Abstract
Objective
From 2007–2017, pediatric emergency department (ED) visits for mental health concerns increased by 66% in Canada, with repeat visits accounting for a significant proportion of all visits. Our objective was to examine patient and visit characteristics associated with repeat visits to a tertiary care pediatric ED for mental health concerns.
Method
Data were obtained from the administrative records of McMaster Children’s Hospital ED for mental health-related visits from February 2013–December 2017. Data on 9,018 ED visits made by 4,976 unique patients were included in this study. Logistic regression analysis was used to examine characteristics associated with repeat visit within six months of index presentation.
Results
22% (n=1,088) of individuals returned to the ED for a mental health concern within six months following their index visit. A repeat visit within six months was associated with female sex (OR=1.19, p=0.019), age of 14–17 years (OR=1.42, p=0.016), receiving a risk assessment by the emergency psychiatry team (OR=1.63, p<0.001) and having an inpatient psychiatric admission (OR=1.67, p<0.001) at the index visit. Receiving anxiety-related discharge diagnoses at an index visit reduced the odds of a repeat visit within 6 months (OR=0.76, p=0.035), while receiving depression-related discharge diagnoses increased the odds of a repeat visit, but only for females (OR=1.3, p=0.011 vs. OR=0.93, p=0.589 for males).
Conclusions
We found that approximately one in five patients presenting to the ED for a mental health concern have a repeat visit within six months, consistent with previous studies. This study provides support for previously identified risk factors for repeat visits and offers information on interactions between patient sex and diagnosis.
Keywords: emergency room, return visit, mental health, child and adolescent
Résumé
Objectif
De 2007 à 2017, les visites au service d’urgence (SU) pédiatrique pour des problèmes de santé mentale ont augmenté de 66 % au Canada, les visites répétées représentant une proportion significative de toutes les visites. Notre objectif était d’examiner les caractéristiques des patients et des visites associées aux visites répétées à un SU pédiatrique de soins tertiaires pour les problèmes de santé mentale.
Méthode
Les données ont été obtenues des dossiers administratifs du SU de l’Hôpital pour enfants McMaster pour les visites liées à la santé mentale de février 2013 à décembre 2017. Les données de 9 018 visites au SU faites par 4 976 patients uniques ont été incluses dans l’étude. L’analyse de régression logistique a servi à examiner les caractéristiques associées aux visites répétées en dedans de six mois de la première visite.
Résultats
22 % (n = 1 088) des personnes sont revenues au SU pour un problème de santé mentale en dedans de six mois de leur première visite. Une visite répétée en dedans de six mois était associée au sexe féminin (RC = 1,19, p = 0,019), à l’âge de 14 à 17 ans (RC = 1,42, p = 0,016), à la réception d’une évaluation du risque par l’équipe psychiatrique de l’urgence (RC = 1,63, p < 0,001) et à une hospitalisation psychiatrique (RC = 1,67, p < 0,001) à la première visite. Recevoir des diagnostics liés à l’anxiété au congé de la première visite réduisait les probabilités d’une visite répétée en dedans de 6 mois (RC = 0,76, p = 0,035), alors que recevoir des diagnostics liés à la dépression au congé augmentait les probabilités d’une visite répétée, mais seulement pour les femmes (RC = 1.3, p = 0,011 c. RC = 0,93, p = 0,589 pour les hommes).
Conclusions
Nous avons constaté qu’environ un patient sur cinq qui se présente au SU pour un problème de santé mentale a une visite répétée en dedans de six mois, conformément aux études précédentes. Cette étude apporte un appui aux facteurs de risque précédemment identifiés pour les visites répétées, et offre de l’information sur les interactions entre le sexe des patients et le diagnostic.
Mots clés: service d’urgence, visite répétée, santé mentale, enfant et adolescent
Introduction
Across Canada, child and youth emergency department (ED) visits for mental health concerns are increasing, while the rates of visits for other reasons have plateaued or decreased (CIHI, 2015). Between 2007 and 2017, ED visits for mental health concerns made by patients aged 5–24 years increased by 66% (CIHI, 2018), with mental health visits accounting for about 5% of all ED visits (CIHI, 2015).
Despite the increase in ED visits, evidence suggests that the population prevalence of most pediatric mental health problems is not rising substantially (McMartin, Kingsbury, Dykxhoorn, & Colman, 2014). However, perceived need for intervention has increased dramatically (Comeau, Georgiades, Wang, Boyle, & 2014 Ontario Child Health Study Team, 2019). One possible explanation for the observed overall increase in pediatric mental health service utilization is an increase in repeat presentations. Canadian population data reveal that 39% of children visiting the ED for a mental health concern have three or more ED visits for this concern (CIHI, 2015). In some centers, repeat visits represent more than 30% of all mental health-related visits (Mapelli, Black, & Doan, 2015; Newton et al., 2010; Cloutier et al., 2017; Newton et al., 2009).
