Abstract
Background:
Effective communication between healthcare professionals and relatives of patients approaching the end-of-life is vital to ensure patients have a ‘good death’. To improve communication, it is important to first identify how this is currently being accomplished.
Aim:
To review qualitative evidence concerning characteristics of communication about prognosis and end-of-life care between healthcare professionals and relatives of patients approaching the end-of-life.
Design:
Qualitative systematic review (PROSPERO registration CRD42017065560) using thematic synthesis. Peer-reviewed, English language articles exploring the content of conversations and how participants communicated were included. No date restrictions were applied. Quality of included studies was appraised using the Joanna Briggs Institute Critical Appraisal Checklist for Qualitative Research.
Data sources:
An electronic database search of CINAHL, MEDLINE, PsycINFO and EMBASE was performed.
Results:
Thirty-one papers were included. Seven themes were identified: highlighting deterioration; involvement in decision-making, post-decision interactional work, tailoring, honesty and clarity, specific techniques for information delivery and roles of different healthcare professionals. Varied levels of family involvement in decision-making were reported. Healthcare professionals used strategies to aid understanding and collaborative decision-making, such as highlighting the patient’s deterioration, referring to patient wishes and tailoring information delivery. Doctors were regarded as responsible for discussing prognosis and decision-making, and nurses for providing individualized care.
Conclusion:
Findings suggest training could provide healthcare professionals with these strategies to improve communication. Interventions such as question prompt lists could help relatives overcome barriers to involvement in decision-making. Further research is needed to understand communication with relatives in different settings and with different healthcare professionals.
Keywords: Communication, terminal care, palliative care, family, caregivers, qualitative research
What is already known about the topic?
Poor communication from healthcare professionals is a common complaint from relatives of patients at the end-of-life.
Communication with relatives at this time is important for high quality end-of-life care and for relatives’ long-term well-being.
What this paper adds
Common communication strategies are identified including highlighting the patient’s deterioration to aid decision-making, references to patient wishes, providing relatives with options, tailoring information to individuals and using pacing and staging of information.
Healthcare professionals state a belief in using honest, direct language and involving families in decision-making, but there is variation in the extent to which this is implemented in practice.
Nurses and allied healthcare professionals play an important role in providing individualized communication with relatives.
Implications for practice, theory or policy
There is a need for more research on communication with relatives in palliative care settings and with different members of the multidisciplinary team.
Training is needed to help healthcare professionals to translate communication guidelines into practice while considering their own emotional needs.
Interventions such as question prompt list could also be used to help relatives get the information they need.
Introduction
Family members of patients at the end-of-life value high quality communication about their relatives’ prognosis and care.1–4 Patients in the terminal phase of their illness often have difficulty communicating and so their relatives need clear information to make decisions on their behalf. Honest and timely communication can give relatives time to say goodbye and improve psychological outcomes and satisfaction with end-of-life care.5–10
Healthcare professionals report finding end-of-life communication challenging and often wait for patients or families to initiate these conversations.11 In an international survey of palliative care experts, 83% agreed more evidence-based guidance on strategies for communication with relatives would improve end-of-life decision-making.12 A report by the English Parliamentary and Health Service Ombudsman found a key area of complaints about end-of-life care was failing to recognize when a person was dying and communicate this to the patient and their relatives.13
In response to criticisms of end-of-life care in the United Kingdom, the National Institute for Health and Care Excellence (NICE) have produced guidelines for healthcare professionals, including advice on communication.14 NICE make recommendations including discussing what patients understand and want to know, explaining uncertainty, avoiding false optimism, providing opportunities to ask questions and highlighting opportunities for further discussions. Bernacki and Block15 made similar recommendations for a conversation guide to support clinicians in the United States. However, the primary focus of these recommendations is communication with patients rather than relatives. While these recommendations can be useful for relatives, their communication needs are different. For example, a previous review found caregivers wanted more information about the dying process than patients.16
Recommendations about what to discuss with relatives are needed, alongside specific strategies on how to do this. Previous reviews have explored relatives’ communication preferences and how they are prepared for the patient’s death more generally. They found a desire for honest information about disease progression, the dying process and pain management; jargon-free information with time to understand; and opportunities to discuss spiritual needs.16–20 However, these reviews did not focus on how healthcare professionals discuss these issues with relatives. To provide recommendations for change, we must first understand how this communication is currently being accomplished. Healthcare professionals and relatives sometimes have different perceptions of how much prognostic information relatives have been given.21,22 It is therefore important to consider a range of perspectives when addressing this issue.
Objectives
The primary objective of this article is to review existing qualitative evidence about the characteristics of communication about prognosis and end-of-life care between healthcare professionals and relatives of patients approaching the end-of-life:
From the perspective of healthcare professionals;
From the perspective of relatives;
As identified from observational studies.
Method
An initial scoping of the literature suggested only qualitative literature could explore what happens during these conversations in sufficient depth. A qualitative systematic review was therefore conducted.
Search strategy
A comprehensive electronic database search was last updated on 16 July 2018. The databases searched were CINAHL plus (1937–2018), MEDLINE (1950–2018), PsycINFO (1967–2018) and EMBASE (1980–2018). Text and MeSH terms for the following word groups were searched: communication, relatives, healthcare professionals, settings with patients at the end-of-life and qualitative methodology. Searches included peer-reviewed, English language articles, and there were no search restrictions based on the date of publication (see full electronic search strategy in Supplementary Table 1). Reference lists of all included studies were hand-searched and citation searching was performed. Reference lists of five relevant reviews were hand-searched.16,17,19,20,23
Study selection
The lead author (R.A.) ran the searches, removed duplicates and screened titles and abstracts to exclude ineligible papers. Full texts of all remaining papers were reviewed for inclusion/exclusion by R.A. and M.A. Studies identified from the search had a broad range of research questions and so study selection was complex, requiring numerous decisions within the research team. For example, articles involving both relatives and patients were included only if the findings relating to relatives could be separated from those relating to patients. Disagreements and uncertainty were resolved through discussion and referral to a third reviewer, J.L. when required.
Inclusion criteria included qualitative studies focusing on communication between adult relatives and healthcare professionals, in settings with patients at the end-of-life, about prognosis and end-of-life care and exploring what and how communication occurs (as opposed to preferences or challenges). Authors were contacted when the eligibility of papers was unclear. A full list of inclusion and exclusion criteria is included in Supplementary Table 2.
Quality appraisal
The 10-item Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Qualitative Research24 was used to assess the quality of included articles. While there is no ‘gold standard’ tool for quality appraisal of qualitative studies, a comparative analysis concluded the JBI checklist was the most coherent.25
R.A. and M.A. assessed all studies against the JBI checklist. Disagreements were resolved through discussion and referral to other authors (J.L. or S.B.). The JBI checklist does not allocate scores to studies and papers were not excluded based on the checklist; instead, results were used to identify weaknesses in the literature and considered when synthesizing the data. Authors’ descriptions/interpretations were only included in the synthesis if they were supported with illustrative quotes.
Data extraction and synthesis
The following data were extracted by R.A. and checked by M.A.: title, authors, year, journal, country, setting, research question/aims, theoretical/philosophical perspective, research methodology, data collection/analysis, study population and relevant findings. Only findings relevant to the aim of this review were extracted. For example, one study26 included findings related to physicians’ beliefs on children’s best interests. These were not extracted but all findings relating to communication with parents were.
Findings, including participant quotes and authors’ descriptions/interpretations, were entered into NVivo 11. Thematic synthesis, which allows conclusions to be drawn across heterogeneous methodologies, was used to synthesize findings. Thomas and Harden’s27 steps of thematic synthesis were followed, beginning with line-by-line coding of findings. Initial codes were grouped into descriptive themes and put into a coding framework, which was applied to the whole dataset. These themes were discussed within the team to develop analytic themes. For example, descriptive themes ‘problem listing’ and ‘perspective display invitations’ both highlighted a patient’s deterioration, and so this became an analytic theme.
