Introduction
Clinical and community-based organizations (CBOs) can best care for patients through collaboration (Centers for Disease Control and Prevention, 2016). These partnerships, or Community-Clinical Linkages (CCLs), can link patients to specific services to address external barriers to healthcare delivery (Schroeder, 2007). CCLs “help to connect health care providers, community organizations, and public health agencies so they can improve patients’ access to preventive and chronic care services” (Agency for Healthcare Research and Quality, 2016). CCL models are evolving across the United States as a health systems approach that seeks to extend the continuum of care from the clinic to the community (Porterfield et al., 2012). In this context, productive application and adaptation of the CCL concept would benefit from further exploration on effective mechanisms for linking patients and community resources as well as the differentiation between a simple referral process and an actual linkage, or the assurance that the resources referred to have been accessed. In this paper, we present the results of a scoping review designed to examine the role of community health workers as a mechanism for linking patients to community resources.
CCLS and the Social Determinants of Health
Creating CCLs has the potential to improve patient health outcomes by addressing the social determinants of health (SDH) (Balasubramanian et al., 2008; Etz et al., 2008; Quigley, Matsuoka, Montgomery, Khanna, & Nolan, 2014). SDHs are the “conditions in the environments in which people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks” (Office of Disease Prevention and Health Promotion, 2014). Addressing SDH for adverse health outcomes is often motivated by the difficulty in improving healthcare outcomes for low-income groups who are experiencing health inequities (Rosenthal, Rush, & Allen, 2016). The high cost of inpatient and emergency care has also contributed to efforts to identify lower cost community-based approaches (Islam et al., 2016).
In an ideal linkage model, clinic staff have additional resources to support patients in addressing healthy behaviors, while community organizations may also gain clients for the SDH services that are available (Agency for Healthcare Research and Quality, 2016). In this scenario, there is a continuum of care that moves beyond a patient’s clinical needs to include broader SDH services such as housing or transportation. Improved health outcomes stemming from connecting clinics with community resources have been documented as: BMI and weight loss (Holtrop, Dosh, Torres, & Thum, 2008; Lavin et al., 2006; McQuigg et al., 2005), dietary patterns, alcohol and tobaccos use (Holtrop et al., 2008), and increased physical activity (Balasubramanian et al., 2008; Holtrop et al., 2008). Funding for such programs exists through a variety of sources including the Centers for Medicare and Medicaid Services (CMS) Accountable Health Communities Model (2017). Few studies identify the most effective ways to create and sustain linkages.
CCLs and Community Health Workers
One promising way to form CCLs is by building interventions with Community Health Workers (CHWs) (Quigley et al., 2014). The American Public Health Association (APHA) defines a CHW as a “frontline public health worker who is a trusted member of and/or has an unusually close understanding of the community served” (American Public Health Association, 2016). CHWs act as a linkage broker connecting clinic and community resources in ways that benefit patients (Ingram et al., 2012). Frequently, CHWs are hired to participate in disease and/or population specific programs (Rush, 2012) that may not provide them the space to develop CCLs. In cases where CHWs can link clients to resources, results may include medical outcomes with limited information about CCLs. Consequently, little is known about CCL with CHW interventions and whether they are an effective and efficient mechanism for improving patient health outcomes. In order to advance the field of CCLs with CHWs, a review of existing approaches to linkage is warranted.
Given the proliferation of CCLS with CHWs, the objective of this research was to conduct a scoping review to fill the identified need for more information on effective mechanisms of CCLs with CHWs. Unlike a systematic review that examines the effectiveness of an intervention based on specific outcomes, a scoping review can be useful to map existing evidence especially in new topic areas (Arksey, & O’Malley, 2005). Specifically, we sought to examine the range of CCL with CHW interventions in the United States with a focus on linkage formation, maintenance, and outcomes. In this scoping review we (1) describe existing CCL models using the CHW workforce; (2) analyze application of CHW core competencies using the Progress Report of the Community Health Worker Core Consensus (C3) Project (Rosenthal, Rush, & Allen, 2016); and (3) make recommendations for future research and practice in the field (Peters et al., 2015).
Extensive Literature Review
We performed a scoping review to synthesize evidence concerning the role of CHWs in creating and sustaining CCL interventions aimed at improving individual health outcomes. We conducted a preliminary search for scoping reviews on CCLs with CHWs in the Joanna Briggs Institute Database of Scoping Reviews and Implementations Reports, the Cochrane Database of Scoping Reviews, and the Campbell Collection. We did not find any scoping reviews in our topic area.
Methods
Our objective was to find articles that described the core concept of CCL with CHW programs in the context of the United States in order to compare linkages across interventions that function within similar healthcare systems. We conducted a search for English-language articles in the electronic databases PubMed, CINAHL, and Web of Science. We also hand-searched journal issues for additional studies. Recognizing that linkage models were in practice prior to the development of the term CCL and particularly using the CHW workforce, we did not apply a time frame or parameters for the priority population to our search to ensure the inclusion of all examples. Because the terms CCL and CHW have many synonyms, we developed search terms relating to each (see Appendix A).
