Abstract
Background/Aims
In the treat-to-target era, psoriasis disease activity measures that can be easily performed in routine clinical practice are needed. This retrospective pooled analysis explored cutoff values of the product of the 5-point Investigator's Global Assessment and percentage of affected body surface area (IGA × BSA) correlating with achievement of minimal disease activity (MDA).
Methods
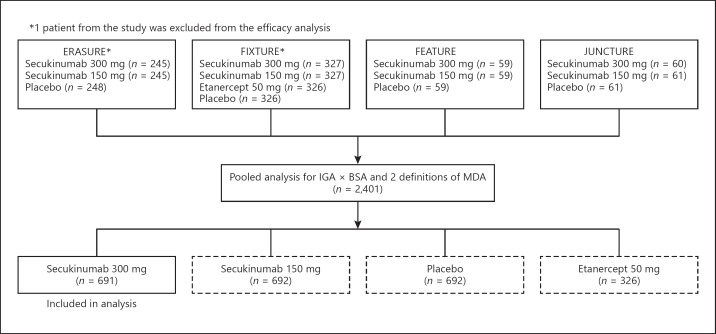
Post hoc analysis of the phase 3 clinical trials ERASURE, FIXTURE, FEATURE, and JUNCTURE was conducted to determine associations between IGA × BSA and 2 MDA definitions (Psoriasis Area and Severity Index [PASI] 90 and Dermatology Life Quality Index [DLQI] 0/1, or PASI score ≤1 or BSA <3%) in patients with moderate-to-severe psoriasis receiving secukinumab 300 mg. For each definition of MDA, a range of possible cutoff values of IGA × BSA was examined at each time point. The optimal cutoff value was determined using Youden index (YI), calculated as (sensitivity + specificity – 1).
Results
For MDA defined as PASI 90 and DLQI 0/1, optimal IGA × BSA cutoffs were 2.10 at week 12 (YI, 0.60; sensitivity, 0.78; specificity, 0.82), 1.02 at week 24 (YI, 0.55; sensitivity, 0.73; specificity, 0.82), and 1.00 at week 52 (YI, 0.65; sensitivity, 0.79; specificity, 0.86). For MDA defined as PASI score ≤1 or BSA <3%, optimal IGA × BSA cutoffs were 2.98 at week 12 (YI, 0.91; sensitivity, 0.99; specificity, 0.92), 2.80 at week 24 (YI, 0.94; sensitivity, 0.99; specificity, 0.95), and 3.00 at week 52 (YI, 0.96; sensitivity, 1.00; specificity, 0.96).
Conclusion
IGA × BSA could be a valid measure highly associated with achievement of MDA.
Keywords: Psoriasis, Investigator's Global Assessment, Physician's Global Assessment, Affected body surface area, Minimal disease activity
Introduction
Psoriasis is a common, systemic, chronic immune-mediated disease that manifests mainly as plaque, but other manifestations include guttate, flexural, erythrodermic, pustular, palmoplantar, and/or nail psoriasis [1, 2]. The goal of treatment in patients with psoriasis is to clear skin and normalize health-related quality of life, with the target of achieving minimal disease activity (MDA). Physicians and payers want a treatment target that will be used to make decisions regarding continuing, stopping, or changing treatment [3]. Currently, a variety of treatments, including topical agents, phototherapy, systemic therapies, and/or biologic therapies are used clinically for psoriasis [4]. The National Psoriasis Foundation guidelines for management of psoriasis recommend a treat-to-target strategy for clinicians and patients to work together to improve treatment decisions, reduce disease burden, and improve clinical outcomes [5].
The Psoriasis Area and Severity Index (PASI) is typically used as a measure of psoriasis disease activity in clinical trials but may not be practical for use in clinical practice. Limitations of the PASI include (1) the need for complex calculations; (2) time-consuming documentation; (3) complex scoring that may not be understood by most clinicians; and (4) non–reader-friendly format due to nonlinearity, with poor sensitivity to change and poor discrimination at lower score ranges [6, 7]. Alternatively, the 5-point Investigator's Global Assessment (IGA) and percentage of affected body surface area (BSA) are measures of psoriasis disease activity that are easily performed in routine clinical practice. Valid but simple, highly feasible measures, such as the product of the 5-point IGA or Physician's Global Assessment (PGA) and percentage of affected BSA (IGA × BSA or PGA × BSA, respectively), are easily captured by health-care providers and understood by providers, regulators, and payers.
