Abstract
The occurrence of chronic proctitis as a side effect among radiotherapy patients is about 5%. Radiation proctitis and consequent development of chronic proctitis are not associated to each other. However, a lot of samples of proctitis that are limited easily could be treated by typical remedial techniques. Improvements in radiotherapy techniques that make possible the delivery of superior doses of radiation could easily reduce both chronic and acute proctitis. The step-by-step remedial procedure for treatment of this disorder starts with conservative remedial management and includes iron substitution as a second-line therapy. For patients who did not receive initial therapies, sucralfate injection, topical corticosteroids, and antidiarrhea therapy were provided as a means of aggressive care. In cases of continuous rectal bleeding, remedial laser techniques and formaldehyde administration should be attempted before surgical therapy. When surgical therapy is required, a descending or transverse colostomy must be carried out. Advanced methods such as intraperitoneal injections of formalin or novel methods of cold therapy and radiofrequency ablation (RFA) provide a wider remedial field. Exceptionally, unanticipated conclusion of neosquamous wound healing via RFA may have additional preponderances in stopping symptoms and may require better assessment through accurate randomized examination. Since aggressive treatments like coloanal anastomosis and colorectal surgery are correlated with remarkable mortality and morbidity, they must be considered as the final course of remedial treatment.
Keywords: Colorectal surgery, laser therapy, radiation proctitis, rectal bleeding
Introduction
Radiation could induce both cell death and apoptosis as a result of damage to DNA, lipids, and proteins and generally affects cell growth like cancer cells.[1] Nowadays, pelvis radiation therapy is a main component of the remedial treatment for pelvic malignancies and is also applied as an effective neoadjuvant therapy. Radiotherapy was initially not considered as advantageous to patients, mainly those with rectal cancer, as the tumors are considered to be resistant to radiation. Recently, researchers have discovered that application of higher doses of radiation could be useful in dominating this persistence. On the other hand, application of radiation in higher doses may result in adverse effects to the organs of the body. Presently, the most recurrent complication of radiotherapy, as a side effect of applying higher doses, is the occurrence of proctitis following the treatment of prostate cancer.[2]
Radiotherapy could be applied via radioactive seed implants known as brachytherapy or external beam therapy (EBT). EBT in most cases is manipulated via an external photon generator accompanied by diverse sources such as electron beams, X-rays, and gamma rays through a four-beam procedure that could considerably control exposure of the surrounding organs.[3] In particular, during prostate cancer treatment, adjacent rectum regions will receive similar dose of radiation. Novel EBTs such as intensity-modulated radiotherapy (IMRT) and three-dimensional conformal radiotherapy (3D-CRT) deliver higher doses of radiation while reducing the toxicity effects of surrounding areas[2]
IMRT is one of the significant latter oncology evolutions which uses computational procedures for dose delivery and beam orientation through the same beam scope. The 3D-CRT technique applies computed tomography scan to focus the radiation scope in a permanent rate of dose.[4] Remedial cancer method with brachytherapy could be done through two delivery procedures which try to get the same target of the aimed tissue localized exposure.[5]
Another procedure which requires the application of hollow thin medical tubes known as catheters could be increasingly filled with larger amounts of radioactive pellets during the time periods. On the other hand, brachytherapy could help in reduction of surrounding tissue damage as the pellets are implanted with precise positioning.[5] The rate of colorectal complications after brachytherapy is effectively less in comparison with external beam radiation. A comprehensive study of colorectal complications of external beam radiation and brachytherapy for prostate cancer by Lesperance et al.[6] demonstrated reduced chronic and acute complications after brachytherapy in comparison with external beam radiation.[6] The common doses delivered to the pelvis ranged between 45 to 50 Gy for neoadjuvant therapy and up to 85 Gy for prostate or anorectal mucosal melanoma. It is reported to be the decisive therapy for gynecologic cancers.[7,8]
As shown in Table 1, based on the research by Zelefsky et al.,[9] the European Organization For Research and Treatment of Cancer (EORTC), and the radiotherapy oncology group (RTOG), the comprehensive classification of degrees of radiation proctitis based on an organized system of symptoms range from no symptoms to deadly complications.[9] The studies regarding external beam radiation have reported a 3%–40%[6] occurrence of radiation proctitis depending on the grade/severity of the proctitis. IMRT trials have reported that the occurrence rates vary from 2% to 10% and that of particle radiotherapy is less than 1%,[10,11] compared with other remedial methods.
