-regulation, and reinforcement-ratio) mediated the significant treatment effects (active treatment vs. assessment only) on typical drinking and alcohol-related problems over time. All models provided adequate fit to the data based on Root Mean Square Error of Approximation (RMSEA; Browne & Cudeck, 1993) <0.08 and the Comparative Fit Index (CFI; Bentler, 1990) >0.95. For the contrast of active treatment versus assessment, change in PBS and the reinforcement ratio mediated the effect of condition on both typical drinking [mediated effect PBS=0.21(0.07), p=0.002 (95% CI: 0.10, 0.347); (mediated effect reinforcement-ratio =-0.240 (0.069), p<0.001 (95% CI: .111, .382)] and alcohol problems [mediated effect PBS=-0.174 (0.062), p=0.005 (95% CI: .075, .283); mediated effect reinforcement ratio= 0.226 (0.064), p<0.001 (95% CI: .105, .356)]. Mediation effects for PBS and reinforcement-ratio were moderate to large. Self-regulation and anxiety were not significant mediators and there was a non-significant trend-level effect for depression as a mediator of change in alcohol problems (mediated effect=0.079 (0.41), p=0.08 (95% CI: .003, .165).
Discussion
This study evaluated the efficacy of a BMI augmented with either a behavioral economic SFAS or a Relaxation Training (RT) session among heavy drinking college students recruited from two public universities. The combination of a BMI plus either the SFAS or RT session was associated with significant, moderate to large effect-size reductions in alcohol use and problems that persisted across the 16-month follow-up compared to assessment only.
Our study extends the results of two previous pilot studies demonstrating that BMI+SFAS is associated with short-term reductions in alcohol use and problems (Murphy et al., 2012a; Yurasek et al., 2015). Contrary to the results of Murphy et al. (2012a), however, the BMI+SFAS was not associated with significantly greater reductions in alcohol problems compared to BMI+RT. The difference was a product of greater efficacy for the BMI+RT condition in the present trial, rather than diminished efficacy of the BMI+SFAS, as the SFAS was associated with slightly larger reductions in drinking and alcohol problems than in the previous two trials. Previous research suggests that RT is not an effective stand-alone intervention for alcohol misuse (Colby et al., 2018; Kamboj et al., 2017), and we initially conceptualized it as an active control session added to the efficacious BMI to control for the contact time required to complete the SFAS. However, the present results suggest that it merits further study as a potentially effective supplement to BMIs. It is possible that the high prevalence of stress among college students (American College Health Association, 2015) combined with the greater societal acceptance of mindfulness, and the inclusion of a booster call, enhanced the potency of RT relative to the previous trial.
Because the present study did not include a stand-alone BMI condition, we cannot determine whether these 2-session interventions are more efficacious than the popular assessment plus single session approaches that have been widely disseminated (Huh et al., 2015). However, meta-analyses suggest that single-session BMIs are associated with only small effect size reductions for alcohol use and problems (e.g., Tanner-Smith et al., 2015). A previous study in our laboratory that investigated a single-session BMI with the same treatment manual that was used in the present study found within-group effect size reductions of .29 for both consumption and problems at 6-months (Murphy et al., 2015), which are substantively smaller than the 6-month reductions we observed in the current BMI+SFAS (dws = .93 & .83, respectively) and BMI+RT (dws = .83 & .67, respectively) conditions. This present study suggests that treatment effects dissipated slightly from the 6 to the 16th month follow-up but remained significant relative to assessment across the entire follow-up period. Thus, these results provide strong support for two-session BMIs with a phone booster. Although drinking is not a primary focus of either the SFAS or the RT session, both sessions do briefly address alcohol and might provide an occasion for participants to further contemplate the BMI session that occurred the week before, possibly enhancing the deliberative processing and retention of the alcohol-related content (Jouriles et al., 2010).
