Abstract
Bavachinin (BNN), one of the main active ingredients of Psoraleacorylifolia, can activate peroxisome proliferator-activated receptor γ (PPARγ). PPARγ has become a promising therapeutic target in cancer. The aim of the present study was to explore the antitumor effects of BNN in non-small cell lung cancer (NSCLC). Cell Counting Kit-8 and lactate dehydrogenase release assays were performed to measure cell toxicity. Western blotting and immunofluorescence were used to analyze the expression of apoptosis-related factors and PPARγ. The ability of PPARγ to bind to BNN was evaluated by drug affinity responsive target stability (DARTS) and cellular thermal shift assay (CETSA). A reactive oxygen species (ROS) assay kit was used to detect the ROS level. The results revealed that the survival rates and cell viability of A549 cells were reduced by BNN in a dose-dependent manner. The present results also demonstrated that BNN dose-dependently changed the expression of Bcl-2, Bax, caspases-3/9 and PPARγ. In addition, through the cytotoxic and anti-proliferative effects, the apoptosis-related proteins' inhibitive properties of BNN were completely inhibited by the PPARγ antagonists T0070907 and GW9662. The DARTS and CETSA results confirmed the protein binding activity of PPARγ. Furthermore, it was demonstrated that the BNN-induced ROS generation was dependent on PPARγ activation. Taken together, the present study demonstrated that BNN induced the death of A549 cells by activating PPARγ, an effect mediated by the increased ROS level. These results highlighted the potential role of BNN as a chemotherapeutic agent against NSCLC.
Keywords: bavachinin, A549 cells, lung cancer, peroxisome proliferator-activated receptor-γ, reactive oxygen species
Introduction
Lung cancer is a common malignant tumor worldwide. There are 3 main types of lung cancer; ~85% of lung cancer cases are non-small cell lung cancer (NSCLC) (1). The 5-year survival rate of patients with some types of cancer has markedly improved during the last two decades, however, that of patients with lung cancer remains low (2). It has been reported that >50% of patients with lung cancer are already at an advanced stage upon initial diagnosis (3). In addition, progress in the treatment of lung cancer is slow. Therefore, new approaches and drugs to prevent and treat lung cancer are urgently required in order to improve clinical outcomes.
Peroxisome proliferator-activated receptor γ (PPARγ) belongs to the nuclear hormone receptor superfamily and translocates to the nucleus when ligands bind to it (4). PPARγ participates in multiple physical and pathological processes, including inflammation, adipocyte differentiation, and lipid and glucose metabolism (5). A recent study has confirmed that PPARγ also plays an important role in inhibiting proliferation and development in lung cancer (6). Therefore, PPARγ agonists have become a potential therapeutic drug candidate for the treatment of lung cancer.
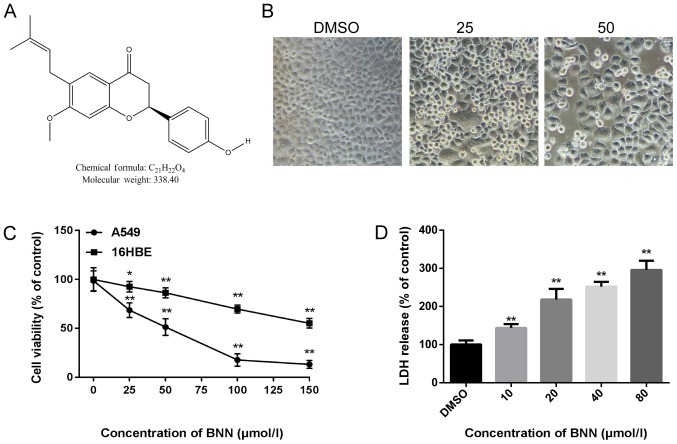
Natural traditional Chinese medicine products are becoming popular in the search for antitumor drugs, both in China and the rest of the world. Bavachinin (BNN; Fig. 1A) is a naturally occurring compound of Psoraleacorylifolia, which is widely used for the treatment of various conditions, including eczema, psoriasis, diabetes and cancer (7). Several recent studies have indicated that BNN has PPARγ-activating properties and is a PPARγ agonist (8,9). The aim of the present study was to explore the antitumor effect of BNN in NSCLC A549 cells, as well as the biomechanism involved.
