Abstract
Aim:
To assess the association of dental caries with health capital among 12-year old in Private and Government school children with differing family-related characteristics.
Objectives:
To know the influence of height, weight, and family-related characteristics on dental caries.
Materials and Methods:
A cross-sectional study was done on a sample of 800 students. Stratified systematic random sampling technique was used. Data were collected on health variables that include their height and weight; family characteristics include type of family and time spent with their mothers in a school day and number of children in their family. Clinical examination was done using dentition status and treatment needs.
Results:
The prevalence of dental caries in government school was 64% and in private school was 59.2%. Logistic regression analysis identified that dental caries was significantly associated with type of school, height, and socioeconomic status and the factors which are not significantly associated are weight, time spent with their mothers, number of siblings, dental visits, and type of family.
Conclusion:
This study reported dental caries prevalence to be 61.6% with a mean DMFT (Decayed Missing Filled Teeth) of 1.26 ± 1.32 in 12-year old children. The cooperation of dentists and pediatricians is necessary in assessment of general and dental health in a holistic context throughout the life course to enhance the well-being of adolescents.
Keywords: Dental caries, life course, school children
Introduction
The life course approach, recently popular in conceptualizing chronic disease etiology, proposes assessing the effects of physical and psychosocial exposures on chronic disease risk at different stages of life such as gestation, childhood, and adolescence.[1] Exposure to one factor at one stage of life is likely to be connected with exposure to other factors at another life stage, and these exposures are likely to accumulate over the lifespan of the individual.[2] It provides a more comprehensive approach than traditional risk factor epidemiology as it seeks to understand when and how particular exposures act on later health outcomes.
An individual's biological resources are influenced by their genetic endowment, their prenatal and postnatal development, and their social and physical environment in early life. Adversity in childhood becomes “embodied” at an early age and its full impact manifests later in life.[3,4]
Height and weight is an important surrogate marker of early development and of social and physical environment exposures in early life. Socioeconomic circumstances influence fetal development and growth during childhood. Subsequently, poor fetal development and delayed linear growth, as indexed, respectively, by low birth weight and shorter leg-length. Social inequalities in oral health have been well documented in the dental scientific literature, providing plenty of evidence for the poorer oral health of lower-socioeconomic status (SES) groups compared with their higher-SES counterparts.
First, life course approach appears to be well suited for dental caries as it is cumulative in nature, which would allow comparison of the degree of disease development among individuals. Second, dental caries is a chronic disease, which is more likely to be detected only during assessment. Third, its validly and reliably can be measured. Fourth, dental caries is prevalent, so that the required sample size for the cohort is manageable.[5]
The life course approach is recommended for the prevention of obesity as well as of other chronic diseases by the World Health Organization (WHO).[6] This approach is important among school aged-children in attainment of a common preventive approach for general and dental well-being, because increased body weight relative to body height (overweight and obesity) are more likely to be common among adolescents with higher caries.[7]
There are very few studies exploring this plausible relation, so the aim of this study is to assess the association of dental caries experience with health factors among 12-year-old private and government school children with differing family-related characteristics in Guntur city, Andhra Pradesh.
Material and Methods
A cross-sectional study was done by clinical examination of the children attending private and government schools located in Guntur city. Children who have completed 12 years of age by March 31 and who were willing to participate in the study were included in the study. Any medically compromised condition that contraindicated oral examination was the exclusion criterion. Informed consent was taken from children parents for participating in the study.
Ethical clearance and permission for execution of the study from D.E.O office; respective school authorities were taken prior to the start of the study. Sample size was calculated using this formula
Where zα is standard normal variate value (1.96 for 95% CI), p is the prevalence of disease (80%), q is alternative prevalence (20%), and d is permissible error in prevalence rate (2.4); and estimated to be 800. A pilot study was carried out on 25 school children selected from one private and one government school to see the feasibility of the study.
Stratified systematic random sampling was done to select children. Schools were divided into 2 strata, i.e. private and government schools. Eight private and eight government schools were selected by systematic random sampling expecting 50 students in each school. All the eligible children in the selected schools present on the day of examination were included in the study.
The survey proforma prepared included demographic information on gender; school name; health factor which includes height (cm) and weight (kg); and family characteristics that includes type of family, number of children in their family, dental visits, and socioeconomic status. Socioeconomic status of study subjects was classified according to modified Kuppuswamy scale 2007.[8] Proforma was filled by the examiner, height was recorded using measuring tape with least measurement of 1 cm, and weight was recorded using “Krups” bathroom weighing machine with least measurement of 0.5 kg and corrected for zero error every time before recording a new measurement.
