Abstract
INTRODUCTION:
Findings from studies examining the relationship between dementia and suicide have been inconsistent. This study examined the characteristics, precipitants, and risk factors for suicide among persons with dementia.
METHODS:
Data from the Georgia Alzheimer’s Disease and Related Dementia (ADRD) registry were linked with 2013-2016 data from Georgia Vital Records and Georgia Violent Death Reporting System. Descriptive statistics were calculated and logistic regression was used to examine risk factors for suicide.
RESULTS:
Ninety-one Georgia residents with dementia who died by suicide were identified. Among decedents with known circumstances, common precipitants included depressed mood (38.7%) and physical health problems (72.6%). Suicide rate among persons with dementia was 9.3/100,000 person-years overall and substantially higher among those diagnosed in the past 12 months (424.5/100,000 person-years). Being male, dementia diagnosis before age 65, and a recent diagnosis of dementia independently predicted suicide, but not depression or cardiovascular diseases.
CONCLUSION:
Prevention strategies that identify at-risk individuals, provide support, and ensure continuity of care for persons diagnosed with dementia may help reduce suicide in this population.
INTRODUCTION
Suicide is a major public health problem throughout the life course. In 2016, suicide was the 10th leading cause of death in the United States (U.S.), with approximately 45,000 individuals taking their own lives.1 During this time, approximately 8,200 older adults aged 65 years and older died by suicide, representing an age-adjusted suicide rate of 16.8 per 100,000 population, which was a little higher than the national rate of 13.5 per 100,000.1 Suicide is generally the result of multiple factors such as mental health problems, substance use, stressful life events, and social isolation.2-3 In addition, comorbid medical conditions and life threatening illnesses such as Alzheimer’s disease and related dementia (ADRD) have been noted to increase the risk of suicide in older adults.4-6 Understanding the characteristics of persons with dementia who die by suicide, as well as the risk factors for suicide in this population is critical for suicide prevention efforts.
Dementia is common among older Americans. In 2002, approximately 13.8% of Americans aged 71 years and older had dementia.7 Alzheimer’s disease is the most common form of dementia in the U.S., accounting for about 70% of all cases.7 It is estimated that nearly 10% of Americans (representing 5.3 million people) aged 65 years and older were living with Alzheimer’s disease in 2017.8
The prevalence of non-fatal suicidal behaviors among persons with dementia and the role of dementia in suicide among older populations has been debated in the literature. Previous studies have also reported conflicting results on the association between dementia and completed suicide.9 Studies finding no association between dementia and suicide have cited reasons such as the low estimated prevalence of suicide attempts (less than 1%), limited cognitive abilities to plan and carry out suicide, and increased supervision and limited access to lethal means among persons with dementia.5, 10-11 Yet psychosocial impairment, decline in cognitive function, and disability are factors that may place those with dementia at increased risk for suicide.5, 12 For example, dementia is often associated with neuropsychiatric symptoms such as anxiety, major depression, delusions, irritability, hallucinations and agitation, with about 90% of all dementia patients experiencing one or more of these symptoms over the course of the disease.13 These psychological symptoms are also risk factors for suicidal behaviors in older adults, and might provide insight into the connection between dementia and suicide.14-16 Previous studies that found an association between dementia and suicide have noted a number of risk factors for suicide among persons with dementia, including disease awareness, early age of disease onset, and recent diagnosis of dementia.17-20 For example a case report about a person with young onset of dementia noted that the patient had observed memory decline, high degree of dependence, experience of depression, and suicidal behaviors.17 Another study noted that young onset of dementia was associated with preserved awareness, which was associated with depressive symptoms and suicidal behaviors.18 A study using data from Veterans Affairs also observed that among persons with dementia, depression, history of inpatient psychiatric hospitalizations, anti-depressants prescription fills, and a recent diagnosis of dementia were associated with suicide.20 Using a selective literature review, Draper and colleagues also noted that early dementia or mild cognitive changes was associated with increased risk of suicide.19 Explaining this association, Hiesel and colleagues suggested that major depression and hopelessness, which are common among patients with dementia, may mediate the effect of cognitive functioning on suicidal behaviors, and may actually be exacerbated by the failure of the patient to respond to anti-dementia medication.21 Consistent with this explanation, some studies have reported on suicides among patients in the early stages of Alzheimer’s disease who did not respond to treatment with a cholinesterase inhibitor, a medication used to treat Alzheimer’s disease symptoms.22-23 Whereas these previous studies have provided some insight into the association between dementia and suicidal behaviors, they either utilized limited sample sizes,17 a specialized population,20 or a population outside the U.S. (Netherlands).18 These studies also provided limited information about patients’ dementia diagnosis and circumstances surrounding the suicide to provide the needed context and description of this population.6, 24-25