Table 1.
| Stages | Symptoms | General therapeutic management |
|---|---|---|
| 0 | Without symptoms | None |
| I | Periodic urgency and pain; external ulcer less than one cm2, oracular bleeding and mild lesion | Outpatient operation; without lifestyle arrangement |
| II | Periodic urgency and pain; external ulcer higher than one cm2, infrequent bleeding and temperate lesion | Outpatient operation; some lifestyle arrangement |
| III | Resistant urgency and pain, deep ulcer, prolonged bleeding and intense lesion | Practical brief hospitalization or minor surgical therapy; major lifestyle arrangement |
| IV | Resistant urgency and irrepressible pain; fistula, perforation, gross bleeding and thorough blockage | Long-time hospitalization or major surgical treatment |
| V | Multiple organ failure, death and medical emergency of sepsis | Severe mortal complications |
Materials and Methods
A total of 315 records were selected by searching databases such as EMBASE, PUBMED, LILACS, EBSCO, COCHRANE and SCOPE. After removing irrelevant records and including certain additional records to the main subject of the research, 29 purely related records were selected for research [Figure 1].
Figure 1.
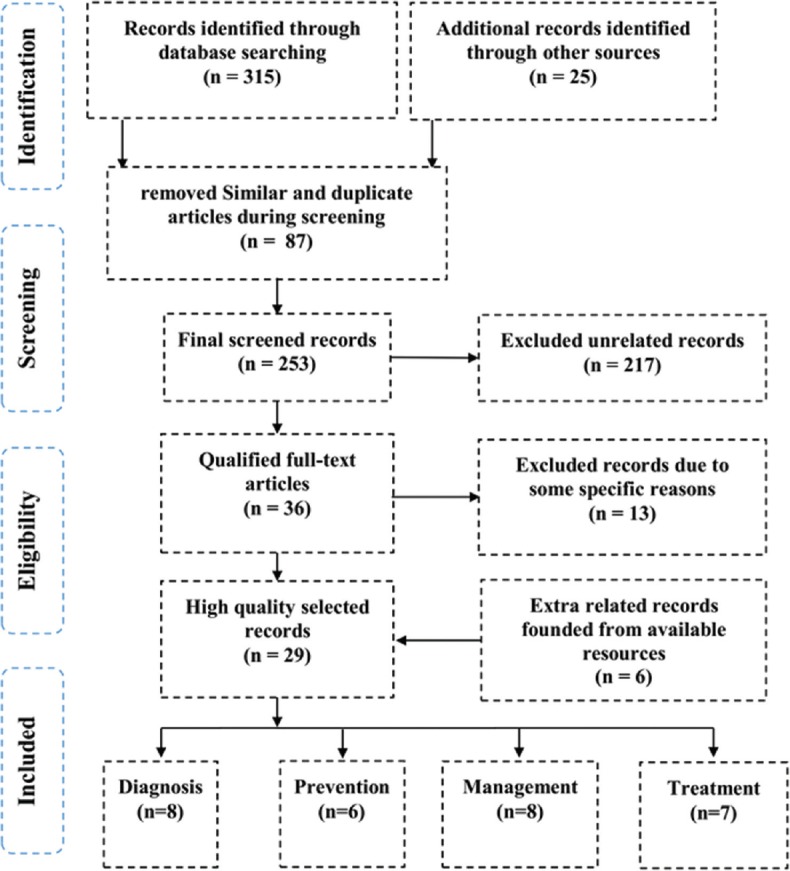
Flow diagram of selected studies in accordance with PRISMA (2009)
Clinical appearance
Initial symptoms may occur one or two weeks after radiotherapy. Vomiting and nausea are experienced after radiotherapy of upper abdomen in opposition to pelvic radiation.[12] Involvement of small intestine could cause stomach cramps, short-term diarrhea, and nausea. Large bowel irradiation could cause tenesmus, diarrhea, and rectal bleeding and discharge in case of rectal ulcer.[13]
The secondary symptoms may be developed after 3 months of the first radiotherapy. The most frequent symptoms of mild radiation damages to the bowel include renal colic pain, vomiting, nausea and, in some cases, mild blockage of the bowel. Within small intestine, when ileum is involved highly, the outstanding disorder may be malabsorption.[14] Patients affected by chronic radiation of rectum would have proctitis symptoms such as mucous rectal discharge, tenesmus, and hematochezia. Patients may sometimes experience constipation and rarely low grade large-bowel obstruction.[15]
Acute proctitis
Acute radiation proctitis is a result of radiotherapy involving outward mucosal layer and occurs approximately three months after the start of the therapy and sometimes may remain up to six months.[16] Up to one-fifth of the patients develop symptoms such as cramps, nausea, tenesmus, diarrhea, minor bleeding, mucus discharge and urgency and remedial treatment. Radiation proctitis is the result of the inflammatory process of rectal mucosa which appears as a beefy red, dropsical and is accompanied by ulcer.[17] Colonoscopic biopsy of the inflammatory rectal mucosa is usually not suggested because of the enhanced fistula and the risk of bleeding. Acute radiation proctitis involving superficial mucosa would not lead to chronic radiation proctitis and will be restricted spontaneously by discontinuing radiotherapy.[2]
Chronic proctitis
Chronic proctitis symptoms are similar to those of acute radiation proctitis and include fistula, perforation, strictures, occlusion of bowel, and severe bleeding. However, the pathological procedure is not alike the acute phase and eventually involves the compromised blood supply to the wall of the rectum which will lead to fibrotic changes and full thickness infarction.[18] Demolition and focal distortion of arterioles and coronary microvascular dysfunction with intimal fibrosis of muscular pulmonary arteries may be observed.[18] As a result, the patient's life quality could be affected by chronic radiation proctitis more crucially than patients with acute proctitis.[2]