Secondary Outcomes and Mechanisms of Behavior Change
Both active treatments were associated with improvements in several secondary outcomes – including symptoms of depression and anxiety, the proportion of reinforcement related to substance-using activities, self-regulation, and PBS- that might support changes in drinking and more general college success. These results replicate and extend previous research indicating that PBS is a consistent mediator of alcohol BMI results (Barnett, Murphy, Colby, & Monti 2007; Magill et al., 2017; Murphy, et al., 2012a). All participants received feedback on PBS in the individual BMI session and their implementation of those harm reduction strategies facilitated reductions in drinking and problems. These results also replicate the finding of Murphy et al. (2012a) that both BMI+SFAS and BMI+RT are associated with reductions in depressive symptoms. Reductions in depressive symptoms may be facilitated by either relaxation strategies or the engagement strategies of the SFAS (which are similar to behavioral activation; (Daughters et al., 2018)). The SFAS also includes personalized feedback on coping with symptoms of stress and depression (Geisner, Neighbors, & Larimer, 2006). Given that approximately 35% of college students experience subclinical depression that is nevertheless associated with impairment and risk for persistent alcohol problems (Kenney, Merrill, & Barnett, 2017), this is an important secondary benefit of these BMIs.
The present results also provide further evidence for the role of substance-free reinforcement as a mechanism of change for brief alcohol interventions (Magill et al., 2017; Murphy et al., 2005, 2015). The current results extend previous research by indicating that reducing the proportion of total reinforcement associated with drug and alcohol use mediates the effect of BMI on alcohol use and problems and suggest that reward-related mechanisms account for change even if not directly targeted with an intervention such as the SFAS. Although we failed to replicate previous research indicating that self-regulation mediated the treatment effects associated with BMI+SFAS (Soltis et al., 2018), both BMI conditions were associated with increases in self-regulation, which has previously been identified as a risk factor for poor BMI response (Carey, et al., 2007). Consistent with previous results (Murphy et al., 2012a), neither intervention impacted delay discounting, which is a robust predictor of substance in more severe substance-abusing populations (Bickel et al., 2014) but has not shown consistent associations with young adult drinking (Lemley, Kaplan, Reed, Darden, & Jarmolowicz, 2016).
Strengths and Limitations
Limitations of this study include the reliance on retrospective self-report measures of drinking and activity participation, the fact that BMI+RT participants drank less than participants in the other two conditions at baseline, and the absence of a stand-alone BMI condition or a single session active control rather than assessment only. Although repeated in-person assessment control for reactivity effects, meta-analytic reviews suggest that effect sizes for BMI are smaller when they are compared to an active control versus assessment only (Scott-Sheldon et al., 2014). Another limitation of this study is that the results may not be generalizable to all young adults including those who are not college students, students who drink substantively more than our participants, or students who work more than 20 hours a week or who are junior or seniors. Interestingly, although alcohol BMI is generally less effective with non-college young adult samples (Davis, Smith, & Briley, 2017), Colby et al. (2018) found that a single session BMI that included some SFAS elements (feedback on time allocation and discussion of future goals) was efficacious across a 3-month follow-up with a sample of young adults who were not attending college. Finally, all active treatment participants received phone boosters so we are unable to determine their incremental efficacy. Strengths of this study include the fact that it evaluated two distinct approaches for enhancing BMI outcomes in a relatively large sample recruited from two different universities with high retention over a 16-month follow-up period. Additionally, we evaluated internal validity and a variety of theoretically relevant secondary outcomes and mechanisms of change. Our results demonstrated enduring treatment effects and significant mediation by proportionate reinforcement from substance use and PBS (with trend level findings for depression) and thus provide support for interventions that target these mechanisms. Men and Greek life students reported lower PBS and higher reinforcement from substance-use relative to alternatives and these students may thus be especially in need of more intensive intervention approaches that directly target these mechanisms.
Implications and Future Directions
BMIs for alcohol misuse have been widely disseminated across a number of educational and healthcare settings, yet there has been very little research aimed at enhancing efficacy by adding novel theoretically grounded intervention elements (Huh et al., 2015). The current results suggest that BMI plus either the SFAS or RT session with a booster phone call is associated with enduring reductions in alcohol use and problems, as well as improvements in symptoms of anxiety, depression, self-regulation, PBS and proportionate reinforcement from substance-free activities. Although further research is required to determine the optimal intervention duration and content, our results provide support for exploring slightly longer brief alcohol intervention approaches than standard SBIRT models, that have space to integrate novel content, perhaps as part of a stepped-care approach (Borsari et al., 2015).
Public Health Significance:
Heavy drinking among college students is a significant public health concern. Brief alcohol interventions are effective, but drinking reductions are generally small, suggesting the need for additional intervention elements. The results of this randomized clinical trial suggest that brief alcohol interventions that are supplemented with either relaxation training or a behavioral economic session focused on increasing substance-free activities are associated with reductions in alcohol misuse over a 16-month follow-up period.