Figure 1.
Cytotoxic effect of BNN on A549 cells. (A) The chemical structure of BNN (structural formula, C21H22O4; molecular weight, 338.40). (B) A549 cell morphology was observed following BNN treatment for 24 h. (C) Cell viability was measured by Cell Counting Kit-8 assay. (D) Cell death was measured by LDH cytotoxicity assay. Data are presented as the mean ± standard deviation (n=3) obtained from 3 independent experiments (n=6). *P<0.05 and **P<0.01 vs. 0 µmol/l BNN. Magnification, ×400. BNN, bavachinin; LDH, lactate dehydrogenase.
Materials and methods
A549 cell culture
The human NSCLC A549 and human bronchial epithelial 16HBE cell lines were obtained from the Cell Bank of Type Culture Collection of the Chinese Academy of Sciences and cultured in DMEM (Gibco; Thermo Fisher Scientific, Inc.) supplemented with 10% fetal bovine serum (Gibco; Thermo Fisher Scientific, Inc.) and 1% penicillin-streptomycin in 5% CO2 at 37°C. BNN was obtained from Chengdu Herbpurify Co., Ltd. DMSO was purchased from Beijing Solarbio Science & Technology Co., Ltd. The PPARγ antagonists GW9662 and T0070907 were obtained from Beyotime Institute of Biotechnology.
Cell Counting Kit-8 (CCK-8) assay
Both A549 and 16HBE cells were seeded on 96-well culture plates (2×103 cells/well) and the cell culture medium was removed 24 h later. Medium containing different concentrations of BNN (0, 25, 50, 100 and 150 µmol/l) was added to the cells. Following treatment for 24 h at 37°C, 10 µl CCK-8 solution was added to each well and incubated for 1 h at 37°C with 5% CO2. The absorbance value at 450 nm was then measured using a SpectraMax iD3 microplate reader (Molecular Devices, LLC). The IC50 was calculated by comparing the cell viability with the BNN concentration.
Lactate dehydrogenase (LDH) release assay
A549 cells were seeded on 96-well culture plates (2×103 cells/well) and treated with different concentrations of BNN (10, 20, 40 or 80 µM) or in the presence of PPARγ antagonists GW9662 (20 µM) and T0070907 (10 µM) for 24 h. Cell culture medium (100 µl) was collected for LDH determination using an LDH cytotoxicity assay kit according to the manufacturer's instructions (Beyotime Institute of Biotechnology). Foll owing the reaction, the absorbance was read at a wavelength of 490 nm using the SpectraMax iD3 microplate reader.
Measurement of intracellular reactive oxygen species (ROS)
An ROS assay kit (Beyotime Institute of Biotechnology) was used to measure intracellular ROS accumulation. A549 cells were seeded on 6-well culture plates (8×103 cells/well) and treated with different concentrations of BNN (10, 20, 40 µM), with or without PPARγ antagonists GW9662 (20 µM) and T0070907 (10 µM). The cells were incubated with 10 µM DCFH-DA for 20 min at 37°C, and images were captured using a fluorescence microscope (Olympus Corporation). Cells were then collected and measured using a SpectraMax iD3 microplate reader at an excitation wavelength of 488 nm and an emission wavelength of 525 nm.
Immunofluorescence
Cells seeded in 48-well plates (3×103 cells/well)were fixed with 4% paraformaldehyde at room temperature for 15 min and permeabilized with 0.3% Triton X-100 (Beyotime Institute of Biotechnology) at room temperature for 30 min. The cells were then blocked at 37°C for 1 h with Immunol Staining Blocking Buffer (Beyotime Institute of Biotechnology), followed by incubation with an anti-PPARγ antibody (16643-1-AP, 1:200; ProteinTech Group, Inc.) at room temperature for 1 h. Next, cells were incubated with an Alexa-488-conjugated secondary antibody (SA00013-2, 1:500; ProteinTech Group, Inc.) at 37°C for 50 min. Nuclei were stained with DAPI (Beyotime Institute of Biotechnology). PPARγ was stained green and the nuclei were stained blue. Fluorescent imaging was performed using a laser scanning confocal microscope (Olympus Corporation).