PGA × BSA has been validated and used in several studies [7, 8, 9, 10, 11, 12]; most notably, PGA × BSA was highly correlated with PASI [7]. Furthermore, correlations between static PGA × BSA and PASI were stronger than that between BSA and PASI [13]. PGA × BSA also provided a clinically relevant assessment of MDA in patients with psoriasis, using PASI and Dermatology Life Quality Index (DLQI) response categories as anchors [14, 15].
The simplicity of IGA × BSA or PGA × BSA may allow for their potential use in a number of novel applications, such as defining a useful minimal disease criterion for treat-to-target strategies. The focus of this study is on the 5-point IGA and its product with BSA [16, 17, 18] that correlates with defined MDA, using data from four phase 3 clinical trials of secukinumab in patients with moderate-to-severe psoriasis.
Materials and Methods
For further details, see the online supplementary material (see www.karger.com/doi/10.1159/000499925 for all online suppl. material) (Fig. 1).
Fig. 1.
Flowchart of Materials and Methods.
Results
Pooled Baseline Characteristics
A total of 691 patients randomized to receive secukinumab 300 mg were included in the pooled patient population from the ERASURE, FIXTURE, FEATURE, and JUNCTURE clinical trials (Table 1). Patients were mostly male (69.0%) and white (73.1%), with a mean (SD) age of 44.9 (13.3) years and a mean (SD) disease duration of 17.0 (12.0) years. All patients had IGA scores of 3 (63.1%) or 4 (36.9%), indicating moderate or severe psoriatic arthritis, respectively. In addition, patients had a mean (SD) percentage of affected BSA of 33.0% (18.8%), a mean (SD) PASI score of 22.7 (9.4), and a mean (SD) DLQI score of 13.5 (7.3), further indicating moderate-to-severe disease activity. Approximately one-fifth of patients (21.1%) had previous exposure to biologic therapy.
Table 1.
Pooled baseline demographics, clinical characteristics, and treatment history of patients treated with secukinumab 300 mg (n = 691)a
| Age, years | 44.9 (13.3) |
| Male, n (%) | 477 (69.0) |
| Body weight, kg | 86.6 (23.2) |
| Body mass index, kg/m2 | 29.4 (6.9) |
| Race, n (%) | |
| White | 505 (73.1) |
| Asian | 129 (18.7) |
| Native American | 29 (4.2) |
| Black | 9 (1.3) |
| Pacific Islander | 4 (0.6) |
| Other | 13 (1.9) |
| Unknown | 2 (0.3) |
| IGA score, n (%) | |
| 0 = clear | 0 |
| 1 = almost clear | 0 |
| 2 = mild | 0 |
| 3 = moderate | 436 (63.1) |
| 4 = severe | 255 (36.9) |
| BSA, % involvement (n = 690) | 33.0 (18.8) |
| PASI score | 22.7 (9.4) |
| DLQI score (n = 676) | 13.5 (7.3) |
| Severity of psoriasis, n (%) | |
| Moderate | 202 (29.2) |
| Severe | 489 (70.8) |
| Time since first diagnosis of psoriasis, years | 17.0 (12.0) |
| Psoriatic arthritis present, n (%) | 126 (18.2) |
| Time since first diagnosis of psoriatic arthritis, years | 8.1 (8.3) |
| Previous exposure to psoriasis therapy, n (%) | |
| Systemic therapy | 438 (63.4) |
| Biologic systemic therapy | 146 (21.1) |
| Nonbiologic systemic therapy | 373 (54.0) |
All values were calculated on the basis of available data and are presented as means (SD) unless otherwise stated. BSA, body surface area; DLQI, Dermatology Life Quality Index; IGA, 5-point Investigator's Global Assessment; PASI, Psoriasis Area and Severity Index.