Previous studies have attempted to examine reasons for repeat visits (Berry, Brousseau, Brotanek, Tomany-Korman, & Flores, 2008; Goldstein, Frosch, Davarya, & Leaf, 2007; Yu, Rosychuk, & Newton, 2011). Difficulty accessing outpatient services may be an important factor leading to repeat presentations (Berry et al., 2008), although repeat visits have been associated with already being connected to mental health services (Goldstein et al., 2007). It does not appear that clinical acuity, which may be understood to reflect illness severity, increases between repeat ED visits for mental health concerns (Yu et al., 2011).
For more than half of youth with a first mental health-related ED visit, the visit represents their first contact for outpatient mental health care (Gill et al., 2017). Previous studies have examined features of a first visit that predict repeat visits with the notion that this may lead to development of interventions that can decrease repeat visits. Several recently published Canadian studies examine repeat mental health presentations to pediatric EDs in this way (Mapelli et al., 2015; Newton et al., 2010; Cloutier et al., 2017; Newton et al., 2009; Yu et al., 2011). Repeat visits appear to be associated with patients who are older (Newton et al., 2010), female (Mapelli et al., 2015; Newton et al., 2010; Cloutier et al., 2017), of lower socioeconomic status (Newton et al., 2010), in the care of child protective services (Cloutier et al., 2017), already connected with outpatient services (Cloutier et al., 2017), and those who have mood (Newton et al., 2010; Cloutier et al., 2017) or psychotic disorders (Newton et al., 2010). Many of these characteristics are fixed and not directly amenable to intervention (e.g., patient age and sex), however if these characteristics prove to have predictive power for repeat visits, targeted services or resources may be established in attempt to mitigate this risk. Better understanding factors associated with repeat presentation may also assist with informed and improved use of hospital resources.
A systematic review conducted by Leon et al. in 2017 identified some of the most common predictors of repeat visits to include previous psychiatric hospitalization, involvement with mental health services, and socioeconomic status. (Leon et al., 2017). This review also identified significant variability in the determinants of repeat visit explored, statistical approaches employed, and the return window considered (from two months to six years, with the exception of studies employing survival analysis) (Leon et al., 2017). Previous US studies have shown that 85% of repeat mental health visits occur within six months following a first visit (Goldstein et al., 2007) and that repeat visits within six months are associated with the highest health care costs (Frosch, dosReis, & Maloney, 2011). Shorter time to repeat visit is hypothesized to more likely represent a repeat visit for the same mental health concern (Frosch et al., 2011).
In this study of mental health visits to a tertiary care pediatric ED in Hamilton, Ontario, we aimed to answer the following primary research questions:
What patient characteristics and visit characteristics were associated with increased odds of a repeat visit within six months?
What characteristics at index visit differ between patients with a repeat visit and those without a repeat visit within six months?
What characteristics at index visit are associated with greater frequency of repeat visits within the study period?
What was the proportion of repeat visits: a) during the study period; and b) within six months of the index visit?
This study sought to replicate, at a hospital-specific setting, previous studies conducted at a provincial level to examine whether the more general findings hold. We also examined several new factors that have not, to our knowledge, been explored in previous studies including weekend and overnight visits and receiving a risk assessment by the psychiatric team, in contrast to ED physician assessment only. These visit factors were selected following consultation with our expert co-author group which included emergency medicine and psychiatry physicians at the McMaster Children’s Hospital. If found to be associated with repeat visits, such visit factors could represent opportunities for systems-level interventions (e.g., services provided at off-hours).
This study offers both a replication of previous Canadian studies and addresses limitations identified by Leon et al., by using a six-month time period to define repeat visits and by including an examination of interaction effects, specifically gender interactions. Better understanding interaction effects has the potential to contribute to clinical decision making by identifying in finer detail patients who are at greater risk of an outcome. Studies using administrative records, which have the potential to include data on thousands of patients, are well suited for examining interaction effects due to their relatively larger power than other types of observational studies. Our focus on gender interactions in this study is in keeping with the Government of Canada’s Health Portfolio Sex- and Gender-based Analysis Policy, which acknowledges that biological and social differences between males and females contribute to differences in their health, treatment outcomes, and interaction with the healthcare system.
Methods
Data
We used data obtained from hospital administrative records for ED visits to McMaster Children’s Hospital in Hamilton, Ontario. Ethics approval was obtained from the Hamilton Integrated Research Ethics Board (ID 4514-C). This study is reported in accordance with the Reporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) guidelines (Nicholls et al., 2015).
All ED visits (N=9,018) between February 2013 and December 2017, inclusive, identified as relating to a mental health concern at triage using the Canadian Emergency Department Information System (CEDIS) presenting complaints were included in the study (Grafstein, Bullard, Warren, Unger, & CTAS National Working Group, 2008). As per CEDIS, the following presenting complaints are considered to be mental health problems: depression/suicidal/deliberate self-harm, anxiety/situational crisis, hallucinations/delusions, insomnia, violent/homicidal behavior, social problem, bizarre behavior, concern for patient’s welfare, and pediatric disruptive behavior (Grafstein et al., 2008). Within CEDIS classification of presenting complaints, substance misuse is not identified as a mental health problem, and therefore records identifying this presenting complaint are not included in this study. Any duplicate cases in the administrative records were removed.