The Georgia Alzheimer’s disease and related dementia registry and violent death reporting system data provide a unique dataset and an opportunity to examine suicide among persons with dementia at the population level. Addressing some of the limitations in the previous work, the current study has two main objectives – 1) to describe the characteristics and circumstances of suicide among persons with dementia and 2) to examine some of the risk factors associated with suicide among persons with dementia. Specifically, depression and cardiovascular disease (CVD) diagnosis were examined due to their established association with suicide in older adults.26-27
METHODS
Data Sources
Three datasets were used – 1) the Georgia Alzheimer’s Disease and Related Dementia (ADRD) registry, 2) the Georgia Violent Death Reporting System (GA-VDRS), and 3) the Georgia Vital Records death data. The Georgia ADRD registry is a population-based registry of Georgia residents with diagnosis of ADRD. Established in 2014, the ADRD registry collects data from multiple sources, including reporting by physicians, Georgia Vital Statistics Records, emergency department visits and hospital discharge records, and Georgia Medicaid, Medicare, and State Health Benefit Plan claims.28 This study used 2013-2014 fee-for-service claims data for Georgia Medicare beneficiaries. The data provided information on demographic characteristics of beneficiaries and contained flags that indicated the diagnosis of, or treatment for, 27 common chronic conditions during a three-year reference period.29 Although the Medicare fee-for-service dataset was only for 2013-2014, it had decades’ worth of historical information for cases on when beneficiaries were first diagnosed with any of the 27 common chronic conditions. A person was flagged as ADRD if there is a valid ADRD International Classification of Diseases, 9th Revision (ICD-9), Current Procedural Terminology, 4th Edition (CPT4), or Healthcare Common Procedure Coding System (HCPCS) claim for at least one inpatient, skilled nursing facility, home health agency, hospital outpatient, or carrier claim.30 All variables used in the logistic regression model including dementia, depression, and cardiovascular diseases (CVD) diagnosis came from the Georgia ADRD registry data.
The Georgia Violent Death Reporting System (GA-VDRS), a part of the CDC’s National Violent Death Reporting System,31 is an active surveillance system of all violent deaths in Georgia including suicides, homicides, and legal intervention deaths. It collects and links information from multiple sources, including death certificates, coroner and medical examiner reports, and law enforcement reports, into a single record. Using information from law enforcement and CME reports, trained data abstractors coded for the presence of a number of potential precipitators of suicide, such as mental health problems, physical health problems, history of drug or alcohol abuse, as well as history of suicidal behaviors. Data from 2013-2016 were included in this study. A detailed description of the NVDRS methodology has been reported elsewhere.31 The Georgia Vital Records data on deaths is maintained by the Georgia Department of Public Health Office of Vital Records. The data received from this source included information on the manner of death, ICD-10 codes, and demographic characteristics of decedents.
The Georgia Department of Public Health Institutional Review Board (project #161107) approved the study protocol.
Case selection and data linking procedure
Several steps were taken to identify and link cases across the data systems (Figure). First, the 2013-2014 ADRD Medicare fee-for-service data were linked to the 2013-2016 death data from the Georgia Vital Records using decedents’ 9-digit social security number (Data 1). This linkage was done to obtain (1) final dataset for estimating the rate of suicide, (2) dataset for logistic regression analyses, and (3) information on death certificate number, decedent’s name, date of death, and year of death for subsequent linkage with the GA-VDRS data. Next, the ADRD-death records linked dataset was linked with the 2013-2016 GA-VDRS data using last four digits of the victim’s death certificate number, first initial of last name, day of the month of death, and year of death (Data 2). To identify suicide decedents in the GA-VDRS data with dementia who were not in the ADRD-death data, a key word search was performed in the GA-VDRS law enforcement and coroner/medical examiners narrative fields using the following key words: dementia, Alzheimer’s, senile, presenile, delirium, amnestic, Huntington, pick, delusion, memory, memory loss, Parkinson, and forgetfulness. The cases identified through the key word search were independently reviewed and coded by two authors to ensure they met the case definition of individuals with dementia who died by suicide. Coded data were compared and where disagreement emerged, a joint review was performed, the case was discussed and agreement reached before including or excluding a case in the analyses. The agreement between the two independent reviewers was 98.5%. The final dataset for the survival analyses included all persons in the 2013-2014 ADRD Medicare fee-for-service data, linked with both the death data and GA-VDRS data.
Figure.
