Abstract
Purpose of Review
Metabolic disorders encompass a group of inherited inborn errors of metabolism that are uncommonly encountered but can pose challenges when encountered during the perioperative period. Hence, it is paramount that anesthesiologists are experienced and familiar with management of these conditions.
Recent Findings
Hundreds of inborn errors of metabolism have already been identified, yet new metabolic disorders continue to be discovered with advancements in genomic science.
Summary
In our general review, we define the more common metabolic disorders encountered in perioperative medicine and discuss the perioperative anesthetic considerations and challenges associated with each disorder. The following disorders are covered in our review: disorders of carbohydrate metabolism, disorders of amino acid metabolism, disorders of branched-chain amino acid metabolism, organic acidemias, mitochondrial disorders, lysosomal storage disorders, metal metabolism disorders, and urea cycle disorders.
Keywords: Metabolic disorders, Carbohydrate metabolism, Amino acid metabolism, Branched-chain amino acid metabolism, Organic acidemias, Mitochondrial disorders, Lysosomal storage disorders, Metal metabolism disorders, Urea cycle disorders, Anesthesia
Introduction
Metabolic disorders are a group of inherited inborn errors of metabolism that present infrequently yet can be challenging when encountered during anesthesia and surgical care. Hence, it is paramount that anesthesiologists are experienced and familiar with management of these conditions.
In this general review, we define the more common metabolic disorders encountered in perioperative medicine and discuss the perioperative anesthetic considerations and challenges associated with each disorder.
Disorders of Carbohydrate Metabolism
Galactosemia
Pathophysiology
Lactose, found in milk and dairy products, breaks down into galactose and glucose via hydrolysis. To use galactose as fuel for cellular metabolism, it needs to be converted into glucose-1-phosphate by one of the 3 enzymes: galactose-1-phosphate uridyltransferase, galactokinase, or uridine diphosphate galactose-4-epimerase (Table 1). Galactosemia, a condition with elevated level of galactose in the blood, can be caused by deficiency in any of the 3 enzymes, but usually is due to transferase deficiency. Without the transferase enzyme, the accumulation of galactose-1-phosphate in cells can result in injury to the kidney, liver, eyes, and brain [1••].
Table 1.
Galactosemia subtypes and clinical presentations [1••]
| Galactosemia subtypes | Enzyme defect | Clinical presentation |
|---|---|---|
| Classic/type I galactosemia | Galactose-1-phosphate-uridyl-transferase | Vomiting, hepatomegaly, cataracts, failure to thrive, aminoaciduria |
| Galactokinase deficiency | Galactokinase | Cataract |
| UDP-galactose-4-epimerase deficiency | UDP-galactose-4-epimerase | Similar to transferase deficiency with additional findings of hypotonia and nerve deafness |
Presentation
Classic galactosemia, or type I galactosemia, due to the complete deficiency of transferase, is an autosomal recessive disorder, and usually manifests by the first 2 weeks of life as a life-threatening disease [1]. It has an incidence of 1 in 60,000. Affected neonates may present with any of the following symptoms: Escherichia coli sepsis, jaundice, hepatomegaly, vomiting, hypoglycemia, seizures, lethargy, irritability, feeding difficulties, poor weight gain, aminoaciduria, cataracts, vitreous hemorrhage, liver cirrhosis, ascites, hepatic failure, splenomegaly, or mental retardation [2••, 3]. Symptoms improve when milk is temporarily withheld or replaced by lactose-free nutrition. Partial transferase deficiency occurs at a higher incidence, but is usually asymptomatic and only diagnosed in neonate screening due to moderately low transferase activity or moderately elevated galactose level [2••]. In galactosemia caused by deficiency of galactokinase or epimerase, symptoms are usually milder or can be asymptomatic (Table 1).
Treatment
The only treatment for classic galactosemia is life-long elimination of galactose intake [1]. Lactose-free milk substitutes are available as an alternative nutrient. Although elimination of galactose reverses hepatic dysfunction, cataract, and growth delay, patients suffer long-term effects secondary to galactose restriction such as ovarian failure, decreased bone mineral density, learning disabilities, developmental delay, and impaired motor function since galactose is an essential component of nervous system proteins during early development [1••, 2••]. In galactosemia caused by deficiency of the other two enzymes, galactokinase or epimerase, the treatment is galactose restriction for severe disease, while mild forms of disease does not require treatment [2••].
Perioperative Anesthesia Considerations
Patients with galactosemia may have existing hepatic and renal dysfunction and are prone to prolonged clotting times, hemolysis, E. coli sepsis, and albuminuria.
Preoperative evaluation should include laboratory testing, including coagulation panel, liver function tests, complete blood count, and basic metabolic panel to evaluate for the aforementioned medical considerations [4].
Prolonged clotting times due to hepatic dysfunction can make the patient more prone to bleeding during surgery. Presence of hemolysis may result in pronounced anemia. Albuminuria, secondary to renal tubular dysfunction, can cause osmotic diuresis, so urine output is not a reliable marker of intravascular volume [4].
Considering the baseline hepatic and renal dysfunctions, it is crucial to avoid extreme hypotension and organ hypoperfusion. Also, hepatotoxic and nephrotoxic agents must be administered with caution and avoided whenever possible [4, 5].
E. coli sepsis is the most common cause of mortality for infants with galactosemia, especially if it was not diagnosed in the first week of life; therefore, special attention should be paid to reduce the infection risks during line placements and medication administration for these patients in the perioperative period [5].
Glycogen Storage Diseases
Pathophysiology
Glycogen, a long-chain polymer of glucose, is the main form of glucose storage in human body. Glycogen in skeletal muscles provides a ready source of fuel during exercise, and hepatic glycogen helps maintain plasma glucose level during fasting [4].
In glycogen storage diseases (GSD), glycogen breakdown is impaired, and patients are at risk of hypoglycemia. It is an inherited enzymatic defect without sex predilection. Because of the impaired glycogenolysis, amino acids are used instead as an alternate substrate to maintain glucose homeostasis, resulting in muscle breakdown [6]. In addition, glycogen accumulates in tissues such as the liver, muscles, or central or peripheral neurons, causing organ dysfunction [2••]. There are 14 types of GSD, although 90% of patients have type I and five variants are commonly encountered.
Presentation and Treatment
Type I GSD, or Von Gierke disease, is an autosomal recessive disorder caused by the deficiency of glucose-6-phosphatase activity in the liver and kidney. Its incidence is 1:50,000–100,000 patients. The disease may manifest in neonates with hypoglycemia and lactic acidosis, or more commonly in infants 3–4 months of age with hepatomegaly or hypoglycemic seizures. Children with type I GSD often have doll-like faces with round cheeks, short stature, and protuberant abdomen due to enlarged liver and kidney. Other features include intermittent diarrhea due to loss of mucosal barrier function and neutrophil dysfunction, hyperuricemia and gout, hyperlipidemia and increased risk of pancreatitis, and bruising and epistaxis due to impaired platelet function. Almost all female patients have polycystic ovaries on ultrasound, without other features of polycystic ovarian syndrome such as hirsutism and infertility. Later in life, after the second decade of life, patients may develop organ dysfunction such as hepatic adenomas that have malignant potential and may have hemorrhage, proteinuria, and renal disease sometimes progressing to failure, and pulmonary hypertension [2••].
The main goal of treatment for type I GSD is to maintain euglycemia with dietary therapy. It consists of continuous infusion of glucose or oral feeding of elemental formula that contains only glucose in early infancy, and transitions to feeding of uncooked cornstarch or other new starch products that provide a slow-release form of glucose. Other types of sugars such as fructose, sucrose, and lactose should be avoided because they cannot be converted in glucose in GSD type I. Liver transplant is a potential cure for type I GSD but is reserved as a last resort for patients with liver malignancy or liver failure given its inherent morbidity.
Type II GSD, or Pompe disease, is an autosomal recessive disorder caused by the deficiency of acid-α-glucosidase (acid maltase), an enzyme that degrades glycogen in lysosomes. In Pompe disease, glycogen accumulates in lysosomes in tissues of multiple organs, especially cardiac and skeletal muscles. In infantile Pompe disease, patients present in the first few months of life with hypotonia, macroglossia, hepatomegaly, and hypertrophic cardiomyopathy, followed by cardiorespiratory failure by 2 years of age. Patients with late-onset Pompe disease have fewer cardiac conditions but suffer muscle weakness that progresses to respiratory failure. Most patients succumb to their disease between early childhood and late adulthood [2••]. Enzyme replacement therapy with recombinant acid α-glucosidase is the treatment for Pompe disease, and should be initiated preferably < 6 months of age [2••].
Type III GSD is an autosomal recessive disease caused by a deficiency of glycogen debranching enzyme, leading to accumulation of abnormal glycogen with short-branch chains in the liver and cardiac and skeletal muscles. Patients present in infancy or childhood with hepatomegaly, hypoglycemia, short stature, skeletal myopathy, and cardiomyopathy. Despite the elevated liver transaminase levels, hepatomegaly in type III GSD usually improves with age, unlike in type I GSD. Muscle weakness, however, slowly progresses and becomes severe after the third decade of life. Like type I GSD, polycystic ovarian syndrome is also common in female patients, without decrease in fertility [2••].
The dietary modification required for type III GSD is less rigorous than that for type I GSD. Fructose and galactose do not need to be restricted. There is no definitive treatment for progressive myopathy, other than a high-protein diet that can prevent hypoglycemia and endogenous protein breakdown. Liver transplant is again a potential treatment, but mostly reserved for patients with end-stage cirrhosis and/or hepatic carcinoma [2••].
Type IV GSD, or Anderson disease, results in delayed growth, and hepatomegaly that may progress to liver failure and may affect muscles and the heart late in the disease.
Type V GSD, or McArdle disease, is an autosomal recessive disorder caused by the deficiency of muscle phosphorylase that normally cleaves glucose from straight chain of glycogen. This leads to accumulation of glycogen in muscle, manifesting as exercise intolerance with muscle cramps and pain starting in late childhood or as an adult. Patients are prone to rhabdomyolysis after exercise of high intensity or long duration. Patients usually do not require treatment other than avoiding strenuous exercise. Glucose intake or glucagon injection prior to exercise can improve exercise tolerance, as well as high-protein diet and creatine supplement [2••].
Table 2 provides a summary of the aforementioned GSDs including affected organs, clinical features, treatment, and anesthetic modifications.
Table 2.
| Disease | Organ affected | Clinical features | Treatment | Comments | Anesthetic modifications |
|---|---|---|---|---|---|
| Type I (von Gierke) | Liver, Renal | Hypoglycemia, lactic acidosis, ketosis, hepatomegaly, hypertriglyceridemia, hyperuricemia, gout, short stature, platelet dysfunction | Uncooked cornstarch; avoid fructose, galactose, sucrose | Good prognosis with supportive treatment. Early onset | Minimize fasting, IV dextrose solution, avoid IV lactate, glucose and pH monitoring |
| Type II (Pompe) | Cardiac, liver, muscle | Hypotonia, hypertrophic cardiomyopathy, cardiorespiratory failure, hepatomegaly | Enzyme replacement therapy | Death by age 2 in infantile form | Avoid propofol and high sevoflurane, use ketamine or etomidate, no succinylcholine. Maintain BP and preload |
| Type III (Cori or Forbes) | Liver, muscle | Hypoglycemia, ketonuria, hepatomegaly, muscle fatigue, transaminitis, hyperlipidemia | High-protein diet, liver transplant | Good prognosis. Intermediate severity of hypoglycemia. Early childhood | Limit fasting, IV dextrose solution, glucose monitoring, preop echo, no succinylcholine |
| Type V (McArdle) | Muscle | Exercise intolerance, fatigability | Avoid strenuous exercise | Good prognosis. Male predominance. Most common in adults |
MH precaution, rhabdomyolysis, acute renal failure, avoid tourniquet, avoid shivering |
Perioperative Anesthesia Considerations
Type I GSD
Anesthetic considerations for type I GSD, or Von Gierke disease, include the risks of hypoglycemia, lactic acidosis, and platelet dysfunction.