Western blotting
Cells were lysed with RIPA buffer containing 1% protease inhibitor and centrifuged at 14,000 × g for 20 min at 4°C. The supernatants were collected and the protein concentrations were measured by bicinchoninic acid assay kit (Beyotime Institute of Biotechnology). The extraction of nuclear and cytoplasmic protein was performed according to the manufacturer's instructions using nuclear and cytoplasmic protein extraction kit (Beyotime Institute of Biotechnology). Protein (20 µg) was applied to 10% SDS-PAGE, and then transferred on to 0.45 µm PVDF membranes. The membranes were incubated in blocking solution (5% non-fat milk) for 1 h at room temperature and then incubated with the following primary antibodies: Bax (50599-2-Ig; 1:2,000; Proteintech Group, Inc.), Bcl-2 (12789-1-AP; 1:1,000, Proteintech Group, Inc.), PPARγ (16643-1-AP; 1:2,000; ProteinTech Group, Inc), Caspase-3 (AC030; 1:2,000; Beyotime Institute of Biotechnology), Caspase-9 (10380-1-AP; 1:2,000; ProteinTech Group, Inc), GAPDH (60004-1-Ig; 1:3,000; Proteintech Group, Inc.) and Histone-H3 (17168-1-AP; 1:2,000; ProteinTech Group, Inc) overnight at 4°C. Then the membranes were incubated with the horseradish peroxidase-conjugated goat anti-rabbit IgG (A0208; 1:2,000; Beyotime Institute of Biotechnology) for 1 h at room temperature. Western blotting bands were visualized by enhanced chemiluminescent reagent (Beyotime Institute of Biotechnology) and quantified using ImageJ software (version 1.51j8; National Institutes of Health) and standardized against GAPDH or Histone-H3 (nuclear protein quantification).
Drug affinity responsive target stability (DARTS)
DARTS was performed as described in our previous study (10). Cells were lysed with M-PER lysis buffer (Thermo Fisher Scientific, Inc.) supplemented with 1% phosphatase and protease inhibitors and centrifuged at 16,000 × g for 20 min at 4°C. Next, 10X TNC buffer (50 mM Tris·Cl, 50 mM NaCl, 10 mM CaCl2) was added to the supernatant at room temperature for 10 min. The lysates were incubated with DMSO or BNN (1, 10 or 100 µM) at room temperature for 1 h, followed by incubation with 0.03 mg/ml pronase (Roche Diagnostics GmbH) at room temperature for 30 min. The proteolysis was stopped using SDS loading buffer. All samples were analyzed by western blotting.
Cellular thermal shift assay (CETSA)
Cells treated with BNN (10 µM) or DMSO at 37°C for 24 h were collected, and the cell suspension was distributed into 0.2 ml PCR tubes, with 200 µl cell suspension in each tube. The PCR tubes were heated at the designated temperature (42, 45, 48, 51 and 54°C) for 3 min. They were then removed and incubated at 4°C immediately following heating. Cells were then lysed using cell lysis buffer for western (Beyotime Institute of Biotechnology) and analyzed by western blotting as described in the western blotting methods above.
Statistical analysis
Statistical analysis of the data was performed using GraphPad Prism v.6.0 (GraphPad Software, Inc.). Data are presented as the mean ± standard deviation. Significance was determined by one-way ANOVA, and Tukey's post hoc test for multiple comparisons. P<0.05 was considered to indicate a statistically significant difference.
Results
BNN inhibits cell viability in human A549 cells
In order to detect the toxicity of BNN, A549 cell morphology following BNN exposure was first examined. When human A549 cells were treated with BNN for 24 h, the cell number decreased while the cell size increased. When the BNN concentration was increased to 25 µM, the cell density was decreased. When the BNN concentration was increased to 50 µM, the cell density was markedly decreased, and a great number of dead cells were suspended in the culture medium (Fig. 1B). Next, a CCK-8 assay was performed to detect the cell viability using the A549 and 16HBE cell lines following treatment with different concentration of BNN (0, 25, 50, 100 or 150 µmol/l) for 24 h. As shown in Fig. 1C, the proliferation of A549 cells was significantly suppressed by BNN in a dose-dependent manner; BNN exerted less toxicity on 16HBE than on A549 cells. To further evaluate the toxicity of BNN, the LDH release from A549 cells treated with BNN was measured in order to determine whether necrosis was involved in the BNN-induced decrease in cell viability. LDH release is a typical property of cell necrosis (11). As shown in Fig. 1D, BNN dose-dependently increased the release of LDH, which reflected the levels of necrotic cell death. In addition, BNN increased the expression of apoptosis-related factors caspase (CAS)-3, CAS9 and Bax, but decreased the expression of Bcl-2 (Fig. 2A). These proteins act as pro- or anti-apoptotic regulators in cellular activities (12).
