Abstract
Background:
Delirium is a common and distressing neurocognitive condition that frequently affects patients in palliative care settings and is often underdiagnosed.
Aim:
Expanding on a 2013 review, this systematic review examines the incidence and prevalence of delirium across all palliative care settings.
Design:
This systematic review and meta-analyses were prospectively registered with PROSPERO and included a risk of bias assessment.
Data sources:
Five electronic databases were examined for primary research studies published between 1980 and 2018. Studies on adult, non-intensive care and non-postoperative populations, either receiving or eligible to receive palliative care, underwent dual reviewer screening and data extraction. Studies using standardized delirium diagnostic criteria or valid assessment tools were included.
Results:
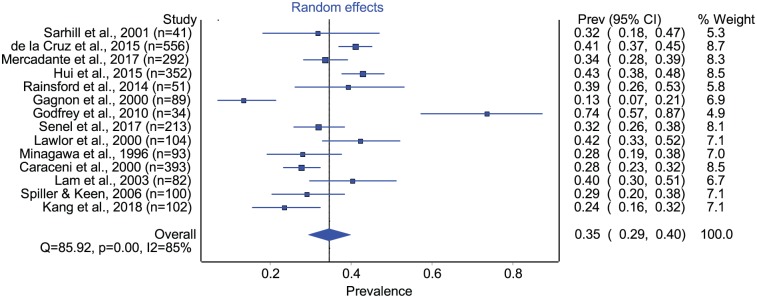
Following initial screening of 2596 records, and full-text screening of 153 papers, 42 studies were included. Patient populations diagnosed with predominantly cancer (n = 34) and mixed diagnoses (n = 8) were represented. Delirium point prevalence estimates were 4%–12% in the community, 9%–57% across hospital palliative care consultative services, and 6%–74% in inpatient palliative care units. The prevalence of delirium prior to death across all palliative care settings (n = 8) was 42%–88%. Pooled point prevalence on admission to inpatient palliative care units was 35% (confidence interval = 0.29–0.40, n = 14). Only one study had an overall low risk of bias. Varying delirium screening and diagnostic practices were used.
Conclusion:
Delirium is prevalent across all palliative care settings, with one-third of patients delirious at the time of admission to inpatient palliative care. Study heterogeneity limits meta-analyses and highlights the future need for rigorous studies.
Keywords: Delirium, palliative care, incidence, prevalence, systematic review
What is already known about the topic?
Delirium is a common, neuropsychiatric disorder that causes significant distress to patients and caregivers, affects patient quality of life, and leads to prolonged hospital stays and increased health care costs.
A 2013 systematic review revealed that delirium is highly prevalent in the acute inpatient palliative care setting, but the rate of occurrence in other palliative care settings such as the palliative care consultative setting, general inpatient setting, and community settings is not well understood.
There are many validated tools to screen for and diagnose delirium in palliative care patients; however, no consensus exists as to the optimal tools or diagnostic practices.
What this paper adds?
This paper also includes new estimates of delirium occurrence in general inpatient settings, palliative care consultative settings, and community settings.
This review is the first to conduct a meta-analysis of delirium prevalence in palliative care, which identified that one-third of patients experience delirium at the time of admission to inpatient palliative care units.
A formal risk of bias assessment of all studies revealed only one study with an overall low risk of bias. Substantial variability in delirium diagnostic and screening practices may contribute to significant bias in studies of delirium.
Implications for practice, theory, or policy
This review illustrates that delirium is highly prevalent across all palliative care settings, with one-third of patients experiencing delirium at the time of admission to acute palliative care.
The timely and accurate recognition of delirium both in clinical practice and in future research studies is crucial.
The review also identifies a gap in knowledge with respect to optimal delirium screening and diagnostic practices and provides a foundation on which research can be built.
Introduction
Delirium is an acute, complex, neurocognitive syndrome that commonly complicates medical illness. It is associated with impaired decision making and often causes significant distress to patients and their caregivers.1–3 Across health care settings, delirium is known to contribute to increased patient morbidity and mortality4,5 and is associated with longer hospital stays and increased health care costs.6,7 Delirium frequently occurs in association with acute, often reversible, precipitating events such as infection and dehydration. In the palliative care population, these precipitating events are often superimposed on an underlying vulnerability that accompanies advanced disease. In addition to contributing to patient and caregiver distress, delirium frequently necessitates inpatient admission for care or complicates the care of an existing inpatient. In some cases, this may progress to a terminal, refractory delirium at end of life.8 Although delirium is highly prevalent in palliative care settings, its occurrence is often not recognized and is poorly documented.9,10
Standard consensus criteria such as the International Classification of Diseases (ICD)11 and Diagnostic and Statistical Manual of Mental Disorders (DSM)12 exist to aid physicians in the diagnosis of delirium. There have been multiple editions and updates of these gold standard criteria to reflect diagnostic advances. The original (DSM-I) and the most recent (DSM-5) editions were published in 1980 and 2013, respectively. Various tools have been developed to operationalize these criteria, particularly those of DSM, and facilitate delirium diagnosis and screening in clinical practice. Although many of these tools, such as the Confusion Assessment Method (CAM),13 are validated in palliative care settings, no clear consensus exists as to the superior tool or the optimal frequency of delirium assessments. Consequently, the utility of these tools in clinical practice remains highly variable.14–16
Delirium can be further classified into psychomotor subtypes such as hypoactive, hyperactive, and mixed (both hypo- and hyperactive features).17,18 Normal (no psychomotor disturbance) subtype19 and subsyndromal delirium20 (the presence of some features of delirium while not clinically meeting diagnostic criteria) have also been described. Researchers have posited that hypoactive delirium, while common, is largely underdiagnosed, particularly due to overlapping clinical similarities with dementia and depression.21,22 Thus, the importance of screening for delirium and the use of both clear documentation and diagnostic tools are considered pivotal.15
Past reviews of delirium and its assessment in palliative care have examined the incidence and prevalence rates of delirium in this population.8,23,24 Previously, a systematic review with eight included studies reported incidence and prevalence data from exclusively acute inpatient palliative care settings.8 However, the palliative care context and population is not limited to the inpatient palliative care setting, and patients are often managed by specialist palliative care clinicians and generalists in both inpatient and outpatient settings. Currently, our awareness of how the incidence, prevalence, and clinical manifestations of delirium vary across these care settings is limited.25 A formal knowledge synthesis of these domains will guide screening and diagnosis, in addition to identifying potential areas in which to focus future preventive and management strategies.
Following an initial scoping review of delirium in palliative care settings,26 we undertook a systematic review with the aims of (1) estimating the incidence and prevalence of delirium in the adult palliative care population across health care settings, and (2) determining whether the incidence or prevalence of delirium varies by the clinical setting, the psychomotor sub-classification of delirium, patient factors, the proximity to death, delirium diagnostic criteria, study methodology, or study duration.