Both English and Telugu questionnaires were used. Telugu is the regional language; hence, questionnaire was translated into Telugu language. The validity was checked by back translation method, involving blind translation into English. The validity of translation was verified by experts in both languages.
Clinical examination was done using Dentition status and treatment needs as per WHO Basic oral health survey 1997.[9] One trained and calibrated dentist conducted all clinical oral examination with the trained recorder recording the observations. Before conducting the survey, the training and calibration of examiner was done to ensure reliability (k = 0.80). After taking permission from school authority, study proforma were distributed to the school children. This was followed by Type III ADA examination[10] using autoclaved mouth mirror, CPI probe, and adequate illumination. A table and a two chair were arranged so as to allow maximum efficiency and ease of examination.
Data were compiled using Microsoft excel software and analyzed using SPSS V.20:0. Chi-square test by cross tabulations was used to compare the frequencies (level of significance, P < 0.05). Analysis of variance is used to compare the health variables with DMFT. Kruskal–Wallis test was used to compare the socioeconomic status between caries experience. Logistic regression analysis was done for odds ratio to know the association between DMFT, health factor, and family-related characteristics.
Results
In this study, 53% were males and 47% were females in government school. About 49.6% were males and 50.4% were females in private school as shown in Graph 1.
Graph 1.
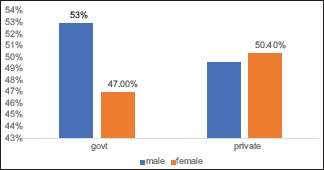
Percentage distribution of males and females in government and private schools
The total caries experience of government school children was 1.26 ± 1.32, whereas the private school children was 1.08 ± 0.63 [Table 1], which shows that government school children were more dentally diseased than the private school children.
Table 1.
Caries experience among school children
| Caries experience | DT | MT | FT | DMFT, mean±SD |
|---|---|---|---|---|
| Government | 256 (64%) | 7 (0.8%) | 2 (1.5)% | 1.26±1.32 |
| Private | 237 (59.2%) | 22 (2.75%) | 6 (0.75)% | 1.08±0.63 |
DT=decayed teeth, MT=missing teeth, FT=filled teeth, SD=standard deviation
Table 2 shows that mean body height and weight of private school children were more than those of government school children. Private (0.041 < 0.05) and government (0.028 < 0.05) school children height was statistically significantly associated with DMFT, whereas no statistical significance was found between weight and DMFT of private and government school children.
Table 2.
The relationship between height and weight with DMFT in private and government school children
| Government | DMFT 0 (mean) | DMFT (1-3) (mean) | DMFT >3 (mean) | P |
|---|---|---|---|---|
| Height | 141.2 | 138.6 | 113.2 | 0.02* |
| Weight | 35.7 | 32.8 | 31.7 | 0.061 |
| Private | ||||
| Height | 143.7 | 139.7 | 138.9 | 0.041* |
| Weight | 38.7 | 36.5 | 31.3 | 0.072 |
ANOVA test, * statistically significant (P<0.05)
Table 3 shows the measures of family-related characteristics among government school children. Government school children spent >6 h with their mother 186 (46.5%) and most of them visited dentist only in pain 351 (87.75%). These variables had no significant relation with dental caries. Most of the private school children spent more time with their mothers 147 (36.75%) and visited dentist only in pain 346 (86.5%). The P values shows that they are not significantly related to dental caries [Table 4]. Socioeconomic status of the government school children (P = 0.04) and private school children (P = 0.046) had a statistically significant relation with dental caries [Table 5].
Table 3.
Shows the relationship between family-related characteristics with DMFT among government school children
| Time spent with their mother | DMFT 0 | DMFT (1-3) | DMFT >3 | P |
|---|---|---|---|---|
| <2 h | 23 (15.54%) | 28 (13.02%) | 12 (32.43%) | 0.391 |
| 2-4 h | 26 (17.57%) | 38 (17.67%) | 9 (24.32%) | |
| 4-6 h | 24 (16.22%) | 48 (22.33%) | 6 (16.22%) | |
| >6 h | 75 (50.68%) | 101 (46.98%) | 10 (27.03%) | |
| Visiting the dentist | ||||
| Regular check-up | 24 (16.22%) | 19 (8.84%) | 6 (16.22%) | 0.728 |
| In trouble | 124 (83.78%) | 196 (91.16%) | 31 (83.78%) | |
| Family type | ||||
| Single parent | 10 (6.75%) | 21 (9.76%) | 2 (5.4%) | 0.06 |
| Two parent | 91 (61.48%) | 142 (66.04%) | 30 (81.08%) | |
| Joint family | 47 (31.75%) | 52 (24.18%) | 5 (13.51%) | |
| Number of children | 0.51 | |||
| One | 8 (5.4%) | 5 (2.38%) | 1 (2.7%) | |
| Two | 43 (29.05%) | 116 (53.95%) | 21 (56.76%) | |
| More than two | 97 (65.54%) | 94 (43.72%) | 15 (40.54%) |
Chi-square test
Table 4.