Patients with moderate-to-severe psoriasis randomized to secukinumab 300 mg in the ERASURE, FIXTURE, FEATURE, and JUNCTURE clinical trials.
Correlations between IGA × BSA and PASI Score
IGA × BSA and PASI scores were significantly correlated at week 12 (Pearson correlation coefficient, 0.92), week 24 (0.94), and week 52 (0.90; p < 0.001 for all). IGA × BSA and PASI score improvements between ≥75 and <90% from baseline were significantly correlated at week 12 (Pearson correlation coefficient, 0.64), week 24 (0.75), and week 52 (0.75; p < 0.001 for all).
Correlations between IGA × BSA and Achievement of Defined MDA
With the MDA definition of PASI 90 and DLQI 0/1, the IGA × BSA cutoff with the best sensitivity and specificity was 2.10 at week 12 (Youden index [YI], 0.60; sensitivity, 0.78; specificity, 0.82), 1.02 at week 24 (YI, 0.55; sensitivity, 0.73; specificity, 0.82), and 1.00 at week 52 (YI, 0.65; sensitivity, 0.79; specificity, 0.86) (Table 2; online suppl. Fig. 1).
Table 2.
Optimal IGA × BSA cutoffs for predictability of PASI 90 and DLQI 0/1 MDA definition (pooled secukinumab 300 mg treatment group)
| Week | IGA × BSA | Sensitivity | Specificity | Youden indexa |
|---|---|---|---|---|
| 4 | 8.90 | 0.8440 | 0.9000 | 0.74398 |
| 8 | 3.20 | 0.8034 | 0.8261 | 0.62949 |
| 12 | 2.10 | 0.7790 | 0.8191 | 0.59815 |
| 24 | 1.02 | 0.7317 | 0.8190 | 0.55073 |
| 36 | 0.62 | 0.8030 | 0.8333 | 0.63636 |
| 52 | 1.00 | 0.7857 | 0.8605 | 0.64626 |
BSA, body surface area; DLQI, Dermatology Life Quality Index; IGA, 5-point Investigator's Global Assessment; MDA, minimal disease activity; PASI, Psoriasis Area and Severity Index.
Youden index = sensitivity + specificity − 1.
Furthermore, with the MDA definition of PASI score ≤1 or BSA <3%, the IGA × BSA cutoff with the best sensitivity and specificity was 2.98 at week 12 (YI, 0.91; sensitivity, 0.99; specificity, 0.92), 2.80 at week 24 (YI, 0.94; sensitivity, 0.99; specificity, 0.95), and 3.00 at week 52 (YI, 0.96; sensitivity, 1.00; specificity, 0.96) (Table 3; online suppl. Fig. 2).
Table 3.
Optimal IGA × BSA cutoffs for predictability of PASI score ≤1 or BSA <3% MDA definition (pooled secukinumab 300 mg treatment group)
| Week | IGA × BSA | Sensitivity | Specificity | Youdenindexa |
|---|---|---|---|---|
| 2 | 3.50 | 0.9985 | 1.0000 | 0.99850 |
| 3 | 4.50 | 0.9849 | 1.0000 | 0.98487 |
| 4 | 5.20 | 0.9637 | 0.9583 | 0.92203 |
| 8 | 2.99 | 0.9906 | 0.8972 | 0.88782 |
| 12 | 2.98 | 0.9897 | 0.9167 | 0.90636 |
| 13 | 3.00 | 0.9851 | 0.9419 | 0.92701 |
| 14 | 3.10 | 0.9677 | 0.9269 | 0.89464 |
| 15 | 3.00 | 0.9832 | 0.9511 | 0.93439 |
| 16 | 3.00 | 0.9750 | 0.9551 | 0.93015 |
| 20 | 3.00 | 0.9937 | 0.9503 | 0.94393 |
| 24 | 2.80 | 0.9928 | 0.9470 | 0.93978 |
| 28 | 2.80 | 1.0000 | 0.9360 | 0.93596 |
| 32 | 2.65 | 1.0000 | 0.9521 | 0.95214 |
| 36 | 3.00 | 1.0000 | 0.9645 | 0.96447 |
| 40 | 3.00 | 0.9915 | 0.9617 | 0.95326 |
| 44 | 3.00 | 0.9836 | 0.9485 | 0.93206 |
| 48 | 3.00 | 1.0000 | 0.9490 | 0.94898 |
| 52 | 3.00 | 1.0000 | 0.9631 | 0.96306 |
BSA, body surface area; IGA, 5-point Investigator's Global Assessment; MDA, minimal disease activity; PASI, Psoriasis Area and Severity Index.