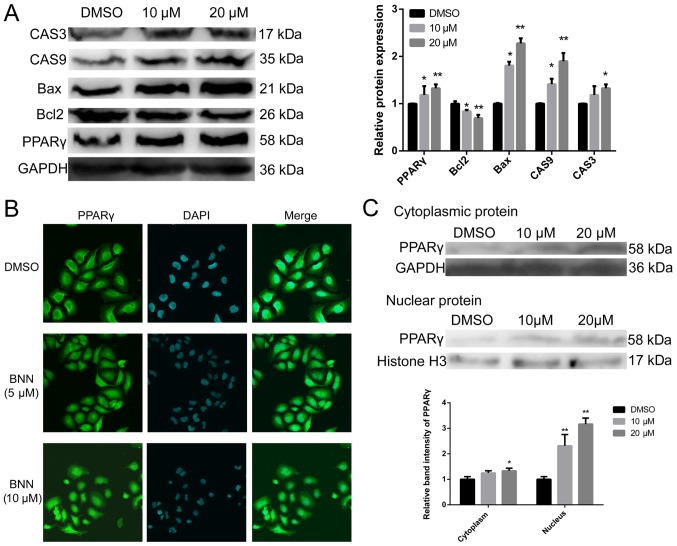
Figure 2.
Effects of BNN on PPARγ expression (24 h). (A) BNN promoted CAS3, CAS9, Bax and PPARγ protein expression, but decreased Bcl-2 expression in A549 cells. (B) Immunofluorescence of PPARγ was performed 24 h following treatment with BNN. Magnification, ×400. (C) Effect of BNN on PPARγ protein expression in both the cytoplasm and the nucleus. Data are presented as the mean ± standard deviation (n=3). *P<0.05 and **P<0.01 vs. DMSO. BNN, bavachinin; PPARγ, peroxisome proliferator-activated receptor γ; CAS, caspase.
BNN promotes PPARγ protein expression
During carbohydrate and lipid metabolism, BNN exhibits pan-PPAR activity (8). We therefore speculated that BNN may exert a growth inhibition effect on human A549 cells by activating PPARγ, which may serve as a promising therapeutic target in lung cancer. As shown in Fig. 2A, BNN significantly (P<0.05) increased PPARγ protein expression. PPARγ is a ligand-activated nuclear transcription factor that belongs to the nuclear hormone receptor superfamily (13). The results of the immunofluorescence experiments showed that PPARγ protein levels in both the cytoplasm and the nucleus were markedly higher following treatment with BNN (Fig. 2B). To further confirm this result, cytoplasmic and nuclear proteins were separated from cultured A549 cells following treatment with BNN. The results of western blotting were consistent with those of immunofluorescence (Fig. 2C).
