Abstract
Objectives:
The aim of the study is to assess the awareness of family medicine residents about influenza and pneumococcal vaccination for high-risk patients and to verify the most significant variables that might affect residents’ knowledge and the tools needed to enhance their practice.
Materials and Methods:
This cross-sectional study was conducted at four major hospitals in Riyadh, Saudi Arabia, during the period, October through December 2017. A pretested self-administered questionnaire was handed to 180 family residents. Descriptive statistics were used to analyze the study data. The Chi-square test was used to compare categorical variables data. The One-way ANOVA test was used to detect the significant difference.
Results:
The overall knowledge of physicians about influenza and pneumococcal vaccines was inadequate and was more toward pneumococcal vaccine, in spite their respectable knowledge about the target population. The main reasons for non- prescribing of vaccines were forgetfulness (59.4%), the availability of vaccines (33.9%), and the patients’ refusal (23.3%). The tools that might help for prescribing were the need for the presence of electronic reminder (69.4%) and the patients should follow a regular family physician (47.2%).
Conclusion:
Knowledge and practice of influenza and pneumococcal vaccination are inadequate. This is mainly because of forgetfulness owing to minimal guideline awareness, lack of vaccine availability, and patients’ refusal. The important recommendations to enhance vaccination practice among physicians are the implementation of electronic reminders, regular follow-up with the same physician in addition to educational programs during residency, and patient education about the importance of vaccinations as a means of disease prevention.
Keywords: Family residents and knowledge, influenza vaccination, pneumococcal vaccination
Introduction
Influenza is renowned as the main cause of morbidity and mortality in the human population that leads to the formation for using vaccines to reduce the subsequent health as well the economic influences. Every year, an estimate of 5 to 10% of adults and 20% to 30% of children's were infected with influenza, which results 3 to 5 million cases of severe disease and approximately 1 million deaths globally.[1,2] The children under the age of 5 years, approximately 826,000 deaths happened due to pneumococcal disease, and out of which, 91,000 were HIV-positive. It was estimated of 14.5 million (11.1 to 18.0 million) severe incidents of pneumococcal disease.[3] During the year 2016, 652,572 deaths (95% uncertainty interval [UI] 586 475-720 612), children below 5 years occurred due to lower respiratory infections, whereas 1, 080, 958 deaths (943 749-1 170 638) in adults older than 70 years, and 2 377 697 deaths (2 145 584-2 512 809) in populations irrespective of their ages, globally.[4] For pneumococcal infections, two vaccines are available. The pneumococcal conjugate vaccine (PCV13) for infants, young children, and adults 65 years or older protects against 13 types of pneumococcal bacteria. The other type, pneumococcal polysaccharide vaccine (PPSV23) for all adults 65 years or older and for those 2 years or older protects against 23 types of pneumococcal bacteria.[5] Both are inactivated vaccines and available in Saudi Arabia. Influenza-related hospitalization was reduced by 70% as a result of vaccination.[6] Approximately, 30-40% reduction in illness incidence was reported in vaccinated elderly in nursing homes[7] and 50-60% reduction in hospitalization. The vaccinated adults were less likely to die than unvaccinated influenza-hospitalized patients.[8] Influenza vaccination among patients with type 2 diabetes was associated with significantly lower admission rates for stroke, heart failure, and pneumonia or influenza, as well as all-cause death, and a non-significant change for acute Myocardial infarction (MI) during the influenza seasons.[9] The Canadian Community Health Survey 2009/2010 reported that the coverage for influenza vaccination was 62.9% in individuals over 64 years and 28.8% in individuals aged 12 years and above, which is considered low coverage.[10] In Saudi Arabia, the available vaccine is a trivalent influenza vaccine, containing inactivated antigens for two different subtypes of influenza viruses (type A) and one subtype of influenza viruses (type B). Physicians have a very important role for the delivery of pneumococcal (PPSV23 vaccine and PCV13 vaccine) and influenza vaccines for high-risk patients.[11,12] The study of Santoli JM concluded that delay of implementation of adult vaccination is owing to many reasons such as poor vaccine supply, lack of physicians’ knowledge, and inadequate access to health services.[13] For the best of our knowledge, no previous studies addressing awareness of primary health care physicians toward influenza and pneumococcal vaccination was conducted before in the Gulf area. The present study was performed to assess the awareness of family medicine residents toward influenza and pneumococcal vaccinations for high-risk individuals and to verify the most significant variables that might affect residents’ knowledge and the tools needed to enhance their practice.
