Abstract
Background and Aims:
Fentanyl can facilitate controlled intraoperative hypotension by its sympatholytic effect in patients undergoing functional endoscopic sinus surgery (FESS). We investigated the effects of different doses of pre-induction fentanyl on controlled hypotension profile during FESS.
Methods:
This prospective, randomised study included 120 patients randomly allocated to three groups (40 each) based on administration of pre-induction fentanyl; 2 μg/kg group, 3 μg/kg group and 4 μg/kg group. The primary objective was to assess effect on intraoperative heart rate and mean arterial pressure. Use of additional hypotensive agents, surgical field condition and surgeon satisfaction were also analysed.
Results:
Controlled hypotension was achieved adequately in all participants. Patients belonging to fentanyl 4 μg/kg group had significantly lower heart rate for the duration of controlled hypotension intraoperatively versus fentanyl 2 μg/kg group (P < 0.05). Trinitroglycerin [TNG] and metoprolol were administered to 3 [7.5%] and 9 [22.5%] patients respectively in the fentanyl 3 μg/kg group, and to 3 [7.5%] and 5 [12.5%] patients respectively in the 4 μg/kg group, compared to 14 [35%] and 20 [50%] in the fentanyl 2 μg/kg group, respectively (TNG, P < 0.001). Surgical field conditions and surgeon satisfaction scores were significantly superior in fentanyl 3 μg/kg and 4 μg/kg groups than in fentanyl 2 μg/kg group.
Conclusion:
Pre-induction fentanyl 3 μg/kg and 4 μg/kg group showed superior controlled hypotension facilitation than 2 μg/kg fentanyl during FESS in terms of measurable haemodynamic endpoints and favourable operative conditions, surgeon's satisfaction and sparing of additional hypotensive agents.
Key words: Controlled hypotension, endoscopy, fentanyl, paranasal sinuses, surgery
INTRODUCTION
Functional endoscopic sinus surgery (FESS) is a commonly performed procedure for paranasal sinus disease. Since the proximity of vital structures (the brain, orbit and carotid vessels), limited space to operate and bleeding during the procedure obscuring endoscopic vision may result in greater propensity of negative surgical outcomes (dural puncture, orbital/optic nerve trauma, heamorrhage),[1] institution of induced hypotension during FESS is an absolute necessity. However, the commonly used hypotensive agents utilised to effect controlled hypotension for providing bloodless surgical field may have distressing side effects including vasodilatation (halogenated compounds),[2] tachyphylaxis (nitrates);[3] sedation, delayed recovery (clonidine);[4] heart blocks and rebound hypertension (beta-blockers)[5] among others.
This study explored the impact of predominant sympatho-adrenal suppression effect (lowers heart rate and blood pressure)[6] of different fentanyl doses (2 μg/kg, 3 μg/kg, 4 μg/kg) in facilitating controlled hypotension during FESS (primary objective); hypotensive agent sparing, surgical field condition and surgeon satisfaction (secondary objectives).
METHODS
After acquiring Institutional Ethics Committee approval (no. EC/06/10/132) and written informed consent from the patient/participants; this single-centre, prospective, randomised-controlled, double-blind, three-arm, dose-finding study included 120 adults, of either sex, aged between 20–60 years and belonging to American Society Anaesthesiologists (ASA) physical status I/II. The patients underwent bilateral FESS for sinusitis of non-fungal origin under general anaesthesia (GA). The study duration was 24 months and the study period was from 2nd September 2010 to 30th August 2012. Patients with uncontrolled hypertension, pre-existing hyper-reactive airway disease, known opioid hypersensitivity/allergy, uncompensated systemic illness (hepato-renal, cardiovascular, respiratory and endocrine), psychiatric disorders, alcohol/substance abuse and smokers were excluded from the study. The clinical trial was registered with the Clinical Trial Registry of India (CTRI No. 2014/03/004457). In all respect, the study was conducted in adherence to principles enshrined in the Declaration-of-Helisinki (DoH).
Prior to induction of anaesthesia, different doses of fentanyl were administered to the patients randomly assigned to one of the three groups. To effect blinding, a bolus of 5 ml 0.9% saline containing 1 μg/kg fentanyl or none was administered as per group allocation plan given below.