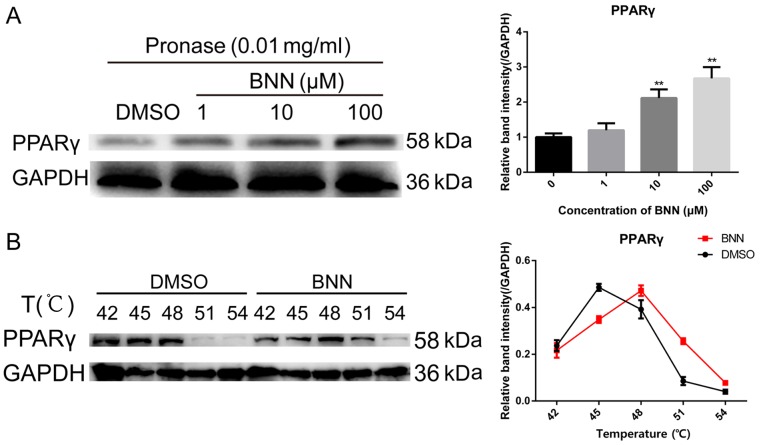
PPARγ directly binds BNN in A549 cells
Since BNN affected PPARγ expression at the protein level, BNN may directly bind to PPARγ and act as a PPARγ agonist to exert antitumor effects. To identify whether PPARγ directly binds to BNN, DARTS and CETSA were employed to validate the affinity between PPARγ and BNN. DARTS is a label-free strategy to identify the small molecule targets that are stabilized by binding to small molecules and can therefore be protected from proteolysis (14,15). Following incubation with 0.03 mg/ml pronase for 30 min at room temperature, significant (P<0.01) protection from the proteolysis of PPARγ was observed in the A549 whole cell lysate in the presence of 10 and 100 µM BNN (Fig. 3A). The physical interaction of BNN with PPARγ was further investigated by CETSA, which is based on the physical phenomenon of small molecule-induced thermal stabilization of target proteins (16). The A549 cells were incubated with 10 µM BNN for 24 h and the collected cells were heated. Compared with the DMSO-treated cell lysate, BNN markedly changed the thermal stability of PPARγ at 42, 45, 48, 51 and 54°C (Fig. 3B).
Figure 3.
BNN directly binds to PPARγ. (A) For the DARTS assay, A549 cell lysates (5 mg/ml) were incubated with BNN (1, 10 or 100 µM) or an equal volume of DMSO for 1 h at room temperature, followed by digestion with pronase (0.03 mg/ml) for 30 min. (B) For CETSA experiments, A549 cells were incubated with BNN (10 µM) or an equal volume of DMSO for 24 h, followed by heating at the indicated temperatures. Cells were lysed, and the soluble portion was analyzed by western blotting. The abundance of PPARγ normalized to GAPDH is presented. **P<0.01 vs. 0 µmol/l BNN. BNN, bavachinin; PPARγ, peroxisome proliferator-activated receptor γ; DARTS, drug affinity responsive target stability; CETSA, cellular thermal shift assay.
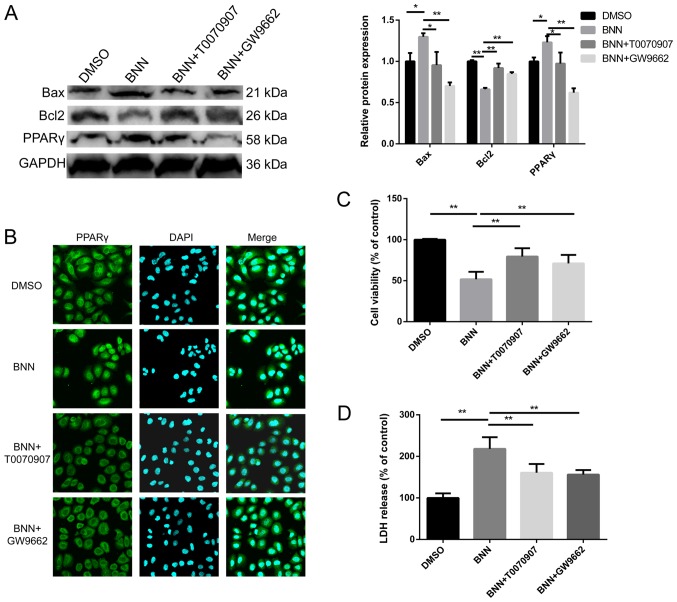
Effects of PPARγ antagonists on cell toxicity and BNN-induced PPARγ expression
To clarify whether the effect of BNN on A549 was dependent on PPARγ, cells were co-treated with BNN and PPARγ antagonists. The BNN-induced alterations in the expression of the apoptosis-related factors Bcl-2 and Bax were inhibited by the PPARγ antagonists T0070907 and GW9662 (Fig. 4A). The upregulation of PPARγ and the BNN-induced translocation of PPARγ to the nucleus were also restrained by T0070907 and GW9662 (Fig. 4A and B). Additionally, the present study investigated the impact of T0070907 and GW9662 alone on A549, which had no significant effect on A549 cell viability. In order to measure the effect of PPARγ antagonists on cell toxicity, CCK-8 and LDH release assays were performed. The cell viability of cells co-treated with PPARγ antagonists and BNN was higher than that observed in the BNN only group, while LDH release was decresed, when compared with the BNN only group (Fig. 4C and D).