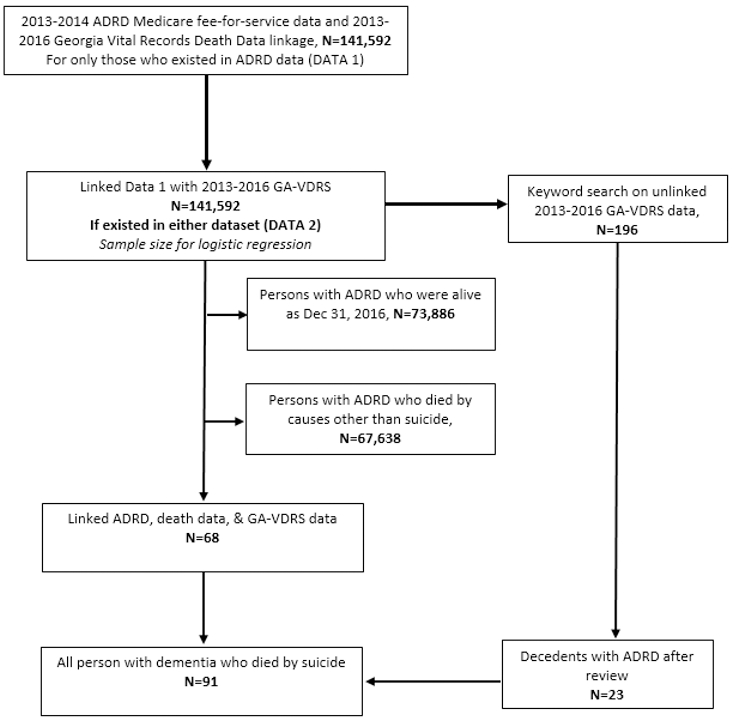
Data linkage and case selection
Statistical Analyses
Descriptive statistics were used to describe the demographic characteristics, precipitating circumstances, and method of suicide among persons with dementia who died by suicide during 2013-2016 in Georgia. Crude suicide mortality rates by person-years were estimated by dividing the number of suicides in a specific subpopulation by the number of person-years that ADRD patients were retrospectively followed from the dementia diagnosis date. All crude suicide mortality rates were reported per 100,000 person-years.
Logistic regression was used to identify potential predictors of suicide in this population. Logistic regression analyses were used because there were no loss to follow-up during the time under consideration and there were few cases that experienced the outcome, thus making the power of logistic regression similar to a proportional hazard model.32 In addition, a proportional cause-specific hazard model was used to check for consistency of the results. The conclusions from both models were similar, except for depression, which was significant in the proportional hazard model (as a time-varying covariate) but was not statistically significant in the logistic regression models. However, due to small number of cases experiencing the outcome and the concerns that the computationally demanding hazard model may not fit the data well, only the logistic regression analyses results are presented. Unadjusted and adjusted odds ratios were estimated for sex, age at dementia diagnosis, length of time since dementia diagnosis, depression, and CVD (if patient had the diagnosis of one or more of the following conditions: hypertension, stroke, acute myocardial infarction, atrial fibrillation, congestive heart failure, and ischemic heart attack). Due to privacy concerns, circumstances with fewer than six decedents in the numerator were excluded from the results tables. All data management and statistical analyses were performed in SAS version 9.4.
RESULTS
Study population
There were 141,592 persons with dementia in the 2013-2014 Medicare fee-for-service ADRD registry data. Linkage of these data with the death data identified 67,706 persons with dementia who died during 2013-2016 (i.e., “Data 1”). The linkage of the GA-VDRS data with Data 1 yielded 68 persons with dementia who died by suicide. The text search yielded an additional 196 suicide decedents who potentially had dementia, 23 of whom were identified as individuals with dementia after careful review and coding of cases. The total cases included at different stages of the analyses were: 91 for descriptive statistics of suicide among persons with dementia and all 141,592 persons with dementia diagnosis in the logistic regression analyses (Figure).
Demographic and Other Characteristics of suicide decedents
Among individuals with dementia who died by suicide (n=91), 69.2% were male, 54.9% were older than 75 years, and 93.4% were white. About 47.0% of decedents had a high school degree or higher; 41.8% were married, in civil union, or were in a domestic partnership (41.8%); and 35.2% had served in the U.S. Armed Forces (Table 2). Additionally, the most common method of suicide was firearm (55.0%), followed by poisoning (13.2%). Sixty-seven percent of decedents sustained the fatal injury at home (Table 1).
Table 2.
Common precipitating circumstances of suicide decedents with dementia (n=62)*, Georgia, 2013-2016
| Variable | N | Percent |
|---|---|---|
| Current Diagnosed mental health problems | 19 | 30.7 |
| Current mental health treatment† | 7 | 36.8 |
| Current depressed mood | 24 | 38.7 |
| History of mental health problems | 6 | 9.7 |
| Physical health problems | 45 | 72.6 |
| Physical health as a crisis‡ | 15 | 33.3 |
| History of suicide thoughts or attempt | 23 | 37.1 |
| Disclosed intent | 13 | 21.0 |
| Left a suicide note | 14 | 22.5 |
The original number of cases for examining the precipitating circumstances was 91 but 29 decedents who were missing information on all circumstances were excluded from the analyses, bringing the analytic sample size to 62 cases.
The denominator are individuals with diagnosed mental health problems.
The denominator are individuals with physical health problems.
Table 1.