Youden index = sensitivity + specificity − 1.
Discussion
This post hoc analysis of four phase 3 clinical trials in patients with moderate-to-severe psoriasis receiving secukinumab 300 mg showed that an IGA × BSA cutoff of 2.10–2.98 at week 12 could be a valid measure highly associated with achievement of MDA. A lower cutoff value may be needed for evaluations up to week 52 (range, 1.00–3.00), but values were mostly within the ranges reported for week 12. These results are comparable to the PGA × BSA banding of 0.0–3.0 that correlated with achievement of MDA defined as PASI ≥90 and DLQI 0/1 [14]. This further indicates the validity of IGA × BSA as a composite tool for assessing clinical response to treatment.
The treat-to-target approach has become the recommended strategy for the treatment of patients with psoriasis. New National Psoriasis Foundation guidelines for the treatment of psoriasis state that the initial treatment goal should be to reduce BSA to ≤1% after 3 months; however, a reduction in BSA to ≤3% is considered an acceptable response [5]. Calculating the optimal IGA × BSA cutoff (2.98) at week 12 on the basis of BSA <3% aligns with the treat-to-target goal. Nevertheless, a more meaningful assessment of MDA that coincides with clinical trial endpoints in patients with moderate-to-severe psoriasis is needed in routine clinical practice and could also be a clinically relevant measure for database analyses. IGA × BSA is strongly correlated with absolute PASI score, providing further support that IGA × BSA captures disease severity and could be used to evaluate treatment response in place of the PASI. Furthermore, IGA × BSA cutoff values associated with MDA measures of PASI 90 and DLQI 0/1 include health-care provider– and patient-reported outcomes that allow patients and providers to be partners in their treat-to-target strategies, while also providing insight into patient quality of life as affected by skin clarity.
The IGA/PGA is categorized into 2 distinct basic forms: a static form, which measures the physician's evaluation of the disease activity at a single point, and a dynamic form, in which the physician assesses the global improvement from the baseline disease activity [19]. The US Food and Drug Administration prefers static IGA/PGA; thus, clinical research generally uses static IGA/PGA instruments. However, multiple versions of the static IGA/PGA exist, ranging from a 4-point to an 11-point scale, with varying descriptions of each point value [20, 21]. The static 5-point IGA scale, which was modified from the 6-point IGA/PGA scale [22], has become the standard form used in many phase 3 clinical trials [16, 17, 18]. Notably, the IGA/PGA does not account for the extent of disease. Therefore, IGA × BSA can aid physicians in the evaluation of treatment responses and assessments of therapeutic options to optimize patient care.
Limitations
Despite several strengths, this study has a few limitations, mainly related to the nature of the analysis. This was a post hoc analysis using pooled trial data, the use of which was not prespecified in the protocol of the individual studies. Furthermore, no adjustments for any potential confounding variables were conducted using multivariate analyses. Currently, there is no agreed-upon standard IGA/PGA to be used for clinical assessment of disease activity; the 5- and 6-point forms commonly used in clinical trials have different definitions of each scale value, complicating the physician's ability to efficiently and consistently measure treat-to-target goals. Including patients treated with the highly effective biologic agent secukinumab in this study leaves the potential for underestimation of cutoff values when evaluating the efficacy of other therapies; this measure needs to be tested in studies that include other psoriasis treatments. As IGA × BSA was validated as an indication of MDA achievement only for patients with moderate-to-severe psoriasis, further examination of the criteria is needed for patients with all levels of psoriasis severity.