Figure 4.
PPARγ antagonist co-treatments. (A) T0070907 and GW9662 treatment attenuated the BNN-induced effects on Bax, Bcl-2 and PPARγ expression in A549 cells. (B) The BNN-induced nucleocytoplasmic shuttling of PPARγ was suppressed by T0070907 and GW9662. Magnification, ×400. PPARγ inhibitors attenuated BNN-induced cell death in A549 cells, as shown by the (C) Cell Counting Kit-8 and (D) LDH release assay results. *P<0.05 and **P<0.01, as indicated. BNN, bavachinin; PPARγ, peroxisome proliferator-activated receptor γ; LDH, lactate dehydrogenase.
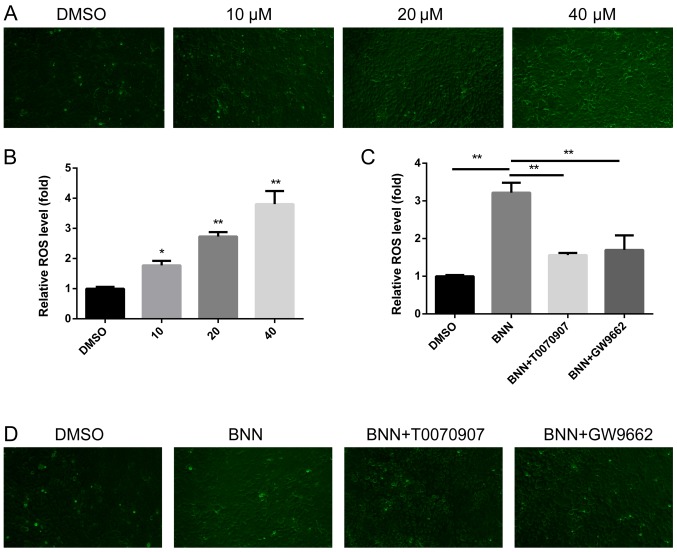
BNN induces ROS generation in a PPARγ-dependent manner
ROS exerts a complex role in tumor survival and proliferation; excessive ROS leads to DNA damage, which results in cell necrosis and apoptosis (17). The present study therefore investigated whether ROS participated in the BNN-induced anti-cancer effect. ROS was detected using a fluorescenct microscope, and the fluorescence intensity was then measured using a microplate reader. BNN promoted ROS generation in a dose-dependent manner (Fig. 5A and B). In order to clarify whether the generation of ROS was dependent on PPARγ, PPARγ antagonists were applied for co-treatments with BNN. The upregulation of ROS induced by BNN could be inhibited by PPARγ antagonists (Fig. 5C and D). These results indicated that the generation of ROS in A549 cells was dependent on the expression of PPARγ.
Figure 5.
Effect of BNN on intracellular ROS accumulation. (A and B) BNN induced ROS production in a dose-dependent manner following treatment with 10, 20 and 40 µM BNN for 24 h. *P<0.05 and **P<0.01 vs. DMSO. (C and D) BNN-induced ROS accumulation was inhibited by the PPARγ antagonists T0070907 and GW9662. Magnification, ×200. **P<0.01, as indicated. BNN, bavachinin; ROS, reactive oxygen species; PPARγ, peroxisome proliferator-activated receptor γ.
Discussion
Psoralea corylifolia is a popular multipurpose medicinal plant that has been used to treat nephritis, osteoporosis, hypertension, cardiovascular diseases and various types of cancer (18). As one of the main active ingredients of Psoralea corylifolia, BNN is a novel natural PPARγ agonist. PPARγ is a nuclear transcription factor and changes the expression of a series of genes upon its activation. A previous study has indicated that PPARγ activation plays a critical role in lung cancer development and progression by modulating cell differentiation, proliferation, apoptosis and motility (19). Therefore, PPARγ may act as a promising therapeutic target in lung cancer, either as a monotherapy or synergistic therapy.