Acknowledgments
This research was supported by a RO1 from NIAAA (NIAAA R01AA020829; JGM).
Footnotes
Institution of origin: The University of Memphis
Analyses examining frequency of binge drinking revealed similar results
References
- American College Health Association. (2015). American College Health Association-National College Health Assessment II: Reference Group Executive Summary Spring 2015 Hanover, MD: American College Health Association. [Google Scholar]
- Amlung M, & MacKillop J (2011). Delayed reward discounting and alcohol misuse: The roles of response consistency and reward magnitude. Journal of Experimental Psychopathology, 2(3), 418–431. doi: 10.5127/jep.017311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett NP, Murphy JG, Colby SM, & Monti PM (2007). Efficacy of counselor vs. computer-delivered intervention with mandated college students. Addictive Behaviors, 32(11), 2529–2548. doi: 10.1016/j.addbeh.2007.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM (1990). Comparative fit indexes in structural models. Psychological Bulletin, 107(2), 238–246. doi: 10.1037//0033-2909.107.2.238 [DOI] [PubMed] [Google Scholar]
- Bickel WK, Johnson MW, Koffarnus MN, MacKillop J, & Murphy JG (2014). The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annual Review of Clincal Psychology, 10, 641–677. doi: 10.1146/annurev-clinpsy-032813-153724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borsari B, Apodaca TR, Jackson KM, Mastroleo NR, Magill M, Barnett NP, & Carey KB (2015). In-session processes of brief motivational interventions in two trials with mandated college students. Journal of Consulting and Clinical Psychology, 83(1), 56–67. doi: 10.1037/a0037635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R (1993). Alternative ways of assessing model fit. In Bollen KA & Long JS (Eds.), Testing structural equation models (pp. 136–162). Newbury Park, CA: Sage. [Google Scholar]
- Carey KB, Henson JM, Carey MP, & Maisto SA (2007). Which heavy drinking college students benefit from a brief motivational intervention? Journal of Consulting and Clinical Psychology, 75(4), 663. doi: / 10.1037/0022-006X.75.4.663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey KB, Neal DJ, & Collins SE (2004). A psychometric analysis of the self-regulation questionnaire. Addictive Behaviors, 29(2), 253–260. doi: 10.1016/j.addbeh.2003.08.001 [DOI] [PubMed] [Google Scholar]
- Cicchetti DV, & Nelson LD (1994). Reexamining threats to the reliability and validity of putative brain-behavior relationships - New guidelines for assessing the effect of patients lost to follow-up. Journal of Clinical and Experimental Neuropsychology, 16(3), 339–343. doi:Doi 10.1080/01688639408402644 [DOI] [PubMed] [Google Scholar]
- Colby SM, Orchowski L, Magill M, Murphy JG, Brazil LA, Apodaca TR, … Barnett NP. (2018). Brief motivational intervention for underage young adult drinkers: Results from a randomized clinical trial. Alcoholism-Clinical and Experimental Research, 42(7), 1342–1351. doi: 10.1111/acer.13770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Parks GA, & Marlatt GA (1985). Social determinants of alcohol-consumption - the effects of social-interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology, 53(2), 189–200. doi: 10.1037/0022-006x.53.2.189 [DOI] [PubMed] [Google Scholar]
- Daniel TO, Stanton CM, & Epstein LH (2013). The future is now: reducing impulsivity and energy intake using episodic future thinking. Psychological Science, 24(11), 2339–2342. doi: 10.1177/0956797613488780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daughters SB, Magidson JF, Anand D, Seitz-Brown CJ, Chen Y, & Baker S (2018). The effect of a behavioral activation treatment for substance use on post-treatment abstinence: a randomized controlled trial. Addiction, 113(3), 535–544. doi: 10.1111/add.14049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JP, Smith DC, & Briley DA (2017). Substance use prevention and treatment outcomes for emerging adults in non-college settings: A meta-Analysis. Psychology of Addictive Behaviors, 31(3), 242–254. 10.1037/adb0000267 [DOI] [PubMed] [Google Scholar]