Presentations for mental health concerns accounted for 3.9 to 4.5% of all ED visits at the McMaster Children’s Hospital between 2013 and 2017, inclusive. All patients younger than 18 years presenting to the McMaster Children’s Hospital ED are triaged and receive an assessment by an ED physician. Some patients receive a referral for additional psychiatric risk assessment which may involve a face-to-face assessment with a psychiatrist, or an assessment by a mental health clinician (e.g., social worker) with phone consultation with a psychiatrist. Patients who receive a psychiatric risk assessment are admitted to the short-term mental health assessment unit in the ED.
Measures
The primary objective of this study was to identify factors associated with repeat mental health visit to the pediatric ED, within six months following an index mental health visit. Unique individuals were identified for a first ED visit during the study period, defined in this study as the index visit, and any subsequent ED visits for a mental health concern during the study period were identified as a repeat visit. The main outcome measure was repeat ED visit for a mental health problem within six months of the index visit.
Analysis
To evaluate factors associated with repeat visit, we constructed a logistic regression model in which repeat visit was the binary dependent variable. Covariates included both patient factors and visit factors present at the index visit. Patient factors were selected for inclusion in the model based on previous literature. These included age (Newton et al., 2010), sex (Mapelli et al., 2015; Newton et al., 2010; Cloutier et al., 2017), and diagnosis by the ED physician (Newton et al., 2010; Cloutier et al., 2017). Data on diagnosis is based on ICD-10 codes, and related diagnoses were grouped together into larger categories as detailed in Appendix A. This included acute stress reaction, anxiety, behavioral concern, depression, developmental or intellectual disability, eating disorder, mania or psychosis, medical illness (i.e., not psychiatric), self-harm behavior, substance use, other psychiatric diagnoses, and violent behavior. Each patient receives a single discharge diagnosis for a visit. Visit factors included weekend versus weekday visit, overnight presentation (defined as ED registration between the hours of 10pm and 6am), receipt of a risk assessment by the psychiatric team (in contrast to an assessment by an ED physician only), and location of admission to hospital including ED-only (no admission), admission to the short-term mental health assessment unit in the ED, admission to the inpatient psychiatry unit, and admission to another non-psychiatric inpatient unit. These visit factors have not been readily assessed in previous studies in the same way that the aforementioned patient factors have been. Visit factors are nevertheless important to explore and may offer avenues for intervention that patient factors do not. As patients age out of the pediatric system at age 18, those closer to their eighteenth birthday will be less likely to have a repeat visit captured through pediatric administrative records. Therefore, we conducted a sensitivity analysis excluding individuals aged 17 years and older at the index visit. Post-hoc exploratory analyses for interactions between gender and discharge diagnoses were conducted. Finally, we conducted a negative binomial regression analysis to examine the association between the aforementioned factors and the total number of repeat visits made during the entire study period for patients who made at least one repeat visit. This analysis uses the count of repeat visits as the dependent variable. To control for length of time in the study, we adjusted the model for both patient age and study year at index visit.
Appendix A.
ED physician discharge diagnosis grouped by ICD-10 classification
| Depression |
| Adjustment disorders (F43.2) |
| Depressive conduct disorder (F92.0) |
| Depressive episode unspecified (F32.9) |
| Dysthymia (F34.1) |
| Mild depressive episode (F32.0) |
| Other specified mood (affective) disorders (F38.8) |
| Other childhood emotional disorders (F93.8) |
| Other depressive disorders (F32.8) |
| Recurrent depressive disorder current severe without psychotic symptoms (F33.3) |
| Recurrent depressive disorder, unspecified (F33.9) |
| Severe depressive episode without psychotic symptoms (F32.2) |
| Unspecified mood (affective) disorder (F39) |
|
|
| Mania and psychosis |
| Bipolar affective disorder current manic w psych symptoms (F31.2) |
| Bipolar affective disorder current manic without psychotic symptoms (F31.1) |