The present study first confirmed the effect of BNN on lung cancer A549 cell proliferation. The CCK-8 and LDH release assays revealed that BNN caused a marked toxic effect on A549 cells. In order to examine cell activity, the protein expression of apoptosis-related factors, Bax, Bcl-2, CAS3 and CAS9, was also detected; the results indicated that BNN also promoted the apoptosis of A549 cells. These results confirmed that BNN can act as a therapeutic target for lung cancer. To explore the mechanism of BNN cytotoxicity in lung cancer cells, PPARγ protein expression was measured. BNN not only upregulated the expression of PPARγ at the protein level, but also promoted the nuclear translocation of PPARγ, which was confirmed by the separation of cytoplasmic and nuclear proteins. These results indicated that BNN could activate PPARγ, but the affinity between BNN and PPARγ remains unclear. The DARTS and CETSA results confirmed that BNN could directly bind to PPARγ.
To further explore the mechanism through which BNN regulates A549 cell proliferation, the ROS level was also measured. The results showed that BNN promoted the generation of ROS in a dose-dependent manner. ROS is generated via the reduction of molecular oxygen mainly formed in the mitochondrial respiratory chain (20). In normal cells, there is a balance between ROS and intracellular biochemical antioxidants. However, excessive ROS causes oxidative damage to intracellular biomacromolecules (21). In cancer cells, excessive ROS production can lead to cell death, including necrotic cell death, apoptosis, autophagy and ferroptosis (17). A previous study has confirmed that PPARγ activation has a direct impact on ROS levels (22). The present results also showed that BNN promoted the production of ROS in a PPARγ-dependent manner.
In conclusion, the present study demonstrated that BNN induced A549 cell death by promoting PPARγ protein expression and nuclear translocation. Furthermore, the present results also suggested that BNN-induced PPARγ activation inhibited A549 cell proliferation via an ROS dependent-mechanism. The results of the present study provide a theoretical basis for the clinical application of BNN in the treatment of NSCLC.
Acknowledgements
Not applicable.
Funding
The present study was funded by The Innovation Project of Shandong Academy of Medical Sciences.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Authors' contributions
KC conceived and designed the experiments, and wrote the manuscript. LNG performed experiments. LY and CL performed the statistical analysis and figure editing. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Parums DV. Current status of targeted therapy in non-small cell lung cancer. Drugs Today (Barc) 2014;50:503–525. doi: 10.1358/dot.2014.50.07.2185913. [DOI] [PubMed] [Google Scholar]
- 2.Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin. 2017;67:7–30. doi: 10.3322/caac.21387. [DOI] [PubMed] [Google Scholar]
- 3.Blandin Knight S, Crosbie PA, Balata H, Chudziak J, Hussell T, Dive C. Progress and prospects of early detection in lung cancer. Open Biol. 2017;7(pii):170070. doi: 10.1098/rsob.170070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kahremany S, Livne A, Gruzman A, Senderowitz H, Sasson S. Activation of PPARdelta: From computer modelling to biological effects. Br J Pharmacol. 2015;172:754–770. doi: 10.1111/bph.12950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marion-Letellier R, Savoye G, Ghosh S. Fatty acids, eicosanoids and PPAR gamma. Eur J Pharmacol. 2016;785:44–49. doi: 10.1016/j.ejphar.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 6.Reddy AT, Lakshmi SP, Reddy RC. PPARgamma as a novel therapeutic target in lung cancer. PPAR Res. 2016;2016:8972570. doi: 10.1155/2016/8972570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lin CH, Funayama S, Peng SF, Kuo CL, Chung JG. The ethanol extraction of prepared Psoralea corylifolia induces apoptosis and autophagy and alteres genes expression assayed by cDNA microarray in human prostate cancer PC-3 cells. Environ Toxicol. 2018;33:770–788. doi: 10.1002/tox.22564. [DOI] [PubMed] [Google Scholar]