R.A. coded findings with regular discussions with the analytic team, which included five researchers (three with Psychology backgrounds, one with a speech and language background and one palliative care consultant). An interpretivist approach was taken towards the synthesis, which involves providing narrative descriptions to represent the subjective experiences of a range of stakeholders.28 A broad range of populations and clinical settings were therefore included in the review and are presented together within the synthesis.
Results
Search results
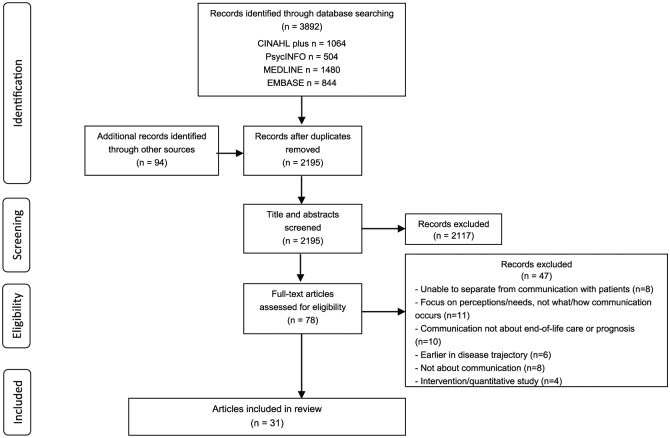
The search strategy identified 2195 unique citations published between 1975 and 2018, 31 of which were included in the review (Figure 1). The 31 articles originated from 10 countries and reported results from 25 individual studies (see Table 1). Fourteen papers were observational (non-participant observations or video/audio-recordings), 10 used interviews or focus groups with healthcare professionals, five used interviews with relatives and two used a combination of these approaches in ethnographic studies. The majority of studies were based in adult acute care (18 papers); eight were in paediatric or neonatal intensive care units (ICUs), three in palliative care settings and two in other settings (older adult wards and family physicians).
Figure 1.
PRISMA diagram of included articles, adapted from Moher et al.29
Table 1.
Summary of included papers.
| Author | Country | Research question/aim | Setting | Population | Data collection Data analysis |
Summary of relevant findings |
|---|---|---|---|---|---|---|
| Observational studies | ||||||
| Aldridge and Barton30a | USA | Compare the ‘description of current status’ in end-of-life discussions with family members that did and did not result in a change from therapeutic to comfort care | Surgical ICU | Critical care intensivists, surgeons and families of current SICU patients | Secondary analysis of audio-recordings of family conferences Discourse analysis |
Highlighting negative outcomes and direct summaries implying terminal status led to more decisions to move to comfort care Decisions were less likely to be made when more positive outcomes were described and possible treatment was discussed |
| Barton et al.31a | USA | 1. Describe the structure and variations within each phase of the end-of-life discussion 2. Look specifically at interaction between physicians and families within each phase |
Surgical ICU | Critical care intensivists, surgeons and families of current SICU patients | Secondary analysis of audio-recordings of family conferences Discourse analysis |
Description of current status used to develop consensus on terminal status. Some used perspective display questions. Framed decision as expressing patient’s wishes. If no consensus of terminal status was established, decisions were not made Explained logistics of dying (often initiated by family) with more direct language |
| Barton32a | USA | Describe how physicians and families construct an ethical frame to present the decision to withdraw life support as the ‘right’ decision | Surgical ICU | Critical care intensivists, surgeons and families of current SICU patients | Secondary analysis of audio-recordings of family conferences Discourse analysis |
Process of dying and comfort care repeated by doctors and families Doctors repeated problem listing and emphasized the decision as being a consensus between the medical team Families discussed personhood and consciousness – doctors repeated ‘best interests’ and described the decision as ethical because of loss of consciousness Both families and doctors described the decision as ‘right’ |
| Curtis et al.33b | USA | Establish a framework that will allow future analyses and studies to describe and understand the communication in family conferences in which the issue of withholding or withdrawing life support is discussed | ICU | Attending, resident and fellow physicians and families of current ICU patients | Audio-recording of family conferences Limited application of grounded theory |
Discussed substituted judgement: encouraged the family to describe personhood to elicit patient wishes Described the dying process (often raised by family) Stressed continuing care, patient comfort and supported decision to withdraw treatment Varied in directness and use of strategies (e.g. repeating what family says, allowing silence, confirming understanding) |
| Curtis et al.34b | USA | Identify missed opportunities for physicians to provide support or information to families during family conferences | ICU | Attending, resident and fellow physicians and families of current ICU patients | Audio-recording of family conferences Limited application of grounded theory |
15/51 family conferences had examples of missed opportunities: Some avoided answering difficult questions and didn’t ask for clarification about families’ vague concerns Failed to explore/acknowledge expressions of emotion Missed chances to explore comments about patient treatment preferences |
| De Vos et al.35 | Netherlands | 1. How do physicians and parents communicate about decisions to withhold or withdraw life sustaining treatment 2. To what extent do parents share in the decision-making process? |
Paediatric ICU | Physicians and parents of children currently in PICU | Audio-recording of conversations Qualitative coding |
Discussed deterioration: 1/3 asked for parents’ perspective on child’s condition. Parents demonstrated good understanding when asked Physicians expressed a team preference. Parents often gave their preference unprompted Most presented as medical decision and didn’t ask parents. Parents expressed concern about suffering and physicians reassured them of comfort and peace Nurses often spoke with parents at the bedside after the meeting (not recorded) |
| Ekberg et al.36 | Australia | Explore how discussions about deterioration are managed within actual paediatric palliative care consultations | Paediatric palliative care service (inpatient, outpatient, telehealth and home) | Specialist palliative care consultant and parents of children in a paediatric palliative care service | Video-recordings of consultations Conversation analysis |
Solicited the family’s agenda to allow opportunity for them to raise prognosis/deterioration Used topic shading (brought up another issue where deterioration may be relevant). This allowed the family to raise deterioration if they wished to |
| Engelberg et al.37b | USA | Describe physicians’ responses to families’ questions about the meaning of critically ill patients’ movements | ICU | Attending, resident and fellow physicians and families of current ICU patients | Audio-recording of family conferences Limited application of grounded theory |
6/51 family conferences had unresolved questions about patient movement: Majority responded with clinical information (physiological reasons) Acknowledged emotions (e.g. with active listening) Only one physician explored emotions and gave the family more time to consider |
| Hsieh et al.38b | USA | Identify inherent tensions that arose during family conferences in the ICU, and the communication strategies clinicians used in response | ICU | Attending, resident and fellow physicians and families of current ICU patients | Audio-recording of family conferences Qualitative content analysis from a dialectic perspective |
Contradictions identified included: killing versus allowing to die, death as benefit versus burden, patient wishes versus family wishes Physicians’ decision-centred strategies: argued against one side (e.g. killing), argued for one side (e.g. patient over family wishes) or avoided Physicians’ information-seeking strategies: acknowledged the contradiction, clarified family’s statements, emphasized patient wishes and segmented decision |
| Kawashima39 | Japan | Explicate the structure of interactions between medical professionals and patients’ family members in a Japanese emergency room, when the patient is seriously ill and may be at the point of death | Emergency room | Physicians and family members of patients at risk of imminent death in an emergency room | Video recordings of consultations Conversation analysis |
Storytelling: Physicians described what has happened or asked relatives what has happened to forecast bad news Online commentary: Physicians used sight and touch to explain symptoms Paradoxical proposals: Physicians sometimes put forward continuing treatment despite suggestion that treatment is futile, giving time for families to make the decision or express deontic authority Physicians left sentences unfinished to allow for co-completion of final decision Following online commentaries/paradoxical proposals, families themselves sometimes raised the possibility of stopping treatment |
| Miller et al.40 | USA | Examine the decision-making process to withhold or stop life support | ICU | Attending, resident and fellow physicians and families of current ICU patients | Audio-recordings of family conferences Conversation analysis |
Framing of options ‘shaded’ (e.g. not all options presented) in 6/15 cases Framed decision as consensus between healthcare professionals, the family and the patient’s wishes When couldn’t agree, gave family time to decide (but imposed time limit) |
| Pecanac41 | USA | Explore how clinicians introduce the need to make a decision about the use of life-sustaining treatment and how surrogates respond | ICU | Physicians and families of current ICU patients | Audio-recordings of family conferences/ Conversation analysis |
Clinicians used ‘perspective-display invitations’ to elicit the surrogate’s view of patient preference – used this as basis for shared decision-making Direct questions were more successful than tacit invitations Perspective display invitations were reformulated when unsuccessful |
| Shaw et al.42 | UK | Explore decision-making related to the move from active to palliative care in the neonatal ICU | Neonatal ICU | Consultants and families of babies currently in NICU | Audio-recordings of discussions/ Conversation analysis |
Identified two different ways doctors initiated the decision-making process: 1. Making recommendations: Presented strong recommendation as coming from the medical team in the best interests of the baby. Parents often asked challenging questions, about options and responded negatively to explanations 2. Providing options: Presented as a joint plan for parents and doctors to make. Told parents the decision can be deferred and options for the decision were provided. Parents could ask questions without appearing challenging |