Methods
This systematic review protocol was developed using the Joanna Briggs Institute Guide for conducting a systematic review of incidence and prevalence data.27 Data are reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline.28 The protocol was prospectively registered with PROSPERO.29
Search strategy
The comprehensive search strategy consisted of peer-reviewed articles obtained from MEDLINE, EMBASE, CENTRAL, PsycINFO, and CINAHL electronic databases. It was validated by performing a Peer Review of the Electronic Search Strategy (PRESS), and records were initially retrieved on 21 November 2017 and updated on 15 March 2019. The search was limited to articles published after 1980, as no standardized diagnostic criteria for delirium existed prior to DSM-I. A hand-search of reference lists from included studies was also performed. In the search strategy, Medical Subheadings (MeSH) captured “delirium” and “palliative care” and their associated derivatives (Supplemental Table 1). More specific epidemiological terms such as “incidence” and “prevalence” were not used to ensure inclusion of a wider scope of articles in primary screening.
Study selection
Titles, abstracts, and full texts of studies identified through the literature search were uploaded into DistillerSR software.30 Two reviewers (P.G.L. and C.L.W.) independently performed title and abstract (Level 1) and full-text (Level 2) screening to determine study eligibility. Studies that did not meet a priori eligibility criteria were excluded, and the single best reason for exclusion at Level 2 screening was recorded. Conflicts at Level 1 and Level 2 screening were discussed and resolved without optional third-party arbitration.
Cross-sectional, cohort, nested-case control and experimental studies were included if they contained relevant epidemiological data on adult patients with delirium in any palliative care setting (as defined by Lawlor et al.26). Studies were excluded if they did not use standard delirium diagnostic criteria (such as the DSM) or a validated diagnostic tool (such as the CAM), if they were published prior to 1980, or if they focused on alcohol withdrawal delirium. Studies performed in the post-operative and intensive care unit settings were also excluded, as were studies published in a language other than English and studies for which full text was unavailable.
Data extraction and risk of bias assessment
Two reviewers (P.G.L. and C.L.W.) independently extracted general study and population characteristics, settings, and relevant epidemiological data from included studies using predesigned and piloted forms in DistillerSR software.30 A risk of bias tool was developed to examine the potential selection, detection, attrition, and analytic biases specific to the unique nature of studies focused on delirium in palliative care populations (Supplemental Table 2). This tool was also integrated into DistillerSR software, and each study underwent dual, independent assessment for risk of bias. Included studies were also assessed for applicability to the general palliative care population.
Data analyses/reporting
Incidence and prevalence data were pooled when heterogeneity between studies was minimal or could not be explained by clinical or methodological differences. Cochrane Q and I² values were used to quantify heterogeneity in addition to the χ² test for its statistical significance. A random effects model was used to formally generate pooled estimates of the point prevalence of delirium in inpatient palliative care units. When meta-analyses were not possible, incidence and prevalence data were synthesized narratively and presented as median summary estimates and associated range.
Results
Selection of relevant studies
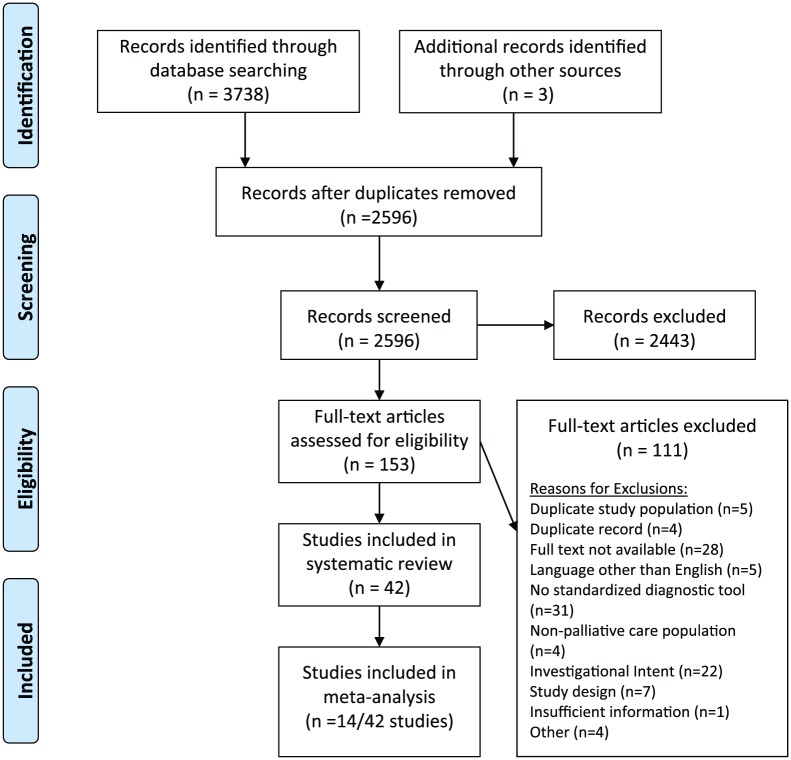
The initial search strategy identified 3031 records, with another three records identified via handsearching. The updated literature search on 15 March 2019 identified an additional 707 records published up to 31 December 2018. The sequential processes of record identification, screening, and data extraction are summarized in the PRISMA diagram (Figure 1). After the removal of duplicates, 2596 records were subject to title and abstract screening, and 153 of these underwent full-text screening. Of the 111 studies excluded during full-text review, 31 did not employ standard delirium diagnostic criteria and 22 were excluded as the investigational intent of the paper did not allow for epidemiological data to be obtained. One record lacked sufficient information to determine eligibility, and five were published in a language other than English. Full text was unavailable for 28 records. Duplicate study populations were used in five studies, and in these cases, the first published studies were included in the review and the remaining studies excluded. Ultimately, 42 studies met the eligibility criteria for study inclusion (Supplemental Table 3).
Figure 1.
PRISMA flowchart of studies included in systematic review.
Study demographics
An aggregate summary of the 42 included studies is shown in Table 1, and individualized study summaries are available in Supplementary Table 3. The included studies originated from 13 different countries, with the majority (n = 20) from North America. Twenty-six studies were conducted in a single-center, specialist palliative care unit, based in a hospital (n = 12), a cancer center (n = 7) or a residential hospice (n = 7). Of the remaining studies, most (n = 7) involved inpatient medical or oncology patients in which a specialist palliative care team was consulted. Three studies were based in the community.
Table 1.
