Abstract
Background:
Diabetes mellitus (DM) is a metabolic disease that is characterized by distortion in the metabolism of carbohydrates, lipids, and proteins and involves hyperglycemia. DM has different types. Several complications are associated with diabetes including diabetic retinopathy (DR). DR can further results in bad outcomes that can be avoided by early diagnosis and management.
Aim:
The aim of this paper is to assess the awareness and knowledge level about DR among type 2 DM patients in primary health care in security forces hospital.
Methods:
This is a cross-sectional study that was conducted on Saudi patients with type 2 DM who visited primary health care in security forces hospital.
Results:
This study included 174 participants, with equal male to female ratio was 1:1, there were 64.9% participants who reported controlled blood glucose level, and 47.1% reported that eye was affected by diabetes. There were 82.8% participants who had awareness about DR; the level of awareness differs significantly with sex (P value = 0.04) and the level of DM control (P value = 0.02).
Conclusion:
There was high level of knowledge regarding DR; however, there were few percent of participants who had no awareness and still at risk.
Keywords: Diabetic complications, diabetes mellitus, diabetic retinopathy, diabetic retinopathy awareness, T2DM
Introduction
Diabetes mellitus (DM) is a metabolic disease that is characterized by a defect in insulin action or secretion leading to an increase in the glucose level in blood which is known as hyperglycemia.[1] DM is of three main types: type 1 (T1DM), type 2, (T2DM) and gestational diabetes.[1] The global prevalence of DM was reported to be as low as 8% in 2011; however, it is expected to increase to 10% by 2030.[2] KSA and other Middle Eastern countries have a high prevalence of DM.[3] KSA was in the second rank having the highest prevalence of DM among the Middle East and the 7th rank among the world according to a WHO report. In KSA, the prevalence of DM reached an epidemic proportion,[4,5] according to the Saudi Ministry of Health, there were 0.9 million individuals who were diagnosed with diabetes in 1992, this number increased by 2.7 times to 2.5 million in 2010.[6] DM can result in several complications such as diabetic retinopathy (DR) which is considered the most common microvascular complication of DM,[7] neuropathy, neurologic, and cardiovascular complications.[8] DR is a retinal disease that involves the compromising of the oxygen and nutrients delivery to the retina.[9] DR may lead to vision impairment and loss.[8,10,11] DR develops among 34.6% of diabetic patients.[12] Among DM patients, there are several risk factors for DR have been reported including long duration of DM, uncontrolled DM, older age, presence of additive systematic diseases such as hypertension, dyslipidemia, and obesity.[13,14,15] The prevalence of DR varies among various regions in the world.[16] Awareness about DR among DM patients is an important factor for early diagnosis and the treatment of the disease to avoid further complications such as visual impairment.[17] Several studies reported low to average screening pattern where 31–53% of patients performed an annual eye examination.[18,19,20,21,22] The present study was conducted to assess the awareness, compliance, and barriers of DR among T2DM patients in Saudi Arabia.