| West et al.43b | USA | Identify the categories of expressions of non-abandonment and develop a conceptual model describing the ways this is expressed by families and clinicians, in ICU family conferences concerning withdrawing life-sustaining treatments or the delivery of bad news | ICU | Attending, resident and fellow physicians and families of current ICU patients | Audio-recording of family conferences Limited application of grounded theory |
44/51 family conferences contained expressions of non-abandonment from either the family or clinician: Clinicians: Highlighted continuing care; emphasized physician availability; gave the family the choice of when treatment is removed Family: expressed decision as reducing suffering and following patient wishes; expressed a desire to be at the bedside |
| Family perspective | ||||||
| Abib El Halal et al.44 | Brazil | Explore parents’ perspectives of the quality of care offered to them and their terminally ill child in the child’s last days of life | Paediatric ICU | Parents of children who died in PICU | Interviews Thematic content analysis |
Parents reported healthcare professionals using medical jargon Decisions were communicated but families not involved Lack of communication around the time of death |
| Gordon et al.45c | USA | Examine bereaved parents’ perspectives of their and clinicians’ communicative roles and responsibilities in the PICU | Paediatric ICU | Parents of children who died in PICU | Secondary analysis of interviews Discourse analysis |
Varied in how much parents were included in decisions Some struggled to understand uncertainty. Clarity varied (e.g. medical jargon) Some felt clinicians created false hope by saying child was going to be ok Parents were sometimes ‘rude’ or shouted at clinicians |
| Lind46 | Norway | Examine and describe relatives’ experiences of responsibility in the ICU decision-making process | ICU | Relatives of patients who died in ICU | Secondary analysis of interviews Narrative analytical approach |
Three variants of involvement in decisions: 1. Informed not involved: families told of decision with a medical explanation 2. Informed and asked for approval (directly or waiting for a nod/yes) 3. Involved – shared decision-making: Discussed what the patient would want |
| Meert et al.47c | USA | Describe parents’ perceptions of their conversations with physicians regarding their child’s terminal illness and death in the PICU | Paediatric ICU | Parents of children who died in PICU | Secondary analysis of interviews Qualitative coding |
Honest communication built trust and prepared parents. Others held back prognostic information leading to false hope Honesty was either communicated with empathy which was appreciated or as ‘matter of fact’ which felt cold and insensitive Some felt healthcare professionals used medical jargon or too much information was given at once |
| Odgers et al.48 | Australia | Explore the family’s experience of end-of-life care for their relative during the dying process | Acute hospital | Next of kin to patients who died in acute hospital | Interviews Thematic analysis |
Some felt doctors were not clear and honest with them (e.g. used euphemisms and were indirect about prognosis) Others had open conversations including discussing patient wishes |
| Healthcare professional perspective | ||||||
| Bach et al.49 | Canada | Bring to light the role of critical care nurses in decision-making at the end-of-life | ICU and cardio-respiratory care unit | Critical care nurses | Interviews Grounded theory |
Nurses clarify information and help families see the whole picture Act as a go-between for the physicians and families Felt that honesty is important (but balanced with hope) |
| Bartel et al.50 | USA | Describe physicians’ experiences in attempting to provide optimal care for families of children who suffer sudden, acute life threatening conditions | Paediatric ICU | Resident, attending and fellow PICU physicians | Interviews and focus groups Qualitative coding |
Provide families with options and they make the final decision Denial common in families – physicians repeat information and give time Highlighted the role of nurses/social workers taking time with families Identify a family spokesperson Try to give clear summaries, non-medical language, staged information and not give false hope |
| Bloomer et al.51 | Australia and New Zealand | Explore how nurses navigate communication with families during treatment withdrawal processes | ICU | Critical care nurses | Focus groups Inductive content analysis |
Look for non-verbal cues that a relative does/doesn’t want to talk and verbal signs of understanding Identify a spokesperson Use staging of information to give families time to digest it Following family meetings check understanding and discuss the process of death |
| Epstein52 | USA | Explore nurses’ and physicians’ end-of-life experiences in the new-born ICU | New-born ICU | NICU registered nurses, nurse practitioners and resident and fellow physicians | Interviews Hermeneutic circle approach |
Physicians delayed conversations to give families time to understand patients’ terminal status Nurses felt false hope could be promoted Nurses informally/gently discussed options with parents in more detail Physicians begin more indirectly but use direct language if families don’t understand Explain what changes to expect in dying process Involve parents in decision but take responsibility themselves |
| Kehl53 | USA | Describe how hospice clinicians prepare family for the final days of life | Home hospice | Nurses, nursing assistant, social workers, bereavement counsellors and chaplain | Interviews Conventional content analysis |
Discuss signs/symptoms of death and time to death (including uncertainty) Repetition to ensure the message gets through, staged preparation over time Use active listening/questions to tailor content and delivery Building trust improves acceptance of messages |
| Liaschenko et al.54 | USA | Understand factors that influence ICU nurses’ inclusion of families in end-of-life care | Critical care unit | Experienced critical care nurses | Focus groups Content analysis |
Nurses bring together information from different physicians to provide the ‘big picture’. Draw attention to quality of life consequences of treatment Highlight deterioration and prepare families for death |
| Peden-McAlpine55 | USA | Describe the communication practices experienced intensive care nurses use with families to negotiate consensus on withdrawal of aggressive treatment and/or shift to palliative care | ICU | ICU nurses comfortable with dying patients/families | Unstructured interviews Narrative approach |
Changes in the patient’s status can a trigger conversations Nurses check understanding and explain consequences of treatment after discussions with physicians Ask about the patient, emphasize quality of life and what they would want Help families see deterioration. Tailor to what the person is ready to hear |
| Rejno et al.56 | Sweden | Deepen the understanding of stroke team members’ reasoning about truth-telling in end-of-life care due to acute stroke | Acute stoke ward | Physicians, registered nurses and enrolled nurses | Interviews Qualitative content analysis |
Truth above all: approach discussions with complete honesty and direct language to prepare them and establish trust Hide truth to protect: Withhold certain distressing information if don’t feel it’s necessary to tell; wait until have clearer info/better environment to discuss; some nurses waited for doctor to give the bad news |
| Richards et al.26 | USA | Understand how neonatal and paediatric critical care physicians balance and integrate the interests of the child and family in decisions about life-sustaining treatments | Paediatric and Neonatal ICU | Attending paediatric critical care physicians | Interviews Content and thematic analysis |
Limiting options: don’t mention treatment options that they believe to be futile Being directive: when feel parents can’t make decisions, physicians take control to relieve burden and give families ‘permission’ to remove life support Staying neutral: by providing options and avoiding giving own opinion Allowing parents to come to own conclusions (e.g. delay decisions/discussions and give time so that parents can see that their child is dying) |
| Tan and Manca57 | Canada | Describe conflict experiences that family physicians have with substitute decision-makers of dying patients and identify factors that facilitate or hinder the end-of-life decision-making process | Family physicians | Family physicians | Interviews Grounded theory |
Staged information as trust increases; gauge surrogate’s understanding; use patient’s previous statements to help decisions Bringing other professionals in can help resolve conflict |
| Mixed perspectives | ||||||
| Caswell et al.58 | UK | Understand the factors and processes which affect the quality of care provided to frail older people who are dying in hospital and their family carers | Hospital wards caring for older adults | Healthcare professionals and bereaved relatives of older patients who died | Ethnographic: interviews, focus groups, non-participant observations and review of case notes Constant comparative method |
Doctors discussed prognosis, nurses translated into lay language Staff thought often one conversation wasn’t enough but didn’t always repeat this Observations showed it was rare to explain process of dying Euphemistic/vague language meant carers didn’t always understand that their relative was dying |
| Meeker et al.59 | USA | Examine the nature of family meetings as conducted in an inpatient hospice care unit in order to generate an inductive theoretical model | Hospice inpatient unit | Nurses, social workers, physicians and family members of current hospice inpatients | Ethnographic: observations of family meetings, informed by healthcare professional interviews Constant comparative method of grounded theory |
Healthcare professionals elicited understanding to ensure their views were aligned on prognosis (e.g. discuss prior symptoms that signal dying). Families described patient’s personhood Explained process of dying, paced info in line with family responses Separated the person from the illness (e.g. explaining agitation), gave time to ask questions |
SICU: surgical intensive care unit, ICU: intensive care unit, PICU: paediatric intensive care unit, NICU: neonatal intensive care unit.