| Bipolar affective disorder unspecified (F31.9) |
| Bipolar affective disorder current hypomanic (F31.0) |
| Bipolar affective disorder currently mixed (F31.6) |
| Hypomania (F30.0) |
| Mania with psychotic symptoms (F30.2) |
| Manic episode unspecified (F30.9) |
| Other bipolar affective disorders (F31.8) |
| Acute and transient psychotic disorder, unspecified (F23.9) |
| Auditory hallucinations |
| Hallucinations unspecified |
| Other hallucinations |
| Visual hallucinations |
| Other schizophrenia (F20.8) |
| Schizoaffective disorder mixed type (F25.2) |
| Schizoaffective disorder unspecified (F25.9) |
| Schizophrenia unspecified (F20.9) |
| Severe depressive episode with psych symptoms (F32.3) |
| Unspecified nonorganic psychosis (F29.0) |
| Delusional disorder (F22.0) |
|
|
| Acute stress reaction |
| Acute stress reaction (F43.0) |
| Reaction to severe stress unspecified (F43) |
| Shock unspecified |
| State of emotional shock and stress unspecified |
|
|
| Anxiety |
| Agoraphobia (F40.0) |
| Anxiety disorder unspecified (F41) |
| Generalized anxiety disorder (F.41.1) |
| Obsessive compulsive disorder (F42) |
| Other specified anxiety disorders (F41) |
| Panic disorder (episodic paroxysmal anxiety) (F41.0) |
| Phobic anxiety disorder unspecified (F40.9) |
| Post-traumatic stress disorder (F43.1) |
| Separation anxiety disorder of childhood (F93.0) |
| Social anxiety disorder of childhood (F93.2) |
| Eating disorder |
| Abnormal weight loss |
| Anorexia nervosa (F50.0) |
| Atypical anorexia nervosa (F50.1) |
| Bulimia nervosa (F50.2) |
| Eating disorder unspecified (F50.8) |
|
|
| Developmental or intellectual disability |
| Asperger’s syndrome (F84.5) |
| Atypical autism (F84.1) |
| Childhood autism (F84.0) |
| Developmental disorder of scholastic skills, unspecified (F81.9) |
| Disorder psychological development NOS |
| Other disorder psychological development (F88) |
| Pervasive developmental disorder (F84) |
|
|
| Self-harm |
| ICD-10 codes for injury, poisoning and certain other consequences of external causes |
|
|
| Pediatric behavioral |
| Combined vocal & multiple motor tic disorder (F95.2) |
| Conduct disorder unspecified (F91.9) |
| Disturbance of activity and attention (F90) |
| Habit and impulse disorder unspecified (F63.8) |
| Oppositional defiant disorder) (F91.3) |
| Other conduct disorders (F91.8) |
| Tic disorder unspecified (F95.9) |
| Unsocialized conduct disorder (F91.1) |
|
|
| Substance use |
| ICD-10 codes for mental and behavioral disorders due to psychoactive substance use |
| Violence |
| Hostility |
| Physical violence |
|
|
| Medical illness (not psychiatric) |
| ICD-10 codes for non-mental health related diagnoses |
|
|
| Other psychiatric |
| ICD-10 codes for personality disorder, conversion disorder, sexual/physical abuse, social problems, and insomnia |
All statistical analyses were performed using STATA version 15.1 (StataCorp LP, College Station, TX, USA) (StataCorp, 2017). We present patient demographic and clinical data with mean values and standard deviations (SDs) reported for continuous variables, and percentages for categorical variables. Skewed data is presented as median and interquartile range (IQR). Independent sample t-tests and chi-square tests were used to determine differences between groups. The level of significance for hypothesis testing was set at alpha=0.05. Results of the logistic regression are reported as odds ratios and their corresponding 95% confidence intervals (CI) with associated p-values. Odds ratios greater than one reflect an increased risk of a repeat visit. Results of the negative binomial regression are reported as incidence rate ratios (IRR) and their corresponding 95% CI with associated p-values. An IRR greater than one reflects an increased rate of repeat visit. Our sample size of 4,976 unique patients was adequately powered to perform these analyses, allowing for more than ten participants per covariate (Peduzzi, Concato, Kemper, Holford, & Feinstein, 1996).
Results
Sample characteristics
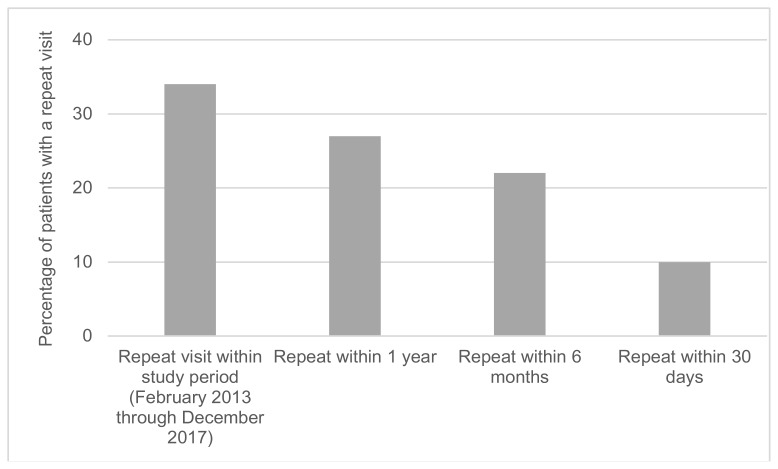
From February 1, 2013 until the end of December 31, 2017, 9,018 ED visits for mental health concerns were made by 4,976 unique patients. Therefore, repeat ED visits made up 44.8% of the total visits during the study period. Of the 4,976 patients, 34% made a repeat visit at some point during the nearly four-year study period (1 visit = 18.0%, 2 visits = 6.7%, 3+ visits = 9.3%). A total of 1,088 patients made a repeat visit within six months of index presentation (22%), and within this, 498 patients (10%) made their repeat visit within 30 days of the index visit (Figure 1).
Figure 1.