Demographic and Other Characteristics of Suicide Decedents with Dementia (n=91), Georgia, 2013-2016.
| Variable | Dementia Suicide Decedents | |
|---|---|---|
| n | Percent | |
| Sex | ||
| Male | 63 | 69.2 |
| Female | 28 | 30.8 |
| Age Group | ||
| Under 65years | 14 | 15.4 |
| 65-74 years | 27 | 29.7 |
| 75 years and older | 50 | 54.9 |
| Race/Ethnicity | ||
| White | 85 | 93.4 |
| Non-white | 6 | 6.6 |
| Educational Level | ||
| Less than HS | 14 | 15.4 |
| HS Grads and higher | 43 | 47.3 |
| Unknown/missing | 34 | 37.3 |
| Marital Status | ||
| Married/civil union/domestic partnership | 38 | 41.8 |
| Widowed | 25 | 27.5 |
| Other/unknown* | 28 | 30.7 |
| Ever served in U.S. Armed Forces | ||
| Yes | 32 | 35.2 |
| No | 55 | 60.4 |
| Unknown/missing | 7 | 4.4 |
| Mechanism of suicide | ||
| Firearm | 50 | 55.0 |
| Poisoning | 12 | 13.2 |
| Other/unknown† | 29 | 31.8 |
| Location of injury | ||
| Home | 61 | 67.0 |
| Other/unknown‡ | 30 | 33.0 |
Included never married, single or otherwise not specified, divorced, married, but separated, and unknown.
Included sharp instrument, hanging, strangulation, suffocation, fall, drowning, motor vehicle, and unknown.
Included street/road, sidewalk, alley, motor vehicle, natural area (such as field and woods), and unknown.
Precipitating Circumstances
Twenty-nine of the 91 decedents were missing information on all circumstance variables, decreasing the analytic sample size for the precipitating circumstances to 62. Of those with data, common precipitating circumstances included a mental health problem diagnosis (30.7%), depressed mood (38.7%), history of mental health problems (9.7%), and physical health problems (72.6%). Among those with a mental health problem diagnosis at the time of death, over a third (36.8%) were in treatment. Of those with physical health problems, 33.3% had experienced the physical health event as a recent crisis, defined as an event within 2 weeks of death that was indicated to have contributed to the suicide. Over 37.0% of decedents with information had a history of suicidal thoughts or attempts, 21.0% had disclosed their intent to die by suicide, and 22.5% left a suicide note (Table 2).
Rate of suicide and logistic regression analyses
There were 141,592 Medicare fee-for-service beneficiaries flagged as having dementia in Georgia and who existed in the ADRD registry as of December 31st, 2016. Approximately 65% were female, 8.1% were diagnosed with dementia before age 65 years and 65.3% were diagnosed after the age of 75 years (Table 3). Among this group, 68 died by suicide and 67,638 died by other causes between January 1, 2013 and December 31, 2016. Between the time of dementia diagnosis and death or end of study, persons with dementia were retrospectively followed (from the date they first met diagnosis criteria for dementia) a total of 732,101 person-years, with a median follow-up time of 4.3 person-years. For individuals who died by suicide, the median time from dementia diagnosis to suicide was 2.1 years, with 11 decedents dying within 70 days from the date of dementia diagnosis.
Table 3.
Unadjusted mortality rates among persons with dementia who died by suicide, Georgia, 2013-2016
| Variable | Total Sample |
# of suicides |
# of person- years followed |
Unadjusted Rate/ 100,000 (95% CI) |
|
|---|---|---|---|---|---|
| n | % | ||||
| Total | 141592 | 100 | 68 | 732101 | 9.3 (7.1-11.5) |
| Sex | |||||
| Male | 49669 | 35.1 | 52 | 231336 | 22.5 (16.3-28.6) |
| Female | 91923 | 64.9 | 16 | 500766 | 3.2 (1.6-4.8) |
| Age at dementia diagnosis | |||||
| Under 65 yrs | 11415 | 8.1 | 13 | 65355 | 19.9 (9.0-30.7) |
| 65-74 yrs | 37692 | 26.6 | 26 | 223932 | 11.6 (7.1-16.1) |
| 75+ yrs | 92485 | 65.3 | 29 | 442813 | 6.5 (4.2-8.9) |
| Time since diagnosis* | |||||
| Up to 12 months | 13298 | 9.4 | 22 | 5183 | 424.5 (247.1-601.8) |
| 12-24 months | 10213 | 7.2 | 11 | 16530 | 66.5 (27.2-105.9) |
| More than 24 months | 118027 | 83.4 | 35 | 710392 | 4.9 (3.3-6.6) |
| Depression diagnosis | |||||
| Yes | 42365 | 29.9 | 23 | 213215 | 10.8 (6.3-15.2) |
| No | 99227 | 70.1 | 45 | 513215 | 8.8 (6.2-11.3) |
| Cardiovascular diseases† | |||||
| Yes | 115315 | 81.4 | 51 | 582487 | 8.8 (6.4-11.2) |
| No | 26228 | 18.5 | 17 | 149615 | 11.4 (6.0-16.8) |
Number of months between dementia diagnosis and death by suicide.
Included the diagnosis of one or more of the following conditions - hypertension, stroke, acute myocardial infarction, atrial fibrillation, congestive heart failure, and ischemic heart attack.
CI=Confidence Interval.