Fasting should be minimized. Enteral feeds should be discontinued prior to surgery and transitioned to intravenous glucose solution to maintain normoglycemia. In a case report where attempts at peripheral intravenous cannulation failed and central venous access could not be obtained awake, and patient was acutely hypoglycemic, sublingual 40% dextrose gel and subcutaneous 10% dextrose infusion had been given successfully before induction of anesthesia [7]. Intraosseous access can also be considered in life-threatening hypoglycemia [7].
Glucose level should be monitored intraoperatively via arterial line blood sampling or intravenous blood sampling [8]. Glucose levels should be maintained in the normal range throughout surgery by titrating the rate of infusion of 10% dextrose [2••]. Post-operatively, the dextrose infusion should be continued until the patient is fully conscious and tolerating the preoperative enteral feeding regimen [9].
Bispectral index (BIS) can be helpful in monitoring depth of anesthesia, but in patients of GSD, a decrease in BIS might reflect hypoglycemia that is indistinguishable from increased depth of general anesthesia [10].
Lactate containing fluid should be avoided because lactate cannot be completely converted to glycogen, and lactic acidosis can develop. Lactated Ringer’s solution should be avoided. Blood pH and base deficit should be monitored intraoperatively. If metabolic acidosis occurs, sodium bicarbonate should be administered according to the base deficit. Tracheal intubation and mechanical ventilation are preferred to avoid respiratory acidosis, but hyperventilation should also be avoided because respiratory alkalosis can lead to release of lactate from muscle tissue and exacerbate lactic acidosis [8].
Platelet dysfunction is a concern, and prolonged bleeding times can be normalized by normalizing glucose level preoperatively [8]. Use of 1-deamino-8-d-arginine vasopressin (DDAVP) can reduce bleeding complications [6].
Type II GSD
Infantile type II GSD, or Pompe disease, is usually fatal by 1 year of age without treatment. Now with enzyme replacement therapy, patients with Pompe disease are living longer and presenting in increasing numbers for central line placement for enzyme replacement therapy infusion, percutaneous gastrostomy for swallowing dysfunction, or other unrelated surgeries.
Preoperative cardiac assessment including EKG and echocardiography is important for Pompe disease, where hypertrophic cardiomyopathy may cause significant left ventricular outflow tract obstruction and glycogen deposit can disrupt conduction pathways and cause arrhythmia [6, 11]. There appears to be an association between LV mass and mortality risk [11]. In the preoperative echocardiogram, a normal ejection fraction can be misleading, and indices of 2D LV mass and ventricular cavity volume are more helpful for the severity of cardiac hypertrophy [12]. Any elective surgery should be delayed until enzyme replacement therapy is initiated to reduce LV mass and arrhythmia risk [11]. For urgent surgeries, perioperative hydration to increase preload and ventricular filling can decrease the risk of LVOT obstruction [11, 12].
Blood pressure should be measured continuously with pre-induction arterial line if possible. ST segments should be monitored with 5 lead EKG to diagnose myocardial ischemia [11, 12]. Defibrillator and resuscitation medications should be in the OR and readily available [11]. Decreased coronary perfusion and arrhythmia leading to cardiac arrest after induction of general anesthesia have been reported and associated with the use of induction agents with vasodilatory properties such as propofol and high concentration of sevoflurane in patients with infantile Pompe disease [11, 12]. Use of ketamine, supplementing with phenylephrine or esmolol to counteract tachycardia, can better support coronary perfusion pressure and avoid decreasing diastolic blood pressure [11]. Etomidate may also be an acceptable induction agent [12].
Other anesthetic considerations include diaphragmatic weakness, an important feature of untreated Pompe disease [13]. Preoperative assessment may reveal pulmonary function test with reduced lung volume and more than 20% difference between sitting and supine positions, or the need for nocturnal ventilation therapy [13]. Regional anesthesia with sedation should be considered to avoid intubation and prolonged mechanical ventilation [12]. Patients with GSD type II may be more sensitive to nondepolarizing neuromuscular blockade because of their baseline myopathy, and succinylcholine should be avoided due to the risk of hyperkalemia and rhabdomyolysis [12, 13]. Lastly, macroglossia can cause difficult ventilation and intubation [6]. In the presence of hypotonia, awake fiberoptic intubation may be feasible [14].
Type III GSD
The anesthetic considerations for type III GSD, or Cori/Forbes disease, are related to the features of skeletal and cardiac myopathy, hepatomegaly and liver dysfunction, macroglossia, and hypoglycemia.
Preoperative assessment should include EKG and echocardiography. There is variable cardiac muscle involvement, and although most patients are initially asymptomatic until the third or fourth decade of life, many have thickened interventricular septum, systolic anterior motion of the mitral valve, and dilatation of the left ventricle and left atrium on echocardiogram early on [15, 16]. Cases of sudden death, ventricular tachycardia, ventricular fibrillation secondary to premature coronary artery disease, and congestive heart failure have been reported [17–20].
Macroglossia is a challenge to airway management and can cause significant obstruction to ventilation and to laryngoscopy [21]. In addition, hepatomegaly may impede optimal diaphragm excursion and increased intraabdominal pressure. Reverse Trendelenburg position may help improve ventilation and decrease risk of aspiration [21].
Preoperative laboratory testing for liver function and coagulation panel can provide insight into the degree of liver dysfunction, which can have implication on the duration and action of medications and selection of anesthetics. Neuromuscular blocker should be carefully selected due to the underlying hypotonia in patients with GSD. Succinylcholine should be avoided due to the risk of rhabdomyolysis and hyperkalemia. Nondepolarizing neuromuscular blocking drugs may have prolonged durations of action; short- or intermediate-acting agents should be considered and the dosing interval adjusted accordingly [21].
Lastly, hypoglycemia should be carefully managed, limiting preoperative fasting and starting intravenous dextrose infusion preoperatively if necessary [21]. Blood glucose level should be monitored intraoperatively. Intra-arterial cannulation has been recommended not only for intraoperative glucose monitoring but also to avoid muscle cramping induced by repeated cuff pressure measurement [22].
Type V GSD
Type V GSD, or McArdle disease, involves mainly skeletal muscles. Anesthetic considerations include rhabdomyolysis, and renal injuries secondary to myoglobinuria. Patients are prone to muscle ischemia secondary to tourniquet use, poor position, or shivering, and acute renal failure has been reported secondary to myoglobinuria after strenuous exercises [23]. Therefore, optimizing positioning, minimizing tourniquet use, and maintaining normothermia are important [24, 25]. Forced diuresis can be used to prevent renal failure in patients with myoglobinuria and high creatinine kinase [26]. Glucose infusion perioperatively can ensure availability of energy substrate and possibly prevent muscle injuries and weakness [25, 26].
Disorders of amino acid metabolism
Homocysteinemia
Pathophysiology
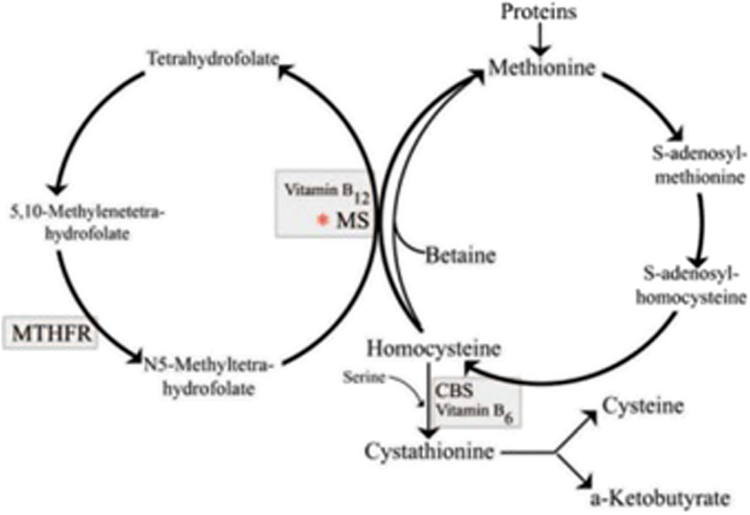
Homocysteine is an intermediary amino acid formed by the conversion of methionine to cysteine. In this pathway, conversion from homocysteine to methionine and back to cysteine requires several enzymes. Homocysteine is methylated to form methionine through a folate-dependent pathway and B12-dependent methionine synthase enzyme. On the other hand, methionine can be converted to cystathionine through a B6-dependent cystathionine-beta synthase (CBS) enzyme. At each of these levels, homocysteine can accumulate if either a vitamin or an enzyme function is decreased (Fig. 1).
Fig. 1.
Biochemical pathway of the creation of homocysteine and specific enzymes/vitamins necessary for conversion to methionine vs. cystathionine [27]
Presentation
In its most extreme form, homocysteinuria is a rare autosomal recessive disorder marked by CBS deficiency which causes impaired synthesis of cystathionine, decreased cysteine, and increased methionine and homocysteine. This can manifest as developmental delay, marfanoid appearance, ocular malformations, and osteoporosis. The decrease in cysteine leads to weakened collagen in connective tissue, while elevated homocysteine can lead to oxidative radicals and platelet aggregation causing vascular malformations and severe premature atherosclerosis and evidence of thromboembolic disease [28–30].
Normal blood levels of homocysteine are 5–15 μmol/L with moderate levels 15–30 μmol/L, intermediate 30–100 μmol/L, and severe > 100 μmol/L) [31]. Increased homo-cysteine results from genetic factors like that of methylene tetrahydrofolate reductase (MTHFR), vitamin deficiencies like folate and vitamin B6 or B12 [32, 33], chronic kidney disease (CKD), and medications like that of fibrates used for hypercholesterolemia, methotrexate, and metformin. Clinical significance of increased homocysteinemia in response to medications has not been proven [34, 35].
Mild to moderate increases in homocysteine (hyperhomocysteinemia) occur in 5–7% of the population [36] and has been associated with increased risk for atherosclerotic vascular disease in adults.
Treatment
Unless a patient has homocysteinuria (diagnosed or highly suspicious), studies have suggested to not test or treat hyperhomocysteinemia. Decreasing levels of homocysteine with vitamin supplementation does not reduce cardiovascular disease or the recurrence of VTE [37–40].
Perioperative Anesthetic Considerations
Due to risk of thromboembolism, administration of antiplatelets and anticoagulants, like that of baby aspirin, dipyridamole, and heparin/LMWH, is recommended. Any drugs that increase a patient’s coagulable state (e.g., oral contraceptives) should be stopped [41–43].
In the intraoperative period, avoid hypovolemia, maintain cardiac output, apply venodynes to prevent peripheral stagnation of blood, monitor glucose for hypoglycemia, and reduce peripheral vascular resistance. Postoperatively, early ambulation is encouraged, as well as close monitoring of basic labs.
Use of nitrous oxide as an anesthetic for patients with hyperhomocysteinemia is discouraged. Nitrous oxide blocks the conversion of homocysteine to methionine increasing levels of homocysteine. Badner et al. [44] found an increased association with nitrous oxide use intraoperatively, increased homocysteine levels, and subsequently greater incidence/duration of myocardial ischemia in patients undergoing a carotid endarterectomies.
In instances of increased methionine, hypoglycemia can result in increased release of insulin. Avoidance of this can be prevented by perioperative bolus of dextrose containing fluids or effectively decreasing the fasting interval [45].
Phenylketonuria
Pathophysiology
Phenylketonuria (PKU) is a rare metabolic disorder (affecting 1 in 15,000 infants in the USA) [46]. This disease results from a deficiency of the liver enzyme phenylalanine hydroxylase (PAH). In newborn screening, tandem-mass spectrometry is often employed to measure phenylalanine (Phe) and other amino acids including tyrosine and acylcarnitine ester with a high concentration of Phe together with low to low-normal tyrosine concentration conferring a diagnosis of PKU.
Presentation
Elevated levels of amino acid Phe throughout the body leads to a variety of symptoms listed below:
Mental retardation
Microcephaly
Severe vomiting, mimicking infantile pyloric stenosis
Seizures
Delayed speech
Behavioral abnormalities
Eczema
“Mousy” odor due to the increased concentration of phenylacetic acid
Hyperphenylalaninemia (HPA) due to PKU tends to have a complete or significant deficiency of enzyme activity with blood Phe reaching levels of > 20 mg/dL.