Repeat ED visits for a mental health concern (n = 4,976)
Patient and visit characteristics at index visit are detailed in Table 1. Patients with a repeat visit were slightly older, on average, than those without (mean age 14.4 years (SD=2.3) versus 13.9 years (SD=2.8), respectively, p<0.001). Of those with a repeat visit, 66.4% were female, as compared to 60% of patients with no repeat visits (p<0.001). The mean number of repeat visits throughout the entire four-year study period was higher for those patients who had an initial repeat within six months (3.66 versus 1.32, p<0.001). The most common discharge diagnosis in both six-month repeaters and non-repeaters was depression, however depression represented a larger proportion of discharge diagnoses in patients who had a repeat visit (53.9%) compared to those who did not (44.1%, p<0.001). Conversely, patients who did not have a repeat visit within six months more frequently received discharge diagnoses of acute stress reaction (13.5%) or anxiety (11.2%) at the time of index visit (p=0.01, and p<0.001, respectively).
Table 1.
Demographic and clinical characteristics at index visit (N = 4,976)
| Characteristic | No-repeat within 6 months n = 3,888 (78%) |
Repeat within 6 months n = 1,088 (22%) |
p value |
|---|---|---|---|
| Patient characteristics | |||
| Age (years) | 13.94 (SD = 2.8) | 14.35 (SD = 2.3) | <0.001 |
| Min-max = 6–17 | Min-max = 6–17 | ||
| Female sex | 2,332 (60%) | 772 (66.4%) | <0.001 |
| Mean number of repeat visits throughout entire study period | 1.32 (SD = 1.17) | 3.66 (SD = 3.45) | <0.001 |
| Min-max = 1–33 | Min-max = 2–52 | ||
| Discharge diagnosis | |||
| Depression | 1,715 (44.11%) | 586 (53.86%) | <0.001 |
| Acute stress reaction | 524 (13.48%) | 115 (10.57%) | 0.011 |
| Anxiety | 435 (11.19%) | 85 (7.81%) | 0.001 |
| Self-harm | 363 (9.34%) | 86 (7.9%) | 0.145 |
| Mania or psychosis | 112 (2.88%) | 36 (3.31%) | 0.462 |
| Substance usea | 87 (2.24%) | 25 (2.3%) | 0.906 |
| Behavioral | 62 (1.59%) | 25 (2.3%) | 0.118 |
| Violence | 38 (0.98%) | 9 (0.83%) | 0.651 |
| Eating disorder | 18 (0.46%) | 4 (0.37%) | 0.675 |
| Developmental or intellectual disability | 17 (0.44%) | 3 (0.28%) | 0.457 |
| Medical illness, not psychiatric | 120 (3.09%) | 18 (1.65%) | 0.011 |
| Other psychiatric diagnosisb | 397 (10.21%) | 96 (8.82%) | 0.176 |
| Visit characteristics | |||
| Triage acuity level (CTAS): | |||
| 1 | 8 (0.21) | 1 (0.09%) | |
| 2 | 1,367 (35.16%) | 446 (40.99%) | |
| 3 | 2,077 (53.42%) | 560 (51.47 %) | |
| 4 | 378 (9.72%) | 74 (6.8%) | |
| 5 | 58 (1.49%) | 7 (0.64%) | |
| Weekend presentation | 710 (18.26%) | 181 (16.64%) | 0.216 |
| Overnight presentation | 734 (18.88%) | 190 (17.46%) | 0.289 |
| Risk assessment completed by mental health team | 1,489 (38.3%) | 579 (53.22%) | <0.001 |
| Admission to hospital: | |||
| None | 2,541 (65.35%) | 581 (53.4%) | |
| Mental health assessment unit | 903 (23.23%) | 278 (25.55%) | |
| Inpatient psychiatry | 289 (7.43%) | 167 (15.35%) | |
| Other inpatient unit | 155 (3.99%) | 62 (5.7%) | |
| Length of admission (days)c | 1 (6) | 2 (7) | 0.026 |
| Median (IQR) | |||
CTAS = Canadian Triage Acuity Scale, Min-max = Minimum to maximum, IQR = Interquartile range
This does not reflect all ED presentations for substance use as triage chief complaints of substance intoxication, misuse, or withdrawal are not included in this study.
Other psychiatric diagnoses include: personality disorder, conversion disorder, sexual/physical abuse, social problems, and insomnia.
n = 1,848
In both patients who had a repeat visit within six months, and those who did not, fewer ED visits occurred on the weekend or overnight than during the week and within daytime hours. Risk assessment by the psychiatric team was requested for 53.2% of patients who later had a repeat visit, as compared to 38.3% of those who did not repeat (p<0.001).
Regression analysis
Factors associated with repeat visit within six months of the index visit are reported in Table 2 and the results of both unadjusted and adjusted analyses can be found in Appendix B. Children age 14 to 17 at the index visit and female patients were more likely to have a repeat visit (OR=1.42, CI 1.07–1.89, p=0.016; OR=1.19, CI 1.03–1.38, p=0.019, respectively). Patients who received a mental health team risk assessment (OR=1.63, CI 1.35–1.96, p<0.001) and had an inpatient psychiatry admission (OR=1.67, CI 1.3–2.14, p<0.001) at the index visit were associated with having a repeat visit within six months. A trend was seen in which patients who had a repeat visit were less likely to have presented to the ED overnight during their index visit (OR=0.84, CI 0.7–1.01, p=0.063).
Table 2.