Care settings of included records.
| Study characteristics | Number of studies, n = 42 (%) |
|---|---|
| Geographic region | |
| USA31–42 | 12 |
| Canada43–50 | 8 |
| Italy51–54 | 4 |
| UK55–57 | 3 |
| Japan58–60 | 3 |
| Australia61,62 | 2 |
| Ireland63,64 | 2 |
| South Korea65,66 | 2 |
| Germany67 | 1 |
| Hong Kong68 | 1 |
| Belgium69 | 1 |
| Taiwan70 | 1 |
| Turkey71 | 1 |
| Multiple countries72 | 1 |
| Care setting | |
| Single unit palliative care | |
| Hospital-based46,53,54,59,62,65–71 | 12 (28) |
| Hospice-based33,34,43,55,61,63,64 | 7 (17) |
| Cancer center–based32,35,37,40,50,52,72 | 7 (17) |
| >1 inpatient palliative care setting44 | 1 (2) |
| Other palliative care settings | |
| Community palliative care31,38,48 | 3 (7) |
| Medical/Oncologyinpatients36,41,42,47,49,56,60 | 7 (17) |
| Both inpatient and outpatient settings39,51 | 2 (5) |
| Other care settings45,57,58 | 3 (7) |
Among the 42 included studies, some described epidemiological information in more than one care setting.45,57,58 As a result, data from 46 discrete study populations were obtained (Table 2), with a total of 16,491 palliative care patients included across all studies. Of the included study populations, 34 had >90% of the study subjects with a cancer diagnosis; another 7 had a heterogeneous mix of cancer and non-cancer diagnoses. One study population focused solely on patients with AIDS. The majority of study populations were not selected for age or gender. Patients with pre-existing cognitive impairment (presence of underlying dementia) were included in 17 study populations and excluded in 4 study populations. In 25 of the study populations, pre-existing cognitive impairment status (presence or absence of dementia) was not reported.
Table 2.
Study demographics of included study populations (total 46 distinct study populations described in 42 included studies).
| Study population characteristics | Number of distinct study populations, n = 46 (%) |
|---|---|
| Palliative care diagnosis | |
| ⩾90% cancer | 34 (74) |
| Mix of cancer and non-cancer diagnoses | 7 (15) |
| AIDS | 1 (2) |
| Other | 1 (2) |
| Not reported/Unknown | 3 (7) |
| Patient demographics | |
| Age | |
| Age mixed | 41 (89) |
| Not reported/Unknown | 5 (11) |
| Gender | |
| Gender mixed | 42 (91) |
| ⩾80% male | 1 (2) |
| ⩾80% female | 0 |
| Not reported/Unknown | 3 (7) |
| Pre-existing cognitive impairment | |
| Included in study | 17 (37) |
| Excluded from study | 4 (9) |
| Unknown or not assessed | 25 (55) |
Delirium diagnosis
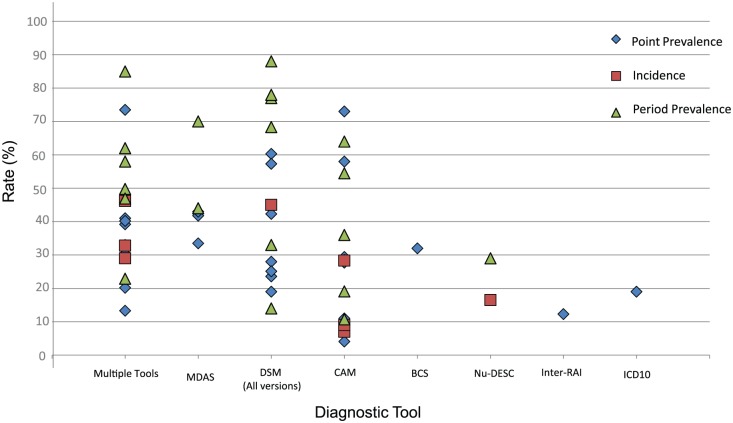
A total of 17 different delirium diagnostic tools were used among the 42 included studies: 27 studies used more than one tool to diagnose delirium and 15 studies relied on a single tool. Of the diagnostic tools used, the CAM was most frequently used (n = 17), followed by DSM-IV (n = 10). DSM criteria of any kind (DSM-III to DSM-5) were used in 21 studies. The epidemiological data obtained from each diagnostic tool are shown in Figure 2.
Figure 2.
Delirium incidence and prevalence rate by diagnostic tool used.
MDAS: Memorial Delirium Assessment Scale; DSM: Diagnostic and Statistical Manual of Mental Disorders; CAM: Confusion Assessment Method; BCS: Bedside Confusion Scale; Nu-DESC: Nursing Delirium Screening Scale; ICD: International Classification of Diseases.
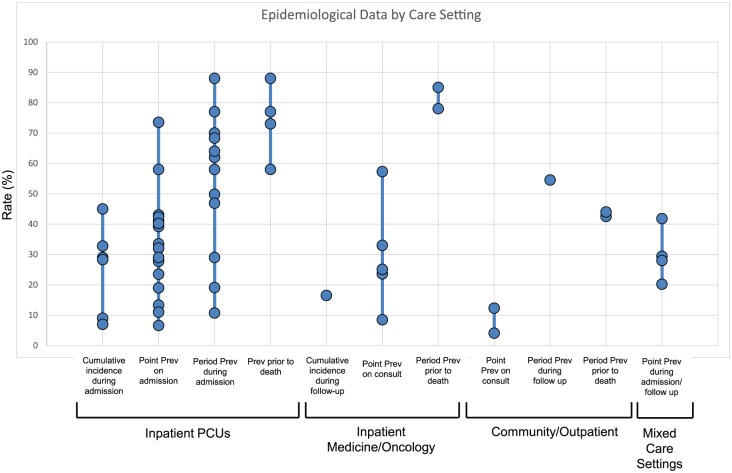
Assessment of epidemiological data
The incidence and prevalence of delirium in studies across various care settings are depicted in Figure 3.
Figure 3.
Incidence and prevalence of delirium across palliative care settings.
Prev: prevalence.
Inpatient palliative care settings
Epidemiological data were extracted from studies in 23 inpatient palliative care settings; 12 were hospital-based,46,53,54,59,62,65–71 7 were in inpatient hospices,33,34,43,55,61,63,64 and 7 were in acute palliative care units within a cancer center.32,35,37,40,50,52,72 The median (range) cumulative incidence of delirium in inpatient palliative care units during the entire admission was 29% (7%–45%).37,44,46,55,57,66 Length of stay in relation to cumulative incidence was represented by a wide range of median values. Delirium incidence rate during admission was estimated in one study at 25.4/1000 person-days.44 The point prevalence of delirium on admission was recorded in 18 different study populations35,37,40,44,46,52–55,57,59,61,63,64,66,68,71,72 with a median (range) of 32% (6.6%–73%). The median (range) period prevalence during the course of an entire inpatient admission was 60% (19%–88%, n = 11 studies, 12 distinct populations),33,37,44–46,50,55,67,70–72 noting again that a wide range of median and mean lengths of stays were reported.