In order to better understand the broad scope of CHW activities in the 11 articles reviewed, we categorized CHW activities using the Progress Report of the Community Health Worker Core Consensus (C3) Project. The C3 Project is a recent report of CHW core activities based on a nation-wide study, previous CHW research, and a consensus process among state CHW professional organizations and stakeholders (Rosenthal, Rush, & Allen, 2016). By applying the C3 Project roles to the CCLs with CHW activities identified in our review, we sought to use a standardized framework to analyze CHW work that can be compared to future CHW studies.
Results
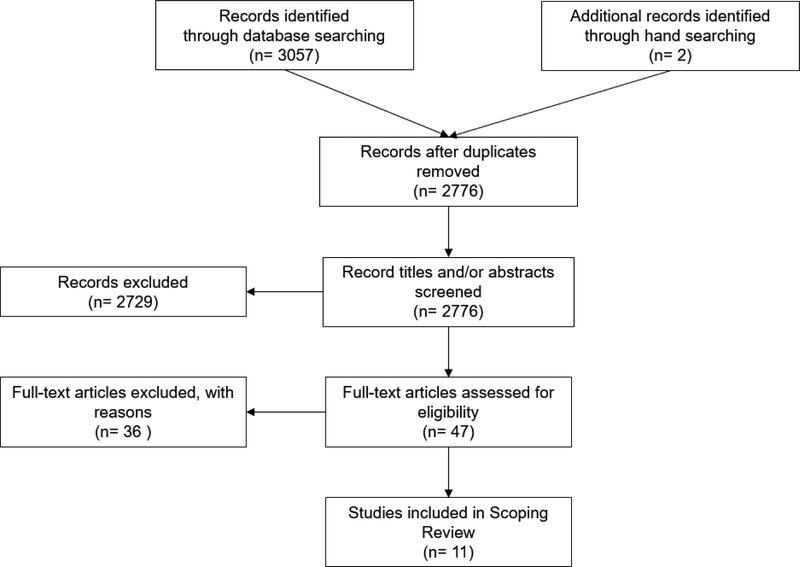
We identified 3057 records from the databases and 2 records through hand searching (see Figure 1). We removed duplicates and reviewed the title and/or abstracts of the remaining 2776 articles to determine eligibility for our secondary inclusion criteria: titles or abstracts that described a CHW intervention in the United States in which a healthcare organization (an organization providing clinical services to patients) and a CBO (an organization providing social determinant of health services such as a community center) collaborated.
Figure 1.
Flow Diagram of the Literature Review Process for Examining Community-Clinical Linkages with Community Health Workers
A total of 47 articles underwent full text review. Two independent reviewers rated the 47 screened programs. There was high inter-reviewer agreement (Ƙ=.70) for the final article inclusion. In cases of disagreement, the reviewers reconciled differences of opinion and came to a consensus based on the tertiary inclusion criteria: articles that described an intervention where the CHW’s relationship to the community aligns with the APHA definition of CHWs; articles that described CCLs that include the participation of a CHW either within the clinic or community setting; articles that include an actual linkage; and articles with outcomes. We extracted information about the priority community, health issue addressed, CHW role and training, the intervention and how participants were linked to resources, measurement methods, and outcomes. Eleven peer-reviewed articles were included in the final review. In the case of the Lay Health Advisor program described by Earp, we found that the background information we needed for the review was in the 1997 article while the outcome information was in the follow-up article from 2002. We included both articles as one study and noted in the results section which details were retrieved from which article. We emailed study authors to clarify details as necessary.
The majority of studies included in this review focused on adults. Only one study concentrated on children with asthma. Diabetes was the focus of four studies while the remaining articles targeted a range of health issues. The 11 reviewed studies prioritized several different populations including: Latinos, African Americans, pregnant women, farmworkers, as well as uninsured people, children, Vietnamese Americans and adults with unmet long-term care needs. Characteristics of the CHW role are described in Table 1.
Table 1.
Characteristics of Community Health Workers in Community-Clinical Linkages
| Priority Population and Health Issue | CHW Job Title | Location where CHWs based their work | CHW Training | |
|---|---|---|---|---|
| Balcazar 2005 | Cardiovascular disease risk among Latinos | Promotora | Community-based organization (CBO) | Intervention protocol |
| de Heer 2015 | Cardiovascular disease risk among Latinos | Promotora | CBO | No details provided |
| Earp 1997 | Breast cancer screening for African American women | Lay Health Advisor and Community Outreach Specialist | LHAs in community; COS employed by health agencies |
CHW core competencies; disease specific training (breast cancer); health education |
| Felix 2011 | Long term care services for at-risk disabled/elderly adults | Community Health Worker | CBO | Intervention protocol |
| Ingram 2005 | Diabetes self-management among Latinos | Promotora | Clinic | Not reported |
| Ingram 2007 | Diabetes among Farmworkers | Promotora | Clinic and CBO | Not reported |
| Johnson 2014 | Diabetes among African Americans | Church Health Representative (CHR) | Volunteers based in churches | Health education (Stanford Chronic Disease Self-Management Program) |
| Lemak 2004 | Health insurance for the Uninsured | Health Navigator | Clinics | Not reported |
| Peretz 2012 | Pediatric asthma in immigrant neighborhoods | Community Health Worker | CBO | CHW core competencies; disease specific training (pediatric asthma); intervention protocol |
| Redding 2015 | Low birth weight prevention for women at risk for poor birth outcomes | Community Health Worker | CBO | CHW core competencies |
| Wennerstrom 2015 | Hypertension and diabetes among Vietnamese Americans | Community Health Worker | CBO | CHW core competencies; disease specific training (diabetes, hypertension, and mental health); intervention protocol |
The articles described CHWs using the following terms: Promotoras, Community Health Workers, Community Outreach Specialists, Lay Health Advisors, Church Health Representatives, Outreach Workers, and Health Navigators. In five studies, the CHWs were employed in CBOs, in two studies the CHWs were based in clinics and in one study there were CHWs working together in both locations. Two studies reported CHWs working from the community, one of which had a secondary CHW role in clinics or the county health department.