Review of literature
The prevalence of T2DM in Saudi Arabia is high and it is increasing; one cross-sectional study in 2009 from KSA in Jeddah to assess the prevalence of diabetes in Saudi community showed that the prevalence rate was 30%,[23] and in 2011 another cross-sectional study reported that the prevalence was 31.6% among 9149 individuals.[24] Saudi Arabia had the highest prevalence of DM in 2015 among the Middle East and North Africa region as the prevalence was 17.6%.[25] It was reported in a global review that 34.6% of all diabetic patients have some forms of DR.[26] The prevalence of DR was reported to be 28.5%, 30.3%, 32.2%, 39.6%, and 39.3% in USA, UK, Australia, Japan, and Malaysia, respectively.[16] The prevalence of DR in KSA was found to be 31.3% in the capital Riyadh; the prevalence was estimated in other Saudi regions including AlTaif, Al-Hasa which was found 33% in the both region, but the highest prevalence was found in Al-Madinah 36%.[25,26,27,28,29] A study from Saudi Arabia reported that 36.4% of T2DM patients suffered DR.[30] The level of awareness about DR varies among different countries and different regions; a study from Australia[31] reported there were 37% only of DM patients who knew about ocular complications of DM. A lower level of awareness was reported from India (27%),[32] and the highest level of awareness was reported from the USA, where 65% of DM patients were aware of DR.[9] A study from Jordan demonstrated that there was a high level of awareness among diabetic patients regarding DR.[16] A study from KSA among physicians in Riyadh showed that the mean score of their awareness regarding DR was 57 out of 100.[33] A study from AlJouf and Hail province, KSA reported that 75.62% of diabetic patients were aware that diabetes can result in eye diseases.[34] A study from Taif, KSA showed that two-thirds of screened T2DM patients had good knowledge about DR.[35] A study from Jeddah, KSA demonstrated that DM patients had a good awareness about DM and its effects on eye; however, they showed the lack of awareness regarding DR.[36] Another study from Jeddah, King Abdul Aziz University found that 61% of diabetic patients had awareness about DR.[37]
Subjects and Methods
Subjects and study design
This study is cross sectional which was conducted from 1st October 2018 to 1st January 2019 in security forces hospital. The study was performed on Saudi patients with type 2 DM who visited PCC and their age ranged from 35–75 years old. The patients excluded from this study were either type 1 diabetic patients, non-Saudi, their ages less than 35 or older than 75 years, having congenital eye disease, suffering previous eye trauma, patient who known case or treat for other eye diseases like cataract or glaucoma and patient having a previously known cognitive impairment that would affect their ability to complete the survey or follow directions (e.g., mental retardation, dementia, psychosis).
Sample size and technique
Using expected awareness was reported 88% as given in the literature for calculating our sample size. Under the simple random sampling with a margin of error at 5% and the confidence level at 95%, we will need a sample of size 174.
We use the following formula:

Where n = sample size, z = z statistic for the level of confidence, p = expected prevalence, and d = allowable error. This formula assumes that “p” and “d” are decimal values. The study used a validated self-administered questionnaire. There was neither laboratory nor investigational techniques that were applied in this study. Medical records were used to be reviewed to check all participants who treated for other eye diseases like cataract or glaucoma.
Statistical analysis
SPSS program version 20 was used for statistical analysis, number and percent were used for qualitative variables, whereas mean and standard deviation were used for quantitative variables. Chi-square test was used for univariate analysis; significance was at P < 0.05.
Results
The present study included 174 individuals, the range of participants’ age was 35–75 years old with mean ± SD of 45.8 ± 11 years, and the most dominant age group was those with age range of 51–60 years 83 (47.7%). The ratio of male to female was1:1, regarding education, the most dominant group was those who had a high school education 64 (36.8%). Most of the participants 129 (74.1%) reported that they had some relatives diagnosed with DM, there were 68 (39.1%) reported having diabetes for ≥11 years and the mean ± SD of their age at diagnosis was 39.88 ± 15.6. Most of the individuals [113 (64.9%)] reported that their blood glucose was controlled, and more than half [92 (52.9%)] stated that the eye was not affected, the most common source of referral to the eye doctor was GP 96 (55.1%) [Table 1].
Table 1.