Among those with dementia diagnosis, the overall unadjusted suicide rate was 9.3 per 100,000 person-years. The rate varied by demographic characteristics and other selected factors. The rate was higher for males than females and for those diagnosed with dementia before age 65 years than those diagnosed after age 75 years. Additionally, the rate was higher for those recently diagnosed with dementia. For instance, the rate was over 86 times higher for those who had been diagnosed with dementia within the previous 12 months compared to those who had been diagnosed more than 2 years ago (Table 3).
In both the unadjusted and adjusted logistic regression models, being male, being diagnosed with dementia before age 65 years, and being diagnosed with dementia in the past 12 months were independent predictors of suicide in this population. In the adjusted model, males had approximately 5 times higher odds of dying by suicide than females. Those diagnosed with dementia before age 65 had over 3 times higher odds of dying by suicide than those diagnosed at or after age 75, and those diagnosed with dementia within the previous 12 months had 6 times higher odds of dying by suicide than those diagnosed more than 24 months ago. However, neither depression nor CVD diagnosis was a significant independent predictor of suicide among this population (Table 4).
Table 4.
Crude and adjusted odds for suicide among persons with dementia, Georgia, 2013-2016
| Variable | n | Unadjusted OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|---|
| Sex | |||
| Male | 49669 | 6.0 (3.4-10.5) | 4.8 (2.7-8.4) |
| Female | 91923 | -- | -- |
| Age at dementia diagnosis | |||
| Under 65yrs | 11415 | 3.6 (1.9-7.0) | 3.3 (1.7-6.4) |
| 65-74yrs | 37692 | 2.2 (1.3-3.7) | 2.3 (1.4-4.0) |
| 75+yrs | 92485 | -- | -- |
| Time since dementia diagnosis | |||
| Up to 12 months | 13298 | 5.5 (3.3-9.5) | 6.0 (3.5-10.4) |
| 12-24months | 10213 | 3.6 (1.8-7.2) | 3.9 (2.0-7.7) |
| More than 24months | 118027 | -- | -- |
| Depression diagnosis | |||
| Yes | 42365 | 1.2 (0.7-2.0) | 1.3 (0.7-2.1) |
| No | 99227 | -- | -- |
| Cardiovascular diseases† | |||
| Yes | 115315 | 0.7 (0.4-1.2) | 0.6 (0.3-1.0) |
| No | 26228 | -- | -- |
Included the diagnosis of one or more of the following conditions - hypertension, stroke, acute myocardial infarction, atrial fibrillation, congestive heart failure, and ischemic heart attack.
OR=Odds Ratio.
CI=Confidence Interval.
The adjusted OR for each variable controlled for the other remaining variables listed on table.
DISCUSSION
During 2013 through 2016, 91 persons with dementia were identified to have died by suicide in Georgia (of which 68 existed in the ADRD registry). Among decedents, common precipitating circumstances included mental health and physical health problems and odds of suicide was higher among those who were male, those diagnosed with dementia at younger age, and those who had recently been diagnosed with dementia.
Suicide is a major public health problem that is usually the result of multiple factors. The finding that mental health problems and depressed mood were common precipitating circumstances in this population is consistent with psychological autopsy studies that have indicated that mental illnesses, particularly depression, are major contributing factors for suicide throughout the life course.27, 33 Because psychological symptoms, including major depression, are common in persons with dementia,13 early recognition, treatment, and management of these symptoms may improve the overall health of persons with dementia and may help reduce risk for suicide in this population.
However, in the logistic regression analyses, depression was not a significant predictor for suicide. One possible reason for this finding is that depression may have gone undiagnosed among those who died soon after dementia diagnosis, and therefore, depression may seem to have not played a role in those suicides. For example, 11 people died by suicide within 70 days after dementia diagnosis. During that time, there may have not been follow-up with a physician who could have diagnosed depression. Another reason could be that among those with dementia, increased suicide risk from range of other physical, emotional, and social stressors associated with dementia diagnosis may have overshadowed the effect of depression in predicting suicide.
Physical health problems, particularly debilitating (conditions that would generally leave a person confined to bed or to require basic care from others) and life threatening conditions, have also been identified as important risk factors for suicide in older adults.34 Consistent with this, physical health problems were common precipitating circumstance in this population, occurring in 7 out of 10 decedents. This was higher than a previously reported 5 in 10 adults aged 65 years and older whose suicide was precipitated by physical health problems.34 However, cardiovascular diseases did not predict suicide contrary to previous studies that noted that cardiovascular diseases are important predictors of suicide among older adults.26, 35 The non-significant association between suicide and CVD suggest that CVD may not contribute beyond the risk associated with dementia in this population. Other chronic diseases such as cancers, COPD, and hip fractures have also been associated with suicide in older adults.26, 35 However, because few decedents experienced these conditions in this study, they were not included in the analyses.