Of the 11 studies we reviewed, seven reported on CHW training. The topics covered in CHW training for each study differed and reflected how CHW scope of practice is evolving. CHWs were trained on study intervention protocols, core competencies, capacity building, and the target disease being addressed. CHW core competencies are the potential range of skills and qualities that make up CHW work such as advocacy, patient support, or education (Rosenthal, Rush, & Allen, 2016). In addition, CHWs were trained on the local community and available social services, family-focused disease management, environmental assessment, problem solving, and goal setting.
Table 2 describes the components and outcomes of the included CCLs with CHW interventions. The study sample size ranged from 31 to 3,666 participants. Study entry criteria included Latino families, Hispanic adult residents living in Texas, rural African American women 50 years and older, Medicaid recipients in Alabama, Hispanic adults living in Arizona, Hispanic adults with Type II diabetes, African American adults with Type II diabetes living in Tennessee, uninsured individuals living in Florida, families of children with asthma, residents of Ohio census tracts with high rates of low birth weight and poverty, and Vietnamese American adults with hypertension and diabetes. CHWs recruited patients through community outreach in five studies, clinical referral in one study, and both in four studies. One study did not report on how participants were recruited.
Table 2.
Intervention Components and Outcomes of Included Studies Describing Community-Clinical Linkages with Community Health Workers
| Article | Sample Size | Study Entry Criteria | Community Health Worker Activities | Study Design; Method | Outcome | |||
|---|---|---|---|---|---|---|---|---|
| Participant Recruitment | Linkage | Follow-up Method | Other Activities | |||||
| Balcazar 2005 | 223 families or 320 individual family members | Latino families | Promotora outreach in community settings | Cross linkage: a) nurse attended Promotora classes to facilitate screenings or b) Promotoras transported participants to clinics | Telephone home visits | Health education (group); outreach and awareness; participant advocacy | Program evaluation; Pre/post questionnaire and interviews | Improved heart-healthy behaviors; enhanced information sharing beyond families |
| de Heer 2015 | 413 participants | Hispanic adult, residents of 2 specific El Paso, TX zip codes; not pregnant | Promotora outreach in community settings | Promotoras based at YWCA, received referrals from clinic, linked participants to recreational resources | Telephone home visits email** | Health education (group); outreach and awareness; | Cohort study; Pre/post survey and clinical measures | Improved health-healthy behaviors and cardiovascular risk factors |
| Earp 1997 Earp 2002* | 801 participants | Rural African American women 50 years and older | Lay Health Advisor outreach in community settings | LHAs linked women to Community Outreach Specialists based in county health department or clinics | Not specified* | COS: trained and coordinated LHAs; LHA: outreach and awareness; health education (group and one on one); navigation; participant advocacy* | Nonrandomized community trial; survey | Increased mammography screening |
| Felix 2011 | 919 participants | Medicaid recipients in 3 Alabama counties | CHW outreach in community settings and clinic referral | CHWs used clinic referrals to recruit participants and link them to resources | Not specified | Outreach and awareness; navigation | Longitudinal, quasi-experimental; Pre/post Medicaid record review | Reduced long term care service use and spending |
| Ingram 2005 | 589 graduated from program and were reached for follow-up | People of Hispanic decent living in 2 Arizona counties | Promotora outreach in community settings and clinic referral | Promotoras used clinic referrals to recruit participants and link them to resources | Telephone in 1st site; not specified in 2nd site | Health education; participant advocacy; social support | Participatory evaluation; Pre/post clinical measures, survey, qualitative interviews | Improved clinical measures and self-management behaviors |
| Ingram 2007 | 260 participants | People of Hispanic decent with type 2 diabetes | Promotora outreach in community settings and clinic referral | Clinic Promotoras cross referred to Community Promotoras; both provided referrals to SDH services | In-person telephone home, hospital, office visits | Health education (group); collaborating with providers; providing social support; participant advocacy | Participatory evaluation; Pre/post clinical measures, questionnaires, participation logs | Improved clinical measures among high risk patients; increased support from family and friends |
| Johnson 2014 | 224 patients | African American adults living with type 2 diabetes in Memphis, TN | Church Health Representative outreach in community settings | CHRs linked church members to resources | Case Managers followed-up via phone, email, mail, or other means such as text messaging | Outreach and awareness; participant advocacy | Program evaluation; Pre/post clinical data and survey | Improved: access to resources, self-management, trust and communication with provider, quality of life; improved clinical measures |
| Lemak 2004 | 3,666 client baseline survey respondents 266 client subset for follow-up information 40 stakeholder organizations | Uninsured individuals living in 1 Florida county | Health Navigator outreach in community settings | Health Navigators referred participants to the clinic | Not specified | Outreach and awareness; navigation | Case study; interviews, focus groups, reviews of notes and meeting minutes, surveys | Improved coordination between collaborative organizations |
| Peretz 2012 | 212 individuals | Families of children with asthma | CHW outreach in community settings and clinic referral | CHWs followed-up on hospital referrals and linked participants to resources | Weekly, monthly, then bimonthly check-ins, the manner of communication is not specified | Providing social support; health education | Program evaluation; Pre/post interview survey | Decrease in emergency department visits; increase in self-efficacy |
| Redding 2015 | 115 clients | Residents in 1 of 7 Ohio census tracts with high, low birth weight and poverty rates | Not specified | CHWs used Pathway model to link participants to resources and follow-up | Pathways | Navigation | Cohort study; vital statistics, intervention program, and medical records reviews | Decrease in LBW infants; cost savings |
| Wennerstrom 2015 | 31 patients | Vietnamese American adults with hypertension or diabetes | Clinic referral | CHWs used clinic referrals to recruit participants and link them to resources | Telephone home visits | Intervention protocol; participant advocacy; collaborating with providers; providing social support; health education | Program evaluation; Case conference meetings, project team meetings, survey | Participants satisfied with health education and CHW services; recommendations for CHW integration in PCMH |
As noted earlier, in the case of the Lay Health Advisor program described by Earp, we found that the background information we needed for the review was in the 1997 Earp et al. article while the outcome information was in the follow-up article from 2002 (marked by a *). We included both articles as one study and noted in the methods section which details were retrieved from which article.