Detailed demographic information is provided in Supplementary Table 3 and quality appraisal information in Supplementary Table 4.
Papers using data from Cassell.60
Papers using data from Curtis et al.33
Papers using data from Meert et al.61
Study participants
Overall, sample sizes are reported below. In samples used for multiple papers, only the original sample size is included in this total. Further demographic information for study participants is included in Supplementary Table 3.
Observational, ethnographic and interview/focus group studies with healthcare professionals had a total sample size of 343 healthcare professionals (170 physicians, 127 nurses, 9 other healthcare professionals, 37 unspecified), with a median sample size of 19 healthcare professionals (range = 1–37). Numbers of healthcare professionals were not reported for two primary observational studies. Physicians were mostly attending, resident and fellow physicians, intensivists and palliative care consultants, although this information could not be obtained for five studies. Nurses worked in ICU, paediatric ICU, other acute care or hospice. Other healthcare professionals such as social workers were also present at observations but were not the focus of these observations. Two studies interviewed other healthcare professionals. Where reported, healthcare professionals’ years of clinical or specialty experience ranged from <2 to 40 years.
Observational, ethnographic and interview studies with family members had a total sample size of 495 individual family members with a median sample size of 27 (range = 12–227). The number of individual family members could not be obtained for five primary studies. These five studies reported a total sample size 92 families with a median sample size of 19 families (range = 8–36). Where reported, family members included parents, spouses, adult children, siblings, friends and other family members. Six primary studies reported including multiple different family members and five reported including parents only.
Quality appraisal results
The main findings from the quality appraisal were the high number of articles which did not report a philosophical perspective (22 articles), the researchers’ background (21 articles) or address the influence of the researcher on the research (21 articles). All studies used quotes to support their analysis, but there were seven papers where it was unclear if an adequate range of participants’ views were represented, mostly due to a lack of patient identifiers. Ten papers did not report their analysis in a way that was wholly consistent with their stated methodology. The full results of the quality appraisal are reported in Supplementary Table 4.
Overview of findings
Included papers described how healthcare professionals and relatives discussed the patient’s deterioration, made decisions and the interactional work accomplished by both parties following decisions. Papers identified communicative practices from healthcare professionals and family members and the roles different healthcare professionals played in communication. The synthesis identified seven key themes to describe this communication: highlighting deterioration, involvement in decision-making, post-decision interactional work, tailoring, honesty and clarity, specific techniques for information delivery and roles of different healthcare professionals. Supplementary Table 5 provides extracts from original papers demonstrating these themes.
Highlighting deterioration
The first theme identified was highlighting deterioration, which was found in 11 papers.26,30–32,35,36,39,54,55,58,59 This describes how healthcare professionals enabled relatives to recognize the patient’s deterioration (referred to as ‘establishing terminal status’ by one study30). Highlighting deterioration involved listing the patient’s previous and ongoing problems to provide evidence that further active treatment was futile and the patient was reaching the end-of-life. Often this was accomplished by healthcare professionals, but studies also found evidence of perspective display invitations,62 where healthcare professionals asked relatives to describe what had happened so far and how the patient was doing.31,32,35,36,39,55,58,59 Perspective display invitations highlighted deterioration in collaboration with families and provided healthcare professionals with information about their level of acceptance and understanding.
Usually, this phase ended with a summary statement to demonstrate they had reached a consensus that the patient was dying. However, one study described more ambiguous problem listing, including references to treatment. In these conversations, a consensus on terminal status was less likely to be reached and decisions relating to withdrawal of treatment were made less often.30
The practice of highlighting deterioration was identified in healthcare professional interview and focus group studies54,55,58,59 and observational studies,30–32,35,36,39,59 but not interviews with families. It was seen in adult and paediatric settings, but was not always consistent. For example, in an ethnographic study on older adult wards, only one healthcare professional described this practice and there was no evidence of it from non-participant observations.58
Involvement in decision-making
Varied levels of family involvement in patient care decisions were identified, particularly relating to withdrawal of treatment. The reported styles of involvement can be divided into presenting the medical team’s decision (either as what has already been decided35,44–46 or a recommendation for families to agree with previous studies26,42,45,46,52) or a collaborative process where the family made the final decision. Reports of less collaborative decision-making were more common in paediatric settings and were found mostly by observational studies35,42 and those interviewing family members.44–46 Healthcare professionals rarely described non-collaborative decision-making, but in two healthcare professional interview studies, some described taking responsibility for decisions to relieve burden for families.26,52 While this could be helpful when families felt unable to make decisions, it could cause interactional difficulties. Where healthcare professionals presented recommendations, family members often passively agreed, without always receiving clear information about the reason for the decision. At other times, family members objected to the decision. One conversation analytic study42 described how giving recommendations made it difficult for families to ask questions as they came across as challenging the medical team’s opinion. However, there was evidence of families actively involving themselves in these conversations by asking questions and expressing preferences.32,35,39,42,45
Collaborative decision-making was reported across observational studies and interviews/focus groups with healthcare professionals and relatives, and in both child and adult settings.26,30–33,35–43,45–50,52,55,57 When papers reported collaborative decision-making, several strategies were used. In adult settings only, the most common identified was invoking the patient’s wishes.31–33,38,40–42,46–49,55 Healthcare professionals asked families what the patient was like prior to hospitalization and whether they had discussed their care preferences. They emphasized the family member was a voice for the patient, rather than making decisions based on their own feelings. There were, however, examples in observational studies and one nurse interview study, where doctors missed opportunities to discuss patients’ wishes or did not clarify the meaning of surrogate decision-making.33,34,46
Another strategy was presenting options to the family (e.g. to remove some life-sustaining treatments and leave others in place) and framing the discussion as forming an evolving plan, rather than one overall decision.26,35,38–40,42,50,52 Options could be presented with a subtle preference for a certain course of action,40 but it was stressed the family’s decision would be supported. Families were given time to make decisions and if withdrawing treatment, control over how and when this would happen.33,37,39,42,43,46 These practices were mostly identified by observational studies,33,37–40,42,43 but some relatives described the same practices35,46 and healthcare professionals reported providing options.26,50,52
Post-decision interactional work
Observational studies and healthcare professional interviews reported that healthcare professionals emphasized the continued care of the patient33,35,43,47,57,59 (described in one study as ‘expressing non-abandonment’43), particularly following decisions to withdraw active treatment. Healthcare professionals stressed they would ensure the patient was comfortable, explained what would happen next and reassured families they would be available for further discussions. There were however reports from families44,58 and some observations43 of healthcare professionals failing to do this and where it appeared to families that healthcare professional involvement would reduce following the move to comfort care.