Patients belonging to the fentanyl 2 μg/kg group (group 1, n = 40) received fentanyl 1 μg/kg IV bolus (diluted in 5 ml 0.9% saline) administered twice at 0 and 3 min time point followed by two empty IV boluses (5 ml 0.9% saline) at 6 and 9 min time point. The patients of fentanyl 3 μg/kg group (group 2, n = 40) received fentanyl 1 μg/kg IV bolus (diluted in 5 ml 0.9% saline) administered thrice at 0, 3 and 6 min time point followed by one empty bolus (5 ml 0.9% saline) at 9 min time point. The patients of the fentanyl 4 μg/kg group (group 3, n = 40) were administered fentanyl 1 μg/kg IV bolus (diluted in 5 ml 0.9% saline) four times at 0, 3, 6 and 9 min time point and no empty bolus (5 ml 0.9% saline) was given. The investigator, patient and clinical assessor were blinded to the study groups.
All patients received oral diazepam (5 mg) the evening before and ranitidine (150 mg) 45 min before surgery. Routine monitoring (pulse-oximetry, electrocardiogram [ECG], non-invasive blood pressure [NIBP]) was applied. Two peripheral intravenous accesses were established, one for fluids and drug administration and the other dedicated to propofol infusion. Pre-induction fentanyl was administered to the participants as per the randomised dose allocation plan (2 μg/kg or 3 μg/kg or 4 μg/kg). Anaesthesia was induced with propofol 2 mg/kg IV followed by atracurium besylate 0.5 mg/kg IV to facilitate tracheal intubation. GA was maintained with propofol total intravenous anaesthesia (TIVA) started at 150 μg/kg/min and was titrated to maintain a bi-spectral index (BIS) score from range 40–60. Muscle relaxation for the operative duration included atracurium infusion at 25 mg/h. Ventilator settings (volume-controlled ventilation, frequency 14/min, tidal volume 8.0 ml/kg, I: E ratio1:2; Penlon AVS, Penlon Ltd., Abingdon, UK), tracheal-tube size (7.5mm I.D [males], 6.5mm I.D [females]) and breathing-system (circle-CO2 absorber) were standardised across the study participants. For the duration of controlled ventilation, N2O was not used. Patients lungs were ventilated with O2: air mixture with FiO2 set at 0.5 and fresh gas flow 1.0 l/min. Atracurium infusion was stopped once the endoscopic intervention was finished and before nasal packing was undertaken. Continuous propofol infusion was stopped once nasal packing was completed. At the end of the surgery, the residual neuromuscular blockade was reversed with neostigmine (50 μg/kg) and glycopyrrolate (10 μg/kg) IV. Tracheal extubation was undertaken once the patients were wide awake and following commands.
As a safety measure, after the institution of GA, trinitroglycerine (TNG) IV infusion was used to maintain MAP within the targeted range of 60–70 mmHg throughout the duration of controlled hypotension. NIBP was monitored every 5 min. A single bolus of fentanyl 0.5 μg/kg was administered if the MAP exceeded 70 mmHg. Any exclusive or attendant (to NIBP rise) increase in HR above 90 beats/min was treated with metoprolol (1 mg) IV bolus. In case of non-response to additional fentanyl IV bolus, TNG infusion was started at 0.5 μg/kg/min and titrated to effect all the groups. Every time care was exercised to keep the dose range within the standard prescribed limits (0.5–2 μg/kg/min). The frequency of use of fentanyl, metoprolol and trinitroglycerine was noted for each group.
The outcome measures assessed were surgical field condition (SFC)[3] surgeon satisfaction profile (SSP),[7] emergence agitation using Aono's scale,[8] post-operative pain using visual analogue scale (VAS),[9] and post-operative nausea and vomiting using PONV scoring system[10] [Table 1].
Table 1.