Sociodemographic characteristics
| Characteristics | n (%) |
|---|---|
| Age in years | |
| ≤40 | 21 (12.1) |
| 41-50 | 37 (21.3) |
| 51-60 | 83 (47.7) |
| ≥61 | 33 (19.0) |
| Mean±SD | 45.8±11 |
| range | 35-75 |
| Sex | |
| male | 87 (50.0) |
| female | 87 (50.0) |
| Education | |
| illiterate | 45 (25.9) |
| Elementary | 51 (29.3) |
| High School | 64 (36.8) |
| Higher education | 14 (8.0) |
| Do you have any of your relatives diagnosed with DM | |
| yes | 129 (74.1) |
| no | 45 (25.9) |
| Duration of diabetes | |
| Less than 5 | 57 (32.8) |
| 6-10 | 49 (28.2) |
| ≥11 years | 68 (39.1) |
| Age at diagnosis | |
| Mean | 39.88±15.6 |
| Median ( IQR) | 42 (36-50) |
| How is your blood glucose levels | |
| controlled | 113 (64.9) |
| uncontrolled | 61 (35.6) |
| Is eye affected | |
| yes | 82 (47.1) |
| no | 92 (52.9) |
| Source of referral to an eye doctor | |
| GP | 96 (55.1) |
| patient himself | 29 (16.7) |
| have no referral yet | 49 (28.2) |
The knowledge of participants is shown in details in Table 2. There were 114 (82.8%) participants who were aware that DM can affect the retina of the eye, 127 (73%) were aware that DR can lead to blindness, and 135 (77.6%) thought that blood sugar control may reduce the risk of DR. There were 144 (82.8%) participants eho thought that routine eye check-up is necessary during DM and less than half of participants 81 (46.6%) reported that check-up should be performed every 6 months. More than half of the individuals 98 (56.3%) stated that laser treatment for DR does not improve the vision, and more than half of participants 90 (51.7%) reported that the main source of knowledge about DM and DR was physicians.
Table 2.
Knowledge of participants
| Knowledge questions | n (%) |
|---|---|
| Are you aware that DM can affect the retina of the eye | |
| yes | 144 (82.8) |
| no | 30 (17.2) |
| Are you aware that DR can lead to blindness | |
| yes | 127 (73.0) |
| no | 47 (27.0) |
| Do you think that blood sugar control may reduce the risk of DR | |
| yes | 135 (77.6) |
| no | 39 (22.4) |
| Do you think that routine eye checkups are necessary during DM | |
| yes | 144 (82.8) |
| no | 30 (17.2) |
| How frequently do you think you should undergo an eye check-up? | |
| 6months | 81 (46.6) |
| 1 year | 58 (33.3) |
| 2 years | 4 (2.2) |
| Don’t know | 31 (17.8) |
| Do you know that laser treatment for DR does not improve vision but reduce further deterioration in vision? | |
| yes | 98 (56.3) |
| no | 84 (43.7) |
| Main source of information about DM and DR? | |
| internet | 26 (14.9) |
| physician | 90 (51.7) |
| friends | 31 (17.8) |
| books | 9 (5.2) |
| None | 18 (10.3) |
The compliance of participants is shown in Table 3. There were 136 (78.2%) and 128 (73.6%) participants who reported that they fully adhere to DM treatment and measure their blood sugar at home, respectively. There were 45 (25.9%) participants who reported that they measure their blood sugar every day. There were 61 (35.1%) participants who reported that they never had vision examination, and 73 (42%) participants reported that the most common reason to get early retinal assessment was living in a remote area.
Table 3.
Compliance of participants
| Compliance questions | Answers | n | Percentage |
|---|---|---|---|
| Are you fully adherent to your current DM treatment? | yes | 136 | 78.2 |
| no | 38 | 21.8 | |
| Do you measure your blood sugar at home | yes | 128 | 73.6 |
| no | 46 | 26.4 | |
| How frequently do you measure your blood sugar at home? | Every month | 36 | 20.7 |
| Every week | 38 | 21.8 | |
| Everyday | 45 | 25.9 | |
| Once I feel unwell | 37 | 21.3 | |
| Never | 18 | 10.3 | |
| When you did last time had your vision exam | During the last 6 months | 58 | 33.3 |
| Last year | 55 | 31.6 | |
| never | 61 | 35.1 | |
| Whatare possible reasons that you think may prevent you to get an early retinal assessment | Lack of information about DR | 52 | 29.9 |
| Lack of time | 16 | 9.2 | |
| Cost of the test | 19 | 10.9 | |
| Fearing of discovering something bad | 14 | 8.0 | |
| Living in a remote area | 73 | 42.0 |
The overall awareness was among 144 (82.8%) participants, and only 30 (17.2%) were had unawareness [Figure 1].