The study also found a higher rate and odds of suicide among persons with a recent dementia diagnosis. Individuals who were diagnosed in the previous 12 months had higher odds of dying by suicide than those diagnosed more than 24 months ago. Previous studies have noted an increased risk of suicide among persons who had been recently diagnosed with dementia.6, 20 Some have suggested that this may be because during the early stages of the disease, patients who are concerned about the progression of the disease and its impact on them and their families can plan and execute suicidal intentions when they have the mental capability to do so.5 Being diagnosed with dementia may also be devastating to patients due to social implications such as experience of shame, discrimination, rejection, social isolation, and perceived loss of control.36 A selective review of suicide risk among persons with dementia also noted that the increased risk of suicide after dementia diagnosis is often in the context of depression comorbidity.19 With the current recommendation to disclose dementia diagnoses to patients,37 the study findings suggest that patients may benefit from counselling and adequate support when dementia diagnoses are disclosed.
The findings that over half of decedents had used firearms for suicide is consistent with a recent study which noted that suicide by firearm was common among U.S. adults aged 50 years and older.38 Education and counselling programs for families and loved ones on safe storage of firearms for older adults at risk of suicide may be helpful in reducing suicide among this population.39
Finally, it is important to highlight the proportion of decedents with history of suicidal ideation, suicide attempt, or who disclosed their intentions to die by suicide. Although the timeline from the disclosure of suicidal intentions or attempts to the time of suicide could not be determined, most persons with dementia being older adults are likely to have regular encounters with the healthcare system. This may represent a missed opportunity for prevention. A previous study noted that about 77% of suicide decedents had visited a general practitioner in the three months prior to death by suicide.40 Therefore, an opportunity exists for health care providers to screen and identify older adults at higher risk for suicide, and provide appropriate care to such individuals. This is in light of evidence suggesting that identifying individuals at risk for suicide and providing support could reduce suicidal behaviors and associated risk factors.39 For example, Improving Mood- Promoting Access to Collaborative Treatment (IMPACT), a program aimed at preventing suicide in older individuals attending primary care has been found to be effective in reducing suicidal ideation and depression.41 Additionally, health care systems that successfully provide continuity of care, and ensure that health care providers system-wide closely follow patients over the course of their diagnoses, have demonstrated decreases in suicide; one such program is the Henry Ford Health System’s Perfect Depression Care program.42
LIMITATIONS
This study is subject to at least four limitations. First, the study may have underestimated the number of persons with dementia who died by suicide. This could be due to underestimation of death by suicide from the death certificate.43 Second, the data used were based on Medicare fee-for-service claims data. Individuals were classified as having dementia if they had a valid claim for diagnosis or treatment of dementia. As such, there is the possibility of a misclassification of individuals as having or not having dementia. However, the Centers for Medicaid and Medicare Services (CMS) applies specific algorithms to diagnoses and/or procedures codes in multiple claims files to identify persons with dementia, 29, 44 thus reducing the chances of misclassifying individuals’ dementia status. Third, since most of older adults gain eligibility for Medicare when they are 65 years old, those who were younger than 65 years and who did not qualify for Medicare are not included in this data. Therefore, the study may not be representative of all individuals with dementia in Georgia, although, dementia risk increases with age and the majority of individuals with dementia are aged 65 years and older7 For example, over 96% of individuals with Alzheimer’s disease are aged 65 years and older.8 Finally, the models did not fully control for socio-economic variables because they were not available in the current data.
CONCLUSIONS
Among persons with dementia, suicide predictors included being male, early age of dementia diagnosis, and diagnosis of dementia within the past 12 months. There is the need for suicide prevention efforts in this population that takes into account these factors. The Centers for Disease Control and Prevention released a technical package describing evidence-based prevention strategies and approaches that can assist states and communities in their efforts to reduce and prevent suicide. Approaches included in the technical package that are particularly relevant for preventing suicide persons with dementia include identifying and supporting people at risk through gatekeeper training and treatment for people at risk of suicide; strengthening access to and delivery of care for suicidal individuals; and creating protective environments, for instance by reducing access to lethal means among persons at risk of suicide.39 Specifically, counseling and provision of timely support for persons diagnosed with dementia, particularly those who are newly diagnosed, may help them to successfully navigate through the challenges that come with progression of the condition, and overcome the sense of burden associated with dementia-related debilitation.
ACKNOWLEDGEMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
This research was conducted in Atlanta as a collaboration between researchers at the U.S. Centers for Disease Control and Prevention and the Georgia Department of Public Health. Other than working in our official capacities as government employees (federal and state), this research was not supported by any other funds. The study has not yet been presented at any scientific conference/meeting.