Outcome measures assessment scores
| Surgical field conditions (SFC) |
| No bleeding |
| Slight bleeding- blood evacuation not necessary |
| Slight bleeding- occasional blood evacuation needed and operative field visible always |
| Slight bleeding- blood must be often evacuated and operative field is visible for some seconds after evacuation |
| Average bleeding- blood must be often evacuated and operative field visible only immediately after the evacuation |
| Severe bleeding- constant evacuation required and the bleeding appears faster than can be evacuated by suction, severely threatening the surgical field |
| Surgeon satisfaction profile (SSP) |
| Fully satisfied |
| Satisfied |
| Just satisfied |
| Not satisfied |
| Aono’s scale for post-operative emergence agitation |
| Calm |
| Not calm but could be easily calmed |
| Moderately agitated or restless |
| Combative, excited, disoriented |
| Post-operative pain |
| 10 cm visual analogue scale (VAS) |
| Post-operative nausea and vomiting scoring system |
| No emetic symptoms |
| Nausea |
| Vomiting |
In the early recovery period (up to 6 hours), post-operative analgesia was given in the form of a single diclofenac sodium 75 mg bolus. Thereafter, the analgesic protocol of the surgical unit was followed. Post-operative nausea and vomiting were treated with ondansetron 4–8 mg bolus.
For an effective institution of intraoperative controlled hypotension, a mean arterial pressure (MAP) range of 60–70 mmHg was adjudicated as the desired target. The total sample size of 120 (40 patients/group) was calculated with a power of 80% and α-value of 0.05. A standard deviation of 10 mmHg was assumed to detect a significant difference of 10% in MAP between any of the two groups from the point of institution of controlled hypotension. A P value of less than 0.05 was considered statistically significant.
The patients were randomly allocated to one of the three groups based on a computer generated random number table (url:stattrek.com/statistics/random-number-generator.aspx). Randomisation sequence concealment included opaque-sealed envelopes with alphabetic codes whose distribution was in control of an independent analyst. The envelopes were opened in the pre-operative waiting room just before shifting the patient to the operating room (OR) area. After allocation, patient's data-slip was pasted on the empty envelope, which was then sent back to the control analyst.
Statistical analysis was performed using the Statistical Package for the Social Sciences software (SPSS) version 17.0 programme for Windows (SPSS Inc., Chicago, IL, USA). Normal distribution of the data was verified with the Shapiro Wilk test. Reporting of parametric and non-parametric data was represented by mean ± standard deviation and medians with quartiles, respectively. Categorical data were presented as the frequency with percentage. Normally distributed continuous variables including age, weight, height, duration of surgery, mean arterial pressure, heart rate and propofol dosage were compared using analysis of variance (ANOVA). Corrections for comparing three treatment groups were made. Multiple comparison test was utilised to assess the homogeneity/differences between the individual groups using Bonferroni or Tamhane's T2 test. The Kruskal-Wallis test was used for surgeon satisfaction score and Aono's scale. Further comparisons were done using the Mann Whitney U test. Categorical variables such as gender distribution; frequency of TNG, metoprolol and fentanyl administration; and incidence of PONV were analysed using the Chi-square test.
RESULTS
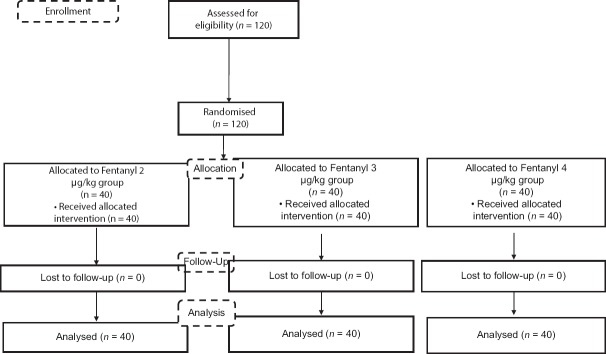
All the participants, randomised to one of the three study groups (40 group; n = 120) completed the study [Figure 1: Consolidated Standards for Reporting Trials [CONSORT] flow diagram]. The participants in the three study groups, viz. fentanyl 2 μg/kg, fentanyl 3 μg/kg and fentanyl 4 μg/kg, were comparable for demographic parameters (age, height, weight, gender). The duration of surgery in fentanyl 2 μg/kg group (127.53 ± 12.39 min) was significantly lower than the patients belonging to fentanyl 3 μg/kg (135.35 ± 19.80 min) and fentanyl 4 μg/kg (136.28 ± 14.51 min) group (P = 0.002).