Figure 1.
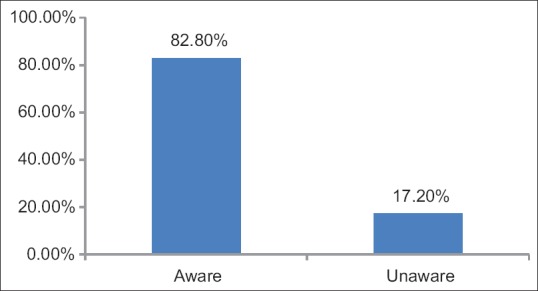
Awareness among participants
The univariate analysis showed that sex and controlling of DM have a significant effect on awareness of participants (P value = 0.045, 0.021, respectively) [Table 4]. There were two factors that affected the awareness of participants who have diabetes for less than 5 years and those who have diabetes for more than 5 years, these factors included adherence to DM treatment (P value < 0.001), measuring blood glucose at home (P value = 0.001), and the number of times measuring blood glucose (P value = 0.001) [Table 5].
Table 4.
Univariate analysis for the association between awareness of DR and selected variables
| Variables | Aware (144) n (%) | OR | P |
|---|---|---|---|
| Sex | 2.3 (1.1-5.3) | 0.045 | |
| Male | 77 (88.5%) | ||
| Female | 67 (77%) | ||
| Education | |||
| Illiterate | 37 (82.2%) | ----- | 0.689 |
| Elementary | 43 (84.3%) | ||
| High school | 54 (84.4%) | ||
| Higher education | 10 (71.4%) | ||
| Family history of DM | |||
| Yes | 103 (79.8%) | 0.39 (0.127-1.18) | 0.085 |
| NO | 41 (91.1%) | ||
| DM | |||
| Controlled | 99 (87.6%) | 5.3 (1.13-5.59) | 0.021 |
| uncontrolled | 45 (73.8%) | ||
| Duration of DM | 2.4 (1.1-5.4)* | 0.081 | |
| Less than 5 years | 42 (73.7%) | ||
| 6-10 years | 42 (85.7%) | ||
| ≥11 years | 60 (88.2%) |
Table 5.
Factors affecting awareness among those with more than and less than 5 years of diabetes
| Variables | Are you aware that DM can affect the retina of the eye n (%) | P | |
|---|---|---|---|
| Aware | Unaware | ||
| Are you fully adherent to your current DM treatment? | <0.001 | ||
| Yes | 120 (88.2%) | 16 (11.8%) | |
| No | 24 (63.2%) | 14 (36.8%) | |
| Measuring blood glucose at home | 32 (69.6%) | 14 (30.4%) | 0.001 |
| Yes | 112 (87.5%) | 16 (12.5%) | |
| No | |||
| How frequently do you measure your blood sugar at home? | 0.001 | ||
| Every day | 29 (80.6%) | 7 (19.4%) | |
| Every week | 38 (100%) | 0 (0%) | |
| Every month | 40 (88.9%) | 5 (11.1%) | |
| Once feel unwell | 26 (70.3%) | 11 (29.7%) | |
| Last measure | 0.565 | ||
| 6 months | 47 (81%) | 11 (19%) | |
| 1 year | 44 (80%) | 11 (20%) | |
| Never | 53 (86.9%) | 8 (13.1%) | |
Discussion
In the present study, there was a high level of awareness where 82.8% of the participants had awareness toward DR, only 17.2% had no awareness. Also, there were 82.8% of participants who knew that DM affects the retina of the eye, 77.6% knew that controlling blood sugar reduces the risk of DR, and 82.8% thought that a routine eye check-up is necessary during DM. The main source of information reported was GP (55.1%). Similar findings were reported in Jordanian study,[16] where 88.2% were aware that diabetes can affect the eyes, and the main source of information was GP 47.3%. A study from Hail province, Saudi Arabia, showed that 75.62% of diabetic patients were aware that eye disorders can be caused by diabetes.[34] A study from Taif, Saudi Arabia, reported that 64% of patients screened T2DM had awareness about DR.[35] A study from Jeddah reported that 82.6% of patients were aware that DM can affect the eye and 37% were aware that the main source of information was physicians.[36] Another study from Jeddah, King Abdul Aziz University hospital reported awareness of DR among 61% of the patients.[37] Studies from different countries reported different level of knowledge about the eye disease caused by diabetes; in India, USA, and Oman there were 50%, 52% and 75% patients, respectively, who had awareness.[38,39,40] The rates of awareness were higher in Myanmar and Nigeria, where the awareness rates were 86% and 84.3%, respectively.