Oxidative stress, a disturbance in the balance of reactive oxygen species production also leads to the spread of chronic radiation proctitis. In patients with inflammatory bowel disease (IBD), the rate of progress of radiation proctitis is on par with those of other external beam irradiation complications.[19] In patients with HIV, insufficiency of glutathione (GSH) could lead to the depletion of radioprotective thiols and increased oxidative stress. A study by Alex et al.[20] reported that HIV patients who are affected via anal cancer and have a CD4 test outcome of fewer than 200 have increased mucositis and bleeding and decreased tolerance suggesting a high requirement for lower remedy doses.[20]
Diagnosis
The main factors that could be considered for diagnosis are pelvic irradiation history for malignant tumor, diarrhea, tenesmus, and hematochezia. During the early stage of intestinal inflammation that happens after radiation, the plain radiograph could demonstrate the ileus clearly. Detailed information on barium X-rays mostly show mucosal edema and hypotonic, dilated loops of small intestine.[21] In the acute phase, rectum demonstrates intense spasm and, rarely, anterior wall ulcer could be seen. On inflammation of both the small intestine and the colon caused by radiation, tumor regression must be eliminated as the clinical development of chronic radiation inflammation of the intestines are not specified. Under same conditions, barium X-rays of the small intestine might demonstrate small intestine loops separation, extreme secretion, and mucosal edema within the intestinal lumen.[22] Sigmoidoscopy or colonoscopy might be needed for examination of bleeding from lower colon or rectum and also to determine the location of lesion. In addition, barium X-ray examination of the enema is required for tumor recurrence detection. Additionally, CT scan, MRI, or ultrasonography (USG) of abdomen could be instructional adequately. While lesion biopsy could be helpful in recognition, it would not be chosen as a practicable method due to necrotic wall perforation and bleeding.[23,24]
Prevention
Radiotherapy delivery has varied considerably during the years, with purification radiation delivery restricting the exposure of radiation to neighboring tissues. The lower gastrointestinal tract injury caused via radiation could be reduced by adopting two essential remedial tactics including: decreasing the relative radiation susceptibility of tissues which are at risk and decreasing doses delivered to the adjacent tissues. These strategies could be done via physical obstacles like holding chambers.[11] Among men who are affected via prostate cancer, by application of a collagen spacer by transperineal injection a 50% decrease in radiation dose to the rectal wall could be accomplished. This achievement could enhance the distance among the prostate gland and the rectal wall, consequently providing radiation in extra doses with relative sparing of the rectum.[25]
Newly various procedures of delivering remedial treatment such as volumetric-modulated arc therapy (VMAT), intensity-modulated radiotherapy (IMR), and image-guided radiotherapy (IGR) which apply a mixture of varying intensity multiple beams and managements of real-time monitoring of the organ movement for accurately delivery of the external beam to the subjective tissue without the smallest effect on adjacent organs.[26] Another aforementioned strategy for preventing radiotherapy-induced injuries is by applying biological procedures for modifying the radiosensitivity of normal tissues to ionizing radiation. Amifostine is a cytoprotective remedial adjuvant and a compound drug which removes free radicals of oxygen and was applied in randomized clinical trial for the first time by Athanassiou et al.[27]