Conclusion
This exploratory post hoc analysis identified IGA × BSA as a potential simple tool to assess achievement of MDA as a treat-to-target goal; however, additional observational studies with other psoriasis treatments are needed to further investigate this measure. For example, studies examining and comparing the cutoff values for other psoriasis treatments to identify treatment targets should be conducted to provide information that may be used by physicians for making proper formulary decisions. Findings from this study may provide physicians with a more practical way to capture disease activity in routine clinical practice beyond the traditional PASI.
Key Message
IGA × BSA may provide clinicians with a simple tool to measure treat-to-target goals.
Statement of Ethics
This article is based on previously conducted studies and does not involve any new studies of humans or animal subjects performed by any of the authors. The previously conducted individual study protocols were approved by institutional review boards or ethics committees at all investigational sites. These studies were conducted in accordance with the ethical principles of the Declaration of Helsinki, and US sites maintained compliance with Health Insurance Portability and Accountability Act regulations. All study subjects were required to provide written consent prior to participating. Clinicaltrials.gov listings are as follows: NCT01365455, NCT01358578, NCT01555125, and NCT01636687.
Disclosure Statement
Dr. Gottlieb has served as an advisor, consultant, or speaker for Janssen, Celgene, Bristol-Myers Squibb, Beiersdorf, AbbVie, UCB, Novartis, Incyte, Eli Lilly and Company, Dr. Reddy's Laboratories, Valeant, Dermira, Allergan, and Sun Pharmaceutical Industries and has received research funding from Janssen, Incyte, UCB, Novartis, and Eli Lilly and Company. Drs. Germino, Herrera, and Meng are employees of Novartis. Dr. Merola has served as a consultant, advisor, or investigator for Biogen Idec, AbbVie, Eli Lilly and Company, Novartis, Pfizer, Janssen, UCB, Samumed, Celgene, Sanofi Regeneron, Merck, and GlaxoSmithKline.
Funding Sources
This study was sponsored by Novartis Pharmaceuticals Corporation, East Hanover, NJ, USA.
Author Contributions
All authors made substantial contributions to the conception and design, execution, or analysis and interpretation of the data; were involved in drafting and critically revising the manuscript; have given necessary attention to ensure the integrity of the work; have read and approved all versions of this manuscript.
Supplementary Material
Supplementary data
Supplementary data
Acknowledgments
Support for third-party writing assistance for this manuscript, furnished by Meaghan Paganelli, PhD, and Eric Deutsch, PhD, CMPP, of Health Interactions, Inc., was provided by Novartis Pharmaceuticals Corporation.
References
- 1.Myers WA, Gottlieb AB, Mease P. Psoriasis and psoriatic arthritis: clinical features and disease mechanisms. Clin Dermatol. 2006 Sep-Oct;24((5)):438–47. doi: 10.1016/j.clindermatol.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 2.Langley RG, Krueger GG, Griffiths CE. Psoriasis: Epidemiology, clinical features, and quality of life. Ann Rheum Dis. 2005 Mar;64(Suppl 2) doi: 10.1136/ard.2004.033217. ii18-23;64 Suppl 2:ii18,23; discussion ii24-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Greb JE, Merola J, Garg A, Latella J, Howard L, Acharya N, et al. The psoriatic disease payer advisory panel. J Drugs Dermatol. 2016 May;15((5)):641–4. [PubMed] [Google Scholar]