- Del Boca FK, Darkes J, Greenbaum PE, & Goldman MS (2004). Up close and personal: Temporal variability in the drinking of individual college students during their first year. Journal of Consulting and Clinical Psychology, 72(2), 155–164. doi: 10.1037/0022-006x.72.2.155 [DOI] [PubMed] [Google Scholar]
- DeMartini KS, Fucito LM, & O’Malley SS (2015). Novel approaches to individual alcohol interventions for heavy drinking college students and young adults. Current Addictions Report, 2(1), 47–57. doi: 10.1007/s40429-015-0043-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dimeff LA (1999). Brief Alcohol Screening and Intervention for College Students (BASICS) : a harm reduction approach New York: Guilford Press. [Google Scholar]
- Enders CK (2011). Analyzing longitudinal data with missing values. Rehabilitation Psychology, 56(4), 267–288. doi: 10.1037/a0025579 [DOI] [PubMed] [Google Scholar]
- Foxcroft DR, Coombes L, Wood S, Allen D, Santimano NMLA, & Moreira MT (2016). Motivational interviewing for the prevention of alcohol misuse in young adults. Cochrane Database of Systematic Reviews(7). doi:ARTN CD007025 10.1002/14651858.CD007025.pub4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geisner IM, Neighbors C, & Larimer ME (2006). A Randomized clinical trial of a brief, mailed intervention for symptoms of depression. Journal of Consulting and Clinical Psychology, 74(2), 393–399. doi: 10.1037/0022-006x.74.2.393 [DOI] [PubMed] [Google Scholar]
- Hallgren KA, Greenfield BL, & Ladd BO (2016). Psychometric properties of the adolescent reinforcement survey schedule-alcohol use version with college student drinkers. Substance Use & Misuse, 51(7), 812–822. doi: 10.3109/10826084.2016.1155609 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallgren M, Leifman H, & Andreasson S (2012). Drinking less but greater harm: Could polarized drinking habits explain the divergence between alcohol consumption and harms among youth? Alcohol and Alcoholism, 47(5), 581–590. doi: 10.1093/alcalc/ags071 [DOI] [PubMed] [Google Scholar]
- Hingson R, Zha WX, & Smyth D (2017). Magnitude and trends in heavy episodic drinking, alcohol-impaired driving, and alcohol-related mortality and overdose hospitalizations among emerging adults of college ages 18–24 in the United States, 1998–2014. Journal of Studies on Alcohol and Drugs, 78(4), 540–548. doi:DOI 10.15288/jsad.2017.78.540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmeyr A, Ainslie G, Charlton R, & Ross D (2011). The relationship between addiction and reward bundling: an experiment comparing smokers and non-smokers. Addiction, 106(2), 402–409. doi: 10.1111/j.1360-0443.2010.03166.x [DOI] [PubMed] [Google Scholar]
- Huh D, Mun EY, Larimer ME, White HR, Ray AE, Rhew IC, … Atkins DC. (2015). Brief motivational interventions for college student drinking may not be as powerful as we think: An individual participant-level data meta-analysis. Alcoholism-Clinical and Experimental Research, 39(5), 919–931. doi: 10.1111/acer.12714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jennison KM (2004). The short-term effects and unintended long-term consequences of binge drinking in college: A 10-year follow-up study. American Journal of Drug and Alcohol Abuse, 30(3), 659–684. doi: 10.1081/Ada-200032331 [DOI] [PubMed] [Google Scholar]
- Jouriles EN, Brown AS, Rosenfield D, McDonald R, Croft K, Leahy MM, & Walters ST (2010). Improving the effectiveness of computer-delivered personalized drinking feedback interventions for college students. Psychology of Addictive Behaviors, 24(4), 592–599. doi: 10.1037/a0020830 [DOI] [PubMed] [Google Scholar]