Inpatient settings involving palliative care consultation
Of the seven studies in inpatient settings where palliative care services were consulted, five were conducted in general medical inpatients41,47,49,60,56 and two in oncology inpatients.36,42 The cumulative incidence of delirium was reported in one study as 16.5%.49 The median (range) point prevalence of delirium reported at the time of initial palliative care consultation was 25% (9%–57%).36,41,47,56,60
Community palliative care
Point prevalence of delirium on initial community assessment was reported in the range of 4%–12% in two studies.38,48 The period prevalence of delirium throughout the course of community follow-up (median length of 81 days) was 55% in one study.38
Prior to death
In the inpatient palliative care setting, the median (range) period prevalence of delirium prior to death was 75% (58%–88%) in four distinct study populations (reported in three studies).45,50,68 In two studies of the inpatient setting with palliative care consultation, delirium at end of life was reported in the range of 78%–85%;42,45 whereas in the community setting, a lower range of 42.5%–44% was reported, also in two studies.31,38 Of note, there was variability in the time of delirium assessment prior to death. While some studies reported delirium prevalence at the time of death50 or in the last week of life,31,68 other studies did not clarify the timing of assessments in the “prior to death” interval.38,45
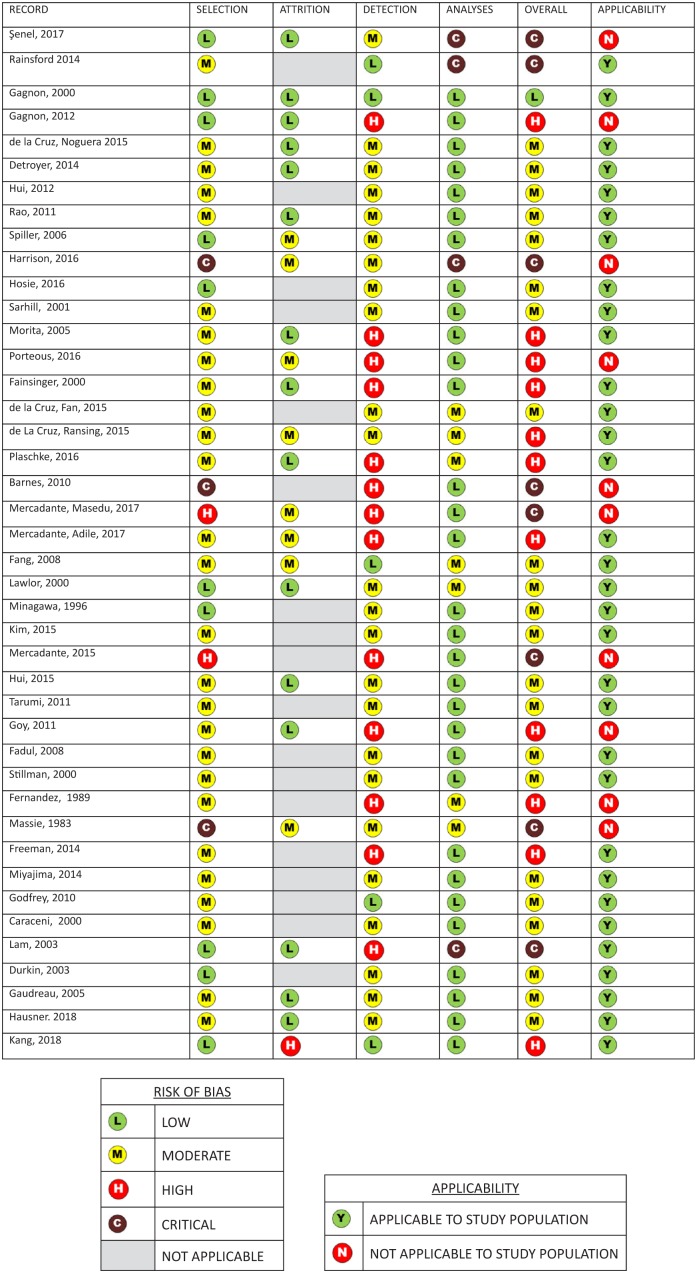
Risk of bias
The results of the risk of bias and validity assessments are presented in Figure 4. Remarkably, only one study had a low risk of bias as determined by the risk of bias tool (Supplementary Table 2). The remaining studies were rated as having moderate (n = 22), high (n = 11), and critical (n = 8) risk of bias. The most frequent area in which risk of bias was introduced was detection (delirium diagnosis), with 13 studies (33%) scoring high risk of bias in this area. Study population findings were considered applicable to the general adult palliative care population, as defined in the study protocol,29 in 32 studies (76%).
Figure 4.
Risk of bias of included studies and applicability to defined study population. Results of risk of bias and applicability assessment as outlined in Supplemental Table 2.
Meta-analyses
Fourteen studies were included in meta-analyses. All of these studies reported the point prevalence of delirium upon admission to an inpatient palliative care unit, consisted of >90% of patients with a cancer diagnosis, and were not selected for age or gender. The relevant inpatient palliative care units consisted of inpatient hospices (n = 4), palliative care units in a tertiary care hospital (n = 6), and palliative care units in a cancer center (n = 4). Due to insufficient reporting of other pre-specified covariate data and limited number of studies in the meta-analysis, further exploration of heterogeneity was not possible. Considering this heterogeneity as unexplained, pooled point prevalence across the included studies yielded a point prevalence estimate of 35% (95% confidence interval (CI) = 0.29–0.40) at inpatient admission, with high heterogeneity between studies (I2 = 85%) (Figure 5). Inter-study heterogeneity was not secondary to care setting or overall risk of bias. When outlier studies43,63 were removed from meta-analyses, there was minimal change in pooled point prevalence, but some improvement in overall heterogeneity was noted (point prevalence = 34%, 95% CI = 0.30–0.39, I2 = 74%, n = 12 studies).
Figure 5.
Meta-analyses of delirium point prevalence at the time of admission to inpatient palliative care units (n = 14 studies, 2502 total patients).
Delirium subtypes
The psychomotor subtypes of delirium were reported in 11 studies, with median rates (range) of hypoactive and hyperactive delirium reported as 39% (22%–86%) and 14% (0%–33%), respectively.35–37,57,61,65–68,70,71 Mixed delirium was reported in 10 distinct study populations in nine studies, with a median prevalence (range) of 23% (10%–45%).36,37,57,65–68,70,71 The prevalence of subsyndromal delirium was reported in one study population as 9.8%.61 One study also reported “level of alertness” as normal in 46% of delirious patients.35
Discussion
Main findings of the study
Drawing from a richer pool of estimates, this study updated and expanded on the 2013 systematic review by Hosie et al., which included eight studies and examined the incidence and prevalence of delirium in patients specifically admitted to inpatient palliative care units and hospices.8 The inclusion of 34 additional studies in the current systematic review not only generates updated estimates in inpatient palliative care patients but also identifies novel information with regard to the occurrence rates of delirium in general inpatient settings and in the community setting. In addition, this review includes a formal risk of bias assessment for all studies. To our knowledge, it is the first systematic review to formally conduct a risk of bias assessment as it pertains to the diagnosis and monitoring of delirium in palliative care settings. Moreover, the included studies allowed for a limited meta-analysis of their data, identifying a pooled point prevalence of delirium on admission to inpatient palliative care units. These findings enhance our knowledge of the epidemiological burden of delirium across multiple care settings. Such estimates will in turn prove useful in informing the design of future primary research studies, particularly regarding sample size estimation.