Figure 1.
CONSORT Flow Diagram
Controlled hypotension was achieved adequately in all the participants belonging to the three groups. With incidental exceptions, the MAP was comparable across the three study groups [Table 2]. Though there was no difference in the baseline (pre-induction) heart rate in the three study groups; intraoperatively, patients in receipt of fentanyl 4 μg/kg had significantly lower heart rate when compared with fentanyl 2 μg/kg for the larger duration of controlled hypotension [Table 3]. Intraoperatively, the difference in propofol usage (absolute total, rate-mg/min) was non-significant for the three groups [Table 4]. When compared to the patients of fentanyl 3 μg/kg (n = 3, 7.5%) and fentanyl 4 μg/kg (n = 3, 7.5%) groups, significantly greater number of participants in the fentanyl 2 μg/kg group (n = 14, 35%) required trinitroglycerine infusion (P < 0.001) [Table 4]. Further, the use of intraoperative metoprolol and fentanyl was significantly lower in the fentanyl 4 μg/kg group (P < 0.001) [Table 4].
Table 2.
Mean arterial pressure profile
| Time | Fentanyl 2 µg/kg Group (n=40) | Fentanyl 3 µg/kg Group (n=40) | Fentanyl 4 µg/kg Group (n=40) | P | Fentanyl 2 µg/kg vs 3 µg/kg | Fentanyl 2 µg/kg vs 4 µg/kg | Fentanyl 3 µg/kg vs 4 µg/kg |
|---|---|---|---|---|---|---|---|
| Pre-induction | 97.50±13.20 | 95.64±13.06 | 94.70±11.68 | 0.604 | 0.791 | 0.585 | 0.942 |
| Pre-intubation | 75.52±13.14 | 72.35±13.45 | 71.18±11.48 | 0.290 | 0.506 | 0.281 | 0.910 |
| 5 min post-intubation | 90.60±16.38 | 88.28±18.27 | 86.05±15.30 | 0.478 | 0.808 | 0.445 | 0.823 |
| 10 min post-intubation | 69.52±12.89 | 69.68±10.15 | 70.55±11.87 | 0.914 | 0.998 | 0.919 | 0.940 |
| 20 min post-intubation | 68.32±9.38 | 62.22±8.40 | 62.22±12.85 | 0.012* | 0.026* | 0.026 | 1.000 |
| 30 min post-intubation | 66.38±8.55 | 64±8.69 | 66.12±8.13 | 0.389 | 0.423 | 0.990 | 0.502 |
| 40 min post-intubation | 68±9.70 | 64.38±9.04 | 65.12±6.76 | 0.142 | 0.147 | 0.297 | 0.920 |
| 50 min post-intubation | 69.68±10.38 | 66.65±12.09 | 66.22±7.74 | 0.262 | 0.385 | 0.291 | 0.981 |
| 60 min post-intubation | 69.35±9.81 | 65.72±8.70 | 66.15±6.51 | 0.116 | 0.138 | 0.212 | 0.973 |
| 70 min post-intubation | 69.48±8.36 | 66.40±7.60 | 67.38±7.31 | 0.199 | 0.184 | 0.451 | 0.841 |
| 80 min post-intubation | 68.42±7.93 | 65.75±8.77 | 67.52±6.93 | 0.310 | 0.289 | 0.867 | 0.576 |
| 90 min post-intubation | 70.78±10.54 | 68.80±9.32 | 66.30±7.08 | 0.092 | 0.596 | 0.075 | 0.438 |
| 100 min post-intubation | 68.70±7.77 | 67.78±8.81 | 67.72±7.34 | 0.828 | 0.863 | 0.849 | 1.000 |
| 110 min post-intubation | 68.50±7.09 | 66.35±8.75 | 69.05±7.22 | 0.260 | 0.430 | 0.946 | 0.266 |
| 120 min post-intubation | 70.02±7.83 | 68.80±9.03 | 68.72±7.65 | 0.729 | 0.782 | 0.758 | 0.999 |
Values expressed as mean±SD; *P<0.05 significant
Table 3.