Factors associated with repeat visit within six months of index visit and factors associated with total number of repeat visits within the study period
| Factors associated with repeat visit within 6 months of index visit | Factors associated with the total number of repeat visits within the study period (February 2013 to December 2017) | |||
|---|---|---|---|---|
|
|
|
|||
| Covariates | Odds Ratioa [95% CI] | p value | Incidence Rate Ratiob [95% CI] | p value |
| Age | ||||
| <10 years | [reference] | [reference] | ||
| 10–13 years | 1.29 [0.95–1.75] | 0.1 | 1.16 [1.0–1.33] | 0.05 |
| 14–17 years* | 1.42 [1.07–1.89] | 0.016 | 1.0 [0.87–1.15] | 0.96 |
| Female sex * | 1.19 [1.03–1.38] | 0.019 | 1.17 [1.09–1.26] | <0.001 |
| Risk assessment by psychiatry*** | 1.63 [1.35–1.96] | <0.001 | 1.11 [1.02–1.21] | 0.017 |
| Weekend presentation | 0.9 [0.75–1.08] | 0.253 | 0.98 [0.9–1.06] | 0.587 |
| Overnight presentation | 0.84 [0.7–1.01] | 0.063 | 1.03 [0.95–1.12] | 0.465 |
| Admission to hospital: | ||||
| None | [reference] | [reference] | ||
| Mental health assessment unit | 0.91 [0.74–1.12] | 0.372 | 0.88 [0.78–0.99] | 0.03 |
| Inpatient psychiatry *** | 1.67 [1.3–2.14] | <0.001 | 1.13 [1.01–1.26] | 0.027 |
| Other inpatient unit | 1.35 [0.98–1.86] | 0.066 | 1.1 [0.94–1.29] | 0.219 |
| Anxiety diagnosisc* | 0.76 [0.6–0.98] | 0.035 | 0.98 [0.88–1.11] | 0.798 |
| Depression diagnosisc | 1.15 [0.98–1.33] | 0.081 | 0.99 [0.92–1.07] | 0.844 |
| Female sex*, Depression diagnosis* | 1.3 [1.06–1.59] | 0.011 | 1.3 [1.05–1.28] | 0.003 |
| Male sex*, Depression diagnosis | 0.93 [0.73–1.19] | 0.589 | 0.96 [0.85–1.09] | 0.544 |
| Study year d | - | - | 0.92 [0.9–0.95] | <0.001 |
p < 0.001,
p < 0.01,
p < 0.05
All participants are included in the logistic regression analysis (N = 4,976)
Participants with at least one repeat visit within the study period are included in this negative binomial regression analysis (n = .1,692)
All diagnosis variables were entered into the model individually, with covariates including age, sex, risk assessment by psychiatry, weekend presentation, overnight presentation, and location of admission to hospital. Results that do not approach statistical significance are not shown.
The negative binomial regression analysis was adjusted for study year and patient age to control for length of follow up.
Appendix B.
Unadjusted and adjusted analyses: factors associated with repeat visit within 6 months of index visit (N = 4,976)
| Unadjusted | Adjusted | |||
|---|---|---|---|---|
|
|
|
|||
| Covariates | OR [95% CI] | p value | OR [95% CI] | p value |
| Age | ||||
| <10 years | [reference] | [reference] | ||
| 10–13 years | 1.48 [1.1–2.0] | 0.01 | 1.29 [0.95–1.75] | 0.1 |
| 14–17 years* | 1.83 [1.39–2.41] | <0.001 | 1.42 [1.07–1.89] | 0.016 |
| Female sex * | 1.32 [1.14–1.51] | <0.001 | 1.19 [1.03–1.38] | 0.019 |
| Risk assessment by psychiatry*** | 1.83 [1.6–2.1] | <0.001 | 1.63 [1.35–1.96] | <0.001 |
| Weekend presentation | 0.89 [0.75–1.07] | 0.217 | 0.9 [0.75–1.08] | 0.253 |
| Overnight presentation | 0.91 [0.76–1.08] | 0.289 | 0.84 [0.7–1.01] | 0.063 |
| Admission to hospital: | ||||
| None | [reference] | [reference] | ||
| Mental health assessment unit | 1.35 [1.15–1.58] | <0.001 | 0.91 [0.74–1.12] | 0.372 |
| Inpatient psychiatry *** | 2.53 [2.05–3.12] | <0.001 | 1.67 [1.3–2.14] | <0.001 |
| Other inpatient unit | 1.75 [1.29–2.38] | <0.001 | 1.35 [0.98–1.86] | 0.066 |
| Anxiety diagnosis * | 0.67 [0.53–0.86] | <0.001 | 0.76 [0.6–0.98] | 0.035 |
| Depression diagnosis | 1.48 [1.29–1.69] | <0.001 | 1.15 [0.98–1.33] | 0.081 |
| Female sex*Depression diagnosis* | 1.72 [1.43–2.07] | <0.001 | 1.3 [1.06–1.59] | 0.011 |
| Male sex*Depression diagnosis | 1.17 [0.92–1.47] | 0.197 | 0.93 [0.73–1.19] | 0.589 |
| Acute stress | 0.76 [0.61–0.94] | 0.011 | 0.99 [0.79–1.24] | 0.922 |
| Self-harm | 0.83 [0.65–1.07] | 0.146 | 0.82 [0.63–1.06] | 0.125 |
| Mania or psychosis | 1.15 [0.79–1.69] | 0.463 | 0.93 {0.63–1.38] | 0.731 |
| Violence | 0.85 [0.41–1.75] | 0.651 | 1.01 [0.48–2.12] | 0.973 |
| Substance use | 1.03 [0.66–1.61] | 0.906 | 1.14 [0.72–1.82] | 0.571 |
| Behavioural | 0.86 [0.41–1.75] | 0.651 | 1.01 [0.48–2.12] | 0.973 |
| Medical illness | 0.53 [0.32–0.87] | 0.012 | 0.69 [0.31–1.14] | 0.143 |
OR = Odds Ratio, CI = Confidence Interval
For adjusted analyses:
p < 0.001,
p < 0.01,
p < 0.05
Note: For unadjusted analyses, each covariate was entered into the model individually. For adjusted analyses, covariates were entered into the model controlling for age, sex, risk assessment by psychiatry, weekend presentation, overnight presentation, and location of admission to hospital.