Materials and Methods
This was a cross-sectional study, conducted during the period from October to December 2017. Family physician residents in primary health care centers of four major hospitals namely King Saud University Medical City, Prince Sultan Military Medical City, King Abdulaziz Medical City, and Security Forces Hospital, in Riyadh, Saudi Arabia were invited to participate in the study. The formula for calculating sample size was [N = Z2× (P) x (1–P)/D2], where (P) is the average knowledge from previous studies conducted in this field, which was 58%, and (Z) is constant value (1.96) with 95% confidence interval, for precision with 80% power (D = 0.05). After using this mathematical technique, we needed a minimum of 165 residents to participate in the study. Anticipated non-response rate was 10%.
The questionnaire was developed and modified from previous studies that addressed the same objectives and recommendation of Centers for Disease Control and Prevention (CDC).
Participants were interviewed in person using questionnaires. The questionnaire comprised of 5 sections: (a) socio-demographic data; (b) physicians’ knowledge toward influenza and pneumococcal vaccine; (c) reasons preventing the physician from prescribing vaccination to high-risk patients; (d) the tools that might help in prescribing vaccines for high-risk patients; and finally (e) the target population that requires flu and pneumococcal vaccines.
Eight questions were used to verify residents’ knowledge about influenza vaccine, and nine questions were allocated for pneumococcal vaccine. Each correct answer was designated one point, whereas the wrong answer and “do not know” were given zero. The total knowledge score for influenza vaccine ranged from 1 to 8 points, while that for pneumococcal vaccine ranged from 1 to 9 points.
Participants were informed about the objectives and rationale of the study, and their consent was obtained.
A pilot study was conducted, where 20 questionnaires were distributed for validation purposes regarding feasibility and clarity and the possibility of any changes. The Cronbach's alpha was 84.2%.
Ethical approval
Ethical approval to conduct the study was obtained from the Institution Review Board at King Saud University Medical City.
Data analysis
Descriptive statistics were used to analyze the study data. Categorical variables were presented as number and percentage. The Chi-square test was used to compare categorical variables data. A P value ≤ 0.05 was considered to be statistically significant. The one-way ANOVA test was used to detect the significant difference of the total knowledge scores for influenza and pneumococcal vaccines regarding socio-economic factors.
Results
Out of 203 questionnaires distributed over the family medicine residents in the four hospitals, 180 residents participated with a response rate 88.66%.
The majority of residents (96.7%) were in the age group of 25–29 years. Approximately, half of them were males (51.1%). Their years of experience ranged from 1 to 5 years. Most of them (95%) had experience of less than 5 years.
Residents’ knowledge of influenza vaccine was very poor. The mean of the total influenza knowledge score was 3.8 (1.5). The percentage of correct answers among residents ranged from 22.8% to 72.2%. The two questions with the lowest percentages of correct answers were (1) Patients who had received the influenza vaccine they might get Guillain-Barré syndrome (22.8%); and (2) If individuals with a history of egg allergy who have experienced only hives after exposure to eggs should receive any of the recommended age-appropriate influenza vaccines (28.6%). The question with the highest percentage of correct answers (72.8%) was about the nature of the vaccine, is it live attenuated or inactivated vaccine. Regarding pneumococcal vaccine, the residents’ knowledge was even less when compared to the influenza vaccine. The mean of the total pneumococcal knowledge score was 3.01 (1.5). The percentage of correct answers among residents ranged from 17.2% to 57.2%. The questions with the lowest percentage of correct answers were (1) Whether adults aged ≥65 years who have previously received one dose of PPSV23 also should receive a dose of PCV13 or not (17.2%); and (2) Pneumococcal vaccine could be live attenuated or inactivated vaccine (17.2%). The highest percentage for correct answer, (57.2%), was for the question: should PCV13 and PPSV23 be administered routinely in series to all adults aged ≥65 years?