Heart rate profile
| Time | Fentanyl 2 µg/kg Group (n=40) | Fentanyl 3 µg/kg Group (n=40) | Fentanyl 4 µg/kg Group (n=40) | P | Fentanyl 2 µg/kg vs 3 µg/kg | Fentanyl 2 µg/kg vs 4 µg/kg | Fentanyl 3 µg/kg vs 4 µg/kg |
|---|---|---|---|---|---|---|---|
| Pre-induction | 88.30±14.77 | 88.48±12.90 | 89.05±12.87 | 0.967 | 0.998 | 0.967 | 0.980 |
| Pre-intubation | 73.30±11.94 | 72.58±10.83 | 67.62±11.34 | 0.056 | 0.656 | 0.070* | 0.131 |
| 5 min post-intubation | 85.72±15.28 | 77.40±14.30 | 77.30±12.07 | 0.010* | 0.023* | 0.021* | 0.999 |
| 10 min post-intubation | 71.35±12.68 | 70.10±12.96 | 68.95±11.85 | 0.693 | 0.896 | 0.668 | 0.911 |
| 20 min post-intubation | 67.88±10.18 | 64.18±9.49 | 62.48±8.66 | 0.036* | 0.192 | 0.032* | 0.702 |
| 30 min post-intubation | 64.35±8.18 | 60.22±11.78 | 59.38±7.50 | 0.043* | 0.123 | 0.049* | 0.913 |
| 40 min post-intubation | 62.28±7.17 | 60.92±8.13 | 57.48±5.96 | 0.010* | 0.676 | 0.009* | 0.082 |
| 50 min post-intubation | 61.75±6.78 | 61.35±9.03 | 57.10±5.73 | 0.008* | 0.968 | 0.014* | 0.028* |
| 60 min post-intubation | 61.78±7.12 | 61.12±8.04 | 57.48±6.11 | 0.017* | 0.913 | 0.022* | 0.061 |
| 70 min post-intubation | 62.18±8.14 | 60.05±7.44 | 58.25±6.46 | 0.063 | 0.405 | 0.050 | 0.522 |
| 80 min post-intubation | 63.28±9.51 | 61.10±8.73 | 58.40±7.08 | 0.040* | 0.489 | 0.031* | 0.334 |
| 90 min post-intubation | 62.98±7.75 | 61.32±8.00 | 58.10±6.44 | 0.014* | 0.583 | 0.011* | 0.132 |
| 100 min post-intubation | 61.52±6.50 | 60.98±7.10 | 57.38±5.27 | 0.008* | 0.920 | 0.011* | 0.033* |
| 110 min post-intubation | 62.50±8.29 | 60.22±6.67 | 58.85±4.94 | 0.056 | 0.294 | 0.046* | 0.636 |
| 120 min post-intubation | 62.32±7.66 | 60.38±6.36 | 57.90±5.45 | 0.012* | 0.381 | 0.009* | 0.214 |
Values expressed as mean±SD, *P<0.05 significant
Table 4.
Intraoperative drug usage
| Drug | Fentanyl 2 µg/kg Group (n=40) | Fentanyl 3 µg/kg Group (n=40) | Fentanyl 4 µg/kg Group (n=40) | P |
|---|---|---|---|---|
| Propofol | ||||
| Total (mg) | 946.22±378.22 | 1000.93±288.89 | 836.57±280.19 | 0.060 |
| Rate (mg/min) | 7.51±3.16 | 7.47±2.30 | 6.17±2.05 | 0.061 |
| TNG (f, %) | 14 (35%) | 3 (7.5%) | 3 (7.5%) | <0.001 |
| Metoprolol (f, %) | 20 (50%) | 9 (22.5%) | 5 (12.5%) | <0.001 |
| Fentanyl (f, %) | 29 (72.5%) | 14 (35%) | 11 (27.5%) | <0.001 |
TNG – Trinitroglycerin, Values expressed as mean±SD and frequency, %, P<0.05 significant
On a 6-point scale, the mean SFC score was significantly higher in patients of fentanyl 2 μg/kg group than those who received fentanyl 3 μg/kg and fentanyl 4 μg/kg (P = 0.041) [Table 5]. The surgeons were significantly less satisfied with the operating condition in fentanyl 2 μg/kg group (P = 0.000) [Table 5]. On Aono's scale [Table 5] for assessing emergence from anaesthesia, the participants belonging to fentanyl 3 μg/kg group were significantly calm (n = 34, 85%, Aono score 1) and less agitated (cumulative Aono's score 3 and 4: fentanyl 3 μg/kg, n = 6, 15%; fentanyl 4 μg/kg, n = 8, 20%; fentanyl 2 μg/kg, n = 11, 27.5%) (P = 0.05) [Table 5]. At 6 hour time point, post-operative pain (10 cm VAS scale) was significantly lower in patients who received fentanyl 3 μg/kg and fentanyl 4 μg/kg than those who received fentanyl 2 μg/kg (P = 0.015) [Table 5]. Except for a solitary incidence of PONV in the fentanyl 3 μg/kg group, none of the study participants experienced PONV [Table 5].