As with most genetic disorders, PKU shows a vast genetic and clinical variability with > 400 identified mutations at the PAH gene (chromosome 12q24.1). Genetic factors can play a role in clinical variability, but environmental and lifestyle factors can also result in significant variation.
Treatment
The mainstay of treatment for PKU is dietary restriction of Phe. Other pharmacological treatments for PKU include:
Cofactor for PAH (tetrahydrobiopterin (BH4)/sapropterin (synthetic BH4)).
Pegylated phenylalanine ammonia lyase (PEG-PAL), an enzyme that degrades phenylalanine.
Long-chain polyunsaturated fatty acids—low blood concentrations of long-chain polyunsaturated fatty acids (LCPUFAs) and docosahexanoic acid (DHA) can result from a Phe-restricted diet thus altering neurodevelopment [47].
LNAA compete with phenylalanine for the same amino transporter at the blood-brain barrier; thus, addition of these amino acids can reduce the amount of Phe in the brain [48].
Perioperative Anesthetic Considerations
There have been very few case reports that demonstrate anesthetic management for patients with PKU [49–51]. Overall general guidelines for anesthetic considerations in patients with PKU include:
Oral intake should not be stopped for an extended period preoperatively causing a catabolic state leading to increased serum Phe levels.
Due to a possibility of post op paraparesis in vitamin B12–deficient individuals with PKU, it is recommended that nitrous oxide, which inactivates B12-dependent methionine synthase, be used with extreme caution in this specific patient population [49].
Intravenous access, application of the face mask and passage of the tracheal tube should be done carefully given increased risk of skin sensitivity and eczema.
Phe levels do not change significantly in minor surgeries, although if the patient requires major or emergency surgery, intravenous dextrose should be given before and after surgery to avoid a catabolic state.
Propofol and PKU
Propofol uncouples oxidative phosphorylation and inhibits mitochondrial complex I—the main mechanism of propofol infusion syndrome (PRIS) [52]. In vitro, HPA can inhibit the activity of mitochondrial complex I as well by competing with nicotinamide adenine dinucleotide phosphate [53]. Combined inhibition of the mitochondrial respiratory chain can manifest as hyperthermia and acidosis.
Disorders of Branched-Chain Amino Acid Metabolism
Maple Syrup Urine Disease
Maple syrup urine disease (MSUD) is an inherited autosomal recessive metabolic disorder resulting from reduced capacity for oxidative decarboxylation of the branched-chain amino acids (BCAA): leucine, isoleucine, and valine [54]. Errors in the metabolism of these specific amino acids can lead to ketoacidosis and neurotoxicity. This disorder occurs in 1:120,000 to 1:150,000 live births and is thought to be more common among children from consanguineous relationships [55, 56]. The severity of the presentation is linked to the amount of enzymatic activity of the branched-chain ketoacid decarboxylase.
Presentation
There are five clinical variants of MSUD. Classic MSUD is the most common and most severe variant of the disease, tending to present at 4–7 days after birth with lethargy, metabolic ketoacidosis, hypotonia, or hypertonia. These symptoms can progress to seizures, coma, and ultimately death if left untreated. Patients with the classic form of the disease require early intervention in order to prevent developmental delay and acute neurological decompensation [56, 57]. Intermittent MSUD, the second most common variant however, has a markedly different clinical presentation from the classic form of the disease. These patients may have normal levels of BCAA except during periods of catabolic stress, such as surgery, exercise, fasting, or acute illness. At these times, patients are at risk for ketoacidosis and neurotoxicity. In the intermittent form of MSUD, symptoms may present between 5 months and 2 years of age.
Intermediate MSUD (not to be confused with Intermittent MSUD) can present at any age with variations in the amount of neurological impairment and developmental delay. These patients are also at risk for decompensation related to acute stress or high protein consumption. Thiamine-responsive MSUD is a milder form of the disease whereby patients have reduced levels of hyperaminoacidemia when given supplemental thiamine, a cofactor of the branched-chain amino acid dehydrogenase complex. These patients still require reductions in their intake of BCAA for adequate metabolic control. Finally, E3-deficient MSUD is a very rare form of the disease with only a handful of cases reported. The patients with this variant tend to present as neonates and have additional lactic acidosis as well as accumulation of pyruvate and alphaketoglutarate [56].
Treatment
The treatment of MSUD is twofold: first, the acute metabolic and neurologic derangements must be managed, and, second, the patients must adhere to a lifelong low-protein diet limiting BCAA intake. In the acute setting, peritoneal dialysis has been reported to successfully reduce BCAA levels in neonates. Long-term management is most often accomplished with the use of MSUD-specific medical foods in combination with ordinary low-protein foods [56]. Rapid diagnosis of the classic form in combination combined with close monitoring and strict adherence to the specific dietary restrictions may actually allow a child to have relatively normal growth and development [57]. Decompensation can occur in the setting of acute illness, fasting, exercise, or other catabolic states. Patients may have non-specific gastrointestinal or neurologic symptoms. If not treated, they may progress to severe ketoacidosis, hypoglycemia, and death secondary to cerebral edema with herniation.
Perioperative Anesthetic Considerations
It is prudent for even minor surgical procedures to take place in a facility capable of overnight monitoring and preferably in a center with expertise in the management of MSUD. Wherever possible, these patients should be scheduled as the first case of the day to minimize fasting time. Dextrose containing fluids should be initiated at the start of the fasting period to minimize protein catabolism. The dextrose infusion should be continued until the patient is able to resume his or her normal diet post operatively. Baseline blood gases are suggested and dehydration and acidosis should be treated preoperatively with IV fluids provided that the surgery is not emergent and/or life-threatening [56].
The goal for fluid management is normovolemia as overhydration risks perioperative cerebral edema [58]. Of note, hypertonic glucose solutions may also represent an additional stress factor by increasing a patient’s O2 consumption, CO2 production, and noradrenaline excretion. In light of this, some sources suggest an infusion of fat emulsion, which allows for continued caloric intake while minimizing overhydration, hemodilution, and glucose loading [55]. Regardless of the choice for fluid management and caloric supplementation, intraoperative management should allow for the monitoring of glucose levels and pH, particularly in prolonged or high-risk surgeries. This can be accomplished with invasive vascular access such as an arterial line or central venous line.
Both general and regional anesthetics have been reported as safe in patients with MSUD. Adequate pain management is essential to minimize post-operative stress on the patient; regional anesthetic techniques should therefore be considered part of a multi-modal approach.
Finally, for patients undergoing procedures where this is a risk that blood may accumulate in the stomach, a nasogastric tube should be placed in the operating room. Blood in the gastrointestinal tract is in fact a large protein load and may precipitate an acute perioperative metabolic decompensation [56].
Organic Acidemias
Pathophysiology
Organic acidemias are a group of autosomal recessive inborn errors of metabolism that result in increased amounts of organic acids in urine. They include propionic acidemia (PA), methylmalonic acidemia (MMA), isovaleric acidemia, and glutaric aciduria and others. PA and MMA are two of the more commonly seen organic acidemias and thus are discussed here [59].
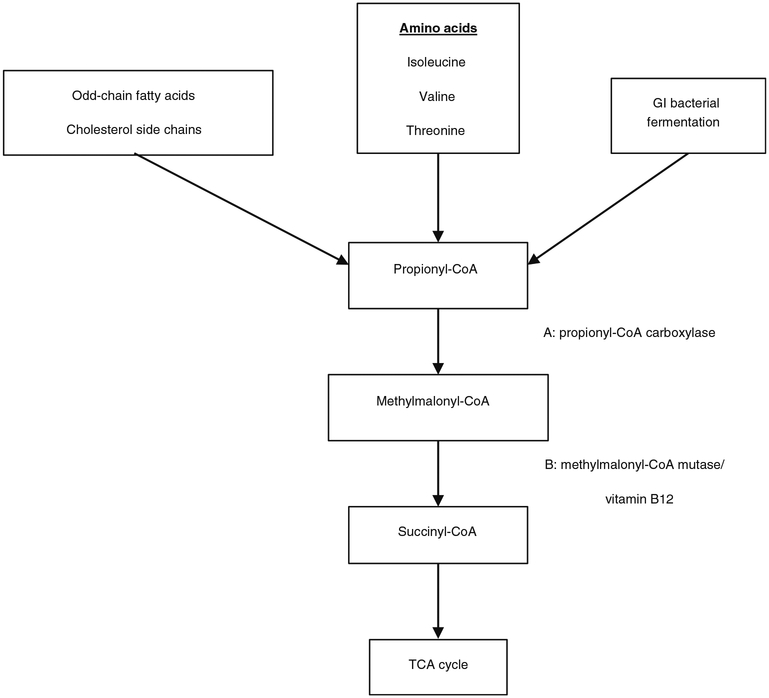
Both PA and MMA result from defects in the metabolic pathway of specific amino acids (isoleucine, valine, methionine, threonine), odd-chain fatty acids, and cholesterol side chains. Propionic acid is also produced by the gastrointestinal flora and contributes to the organic acid load in these disorders.
Defects in propionyl-CoA carboxylase leads to accumulation of propionic acids. In MMA, genetic defects in methylmalonyl-CoA mutase or in its cofactor cobalamin produces excess methylmalonic acid and propionic acid. Additionally, cobalamin deficiency by diet or by decreased gastrointestinal absorption can cause MMA (Fig. 2).
Fig. 2.
Metabolic pathway. Defect in A causes PA. Defect in B causes MMA
Presentation
Patients with PA or MMA have recurrent episodes of severe metabolic acidosis often precipitated by an illness or excessive protein intake. Signs and symptoms are non-specific and affect multiple organ systems including gastrointestinal, neurologic, and hematologic. Neonates generally present within the first few weeks after birth with lethargy, poor muscle tone, poor feeding, and vomiting. If not diagnosed in the neonatal period, patients later in life may show failure to thrive, vomiting, GERD, seizures, developmental delay, and encephalopathy. In propionic acidemia, cardiac involvement is more common including cardiomyopathy and prolonged QTc. Patients with methylmalonic acidemia are more likely to develop renal impairment [60•].
PA and MMA are both diagnosed by the presence of the respective organic acids in urine. In addition to metabolic acidosis, labs usually will show hyperammonemia, hypoglycemia, and lactic acidosis. Cytopenia may also be present.
Treatment
Long-term management of PA and MMA consists of a low-protein diet with supplementation of non-triggering amino acids, l-carnitine, and bicarbonate. For MMA patient, vitamin B12 supplementation is also warranted. For acute episodes of metabolic decompensation, management involves identifying and treating the underlying illness or stressor. Other supportive measures include protein restriction, administration of dextrose-containing fluids, and continuation of carnitine, bicarbonate, and cobalamin. If severely ill with severe metabolic derangements, the patient may need hemodialysis [61].
Perioperative Anesthesia Considerations
Patients with organic acidemias requiring anesthesia present with various challenges and the overall goal of the anesthesiologist is to avoid or minimize factors that may trigger a metabolic crisis (Table 3). Prolonged periods of fasting may lead to the catabolism of protein and fatty acids. Therefore, NPO time should be minimized and dextrose-containing intravenous fluids should be administered during the fasting period. Preoperative evaluation should assess acid-base balance, nutritional status, muscle tone, mental status, and GI function, and labs should include ammonia, glucose, pH, CBC, and electrolytes. Pre-operative medications may include l-carnitine, metronidazole, and bicarbonate. l-Carnitine acts as an antioxidant and helps with renal excretion of organic acids. IV or PO metronidazole decreases the production of organic acids from the GI flora. Bicarbonate helps to treat the acidosis that may result from fasting. Vitamin B12, the cofactor of MM-coA mutase, can be administered to MMA patients. Preoperative admittance to the hospital may be considered to help with the implementation of these management strategies as well as to monitor the patient for metabolic crises.
Table 3.
Perioperative anesthetic management of PA and MMA
| PREOP | INTRAOP | POSTOP |
|---|---|---|
|
|
|
Intraoperatively, care should be taken to avoid hypoxia, hypoglycemia, and hypovolemia and maintain normothermia and hemodynamic stability. Minimizing the stress response to the surgery is important to decrease catabolism. Patients with MMA or PA may have GERD or a high risk of vomiting, so RSI can be considered. For patients with or at risk for bleeding in the GI tract or oropharynx, management may include a nasogastric tube or throat packing to minimize the intestinal absorption of heme proteins [62, 63].