Treatment
Due to the lack of any comprehensive studies which evaluate the various remedial procedures for treatment of radiation proctitis, the existing therapeutic strategies are mostly extracted from clinical trials, case reports, and systematized experiences. In general, the initial step in the management of a disease could be done via applying medical care. More invasive procedures like surgical and endoscopic therapies would be applied for patients whose disease symptoms are resistant and violent.[28] Therapeutic management of chronic radiation proctitis contains three comprehensive groups. The first one is medication therapy management including oral drugs, clyster, oxygen therapy, and topical medication. The second one is therapeutic endoscopy which include dilation enlargement process, laser therapy, medical endoscopic procedure of argon plasma coagulation (APC), cold therapy, mesenchymal stem cells (MSCs) therapy, and radiofrequency ablation (RFA). The last one is the surgical or endovascular therapy. The classification of potential therapeutic management of chronic radiation proctitis is provided in Table 2.[23]
Table 2.
Potential therapeutic management for chronic radiation proctitis derived in accordance with[23]
| Type of remedy | Mechanism | Main role | |
|---|---|---|---|
| Medication therapy management | Butanoate | Applied for medicate epithelial cells of the colon | Mostly applied for acute radiation proctitis treatment |
| Mesalazine derivatives | Antiinflammatory | The first treatment in chronic radiation | |
| Sucralfate | Prevents small artery injury | Proctitis accompanied by other side effects | |
| Metronidazole | Antiinflammatory | N/A | |
| Short chain fatty acid (SCFA) | Applied for medicating epithelial cells of the colon | N/A | |
| Vitamin A | Antiinflammatory | N/A | |
| Topical formaldehyde | Chemical cautery | N/A | |
| Hyperbaric oxygen therapy | Enhances medicate | In spite it’s not existing broadly, proved to be high effective | |
| Therapeutic endoscopy | Dilatation therapy | N/A | For radiation-related constrictions |
| Bipolar cauterization and heater | Thermoelectrical cautery | Extra efficient than medical treatment, particularly in healing bleeding of rectum, in spite of the fact it’s not broadly existing; APC is prior to cold therapy or laser photocoagulation | |
| Neodymium/yttrium aluminum garnet argon laser treatment | Noncontact electrocoagulation | N/A | |
| Cold therapy | Thermal cautery | N/A | |
| APC | Noncontact electrocoagulation | N/A | |
| Surgical or endovascular therapy | Ostomy surgery | Fecal flow diversion | postoperative morbidity risk; reserved for intense rectal fistulas and constrictions of rectum |
| Renovation with flaps | Plenish tissue provided with vessels | N/A | |
| Surgical proctectomy | Damaged tissue elimination | N/A |
Conclusion
One of the most frequent complications of pelvic radiotherapy is radiation proctitis which results as a response to therapeutic management. Due to the progress of radiotherapy techniques, the rates of acute and chronic proctitis have been diminished notably. However, because of these improvements, the delivery of higher doses of radiation to the aimed tissues is possible. For the same reason, a lot of studies that report on chronic radiation proctitis treatment are randomized trials which compare the different treatment modalities. The therapeutic method selection would be mainly based on evidence from anecdotes or clinical experiences. However, some therapeutics have materialized that include application or instillation of topical formaldehyde and therapeutic endoscopy especially via APC would present fine outcomes for bleeding-resistant management to less-invasive remedial managements. Surgical treatment would be applied for violent complications or unmanageable symptoms of radiation proctitis. On the other hand, therapeutic management via injection of mesenchymal stem cells would be a good breaking news for the fact that the treatment of this disorder is still progressing.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Xiao M, Whitnall MH. Pharmacological countermeasures for the acute radiation syndrome. Curr Mol Pharmacol. 2009;2:122–33. doi: 10.2174/1874467210902010122. [DOI] [PubMed] [Google Scholar]