Information gathered from email correspondence with Dr. H.D. de Heer.
As stated in our criteria, we included only those articles that indicated an actual linkage, or the assurance that the resources referred to have been accessed, took place between a clinical and community entity rather than a referral without additional follow-up. In 10 out of 11 articles, the CHWs executed the follow-up while in one article, the CHWs referred clients to a case manager who followed-up.
In six studies, CHWs linked participants only to resources with a focus on the clinical concern being researched. In Balcazar et al. (2005) CHWs based at a CBO linked study participants to the clinic for cardiovascular disease screenings by either bringing nurses to their health education classes or providing transportation to the clinic. CHWs followed-up on screening referrals with participants via telephone and home visits. The CHWs in the study done by de Heer et al. (2015) were based at a YWCA, employed by a clinic, and partnered with the local Parks and Recreation Department to promote physical activity, dietary behavior change, and heart-healthy education. According to an email communication from H.D. de Heer, PhD, the CHWs followed up with participants to encourage involvement in the intervention via home visits and email. Earp et al. (1997) employed CHWs in two different roles: Community Outreach Specialists (COS) oversaw the role of the Lay Health Advisors (LHA). LHA performed community outreach to improve awareness of breast cancer screenings, reduced barriers to access, and linked patients to the COS. The COS were based in a clinic or county health department and linked patients to the healthcare system. In Felix et al. (2011), the clinic connected eligible patients to Medicaid and other long term care services including home and community-based services. One of the ways CHWs recruited participants was through clinic referrals. The CHWs then linked study participants to Medicaid enrollment services and/or long term care options (such as nursing homes), followed-up, and provided system navigation as needed. In Johnson et al. (2014), volunteer Church Health Representatives referred church members to case managers and diabetes educators. Case Managers provided followed-up via phone, email, mail, or text messaging and forwarded quarterly reports to the patients’ primary care provider. In Lemak et al. (2004), Health Navigators worked across clinics where they set up appointments for patients, provided follow-up, and linked patients to the Department of Child and Family services as needed. Over time, the Health Navigators developed relationships with the Department of Child and Family services staff and were able to easily resolve eligibility issues.
The scope of CHW practice in the five remaining studies included the ability to link patients to a broader range of SDH services. In Peretz et al. (2012), CHWs employed in CBOs followed-up on hospital referrals, provided in home education, and linked patients to social resources. In Redding et al. (2015), researchers used an outcome based pay model called Pathways (Agency for Healthcare Research and Quality, 2016) to facilitate study participant access to SDH or medical resources. CHWs navigated participants through the Pathways program and provided follow-up. The article did not report how CHWs communicated with resource providers. In Wennerstrom et al. (2015), CHWs were based at a community non-profit agency where they provided links to resources. CHWs and medical providers met for case conference meetings to ensure patients were receiving all necessary SDH and health-specific services. CHWs called or visited patients weekly to problem solve barriers to accessing resources or offer more support. In Ingram et al. (2005) Promotoras based at a clinic taught classes and then followed-up with participants for a six-month period to assist with health insurance, medications, and other social services. Much like Earp et al. (1997), in Ingram et al. (2007) CHWs based in the clinic provided education, set up appointments, and linked to CHWs in the community. Meanwhile, CHWs in the community facilitated support groups and linked patients to SDH services. CHWs were based at clinical and community sites and worked together to ensure that patients received the services they needed.
The majority of the 11 articles used a pre/post evaluation design with additional information regarding resource referral and access. The remaining three articles included two cohort studies, nonrandomized community trial, a case study, and a longitudinal, quasi-experimental study. All 11 studies reported positive outcomes. The CCLs with CHWs resulted in improved heart healthy practices, increased mammography screening, reduced long term care service use and spending, decreased average HbA1c levels, as well as improved coordination between clinics and CBOs, fewer emergency department visits, fewer low birth weight infants, and satisfaction with health education materials, CHW services, and recommendations for CHW integration into clinics.