Shows the relationship between family-related characteristics with DMFT among Private school children
| Time spent with their mothers | DMFT 0 | DMFT (1-3) | DMFT >3 | P |
|---|---|---|---|---|
| 2 h | 12 (7.55%) | 10 (4.83%) | 7 (20.59%) | 0.424 |
| 2-4 h | 42 (26.42%) | 60 (28.99%) | 8 (23.53%) | |
| 4-6 h | 30 (18.87%) | 76 (36.71%) | 8 (23.53%) | |
| >6 h | 75 (47.17%) | 61 (29.47%) | 11 (32.35%) | |
| Dental visit | ||||
| Regular | 37 (23.27%) | 14 (6.76%) | 3 (8.82%) | 0.095 |
| Trouble (pain) | 122 (76.73%) | 193 (93.24%) | 31 (91.18%) | |
| Family type | ||||
| Single parent | 16 (10.06%) | 19 (9.17%) | 9 (26.47%) | 0.702 |
| Two parent | 131 (82.38%) | 156 (75.36%) | 19 (55.88%) | |
| Joint family | 12 (7.54%) | 32 (15.45%) | 6 (17.64%) | |
| Number of children | ||||
| One | 22 (13.83%) | 10 (4.83%) | 2 (5.88%) | 0.866 |
| Two | 123 (77.35%) | 178 (85.99%) | 24 (70.58%) | |
| More than two | 14 (8.8%) | 19 (9.17%) | 8 (23.52%) |
Table 5.
The relationship between socio economic status and DMFT in private and government school children
| SES - govt | DMFT 0 | DMFT (1-3) | DMFT >3 | P |
|---|---|---|---|---|
| Upper | 4 (2.7%) | 0 | 1 (3.22%) | 0.04* |
| Upper middle | 29 (19.59%) | 9 (4.18%) | 2 (6.45%) | |
| Lower middle | 51 (34.45%) | 117 (54.41%) | 24 (77.41%) | |
| Lower upper | 57 (38.51%) | 84 (39.06%) | 10 (32.25%) | |
| Lower | 7 (4.72%) | 5 (2.32%) | 0 | |
| SES- private | ||||
| Upper | 68 (42.76%) | 77 (37.19%) | 11 (32.35%) | 0.046* |
| Upper middle | 58 (36.47%) | 92 (44.44%) | 16 (47.05%) | |
| Lower middle | 32 (20.12%) | 36 (17.39%) | 7 (20.58%) | |
| Lower upper | 1 (0.62%) | 2 (0.96%) | 0 | |
| Lower | 0 | 0 | 0 |
Kruskal-Wallis test; SES=socioeconomic status. *statistically significant (P<0.05)
Results of multiple logistic regression [Table 6] shows that government school children are 1.67 more times at the risk of dental caries attack when compared to private school children (P = 0.021). The shorter height children are more prone to dental caries compared to the taller children (OR = 1.45; CL = 1.04–2.02). Considering the socioeconomic status, middle-income group (OR = 1.01;CL = 0.7–1.4) and low-income class (OR = 1.16;CL = 0.55–2.18) had more risk of dental caries compared with upper class.
Table 6.
Multivariate logistic regression analysis to assess the risk factors association with dental caries
| Variables | Independent variable (effect) | Chi-square | Sig | OR (95% CI) |
|---|---|---|---|---|
| Demographic variables | School | 5.29 | 0.021* | 1.67 (1.08-8.57) |
| Government | ||||
| Gender female | 0.22 | 0.64 | 0.93 (0.70-1.25) | |
| Health variables | Height <164 cm | 4.80 | 0.028* | 1.45 (1.04-2.02) |
| Weight <39 kg | 0.03 | 0.85 | 1.03 (0.73-1.46) | |
| Family-related characteristics | SES | |||
| Middle | 5.69 | 0.05* | 1.01 (0.7-1.4) | |
| Low | 1.16 (0.55-2.18) | |||
| Dental visits | ||||
| Check up | 0.01 | 0.98 | 0.99 (0.65-1.52) | |
| Family type | ||||
| Single parent | 0.52 | 0.77 | 1.29 (0.63-2.65) | |
| Number of children | 0.59 | 0.74 | ||
| Two | 1.3 (0.7-2.3) | |||
| More than two | 1.04 (0.6-2.0) |
CI=confidence intervals, OD=odds ratio,*statistically significant at (P<0.05)
Discussion
The aims and objectives of the present study were to know the relation between health variables and dental caries among 12-year school going children with differing family-related characteristics in Guntur city. Findings from this study supported the life course approach that health and family-related characteristics contribute to dental health.