Tables 1 and 2 illustrate the results of one-way ANOVA test, showing the differences between socio-demographic factors group means with regard to influenza and pneumococci vaccine knowledge scores. There was no significant difference detected with regard to age, (P = 0.15 and P = 0.07). For position and years of experience, the mean knowledge score is increasing with increased years of residency and of experience, where the fourth level residents (R4) and higher years of experience have the highest mean level for the two groups of knowledge; it was significantly different from other levels of residency and years of experience.
Table 1.
One-way ANOVA results, difference between group means of socio-demographic data and flu vaccine knowledge scores
| Factor | Mean SD | F | P |
|---|---|---|---|
| Gender | |||
| Male | 4.1±1.6 | 2.06 | 0.15 |
| Female | 3.7±1.5 | ||
| Residency | |||
| R1 | 3.4±1.9 | 10.3 | 0.00 |
| R2 | 3.5±1.6 | ||
| R3 | 3.6±1.1 | ||
| R4 | 4.9±1.6 | ||
| Year of experience | |||
| Up to 2 years | 3.4±1.7 | 7.1 | 0.001 |
| 2-5 Years | 4.3±1.2 | ||
| >5 years | 3.7±2.1 |
Table 2.
One-way ANOVA results, difference between group means of socio-demographic data and pneumococcal vaccine knowledge scores
| Factor | Mean SD | F | P |
|---|---|---|---|
| Gender | |||
| Male | 3.2±1.3 | 3.2 | 0.07 |
| Female | 2.8±1.7 | ||
| Residency | |||
| R1 | 2.5±1.6 | 11.01 | 0.000 |
| R2 | 2.8±1.2 | ||
| R3 | 2.7±1.2 | ||
| R4 | 4.0±1.6 | ||
| Year of experience | |||
| Up to 2 years | 2.7±1.3 | 3.6 | 0.2 |
| 2-6 Years | 3.2±1.7 | ||
| >5 years | 3.8±1.1 |
Regarding knowledge about the target population, nearly most of them mentioned the correct answer. Most residents 165 (91.6%) reported that they should be diabetic patients, followed by patients with chronic lung disease 107 (59.4%), kidney disease 74 (41.1%), and liver disease 49 (27.2%). Although the patients of hemoglobinopathies and those of morbid obesity are target for vaccination, only the minority of physicians (11% and 9.4%) choose these disorders as a target. Patients with hypothyroidism are not target for vaccination, but this group was added in the questionnaire as a distractor to test the knowledge of physicians. This was reflected by showing that only (4.4%) choose this incorrect target [Figure 1].
Figure 1.
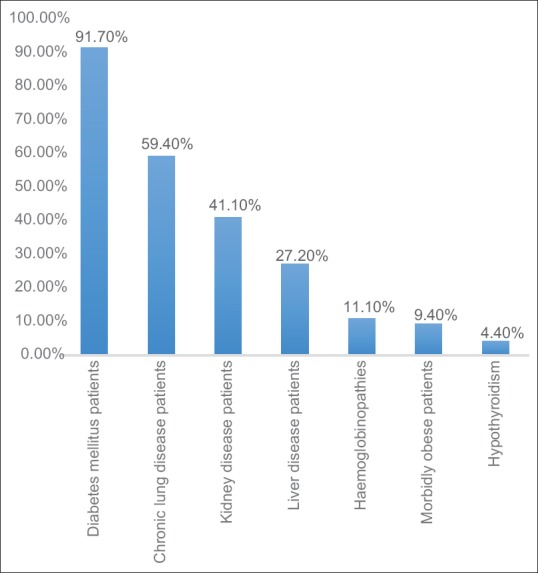
High-risk patients for vaccination as reported by residents
The most common reasons for not prescribing such vaccines to the patients, as mentioned by the residents, were forgetfulness (59.4%) and non-availability of the vaccines (33.9%). In addition to other causes, as lack of knowledge regarding the target population, which vaccines to be give, and lastly, because of the patients’ refusal comprised 32.3%, 29.4%, and 23.3%, respectively [Figure 2].