All ED diagnoses were assessed individually in univariate models and only diagnoses reaching statistical significance at p < 0.05 were retained in the final model. Patients with a repeat visit were less likely to have received a diagnosis of anxiety at their index visit (OR=0.76, CI 0.6–0.98, p=0.035). Though no significant association was found between a discharge diagnosis of depression at index visit and returning within six months in the general sample, a significant interaction between patient sex and depression diagnosis was detected, such that females with a discharge diagnosis of depression were more likely to return (OR=1.3, CI 1.06–1.59, p=0.011). This was not the case for males. Interaction effects between gender and other discharge diagnoses at index visit were examined, revealing no significant effects between gender and the presence of anxiety disorder, self-harm, mania or psychosis, substance use, violence, developmental disability and eating disorder diagnoses (data not shown). A trend towards statistical significance was seen in males with a discharge diagnosis of behavioral concern as more likely to return (OR=1.76, CI 0.996–3.11, p=0.051; data not shown), which was not identified for females with this diagnosis (p=0.764; data not shown).
A sensitivity analysis excluding patients age 17 years and older revealed no substantial changes in the magnitude or direction of effects (with ORs changing within a range of 0.01 to 0.14) and no substantial change in the statistical significance levels for any covariate (data not shown). Analysis of factors associated with frequency of repeat visit within the study period revealed results consistent with those for likelihood of repeat visit within six months (Table 2).
Discussion
In this study, we found that 34% of patients made a repeat visit over the nearly 4-year study period, with repeat visits making up nearly 45% of all visits. Further, 22% of patients returned to the ED within six months of an index mental health presentation. These results are consistent with findings from previous studies, which identify repeat visits as accounting for 20–45% of all ED visits for mental health concerns (Mapelli et al., 2015; Newton et al., 2010; Cloutier et al., 2017). They are also comparable to previous studies that have examined repeat visits within 6 months, finding 12–21% of patients with at least one repeat visit (Goldstein, et al., 2007; Frosch et al., 2011; Sobolewski, Richey, Kowatch, & Grupp-Phelan, 2013).
We identified five factors that were significantly associated with a repeat visit: older age (14–17 years), female sex, receiving a risk assessment by the psychiatry team, having an inpatient psychiatric admission, and – for female but not for male patients – receiving a discharge diagnosis of a depression-related disorder. These results, too, are similar to those of previous studies that have identified patients of older age and female sex as being at higher likelihood of re-presenting (Mapelli et al., 2015; Newton et al., 2010; Cloutier et al., 2017; Leon et al., 2017). There is variability within the literature regarding diagnoses associated with increased repeat visits, including mood disorders (Newton et al., 2010; Cloutier et al., 2017), psychotic disorders (Newton et al., 2010; Boyer et al., 2013), and personality disorders (Goldstein et al., 2007; Boyer et al., 2013). We did not find a significant association with repeat visit for discharge diagnoses related to self-harm or mania and psychosis. We found that patients who received a discharge diagnosis of an anxiety-related disorder at their index visit were less likely to have a repeat visit. A previous study examining time to repeat ED visit for pediatric patients with anxiety disorders found that multiple physician follow-up visits and follow-up visits specifically for mental health were associated with a shorter time to return to ED within 90 days (Newton, Rosychuk, Niu, Radomski, & McGrath, 2015). These findings contrast hypotheses that mental health care provided after an ED visit would lengthen, rather than shorten, the time to ED return. Therefore, the study authors hypothesized that this decreased length of time to return may reflect physician behavior (e.g. providing instructions to return to the ED) or physical proximity to the ED (Newton et al., 2015).