According to gender-wise distribution, 49.6% were males and 51.4% were females, which is in accordance with census Guntur 2011 (Guntur).[11]
Body height is used as a potential indicator of the long-term, cumulative effects of inadequacies of health; weight is an indicator of malnutrition. In this study, height is statistically significantly associated with DMFT among school children which is similar to the study conducted by Belinda Nicolau (2005).[12] Height and dental caries can be related to fetal development and growth during pregnancy. It can be explained by the fact that nutritional deficiency during childhood delays linear growth as indexed by shorter leg length and affects the tooth structure, and even saliva secretion rate, buffering capacity, and immunological systems.
In this study, weight is not statistically significantly associated with DMFT, which is not in accordance with the study done by Nicolau (2003).[13] It can be explained due to the fact that weight is a multifactorial component. Low birth weight may be due to poor maternal nutrition, smoking during pregnancy, and abnormal intrauterine growth.
This study reported dental caries prevalence to be 61.6% with a mean DMFT of 1.26 ± 1.32 in 12-year-old children, which is in accordance with DCI report (2004).[14] In this study, more percentage of caries experience was observed in government school children, the reason could be lack of dental awareness toward dental problems, and less affordability to dental care because of their poor economic background, which simulates with the study done by Sudha (2005).[15]
In this study, 86.25% of subjects visited the dentist only when in trouble or pain, which is similar to the study conducted by Sijjanpoudyal (2010).[16] The possible reason might be due to the fact that tooth pain is an emergency condition, which has forced the subject to visit the dentist.
In this study, 77.25% of the children were from nuclear family, and 17.38% from joint family, and 5.38% were from single parent family, which is similar to the study conducted by Belinda (2005),[17] in which 81.5% were from nuclear families. It did not show a statistically significant association between family type and dental caries which is not in accordance with the study conducted by Mattila (2005).[18] This can be explained by the fact that caries is multifactorial and the type of family plays a less role in the causation of caries and the number of reconstituted families are comparatively less in India compared with foreign countries.
In this study, 38% of the government school children had more number of siblings than private school children (15.5%) and they belonged to low socioeconomic group. They had statistically significantly more caries compared with private school children. It is consistent with the study conducted by Cinar (2008).[19] Children belonging to low socioeconomic class in government schools had more number of untreated caries compared with children from private schools which is similar to the study conducted by Schou (1995)[20] and Goettams (2018).[21] It is well known that children from low socio economic background cannot afford the costly dental treatment. The reason could be lack of dental awareness and less affordability to dental care.
According to logistic regression, the risk factors identified that are significantly associated with dental caries are type of school, height, and socioeconomic status. Government school children, height <164 cm, and children from middle- and low-socioeconomic status are more prone to risk of dental caries.
Conclusion
The life course frame work expands upon the adult lifestyle model to build a bridge where biological, psychological, and social models of disease causation are incorporated. To conclude, “the future value of a life course approach will depend for its success on elucidating new mechanisms and disease pathways as well as its ability to explain social, geographical and temporal patterns of disease distribution. The cooperation of paediatricians and dentists is necessary in assessment of general and dental health in a holistic context throughout the life course.”
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors would like to thank the students of the schools who participated in the research project and contributed their valuable time and support to the research work.