Figure 2.
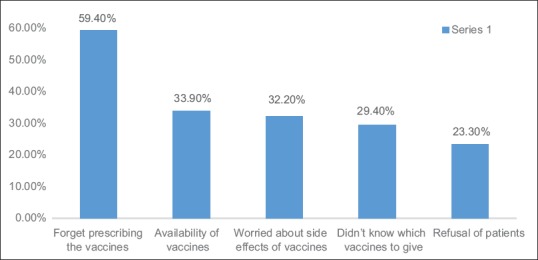
Why family residents are not prescribing influenza and pneumococcal vaccination
The tools that might help for prescribing such vaccines for high-risk patients were the need for presence of electronic reminder about vaccines (69.4%), also near half 93 (51.7%) mentioned that patients should follow a regular family physician, 85 (47.2%) stressed upon the importance of guidelines for special population vaccinations, and lastly, 39 (21.7%) reported the need of brochures to educate patients about the important of the vaccines [Figure 3].
Figure 3.
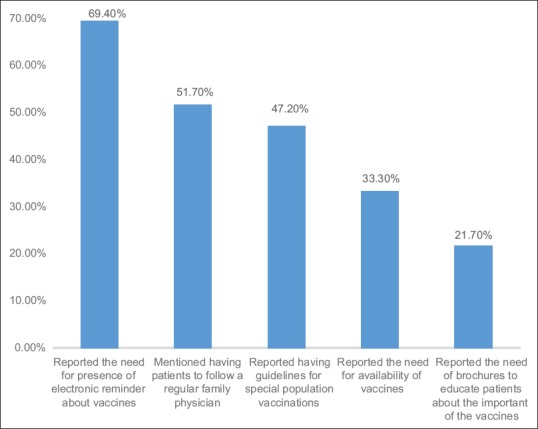
Tools that might help in prescribing vaccines for high-risk patients
Discussion
This study is the first one, which aimed to assess knowledge of family residents about the importance of influenza and pneumococcal vaccines for the high-risk population in Saudi Arabia.
Physicians’ knowledge about the health and cost-effectiveness of the vaccinations strongly influences their recommendation to vaccines. A number of studies reported low coverage of influenza and pneumococcal vaccines for adults and health care workers.[14,15,16,17]
According to the CDC, the coverage of influenza vaccination in 2009/2010 was 69.6% for individuals aged 64 years and above and 41.2% for all ages. The CDC reported that in the first 3 months of 2002, 55% of elderly individuals received pneumococcal vaccines.[18] The reasons for insufficient vaccination for an adult may be attributed to the lack of physicians’ knowledge, lack of adult vaccination national health policy, in addition to concerns about the efficacy and side effects of vaccines and their economic cost.[19,20,21,22]
The majority of the family physician residents in the current study retained respectable information about the target population for whom influenza and pneumococcal vaccines should be prescribed, particularly regarding those with the most common and recommended diseases by guidelines such as diabetes mellitus, which came as the main target, followed by chronic lung diseases, yet their actual practice was poor. Regarding hemoglobinopathies, the response rate as a target people was very low. Sickle cell anemia, which is one of the common hemoglobinopathies in Saudi Arabia should be considered an important target for such vaccination especially for pneumococcal vaccine, unexpectedly the minority of physicians chose them as a target. This could be attributed to their inadequate knowledge regarding influenza vaccines as well as toward pneumococcal vaccines. A study from Lebanon showed that only 58.1% and 53.5% of physicians had accurate knowledge about influenza and pneumococcal vaccines guidelines, respectively, and 61% physicians reported the need for reminders as the most important intervention to promote adult immunization.[23] A study from Saudi Arabia conducted on undergraduate medical students showed that two-thirds of the students knew that influenza vaccination was available. However, most of them were not aware that patients with chronic diseases, pregnant women, elders, auto-immune patients, and extremely obese patients could receive it.[24] Low vaccination rates were reported from South Africa toward seasonal influenza[25] and from Switzerland toward pneumococcal vaccination[26] because of their low priority and missing awareness among physicians and patients.