[41,42] The variation in the level of awareness between different studies and our study can be attributed to the variation in the level of education of each population, the resources of each community, the physicians advice, and information they provide. In this study, there were 64.9% patients who reported controlled blood glucose; several studies[43,44] reported poor diabetic control among T2DM patients which resulted in a high rate of complications. Similar results were reported from Jeddah, where 64% of the patients stated that their DM was controlled.[36] In our study, we investigated variables that may affect the level of awareness; it was found that sex affected awareness significantly (P value = 0.04), where more males had awareness than female (88.5% vs. 77% respectively); also, awareness differed significantly regarding controlling DM (P value = 0.02), where there were 87.6% of those who controlled DM had awareness, whereas 73.8% of uncontrolled DM patients had awareness. In contrast to our findings, it was reported that education affected the level of awareness and higher awareness was significantly associated with a higher education level.[16] In Saudi study,[35] such correlation between awareness and education was reported, where patients with lower education showed lower awareness. A study from Turkey[45] revealed that T2DM patients with diabetes duration more than 10 years tended to be more aware about DR. Similar findings were reported by Saudi study from Taif.[35] In the current study, awareness of patients differed among those with DM duration less than and more than 5 years; regarding adherence to DM, a significant higher percentage of patients who adhere to treatment had awareness toward DR (P value < 0.001). Those who measure glucose at home and perform it every week tended to have awareness than the other (P value = 0.001).
Conclusion
The level of awareness about DR among T2DM in this study was good, controlling DM was associated with a higher level of awareness; hence, physicians should assure patients to control their diabetes.
Strength points, limitations, and recommendations
The strength points of the study are that the study investigated awareness of patients in details, then the overall knowledge was assessed, the weakness point includes the small sample size of the study. It is recommended to increase the awareness of patients who had low awareness by performing educational programs. Also, follow up and continuous screening for those patients are necessary. Further studies are recommended to investigate more factors that may associate with the level of awareness.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Alanazi FK, Alotaibi JS, Paliadelis P, Alqarawi N, Alsharari A, Albagawi B. Knowledge and awareness of diabetes mellitus and its risk factors in Saudi Arabia. Saudi Med J. 2018;39:981–9. doi: 10.15537/smj.2018.10.22938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103:137–49. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 3.Khandekar R. Screening and public health strategies for diabetic retinopathy in the Eastern Mediterranean region. Middle East Afr J Ophthalmol. 2012;19:178–84. doi: 10.4103/0974-9233.95245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al Dawish MA, Robert AA, Braham R, Al Hayek AA, Al Saeed A, Ahmed RA, et al. Diabetes mellitus in Saudi Arabia: A review of the recent literature. Curr Diabetes Rev. 2016;12:359–68. doi: 10.2174/1573399811666150724095130. [DOI] [PubMed] [Google Scholar]
- 5.Elhadd TA, AlAmoudi AA, Alzahrani AS. Epidemiology, clinical and complications profile of diabetes in Saudi Arabia: A review. Ann Saudi Med. 2007;27:241–50. doi: 10.5144/0256-4947.2007.241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The Ministry of Health. Statistics report. 2015. [Last cited on 2015 Nov 05]. Available from: http://www.moh.gov.sa/en/Ministry/Statistics/book/Pages/default.aspx .