Families also displayed their commitment to their relatives’ continued care by discussing the patient’s comfort and emphasizing their continued presence, often wanting to be with the patient when they die.32,35,43 Observational studies found families asked questions about patients’ consciousness and awareness, the dying process and what to expect.31–33,37 Healthcare professionals were generally forthcoming with this information,31–33,47,52,53,59 but there were some reports from observational studies where details about the dying process from healthcare professionals were lacking.33,58 Only two articles (from the same observational study) described how healthcare professionals responded to families’ displays of emotions, finding such displays were rarely explored in depth.34,37
Observational studies and one study interviewing nurses reported both healthcare professionals and families justified decisions to withdraw life-sustaining treatments as ‘right’.31–33,38,43,55 They repeated medical justifications for the decision and referred to patients’ wishes. Healthcare professionals often referenced their medical knowledge and experience32,33 and stressed they were allowing the patient to die, not having an active role in the death.38,43
Tailoring
Healthcare professionals reported and were observed to tailor their communication to individual families.33,36,38,50–53,55,57,59 Healthcare professionals gauged levels of understanding and willingness to discuss dying through questions and observing verbal and non-verbal cues from families.38,50,55,57,59 The content, delivery and timing of communication was tailored to families’ previous experiences of death, levels of understanding, desire for information and the patient’s current symptoms.36,38,51–53,55,59 Healthcare professionals were also observed to take into account different cultural and religious backgrounds of families.33 Some healthcare professionals reported identifying a spokesperson for each family to ensure information was effectively communicated to the whole family at a level of detail with which individuals were comfortable.50,51
Honesty and clarity
One of the most varied findings was healthcare professionals’ honesty and clarity. Healthcare professionals described the need to use direct, simple language to promote understanding.26,50,56 However, while some families agreed straightforward information was given,47 others described not understanding information due to technical or ambiguous language.44,45,48 In observational studies, healthcare professionals’ language varied in its level of directness.30,31,33,40,42,48 In interviews, they highlighted the difficult balance between being honest and allowing families hope, mostly emphasizing the need to avoid false hope and be honest to build trust with families.49,50,52,54,56 However, nurses reported that doctors sometimes felt the need to ‘try everything’ and this could lead to false hope for families and unnecessary, aggressive treatments for patients.52 In line with this, several families reported feeling they had been given false hope because of a lack of honest communication.44,45,47,48,58 In one interview study, some relatives realized when looking back that healthcare professionals had tried to inform them their relative was dying, but said that they had not fully understood at the time,58 suggesting possible ambiguity on the part of the healthcare professional. Others felt healthcare professionals had been ‘blunt’ or ‘cold’ in their communication.45,47,48,58
Specific techniques for information delivery
Various communicative techniques used by healthcare professionals were reported in observational studies and interviews with healthcare professionals, but not interviews with families. Repetition was used both within conversations and across several conversations to ensure families’ understanding.32,33,35,50,53 Healthcare professionals repeated information or asked relatives to summarize what they had been told. Repetition was also used towards the end of conversations, for example, information about patients’ deterioration was repeated to justify decisions to remove life-sustaining treatment later on in conversations.32 However, in a study in older adult hospital wards, healthcare professionals acknowledged the need to repeat information but explained they were reluctant to have this conversation a second time.58
Pacing and staging of information were identified as other communicative strategies.26,33,50,51,53,55–57 This included allowing time for information to be taken in within a conversation, giving smaller chunks of information across several conversations when the family was ready to hear it, or delaying giving information until appropriate support could be provided to families. healthcare professionals also described postponing decisions to allow parents time to see for themselves their child was dying.52,56 Staging was not always possible however, especially if the patient had a sudden deterioration necessitating a timely conversation.53
Roles of different healthcare professionals in communication
The review looked at a range of healthcare professionals and found different communication roles for different professions. Doctors were often seen by both healthcare professionals and relatives as responsible for conducting prognostic and decision-making conversations with family members,50,56,58 although when death was imminent, nurses sometimes had these conversations.35,58 While no observational studies focused primarily on nurse communication, in interviews both physicians and nurses recognized the importance of nurses communicating with families on a more personal, individualized level.33,35,49–51,54,55 Nurses often reported translating what doctors had said into less technical language.49,54,55,58 Nurses highlighted their role in giving patients a clearer idea of what treatments would mean for the individual patient and bringing together information from different sources.46,49,54,55 This role was termed providing ‘the big picture’ in one study.54 Nurses also reported encouraging physicians to have discussions with families.49,52,55 These roles of nurses were mostly identified in observational studies and those interviewing healthcare professionals, but in one study families also reported that nurses made things easier to understand.44 Other allied health professionals, particularly social workers, were identified as playing important roles in communication with relatives,53,59 but included studies focused primarily on doctors and nurses.
Discussion
Key findings and implications
This review has focused on the content and communicative practices in end-of-life conversations about prognosis and care between healthcare professionals and relatives. We have identified common practices reported in the qualitative literature and variation in these practices within and across studies.
Healthcare professionals used problem listing, including eliciting relatives’ perspectives, to highlight patients’ deterioration. NICE guidelines14 and Bernacki and Block’s15 review both suggest prognostic disclosure and exploring patients’ understanding are important elements to be addressed by healthcare professionals. It follows that the same should apply when communicating with relatives. The practice of highlighting deterioration is a collaborative communication strategy that could be used by other healthcare professionals to meet these recommendations.
The involvement of relatives within the decision-making process was varied. Invoking patient wishes was often used for collaborative decision-making. A previous systematic review found having awareness of the patient’s treatment preferences reduced negative emotional effects for surrogate decision-makers.63 Therefore, orienting relatives to patient wishes may have long-term benefits beyond the conversation itself. However, references to patient wishes did not occur in paediatric end-of-life care. Healthcare professionals cannot ask parents what their child would want or whether they have had conversations about end-of-life decisions, particularly in neonatal settings. Perhaps, as a result of not being able to refer to patient wishes, most examples of less collaborative decision-making occurred in paediatric settings. However, there was evidence that collaboration could be achieved in these settings by consulting parents whenever decisions were made and providing them with options and time to make plans. Given recent high profile court cases in the United Kingdom involving end-of-life decision-making in paediatric end-of-life care,64,65 pressure and scrutiny on healthcare professionals communicating difficult decisions to families in these settings is particularly high. The collaborative communicative strategies described in this review could be valuable for these healthcare professionals and should be further researched and put into practice through training.