REFERENCES
- 1.Ten Leading Causes of Injury Deaths by Age Group Highlighting Violence-Related Injury Deaths, United States - 2014. Atlanta, GA: CDC; 2014. [Google Scholar]
- 2.Conwell Y, Van Orden K, Caine ED. Suicide in older adults. Psychiatr Clin North Am. 2011;34(2):451–68, ix. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suresh Kumar PN, Anish PK, George B. Risk factors for suicide in elderly in comparison to younger age groups. Indian J Psychiatry. 2015;57(3):249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szanto K, Gildengers A, Mulsant BH, Brown G, Alexopoulos GS, Reynolds CF 3rd. Identification of suicidal ideation and prevention of suicidal behaviour in the elderly. Drugs Aging. 2002;19(1):11–24. [DOI] [PubMed] [Google Scholar]
- 5.Serafini G, Calcagno P, Lester D, Girardi P, Amore M, Pompili M. Suicide Risk in Alzheimer’s Disease: A Systematic Review. Curr Alzheimer Res. 2016;13(10):1083–99. [DOI] [PubMed] [Google Scholar]
- 6.Erlangsen A, Zarit SH, Conwell Y. Hospital-diagnosed dementia and suicide: a longitudinal study using prospective, nationwide register data. Am J Geriatr Psychiatry. 2008;16(3):220–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Plassman BL, Langa KM, Fisher GG, Heeringa SG, Weir DR, Ofstedal MB, Burke JR, Hurd MD, Potter GG, Rodgers WL, et al. Prevalence of dementia in the United States: the aging, demographics, and memory study. Neuroepidemiology. 2007;29(1-2):125–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alzheimer’s Disease Facts and Figures Alzheimers Dementia. Chicago, IL: Alzheimer’s Association; 2017. [Google Scholar]
- 9.Conejero I, Navucet S, Keller J, Olie E, Courtet P, Gabelle A. A Complex Relationship Between Suicide, Dementia, and Amyloid: A Narrative Review. Front Neurosci. 2018;12:371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schneider B, Maurer K, Frolich L. [Dementia and suicide]. Fortschr Neurol Psychiatr. 2001;69(4):164–9. [DOI] [PubMed] [Google Scholar]
- 11.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–28. [DOI] [PubMed] [Google Scholar]
- 12.Zarit SH, Zarit J. Dementia, delirium and other cognitive problems In: Zarit SH, Zarit J, editors. Mental Disorders in Older Adults: Fundamentals of Assessment and Treatment. New York: Guildford Press; 2006. p. 40–77. [Google Scholar]
- 13.Cerejeira J, Lagarto L, Mukaetova-Ladinska EB. Behavioral and psychological symptoms of dementia. Front Neurol. 2012;3:73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sachs-Ericsson N, Hames JL, Joiner TE, Corsentino E, Rushing NC, Palmer E, Gotlib IH, Selby EA, Zarit S, Steffens DC. Differences between suicide attempters and nonattempters in depressed older patients: depression severity, white-matter lesions, and cognitive functioning. Am J Geriatr Psychiatry. 2014;22(1):75–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kjelby E, Sinkeviciute I, Gjestad R, Kroken RA, Loberg EM, Jorgensen HA, Hugdahl K, Johnsen E. Suicidality in schizophrenia spectrum disorders: the relationship to hallucinations and persecutory delusions. Eur Psychiatry. 2015;30(7):830–6. [DOI] [PubMed] [Google Scholar]
- 16.Gonzalez-Rodriguez A, Molina-Andreu O, Navarro Odriozola V, Gasto Ferrer C, Penades R, Catalan R. Suicidal ideation and suicidal behaviour in delusional disorder: a clinical overview. Psychiatry J. 2014;2014:834901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baptista MAT, Santos RL, Kimura N, Lacerda IB, Dourado MCN. Disease awareness may increase risk of suicide in young onset dementia: A case report. Dement Neuropsychol. 2017;11(3):308–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.van Vliet D, de Vugt ME, Kohler S, Aalten P, Bakker C, Pijnenburg YA, Vernooij-Dassen MJ, Koopmans RT, Verhey FR. Awareness and its association with affective symptoms in young-onset and late-onset Alzheimer disease: a prospective study. Alzheimer Dis Assoc Disord. 2013;27(3):265–71. [DOI] [PubMed] [Google Scholar]
- 19.Draper B, Peisah C, Snowdon J, Brodaty H. Early dementia diagnosis and the risk of suicide and euthanasia. Alzheimers Dement. 2010;6(1):75–82. [DOI] [PubMed] [Google Scholar]
- 20.Seyfried LS, Kales HC, Ignacio RV, Conwell Y, Valenstein M. Predictors of suicide in patients with dementia. Alzheimers Dement 2011;7(6):567–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Heisel MJ, Flett GL, Besser A. Cognitive functioning and geriatric suicide ideation: testing a mediational model. Am J Geriatr Psychiatry. 2002;10(4):428–36. [PubMed] [Google Scholar]
- 22.Rohde K, Peskind ER, Raskind MA. Suicide in two patients with Alzheimer’s disease. J Am Geriatr Soc. 1995;43(2):187–9. [DOI] [PubMed] [Google Scholar]
- 23.Ferris SH, Hofeldt GT, Carbone G, Masciandaro P, Troetel WM, Imbimbo BP. Suicide in two patients with a diagnosis of probable Alzheimer disease. Alzheimer Dis Assoc Disord. 1999;13(2):88–90. [DOI] [PubMed] [Google Scholar]
- 24.Peisah C, Snowdon J, Kril J, Rodriguez M. Clinicopathological findings of suicide in the elderly: three cases. Suicide Life Threat Behav. 2007;37(6):648–58. [DOI] [PubMed] [Google Scholar]
- 25.Rubio A, Vestner AL, Stewart JM, Forbes NT, Conwell Y, Cox C. Suicide and Alzheimer’s pathology in the elderly: a case-control study. Biol Psychiatry. 2001;49(2):137–45. [DOI] [PubMed] [Google Scholar]
- 26.Erlangsen A, Stenager E, Conwell Y. Physical diseases as predictors of suicide in older adults: a nationwide, register-based cohort study. Soc Psychiatry Psychiatr Epidemiol. 2015;50(9):1427–39. [DOI] [PubMed] [Google Scholar]
- 27.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405. [DOI] [PubMed] [Google Scholar]
- 28.Alzheimer’s disease and related dementias among Medicare beneficiaries. Atlanta, GA: Georgia Department of Public Health; 2015. [Google Scholar]
- 29.Centers for Medicaid and Medicare Services. CCW Technical Guidance: Getting Started with CMS Medicare Administrative Research Files. Chronic Conditions Data Warehouse. . www.ccwdata.org/web/guest/technical-guidance-documentation/medicare-administrative-claims-training-course. Published 2016. Accessed December 6, 2017.