The knowledge regarding such vaccination can be exhibited by implementing the practice of vaccination and preventive measures that should be applied in the field of family practice as the first defense of health. It was reported in developing countries that doctors knew they needed to update their information but time availability and financial constraints were a barrier. However, they can get the information through internet and scientific meetings.[23] This was supported by a Turkish study, which revealed that increasing the awareness of the physicians improved the pneumococcal and influenza vaccination rates.[27]
Although the study was conducted in four major hospitals, approximately one-third of the residents were not aware of the availability of such vaccines, which might reflect lack of communication between those who dispense the vaccine, such as the pharmacy or the infection control and physicians.
In addition, a quarter of residents mentioned that patients’ refusal could be one of the reasons. These reasons were supported by Romani MH[23] who reported that vaccine availability was the most important barrier for non-prescribing such vaccination followed by patients’ refusal. In addition, patients’ refusal as a barrier was supported by Canova L,[28] where 12% of the elderly patients refused vaccination. This might be due to lack of education among patients regarding the importance of such vaccines.
Forgetfulness was one of the main barriers for recommending influenza and pneumococcal vaccines, which might be related to lack of enforcement of guidelines. For such reason, most of the residents, nearly 70%, recommended an electronic reminder to enhance the prescription of vaccination. This tool was supported by Baykan Z[29] who reported that most of the family physicians, need an electronic reminder, or a vaccination scheme similar to the one used for childhood vaccines to enhance their awareness.
A study by Laura P[30] was conducted in the United State, where primary care physicians were surveyed regarding adult pneumococcal vaccine recommendation. The majority reported that the current recommendations came to be not clear. They reported some barriers to prescribe such as cost of purchasing vaccine, lack of insurance coverage, inadequate reimbursement, and difficulty determining vaccination history. These barriers came to be of another perspective other than reported in our study, but it showed that the lack of implementation of vaccination is a common problem among family physicians. At the same time, they agreed that optimal implementation of these recommendations will require addressing knowledge gaps among family physicians, which also needed as one of the recommendations in our study.
As we mentioned that the principle reasons for non-prescribing the vaccines in the present study were forgetfulness and non-availability of the vaccines. It is highly recommended to establish urgent educational programs for family residents to increase their knowledge about vaccination. The programs should be implemented in the practice, especially for high-risk patients. Furthermore, the recommendation of electronic reminders should be looked at with interest, as all of these hospitals implement the system of electronic files for patient follow-up. In addition, nearly half of family physicians recommended regular follow-up with the same physician, which can enhance the prompt care of patients.
Further qualitative studies are warranted regarding influenza and pneumococcal vaccination to assess physicians’ practice improvement.
We are in need of studying the prevalence of patients receiving the vaccines, and whether physicians’ education along with the electronic reminders could improve their practice.
Conclusion and Recommendation
Knowledge and practice of pneumococcal and influenza vaccination are inadequate among family physician residents. This is mainly owing to forgetfulness as a result of minimal guideline awareness, lack of vaccine availability, and patients’ refusal. The important recommendations to enhance vaccination practice among physicians are the implementation of electronic reminders, regular follow-up with the same physician in addition to educational programs during residency, and patient education about the importance of vaccinations as a means of disease prevention.