Ultimately, the results of this study demonstrate that delirium is highly prevalent across all palliative care settings. In general, the prevalence of delirium tends to be lowest at the time of admission, rises during follow-up, and is most highly prevalent prior to death, with a rate reported up to 88%. Pooled prevalence estimates indicate that one-third (35%) of patients are diagnosed with delirium at the time of admission to inpatient palliative care. These estimates are of great relevance, as delirium is often under-recognized and under-reported.9,10 It highlights the potential need for delirium screening and the importance of timely recognition of delirium in palliative care.
Interestingly, the overall prevalence of delirium in the community appears to be lower than in inpatient settings. This may relate to a more de-institutionalized, familiar, and less disorienting setting of care. In the community, there tends to be less medical intervention (such as intravenous lines and catheters), and accepted non-pharmacological prevention strategies (such as maintaining sleep hygiene and limiting noise)15,73 are often more easily prioritized and achieved. In addition, patients managed at home may be less complex, requiring lower doses of opioids and other medications. Alternatively, the lower rate of delirium in the community may suggest that delirium prompts a crisis admission to hospital or inpatient hospice and that increasing care burdens and behavioral challenges make staying at home a less viable option for delirious patients and their caregivers.74
Strengths and limitations of the study
Although this study presents novel information with regard to delirium rates across multiple care settings, there are some important limitations. Contrary to the 2013 systematic review by Hosie et al.,8 this review included studies in which the primary study aim was not to examine the incidence or prevalence of delirium but nonetheless obtain epidemiological data from a representative palliative care population using validated delirium diagnostic tools. This may result in a wider range of reported delirium occurrence rates, as the methodological rigor pertaining to delirium diagnosis is increasingly varied when compared to the 2013 systematic review. There are also challenges with the reporting of epidemiological data in these studies, as the majority report a proportion of patients with delirium or discrete numerical rate without confidence intervals. In addition, in the current review, there is significant heterogeneity among the included studies with respect to diagnostic tools, assessment intervals, and the reporting of longitudinal data. For example, the length of patient stays was reported as a wide range of medians and means, with some studies not reporting length of stay at all. This heterogeneity among studies significantly limited further pooling of delirium epidemiological data, and apart from one pooled estimate, epidemiological data in this review are crudely summarized using median figures with associated ranges rather than formally pooled data.
Fourteen studies were included in the meta-analyses of point prevalence data at the time of admission to inpatient palliative care units. These studies were deemed sufficiently homogeneous for inclusion with regard to care setting and patient demographic information. However, meta-analyses revealed a high I2 value (85%), suggesting that additional variables are contributing to inter-study heterogeneity. This heterogeneity is potentially due to variability among diagnostic tools used, screening practices and training of team members, as well as important patient factors such as performance status, risk factors for delirium (such as pre-existing cognitive impairment), and goals of care. Unfortunately, there was inconsistent reporting of these covariate factors, which limited further assessment.
The ability to perform further meta-analyses on gathered data is limited by the higher rates of bias across the included studies. Ultimately, only one study scored a low risk of bias in all potential areas.44 Bias appeared to be introduced most commonly during the diagnosis of delirium (detection bias); however, concerns with selection bias were also highlighted. Only 10 of the included studies scored low with respect to selection bias.43,44,46,57,59,62,64,66,68,71 In these studies, demographics such as age, gender, and primary diagnoses were reported, in addition to disclosing the pre-existing cognitive impairment status of the study population. As underlying dementia is a strong predisposing factor in the development of delirium,75,76 it ought to be considered when evaluating the epidemiological data presented in each study population. Neglecting to adjust for this confounding variable may contribute to falsely higher rates of delirium in some study populations. The lack of consistently reported cognitive impairment data identifies a need to determine the strength of pre-existing cognitive impairment as a risk factor for the occurrence of delirium in palliative care.
What this study adds
This review provides a foundation on which to plan and design future delirium studies: for example, incidence data are critical in informing the design of prevention studies. It again highlights a previously identified gap in knowledge with respect to the role of delirium screening and diagnostic strategies.14,15,25 Among the 42 included studies, a wide variety of screening and diagnostic practices were employed. Nearly all included studies (n = 36) performed some form of screening for delirium; however, the frequency of screening and screening tools varied substantially, with a total of 10 different screening tools used across the 36 studies.31,33–40,42–51,53–57,59,61–64,66–72
This illustrates a need to further evaluate delirium diagnostic and screening strategies in palliative care settings, including their comparative metrics and burden, as well as their validity compared to a reference standard. A systemic review of the utility of delirium diagnostic and screening tools in palliative care settings would help to inform both the development of clinical practice guidelines on delirium assessment and the need for further primary studies.
Conclusion
This systematic review has revealed that delirium is highly prevalent in palliative care across all care settings. Data have shown that a median (range) of 60% of patients developed delirium throughout an admission to inpatient palliative care, and a meta-analysis has shown that 35% of patients were delirious at the time of admission to inpatient palliative care. In the inpatient consultative setting, the median (range) point prevalence of delirium was found to be 25% (9%–57%) at the time of inpatient palliative care consult. Overall, delirium appears to be less prevalent in the community setting, with the point prevalence reported as 4%–12% at the time of community palliative care consultation. In all care settings, delirium is most prevalent prior to death. Hypoactive delirium is the most prevalent psychomotor subtype, followed by mixed delirium. This review also demonstrates the challenges encountered in knowledge synthesis, particularly in relation to the multiplicity of validated delirium diagnostic tools and varied clinical assessment practices, thus highlighting a need for increasingly rigorous and unbiased primary studies of delirium in the various clinical contexts and settings in which palliative care is delivered. Ultimately, the findings of this review provide a foundation on which future studies requiring the identification of delirium can be designed and planned.
