Abstract
After a quadratus lumborum (QL) block, the course of QL plane catheter is unpredictable. This case series discusses the course and fate of trans-muscular QL catheters by following and discussing the contrast spread through the fascial planes. Intrao-peratively, the catheters were tracked by the surgeons and were checked for integrity of anterior thoracolumbar fascia (ATLF) by injecting sterile 0.9% saline. The ATLF was intact upon injection and there was cephalad and medial saline spread with slight bulging of ATLF. On day 3 after written informed consent from all patients, computed tomography (CT) contrast studies were performed. Post-operative contrast spread was variable and was visualised in transversus abdominis plane, QL plane, lower thoracic paravertebral space, inter-vertebral foramina and anterior epidural space. CT contrast images demonstrated a variable spread. In conclusion, injection in ATLF of QL can spread along the path of least resistance and is unpredictable.
Key words: Analgesia, contrast, nerve block, postoperative, quadratus lumborum, regional anaesthesia, surgery, ultrasound
INTRODUCTION
Blanco described ultrasound-guided quadratus lumborum block (QLB) in 2007.[1] A detailed account of the transmuscular quadratus lumborum block (TMQLB) was published by Borglum et.al.[2] Several cadaveric studies postulated the possible mechanism of TMQLB.[3] To our knowledge, this is possibly the first article describing the radiological spread of local anaesthetic (LA) through the catheter in a TMQLB.
CASE REPORT
This case series involves five patients (three males and two females) of the American Society of Anesthesiologist's (ASA) physical status I and II, with a mean body mass index of less than 28 kg/m2, who underwent pyelolithotomy. A consent for general anaesthesia and an ultrasound--guided TMQLB was obtained from allpatients. A standard general anaesthesia technique (intravenous midazolam, fentanyl, propofol, atracurium followed by tracheal intubation and maintainance with oxygen: air and sevoflurane) was used. ECG lead II and V5, oxygen saturation, non-invasive blood pressure and end-tidal carbon dioxide were monitored. The patients were positioned with the operative side up. An ultrasound-guided TMQLB was administered after induction.
A curvilinear ultrasound probe (2–5 MHz, Sonosite Inc.) was placed on the trunk in the mid-axillary line (Shamrock technique). The quadratus lumborum muscle (QLM), psoas major muscle (PMa) and transverse process (TP) were identified [Figure 1a]. A point was chosen as medial and as close as possible to the TP in anterior thoracolumbar fascia (ATLF) of QLM to position the needle tip. 18-G Tuohy needle was inserted close to the probe and the needle tip was identified in the ATLF. The bevel was rotated 90 degrees facing the cephalad andparallel to the QL fibres. A 20-G catheter was inserted at a distance of 5–7 cm in the ATLF. Efforts were made to visualise vascular structures in the needle trajectory. Every attempt was made to identify the catheter in the ATLF of the quadratus lumborum plane (QLP). The catheter was visualised in all the QLPs.
Figure 1.
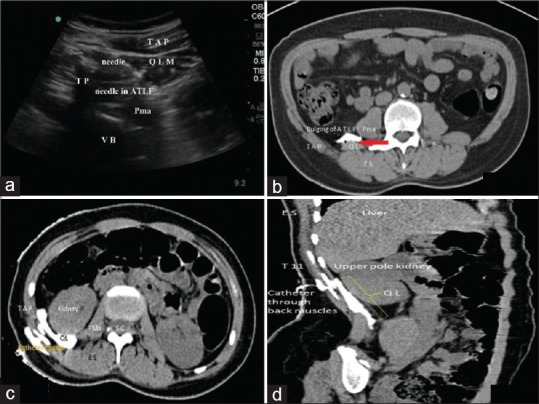
(a) Trans-muscular Quadratus Lumborum block. The Shamrock method depicting the QL (Quadratus Lumborum), PMa (Psoas Major), TAP (Tranversus Abdominis Plane), needle through the QL muscle. (b) The tense and bulging ATLF: axial Plane at Lumbar level, ATLF – Anterior Thoracolumbar Fascia; PMa Psoas Major; TAP – Transversus Abdominis Plane; QL Quadratus Lumborum; ES Erector Spinae. The red arrow above QL muscle shows the location of ilio-hypogastric vessels which can get punctured during needle placement. (c) The perinephric spread across the PTLF (Axial plane) at Thoracic level; Pma–Psoas Major; QLQuadratus Lumborum; SCSpinal Cord; ES–Erector Spinae; TAP-Transversus Abdominis Plane. (d) Sagittal plane: Contrast extends along the entire length of the QLP. (ES – Erector Spinae; QL – Quadratus Lumborum)
After informed consent, all patients underwent a CT contrast study (3 ml Omnipaque – 300 mg iodine/ml diluted in 20 ml of 0.9% saline) which was injected through the existing catheter on post-operative day 3. The serial CT contrast images were studied in the following chronology: axial, sagittal and coronal sections and reported by a consultant radiologist.