Table 5.
Surgical field condition, surgeon satisfaction profile and post-operative morbid variables (emergence agitation, pain, PONV)
| Fentanyl 2 µg/kg Group (n=40) | Fentanyl 3 µg/kg Group (n=40) | Fentanyl 4 µg/kg Group (n=40) | P | |
|---|---|---|---|---|
| SFC | 2.08±0.656 | 1.78±0.577 | 1.75±0.588 | 0.041 |
| SSP | 1 (0-3) | 1 (0-2) | 0 (0-3) | 0.000 |
| Aono’s Scale | 1 (1-4) | 1 (1-3) | 1 (1-4) | 0.204 |
| VAS at 6 h | 2.22±1.09 | 1.80±0.96 | 1.58±0.59 | 0.015 |
| PONV (f, %) | 0 (0.0%) | 1 (2.5%) | 0 (0.0%) | 0.365 |
Values expressed as: SFC – Surgical field condition (mean±SD); SSP – Surgeon satisfaction profile (median with IQR); PONV – Post-operative nausea and vomiting (frequency, %); VAS – Visual analogue scale (mean±SD), P<0.05 significant
DISCUSSION
Our study results revealed that although controlled hypotension could be instituted and maintained adequately in all the participants, superior surgical field conditions (SFC) and surgeon satisfaction scores (SSS) were observed only in patients who received higher doses of pre-induction fentanyl (3 or 4 μg/kg instead of 2 μg/kg). In addition, compared to 2 μg/kg fentanyl group of patients, the quantitative use of TNG and beta-blockers to sustain controlled hypotension was significantly lower in patients who received fentanyl 3 or 4 μg/kg. Probably, the presence of a lower heart rate in the patients who received pre-fentanyl 3 and 4 μg/kg accounted for preceding effect and consequently resulted in improved endoscopic view during FESS. This reinforces our hypothesis that the sympatholytic effect of pre-induction fentanyl, especially its effect on the heart rate, tails into the early intraoperative period and facilitates controlled hypotension. Therefore, a lower heart rate achieved with pre-induction fentanyl before induction of anaesthesia appears to be an important determinant for institution and facilitation of a robust controlled hypotension state during FESS. The supporting evidence for the above effect can be: first, a lower requirement (frequency, quantity) of hypotensive agents in patients who received fentanyl 3 μg/kg and 4 μg/kg was considered significant given that the study population was homogenous and randomised and overall propofol consumption was comparable across the study groups; second, confounders (type of hypotensive agents used, patient factors) notwithstanding the presence of a lower heart rate for the duration of controlled hypotension in participants who received pre-induction fentanyl in doses of 3 μg/kg and 4 μg/kg had significantly superior SFC and SSS than those who were administered 2 mg/kg dose.
A plethora of evidence is available regarding efficient achievement and sustenance of hypotensive anaesthesia during FESS by using specific hypotensive agents.[3,11,12] However, the evidence on the role of opioids in hypotensive anaesthesia during FESS is limited[6,13] and until now only remifentanil has been studied to some extent.[4] While the literature on the facilitatory potential of routinely employed pre-induction fentanyl administered just before induction of anaesthesia is sparse,[14,15] to our knowledge, no study has yet analyzed the impact of (routinely administered) pre-induction fentanyl on institution and maintenance of controlled hypotension during FESS.