Supplemental Material
Supplemental material, 854944_supp_mat_1 for The incidence and prevalence of delirium across palliative care settings: A systematic review by Christine L Watt, Franco Momoli, Mohammed T Ansari, Lindsey Sikora, Shirley H Bush, Annmarie Hosie, Monisha Kabir, Erin Rosenberg, Salmaan Kanji and Peter G Lawlor in Palliative Medicine
Supplemental Material
Supplemental material, 854944_supp_mat_2 for The incidence and prevalence of delirium across palliative care settings: A systematic review by Christine L Watt, Franco Momoli, Mohammed T Ansari, Lindsey Sikora, Shirley H Bush, Annmarie Hosie, Monisha Kabir, Erin Rosenberg, Salmaan Kanji and Peter G Lawlor in Palliative Medicine
Supplemental Material
Supplemental material, 854944_supp_mat_3 for The incidence and prevalence of delirium across palliative care settings: A systematic review by Christine L Watt, Franco Momoli, Mohammed T Ansari, Lindsey Sikora, Shirley H Bush, Annmarie Hosie, Monisha Kabir, Erin Rosenberg, Salmaan Kanji and Peter G Lawlor in Palliative Medicine
Acknowledgments
The authors wish to thank Dr C. Webber for assistance with technical support.
Footnotes
Author contributions: C.L.W. conducted primary and secondary screening, provided methodological support, and helped with PROSPERO registration, manuscript preparation, and data analysis. P.G.L. conducted primary and secondary screening, provided methodological support, and helped with critical appraisal and preparation of manuscript. M.K. helped with manuscript preparation and critical appraisal of manuscript. S.H.B., F.M., M.T.A., A.H., S.K., and E.R. provided methodological support and helped with critical appraisal of manuscript. L.S. helped with development of search criteria/MESH terms and critical appraisal of manuscript, and obtained records from search.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was funded in part by the Gillin Family and Bruyère Foundation Clinician Scientist Fund for Dr PG. Lawlor.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs: Christine L Watt  https://orcid.org/0000-0002-6361-8815
https://orcid.org/0000-0002-6361-8815
Annmarie Hosie  https://orcid.org/0000-0003-1674-2124
https://orcid.org/0000-0003-1674-2124
Monisha Kabir  https://orcid.org/0000-0002-4456-7661
https://orcid.org/0000-0002-4456-7661
References
- 1. Brajtman S. The impact on the family of terminal restlessness and its management. Palliat Med 2003; 17(5): 454–460. [DOI] [PubMed] [Google Scholar]
- 2. Namba M, Morita T, Imura C, et al. Terminal delirium: families’ experience. Palliat Med 2007; 21(7): 587–594. [DOI] [PubMed] [Google Scholar]
- 3. Bruera E, Bush SH, Willey J, et al. Impact of delirium and recall on the level of distress in patients with advanced cancer and their family caregivers. Cancer 2009; 115(9): 2004–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Salluh JI, Wang H, Schneider EB, et al. Outcome of delirium in critically ill patients: systematic review and meta-analysis. BMJ 2015; 350: h2538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Witlox J, Eurelings LS, de Jonghe JF, et al. Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 2010; 304(4): 443–451. [DOI] [PubMed] [Google Scholar]
- 6. Leslie DL, Inouye SK. The importance of delirium: economic and societal costs. J Am Geriatr Soc 2011; 59(Suppl. 2): S241–S123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Leslie DL, Marcantonio ER, Zhang Y, et al. One-year health care costs associated with delirium in the elderly population. Arch Intern Med 2008; 168(1): 27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hosie A, Davidson PM, Agar M, et al. Delirium prevalence, incidence, and implications for screening in specialist palliative care inpatient settings: a systematic review. Palliat Med 2013; 27(6): 486–498. [DOI] [PubMed] [Google Scholar]
- 9. Irwin SA, Rao S, Bower KA, et al. Psychiatric issues in palliative care: recognition of delirium in patients enrolled in hospice care. Palliat Support Care 2008; 6(2): 159–164. [DOI] [PubMed] [Google Scholar]
- 10. Smith J, Adcock L. The recognition of delirium in hospice inpatient units. Palliat Med 2012; 26(3): 283–285. [DOI] [PubMed] [Google Scholar]
- 11. World Health Organization. The ICD-10 classification of mental and behavioural disorders: clinical descriptions and diagnostic guidelines, http://www.who.int/classifications/icd/en/bluebook.pdf (1992, accessed 26 June 2018).
- 12. American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. 5th ed. Arlington, VA: American Psychiatric Publishing, 2013. [Google Scholar]
- 13. Ryan K, Leonard M, Guerin S, et al. Validation of the Confusion Assessment Method in the palliative care setting. Palliat Med 2009; 23: 40–45. [DOI] [PubMed] [Google Scholar]
- 14. Bush SH, Tierney S, Lawlor PG. Clinical assessment and management of delirium in the palliative care setting. Drugs 2017; 77(15): 1623–1643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bush SH, Lawlor PG, Ryan K, et al. Delirium in adult cancer patients: ESMO clinical practice guidelines. Ann Oncol 2018; 29(Suppl. 4): iv143–iv165. [DOI] [PubMed] [Google Scholar]
- 16. Leonard MM, Nekolaichuk C, Meagher DJ, et al. Practical assessment of delirium in palliative care. J Pain Symptom Manage 2014; 48(2): 176–190. [DOI] [PubMed] [Google Scholar]
- 17. Meagher D. Motor subtypes of delirium: past, present and future. Int Rev Psychiatry 2009; 21(1): 59–73. [DOI] [PubMed] [Google Scholar]
- 18. Meagher DJ, O’Hanlon D, O’Mahony E, et al. Relationship between symptoms and motoric subtype of delirium. J Neuropsychiatry Clin Neurosci 2000; 12(1): 51–56. [DOI] [PubMed] [Google Scholar]
- 19. Liptzin B, Levkoff SE. An empirical study of delirium subtypes. Br J Psychiatry 1992; 161: 843–845. [DOI] [PubMed] [Google Scholar]
- 20. Meagher D, Adamis D, Trzepacz P, et al. Features of subsyndromal and persistent delirium. Br J Psychiatry 2012; 200(1): 37–44. [DOI] [PubMed] [Google Scholar]
- 21. Downing LJ, Caprio TV, Lyness JM. Geriatric psychiatry review: differential diagnosis and treatment of the 3 D’s—delirium, dementia, and depression. Curr Psychiatry Rep 2013; 15(6): 365. [DOI] [PubMed] [Google Scholar]
- 22. Farrell KR, Ganzini L. Misdiagnosing delirium as depression in medically ill elderly patients. Arch Intern Med 1995; 155(22): 2459–2464. [PubMed] [Google Scholar]