For longer or more complicated procedures, frequent labs should be drawn to monitor acid-base balance, glucose, and ammonia. Additionally, continuation of dextrose-containing fluid, l-carnitine, and metronidazole should be considered.
Certain anesthetic medications should be avoided or used with caution. These include muscle relaxants that are metabolized by ester hydrolysis into odd-chain organic acids. Examples include succinylcholine, cisatracurium and mivacurium. Analgesics derived from propionic acid such as ibuprofen and naproxen should be avoided in patients with PA and MMA. Ketorolac does not present the same risk since it is derived from acetic acid. Nitrous oxide should not be used in MMA patients since it inhibits cobalamin enzymes. While there are no contraindications to opioids or volatile anesthetics, they should be used with caution in patients with hypotonia and at higher risk of respiratory depression.
Many recommend avoiding propofol because it contains polyunsaturated lipids that are metabolized to propionic acid [64–68]. In a review of 14 cases of patients with MMA undergoing liver transplantation, propofol was used for induction and maintenance of the first 7 of 14 patients. After the seventh patient, propofol was no longer used out of concern that it contributed to metabolic decompensation although the first five patients had no evidence of decompensation [69]. On the other hand, in a review of 28 patients with MMA undergoing 39 procedures, propofol infusions were used for maintenance in all 39 procedures and propofol was used for induction 36 of 39 procedures. Two cases experienced adverse events that were likely unrelated to the propofol. All these cases were brief, simple procedures/investigations including MRIs, exams under anesthesia, lumbar punctures, and central line removals [70]. Therefore, the administration of propofol in children with MMA or PA may be tolerated but should be used with great caution especially in prolonged cases or more traumatic surgeries.
Lactated Ringer’s is generally not recommended for use in patients with organic acidemias. In a retrospective review, 11 patients with organic acidemias underwent 19 total procedures, 9 of whom had MMA or PA and underwent 11 different procedures. These 9 received LR. One patient who had a posterior fusion developed transient mild metabolic acidosis postoperatively, which the authors attributed to massive blood loss and the duration of the surgery. Otherwise, the remaining patients did well intraoperatively and postoperatively [71]. In fact, many of the patients also received other medications such as propofol, atracurium, or nitrous oxide, which suggests that LR and other offending agents may be used in organic acidemia patients, albeit judiciously, and in well-compensated patients.
Regional anesthesia is an alternative to general anesthesia that would potentially allow the anesthesiologist to minimize the use of the aforementioned medications. However, its use for patients with MMA or PA has not been extensively reported. We found only one report of a lower extremity nerve block in an adult patient with PA who underwent foot surgery with dexmedetomidine sedation. Regional anesthesia in patients with organic acidemias do present potential concerns. First, patients with organic acidemia may be at greater risk for local anesthetic systemic toxicity (LAST) [72]. Second, if a patient with organic acidemia develops LAST, the effectiveness of intralipid for rescue is unclear. Nevertheless, the patient in this case did not have any perioperative issues, and also previously had an uneventful dental procedure under local anesthesia [73].
Mitochondrial Disorders
Pathophysiology
Mitochondrial disorders encompass a wide variety of pathological states resulting from impaired cellular metabolism. Within the mitochondrial organelle, the process of oxidative phosphorylation occurs along the mitochondrial respiratory chain (MRC) (complexes I–V) and is responsible for generating energy in the form of adenosine tri-phosphate (ATP). This is accomplished through the oxidation of acetyl coenzyme A (acetyl Co-A) derived from carbohydrates, fatty acids, and amino acids in the citric acid cycle [74]. Thus, high-energy dependent tissues, such as the central nervous system, the heart, the liver, the kidney, the gastrointestinal tract, and the muscular system, suffer the brunt of MRC defects [74, 75••, 76]. There are 13 protein subunits in the MRC and there are approximately 1000 nuclear proteins important to mitochondrial structure and function encoded within the nuclear DNA [74, 77•]. Genetic defects in any of these cellular components may contribute to pathology or may be lethal before birth.
Fatty acid metabolism is another essential function of the mitochondria, and derangements in fatty acid metabolic pathways represent a major category of mitochondrial disorders aside from those arising within the respiratory chain. Acylcarnitine transferase is responsible for transport of fatty acids into the mitochondrial matrix. Acylcarnitine undergoes beta-oxidation to generate acetyl-CoA and donate electrons to electron-transferring flavoprotein; both processes contribute to energy production by the MRC [77•]. Inborn errors in the cellular machinery necessary for fatty acid transport and beta-oxidation carry distinct clinical significance for anesthetic planning.
Presentation
Patients with mitochondrial disorders are typically diagnosed in infancy or early childhood and may present with muscle weakness or dystonia from myopathy, poor respiratory function, cardiomyopathy, conduction defects pre-disposing to arrhythmias, metabolic disturbances, encephalopathy, seizure disorder, renal insufficiency, and gastrointestinal dysfunction [74, 75••, 77•]. A careful history and physical and knowledge of the specific defect are important to ascertain which organ systems are compromised by a patient’s specific disorder. Disorders related to defects in mitochondrial DNA are maternally inherited and show heteroplasmy—clinical manifestations are highly variable [74]. Conversely, disorders related to defects in nuclear DNA are inherited in a Mendelian pattern. Common procedures for patients with mitochondrial disorders include pacemaker implantation, cataract extraction, insertion of cochlear implant, muscle and skin biopsies, orthopedic surgery, and abdominal surgery.
Treatment
While the treatment paradigms of mitochondrial disorders are beyond the scope of this review, certain aspects of treatment may impact anesthetic considerations. For example, while benzodiazepines are used sparingly for anesthesia when there is concern for respiratory failure or liver dysfunction, patients with epilepsy may already be taking benzodiazepines to prevent seizure activity. Patients with epilepsy may also be restricted to ketogenic diets to prevent seizures, and if so, should not receive intravenous fluids containing glucose [77•]. A careful preoperative review of the patient’s medications and current treatment plan is prudent prior to administering any anesthetic, and a discussion with other providers involved in the patient’s care is encouraged.
Perioperative Anesthesia Considerations
Pre-anesthetic laboratory testing should include glucose and lactate levels, electrolytes, liver enzymes, creatine kinase, complete blood count, and coagulation studies. A 12-lead electrocardiogram should be performed to diagnose conduction abnormalities. Lung function assessment with spirometry or blood gas analysis should be considered. The assessment of the degree of muscle weakness and neurological impairment, including an assessment of dysphagia, should be made. Preoperative fasting should be minimized to prevent hypoglycemia and use of glucose-containing maintenance fluids intraoperatively may be advantageous [76, 77•].
General anesthesia is heavily favored, as intravenous sedation carries undue risk for many patients with mitochondrial disorders. Of note, nearly all general anesthetics (volatile and parenteral) depress mitochondrial function. Some patients, particularly those with complex I defects, may display hypersensitivity to volatile anesthetics such as sevoflurane [78]. However, carefully titrated volatile anesthetics have been well tolerated and used safely. Propofol specifically affects the MRC at multiple sites and by multiple mechanisms and inhibits acylcarnitine transferase—these properties are implicated in the pathophysiology of propofol infusion syndrome [79]. Small boluses of propofol are considered acceptable, but continuous infusions of propofol should be avoided. Limited data exist for use of ketamine, etomidate, and barbiturates, but have reportedly been used successfully. Opioid-sparing techniques are favored with remifentanil and dexmedetomidine, although clearance of dexmedetomidine may be prolonged [75••]. While regional anesthesia is not contraindicated, bupivacaine specifically carries an increased risk of cardiac toxicity and ventricular arrhythmia due to its effects on acylcarnitine transferase and should be avoided [80]. Depolarizing neuromuscular blockade with succinylcholine is contraindicated given the risk of developing fatal hyperkalemia [75••]. Intravenous fluids containing lactate should be avoided in patients with difficulty metabolizing lactate, as it may lead to acidosis [81]. Finally, all attempts should be made to maintain normothermia, minimize tourniquet use, ensure adequate analgesia, and prevent postoperative nausea and vomiting, such that further metabolic and cardiorespiratory derangements are avoided to the greatest degree possible [75••, 77•]. Procedures for patients with mitochondrial disorders should be undertaken in facilities with appropriate specialty care resources available, such as trained pediatric intensivists, as careful monitoring in the postoperative setting is essential and advanced care may be necessary.
Lysosomal Storage Disorders
Pathophysiology
The lysosome is the chief organelle responsible for recycling proteins and polysaccharides within the cell. Mucopolysaccharidoses (MPS) comprise a group of genetic lysosomal storage disorders (LSDs) characterized by complete or partial deficiency of lysosomal enzymes necessary for the metabolism of glycosaminoglycans (GAGs). The intracellular buildup of these GAGs can result in cellular and tissue dysfunction and death, manifesting as various clinical abnormalities. LSD encompasses a group of 70 mostly autosomal recessive monogenic diseases of lysosomal function.
Presentation
The incidence of lysosomal disorders is approximately 1 in 8000 live births, but the incidence of each individual disease is closer to 1 in 250,000 [82]. The most common LSDs are Fabry disease, Gaucher disease, metachromatic leukodystrophy, and Pompe disease, although certain features are found across each subtype. Hepatosplenomegaly, cognitive and behavioral impairment, craniofacial abnormalities, cardiomegaly, bony deformities, visual and auditory dysfunction, bleeding diatheses, and immune dysfunction are common [83]. Diagnosis is based on clinical symptoms and confirmatory genetic testing and these are mostly pediatric diseases although some may manifest in adulthood. While classic Fabry Disease will have symptom onset between ages 4 and 8, cardiac disease may be the presenting symptom in patients older than 40 years of age [84].
Treatment
In the last two decades, significant improvements in the biological understanding and treatment of these disorders have been made. There are now over 20 FDA approved medications to treat the lysosomal storage disorders [83]. Enzyme replacement therapy is used to treat defective proteins and prevent accumulation of enzyme substrate. Some diseases are still treated with hematopoietic stem cell transplantation, but in the future gene editing technology in the form of gene replacement or antisense oligonucleotide therapies may be approved [83]. Survival for these disorders has increased, but these therapies do not prevent every sequela of the underlying disease. Orthopedic procedures, tracheostomy, and valve replacement surgery are increasingly required as patients’ lives are extended. These patients may also present for surgery unrelated to their underlying disorder. As more patients with lysosomal storage disorders are surviving into adulthood, the anesthesiologist will need to be familiar with the comorbidities and perioperative considerations of caring for these individuals.
Anesthesia Perioperative Considerations
Hypotonia, dystonia, neurocognitive decline, spasticity, and resulting contractures are common findings in a variety of LSDs. Gaucher disease, the most common LSD, may cause epilepsy, spasticity, trismus, and difficulty swallowing [83]. While airway obstruction is a common reason to reintubate the trachea in the postoperative period [85], the clinician should also be vigilant in monitoring for hypoventilation and respiratory muscle weakness. Approximately 30% of patients with MPS have epilepsy [86]. Neuronal ceroid lipofuscinosis types 1 and 2 are characterized by myoclonus, ataxia, and epilepsy [83]. The preanesthetic evaluation should note that anti-seizure medications were taken the day of surgery if appropriate and what the plan will be for seizure prophylaxis. Occasionally, seizures are the result of increased intracranial pressure and ventriculomegaly, and careful attention should be paid to ventilatory parameters and ETCO2 as well as medications that lower the seizure threshold. While many of these disorders are now successfully treated with enzyme or substrate replacement therapy, many of these medications do not penetrate the blood–brain barrier [83]. A treated patient is not necessarily at lower risk of seizures or hypotonia.