Abbreviations
PCV13: Pneumococcal conjugate vaccine; PPSV23: Pneumococcal polysaccharide vaccine; CCHS: Canadian community health survey; TIV: Trivalent influenza vaccine; CDC: Disease control and prevention; IRB: Institution review board; ANOVA: Analysis of variance.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Gordon A, Reingold A. The Burden of influenza: A complex problem. Curr Epidemiol Rep. 2018;5:1–9. doi: 10.1007/s40471-018-0136-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fischer WA, Gong M, Bhagwanjee S, Sevransky J. Global Burden of influenza: Contribution form resource limited and low income settings. Glob Heart. 2014;9:325–36. doi: 10.1016/j.gheart.2014.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Katherine L, O’Brien, colleagues Worldwide burden of disease: Streptococcus pneumoniae and Haemophilus influenza type b in children less than 5 years old. Arch Dis Child. 2010;95:973. [Google Scholar]
- 4.Estimates of the global, regional, and national morbidities of lower respiratory infections in 195 countries, 1990-2016:Asystematic analysis for the Global burden ofA disease study 2016. Lancet Infect Dis. 2018;18:1191–210. doi: 10.1016/S1473-3099(18)30310-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kobayashi M, Bennett NM, Gierke R, Almendares O, Moore MR, Whitney CG, et al. Intervals between PCV13 and PPSV23 vaccines: Recommendations of the Advisory Committee on Immunization Practices (ACIP) MMWR. 2015;64:944–7. doi: 10.15585/mmwr.mm6434a4. [DOI] [PubMed] [Google Scholar]
- 6.Harper S, Fukuda K, Uyeki T, Cox N, Bridges C. Prevention and control of influenza. Recommendations of the advisory committee on immunization practices (ACIP) MMWR Recomm Rep. 2005;54:1–40. [PubMed] [Google Scholar]
- 7.Chiu PJ, Chen CH, Chih YC. Effectiveness of the influenza vaccination program for the elderly in Taiwan. Vaccine. 2013;31:632–8. doi: 10.1016/j.vaccine.2012.11.055. [DOI] [PubMed] [Google Scholar]
- 8.New CDC Study Shows Flu Vaccine Reduces Severe Outcomes in Hospitalized Patients. [Last accessed on 2018 Aug 01]. Available from: https://www.cdc.gov/flu/spotlights/vaccine-reduces-severe-outcomes.htm .
- 9.Vamos EP, Pape UJ, Curcin V, Harris MJ, Valabhji J, Majeed A, Millett C, et al. Effectiveness of the influenza vaccine in preventing admission to hospital and death in people with type 2 diabetes. CMAJ. 2016;188:E342–51. doi: 10.1503/cmaj.151059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Statistics Canada, Canadian Community Health Survey (CCHS). CANSIM table 105 and 0502: Influenza immunization rate within 2013-2014. Statistics Canada, Catalogue no. 82- 624-X. Health at a Glance. 2015 [Google Scholar]
- 11.Zeitouni MO, Al Barrak AM, Al-Moamary MS, Alharbi NS, Idrees MM, Al Shimemeri AA, et al. The Saudi Thoracic Society guidelines for influenza vaccinations. Annals of Thoracic Medicine. 2015;10:223–30. doi: 10.4103/1817-1737.167065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.AlharbiNS, Al-Barrak AM, Al-Moamary MS, Zeitouni MO, Idrees MM, Al-Ghobain MO, et al. The Saudi Thoracic society pneumococcal vaccination guidelines-2016. Ann Thorac Med. 2016;11:93–102. doi: 10.4103/1817-1737.177470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Santoli JM, Peter G, Arvin AM, Davis JP, Decker MD, Fast P, et al. National Vaccine Advisory Committee. Strengthening the supply of routinely recommended vaccines in the United States: Recommendations from the National Vaccine Advisory Committee. JAMA. 2003;290:3122–8. doi: 10.1001/jama.290.23.3122. [DOI] [PubMed] [Google Scholar]
- 14.Maltezou HC, Maragos A, Halharapi T, Karagiannis I, Karageorgou K, Remoudaki H, et al. Factors influencing influenza vaccination rates among healthcare workers in Greek hospitals. J Hosp Infect. 2007;66:156–9. doi: 10.1016/j.jhin.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 15.Ballestas T, McEvoy SP, Doyle J. Healthcare worker influenza vaccination working party. Co-ordinated approach to healthcare worker influenza vaccination in an area health service. J Hosp Infect. 2009;73:203–9. doi: 10.1016/j.jhin.2009.07.028. [DOI] [PubMed] [Google Scholar]