Categorization of CHW Activities
The C3 Project is a recent report of CHW core activities based on a nation-wide study, previous CHW research, and a consensus process among state CHW professional organizations and stakeholders (Rosenthal, Rush, & Allen, 2016). By applying the C3 Project roles to the CCLs with CHW activities identified in our review, we sought to use a standardized framework to analyze CHW work that can be compared to future CHW studies.
Table 3 demonstrates the application of C3 roles across the included studies. Through home visits, telephone follow-up, or both CHWs conducted outreach in order to follow-up. CHWs advocated for individuals and communities by advocating on behalf of their clients, establishing local advisory committees, expanding awareness of specific health issues in the community, and raising funds for patient care or health programming. The CHWs built individual and community capacity by recruiting, training, and coordinating the efforts of other CHWs. Ten out of eleven articles gave examples of CHWs providing care coordination, case management, and system navigation. In these articles, CHWs referred participants to resources, set up appointments, interacted with providers regarding patient issues, enrolled clients in insurance, and provided system navigation. CHWs also implemented individual and community assessments by participating in the design, implementation, or interpretation of community-level assessments on topics such as the home environment, breast cancer, and daily living activities. In two articles, the CHWs’ role included cultural mediation among individuals, communities, and health and social service systems through the development of relationships with outside agencies and by serving as a cultural mediator. CHWs participated in evaluation and research by recruiting study participants, collecting data, and engaging stakeholders to take action on study findings. CHWs performed direct services by providing basic screening tests for study participants. Some CHWs provided coaching and social support through goal setting, health coaching, and support group facilitation. Finally, in seven studies, CHWs provided culturally appropriate health education and information by teaching health classes and facilitating the use of health promotion resources. The average number of C3 roles performed by CHWs was four.
Table 3.
Community Health Worker Core Consensus (C3) Roles Identified in Included Studies
| C3 Role | Balcazar 2005 | de Heer 2015 | Earp 1997 | Felix 2011 | Ingram 2005 | Ingram 2007 | Johnson 2014 | Lemak 2004 | Peretz 2012 | Redding 2015 | Wennerstrom 2015 | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Building Individual and Community Capacity | x | 1 | ||||||||||
| Providing Direct Service | x | 1 | ||||||||||
| Cultural Mediation among Individuals, Communities, and Health and Social Service Systems | x | x | 2 | |||||||||
| Implementing Individual and Community Assessments | x | x | x | 3 | ||||||||
| Providing Coaching and Social Support | x | x | x | x | 4 | |||||||
| Conducting Outreach | x | x | x | x | x | x | 6 | |||||
| Advocating for Individuals and Communities | x | x | x | x | x | x | 6 | |||||
| Providing Culturally Appropriate Health Education and Information | x | x | x | x | x | x | x | 7 | ||||
| Participating in Evaluation and Research | x | x | x | x | x | x | x | x | x | 9 | ||
| Care Coordination, Case Management, and System Navigation | x | x | x | x | x | x | x | x | x | x | 10 | |
| Total | 6 | 4 | 6 | 3 | 6 | 5 | 2 | 3 | 5 | 2 | 7 |
Discussion: Informing Practice, Policy, and Research
Detailed exploration of the unique role of CHWs within the CCL model provides important guidance to practitioners, scholars and policymakers, in maximizing the impact of this growing workforce in the United States (Islam et al., 2016). All of the 11 studies included in this review described an intervention in which clinics were connecting patients to CBOs facilitated by a CHW.
Our categorization of the roles played by CHWs in the included studies using the C3 Roles indicates that CHW employers may not be consistently taking advantage of the full scope of CHW practice. In some cases, CHWs were tasked with as many as seven roles while in other studies, CHWs were limited to as few as two. While common tasks included care coordination, case management, and system navigation, CHW roles in building individual and community capacity and providing direct services were less utilized. This finding may reflect the emphasis of clinics on the need for care coordination with the exclusion of a range of C3 roles in which CHWs could more directly and broadly engage with community resources. While a specific CHW job may not include all of the C3 Roles, CHW employers could expand opportunities to further improve patient health by empowering CHWs to exercise the full breadth and depth of their linking capabilities. Particularly given the contributions of individual and community capacity building in addressing SDH (Jara, Ritterman Weintraub, Clifton-Hawkins, & Martinez, 2014), integration of these roles in CCL projects may lead to enhanced and sustained health outcomes. Notably, the C3 Roles align with the Institute for Healthcare Improvement Triple Aims that encourage clinics to “improve the patient experience of care, improve the health of populations, and reduce the per capita cost of health care” (SAMHSA, 2012).
Limited understanding of the CHW scope of practice appeared to also restrict the services that CHWs provided to study participants. In half of the reviewed studies, CHWs linked participants to disease or project specific services. In the remaining five studies, CHWs took an approach that encompassed SDH resources as needed by participants. In a scoping review of primary care and public health collaborations, Martin-Misener et al. found that across countries, most collaboration occurred at the grassroots level (2012). As members of the communities at risk for health inequities, CHWs are inherently aware of an array of local SDH needs and services that may assist their clients. CCL interventions would benefit from taking advantage of CHW community knowledge and ability to work at the local level to link patients to a wide range of SDH services.