References
- 1.Kuh D, Ben-Shlomo Y, Lynch J, Hallqvist J, Power C. Life-course epidemiology. J Epidemiol Community Health. 2003;57:778–83. doi: 10.1136/jech.57.10.778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ben-Shlomo Y, Kuh D. A life-course approach to chronic disease epidemiology: Conceptual models, empirical challenges, and interdisciplinary perspectives. Int J Epidemiol. 2002;31:285–93. [PubMed] [Google Scholar]
- 3.Kuh D, Power C, Blane D, Bartley M. Social pathways between childhood and adult health. In: Diana K, Ben-Shlomo Y, editors. The Life Course Approach to Chronic Disease Epidemiology. Oxford: Oxford University Press; 1997. pp. 169–98. [Google Scholar]
- 4.Broadbent JM, Zeng J, Foster Page LA, Baker SR, Ramrakha S, Thomson WM. Oral health-related beliefs, behaviors, and outcomes through the life course. J Dent Res. 2016;95:808–13. doi: 10.1177/0022034516634663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nicolau B, Thomson WM, Steele JG, Allison PJ. Life course epidemiology: Concepts and theoretical models and its relevance to chronic oral conditions. Community Dent Oral Epidemiol. 2007;35:241–9. doi: 10.1111/j.1600-0528.2007.00332.x. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Diet, nutrition, and the prevention of chronic diseases: Report of a joint WHO/FAO expert consultation [serial on the internet] Geneva: WHO; 1990. [Last accessed on 2007 Nov 11]. pp. 916–40-45. Available from: http://www.who.int/hpr/NPH/docs/who_fao_expert_report.pdf . [Google Scholar]
- 7.WHO. Oral health promotion: An essential element of a health-promoting school [serial on the Internet] Geneva: WHO; 2003. [Last accessed on 2007 Nov 11]. Available from: http://www.who.int/oral_health/publications/doc11/en/ [Google Scholar]
- 8.Kumar N, Gupta N, Kishore J. Kuppuswamy socio economic scale. Updating Income range for the year 2012. Indian J Cancer Res and Therapeutics. 2012;8:57–66. [Google Scholar]
- 9.World Health Organization. Oral Health Surveys Basic Methods. 4th ed. Geneva: 1997. [Google Scholar]
- 10.James Morse Dunning. Principles of Dental Public Health. 4th ed. London: Harvard University Press; 1986. [Google Scholar]
- 11. [Last accessed on 2012 Aug 16]. Available from: http://www.census 2011.co.in/census/district/134-Guntur .
- 12.Nicolau B, Marcenes W, Allison P, Sheiham A. The life- course approach: Explaining the association between height and dental caries in Brazilian adolescents. Community Dent Oral Epidemiol. 2005;33:93–8. doi: 10.1111/j.1600-0528.2005.00213.x. [DOI] [PubMed] [Google Scholar]
- 13.Nicolau B, Marcenes W, Bartley M, Sheiham A. A life course approach to assessing causes of dental caries experience: The relationship between biological, behavioral, socio economic and psychological conditions and caries in adolescents. Caries Res. 2003;37:319–26. doi: 10.1159/000072162. [DOI] [PubMed] [Google Scholar]
- 14.Dental Council of India. Multicentric oral health survey report Dental Council of India. 2004 [Google Scholar]
- 15.Sudha P, Bhasin S, Anigundi RT. Prevalence of dental caries among 12-13 year old children of Manglore city. J Indian Soc Pedod Prev Dent. 2005;25:74–9. doi: 10.4103/0970-4388.16446. [DOI] [PubMed] [Google Scholar]
- 16.Poudyal S, Rao A, Shenoy R, Priya H. Utilization of dental services in a field practice area in Manglore Karnataka. Indian J Community Med. 2010;35:424–5. doi: 10.4103/0970-0218.69278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nicolau B, Marcenes W, Hardy R, Sheiham A. The life coarse approach to assess the relationship between social and psychological circumstances and gingival status in adolescents. J ClinPeriodontol. 2003;30:1038–45. doi: 10.1046/j.0303-6979.2003.00424.x. [DOI] [PubMed] [Google Scholar]
- 18.Mattila ML, Rautava P, Aromaa M. Behavioural and demographic factors during early childhood and poor dental health at 10 years of age. Caries Res. 2005;39:85–91. doi: 10.1159/000083152. [DOI] [PubMed] [Google Scholar]
- 19.Cinar AY, Murtomma H, Tseveenjav B. The life course approach in Assessment of dental health: A cross sectional study among finnish and Turkish pre adolescents. Eur J Dent. 2008;2:153–61. [PMC free article] [PubMed] [Google Scholar]
- 20.Schou L, Uitenbroek D. Social and behavioral indicators of caries experience in 5 year old children. Community Dent Oral Epidemiol. 1995;23:276–81. doi: 10.1111/j.1600-0528.1995.tb00248.x. [DOI] [PubMed] [Google Scholar]
- 21.Goettams ML, Ourens M, Cosetti L, Lorenzo S, Álvarez-Vaz R, Celeste RK. Early-life socioeconomic status and malocclusion in adolescents and young adults in Uruguay. Cad Saude Publica. 2018;34:e00051017. doi: 10.1590/0102-311X00051017. [DOI] [PubMed] [Google Scholar]