Careful preoperative evaluation should include evaluation of the number of metabolic equivalents a patient can complete, as well as any history of known cardiac disease, a physical exam looking at signs of heart failure or heart sounds associated with valvulopathy, and a review of any cardiac testing the patient has undergone. Cardiomegaly is relatively common among patients with LSDs. In a series of 39 patients with LSDs, only 31% had normal echocardiograms [87]. Valvular diseases were the most common abnormalities in 59% of patients [87, 88]. As more patients are surviving into adulthood, buildup of enzyme substrate in the heart can lead to valvulopathies that require replacement [88] or perioperative management. ECG findings are common in LSDs, but ventricular dysrhythmias are rare. In one series, 29% of patients had ECG abnormalities, but ventricular dysrhythmias were not detected during the intraoperative period and no patient had greater than second-degree heart block [86]. It should be noted that palpitations in adults with Fabry disease are common and may be due to atrial fibrillation or flutter. Lipid storage diseases such as Wolman disease may result in early atherosclerosis and risk of ischemia [83]. ECG abnormalities and exercise intolerance may require cardiology consultation for medical optimization of underlying cardiac disease prior to elective procedures.
Macroglossia, coarse facial features, glycosaminoglycan accumulation in the airway, obstructive sleep apnea, atlanto-occipital instability, dysarthria, and resulting recurrent aspirations and pneumonias are commonly encountered in LSDs [83]. Joint dysfunction and neurological impairment resulting in spasticity make positioning an already-challenging airway more difficult, particularly among patients with MPS [83]. A case series from the Mayo Clinic of patients with MPS found that up to 14% of patients were difficult to ventilate and 16.7% of patients were difficult to intubate [86]. In another series of 19 patients with MPS undergoing 136 anesthetics, 7% of patients were difficult to ventilate and 25% were difficult to intubate [89]. Direct laryngoscopy has proven difficulty in several case reports, even requiring blind intubation [82]. It was encouraging that 100% of laryngeal mask airway attempts were successful in this series [89]. Sedation without an advanced airway may be an appropriate plan even among pediatric patients. One group found that MRI studies could be safely performed with sedation in patients with metachromatic leukodystrophy [90]. A postoperative plan for airway management should be discussed with the care team in the post anesthesia care unit. The progression from difficult mask ventilation to laryngeal mask airway placement to fiberoptic intubation through an LMA was not uncommon in some series [86]. Stridor and obstruction can occur postoperatively, occasionally requiring reintubation and or elective tracheostomy [86].
Restrictive physiology results from several processes in LSDs. Dysphagia in Niemann-Pick disease causes silent aspirations and chronic lung infections. Symptoms may range from only mild dyspnea on exertion to interstitial lung disease. Chest X-rays of consolidations and computed axial tomography demonstrating ground glass opacities, bronchiectasis, and thickened pleura are common in Niemann-Pick patients [91]. Immune dysfunction in Gaucher disease may result in infiltration of airspaces and interstitial lung disease, but lung function is generally preserved in these patients. Abdominal organomegaly result in reduced diaphragmatic excursion. Contractures and spinal deformity in certain LSDs may decrease functional residual capacity, tidal volumes, and total lung capacity. Glycogen storage disease type II, or Pompe disease, can cause diaphragmatic weakness [83]. In adults with Fabry disease, mild to moderate obstruction has been demonstrated on pulmonary function testing with decreased diffusion capacity even in the absence of symptoms [91]. Occasionally, patients with severe cardiac disease or atherosclerosis such as in Wolman disease may develop pulmonary arterial hypertension [91]. It may be prudent to avoid airway instrumentation and mechanical ventilation in patients in which the success of extubation would be questionable.
Patients with Fabry disease commonly present with proteinuria and may later develop end-stage renal disease [92]. Cystinosis results in renal tubular Fanconi syndrome, characterized by the excretion of water, phosphate, calcium, magnesium, and potassium [93–95]. A basic metabolic panel with creatinine will reveal most renal dysfunction but urinalysis may be needed to detect proteinuria associated with early kidney disease. Bone weakness and pain are common due to depletion of phosphates and altered vitamin D metabolism. As a result, opioid analgesic requirements may be greater than expected in a patient population already at risk of apnea, obstruction, and stridor. Despite skeletal abnormalities, neuraxial anesthetics have been successfully used in a variety of LSD subtypes [96, 97]. There is little literature on regional anesthetics in this patient population. An MRI may be necessary to rule out severe spinal stenosis or epidural abnormalities. Care should be taken when moving and positioning patients with skeletal deformities or contractures.
Hepatosplenomegaly is a common presenting feature of many LSDs. Gaucher disease may present with hepatosplenomegaly and pancytopenias [83]. Sphingomyelin accumulation in macrophages in Niemann-Pick disease results in recurrent bacterial infections, and hepatosplenomegaly [83]. Lysosome-related organelles (LROs) include platelet delta granules, melanosomes, and lytic granules in cytotoxic T cells, and their dysfunction results in increased risk of bleeding, hypopigmentation, and decreased cellular immunity, respectively [98]. The LRO disorders, such as Hermansky-Pudlak, Griscelli syndrome, and Chediak-Higashi disease, are associated with easy bruising [98]. Complete blood counts will identify cytopenias, but thromboelastography may be necessary to determine bleeding risk in patients with normal counts, normal coagulation factors, and a history of easy bruising. Hemophagocytic lymphohistiocytosis, a life-threatening hyperinflammatory state with pancytopenia, may occur in patients with Griscelli or Hermansky-Pudlak syndrome [99]. Careful attention should be paid to aseptic technique in this patient population due to the increased risk of infections. Patients with recurrent inflammation and infection have an increased risk of restrictive lung physiology.
Metal Metabolism Disorders
Metals play critical roles in physiology and although numerous rare metal metabolism disorders are now known, only hemochromatosis and Wilson’s disease will be discussed
Hemochromatosis
Pathophysiology
Iron is essential in heme proteins such as hemoglobin and cytochromes, as well as iron-sulfur cluster proteins, and is incorporated from dietary sources through a regulated multi-step mechanism [100•].
Loss of hepcidin function disinhibits iron absorption, resulting in the iron overload condition hemochromatosis, typified by the classical triad of bronze skin, cirrhosis, and diabetes. These manifestations are due to siderosis, or iron accumulation in tissues. Iatrogenic hemochromatosis can occur from frequent transfusion, while four major types of hereditary hemochromatosis (HH) are recognized [100•].
Presentation
Type I HH is prevalent in non-Hispanic Whites, ranging from 0.44 to 0.5% in the USA [100•]. Phenotypic penetrance varies by gender, with 28% of males and 1.2% females homozygous for HFE C282Y manifesting HH (women may be protected by menses). Alcohol consumption, diabetes, and dietary heme intake (as opposed to non-heme iron, from sources other than fish and meat) are also recognized modifiers. Type I HH disease severity ranges from mild to severe, with patients typically present in their thirties or forties with non-specific symptoms of arthralgia, malaise, and fatigue. They may present with the classic triad of liver dysfunction, skin hyperpigmentation, and diabetes, but can also have endocrine abnormalities (amenorrhea, impotence, hypothyroidism, hypogonadism, osteoporosis), or more rarely cardiac disease. HH predisposes to susceptibility to infection and mortality [101]. Risk of chronic venous leg ulceration is increased [102]. Endocrinopathy, hepatocellular carcinoma, and heart failure are typically complications of long-term iron overload. Renal failure is extremely rare in HH, but may be present independent of HH [103]. Diagnostic laboratory studies for HH include increased plasma iron and transferrin saturation. Ferritin will also be increased in HH but is an acute phase reactant and can be confounded by the presence of infection or chronic inflammatory diseases. Furthermore, all serum iron studies can be confounded by renal failure. Genetic testing now allows diagnosis prior to development of symptoms. Biopsy can be useful in evaluation of liver fibrosis and cirrhosis. Clinical exam can reveal hepatomegaly before symptoms; signs in symptomatic patients can include hepatomegaly, splenomegaly, stigmata of cirrhosis, joint swelling, dilated cardiomyopathy, CHF, increased pigmentation, porphyria cutanea tarda, testicular atrophy, and signs of hypothyroidism [104].
Treatment
Phlebotomy is the mainstay of HH type I maintenance therapy, and reverses chronic fatigue, cardiac dysfunction, and stabilizes or improves hepatic function, though arthritic symptoms can worsen acutely [100•]. Ultimately, late-stage HH can present as cirrhosis and hepatocellular carcinoma may result in presentation for liver transplant, or rarely for cardiac/hepatic double transplantation [105].
Anesthesia Perioperative Considerations
HH patients may present for unrelated surgical indications, or due to complications of HH such as palliative procedures for cirrhosis, liver and/or heart transplant [106], or joint surgery [107]. Mortality for HH liver transplantation is greater than that for other indications [108, 109], and complication rates for bariatric surgery [110]. The preanesthetic assessments of HH patients should include CBC, CMP, coagulation studies, and endocrine assessments (TFTs, pituitary hormones if endocrinopathy suspected). ECG abnormalities are common, though heart failure is unusual; echocardiography may be helpful in cardiac risk assessment and should be routine for transplantation candidates [100, 111]. MRI, but not CT, has utility in assessment of iron deposition in the liver, heart, and anterior pituitary [111]. Intraoperatively, pharmacokinetic and pharmacodynamics aberrations due to hypoalbuminemia should be anticipated, as well as impaired drug metabolism by cirrhotic livers. For example, muscle relaxation with cisatracurium and atracurium will be more predictable than non-depolarizing relaxants subject to metabolism, and sedatives such as midazolam may accumulate especially with multiple or prolonged exposure. Opioids subject to prodrug metabolism such as codeine may be less effective, or have prolonged/delayed effect, and hepatotoxic agents such as acetaminophen should be minimized. Thrombocytopenia and coagulopathy may be present, requiring care with neuraxial and regional anesthetics. Transfusion is associated with an iron burden and should be judiciously employed (22658368). Post cardiac transplant patients suffer the typical loss of response to indirect sympathomimetics due to denervation.
Wilson’s disease
Pathophysiology
Disruption of copper homeostasis is associated with Wilson disease (WD, OMIM 277900), Menkes syndrome (OMIM 309400), and MEDNIK syndrome (OMIM 609313).
Of inborn errors of iron metabolism, WD is the most common [112•]. Due to inadequate biliary secretion, copper accumulates in the liver where it causes hepatitis, fibrosis, and ultimately cirrhosis. With its inability to load onto ceruloplasmin, copper circulates in an unbound form, precipitating in the kidneys, brain, and eyes where it forms Kayser-Fleischer rings (KFRs). Copper deposition in the brain contributes to the neuropsychiatric presentations of WD. Deposition in the heart causes conduction and functional defects.
Presentation
The estimated prevalence is 1/1500–1/3000 [112•]. Typically, patients present with neurological symptoms in the second or third decade of life, though diagnosis as late as the seventh decade has been reported. Five percent of patients present with liver failure at an earlier age, the youngest being 9 months. Adult neurologic presentations are typically dystonia, Parkinson’s-like symptoms, and/or ataxia, often with a mix of these 3 types. Dysgraphia, tremor, dystonia, and drooling are common [113], and psychiatric presentations also occur. Acutely, hepatic encephalopathy can occur due to cirrhosis. Seizures can also occur, before as well as after initiation of treatment. Increased deep tendon reflexes may be seen, but paralysis is rare, and sensory abnormalities make WD less likely. Despite the well-known sign of Keyser Fleisher rings (copper deposition in the iris), visual acuity is unimpaired. On the other hand, defects in vertical smooth pursuit can be elicited in most patients. Autonomic dysfunction has also been reported in WD [114], with involvement of sympathetic and parasympathetic systems. Observed abnormalities include increased resting heart rate, and impaired baroreflex sensitivity including orthostatic hypotension [115]. Meanwhile, known cardiac manifestations of WD include various conduction defects, as well as anatomic alterations and myriad ECG changes [115]. Heart failure has been reported, including systolic and diastolic [116], and acute cardiac death has been reported. Hematologic abnormalities include thrombocytopenia (50%), neutropenia 30%), and acute hemolytic crisis. Ultimately, almost all systems can be involved including renal (Fanconi syndrome) hematologic and endocrine [117].