On axial section, the ATLF [Figure 1b] is tense and bulging confirming moderate compliance which suggests that QL fascia might rupture with high injection pressures. In Figure 1c, the contrast occupies a thin space between the renal tissue and the ATLF. This space is occupied by fat and connective tissue, the density of which is diminished with increasing age and thin patients. Laterally, the contrast occupies the tranversalis fascia plane. The catheter course, backtracking and extravasation of contrast in various tissue planes can also be noticed in this figure. This implies that a high QLB might penetrate the ATLF and the renal tissue.
On sagittal section, in Figure 1d, the QLM can be seen originating from the iliac crest and getting inserted on the 12th rib. The catheter is seen inserted high at the upper pole of the kidney and courses through the erector spinae (ES) muscle and disappears into the thin QLM. Contrast spread vertically and cephalad is seen occupying the entire aspect of the ATLF. This probably might block the sub-costal nerve but definitely blocks the ilio-inguinal and ilio-hypogastric nerves. This is referred to as a “High QLB”. This view implies that ATLF is connected with the lower thoracic paravertebral space (TPVS). Consistent in axial and sagittal images were the hypoechoic vascular structures i.e., the ilio-hypogastric vessels, which are highlighted as a red arrow in Figure 1b, just above QLM. Thus a needle placement should be cautiously done through the QLM due to the possibility of injury to the vascular structures in vicinity.
In Figure 2a–d, the axial plane depicts the contrast spread along the posterior thoracolumbar fascia (PTLF), the thoracic paravertebral space (TPVS) and the lumbar inter-fascial triangle (LIFT). At the thoracic axial plane, the contrast spread occurred in the TPVS, the pre-vertebral area and the inter-costal space. A small white dot consistent with contrast on serial images appeared in the anterior epidural space. In the serial axial images scanned [Figure 2a and b], we observed that the catheter courses along the back muscles and disappears into the QLP, extensive contrast spread from the lateral ATLF to the medial ATLF; cephalad the contrast spread at the level of T9-T12 and TPVS. From PVS, the contrast was visualised in the inter-vertebral foramina and in the anterior epidural space.
Figure 2.
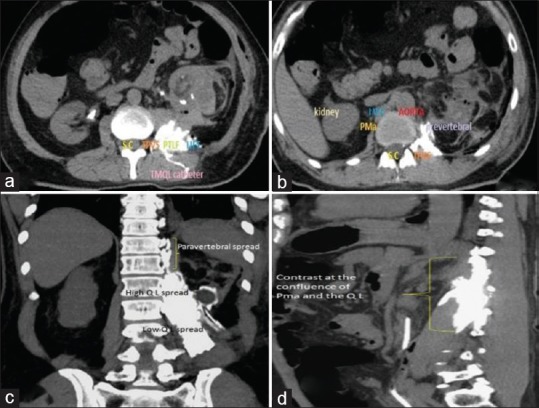
(a) Lumbar Area (Axial plane). SC–Spinal cord; TPVS–Thoracic Paravertebral Space; PTLF-Posterior Thoracolumbar Fascia; LIFT–Lumbar Inter-fascial Triangle. (b) Thoracic Axial plane (Pma – Psoas Major; S C – Spinal cord; TPVS –Thoracic paravertebral space; IVC – Inferior vena cava). (c) Contrast in sagittal plane occupying the confluence of PMa and the QL planes. (d) Coronal image depicting a rectangular spread of contrast
In the coronal plane, the contrast is visualised at the confluence of the PMa and QL and spreading cephalad towards the para-vertebral area. Here the contrast is seen occupying the entire breadth and width of the QLP. This further extends medially close to the para-vertebral area up to T11. The Figure 2d depicts contrast spread around the QLM and close to the lateral margin of the PMa with no medial spread. This is a “Low QLB” and will not block the sub-costal nerve.
DISCUSSION
We observed the spread of contrast in clinical scenarios by performing contrast study on postoperative day 3. With the needle positioned between the upper and mid part of the kidney, medially close to the TP and in the ATLF, there is the more cranial spread of the injectate i.e., a high QLB. A thoracic para-vertebral spread and an epidural extension is a possibility with high TMQLBs. A needle position between the mid and lower pole of the kidney, laterally close towards the junction of the TAP and QL but in the ATLF results in a more caudal and lateral spread.