- 4.Menter A, Gottlieb A, Feldman SR, Van Voorhees AS, Leonardi CL, Gordon KB, et al. Guidelines of care for the management of psoriasis and psoriatic arthritis: Section 1. Overview of psoriasis and guidelines of care for the treatment of psoriasis with biologics. J Am Acad Dermatol. 2008 May;58((5)):826–50. doi: 10.1016/j.jaad.2008.02.039. [DOI] [PubMed] [Google Scholar]
- 5.Armstrong AW, Siegel MP, Bagel J, Boh EE, Buell M, Cooper KD, et al. From the medical board of the national psoriasis foundation: treatment targets for plaque psoriasis. J Am Acad Dermatol. 2017 Feb;76((2)):290–8. doi: 10.1016/j.jaad.2016.10.017. [DOI] [PubMed] [Google Scholar]
- 6.van de Kerkhof PC. On the limitations of the psoriasis area and severity index (PASI) Br J Dermatol. 1992 Feb;126((2)):205–6. doi: 10.1111/j.1365-2133.1992.tb07827.x. [DOI] [PubMed] [Google Scholar]
- 7.Walsh JA, McFadden M, Woodcock J, Clegg DO, Helliwell P, Dommasch E, et al. Product of the Physician Global Assessment and body surface area: a simple static measure of psoriasis severity in a longitudinal cohort. J Am Acad Dermatol. 2013 Dec;69((6)):931–7. doi: 10.1016/j.jaad.2013.07.040. [DOI] [PubMed] [Google Scholar]
- 8.Greb JE, Garber C, Gottlieb AB. Effect of psoriatic arthritis on treatment response in patients with moderate to severe psoriasis. J Drugs Dermatol. 2016 Aug;15((8)):917–22. [PubMed] [Google Scholar]
- 9.Sorensen EP, Fanucci KA, Saraiya A, Volf E, Au SC, Argobi Y, et al. Tumor necrosis factor inhibitor primary failure predicts decreased ustekinumab efficacy in psoriasis patients. J Drugs Dermatol. 2015 Aug;14((8)):893–8. [PubMed] [Google Scholar]
- 10.Garber C, Plotnikova N, Au SC, Sorensen EP, Gottlieb A. Biologic and conventional systemic therapies show similar safety and efficacy in elderly and adult patients with moderate to severe psoriasis. J Drugs Dermatol. 2015 Aug;14((8)):846–52. [PubMed] [Google Scholar]
- 11.Buzney CD, Peterman C, Saraiya A, Au SC, Dumont N, Mansfield R, et al. Clearance of psoriasis: the impact of private versus public insurance. J Drugs Dermatol. 2015 Feb;14((2)):119–25. [PubMed] [Google Scholar]
- 12.Chiesa Fuxench ZC, Callis Duffin K, Siegel M, Van Voorhees AS, Gelfand JM. Validity of the Simple-Measure for Assessing Psoriasis Activity (S-MAPA) for objectively evaluating disease severity in patients with plaque psoriasis. J Am Acad Dermatol. 2015 Nov;73((5)):868–70. doi: 10.1016/j.jaad.2015.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Merola JF, Amato DA, See K, Burge R, Mallinckrodt C, Ojeh CK, et al. Evaluation of sPGA x BSA as an outcome measure and treatment target for clinical practice. J Invest Dermatol. 2018 Sep;138((9)):1955–61. doi: 10.1016/j.jid.2018.01.041. [DOI] [PubMed] [Google Scholar]
- 14.Gottlieb AB, Merola JF, Chen R, Levi E, Duffin KC. Assessing clinical response and defining minimal disease activity in plaque psoriasis with the Physician Global Assessment and body surface area (PGA × BSA) composite tool: an analysis of apremilast phase 3 ESTEEM data. J Am Acad Dermatol. 2017 Dec;77((6)):1178–80. doi: 10.1016/j.jaad.2017.06.162. [DOI] [PubMed] [Google Scholar]