Diagnosis and Treatment
A 24-h urinary copper excretion greater than 100 μg per 24 h in the absence of cholestatic disease is consistent with WD. Other tests supporting WD include low serum copper levels, elevated transaminase levels, aminoaciduria, and hemolytic anemia. “Penicillamine challenge” can increase 24-h urinary copper excretion several-fold after two doses, in pediatric patients. Finally, liver biopsies for assessment of liver copper levels can disambiguate differential diagnoses. Genetic testing for relatives of patients is useful. Brain MRI abnormalities are seen in 100% of patients. Upon diagnosis, chelator (d-penicilla-mine, trientine, tetrathiomolybdate) therapy, and/or zinc supplementation is initiated. The latter competes for intestinal uptake, though by itself is less effective than chelation. Response of hepatic markers is seen in > 90% of patients initiated on chelation therapy, but neurologic symptoms may be irreversible in almost 40% of patients [112•]. Stabilization of treatment may take 1–3 years, and the goal is 24-h urine copper < 0.6 mg. Maintenance therapy should be expected to be lifelong and adverse effects may necessitate drug substitution. Biannual surveillance of copper lab studies, and LFTs, has been suggested for evaluating efficacy of treatment [112•]. Liver ultrasound screening for hepatoma is also justified, and liver transplantation can be considered acute fulminant liver failure or decompensated cirrhosis. For neurologic symptom management, botulinum toxin injections may help with dystonia, while primidone may help with tremor. Thalamotomy or deep brain stimulation are also options for resistant tremors.
Anesthesia Perioperative considerations
Preoperative assessment of WD patients should include assessments of end organ damage, including neuropsychiatric status, liver function, and cardiac function. ECG changes are present in 1/3 of WD patients (3829752), and echocardiography may inform cardiac functional status. Advanced WD patients with hepatorenal syndrome may require dialysis prior to elective surgery. Intraoperative management may be performed with lower doses of propofol, as increased sensitivity to propofol’s sedative and cardiorespiratory depressant effects have been reported [118]. Isoflurane improves hepatic blood flow, while sevoflurane reduces it [119], and isoflurane is suggested to be the volatile anesthetic of choice [120]. Delayed metabolism of anesthetics, analgesics, and muscle relaxants should be anticipated, and cisatracurium or avoidance of relaxants would be preferred [120]. Antiemetics with antidopaminergic effects (antipsychotics, metoclopramide) should be avoided due to concern for exacerbation of dystonia and extrapyramidal symptoms (ondansetron can also rarely cause dystonia and should be used with care). Neuraxial anesthetics may be used, with due diligence for coagulopathy and thrombocytopenia. Regional anesthesia may be reasonable for patients on appropriate maintenance therapy [121]. For advanced WD patients, acute neuropsychiatric flares in the postoperative period could be hepatic encephalopathy masquerading as more typical postoperative delirium and should be included in the differential diagnosis.
Urea Cycle Disorders
Pathophysiology
The urea cycle is an enzymatic pathway responsible for removing waste nitrogen from the bloodstream and the production of several endogenous amino acids [2••]. When functioning properly, the system uses a series of biochemical reactions to convert nitrogen, a waste product of protein metabolism, to urea which is cleared by the kidneys.
Urea cycle disorders (UCDs) typically present in neonates and are due to a deficiency or absence of six enzymes or two transporters of the urea cycle resulting in the accumulation of excess ammonia [122].
Partial UCDs are associated with ammonia accumulation at times of physiologic stress (e.g., peripartum, infection, fasting, surgery, and blood loss) [2••, 4]. Diagnosis may be delayed for months or years, but the majority of patients are diagnosed in childhood and less than 10% of patients are diagnosed over the age of 16 [5]. Because of the rare nature and relative unfamiliarity of many clinicians, there are case reports of fatalities during initial presentation even among adults [6–8, 23].
Presentation
Without a functioning clearance system, serum ammonia levels can increase to toxic levels leading to encephalopathy, seizures, brain damage, coma, and eventually death [1].
UCDs are primarily inherited deficiencies in any of the six enzymes in this pathway. Individuals with complete defects appear normal at birth, but are quickly affected and, if left untreated, develop lethargy, and anorexia, before progressing to seizures, coma, and/or death [2]. Overall mortality rate of patients with urea cycle disorders has been reported as high as 85% within 10 years of diagnosis [3].
Treatment
Treatment consists of appropriate dietary management and supplementation to limit ammonia production and decrease levels in the bloodstream. Patients often need frequent and lifelong blood tests to check ammonia levels. Some even require dialysis and ultimately liver transplantation when optimal treatment fails [123•].
Perioperative Anesthesia Considerations
Anesthesia for patients with urea cycle disorders poses serious risks for the patient during the perioperative period. Elective cases should be referred to pediatric hospitals that specialize in the management of metabolic disorders [4].
If feasible, in the period leading up to the procedure, the patient should maintain the typical low-protein diet, supplementation with certain amino acids, and administration of organic compounds to augment waste nitrogen excretion. For elective surgery, the patient should be admitted the day before. Lab work should include plasma ammonia and amino acid levels to ensure the patient is not trending towards an uncompensated state [10]. Elective surgeries should be delayed in the case of infections or signs of metabolic decompensation [4].
During the NPO period, IV replenishment of fluids, glucose, and electrolytes should be maintained to prevent fasting-induced catabolism of proteins which could trigger hyperammonemic crises. Avoiding hyperglycemia is important to prevent osmotic diuresis and volume contraction. Peritoneal dialysis or hemodialysis may be utilized to reverse metabolic abnormalities associated with the disease [11]. The night before surgery, a discussion with the pediatric metabolic specialists is paramount to determine whether sodium benzoate and arginine should be administered prior to the operation [10, 12].
The anesthetic technique needs to be carefully selected as appropriate for the clinical scenario; goals should include limiting stress, pain, and trauma for the patient, and physiologically to limit protein catabolism, maintain optimal hydration status, and facilitate nitrogen excretion [13].
Avoiding physiologic stressors may be beneficial during this period. Tight control over hemodynamics, use of regional and/or neuraxial anesthesia for pain control, and avoidance of intubation if clinical feasible may all assist in the avoiding catabolic states [4, 14].
During prolonged operations, administration of glucose, intralipid, and/or low-protein total parenteral nutrition should be utilized along with intravenous sodium phenylacetate, sodium benzoate, and arginine hydrochloride.
An overnight observation period in the intensive care setting to closely follow neurological status and frequent measurements of plasma ammonium is recommended [4].
Conclusion
Metabolic disorders encompass a group of hundreds of inherited disorders caused by various genetic defects. This goal of this review is to reacquaint the anesthesiologist with more commonly encountered metabolic disorders and address the major perioperative anesthesia issues.
To best care for these patients, it is important that anesthesiologists perform thorough and detailed pre-anesthesia evaluations. If any uncertainty exists about rarer conditions and how to proceed with perioperative management, the anesthesiologist should not hesitate to seek multidisciplinary consultation to ensure safe and optimal care of these patients.
Funding Statement
The authors’ work was supported and funded in part by NIH/NCI Cancer Center Support Grant P30 CA008748
Footnotes
This article is part of the Topical Collection on Pediatric Anesthesia
Conflict of Interest Cindy B. Yeoh, Howard C. Teng, Jacob C. Jackson, Lee P. Hingula, Takeshi Irie, Aron Legler, Corrine E. Levine, Iris Chu, Casey M. Chai, and Luis E. Tollinche declare they have no conflict of interest.
Human and Animal Rights and Informed Consent This article does not contain any studies with human or animal subjects performed by any of the authors.
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
- 1.••.Kliegman R, Stanton B, Schor N, St. Geme J III, Behrman R. Nelson Textbook of Pediatrics. 19th ed: Elsevier Health Sciences; 2011. [Google Scholar]; Published in 2011 this is a textbook review of common metabolic disorders
- 2.Coelho AI, Rubio-Gozalbo ME, Vicente JB, Rivera I. Sweet and sour: an update on classic galactosemia. J Inherit Metab Dis. 2017;40:325–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karadag N, Zenciroglu A, Eminoglu FT, Dilli D, Karagol BS, Kundak A, et al. Literature review and outcome of classic galactosemia diagnosed in the neonatal period. Clin Lab. 2013;59: 1139–46. [DOI] [PubMed] [Google Scholar]
- 4.Dhillon A, Steadman RH. In: Fleisher LA, editor. Liver diseases, anesthesia and uncommon diseases. 6th ed. Philadelphia: Elsevier Saunders; 2012. p. 162–214. [Google Scholar]
- 5.Choudhury A, Das S, Kiran U. Anaesthetic management of a newborn with galactosaemia for congenital heart surgery. Indian Journal of Anaesthesia. 2009;53:219–22. [PMC free article] [PubMed] [Google Scholar]
- 6.Stuart G, Ahmad N. Perioperative care of children with inherited metabolic disorders. Continuing Education in Anaesthesia Critical Care & Pain. 2011;11:62–8. [Google Scholar]
- 7.Hammond S, Krol A, Hampson-Evans D. Normoglycaemia in type 1b glycogen storage disease with difficult venous access. Anaesthesia. 2009;64:1150. [DOI] [PubMed] [Google Scholar]
- 8.Shenkman Z, Golub Y, Meretyk S, Shir Y, Landau D, Landau EH. Anaesthetic management of a patient with glycogen storage disease type 1b. Can J Anaesth. 1996;43:467–70. [DOI] [PubMed] [Google Scholar]
- 9.Bevan JC. Anaesthesia in Von Gierke’s disease. Current approach to management. Anaesthesia. 1980;35:699–702. [DOI] [PubMed] [Google Scholar]
- 10.Yu X, Huang Y, Du J. Bispectral index may not reflect the depth of anaesthesia in a patient with glycogen storage disease type I. Br J Anaesth. 2009;103:616. [DOI] [PubMed] [Google Scholar]
- 11.Wang LY, Ross AK, Li JS, Dearmey SM, Mackey JF, Worden M, et al. Cardiac arrhythmias following anesthesia induction in infantile-onset Pompe disease: a case series. Paediatr Anaesth. 2007;17:738–48. [DOI] [PubMed] [Google Scholar]
- 12.Ing RJ, Cook DR, Bengur RA, Williams EA, Eck J, Dear Gde L, et al. Anaesthetic management of infants with glycogen storage disease type II: a physiological approach. Paediatr Anaesth. 2004;14:514–9. [DOI] [PubMed] [Google Scholar]
- 13.Kim WS, Cho AR, Hong JM, Kim ES, Park SC, Yoon JY, et al. Combined general and epidural anesthesia for major abdominal surgery in a patient with Pompe disease. J Anesth. 2010;24:768–73. [DOI] [PubMed] [Google Scholar]
- 14.McFarlane HJ, Soni N. Pompe’s disease and anaesthesia. Anaesthesia. 1986;41:1219–24. [DOI] [PubMed] [Google Scholar]
- 15.Moses SW, Gadoth N, Bashan N, Ben-David E, Slonim A, Wanderman KL. Neuromuscular involvement in glycogen storage disease type III. Acta Paediatr Scand. 1986;75:289–96. [DOI] [PubMed] [Google Scholar]
- 16.Momoi T, Sano H, Yamanaka C, Sasaki H, Mikawa H. Glycogen storage disease type III with muscle involvement: reappraisal of phenotypic variability and prognosis. Am J Med Genet. 1992;42: 696–9. [DOI] [PubMed] [Google Scholar]
- 17.Olson LJ, Reeder GS, Noller KL, Edwards WD, Howell RR, Michels VV. Cardiac involvement in glycogen storage disease III: morphologic and biochemical characterization with endomyocardial biopsy. Am J Cardiol. 1984;53:980–1. [DOI] [PubMed] [Google Scholar]