- Joyner KJ, Pickover AM, Soltis KE, Dennhardt AA, Martens MP, & Murphy JG (2016). Deficits in access to reward are associated with college student alcohol use disorder. Alcoholism-Clinical and Experimental Research, 40(12), 2685–2691. doi: 10.1111/acer.13255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamboj SK, Irez D, Serfaty S, Thomas E, Das RK, & Freeman TP (2017). Ultra-brief mindfulness training reduces alcohol consumption in at-risk drinkers: A randomized double-blind active-controlled experiment. International Journal of Neuropsychopharmacology, 20(11), 936–947. doi: 10.1093/ijnp/pyx064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenney SR, Merrill JE, & Barnett NP (2017). Effects of depressive symptoms and coping motives on naturalistic trends in negative and positive alcohol-related consequences. Addictive Behaviors, 64, 129–136. doi: 10.1016/j.addbeh.2016.08.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivlahan DR, Marlatt GA, Fromme K, Coppel DB, & Williams E (1990). Secondary prevention with college drinkers - evaluation of an alcohol skills training-program. Journal of Consulting and Clinical Psychology, 58(6), 805–810. doi: 10.1037/0022-006x.58.6.805 [DOI] [PubMed] [Google Scholar]
- Klajner P, Hartman L, Sobell M (1984). Treatment of substance abuse by relaxation training: A review of its rationale, efficacy and mechanisms. Addictive Behaviors, 9, 41–55. doi: 10.1016/0306-4603(84)90006-6 [DOI] [PubMed] [Google Scholar]
- Latvala A, Rose RJ, Pulkkinen L, Dick DM, Korhonen T, & Kaprio J (2014). Drinking, smoking, and educational achievement: Cross-lagged associations from adolescence to adulthood. Drug and Alcohol Dependence, 137, 106–113. doi: 10.1016/j.drugalcdep.2014.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lemley SM, Kaplan BA, Reed DD, Darden AC, & Jarmoloqicz DP (2016). Reinforcer pathologies: Predicting alcohol related problems in college drinking men and women. Drug and Alcohol Dependence, 167 (1), 57–66. doi: 10.1016/j.drugalcdep.2016.07.025 [DOI] [PubMed] [Google Scholar]
- Lovibond PF, & Lovibond SH (1995). The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behavior Research and Therapy, 33(3), 335–343. doi: 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- MacKillop J, Amlung MT, Few LR, Ray LA, Sweet LH, & Munafo MR (2011). Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology, 216(3), 305–321. doi: 10.1007/s00213-011-2229-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J, & Kahler CW (2009). Delayed reward discounting predicts treatment response for heavy drinkers receiving smoking cessation treatment. Drug and Alcohol Dependence, 104(3), 197–203. doi: 10.1016/j.drugalcdep.2009.04.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP (2008). Introduction to statistical mediation analysis Mahwah, NJ: Erlbaum. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, & Sheets V (2002). A comparison of methods to test mediation and other intervening variable effects. Psychological Methods, 7(1), 83–104. doi: 10.1037//1082-989x.7.1.83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Madden GJ, Begotka AM, Raiff BR, & Kastern LL (2003). Delay discounting of real and hypothetical rewards. Experimental and Clinical Psychopharmacology, 11(2), 139–145. doi: 10.1037/1064-1297.11.2.139 [DOI] [PubMed] [Google Scholar]
- Magill M, Colby SM, Orchowski L, Murphy JG, Hoadley A, Brazil LA, & Barnett NP (2017). How does brief motivational intervention change heavy drinking and harm among underage youngadult drinkers? Journal of Consulting and Clinical Psychology, 85(5), 447–458. doi: 10.1037/ccp0000200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Pedersen ER, LaBrie JW, Ferrier AG, & Cimini MD (2007). Measuring alcohol-related protective behavioral strategies among college students: Further examination of the protective behavioral strategies scale. Psychology of Addictive Behaviors, 21(3), 307–315. doi: 10.1037/0893-164x.21.3.307 [DOI] [PubMed] [Google Scholar]
- Merrill JE, Reid AE, Carey MP, & Carey KB (2014). Gender and depression moderate response to brief motivational intervention for alcohol misuse among college students. Journal of Consulting and Clinical Psychology, 82(6), 984–992. doi: 10.1037/a0037039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2013). Motivational interviewing: Helping people change (3rd ed.). New York: Guilford Press. [Google Scholar]
- Moyers TB, Manuel JK, & Ernst D (2014) Motivational Interviewing Treatment Integrity Coding Manual 4.2.1 Unpublished manual.