From a policy perspective, this review is especially relevant in the current health care landscape. In a recent report, the National Academy of Medicine highlighted the underinvestment in social services in the US healthcare system and the resulting high medical care costs and inequity (Adler et al., 2016). The CCL with CHWs model offers a potential solution to providing patients with improved access to social services (Farquhar et al., 2008; Ingram et al., 2014).
We have identified the need for additional research in three areas: CHW training, CCL follow-up methods, and the CHW role in CCLs. Providing more standardized trainings in CHW core competencies may be one approach to further prepare CHWs to act on a greater range of needs for their clients within complex clinical and community environments (O’Brien, Squires, Bixby, & Larson, 2009). Only seven of the studies provided details on CHW training, and four of these seven included training in core competencies. Not surprisingly, three of these four studies engaged CHWs in more C3 roles than the average. We can thus infer that training in the core competencies contributes to the preparation of CHWs to identify and perform a broader range of activities beyond the scope of a specific project or disease area (Rosenthal, Wiggins, Ingram, Mayfield-Johnson, & De Zapien, 2011). Future CCL studies with CHWs should provide more detail on such trainings and how it may affect the CHW role in CCL interventions in order to understand how to apply this model.
The majority of articles stated the methods that CHWs used to follow-up with patients (e.g. phone calls or home visits), but few additional details on specific protocols were described. In order to continue to identify effective models and expand the field of CCLs, more information on the operationalization of the linkages should be defined. In addition to emphasizing the role of follow-up beyond simple referral, it is worthwhile to consider how linkages between organizations are sustained, as well as the length and regularity of ongoing contact with patients.
In a literature review and environmental scan of CCLs focusing on the delivery of prevention services, Porterfield et al. (2012) determined that a dearth of rigorous evaluation made it difficult to determine the effectiveness of CCLs in achieving intermediate or long-term health outcomes. Porterfield did not look specifically at the use of CHWs in creating CCLs, and Ingram et al. (2005) was the only article that the two reviews have in common. Porterfield’s review also included articles that described simple referrals, while in this review we sought to distinguish between referral and actual linkage with the assumption that assurance of the linkage would be more likely to result in a positive outcome. While the 11 studies in our review reported positive outcomes, the diversity of health issues, study design, and outcome measures make it difficult to draw conclusions on whether CCLs with CHWs result in positive health outcomes over time or whether the interventions can be repeated in other contexts. More research is needed to determine the contribution of CHWs to CCLs in creating successful linkages that result in improved quality of service delivery and health outcomes.
In the current review, we focused on examples of peer-reviewed articles that demonstrated CCLs with CHWs. Outside of the literature, several examples of CCLs with CHWs exist. For example, the Institute for Public Health Innovation employs CHWs in the Early Intervention and Retention in Care program for people living with HIV/AIDS (2017). CHWs are placed in community or clinical organizations where they link patients to medical or other SDH resources. In another example, at the Women-Inspired Neighborhood Network (WIN Network, 2017), CHWs link pregnant clients to resources such as utility assistance, healthcare services, or mental health support. While peer-reviewed evidence of CCLs with CHWs is limited, CBOs are currently utilizing this model. These existing CCL with CHW programs offer additional opportunities to study how linkages can be created at the grassroots level.
We confronted limitations in this scoping review. The studies included were heterogeneous and as a result our conclusions must be taken with some caution. Further analysis should be undertaken when the literature is more substantial. In addition, there was a risk of bias at the review level, including the possible incomplete retrieval of identified research. CCL is not a widely used term and CHWs have many job titles. We investigated and searched using several synonyms or related terms for both but we may have missed articles that used still other terms to describe essentially CCL with CHW interventions. Finally, we restricted the review to US studies. We may have missed rich examples of CCLs with CHWs from other countries.
Conclusions
This review offers a novel contribution to understanding the role of CHWs in creating CCLs. In this scoping review, CCLs with CHWs appear to positively impact the delivery of health care and related services across a range of diseases and public health issues, resulting in positive indicators in a variety of contexts. Future research on the depth and breadth, protocols, consistency, and duration of the CCL interventions as well as the impact of training on CHWs executing their roles within CCLs would further advance this promising model.
Supplementary Material
Acknowledgements:
This journal article was supported by the Grant or Cooperative Agreement Number, U48 DP005002 under the Health Promotion and Disease Prevention Research Centers Program, funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Disease Control and Prevention or the Department of Health and Human Services. We would further like to acknowledge Mari J. Stoddard from the University of Arizona Health Sciences Library for her support with reference extraction.
Contributor Information
Abby M. Lohr, University of Arizona Prevention Research Center..
Maia Ingram, University of Arizona Prevention Research Center..
Annabelle V. Nuñez, University of Arizona Health Sciences Library..
Kerstin M. Reinschmidt, University of Oklahoma Health Sciences Center..
Scott C. Carvajal, University of Arizona Prevention Research Center..