Primarily, controlled hypotension can be instituted by decreasing the systemic vascular resistance (SVR) (inhalation anaesthesia, nitroprusside) and/or by reducing cardiac output (CO) (beta-blockers, opioids).[12] In the setting of FESS, if the SVR and CO are not controlled in balance, the implications on the limited surgical field may be negative and unpredictable. However, it is conceivable that reduction of SVR due to local vasodilatory effect may be counter-productive for the bloodless surgical field; the decrease in MAP and CO (e.g. with opioids) may be more efficient in reducing bleeding.[11] Although propofol-based TIVA has shown promise in reducing blood loss during FESS, it does not necessarily translate into quality of SFC unless co-administered with adequate opioid analgesia.[14,15] Of the several implications of inducing hypotension during FESS, neither the role of the fentanyl administered before induction of anaesthesia nor the influence of anaesthetic technique (intravenous, inhalation)[16,17] on specific drugs (trinitroglycerine, sodium nitroprusside, esmolol) employed to maintain a controlled hypotension state; has been elucidated adequately. Further, it is not known whether modulating the dose and manner of administration of routinely used pre-induction fentanyl for GA facilitate controlled hypotension; and if it does so, whether it reflects linearly with SFC and/or surgeons' satisfaction vis-a-vis operability?[18]
Our study highlights that pre-induction fentanyl can be utilised to facilitate controlled hypotension by situating a favourable haemodynamics state immediately after induction of GA such that commonly used hypotensive agents can be used more efficiently, i.e., effectively and without the development of acute tolerance and/or side effects. Though our randomised study supports the potential of pre-induction fentanyl in achieving intraoperative controlled hypotension endpoints, further studies are desirable to create robust meta-analytic evidence. Till that time, administration of adequate doses of pre-induction fentanyl before induction of anaesthesia could be utilised to replace the irrational practice of supporting controlled hypotension by real-time excessive deepening of anaesthesia depth by increasing anaesthetic concentration (inhalational) or dose (intravenous),[12,16] which not only would attract cardiovascular consequences (myocardial depression, vasodilatation) but also delay emergence and recovery from anaesthesia in a patient going into the post-operative care room with packed nostrils.
As a lateral reflection, the study evidence suggests that an adequate dose of pre-induction fentanyl (i.e., 3–4 μg/kg) could be of help in effectively grounding a uniform intraoperative haemodynamic profile during moderate-to-long duration surgery under GA. Future investigations for analysing the impact of optimised pre-induction fentanyl dose on the surgical outcome would be an exciting proposal. Since the scoring systems used in our study were largely based on subjective responses, not assessing early recovery parameters (time to extubation, time to recovery) can be construed as a study limitation.
CONCLUSION
Pre-induction fentanyl 3 μg/kg and 4 μg/kg seems superior to 2 μg/kg dosage in facilitating controlled hypotension during FESS measured in terms of measurable haemodynamic endpoints and favourable operative conditions, surgeon's satisfaction and hypotensive agents sparing.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bhatti MT. Neuro- ophthalmic complications of endoscopic sinus surgery. Curr Opin Ophthalmol. 2007;18:450–8. doi: 10.1097/ICU.0b013e3282f0b47e. [DOI] [PubMed] [Google Scholar]
- 2.Mandal P. Isoflurane anaesthesia for functional endoscopic sinus surgery. Indian J Anaesth. 2003;47:37–40. [Google Scholar]
- 3.Boezaart AP, Van Der Merwe J, Coetzee A. Comparison of sodium nitroprusside- and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anesth. 1995;42:373–6. doi: 10.1007/BF03015479. [DOI] [PubMed] [Google Scholar]