- 23. Leonard M, Agar M, Mason C, et al. Delirium issues in palliative care settings. J Psychosom Res 2008; 65(3): 289–298. [DOI] [PubMed] [Google Scholar]
- 24. Hjermstad MJ, Loge JH, Kaasa S. Methods for assessment of cognitive failure and delirium in palliative care patients: implications for practice and research. Palliat Med 2004; 18(6): 494–506. [DOI] [PubMed] [Google Scholar]
- 25. Lawlor PG, Davis DHJ, Ansari M, et al. An analytical framework for delirium research in palliative care settings: integrated epidemiologic, clinician-researcher, and knowledge user perspectives. J Pain Symptom Manage 2014; 48(2): 159–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Lawlor PG, Rutkowski N, MacDonald AR, et al. A scoping review to map empirical evidence regarding key domains and questions in the clinical pathway of delirium in palliative care. J Pain Symptom Manage 2018; 57: 661–681.e12. [DOI] [PubMed] [Google Scholar]
- 27. Munn Z, Moola S, Lisy K, et al. Chapter 5: systematic reviews of prevalence and incidence. In: Aromataris E, Munn Z. (eds) Joanna briggs institute reviewer’s manual. The Joanna Briggs Institute, 2017, https://reviewersmanual.joannabriggs.org/ [Google Scholar]
- 28. Swartz MK. The PRISMA statement: a guideline for systematic reviews and meta-analyses. J Pediatr Health Care 2011; 25(1): 1–2. [DOI] [PubMed] [Google Scholar]
- 29. Watt C, Bush S, Kabir M, et al. The incidence, prevalence of delirium in palliative care across healthcare settings: a systematic review. PROSPERO: International prospective register of systematic reviews, Record ID CRD42018084164, 2017, https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=84164 [Google Scholar]
- 30. Evidence Partners. DistillerSR. Systematic review and literature review software. Ottawa, ON, Canada: Evidence Partners, 2018. [Google Scholar]
- 31. De la Cruz M, Noguera A, San Miguel-Arregui MT, et al. Delirium, agitation, and symptom distress within the final seven days of life among cancer patients receiving hospice care. Palliat Support Care 2015; 13(2): 211–216. [DOI] [PubMed] [Google Scholar]
- 32. Hui D, Kilgore K, Fellman B, et al. Development and cross-validation of the in-hospital mortality prediction in advanced cancer patients score: a preliminary study. J Palliat Med 2012; 15(8): 902–909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rao S, Ferris FD, Irwin SA. Ease of screening for depression and delirium in patients enrolled in inpatient hospice care. J Palliat Med 2011; 14(3): 275–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Harrison A, Smith R, Champagne M, et al. Implementation of a delirium assessment protocol in an inpatient hospice setting. J Hosp Palliat Nurs 2016; 18: 227–232. [Google Scholar]
- 35. Sarhill N, Walsh D, Nelson KA, et al. Pain and symptom management. Assessment of delirium in advanced cancer: the use of the Bedside Confusion Scale. Am J Hosp Palliat Care 2001; 18: 335–341. [DOI] [PubMed] [Google Scholar]
- 36. De la Cruz M, Fan J, Yennu S, et al. The frequency of missed delirium in patients referred to palliative care in a comprehensive cancer center. Support Care Cancer 2015; 23(8): 2427–2433. [DOI] [PubMed] [Google Scholar]
- 37. De la Cruz M, Ransing V, Yennu S, et al. The frequency, characteristics, and outcomes among cancer patients with delirium admitted to an acute palliative care unit. Oncologist 2015; 20(12): 1425–1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Goy ER, Ganzini L. Prevalence and natural history of neuropsychiatric syndromes in veteran hospice patients. J Pain Symptom Manage 2011; 41(2): 394–401. [DOI] [PubMed] [Google Scholar]
- 39. Fadul NA, El Osta B, Dalal S, et al. Comparison of symptom burden among patients referred to palliative care with hematologic malignancies versus those with solid tumors. J Palliat Med 2008; 11(3): 422–427. [DOI] [PubMed] [Google Scholar]
- 40. Stillman MJ, Rybicki LA. The Bedside Confusion Scale: development of a portable bedside test for confusion and its application to the palliative medicine population. J Palliat Med 2000; 3(4): 449–456. [DOI] [PubMed] [Google Scholar]
- 41. Fernandez F, Levy JK, Mansell PW. Management of delirium in terminally ill AIDS patients. Int J Psychiatry Med 1989; 19(2): 165–172. [DOI] [PubMed] [Google Scholar]
- 42. Massie MJ, Holland J, Glass E. Delirium in terminally ill cancer patients. Am J Psychiatry 1983; 140: 1048–1050. [DOI] [PubMed] [Google Scholar]
- 43. Gagnon P, Allard P, Gagnon B, et al. Delirium prevention in terminal cancer: assessment of a multicomponent intervention. Psychooncology 2012; 21(2): 187–194. [DOI] [PubMed] [Google Scholar]
- 44. Gagnon P, Allard P, Masse B, et al. Delirium in terminal cancer: a prospective study using daily screening, early diagnosis and continuous monitoring. J Pain Symptom Manage 2000; 19(6): 412–426. [DOI] [PubMed] [Google Scholar]
- 45. Fainsinger RI, De Moissac D, Mancini I, et al. Sedation for delirium and other symptoms in terminally ill patients in Edmonton. J Palliat Care 2000; 16(2): 5–10. [PubMed] [Google Scholar]
- 46. Lawlor PG, Gagnon B, Mancini IL, et al. Occurrence, causes, and outcome of delirium in patients with advanced cancer: a prospective study. Arch Intern Med 2000; 160(6): 786–794. [DOI] [PubMed] [Google Scholar]
- 47. Tarumi Y, Watanabe SM, Lau F, et al. Evaluation of the Palliative Prognostic Score (PaP) and routinely collected clinical data in prognostication of survival for patients referred to a palliative care consultation service in an acute care hospital. J Pain Symptom Manage 2011; 42(3): 419–431. [DOI] [PubMed] [Google Scholar]
- 48. Freeman S, Hirdes JP, Stolee P, et al. Care planning needs of palliative home care clients: development of the interRAI palliative care assessment clinical assessment protocols (CAPs). BMC Palliat Care 2014; 13(1): 58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Gaudreau JD, Gagnon P, Harel F, et al. Psychoactive medications and risk of delirium in hospitalized cancer patients. J Clin Oncol 2005; 23(27): 6712–6718. [DOI] [PubMed] [Google Scholar]
- 50. Hausner D, Kevork N, Pope A, et al. Factors associated with discharge disposition on an acute palliative care unit. Support Care Cancer 2018; 26(11): 3951–3958. [DOI] [PubMed] [Google Scholar]