- 2.Do NL, Nagle D, Poylin VY. Radiation proctitis: Current strategies in management. Gastroenterol Res Pract. 2011;2011:917941. doi: 10.1155/2011/917941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Terasawa T, Dvorak T, Ip S, Raman G, Lau J, Trikalinos TA. Systematic review: Charged-particle radiation therapy for cancer. Ann Intern Med. 2009;151:556–65. doi: 10.7326/0003-4819-151-8-200910200-00145. [DOI] [PubMed] [Google Scholar]
- 4.Mahadevan A, Kupelian PA. Conformal external beam radiation therapy. In: Klein EA, editor. Management of Prostate Cancer. Totowa, NJ: Humana Press; pp. 309–28. [Google Scholar]
- 5.Shah SA, Cima RR, Benoit E, Breen EL, Bleday R. Rectal complications after prostate brachytherapy. Dis Colon Rectum. 2004;47:1487–92. doi: 10.1007/s10350-004-0603-2. [DOI] [PubMed] [Google Scholar]
- 6.Lesperance RN, Kjorstadt RJ, Halligan JB, Steele SR. Colorectal complications of external beam radiation versus brachytherapy for prostate cancer. Am J Surg. 2008;195:616–20. doi: 10.1016/j.amjsurg.2007.12.037. [DOI] [PubMed] [Google Scholar]
- 7.Xiao HW, Li Y, Luo D, Dong JL, Zhou LX, Zhao SY, et al. Hydrogen-water ameliorates radiation-inducedgastrointestinal toxicity via MyD88'seffectsonthegutmicrobiota. Exp Mol Med. 2018;50:e433. doi: 10.1038/emm.2017.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hiram AG, Jeff MM. Radiation therapy for prostate cancer. Mo Med. 2018;115:146–50. [PMC free article] [PubMed] [Google Scholar]
- 9.Zelefsky MJ, Fuks Z, Hunt M, Yamada Y, Marion C, Ling CC, et al. High-dose intensity modulated radiation therapy for prostate cancer: Early toxicity and biochemical outcome in 772 patients. Int J Radiat Oncol Biol Phys. 2002;53:1111–6. doi: 10.1016/s0360-3016(02)02857-2. [DOI] [PubMed] [Google Scholar]
- 10.Zelefsky MJ, Levin EJ, Hunt M, Yamada Y, Shippy AM, Jackson A, et al. Incidence of late rectal and urinary toxicities after three-dimensional conformal radiotherapy and intensity-modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70:1124–9. doi: 10.1016/j.ijrobp.2007.11.044. [DOI] [PubMed] [Google Scholar]
- 11.Zietman AL, Bae K, Slater JD, Shipley WU, Efstathiou JA, et al. Randomized trial comparing conventional-dose with high-dose conformal radiation therapy in early-stage adenocarcinoma of the prostate: Long-term results from proton radiation oncology group/american college of radiology 95-09. J Clin Oncol. 2010;28:1106–11. doi: 10.1200/JCO.2009.25.8475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Phan J, Swanson DA, Levy LB, Kudchadker RJ, Bruno TL, Frank SJ. Late rectal complications after prostate brachytherapy for localized prostate cancer: Incidence and management. Cancer. 2009;115:1827–39. doi: 10.1002/cncr.24223. [DOI] [PubMed] [Google Scholar]
- 13.Housri N, Yarchoan R, Kaushal A. Radiotherapy for patients with the human immunodeficiency virus: Are special precautions necessary? Cancer. 2010;116:273–83. doi: 10.1002/cncr.24878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kertesz T, Herrmann MKA, Zapf A, Christiansen H, Hermann RM, Pradier O, et al. Effect of a prostaglandin—given rectally for prevention of radiationinduced acute proctitis—on late rectal toxicity: Results of a phase III randomized, placebo-controlled, double-blind study. Strahlentherapie Onkologie. 2009;185:596–602. doi: 10.1007/s00066-009-1978-8. [DOI] [PubMed] [Google Scholar]