- 30.CMS Chronic Conditions Data Warehouse (CCW) -CCW Conditions Algorithms https://www.ccwdata.org/documents/10280/19139421/ccw-chronic-condition-algorithms.pdf. Published 2015. Accessed December 6, 2017.
- 31.Blair JM, Fowler KA, Jack SP, Crosby AE. The National Violent Death Reporting System: overview and future directions. Inj Prev 2016;22 Suppl 1:i6–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Syed H, Jorgensen AL, Morris AP. Evaluation of methodology for the analysis of ‘time-to-event’ data in pharmacogenomic genome-wide association studies. Pharmacogenomics. 2016;17(8):907–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Harwood D, Hawton K, Hope T, Jacoby R. Psychiatric disorder and personality factors associated with suicide in older people: a descriptive and case-control study. Int J Geriatr Psychiatry. 2001;16(2):155–65. [DOI] [PubMed] [Google Scholar]
- 34.Choi NG, DiNitto DM, Marti CN, Conwell Y. Physical Health Problems as a Late-Life Suicide Precipitant: Examination of Coroner/Medical Examiner and Law Enforcement Reports. Gerontologist. 2017. [DOI] [PubMed] [Google Scholar]
- 35.Fassberg MM, Cheung G, Canetto SS, Erlangsen A, Lapierre S, Lindner R, Draper B, Gallo JJ, Wong C, Wu J, et al. A systematic review of physical illness, functional disability, and suicidal behaviour among older adults. Aging Ment Health. 2016;20(2):166–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Aminzadeh F, Byszewski A, Molnar FJ, Eisner M. Emotional impact of dementia diagnosis: exploring persons with dementia and caregivers’ perspectives. Aging Ment Health. 2007;11(3):281–90. [DOI] [PubMed] [Google Scholar]
- 37.Lee L, Weston WW. Disclosing a diagnosis of dementia: helping learners to break bad news. Can Fam Physician. 2011;57(7):851–2, e270-2. [PMC free article] [PubMed] [Google Scholar]
- 38.Choi NG, DiNitto DM, Marti CN, Kaplan MS, Conwell Y. Suicide Means among Decedents Aged 50+ Years, 2005-2014: Trends and Associations with Sociodemographic and Precipitating Factors. Am J Geriatr Psychiatry. 2017;25(12):1404–14. [DOI] [PubMed] [Google Scholar]
- 39.Stone DM, Holland KM, Bartholow B, Crosby AE, Davis S, Wilkins N. Preventing Suicide: A Technical Package of Policies, Programs, and Practices. Atlanta, GA: National Center for Injury Prevention and Control, Centers for Disease Control and Prevention; 2017. [Google Scholar]
- 40.De Leo D, Draper BM, Snowdon J, Kolves K. Contacts with health professionals before suicide: missed opportunities for prevention? Compr Psychiatry. 2013;54(7):1117–23. [DOI] [PubMed] [Google Scholar]
- 41.Hunkeler EM, Katon W, Tang L, Williams JW Jr., Kroenke K, Lin EH, Harpole LH, Arean P, Levine S, Grypma LM, et al. Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. BMJ. 2006;332(7536):259–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Coffey M, Coffey C, Ahmedani BK. Suicide in a health maintenance organization population. JAMA Psychiatry. 2015;72(3):294–6. [DOI] [PubMed] [Google Scholar]
- 43.Tollefsen IM, Hem E, Ekeberg O. The reliability of suicide statistics: a systematic review. BMC Psychiatry. 2012;12:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Medicaid and Medicare Services. Condition Categories. Chronic Conditions Data Warehouse. https://www.ccwdata.org/documents/10280/19139421/original-ccw-chronic-condition-algorithms.pdf. Published 2017. Accessed December 7, 2017.