- 7.Nsiah-Kumi P, Ortmeier SR, Brown AE. Disparities in diabetic retinopathy screening and disease for racial and ethnic minority populations-A literature review. J Natl Med Assoc. 2009;101:430–7. doi: 10.1016/s0027-9684(15)30929-9. [DOI] [PubMed] [Google Scholar]
- 8.Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med. 1998;15:539–53. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 9.Tajunisah I, Wong P, Tan L, Rokiah P, Reddy S. Awareness of eye complications and prevalence of retinopathy in the first visit to eye clinic among type 2 diabetic patients. Int J Ophthalmol. 2011;4:519–24. doi: 10.3980/j.issn.2222-3959.2011.05.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Olokoba AB, Obateru OA, Olokoba LB. Type 2 diabetes mellitus: A review of current trends. Oman Med J. 2012;27:269–73. doi: 10.5001/omj.2012.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wong TY, Cheung N, Tay WT, Wang JJ, Aung T, Saw SM, et al. Prevalence and risk factors for diabetic retinopathy: The Singapore Malay eye study. Ophthalmology. 2008;115:1869–75. doi: 10.1016/j.ophtha.2008.05.014. [DOI] [PubMed] [Google Scholar]
- 12.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35:556–64. doi: 10.2337/dc11-1909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chatziralli IP, Sergentanis TN, Keryttopoulos P, Vatkalis N, Agorastos A, Papazisis L. Risk factors associated with diabetic retinopathy in patients with diabetes mellitus type 2. BMC Res Notes. 2010;3:153. doi: 10.1186/1756-0500-3-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liu L, Wu J, Yue S, Geng J, Lian J, Teng W, et al. Incidence density and risk factors of diabetic retinopathy within type 2 diabetes: A five-year cohort study in China (Report 1) Int J Environ Res Public Health. 2015;12:7899–909. doi: 10.3390/ijerph120707899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Al Ghamdi A, Rabiu M, Al Qurashi AM, Al Zaydi M, Al Ghamdi AH, Gumaa SA, et al. Knowledge, attitude and practice pattern among general health practitioners regarding diabetic retinopathy Taif, Kingdom of Saudi Arabia. Saudi J Health Sci. 2017;6:44. [Google Scholar]
- 16.Bakkar MM, Haddad MF, Gammoh YS. Awareness of diabetic retinopathy among patients with type 2 diabetes mellitus in Jordan. Diabetes Metab Syndr Obes. 2017;10:435–41. doi: 10.2147/DMSO.S140841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nathan DM. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: Overview. Diabetes Care. 2014;37:9–16. doi: 10.2337/dc13-2112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang F, Javitt JC. Eye care for elderly Americans with diabetes mellitus: Failure to meet current guidelines. Ophthalmology. 1996;103:1744–50. doi: 10.1016/s0161-6420(96)30432-6. [DOI] [PubMed] [Google Scholar]
- 19.Mukamel DB, Bresnick GH, Wang Q, Dickey CF. Barriers to compliance with screening guidelines for diabetic retinopathy. Ophthal Epidemiol. 1999;6:61–72. doi: 10.1076/opep.6.1.61.1563. [DOI] [PubMed] [Google Scholar]
- 20.Weiner JP, Parente ST, Garnick DW, Fowles J, Lawthers AG, Palmer RH. Variation in office-based quality: A claim-based profile of care provided to Medicare patients with diabetes. JAMA. 1995;273:1503–8. doi: 10.1001/jama.273.19.1503. [DOI] [PubMed] [Google Scholar]