- 15.Kneebone A, Mameghan H, Bolin T, Berry M, Turner S, Kearsley J, et al. Effect of oral sucralfate on late rectal injury associated with radiotherapy for prostate cancer: A double-blind, randomized trial. Int J Radiat Oncol Biol Phys. 2004;60:1088–97. doi: 10.1016/j.ijrobp.2004.04.033. [DOI] [PubMed] [Google Scholar]
- 16.Hille A, Herrmann MK, Kertesz T, Christiansen H, Hermann RM, Pradier O, et al. Sodium butyrate enemas in the treatment of acute radiation-induced proctitis in patients with prostate cancer and the impact on late proctitis. A prospective evaluation. Strahlenther Onkol. 2008;184:686–92. doi: 10.1007/s00066-008-1896-1. [DOI] [PubMed] [Google Scholar]
- 17.Cotti G, Seid V, Araujo S, Souza AH, Jr, Kiss Dr, Habr-Gama A. Conservative therapies for hemorrhagic radiation proctitis: A review. Rev Hosp Clin Fac Med Sao Paulo. 2003;58:284–92. doi: 10.1590/s0041-87812003000500008. [DOI] [PubMed] [Google Scholar]
- 18.Ehrenpreis ED, Jani A, Levitsky J, Ahn J, Hong J. A prospective, randomized, double-blind, placebo-controlled trial of retinol palmitate (vitamin A) for symptomatic chronic radiation proctopathy. Dis Colon Rectum. 2005;48:1–8. doi: 10.1007/s10350-004-0821-7. [DOI] [PubMed] [Google Scholar]
- 19.Willett CG, Ooi CJ, Zietman AL, Menon V, Goldberg S, Sands BE, et al. Acute and late toxicity of patients with inflammatory bowel disease undergoing irradiation for abdominal and pelvic neoplasms. Int J Radiat Oncol Biol Phys. 2000;46:995–8. doi: 10.1016/s0360-3016(99)00374-0. [DOI] [PubMed] [Google Scholar]
- 20.Bryant AK, Mudgway R, Huynh-Le MP, Simpson DR, Mell LK, Gupta S, et al. Effect of CD4 count on treatment toxicity and tumor recurrence in human immunodeficiency virus-positive patients with anal cancer. Int J Radiat Oncol Biol Phys. 2018;100:478–85. doi: 10.1016/j.ijrobp.2017.09.034. [DOI] [PubMed] [Google Scholar]
- 21.Maturen KE, Feng MU, Wasnik AP, Azar SF, Appelman HD, Francis IR, et al. Imaging effects of radiation therapy in the abdomen and pelvis: Evaluating “innocent bystander” tissues. Radiographics. 2013;33:599–619. doi: 10.1148/rg.332125119. [DOI] [PubMed] [Google Scholar]
- 22.Rhodri S, John TG. Radiation-induced small bowel disease: Latest developments and clinical guidance. Ther Adv Chronic Dis. 2014;5:15–29. doi: 10.1177/2040622313510730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tabaja L, Sidani SM. Management of radiation proctitis. Dig Dis Sci. 2018;63:2180–8. doi: 10.1007/s10620-018-5163-8. [DOI] [PubMed] [Google Scholar]
- 24.Najib H. Pathology and pathogenesis of radiation bowel disease: Histopathological appraisal in the clinical setting. EMJ Gastroenterol. 2018;7:113–9. [Google Scholar]
- 25.Noyes WR, Hosford CC, Schultz SE. Human collagen injections to reduce rectal dose during radiotherapy. Int J Radiat Oncol Biol Phys. 2012;82:1918–22. doi: 10.1016/j.ijrobp.2011.02.034. [DOI] [PubMed] [Google Scholar]
- 26.Otto K. Volumetric modulated arc therapy: IMRT in a single gantry arc. Med Phys. 2008;35:310–7. doi: 10.1118/1.2818738. [DOI] [PubMed] [Google Scholar]
- 27.Athanassiou H, Antonadou D, Coliarakis N, Kouveli A, Synodinou M, Paraskevaidis M, et al. Protective effect of amifostine during fractionated radiotherapy in patients with pelvic carcinomas: Results of a randomized trial. Int J Radiat Oncol Biol Phys. 2003;56:1154–60. doi: 10.1016/s0360-3016(03)00187-1. [DOI] [PubMed] [Google Scholar]
- 28.Linard C, Busson E, Holler V, Strup-Perrot C, Lacave-Lapalun JV, Lhomme B, et al. Repeated autologous bone marrow derived mesenchymal stem cell injections improve radiation-induced proctitis in pigs. Stem Cells Transl Med. 2013;2:916–27. doi: 10.5966/sctm.2013-0030. [DOI] [PMC free article] [PubMed] [Google Scholar]