- 51. Mercadante S, Masedu F, Balzani I, et al. Prevalence of delirium in advanced cancer patients in home care and hospice and outcomes after 1 week of palliative care. Support Care Cancer 2018; 26(3): 913–919. [DOI] [PubMed] [Google Scholar]
- 52. Mercadante S, Adile C, Ferrera P, et al. Delirium assessed by Memorial Delirium Assessment Scale in advanced cancer patients admitted to an acute palliative/supportive care unit. Curr Med Res Opin 2017; 33(7): 1303–1308. [DOI] [PubMed] [Google Scholar]
- 53. Mercadante S, Porzio G, Adile C, et al. Pain intensity as prognostic factor in cancer pain management. Pain Pract 2015; 15: E1–E8. [DOI] [PubMed] [Google Scholar]
- 54. Caraceni A, Nanni O, Maltoni M, et al. Impact of delirium on the short term prognosis of advanced cancer patients. Cancer 2000; 89(5): 1145–1149. [DOI] [PubMed] [Google Scholar]
- 55. Porteous A, Dewhurst F, Gray WK, et al. Screening for delirium in specialist palliative care inpatient units: perceptions and outcomes. Int J Palliat Nurs 2016; 22(9): 444–447. [DOI] [PubMed] [Google Scholar]
- 56. Barnes J, Kite S, Kumar M. The recognition and documentation of delirium in hospital palliative care inpatients. Palliat Support Care 2010; 8(2): 133–136. [DOI] [PubMed] [Google Scholar]
- 57. Spiller JA, Keen JC. Hypoactive delirium: assessing the extent of the problem for inpatient specialist palliative care. Palliat Med 2006; 20(1): 17–23. [DOI] [PubMed] [Google Scholar]
- 58. Morita T, Fujimoto K, Tei Y. Palliative care team: the first year audit in Japan. J Pain Symptom Manage 2005; 29(5): 458–465. [DOI] [PubMed] [Google Scholar]
- 59. Minagawa H, Uchitomi Y, Yamawaki S, et al. Psychiatric morbidity in terminally ill cancer patients: a prospective study. Cancer 1996; 78: 1131–1137. [DOI] [PubMed] [Google Scholar]
- 60. Miyajima K, Fujisawa D, Hashiguchi S, et al. Symptoms overlooked in hospitalized cancer patients: impact of concurrent symptoms on oversight [corrected] by nurses. Palliat Support Care 2014; 12: 95–100. [DOI] [PubMed] [Google Scholar]
- 61. Rainsford S, Rosenberg JP, Bullen T. Delirium in advanced cancer: screening for the incidence on admission to an inpatient hospice unit. J Palliat Med 2014; 17(9): 1045–1048. [DOI] [PubMed] [Google Scholar]
- 62. Hosie A, Lobb E, Agar M, et al. Measuring delirium point-prevalence in two Australian palliative care inpatient units. Int J Palliat Nurs 2016; 22(1): 13–21. [DOI] [PubMed] [Google Scholar]
- 63. Godfrey A, Conway R, Leonard M, et al. Motion analysis in delirium: a discrete approach in determining physical activity for the purpose of delirium motoric subtyping. Med Eng Phys 2010; 32(2): 101–110. [DOI] [PubMed] [Google Scholar]
- 64. Durkin I, Keorney M, O’Slorain L. Psychiatric disorder in a palliative care unit. Palliat Med 2003; 17: 212–218. [DOI] [PubMed] [Google Scholar]
- 65. Kim SY, Kim SW, Kim JM, et al. Differential associations between delirium and mortality according to delirium subtype and age: a prospective cohort study. Psychosom Med 2015; 77(8): 903–910. [DOI] [PubMed] [Google Scholar]
- 66. Kang B, Kim YJ, Suh SW, et al. Delirium and its consequences in the specialized palliative care unit: validation of the Korean version of Memorial Delirium Assessment Scale. Psychooncology 2019; 28(1): 160–166. [DOI] [PubMed] [Google Scholar]
- 67. Plaschke K, Petersen KA, Frankenhauser S, et al. The impact of plasma cholinergic enzyme activity and other risk factors for the development of delirium in patients receiving palliative care. J Pain Symptom Manage 2016; 52(4): 525–532. [DOI] [PubMed] [Google Scholar]
- 68. Lam PT, Tse CY, Lee CH. Delirium in a palliative care unit. Prog Palliat Care 2003; 11: 126–133. [Google Scholar]
- 69. Detroyer E, Clement PM, Baeten N, et al. Detection of delirium in palliative care unit patients: a prospective descriptive study of the Delirium Observation Screening Scale administered by bedside nurses. Palliat Med 2014; 28(1): 79–86. [DOI] [PubMed] [Google Scholar]
- 70. Fang CK, Chen HW, Liu SI, et al. Prevalence, detection and treatment of delirium in terminal cancer inpatients: a prospective survey. Jpn J Clin Oncol 2008; 38(1): 56–63. [DOI] [PubMed] [Google Scholar]
- 71. Senel G, Uysal N, Oguz G, et al. Delirium frequency and risk factors among patients with cancer in palliative care unit. Am J Hosp Palliat Care 2017; 34(3): 282–286. [DOI] [PubMed] [Google Scholar]
- 72. Hui D, dos Santos R, Reddy S, et al. Acute symptomatic complications among patients with advanced cancer admitted to acute palliative care units: a prospective observational study. Palliat Med 2015; 29(9): 826–833. [DOI] [PubMed] [Google Scholar]
- 73. Lawlor PG, Bush SH. Delirium in patients with cancer: assessment, impact, mechanisms and management. Nat Rev Clin Oncol 2015; 12: 77–92. [DOI] [PubMed] [Google Scholar]
- 74. Lawlor PG. Cancer patients with delirium in the emergency department: a frequent and distressing problem that calls for better assessment. Cancer 2016; 122(18): 2783–2786. [DOI] [PubMed] [Google Scholar]
- 75. Fong TG, Davis D, Growdon ME, et al. The interface between delirium and dementia in elderly adults. Lancet Neurol 2015; 14(8): 823–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Karuturi M, Wong ML, Hsu T, et al. Understanding cognition in older patients with cancer. J Geriatr Oncol 2016; 7(4): 258–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 854944_supp_mat_1 for The incidence and prevalence of delirium across palliative care settings: A systematic review by Christine L Watt, Franco Momoli, Mohammed T Ansari, Lindsey Sikora, Shirley H Bush, Annmarie Hosie, Monisha Kabir, Erin Rosenberg, Salmaan Kanji and Peter G Lawlor in Palliative Medicine
Supplemental material, 854944_supp_mat_2 for The incidence and prevalence of delirium across palliative care settings: A systematic review by Christine L Watt, Franco Momoli, Mohammed T Ansari, Lindsey Sikora, Shirley H Bush, Annmarie Hosie, Monisha Kabir, Erin Rosenberg, Salmaan Kanji and Peter G Lawlor in Palliative Medicine
Supplemental material, 854944_supp_mat_3 for The incidence and prevalence of delirium across palliative care settings: A systematic review by Christine L Watt, Franco Momoli, Mohammed T Ansari, Lindsey Sikora, Shirley H Bush, Annmarie Hosie, Monisha Kabir, Erin Rosenberg, Salmaan Kanji and Peter G Lawlor in Palliative Medicine