Other common communicative practices identified, including repetition, pacing and staging, and highlighting continuing care are in line with relative’s preferences for receiving detailed information and time to understand this.16–20 Healthcare professionals also recognized the need for simple, direct language and honesty, which have been identified as key relative preferences16–20 and recommended in guidelines.14,15 However, there was evidence of a struggle to balance honesty and hope. This finding demonstrates that while guidelines are a useful start, training on how to implement them in practice is vital to improve communication. Healthcare professionals have reported emotional support needs relating to end-of-life communication, so any intervention should also consider implementing organizational changes to allow reflective practice in a supportive environment.66
Further recommendations from Bernacki and Block’s15 review include focusing on quality of life and assessing what trade-offs are acceptable to patients when making treatment decisions. The review identified nurses as key to facilitating this individualized decision-making. Doctors were responsible for prognostication and decision-making, while nurses helped families understand their options in the context of individual patients’ lives. A recognition of this important role of nurses is needed, and involving them more formally in decision-making may help promote shared decision-making in line with recommendations. While there was little focus on acknowledging spiritual needs in the included articles, relatives have highlighted this as important18,19 and the nurse role in individualized care could put them in a good position to address these needs.
Contributions of different qualitative approaches
Observational studies, those focusing on healthcare professional perspectives and those exploring relatives’ perspectives, all provided valuable findings. However, each approach had strengths and weaknesses in addressing the article’s aim. Interviews with family members contributed more towards understanding the content of conversations than how communication was actually accomplished. This is unsurprising as relatives are less likely to have considered their communicative practices than healthcare professionals who regularly have these conversations. In comparison, healthcare professionals had insights into how they communicate in this context and provided information about communication beyond a single conversation (e.g. spacing information over several conversations). Different healthcare professionals also had insight into each other’s practice, for example, nurses highlighted that doctors sometimes gave families false hope. However, there may be communicative behaviours healthcare professionals are not conscious of. Interviews are also limited by participants’ ability to accurately remember these conversations and recollections are subject to their own interpretations.
Observational studies show what actually happened with the most accuracy, particularly those using audio- or video-recording. However, there are limits to what observations can tell us, for example, these studies could not assess whether clinicians were providing honest information or giving false hope. These studies are also unlikely to observe every conversation a healthcare professional has with relatives and therefore can only capture a snapshot of this communication.
These different approaches revealed differing perspectives on the same experiences. For example, healthcare professionals often described giving detailed information clearly and honestly, but this was not always seen in observations or reported by families. Any clinician training should therefore help healthcare professionals recognize when families have not understood them and avoid assumptions of existing knowledge. Each qualitative approach provides its own benefits and should be combined to get a fuller picture of how communication with relatives is accomplished at the end-of-life and inform effective training.
Limitations of primary studies and systematic review
The main limitations of included articles identified through quality appraisal were related to a lack of insight into the influence of the researchers on the findings. Without stating the study’s philosophical perspective or the potential impact of researchers, it is difficult to know how the research team’s characteristics may have influenced data collection and analysis. In addition, not all studies reported numbers or demographics for individual healthcare professionals or family members, making it difficult to understand who was involved in these conversations.
The review process also has a number of limitations. The search strategy only included English language articles for resource reasons. As a result, 29 of 31 included articles were from Northern European or English-speaking countries, with 19 from the United States alone. Cultural differences in communication practices are likely and so findings from this review may not be generalizable to other cultures.
The review was limited to qualitative studies to gain in-depth insights into how people communicate not accessible through quantitative methods such as surveys. However, qualitative findings are subject to researchers’ interpretations, both in the original studies and during the synthesis. We have aimed to increase rigour in this review through multiple team members independently assessing quality, team discussions during data extraction and synthesis and by reporting our synthesis process transparently.
The search strategy took a broad approach, including studies from a range of patient populations, places of care and methodological approaches. This approach was taken because the review was exploratory and initial scoping of the literature found practices and experiences that applied across different settings. We have highlighted some of the differences between these settings and approaches, but a narrower search strategy would have allowed a more in-depth view of individual settings.
Future research
The majority of studies in this review were in acute care settings. It was not possible to compare the findings from acute settings with palliative care, as there were only three palliative care papers, all in different settings (adult inpatient, adult home hospice and paediatric consultations). However, we can speculate that there are likely to be differences between these settings. The papers in acute settings mostly focused on medical decision-making, particularly withdrawing life-sustaining treatments. In palliative care, these conversations are likely to take place earlier in the disease trajectory and with the patients themselves. By the point of end-of-life care, decision-making conversations will therefore be less common. Family members may have more realistic expectations, particularly in a hospice setting, as hospice inpatient wards generally only admit patients with terminal or life limiting conditions and do not provide curative treatment. Healthcare professionals in palliative care settings may also have more experience of end-of-life communication and more time with families. This is reflected in higher satisfaction and lower unmet needs of families in hospice compared with hospital settings.67 Further palliative care research is therefore needed, particularly in hospices at the very end-of-life when patients are likely to have reduced capacity and so conversations will primarily be taking place with relatives. The experience and expertise of hospice clinicians could provide communication strategies that could be applied in other settings.
Interviews and focus groups with nurses provided insights into their roles and communicative strategies. However, no observational studies focused primarily on nurses. This may be due to these conversations being more spontaneous than those held by doctors, and therefore more difficult to capture in a research project. Observational research focused on nurses could provide practice recommendations for all healthcare professionals. Research into the communication of allied healthcare professionals such as social workers is also needed to develop a fuller picture of communication with relatives at the end-of-life.
More focus on how relatives communicate in these conversations is needed. While there were some references to how relatives communicated, the primary focus of existing literature is healthcare professionals’ communication. Future research should identify how relatives communicate their perspectives, ask questions and respond to different healthcare professional communication practices. This would provide evidence for which strategies are effective and help healthcare professionals recognize how families might express things such as a desire for further information. This evidence could also be used in interventions to empower families to express their perspectives and ask questions to elicit the information they want and need, for example, using question prompt lists.68
Conclusion
Healthcare professionals use a range of practices that could aid effective communication with relatives at the end-of-life. Key strategies include highlighting the patient’s deterioration to aid understanding and decision-making, collaborative decision-making through references to patient wishes and providing options, highlighting continuing care by explaining comfort care, tailoring information to individual understanding and readiness to discuss dying; honesty and clarity to avoid false hope and providing information repeatedly and in small chunks. This systematic review calls for further research to identify the effectiveness of different communicative strategies. This research should be used to develop training for healthcare professionals to help them understand relatives’ perspectives and implement strategies to improve understanding and collaborative decision-making in their practice.
Supplemental Material
Supplemental material, 852007_Supplementary_material for Communication between healthcare professionals and relatives of patients approaching the end-of-life: A systematic review of qualitative evidence by Rebecca J Anderson, Steven Bloch, Megan Armstrong, Patrick C Stone and Joseph TS Low in Palliative Medicine
Acknowledgments
The authors would like to acknowledge Marie Curie for providing funding for the UCL Marie Curie Palliative Care Research Department. P.S., M.A. and J.L. are supported by the University College Hospital National Institute for Health Research Biomedical Research Centre. The authors are grateful to the librarians at the University College London Language & Speech Science Library for their help in developing the search strategy and to Bridget Candy for methodological advice.
Footnotes
Author Contributions: R.A., S.B., P.S. and J.L. were responsible for the study concept and design; R.A., M.A. and J.L. were responsible for the acquisition, analysis and interpretation of the data. R.A. drafted the article; S.B., M.A., P.S. and J.L. revised it critically for important intellectual content. All authors approved the version to be published and have participated sufficiently in the work to take public responsibility for appropriate portions of the content.
Data sharing and management: The full search strategy, inclusion/exclusion criteria, quality appraisal results and example extracts demonstrating the review’s themes are available in the Supplementary material. This review is registered on the PROSPERO database (registration number CRD42017065560).
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This systematic review was carried out as part of a PhD funded by the Marie Curie Chair in Palliative and End of Life Care grant (grant MCCC-FCH-13-U). PS and RA’s posts are supported by the Marie Curie Chair in Palliative and End of Life Care grant funding; JL’s post is supported by the Marie Curie core and programme grant funding (grants MCCC-FCO-16-U and MCCC-FPO-16-U). The funder played no role in the collection, analysis and interpretation of data, in the writing of the report or in the decision to submit the article for publication.