- 18.Miller CG, Alleyne GA, Brooks SE. Gross cardiac involvement in glycogen storage disease type 3. Br Heart J. 1972;34:862–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tada H, Kurita T, Ohe T, Shimomura K, Ishihara T, Yamada Y, et al. Glycogen storage disease type III associated with ventricular tachycardia. Am Heart J. 1995;130:911–2. [DOI] [PubMed] [Google Scholar]
- 20.LaBarbera M, Milechman G, Dulbecco F. Premature coronary artery disease in a patient with glycogen storage disease III. J Invasive Cardiol. 2010;22:E156–8. [PubMed] [Google Scholar]
- 21.Mohart D, Russo P, Tobias JD. Perioperative management of a child with glycogen storage disease type III undergoing cardiopulmonary bypass and repair of an atrial septal defect. Paediatr Anaesth. 2002;12:649–54. [DOI] [PubMed] [Google Scholar]
- 22.Bolton SD, Clark VA, Norman JE. Multidisciplinary management of an obstetric patient with glycogen storage disease type 3. Int J Obstet Anesth. 2012;21:86–9. [DOI] [PubMed] [Google Scholar]
- 23.Bollig G McArdle’s disease (glycogen storage disease type V) and anesthesia–a case report and review of the literature. Paediatr Anaesth. 2013;23:817–23. [DOI] [PubMed] [Google Scholar]
- 24.Baum V, O’Flaherty J. Anesthesia for genetic, metabolic, and dysmorphic syndromes of childhood, 2nd ed edition. Philadelphia: Lippincott Williams & Wilkins; 2007. [Google Scholar]
- 25.Coleman P McArdle’s disease. Problems of anaesthetic management for Caesarean section. Anaesthesia. 1984;39:784–7. [DOI] [PubMed] [Google Scholar]
- 26.Bollig G, Mohr S, Raeder J. McArdle’s disease and anaesthesia: case reports. Review of potential problems and association with malignant hyperthermia. Acta Anaesthesiol Scand. 2005;49: 1077–83. [DOI] [PubMed] [Google Scholar]
- 27.Luzardo GE, Karlnoski RA, Williams B, Mangar D, Camporesi EM. Anesthetic management of a parturient with hyperhomocysteinemia. Anesth Analg. 2008;106:1833–6. [DOI] [PubMed] [Google Scholar]
- 28.Slote MU, Khan KK, Khan AA, Butt MN. Is homocystinuria a real challenge for anesthetist? Are we making a difference? Saudi J Anaesth. 2018;12:172–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chambers JC, McGregor A, Jean-Marie J, Kooner JS. Acute hyperhomocysteinaemia and endothelial dysfunction. Lancet. 1998;351:36–7. [DOI] [PubMed] [Google Scholar]
- 30.Al-Obaidi MK, Stubbs PJ, Collinson P, Conroy R, Graham I, Noble MI. Elevated homocysteine levels are associated with increased ischemic myocardial injury in acute coronary syndromes. J Am Coll Cardiol. 2000;36:1217–22. [DOI] [PubMed] [Google Scholar]
- 31.Kang SS, Wong PW, Malinow MR. Hyperhomocyst(e)inemia as a risk factor for occlusive vascular disease. Annu Rev Nutr. 1992;12:279–98. [DOI] [PubMed] [Google Scholar]
- 32.Rimm EB, Willett WC, Hu FB, Sampson L, Colditz GA, Manson JE, et al. Folate and vitamin B6 from diet and supplements in relation to risk of coronary heart disease among women. JAMA. 1998;279:359–64. [DOI] [PubMed] [Google Scholar]
- 33.Vermeulen EG, Stehouwer CD, Twisk JW, van den Berg M, de Jong SC, Mackaay AJ, et al. Effect of homocysteine-lowering treatment with folic acid plus vitamin B6 on progression of sub-clinical atherosclerosis: a randomised, placebo-controlled trial. Lancet. 2000;355:517–22. [DOI] [PubMed] [Google Scholar]
- 34.Dierkes J, Westphal S, Luley C. The effect of fibrates and other lipid-lowering drugs on plasma homocysteine levels. Expert Opin Drug Saf. 2004;3:101–11. [DOI] [PubMed] [Google Scholar]
- 35.Zhang Q, Li S, Li L, Li Q, Ren K, Sun X, et al. Metformin treatment and homocysteine: a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2016;8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ueland PM, Refsum H. Plasma homocysteine, a risk factor for vascular disease: plasma levels in health, disease, and drug therapy. J Lab Clin Med. 1989;114:473–501. [PubMed] [Google Scholar]
- 37.Bazzano LA, Reynolds K, Holder KN, He J. Effect of folic acid supplementation on risk of cardiovascular diseases: a meta-analysis of randomized controlled trials. JAMA. 2006;296: 2720–6. [DOI] [PubMed] [Google Scholar]
- 38.Miller ER 3rd, Juraschek S, Pastor-Barriuso R, Bazzano LA, Appel LJ, Guallar E. Meta-analysis of folic acid supplementation trials on risk of cardiovascular disease and risk interaction with baseline homocysteine levels. Am J Cardiol. 2010;106:517–27. [DOI] [PubMed] [Google Scholar]
- 39.Ray JG, Kearon C, Yi Q, Sheridan P, Lonn E. Heart Outcomes Prevention Evaluation I: homocysteine-lowering therapy and risk for venous thromboembolism: a randomized trial. Ann Intern Med. 2007;146:761–7. [DOI] [PubMed] [Google Scholar]
- 40.den Heijer M, Willems HP, Blom HJ, Gerrits WB, Cattaneo M, Eichinger S, et al. Homocysteine lowering by B vitamins and the secondary prevention of deep vein thrombosis and pulmonary embolism: a randomized, placebo-controlled, double-blind trial. Blood. 2007;109:139–44. [DOI] [PubMed] [Google Scholar]
- 41.Behman REKR, Jenson HB. Nelson textbook of paediatrics. 16th ed; 2000. [Google Scholar]
- 42.Yap S, Boers GH, Wilcken B, Wilcken DE, Brenton DP, Lee PJ, et al. Vascular outcome in patients with homocystinuria due to cystathionine beta-synthase deficiency treated chronically: a multicenter observational study. Arterioscler Thromb Vasc Biol. 2001;21:2080–5. [DOI] [PubMed] [Google Scholar]
- 43.Teng YH, Sung CS, Liao WW, Kao SC, Huang YY, Tsou MY, et al. General anesthesia for patient with homocystinuria–a case report. Acta Anaesthesiol Sin. 2002;40:153–6. [PubMed] [Google Scholar]
- 44.Badner NH, Beattie WS, Freeman D, Spence JD. Nitrous oxide-induced increased homocysteine concentrations are associated with increased postoperative myocardial ischemia in patients undergoing carotid endarterectomy. Anesth Analg. 2000;91:1073–9. [DOI] [PubMed] [Google Scholar]
- 45.Stoelting RKDS. Anaesthesia and coexisting diseases. 4th ed. Philadelphia: Churchill Livingstone; 2002. [Google Scholar]
- 46.National Institutes of Health Consensus Development P. National Institutes of Health Consensus Development Conference Statement: phenylketonuria: screening and management, October 16–18, 2000. Pediatrics. 2001;108:972–82. [DOI] [PubMed] [Google Scholar]
- 47.Douglas TD, Jinnah HA, Bernhard D, Singh RH. The effects of sapropterin on urinary monoamine metabolites in phenylketonuria. Mol Genet Metab. 2013;109:243–50. [DOI] [PubMed] [Google Scholar]
- 48.Pietz J, Kreis R, Rupp A, Mayatepek E, Rating D, Boesch C, et al. Large neutral amino acids block phenylalanine transport into brain tissue in patients with phenylketonuria. J Clin Invest. 1999;103: 1169–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lee P, Smith I, Piesowicz A, Brenton D. Spastic paraparesis after anaesthesia. Lancet. 1999;353:554. [DOI] [PubMed] [Google Scholar]
- 50.Dal D, Celiker V. Anaesthetic management of a strabismus patient with phenylketonuria. Paediatr Anaesth. 2003;13:740–1. [DOI] [PubMed] [Google Scholar]
- 51.Rayadurg V, Uttarwar A, Surve R. Is propofol safe in patients with phenylketonuria? J Neurosurg Anesthesiol. 2018;30:85–6. [DOI] [PubMed] [Google Scholar]
- 52.Rivera-Cruz B Mitochondrial diseases and anesthesia: a literature review of current opinions. AANA J. 2013;81:237–43. [PubMed] [Google Scholar]
- 53.Rech VC, Feksa LR, Dutra-Filho CS, Wyse AT, Wajner M, Wannmacher CM. Inhibition of the mitochondrial respiratory chain by phenylalanine in rat cerebral cortex. Neurochem Res. 2002;27:353–7. [DOI] [PubMed] [Google Scholar]
- 54.Delaney A, Gal Thomas J. Hazards of anesthesia and operation in maple-syrup-urine disease. Anesthesiology. 1976;44:83–6. [DOI] [PubMed] [Google Scholar]
- 55.Kahraman S, Ercan M, Akkus O, Ercelen O, Erdem K, Coskun T. Anaesthetic management in maple syrup urine disease. Anaesthesia. 1996;51:575–8. [DOI] [PubMed] [Google Scholar]
- 56.Griffiths S, Stuart G, Alp Karahan M, & Frazier D: Anaesthesia recommendations for patients suffering from Maple syrup urine disease. 2015
- 57.Hamosh A, Kniffin C, Krasikov N, & McKusick V : Maple syrup urine disease; MSUD. 2018 [Google Scholar]
- 58.Fuentes-Garcia D, Falcon-Arana L. Perioperative management of a patient with maple syrup urine disease. BJA: Br J Anaesth. 2009;102:144–5. [DOI] [PubMed] [Google Scholar]
- 59.Vaidyanathan K, Narayanan MP, Vasudevan DM. Organic acidurias: an updated review. Indian J Clin Biochem. 2011;26: 319–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.•.Baumgartner MR, Horster F, Dionisi-Vici C, Haliloglu G, Karall D, Chapman KA, et al. Proposed guidelines for the diagnosis and management of methylmalonic and propionic acidemia. Orphanet J Rare Dis. 2014;9:130. [DOI] [PMC free article] [PubMed] [Google Scholar]; Guidelines developed using the SIGN methodology by having professionals on MMA/PA across twelve European countries and the USA gather all the existing evidence, score it according to the SIGN evidence level system, and make a series of conclusive statements supported by an associated level of evidence.
- 61.Aldubayan SH, Rodan LH, Berry GT, Levy HL. Acute illness protocol for organic acidemias: methylmalonic acidemia and propionic acidemia. Pediatr Emerg Care. 2017;33:142–6. [DOI] [PubMed] [Google Scholar]
- 62.Shaikh N, Hashmi MG, Shah C, Dhansura T. Anaesthetic considerations in a patient with methylmalonyl-coenzyme A mutase deficiency. Indian J Anaesth. 2017;61:1018–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Sharar SR, Haberkern CM, Jack R, Scott CR. Anesthetic management of a child with methylmalonyl-coenzyme A mutase deficiency. Anesth Analg. 1991;73:499–501. [DOI] [PubMed] [Google Scholar]
- 64.Arcas-Bellas JJ, Arevalo-Ludena J, Onate ML, Aranzubia M, Alvarez-Rementeria R, Munoz-Alameda L. General anesthesia in an adult female with propionic acidemia: anesthetic considerations. Minerva Anestesiol. 2013;79:313–5. [PubMed] [Google Scholar]
- 65.Harker HE, Emhardt JD, Hainline BE. Propionic acidemia in a four-month-old male: a case study and anesthetic implications. Anesth Analg. 2000;91:309–11. [DOI] [PubMed] [Google Scholar]
- 66.Karagoz AH, Uzumcugil F, Celebi N, Canbay O, Ozgen S. Anesthetic management of a 2-year-old male with propionic acidemia. Paediatr Anaesth. 2006;16:1290–1. [DOI] [PubMed] [Google Scholar]
- 67.Rajakumar A, Kaliamoorthy I, Reddy MS, Rela M. Anaesthetic considerations for liver transplantation in propionic acidemia. Indian J Anaesth. 2016;60:50–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ryu J, Shin YH, Ko JS, Gwak MS, Kim GS. Intractable metabolic acidosis in a child with propionic acidemia undergoing liver transplantation -a case report. Korean J Anesthesiol. 2013;65:257–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Baba C, Kasahara M, Kogure Y, Kasuya S, Ito S, Tamura T, et al. Perioperative management of living-donor liver transplantation for methylmalonic acidemia. Paediatr Anaesth. 2016;26:694–702. [DOI] [PubMed] [Google Scholar]
- 70.Ktena YP, Ramstad T, Baker EH, Sloan JL, Mannes AJ, Manoli I, et al. Propofol administration in patients with methylmalonic acidemia and intracellular cobalamin metabolism disorders: a review of theoretical concerns and clinical experiences in 28 patients. J Inherit Metab Dis. 2015;38:847–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ruzkova K, Weingarten TN, Larson KJ, Friedhoff RJ, Gavrilov DK, Sprung J. Anesthesia and organic aciduria: is the use of lactated Ringer’s solution absolutely contraindicated? Paediatr Anaesth. 2015;25:807–17. [DOI] [PubMed] [Google Scholar]
- 72.Weinberg GL, Laurito CE, Geldner P, Pygon BH, Burton BK. Malignant ventricular dysrhythmias in a patient with isovaleric acidemia receiving general and local anesthesia for suction lipectomy. J Clin Anesth. 1997;9:668–70. [DOI] [PubMed] [Google Scholar]
- 73.Soberon JR, Elliott CE, Bland KS, Weinberg GL. Peripheral nerve block in a patient with propionic acidemia. Reg Anesth Pain Med. 2014;39:560–1. [DOI] [PubMed] [Google Scholar]
- 74.DiMauro S, Schon EA. Mitochondrial respiratory-chain diseases. N Engl J Med. 2003;348:2656–68. [DOI] [PubMed] [Google Scholar]
- 75.••.Hsieh VC, Krane EJ, Morgan PG. Mitochondrial Disease and Anesthesia. J Inborn Errors Metab Screen. 2017;5: 2326409817707770. [Google Scholar]; Published in 2017, this is a good review of mitochondrial disease and anesthesia.