- Murphy JG, Correia CJ, Colby SM, & Vuchinich RE (2005). Using behavioral theories of choice to predict drinking outcomes following a brief intervention. Experimental and Clinical Psychopharmacology, 13(2), 93–101. doi: 10.1037/1064-1297.13.2.93 [DOI] [PubMed] [Google Scholar]
- Murphy JG, & Dennhardt AA (2016). The behavioral economics of young adult substance abuse. Preventive Medicine, 92, 24–30. doi: 10.1016/j.ypmed.2016.04.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Skidmore JR, Borsari B, Barnett NP, Colby SM, & Martens MP (2012a). A Randomized controlled trial of a behavioral economic supplement to brief motivational interventions for college drinking. Journal of Consulting and Clinical Psychology, 80(5), 876–886. doi: 10.1037/a0028763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Dennhardt AA, Yurasek AM, Skidmore JR, Martens MP, MacKillop J, & McDevitt-Murphy ME (2015). Behavioral economic predictors of brief alcohol intervention outcomes. Journal of Consulting and Clinical Psychology, 83(6), 1033–1043. doi: 10.1037/ccp0000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy JG, Skidmore JR, Dennhardt AA, Martens MP, Borsari B, Barnett NP, & Colby SM (2012b). A behavioral economic supplement to brief motivational interventions for college drinking. Addiction Research & Theory, 20(6), 456–465. doi: 10.3109/16066359.2012.665965 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy L, & Dockray S (2018). The consideration of future consequences and health behaviour: a meta-analysis. Health Psychology Review, 12(4), 357–381. doi: 10.1080/17437199.2018.1489298 [DOI] [PubMed] [Google Scholar]
- Muthén LK & Muthén BO (1998–2018). Mplus User’s Guide Eight Edition. Los Angeles, CA: Muthén & Muthén [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). (2015). Planning Alcohol Interventions Using NIAAA’s College Alcohol Intervention Matrix (NIH Publication No. 15-AA-8017) Bethesda, MD: NIAAA [Google Scholar]
- Read JP, Merrill JE, Kahler CW, & Strong DR (2007). Predicting functional outcomes among college drinkers: Reliability and predictive validity of the young adult alcohol consequences questionnaire. Addictive Behaviors, 32(11), 2597–2610. doi: 10.1016/j.addbeh.2007.06.021 [DOI] [PubMed] [Google Scholar]
- Rung JM, & Madden GJ (2018). Experimental reductions of delay discounting and impulsive choice: A systematic review and meta-analysis. Journal of Experimental Psychology, 147(9), 1349–1381. 10.1037/xge0000462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott-Sheldon LAJ, Carey KB, Elliott JC, Garey L, & Carey MP (2014). Efficacy of alcohol interventions for rirst-year college students: A meta-analytic review of randomized controlled trials. Journal of Consulting and Clinical Psychology, 82(2), 177–188. doi: 10.1037/a0035192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singleton RA (2007). Collegiate alcohol consumption and academic performance. Journal of Studies on Alcohol and Drugs, 68(4), 548–555. doi:DOI 10.15288/jsad.2007.68.548 [DOI] [PubMed] [Google Scholar]
- Soltis KE, Acuff SF, Dennhardt AA, Borsari B, Martens MP, & Murphy JG (2018). Self-regulation as a mediator of the effects of a brief behavioral economic intervention on alcohol-related outcomes: A preliminary analysis. Experimental and Clinical Psychopharmacology, 26(4), 347–353. doi: 10.1037/pha0000213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick B & Fidell L (2012). Using multivariate statistics (6th ed.). Boston, MA: Allyn & Bacon. [Google Scholar]
- Tanner-Smith EE, & Lipsey MW (2015). Brief alcohol interventions for adolescents and young adults: A systematic review and meta-analysis. Journal of Substance Abuse Treatment, 51, 1–18. doi: 10.1016/j.jsat.2014.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tofighi D, & MacKinnon DP (2011). RMediation: An R package for mediation analysis confidence intervals. Behavior Research Methods, 43(3), 692–700. doi: 10.3758/s13428-011-0076-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turrisi R, Mallett KA, Cleveland MJ, Varvil-Weld L, Abar C, Scaglione N, & Hultgren B (2013). Evaluation of timing and dosage of a parent-based intervention to minimize college students’ alcohol consumption. Journal of Studies on Alcohol and Drugs, 74(1), 30–40. doi: 10.15288/jsad.2013.74.30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yurasek AM, Dennhardt AA, & Murphy JG (2015). A randomized controlled trial of a behavioral economic intervention for alcohol and marijuana use. Experimental and Clinical Psychopharmacology, 23(5), 332–338. doi: 10.1037/pha0000025 [DOI] [PMC free article] [PubMed] [Google Scholar]