Carline et al. observed the spread of dye in lumbar roots 1-3, sub-costal, femoral, genito-femoral and obturator nerves in embalmed cadavers.[4] Dam et al. visualised the spread of dye to the T9 para-vertebral space after ultrasound-guided TMQLB in 5 cadavers, apart from the other mentioned nerves. No para-vertebral radiopaque contrast spread was observed by Adhikari et al. after bilateral QLB was performed in 6 cadavers.[5] Elsharkawy et al. established that the point of injection in QLB decided the spread of LA in QLP.[6] A TMQLB was associated with para-vertebral spread (T6-T7) and a limited TAP spread was seen. A QLB spread was associated more with a spread in LIFT and a limited cranial spread was seen. The dynamics of contrast spread are different in the cadavers. El-Boghdadly et al. described a high and low QLB. A high QLB is when the injection is performed close to the costal margin, which can also be referred to as a sub-costal QLB. A low QLB is when the injection is performed close to the iliac crest, which can also be referred to as a supra-iliac QLB.[7]
From this clinical and radiological correlation, we propose that the needle positioning for high QLB should be between the upper and middle part of the kidneys and for low QLB, the needle positioning should be below the lower pole of the kidney, laterally close to the junction of TAP and QL, in the ATLF. We recommend the needle bevel rotation by 90 degrees after initial needle bevel placement perpendicular to the QLM fibres and catheter placed parallel to the QLM fibres. The tip of the catheters can be placed 5-6 cm in the QLP. We also postulate that the mechanism of action of high and low TMQLBs can be different. A high QLB leads the injectate to spread through para-vertebral and possible epidural spread and low QLB through caudal and lateral TAP spread. By classifying the QLB into high and low QLBs, the high QLBs can be for visceral analgesia and a low QLBs can be used for non-visceral analgesia. There is a possibility of renal injury during a high QLB.
The limitation of this study is there was a small number of patients getting enrolled. It is not possible to perform CT contrast studies in a large number of patients. Future studies on path traversed by the dye intra-operatively will throw more light on understanding the spread of QLB.
CONCLUSION
The spread of LA in the QLP is unpredictable. The LA will take the path of least resistance and dermatomes involved with the high and low QLB are different. Visceral analgesia could be possible with a high QLB. Multiple factors control the spread of LA injection like the needle and bevel position, speed of LA injection, catheter tip position, resistance during LA injection and the volume of LA injected.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Blanco R. Optimal point of injection: The quadratus lumborum type I and II blocks. [Last accessed on 2019 Apr 25];Anaesthesia. 2013 68:68. Available from: http://www.respond2articles.com/ANA/forums/post/1550.aspx . [Google Scholar]
- 2.Børglum J, Moriggl B, Jensen K, Lønnqvist PA, Christensen AF, Sauter A, et al. Ultrasound-guided trans-muscular quadratus lumborum blockade. [Last accessed on 2019 Mar 30];Br J Anaesth. 2013 110:3. Available from: http://bja.oxfordjournals.org/forum/topic/brjana_el%3b9919 . [Google Scholar]
- 3.Dam M, Moriggl B, Hansen CK, Hoermann R, Bendtsen TF, Børglum J, et al. The pathway of injectate spread with the trans-muscular quadratus lumborum block: A cadaver study. Anesth Analg. 2017;125:303–12. doi: 10.1213/ANE.0000000000001922. [DOI] [PubMed] [Google Scholar]
- 4.Carline L, McLeod GA, Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth. 2016;117:387–94. doi: 10.1093/bja/aew224. [DOI] [PubMed] [Google Scholar]
- 5.Adhikary SD, El-Boghdadly K, Nasralah Z, Sarwani N, Nixon AM, Chin KJ. A radiologic and anatomic assessment of injectate spread following transmuscular quadratus lumborum block in cadavers. Anaesthesia. 2017;72:73–9. doi: 10.1111/anae.13647. [DOI] [PubMed] [Google Scholar]
- 6.Elsharkawy H, El-Boghdadly K, Kolli S, Esa WAS, DeGrande S, Soliman LM, et al. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block: A comparative cadaveric study. Eur J Anesthesiol. 2017;34:587–95. doi: 10.1097/EJA.0000000000000680. [DOI] [PubMed] [Google Scholar]
- 7.El-Boghdadly K, Elsharkawy H, Short A, Chin KJ. Quadratus lumborum block nomenclature and anatomical considerations. Reg Anesth Pain Med. 2016;41:548–9. doi: 10.1097/AAP.0000000000000411. [DOI] [PubMed] [Google Scholar]