- 4.Cardesin A, Pontes C, Rosell R, Escamilla Y, Marco J, Escobar MJ, et al. A randomised double blind clinical trial to compare surgical field bleeding during endoscopic sinus surgery with clonidine-based or remifentanil-based hypotensive anaesthesia. Rhinology. 2015;53:107–15. doi: 10.4193/Rhino14.185. [DOI] [PubMed] [Google Scholar]
- 5.Shams T, El Bahnasawe NS, Abu-Samra M, El-Masry R. Induced hypotension for functional endoscopic sinus surgery: A comparative study of dexmedetomidine versus esmolol. Saudi J Anaesth. 2013;7:175–80. doi: 10.4103/1658-354X.114073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bailey PL, Egan TG, Stanley TH. Intravenous opioid anaesthetics. In: Miller RD, editor. Anaesthesia. New York: Churchill Livingstone; 2000. pp. 273–376. [Google Scholar]
- 7.Dole K, Kulkarni S, Shisode KD, Deshpande R, Kakade N, Khandekar R, et al. Comparison of clinical outcomes, patient, and surgeon satisfaction following topical versus peribulbar anaesthesia for phacoemulsification and intraocular lens implantation: A randomised, controlled trial. Indian J Ophthalmol. 2014;62:927–30. doi: 10.4103/0301-4738.143929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim YS, Chae YK, Choi YS. Comparative study of emergence agitation between sevoflurane and propofol anaesthesia in adults after closed reduction of nasal bone fracture. Korean J Anesthesiol. 2012;63:48–53. doi: 10.4097/kjae.2012.63.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: A critical review. Psychol Med. 1988;18:1007–19. doi: 10.1017/s0033291700009934. [DOI] [PubMed] [Google Scholar]
- 10.Dutta A, Sethi N, Choudhary P, Sood J, Panday BC, Chugh PT. The impact of preinduction fentanyl dosing strategy on postoperative nausea and vomiting in patients undergoing laparoscopic cholecystectomy. J Opioid Manag. 2018;14:283–93. doi: 10.5055/jom.2018.0460. [DOI] [PubMed] [Google Scholar]
- 11.Yoo HS, Han JH, Park SW, Kim KS. Comparison of surgical condition in endoscopic sinus surgery using remifentanil combined with propofol, sevoflurane, or desflurane. Korean J Anesthesiol. 2010;5:377–82. doi: 10.4097/kjae.2010.59.6.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baker AR, Baker AB. Anaesthesia for endoscopic sinus surgery. Acta anaesthesiol Scand. 2010;54:795–803. doi: 10.1111/j.1399-6576.2010.02259.x. [DOI] [PubMed] [Google Scholar]
- 13.Cardesín A, Pontes C, Rosell R, Escamilla Y, Marco J, Escobar MJ, et al. Hypotensive anaesthesia and bleeding during endoscopic sinus surgery: An observational study. Eur Arch Otorhinolaryngol. 2014;271:1505–11. doi: 10.1007/s00405-013-2700-0. [DOI] [PubMed] [Google Scholar]
- 14.Tugrul S, Dogan R, Senturk E, Kocak I, Sezen S, Bakan M, et al. Effect of the premedication with oral clonidine on surgical comfort in patients undergoing fess due to advanced nasal polyposis: A randomized double blind clinical trial. Am J otolaryngol. 2016;37:538–43. doi: 10.1016/j.amjoto.2016.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Mohseni M, Ebneshahidi A. The effect of oral clonidine premedication on blood loss and the quality of the surgical field during endoscopic sinus surgery: A placebo-controlled clinical trial. J Anesth. 2011;25:614–7. doi: 10.1007/s00540-011-1157-9. [DOI] [PubMed] [Google Scholar]
- 16.Kelly EA, Gollapudy S, Riess ML, Woehlck HJ, Loehrl TA, Poetker DM. Quality of surgical field during endoscopic sinus surgery: A systematic literature review of the effect of total intravenous compared to inhalational anaesthesia. Int Forum Allergy Rhinol. 2013;3:474–81. doi: 10.1002/alr.21125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Boonmak P, Boonmak S, Laopaiboon M. Deliberate hypotension with propofol under anaesthesia for functional endoscopic sinus surgery (FESS) Cochrane Database System Rev. 2016;10:CD006623. doi: 10.1002/14651858.CD006623.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahn HJ, Chung SK, Dhong HJ, Kim HY, Ahn JH, Lee SM, et al. Comparison of surgical conditions during propofol or sevoflurane anaesthesia for endoscopic sinus surgery. Br J Anaesth. 2008;100:50–4. doi: 10.1093/bja/aem304. [DOI] [PubMed] [Google Scholar]