- 8.Feng L, Luo H, Xu Z, Yang Z, Du G, Zhang Y, Yu L, Hu K, Zhu W, Tong Q, et al. Bavachinin, as a novel natural pan-PPAR agonist, exhibits unique synergistic effects with synthetic PPAR-γ and PPAR-α agonists on carbohydrate and lipid metabolism in db/db and diet-induced obese mice. Diabetologia. 2016;59:1276–1286. doi: 10.1007/s00125-016-3912-9. [DOI] [PubMed] [Google Scholar]
- 9.Du G, Zhao Y, Feng L, Yang Z, Shi J, Huang C, Li B, Guo F, Zhu W, Li Y. Design, Synthesis, and Structure-activity relationships of bavachinin analogues as peroxisome proliferator-activated Receptor γ agonists. ChemMedChem. 2017;12:183–193. doi: 10.1002/cmdc.201600554. [DOI] [PubMed] [Google Scholar]
- 10.Ge L, Cui Y, Cheng K, Han J. Isopsoralen enhanced osteogenesis by targeting AhR/ERα. Molecules. 2018;23(pii):E2600. doi: 10.3390/molecules23102600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chan FK, Moriwaki K, De Rosa MJ. Detection of necrosis by release of lactate dehydrogenase activity. Methods Mol Biol. 2013;979:65–70. doi: 10.1007/978-1-62703-290-2_7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marimuthu P, Singaravelu K. Deciphering the crucial residues involved in heterodimerization of Bak peptide and anti-apoptotic proteins for apoptosis. J Biomol Struct Dyn. 2018;36:1637–1648. doi: 10.1080/07391102.2017.1331863. [DOI] [PubMed] [Google Scholar]
- 13.Guo L, Tabrizchi R. Peroxisome proliferator-activated receptor gamma as a drug target in the pathogenesis of insulin resistance. Pharmacol Ther. 2006;111:145–173. doi: 10.1016/j.pharmthera.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Pai MY, Lomenick B, Hwang H, Schiestl R, McBride W, Loo JA, Huang J. Drug affinity responsive target stability (DARTS) for small-molecule target identification. Methods Mol Biol. 2015;1263:287–298. doi: 10.1007/978-1-4939-2269-7_22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lomenick B, Jung G, Wohlschlegel JA, Huang J. Target identification using drug affinity responsive target stability (DARTS) Curr Protoc Chem Biol. 2011;3:163–180. doi: 10.1002/9780470559277.ch110180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jensen AJ, Martinez Molina D, Lundbäck T. CETSA: A target engagement assay with potential to transform drug discovery. Future Med Chem. 2015;7:975–978. doi: 10.4155/fmc.15.50. [DOI] [PubMed] [Google Scholar]
- 17.Zou Z, Chang H, Li H, Wang S. Induction of reactive oxygen species: An emerging approach for cancer therapy. Apoptosis. 2017;22:1321–1335. doi: 10.1007/s10495-017-1424-9. [DOI] [PubMed] [Google Scholar]
- 18.Alam F, Khan GN, Asad M. Psoralea corylifolia L: Ethnobotanical, biological, and chemical aspects: A review. Phytother Res. 2018;32:597–615. doi: 10.1002/ptr.6006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Han EJ, Im CN, Park SH, Moon EY, Hong SH. Combined treatment with peroxisome proliferator-activated receptor (PPAR) gamma ligands and gamma radiation induces apoptosis by PPARγ-independent up-regulation of reactive oxygen species-induced deoxyribonucleic acid damage signals in non-small cell lung cancer cells. Int J Radiat Oncol Biol Phys. 2013;85:e239–e248. doi: 10.1016/j.ijrobp.2012.11.040. [DOI] [PubMed] [Google Scholar]
- 20.Sarniak A, Lipińska J, Tytman K, Lipińska S. Endogenous mechanisms of reactive oxygen species (ROS) generation. Postepy Hig Med Dosw (Online) 2016;70:1150–1165. doi: 10.5604/17322693.1224259. [DOI] [PubMed] [Google Scholar]
- 21.Juránek I, Bezek S. Controversy of free radical hypothesis: Reactive oxygen species-cause or consequence of tissue injury? Gen Physiol Biophys. 2005;24:263–278. [PubMed] [Google Scholar]
- 22.Srivastava N, Kollipara RK, Singh DK, Sudderth J, Hu Z, Nguyen H, Wang S, Humphries CG, Carstens R, Huffman KE, et al. Inhibition of cancer cell proliferation by PPARgamma is mediated by a metabolic switch that increases reactive oxygen species levels. Cell Metab. 2014;20:650–661. doi: 10.1016/j.cmet.2014.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.