References
- Adler NE, Cutler DM, Jonathan JE, Galea S, Glymour M, Koh HK, & Satcher D (2016). Addressing Social Determinants of Health and Health Disparities Discussion Paper, Vital Directions for Health and Health Care Series. National Academy of Medicine, Washington, DC: https://nam.edu/wp-content/uploads/2016/09/addressing-social-determinantsof-health-and-health-disparities.pdf. [Google Scholar]
- Agency for Healthcare Research and Quality. (2016). Clinical-Community Linkages. Retrieved from https://www.ahrq.gov/professionals/prevention-chronic-care/improve/community/index.html
- Agency for Healthcare Research and Quality. (2016). The Quick Start Guide to Developing Community Care Coordination Pathways A Companion to the Pathways Community HUB Manual. Retrieved from https://innovations.ahrq.gov/sites/default/files/Guides/CommHub_QuickStart.pdf
- American Public Health Association. (2016). Community Health Workers. Retrieved from https://www.apha.org/apha-communities/member-sections/community-health-workers [DOI] [PubMed]
- Arksey H, & O’Malley L (2005). Scoping studies: towards a methodological framework. International journal of social research methodology,8(1), 19–32. [Google Scholar]
- Balasubramanian BA, Cohen DJ, Clark EC, Isaacson NF, Hung DY, Dickinson LM, … Crabtree BF (2008). Practice-level approaches for behavioral counseling and patient health behaviors. American Journal of Preventive Medicine, 35(5 Suppl), S407–413. [DOI] [PubMed] [Google Scholar]
- Balcazar H, Alvarado M, Hollen ML, Gonzalez-Cruz Y, & Pedregon V (2005). Evaluation of Salud Para Su Corazon (Health for your Heart) -- National Council of La Raza Promotora Outreach Program. Preventing Chronic Disease, 2(3), A09. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2016). Community-Clinical Linkages for the Prevention and Control of Chronic Disease: A Practitioner’s Guide. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; Retrieved from https://www.cdc.gov/dhdsp/pubs/docs/ccl-practitioners-guide.pdf. [Google Scholar]
- Centers for Medicare and Medicaid Services. (2017). Accountable Health Communities Model. Retrieved from https://innovation.cms.gov/initiatives/ahcm [Google Scholar]
- de Heer HD, Balcazar HG, Wise S, Redelfs AH, Rosenthal EL, & Duarte MO (2015). Improved Cardiovascular Risk among Hispanic Border Participants of the Mi Corazon Mi Comunidad Promotores De Salud Model: The HEART II Cohort Intervention Study 2009–2013. Frontiers in Public Health, 3, 149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earp JA, Eng E, O’Malley MS, Altpeter M, Rauscher G, Mayne L, … Qaqish B (2002). Increasing use of mammography among older, rural African American women: results from a community trial. American Journal of Public Health, 92(4), 646–654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earp JA, Viadro CI, Vincus AA, Altpeter M, Flax V, Mayne L, & Eng E (1997). Lay health advisors: a strategy for getting the word out about breast cancer. Health Education and Behavior, 24(4), 432–451. [DOI] [PubMed] [Google Scholar]
- Etz RS, Cohen DJ, Woolf SH, Holtrop JS, Donahue KE, Isaacson NF, … Olson AL (2008). Bridging primary care practices and communities to promote healthy behaviors. American Journal of Preventive Medicine, 35(5 Suppl), S390–397. [DOI] [PubMed] [Google Scholar]
- Farquhar S, Wiggins N, Michael YL, Luhr G, Jordon J, & Lopez A (2008). “Sitting in different chairs:” roles of the community health workers in the Poder es Salud/Power for Health Project. Education for Health. [PubMed] [Google Scholar]
- Felix HC, Mays GP, Stewart MK, Cottoms N, & Olson M (2011). The Care Span: Medicaid savings resulted when community health workers matched those with needs to home and community care. Health Affairs, 30(7), 1366–1374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holtrop JS, Dosh SA, Torres T, & Thum YM (2008). The community health educator referral liaison (CHERL): a primary care practice role for promoting healthy behaviors. American Journal of Preventive Medicine, 35(5 Suppl), S365–372. [DOI] [PubMed] [Google Scholar]
- Ingram M, Gallegos G, & Elenes J (2005). Diabetes is a community issue: the critical elements of a successful outreach and education model on the U.S.-Mexico border. Preventing Chronic Disease, 2(1), A15. [PMC free article] [PubMed] [Google Scholar]
- Ingram M, Reinschmidt KM, Schachter KA, Davidson CL, Sabo SJ, De Zapien JG, & Carvajal SC (2012). Establishing a professional profile of community health workers: results from a national study of roles, activities and training. Journal of Community Health, 37(2), 529–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram M, Schachter KA, Sabo SJ, Reinschmidt KM, Gomez S, De Zapien JG, & Carvajal SC (2014). A community health worker intervention to address the social determinants of health through policy change. The Journal of Primary Prevention, 35(2), 119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ingram M, Torres E, Redondo F, Bradford G, Wang C, & O’Toole ML (2007). The impact of promotoras on social support and glycemic control among members of a farmworker community on the US-Mexico border. Diabetes Educator, 33 Suppl 6, 172s–178s. [DOI] [PubMed] [Google Scholar]