- 76.Muravchick S, Levy RJ. Clinical implications of mitochondrial dysfunction. Anesthesiology. 2006;105:819–37. [DOI] [PubMed] [Google Scholar]
- 77.•.Niezgoda J, Morgan PG. Anesthetic considerations in patients with mitochondrial defects. Paediatr Anaesth. 2013;23:785–93. [DOI] [PMC free article] [PubMed] [Google Scholar]; Published in 2013, this review provides detailed anesthetic considerations for patients with mitochondrial disorders.
- 78.Hanley PJ, Ray J, Brandt U, Daut J. Halothane, isoflurane and sevoflurane inhibit NADH:ubiquinone oxidoreductase (complex I) of cardiac mitochondria. J Physiol. 2002;544:687–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wolf A, Weir P, Segar P, Stone J, Shield J. Impaired fatty acid oxidation in propofol infusion syndrome. Lancet. 2001;357:606–7. [DOI] [PubMed] [Google Scholar]
- 80.Weinberg GL, Palmer JW, VadeBoncouer TR, Zuechner MB, Edelman G, Hoppel CL. Bupivacaine inhibits acylcarnitine exchange in cardiac mitochondria. Anesthesiology. 2000;92:523–8. [DOI] [PubMed] [Google Scholar]
- 81.Parikh S, Saneto R, Falk MJ, Anselm I, Cohen BH, Haas R, et al. A modern approach to the treatment of mitochondrial disease. Curr Treat Options Neurol. 2009;11:414–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Richtsfeld M, Belani KG. Lysosomal storage diseases: past, present, and future. Anesth Analg. 2017;125:716–8. [DOI] [PubMed] [Google Scholar]
- 83.Platt FM, d’Azzo A, Davidson BL, Neufeld EF, Tifft CJ. Lysosomal storage diseases. Nat Rev Dis Primers. 2018;4:27. [DOI] [PubMed] [Google Scholar]
- 84.Yuasa T, Takenaka T, Higuchi K, Uchiyama N, Horizoe Y, Cyaen H, et al. Fabry disease. J Echocardiogr. 2017;15:151–7. [DOI] [PubMed] [Google Scholar]
- 85.Clark BM, Sprung J, Weingarten TN, Warner ME. Anesthesia for patients with mucopolysaccharidoses: comprehensive review of the literature with emphasis on airway management. Bosnian J Basic Med Sci. 18:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Scarpa M, Lourenco CM, Amartino H. Epilepsy in mucopolysaccharidosis disorders. Mol Genet Metab. 2017;122(s):55–61. [DOI] [PubMed] [Google Scholar]
- 87.Mueller P, Attenhofer Jost CH, Rohrbach M, Valsangiacomo Buechel ER, Seifert B, Balmer C, et al. Cardiac disease in children and young adults with various lysosomal storage diseases: comparison of echocardiographic and ECG changes among clinical groups. Int J Cardiol Heart Vessel. 2013;2:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Linhart A, Elliott PM. The heart in Anderson-Fabry disease and other lysosomal storage disorders. Heart. 2007;93:528–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Megens JH, de Wit M, van Hasselt PM, Boelens JJ, van der Werff DB, de Graaff JC. Perioperative complications in patients diagnosed with mucopolysaccharidosis and the impact of enzyme replacement therapy followed by hematopoietic stem cell transplantation at early age. Paediatr Anaesth. 2014;24:521–7. [DOI] [PubMed] [Google Scholar]
- 90.Mattioli C, Gemma M, Baldoli C, Sessa M, Albertin A, Beretta L. Sedation for children with metachromatic leukodystrophy undergoing MRI. Paediatr Anaesth. 2007;17:64–9. [DOI] [PubMed] [Google Scholar]
- 91.Santamaria F, Montella S, Mirra V, De Stefano S, Andria G, Parenti G. Respiratory manifestations in patients with inherited metabolic diseases. 2013;22:437–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Maria Fuller PJM, Hopwood JJ. Epidemiology of lysosomal storage diseases: an overview, Fabry disease: perspectives from 5 years of FOS. Oxford: Oxford PharmaGenesis; 2006. [PubMed] [Google Scholar]
- 93.Gahl WA. Cystinosis, Pediatric Nephrology. Berlin: Springer; 2009. [Google Scholar]
- 94.Schneider JA, Schulman JD. Cystinosis and the Fanconi syndrome In: Andreoli TDHJF, Fanestil DD, Schultz SG, editors. Physiology of Membrane Disorders. Boston: Springer; 1986. [Google Scholar]
- 95.Cherqui S, Courtoy PJ. The renal Fanconi syndrome in cystinosis: pathogenic insights and therapeutic perspectives. Nat Rev Nephrol. 2017;13:115–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Ioscovich A, Elstein Y, Halpern S, Vatashsky E, Grisaru-Granovsky S, Elstein D. Anesthesia for obstetric patients with Gaucher disease: survey and review. Int J Obstet Anesth. 2004;13:244–50. [DOI] [PubMed] [Google Scholar]
- 97.Hernandez-Palazon J Anaesthetic management in children with metachromatic leukodystrophy. Paediatr Anaesth. 2003;13:733–4. [DOI] [PubMed] [Google Scholar]
- 98.Huizing M, Helip-Wooley A, Westbroek W, Gunay-Aygun M, Gahl WA. Disorders of lysosome-related organelle biogenesis: clinical and molecular genetics. Annu Rev Genomics Hum Genet. 2008;9:359–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Campo M, Berliner N. Hemophagocytic lymphohistiocytosis in adults. Hematol Oncol Clin North Am. 2015;29:915–25. [DOI] [PubMed] [Google Scholar]
- 100.•.Brissot P, Pietrangelo A, Adams PC, de Graaff B, McLaren CE, Loreal O. Haemochromatosis. Nat Rev Dis Primers. 2018;4: 18016. [DOI] [PMC free article] [PubMed] [Google Scholar]; Published in 2018, this is a recent overview of hemochromatosis.
- 101.Ganz T. Iron and infection. Int J Hematol. 2018;107:7–15. [DOI] [PubMed] [Google Scholar]
- 102.Zamboni P, Tognazzo S, Izzo M, Pancaldi F, Scapoli GL, Liboni A, et al. Hemochromatosis C282Y gene mutation increases the risk of venous leg ulceration. J Vasc Surg. 2005;42:309–14. [DOI] [PubMed] [Google Scholar]
- 103.Ozkurt S, Acikalin MF, Temiz G, Akay OM, Soydan M. Renal hemosiderosis and rapidly progressive glomerulonephritis associated with primary hemochromatosis. Ren Fail. 2014;36:814–6. [DOI] [PubMed] [Google Scholar]
- 104.Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS. American Association for the Study of Liver D: diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology. 2011;54:328–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Moini M, Mistry P, Schilsky ML. Liver transplantation for inherited metabolic disorders of the liver. Curr Opin Organ Transplant. 2010;15:269–76. [DOI] [PubMed] [Google Scholar]
- 106.Raichlin E, Daly RC, Rosen CB, McGregor CG, Charlton MR, Frantz RP, et al. Combined heart and liver transplantation: a single-center experience. Transplantation. 2009;88:219–25. [DOI] [PubMed] [Google Scholar]
- 107.Barg A, Elsner A, Hefti D, Hintermann B. Total ankle arthroplasty in patients with hereditary hemochromatosis. Clin Orthop Relat Res. 2011;469:1427–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Beaton MD, Adams PC. Prognostic factors and survival in patients with hereditary hemochromatosis and cirrhosis. Can J Gastroenterol. 2006;20:257–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kowdley KV, Brandhagen DJ, Gish RG, Bass NM, Weinstein J, Schilsky ML, et al. National Hemochromatosis Transplant R: survival after liver transplantation in patients with hepatic iron overload: the national hemochromatosis transplant registry. Gastroenterology. 2005;129:494–503. [DOI] [PubMed] [Google Scholar]
- 110.Gerhard GS, Chokshi R, Still CD, Benotti P, Wood GC, Freedman-Weiss M, et al. The influence of iron status and genetic polymorphisms in the HFE gene on the risk for postoperative complications after bariatric surgery: a prospective cohort study in 1,064 patients. Patient Saf Surg. 2011;5:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Shander A, Berth U, Betta J, Javidroozi M. Iron overload and toxicity: implications for anesthesiologists. J Clin Anesth. 2012;24:419–25. [DOI] [PubMed] [Google Scholar]
- 112.•.Bandmann O, Weiss KH, Kaler SG. Wilson’s disease and other neurological copper disorders. Lancet Neurol. 2015;14:103–13. [DOI] [PMC free article] [PubMed] [Google Scholar]; A comprehensive overview of Wilson’s and other copper disorders from 2015.
- 113.Clayton PT. Inherited disorders of transition metal metabolism: an update. J Inherit Metab Dis. 2017;40:519–29. [DOI] [PubMed] [Google Scholar]
- 114.Li K, Lindauer C, Haase R, Rudiger H, Reichmann H, Reuner U, et al. Autonomic dysfunction in Wilson’s disease: a comprehensive evaluation during a 3-year follow up. Front Physiol. 2017;8: 778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Kuan P Cardiac Wilson’s disease. Chest. 1987;91:579–83. [DOI] [PubMed] [Google Scholar]
- 116.Grandis DJ, Nah G, Whitman IR, Vittinghoff E, Dewland TA, Olgin JE, et al. Wilson’s Disease and Cardiac Myopathy. Am J Cardiol. 2017;120:2056–60. [DOI] [PubMed] [Google Scholar]
- 117.Ferreira CR, Gahl WA. Disorders of metal metabolism. Transl Sci Rare Dis. 2017;2:101–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Langley A, Dameron CT. Copper and anesthesia: clinical relevance and management of copper related disorders. Anesthesiol Res Pract. 2013;2013:750901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Kobayashi M The effects of sevoflurane and isoflurane on hepatic blood flow in man. Masui. 1996;45:281–6. [PubMed] [Google Scholar]
- 120.Baykal M, Karapolat S. Anesthetic management of a pediatric patient with wilsons disease. J Clin Med Res. 2010;2:99–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Foubert-Samier A, Kazadi A, Rouanet M, Vital A, Lagueny A, Tison F, et al. Axonal sensory motor neuropathy in copper-deficient Wilson’s disease. Muscle Nerve. 2009;40:294–6. [DOI] [PubMed] [Google Scholar]
- 122.Blair NF, Cremer PD, Tchan MC. Urea cycle disorders: a life-threatening yet treatable cause of metabolic encephalopathy in adults. Pract Neurol. 2015;15:45–8. [DOI] [PubMed] [Google Scholar]
- 123.•.Häberle J, Boddaert N, Burlina A, Chakrapani A, Dixon M, Huemer M, et al. Suggested guidelines for the diagnosis and management of urea cycle disorders. Orphanet J Rare Dis. 2012;7:32. [DOI] [PMC free article] [PubMed] [Google Scholar]; Published in 2012, this comprehensive overview of urea cycle disorders incorporates new trends and emerging therapies.