Supplemental material: Supplemental material for this article is available online.
ORCID iDs: Rebecca J Anderson  https://orcid.org/0000-0002-7095-8914
https://orcid.org/0000-0002-7095-8914
Megan Armstrong  https://orcid.org/0000-0001-6773-9393
https://orcid.org/0000-0001-6773-9393
References
- 1. Kirk P. What do patients receiving palliative care for cancer and their families want to be told? A Canadian and Australian qualitative study. BMJ 2004; 328: 1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nelson JE, Puntillo KA, Pronovost PJ, et al. In their own words: patients and families define high-quality palliative care in the intensive care unit. Crit Care Med 2010; 38(3): 808–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Steinhauser KE, Voils CI, Bosworth H, et al. What constitutes quality of family experience at the end of life? Perspectives from family members of patients who died in the hospital. Palliat Support Care 2014; 13: 945–952. [DOI] [PubMed] [Google Scholar]
- 4. Virdun C, Luckett T, Davidson PM, et al. Dying in the hospital setting: a systematic review of quantitative studies identifying the elements of end-of-life care that patients and their families rank as being most important. Palliat Med 2015; 29(9): 774–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wright AA, Zhang B, Ray A, et al. Associations between end-of-life discussions, patient mental health, medical care near death, and caregiver bereavement adjustment. JAMA 2008; 300(14): 1665–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nielsen MK, Neergaard MA, Jensen AB, et al. Predictors of complicated grief and depression in bereaved caregivers: a nationwide prospective cohort study. J Pain Symptom Manage 2017; 53(3): 540–550. [DOI] [PubMed] [Google Scholar]
- 7. Kim Y, Carver CS, Spiegel D, et al. Role of family caregivers’ self-perceived preparedness for the death of the cancer patient in long-term adjustment to bereavement. Psychooncology 2017; 26(4): 484–492. [DOI] [PubMed] [Google Scholar]
- 8. Barry LC, Kasl SV, Prigerson HG. Psychiatric disorders among bereaved persons: the role of perceived circumstances of death and preparedness for death. Am J Geriatr Psychiatry 2002; 10(4): 447–457. [PubMed] [Google Scholar]
- 9. Royak-Schaler R, Gadalla S, Lemkau J, et al. Family perspectives on communication with healthcare providers during end-of-life cancer care. Oncol Nurs Forum 2006; 33(4): 753–760. [DOI] [PubMed] [Google Scholar]
- 10. Hinkle LJ, Bosslet GT, Torke AM. Factors associated with family satisfaction with end-of-life care in the ICU: a systematic review. Chest 2015; 147: 82–93. [DOI] [PubMed] [Google Scholar]
- 11. Almack K, Cox K, Moghaddam N, et al. After you: conversations between patients and healthcare professionals in planning for end of life care. BMC Palliat Care 2012; 11: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Raijmakers NJH, van Zuylen L, Costantini M, et al. Issues and needs in end-of-life decision making: an international modified Delphi study. Palliat Med 2012; 26(7): 947–953. [DOI] [PubMed] [Google Scholar]
- 13. Parliamentary and Health Service Ombudsman. Dying without dignity. London: Parliamentary and Health Service Ombudsman, 2015. [Google Scholar]
- 14. National Institute for Health and Care Excellence. Care of dying adults in the last days of life, 2015. https://www.nice.org.uk/guidance/NG31 [PubMed]
- 15. Bernacki RE, Block SD. Communication about serious illness care goals. JAMA Intern Med 2014; 174: 1994–2003. [DOI] [PubMed] [Google Scholar]
- 16. Parker SM, Clayton JM, Hancock K, et al. A systematic review of prognostic/end-of-life communication with adults in the advanced stages of a life-limiting illness: patient/caregiver preferences for the content, style, and timing of information. J Pain Symptom Manage 2007; 34(1): 81–93. [DOI] [PubMed] [Google Scholar]
- 17. Coombs MA, Parker R, Ranse K, et al. An integrative review of how families are prepared for, and supported during withdrawal of life-sustaining treatment in intensive care. J Adv Nurs 2017; 73(1): 39–55. [DOI] [PubMed] [Google Scholar]
- 18. Docherty A, Owens A, Asadi-Lari M, et al. Knowledge and information needs of informal caregivers in palliative care: a qualitative systematic review. Palliat Med 2008; 22(2): 153–171. [DOI] [PubMed] [Google Scholar]
- 19. Loke AY, Li Q, Man LS. Preparing family members for the death of their loved one with cancer: a review of literature and direction for future research. J Hosp Palliat Nurs 2013; 15: E1–E11. [Google Scholar]
- 20. Lowey SE. Communication between the nurse and family caregiver in end-of-life care: a review of the literature. J Hosp Palliat Nurs 2008; 10: 35–48. [Google Scholar]
- 21. Hancock K, Clayton JM, Parker SM, et al. Discrepant perceptions about end-of-life communication: a systematic review. J Pain Symptom Manage 2007; 34(2): 190–200. [DOI] [PubMed] [Google Scholar]
- 22. Witkamp FE, van Zuylen L, Vergouwe Y, et al. Concordance between experiences of bereaved relatives, physicians, and nurses with hospital end-of-life care: everyone has their ‘own truth’. Int J Palliat Care 2015; 2015: 623890. [Google Scholar]
- 23. Noome M, Beneken Genaamd Kolmer DM, van Leeuwen E, et al. The nursing role during end-of-life care in the intensive care unit related to the interaction between patient, family and professional: an integrative review. Scand J Caring Sci 2016; 30(4): 645–661. [DOI] [PubMed] [Google Scholar]
- 24. Lockwood C, Munn Z, Porritt K. Qualitative research synthesis: methodological guidance for systematic reviewers utilizing meta-aggregation. Int J Evid Based Healthc 2015; 13(3): 179–187. [DOI] [PubMed] [Google Scholar]
- 25. Hannes K, Lockwood C, Pearson A. A comparative analysis of three online appraisal instruments’ ability to assess validity in qualitative research. Qual Health Res 2010; 20(12): 1736–1743. [DOI] [PubMed] [Google Scholar]
- 26. Richards CA, Starks H, O’Connor MR, et al. Physicians perceptions of shared decision-making in neonatal and pediatric critical care. Am J Hosp Palliat Care 2018; 35(4): 669–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008; 8: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Suri H. Epistemological pluralism in research synthesis methods. Int J Qual Stud Educ 2013; 26: 889–911. [Google Scholar]
- 29. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62: 1006–1012. [DOI] [PubMed] [Google Scholar]
- 30. Aldridge M, Barton E. Establishing terminal status in end-of-life discussions. Qual Health Res 2007; 17(7): 908–918. [DOI] [PubMed] [Google Scholar]
- 31. Barton E, Aldridge M, Trimble T, et al. Structure and variation in end-of-life discussions in the surgical intensive care unit. Commun Med 2005; 2(1): 3–20. [DOI] [PubMed] [Google Scholar]
- 32. Barton E. Situating end-of-life decision making in a hybrid ethical frame. Commun Med 2007; 4(2): 131–140. [DOI] [PubMed] [Google Scholar]
- 33. Curtis JR, Engelberg RA, Wenrich MD, et al. Studying communication about end-of-life care during the ICU family conference: development of a framework. J Crit Care 2002; 17(3): 147–160. [DOI] [PubMed] [Google Scholar]
- 34. Curtis JR, Engelberg RA, Wenrich MD, et al. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005; 171(8): 844–849. [DOI] [PubMed] [Google Scholar]
- 35. De Vos MA, Bos AP, Plotz FB, et al. Talking with parents about end-of-life decisions for their children. Pediatrics 2015; 135(2): e465–e476. [DOI] [PubMed] [Google Scholar]