- Institute for Public Health Innovation. (2017). Using a Community Health Worker Model to Improve HIV Medical Care Systems. Retrieved from http://www.institutephi.org/our-work-in-action/community-health-worker-initiatives/hiv-aids-early-interventions-retention-care/
- Islam N, Nadkarni S, Peretz P, Matiz L, Hirsch G, Kane E, … Trinh-Shevrin C (2016). Integration of Community Health Workers into Primary Care Health Systems: The Time for New York is Now! NYU-CUNY Prevention Research Center. NY, NY. [Google Scholar]
- Jara EA, Ritterman Weintraub M, Clifton-Hawkins N, & Martinez N (2014). Effects of a promotor training on local school wellness advocacy capacity. Health Promotion Practice, 15(1), 63–71. [DOI] [PubMed] [Google Scholar]
- Johnson P, Thorman Hartig M, Frazier R, Clayton M, Oliver G, Nelson BW, & Williams-Cleaves BJ (2014). Engaging faith-based resources to initiate and support diabetes self-management among African Americans: a collaboration of informal and formal systems of care. Health Promotion Practice, 15(2 Suppl), 71s–82s. [DOI] [PubMed] [Google Scholar]
- Lavin JH, Avery A, Whitehead SM, Rees E, Parsons J, Bagnall T, … Ruxton CH (2006). Feasibility and benefits of implementing a slimming on Referral service in primary care using a commercial weight management partner. Public Health, 120(9), 872–881. [DOI] [PubMed] [Google Scholar]
- Lemak CH, Johnson C, & Goodrick EE (2004). Collaboration to improve services for the uninsured: Exploring the concept of health navigators as interorganizational integrators. Health Care Management Review, 29(3), 196–206. [DOI] [PubMed] [Google Scholar]
- Martin-Misener R, Valaitis R, Wong ST, MacDonald M, Meagher-Stewart D, Kaczorowski J, … Austin P (2012). A scoping literature review of collaboration between primary care and public health. Primary Health Care Research & Development, 13(04), 327–346. [DOI] [PubMed] [Google Scholar]
- McQuigg M, Brown J, Broom J, Laws RA, Reckless JP, Noble PA, … Hole DJ (2005). Empowering primary care to tackle the obesity epidemic: the Counterweight Programme. European Journal of Clinical Nutrition, 59 Suppl 1, S93–100; discussion S101. [DOI] [PubMed] [Google Scholar]
- O’Brien MJ, Squires AP, Bixby RA, & Larson SC (2009). Role development of community health workers: an examination of selection and training processes in the intervention literature. American Journal of Preventive Medicine, 37(6 Suppl 1), S262–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Disease Prevention and Health Promotion. (2014). Social Determinants of Health. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health [Google Scholar]
- Peretz PJ, Matiz LA, Findley S, Lizardo M, Evans D, & McCord M (2012). Community health workers as drivers of a successful community-based disease management initiative. American Journal of Public Health, 102(8), 1443–1446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters M, Godfrey C, McInerney P, Soares C, Hanan K, & Parker D (2015). The Joanna Briggs Institute Reviewers’ Manual 2015: Methodology for JBI Scoping Reviews.
- Porterfield DS, Hinnant LW, Kane H, Horne J, McAleer K, & Roussel A (2012). Linkages between clinical practices and community organizations for prevention: a literature review and environmental scan. American Journal of Preventive Medicine, 42(6 Suppl 2), S163–171. [DOI] [PubMed] [Google Scholar]
- Quigley L, Matsuoka K, Montgomery KL, Khanna N, & Nolan T (2014). Workforce development in Maryland to promote clinical-community connections that advance payment and delivery reform. Journal of Health Care for the Poor and Underserved, 25(1 Suppl), 19–29. [DOI] [PubMed] [Google Scholar]
- Redding S, Conrey E, Porter K, Paulson J, Hughes K, & Redding M (2015). Pathways community care coordination in low birth weight prevention. Matern and Child Health Journal, 19(3), 643–650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal EL, Rush C, Allen C. (2016). Progress Report of the Community Health Worker (CHW) Core Consensus (C3) Project: Building National Consensus on CHW Core Roles, Skills, and Qualities. Retrieved from http://www.chwcentral.org/sites/default/files/CHW%20C3%20Project.pdf
- Rosenthal EL, Wiggins N, Ingram M, Mayfield-Johnson S, & De Zapien G (2011). Community health workers then and now. Journal of Ambulatory Care Management, 34(3), 247–259. [DOI] [PubMed] [Google Scholar]
- Rush CH (2012). Return on investment from employment of community health workers. Journal of Ambulatory Care Management, 35(2), 133–137. [DOI] [PubMed] [Google Scholar]
- SAMHSA report: Behavioral Health Homes for People with Mental Health and Substance Use Conditions: The Core Clinical Features. SAMHSA – HRSA Center For Integrated Health Solutions, May 2012, p 27. [Google Scholar]
- Schroeder SA (2007). We Can Do Better — Improving the Health of the American People. New England Journal of Medicine, 357(12), 1221–1228. [DOI] [PubMed] [Google Scholar]
- Wennerstrom A, Bui T, Harden-Barrios J, & Price-Haywood EG (2015). Integrating community health workers into a patient-centered medical home to support disease self-management among Vietnamese Americans: lessons learned. Health Promotion Practice, 16(1), 72–83. [DOI] [PubMed] [Google Scholar]
- Women-Inspired Neighborhood (WIN) Network. (2017). Impacting Wellness through Community Health Workers. Retrieved from http://www.winnetworkdetroit.org/about-us/funding-agency/press-coverage/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.