- 15.Duffin KC, Papp KA, Bagel J, Levi E, Chen R, Gottlieb AB. Evaluation of the physician global assessment and body surface area composite tool for assessing psoriasis response to apremilast therapy: results from ESTEEM 1 and ESTEEM 2. J Drugs Dermatol. 2017 Feb;16((2)):147–53. [PubMed] [Google Scholar]
- 16.Langley RG, Elewski BE, Lebwohl M, Reich K, Griffiths CE, Papp K, et al. ERASURE Study Group. FIXTURE Study Group Secukinumab in plaque psoriasis—results of two phase 3 trials. N Engl J Med. 2014 Jul;371((4)):326–38. doi: 10.1056/NEJMoa1314258. [DOI] [PubMed] [Google Scholar]
- 17.Blauvelt A, Prinz JC, Gottlieb AB, Kingo K, Sofen H, Ruer-Mulard M, et al. FEATURE Study Group Secukinumab administration by pre-filled syringe: efficacy, safety and usability results from a randomized controlled trial in psoriasis (FEATURE) Br J Dermatol. 2015 Feb;172((2)):484–93. doi: 10.1111/bjd.13348. [DOI] [PubMed] [Google Scholar]
- 18.Paul C, Lacour JP, Tedremets L, Kreutzer K, Jazayeri S, Adams S, et al. JUNCTURE study group Efficacy, safety and usability of secukinumab administration by autoinjector/pen in psoriasis: a randomized, controlled trial (JUNCTURE) J Eur Acad Dermatol Venereol. 2015 Jun;29((6)):1082–90. doi: 10.1111/jdv.12751. [DOI] [PubMed] [Google Scholar]
- 19.Feldman SR, Krueger GG. Psoriasis assessment tools in clinical trials. Ann Rheum Dis. 2005 Mar;64(Suppl 2) doi: 10.1136/ard.2004.031237. ii65-8;64 Suppl 2:ii65,8; discussion ii69-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nijsten T, Looman CW, Stern RS. Clinical severity of psoriasis in last 20 years of PUVA study. Arch Dermatol. 2007 Sep;143((9)):1113–21. doi: 10.1001/archderm.143.9.1113. [DOI] [PubMed] [Google Scholar]
- 21.Heydendael VM, Spuls PI, Opmeer BC, de Borgie CA, Reitsma JB, Goldschmidt WF, et al. Methotrexate versus cyclosporine in moderate-to-severe chronic plaque psoriasis. N Engl J Med. 2003 Aug;349((7)):658–65. doi: 10.1056/NEJMoa021359. [DOI] [PubMed] [Google Scholar]
- 22.Gottlieb AB, Griffiths CE, Ho VC, Lahfa M, Mrowietz U, Murrell DF, et al. Multi-Centre Investigator Group Oral pimecrolimus in the treatment of moderate to severe chronic plaque-type psoriasis: a double-blind, multicentre, randomized, dose-finding trial. Br J Dermatol. 2005 Jun;152((6)):1219–27. doi: 10.1111/j.1365-2133.2005.06661.x. [DOI] [PubMed] [Google Scholar]
- 23.Strober B, Papp KA, Lebwohl M, Reich K, Paul C, Blauvelt A, Gordon KB, Milmont CE, Viswanathan HN, Li J, Pinto L, Harrison DJ, Kricorian G, Nirula A, Klekotka P. Clinical meaningfulness of complete skin clearance in psoriasis. J Am Acad Dermatol. 2016 Jul;75((1)):77.e7–82.e7. doi: 10.1016/j.jaad.2016.03.026. [DOI] [PubMed] [Google Scholar]
- 24.Coates LC, Fransen J, Helliwell PS. Defining minimal disease activity in psoriatic arthritis: a proposed objective target for treatment. Ann Rheum Dis. 2010 Jan;69((1)):48–53. doi: 10.1136/ard.2008.102053. [DOI] [PubMed] [Google Scholar]
- 25.Langley RG, Feldman SR, Nyirady J, van de Kerkhof P, Papavassilis C. The 5-point Investigator's Global Assessment (IGA) Scale: A modified tool for evaluating plaque psoriasis severity in clinical trials. J Dermatolog Treat. 2015 Feb;26((1)):23–31. doi: 10.3109/09546634.2013.865009. [DOI] [PubMed] [Google Scholar]
- 26.Youden WJ. Index for rating diagnostic tests. Cancer. 1950 Jan;3((1)):32–5. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary data
Supplementary data