- 21.Schoenfeld E, Greene JM, Wu SY, Leske C. Patterns of adherence to diabetes vision care guidelines: Baseline findings from the diabetic retinopathy awareness program. Ophthalmology. 2001;108:563–71. doi: 10.1016/s0161-6420(00)00600-x. [DOI] [PubMed] [Google Scholar]
- 22.Brechner RJ, Cowie CC, Howie LJ, Herman WH, Will JC, Harris MI. Ophthalmic examination among adults with diagnosed diabetes mellitus. JAMA. 1993;270:1714–8. [PubMed] [Google Scholar]
- 23.Alqurashi KA, Aljabri KS, Bokhari SA. Prevalence of diabetes mellitus in a Saudi community. Ann Saudi Med. 2011;31:19–23. doi: 10.4103/0256-4947.75773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Daghri NM, Al-Attas OS, Alokail MS, Alkharfy KM, Yousef M, Sabico SL, et al. Diabetes mellitus type 2 and other chronic non-communicable diseases in the central region, Saudi Arabia (riyadh cohort 2): A decade of an epidemic. BMC Med. 2011;9:76. doi: 10.1186/1741-7015-9-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.International Diabetes Federation. IDF Diabetes. 7th ed. Brussels, Belgium: International Diabetes Federation; 2015. [Last accessed on 2017 Nov 15]. Available from: https://diabetesatlas.org/ [Google Scholar]
- 26.Raman R, Rani PK, Reddi Rachepalle S, Gnanamoorthy P, Uthra S, Kumaramanickavel G, et al. Prevalence of diabetic retinopathy in India: Sankara Nethralaya diabetic retinopathy epidemiology and molecular genetics study report 2. Ophthalmology. 2009;116:311–8. doi: 10.1016/j.ophtha.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 27.Al Ghamdi AH, Rabiu M, Hajar S, Yorston D, Kuper H, Polack S. Rapid assessment of avoidable blindness and diabetic retinopathy in Taif, Saudi Arabia. Br J Ophthalmol. 2012;96:1168–72. doi: 10.1136/bjophthalmol-2012-301874. [DOI] [PubMed] [Google Scholar]
- 28.Khan AR, Wiseberg JA, Lateef ZA, Khan SA. Prevalence and determinants of diabetic retinopathy in Al Hasa region of Saudi Arabia: Primary health care centre based cross-sectional survey, 2007-2009. Middle East Afr J Ophthalmol. 2010;17:257–63. doi: 10.4103/0974-9233.65502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.El-Bab MF, Shawky N, Al-Sisi A, Akhtar M. Retinopathy and risk factors in diabetic patients from Al-Madinah Al-Munawarah in the Kingdom of Saudi Arabia. Clin Ophthalmol. 2012;6:269–76. doi: 10.2147/OPTH.S27363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hajar S, Al Hazmi A, Wasli M, Mousa A, Rabiu M. Prevalence and causes of blindness and diabetic retinopathy in Southern Saudi Arabia. Saudi Med J. 2015;36:449–55. doi: 10.15537/smj.2015.4.10371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Livingston PM, Wood CA, McCarty CA, Harper CA, Keeffe JE, Taylor HR. Awareness of diabetic retinopathy among people who attended a diabetic retinopathy screening program. Med J Aust. 1998;169:117. doi: 10.5694/j.1326-5377.1998.tb140205.x. [DOI] [PubMed] [Google Scholar]