- 16.Mak KK, Yiu YF, Ko KL, Hui KSH, Mak KM, Mak LY, et al. Attitudes and perceptions of influenza vaccination among Hong Kong doctors and medical students before the 2009 pandemic. Eur J Public Health. 2012;23:257–62. doi: 10.1093/eurpub/cks014. [DOI] [PubMed] [Google Scholar]
- 17.Bednarczyk RA, Chu SL, Sickler H, Shaw J, Nadeau JA, McNutt LA, et al. Low uptake of influenza vaccine among university students: Evaluating predictors beyond cost and safety concerns. Vaccine. 2015;33:1659–63. doi: 10.1016/j.vaccine.2015.02.033. [DOI] [PubMed] [Google Scholar]
- 18.Setse RW, Euler GL, Gonzalez-Feliciano AG, Bryan LN, Furlow C, Weinbaum CM, et al. Centers for disease control and prevention (CDC). Influenza vaccination coverage-United States, 2000-2010. MMWR Surveill Summ. 2011;60(Suppl):38–41. [PubMed] [Google Scholar]
- 19.MülerDandSzucs TD. Influenza vaccination coverage rates in 5 European countries: A population-based cross- sectional analysis of the seasons 02/03, 03/04 and 04/05. Infection. 2007;35:308–19. doi: 10.1007/s15010-007-6218-5. [DOI] [PubMed] [Google Scholar]
- 20.Abramson ZH, Levi O. Influenza vaccination among primary healthcare workers. Vaccine. 2008;26:2482–9. doi: 10.1016/j.vaccine.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 21.Blank PR, Schwenkglenks M, Szucs TD. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health. 2008;8:1–13. doi: 10.1186/1471-2458-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ClarkeTC, Ward BW, Freeman G, Schiller JS. Centers for Disease Control and Prevention. Early release of selected estimates based on data from national health interview survey, 2015. United State Department of Health and Human Services. Centers for Disease Control and Prevention. National Center for Health Statistics. Released. 2016 [Google Scholar]
- 23.Romani MH, Musharrafieh UM, Lakkis NA, Hamadeh GN. Family physicians beliefs and attitudes regarding adult pneumococcal and influenza immunization in Lebanon. Fam Pract. 2015;28:632–7. doi: 10.1093/fampra/cmr038. [DOI] [PubMed] [Google Scholar]
- 24.Unis A, Almutairi S, Almutairi M, Alsayed S, Almutairi A. Awareness about seasonal influenza vaccine among undergraduate medical students in Tabukregion, Saudi Arabia. Am J Adv Med Surg Res. 2015;1:62–6. [Google Scholar]
- 25.Anerney JM, Walaza S, Cohen AL, Tempia S, Buys A, Venter M, et al. Effectiveness and knowledge, attitudes and practices of seasonal influenza vaccine in primary healthcare settings in South Africa, 2010-2013. Influenza Other Respir Viruses. 2015;9:143–50. doi: 10.1111/irv.12305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Badertscher N, Morell S, Rosemann T, Tanjung R. General practitioners’ experiences, attitudes, and opinions regarding the pneumococcal vaccination for adults: Aqualitative study. Int J Gen Med. 2012;5:967–74. doi: 10.2147/IJGM.S38472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Satman I, Akalin S, Cakir B, Altinel S diaVAX Study Group. The effect of physicians’ awareness on influenza and pneumococcal vaccination rates and correlates of vaccination in patients with diabetes in Turkey: An epidemiological Study “diaVAX”. Hum Vaccin Immunother. 2013;9:2618–26. doi: 10.4161/hv.25826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Canova L, Birchmeier M, D’Acremont V, Abetel G, Favrat B, Landry P, et al. Prevalence rate and reasons for refusals of influenza vaccine in elderly. Swiss Med Wkly. 2003;133:598–602. doi: 10.4414/smw.2003.10395. [DOI] [PubMed] [Google Scholar]
- 29.Baykan Z, Nacar M, Ozdemir SB, Poyrazoǧlu S, Çetinkaya F. Knowledge and attitude of family physicians regarding adult vaccination. World J Vaccines. 2011;1:92–7. [Google Scholar]
- 30.Hurley LP, Allison MA, Pilishvili T, O’Leary ST, Crane LA, Brtnikova M, et al. Primary care physicians’ struggle with current adult pneumococcal vaccine recommendations. J Am Board Fam Med. 2018;31:94–104. doi: 10.3122/jabfm.2018.01.170216. [DOI] [PMC free article] [PubMed] [Google Scholar]