- 36. Ekberg S, Danby S, Herbert A, et al. Affording opportunities to discuss deterioration in paediatric palliative care consultations: a conversation analytic study. BMJ Support Palliat Care. Epub ahead of print 7 March 2017. DOI: 10.1136/bmjspcare-2016-001130. [DOI] [PubMed] [Google Scholar]
- 37. Engelberg RA, Wenrich MD, Curtis JR. Responding to families’ questions about the meaning of physical movements in critically ill patients. J Crit Care 2008; 23(4): 565–571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Hsieh HF, Shannon SE, Curtis JR. Contradictions and communication strategies during end-of-life decision making in the intensive care unit. J Crit Care 2006; 21(4): 294–304. [DOI] [PubMed] [Google Scholar]
- 39. Kawashima M. Four ways of delivering very bad news in a Japanese emergency room. Res Lang Soc Interac 2017; 50: 307–325. [Google Scholar]
- 40. Miller DK, Coe RM, Hyers TM. Achieving consensus on withdrawing or withholding care for critically ill patients. J Gen Intern Med 1992; 7: 475–480. [DOI] [PubMed] [Google Scholar]
- 41. Pecanac KE. Communicating delicately: introducing the need to make a decision about the use of life-sustaining treatment. Health Commun 2017; 32(10): 1261–1271. [DOI] [PubMed] [Google Scholar]
- 42. Shaw C, Stokoe E, Gallagher K, et al. Parental involvement in neonatal critical care decision-making. Sociol Health Illn 2016; 38(8): 1217–1242. [DOI] [PubMed] [Google Scholar]
- 43. West HF, Engelberg RA, Wenrich MD, et al. Expressions of nonabandonment during the intensive care unit family conference. J Palliat Med 2005; 8(4): 797–807. [DOI] [PubMed] [Google Scholar]
- 44. Abib El, Halal GM, Piva JP, Lago PM, et al. Parents’ perspectives on the deaths of their children in two Brazilian paediatric intensive care units. Int J Palliat Nurs 2013; 19(10): 495–502. [DOI] [PubMed] [Google Scholar]
- 45. Gordon C, Barton E, Meert KL, et al. Accounting for medical communication: parents’ perceptions of communicative roles and responsibilities in the pediatric intensive care unit. Commun Med 2009; 6(2): 177–188 [PMC free article] [PubMed] [Google Scholar]
- 46. Lind R. Sense of responsibility in ICU end-of-life decision-making: relatives’ experiences. Nurs Ethics 2019; 26: 270–279. [DOI] [PubMed] [Google Scholar]
- 47. Meert KL, Eggly S, Pollack M, et al. Parents’ perspectives on physician-parent communication near the time of a child’s death in the pediatric intensive care unit. Pediatr Crit Care Med 2008; 9(1): 2–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Odgers J. No one said he was dying: families’ experiences of end-of-life care in an acute setting. Aust J Adv Nurs 2018; 35: 21–31. [Google Scholar]
- 49. Bach V, Ploeg J, Black M. Nursing roles in end-of-life decision making in critical care settings. West J Nurs Res 2009; 31(4): 496–512. [DOI] [PubMed] [Google Scholar]
- 50. Bartel DA, Engler AJ, Natale JE, et al. Working with families of suddenly and critically ill children: physician experiences. Arch Pediatr Adolesc Med 2000; 154(11): 1127–1133. [DOI] [PubMed] [Google Scholar]
- 51. Bloomer MJ, Endacott R, Ranse K, et al. Navigating communication with families during withdrawal of life-sustaining treatment in intensive care: a qualitative descriptive study in Australia and New Zealand. J Clin Nurs 2017; 26(5–6): 690–697. [DOI] [PubMed] [Google Scholar]
- 52. Epstein EG. End-of-life experiences of nurses and physicians in the newborn intensive care unit. J Perinatol 2008; 28(11): 771–778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Kehl KA. How hospice staff members prepare family caregivers for the patient’s final days of life: an exploratory study. Palliat Med 2015; 29(2): 128–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Liaschenko J, O’Conner-Von S, Peden-McAlpine C. The ‘big picture’: communicating with families about end-of-life care in intensive care unit. Dimens Crit Care Nurs 2009; 28: 224–231. [DOI] [PubMed] [Google Scholar]
- 55. Peden-McAlpine C, Liaschenko J, Traudt T, et al. Constructing the story: how nurses work with families regarding withdrawal of aggressive treatment in ICU – a narrative study. Int J Nurs Stud 2015; 52(7): 1146–1156. [DOI] [PubMed] [Google Scholar]
- 56. Rejno A, Silfverberg G, Ternestedt BM. Reasoning about truth-telling in end-of-life care of patients with acute stroke. Nurs Ethics 2017; 24(1): 100–110. [DOI] [PubMed] [Google Scholar]
- 57. Tan A, Manca D. Finding common ground to achieve a ‘good death’: family physicians working with substitute decision-makers of dying patients. A qualitative grounded theory study. BMC Fam Pract 2013; 14: 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Caswell G, Pollock K, Harwood R, et al. Communication between family carers and health professionals about end-of-life care for older people in the acute hospital setting: a qualitative study. BMC Palliat Care 2015; 14: 35–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Meeker MA, Waldrop DP, Seo JY. Examining family meetings at end of life: the model of practice in a hospice inpatient unit. Palliat Support Care 2015; 13(5): 1283–1291. [DOI] [PubMed] [Google Scholar]
- 60. Cassell J. Life and death in intensive care. Philadelphia, PA: Temple University Press, 2005. [Google Scholar]
- 61. Meert KL, Eggly S, Pollack M, et al. Parents’ perspectives regarding a physician-parent conference after their child’s death in the pediatric intensive care unit. J Pediatr 2007; 151(1): 50–55.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Maynard DW. On clinicians co-implicating recipients’ perspective in the delivery of diagnostic news. In: Drew P, Heritage J. (eds) Talk at work: interaction in institutional settings. Cambridge: Cambridge University Press, 1992, pp. 331–358. [Google Scholar]
- 63. Wendler D, Rid A. Systematic review: the effect on surrogates of making treatment decisions for others. Ann Intern Med 2011: 336–346. [DOI] [PubMed] [Google Scholar]
- 64. Dyer C. Law, ethics, and emotion: the Charlie Gard case. BMJ 2017; 358: j3152. [DOI] [PubMed] [Google Scholar]
- 65. Dyer C. Doctors can stop ventilating 11 month old boy brain damaged at birth. BMJ 2018; 360: k482. [DOI] [PubMed] [Google Scholar]
- 66. Brighton LJ, Selman LE, Bristowe K, et al. Emotional labour in palliative and end-of-life care communication: a qualitative study with generalist palliative care providers. Patient Educ Couns 2019; 102: 494–502. [DOI] [PubMed] [Google Scholar]
- 67. Addington-Hall JM, O’Callaghan AC. A comparison of the quality of care provided to cancer patients in the UK in the last three months of life in in-patient hospices compared with hospitals, from the perspective of bereaved relatives: results from a survey using the VOICES questionnaire. Palliat Med 2009; 23(3): 190–197. [DOI] [PubMed] [Google Scholar]
- 68. Brandes K, Linn AJ, Butow PN, et al. The characteristics and effectiveness of question prompt list interventions in oncology: a systematic review of the literature. Psychooncology 2015; 24(3): 245–252. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, 852007_Supplementary_material for Communication between healthcare professionals and relatives of patients approaching the end-of-life: A systematic review of qualitative evidence by Rebecca J Anderson, Steven Bloch, Megan Armstrong, Patrick C Stone and Joseph TS Low in Palliative Medicine