- 32.Hussain R, Rajesh B, Giridhar A, Gopalakrishnan M, Sadasivan S, James J, et al. Knowledge and awareness about diabetes mellitus and diabetic retinopathy in suburban population of a South Indian state and its practice among the patients with diabetes mellitus: A population-based study. Indian J Ophthalmol. 2016;64:272–6. doi: 10.4103/0301-4738.182937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al Rasheed R, Al Adel F. Diabetic retinopathy: Knowledge, awareness and practices of physicians in primary-care centers in Riyadh, Saudi Arabia. Saudi J Ophthalmol. 2017;31:2–6. doi: 10.1016/j.sjopt.2017.01.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Al Zarea BK. Knowledge, attitude and practice of diabetic retinopathy amongst the diabetic patients of AlJouf and Hail Province of Saudi Arabia. J Clin Diagn Res. 2016;10:NC05–8. doi: 10.7860/JCDR/2016/19568.7862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Almalki NR, Almalki TM, Alswat K. Diabetics retinopathy knowledge and awareness assessment among the type 2 diabetics. Open Access Maced J Med Sci. 2018;6:574. doi: 10.3889/oamjms.2018.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alzahrani SH, Bakarman MA, Alqahtani SM, Alqahtani MS, Butt NS, Salawati EM, et al. Awareness of diabetic retinopathy among people with diabetes in Jeddah, Saudi Arabia. Ther Adv Endocrinol Metabl. 2018;9:103–12. doi: 10.1177/2042018818758621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alasiri RA, Bafaraj AG. Awareness of diabetic retinopathy among diabetic patients in King Abdulaziz University Hospital, Jeddah, Saudi Arabia. Annl Int Med Dental Res. 2016;2:42–5. [Google Scholar]
- 38.Namperumalsamy P, Kim R, Kaliaperumal K, Sekar A, Karthika A, Nirmalan PK. A pilot study on awareness of diabetic retinopathy among non-medical persons in South India. The challenge for eye care programmes in the region. Indian J Ophthalmol. 2004;52:247–51. [PubMed] [Google Scholar]
- 39.Muñoz B, O’Leary M, Fonseca-Becker F, Rosario E, Burguess I, Aguilar M, et al. Knowledge of diabetic eye disease and vision care guidelines among Hispanic individuals in Baltimore with and without diabetes. Arch Ophthalmol. 2008;126:968–74. doi: 10.1001/archopht.126.7.968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Khandekar R, Harby SA, Harthy HA, Lawatti JA. Knowledge, attitude and practice regarding eye complications and care among Omani persons with diabetes-A cross sectional study. Oman J Ophthalmol. 2010;3:60–5. doi: 10.4103/0974-620X.64228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Muecke JS, Newland HS, Ryan P, Ramsay E, Aung M, Myint S, et al. Awareness of diabetic eye disease among general practitioners and diabetic patients in Yangon, Myanmar. Clin Exp Ophthalmol. 2008;36:265–73. doi: 10.1111/j.1442-9071.2008.01724.x. [DOI] [PubMed] [Google Scholar]
- 42.Mohammed I, Waziri AM. Awareness of diabetic retinopathy amongst diabetic patients at the murtala mohammed hospital, Kano, Nigeria. Niger Med J. 2009;50:38–41. [Google Scholar]
- 43.Rani PK, Raman R, Subramani S, Perumal G, Kumaramanickavel G, Sharma T. Knowledge of diabetes and diabetic retinopathy among rural populations in India, and the influence of knowledge of diabetic retinopathy on attitude and practice. Rural Remote Health. 2008;8:24. [PubMed] [Google Scholar]
- 44.Amir AH, Jadoon MZ, Zeb S, Sabir S. Awareness diabetic retinopathy amongst known diabetics. Journal of Postgraduate Medical Institute (Peshawar-Pakistan) 2011;21:10–15. [Google Scholar]
- 45.Çetin EN, Zencir M, Fenkçi S, Akın F, Yıldırım C. Assessment of awareness of diabetic retinopathy and utilization of eye care services among Turkish diabetic patients. Prim Care Diabetes. 2013;7:297–302. doi: 10.1016/j.pcd.2013.04.002. [DOI] [PubMed] [Google Scholar]