Our study was unable to examine psychiatric comorbidity as patients are given only one discharge diagnosis. Psychiatric comorbidity has previously been found to be associated with repeat visits (Goldstein et al., 2007) and is a suggested area of further examination (Leon et al., 2017). Additionally, we did not assess consistency in diagnosis between visits, this is an area that future studies may wish to examine. Previous studies have found considerable heterogeneity between diagnoses in repeated visits, leading investigators to postulate that these diagnoses better represented behaviours rather than disorders (Newton et al., 2010). We also did not have information on whether individuals were connected with outpatient mental health services (Goldstein et al., 2007; Newton et al., 2015), or had access to primary care (Gill et al., 2017). We found a trend towards a decreased likelihood of repeat visit for those patients who presented to the ED overnight. Overnight presentation has not been previously examined as a potential factor associated with repeat visits, however it may be speculated that overnight presentations indicate higher clinical acuity. The finding that patients presenting overnight were less likely to make a repeat visit challenges this notion. However, the association between clinical severity and ED utilization has been explored previously by examining triage level, yielding no association with repeat visits (Goldstein et al., 2007; Yu et al., 2011). Additionally, in the context of the McMaster Children’s Hospital ED, it is possible that patients presenting overnight may be more likely to remain in the general ED or in the short-term mental health assessment unit in the ED until the following day, perhaps allowing for longer opportunity to work with clinical staff and receive supportive counseling, coaching around skill building, and crisis safety planning. On further evaluation, there do not appear to be meaningful differences in the rates of admission to the mental health assessment unit (23% vs. 25%), inpatient psychiatry (64% vs. 58%) or discharge from ED (9% vs. 11%) between those presenting during the day versus overnight. This is an area that requires further investigation.
The systematic review by Leon et al. highlighted a number of limitations in our current knowledge (Leon et al., 2017). Many prior studies have focused primarily on patient-level factors, rather than hospital or system factors. Few studies have examined the number of repeat visits and characteristics distinguishing frequent repeaters, and there has been a paucity of exploration of interaction terms that may have decision-making utility (Leon et al., 2017). Our study attempted to address one of these knowledge gaps and explore interaction terms with patient sex in post-hoc analyses. The finding that females with a diagnosis of depression were more likely to return within 6 months, not seen in males, and that males with a diagnosis of behavioral concern were more likely to return, not seen in females, suggests that there may be utility in considering presentations in males and females differentially. Given the higher risk of repeat visit identified in specific populations, additional follow-up services such as a phone call to ensure safety (Rengasamy & Sparks, 2019) or connection with rapid-response outpatient services (Greenfield, Larson, Hechtman, Rousseau & Platt, 2002) may be helpful for these identified groups without a general need to increase follow-up for all in a situation of limited resources. Identifying further patterns in the presentations of males and females, or other factors that may influence outcomes for different psychiatric disorders may inform clinical decision-making in the future.
Strengths and limitations
This study is strengthened by the six-month return window applied for a repeat visit as it may be hypothesized that repeat visit within a shorter time period is of greater clinical importance and may be more reflective of a re-presentation as compared to a new concern (Goldstein et al., 2007; Leon et al., 2017; Frosch et al., 2011). As this is a single-center study, the results may not be generalizable to non-tertiary or non-pediatric centers, or other centers outside of Hamilton, Ontario. Like other studies using administrative records, this study faces limitations including misclassification bias and the potential for errors related to identifying mental health concerns at triage and other variables such as coding of discharge diagnoses. As substance misuse is not captured as a mental health concern in CEDIS classification, patients presenting with substance-related presenting problems are not represented in this study. It is possible that some substance misuse presentations result in a mental health discharge diagnosis; how many substance use presentations fail to be captured in this dataset is unknown and a limitation of this study. Many potentially relevant characteristics are not captured in administrative records, therefore limiting our ability to adjust for known confounders, in addition to the risk of unmeasured confounding common to all observational research. Male or female sex captured in administrative records does not necessarily correspond to gender and does not capture gender non-binary or transgendered individuals; but this is a challenge with all administrative health data analysis. There is variability in the methods used by prior Canadian studies to identify mental health presentations, with some studies limiting inclusion to those referred specifically to a crisis intervention program (Cloutier et al., 2017), others identifying visits using discharge diagnoses (Newton et al., 2010; Yu et al., 2011), or a combination of triage chief complaints and discharge diagnoses (Mapelli et al., 2015). There is evidence in the general ED literature that presenting complaints may not accurately predict discharge diagnoses or acuity (Raven, Lowe, Maselli, & Hsia, 2013). The field may benefit from future studies examining the concordance between chief complaints and discharge diagnoses for this reason.
Further, the definition of index visit may not be accurate for all patients if they had a mental health presentation prior to the start of the study period; however, the McMaster Children’s Hospital ED did not begin to see pediatric patients for mental health concerns until February 2013. Previously, pediatric patients were seen at the city’s adult emergency psychiatry department in a separate hospital, at which time rates of pediatric presentations for mental health concerns were considerably lower. As this study includes records from February 2013, the time of inception of the pediatric ED mental health program, the risk of misidentifying an index visit may be somewhat lower. However, this study did not account for individuals lost due to loss of records, moving residence or graduating to the adult hospital system at age 18. Finally, this study does not include data from other hospitals within our health authority and some patients who present to community hospitals may be discharged directly from there or transferred to the McMaster Hospital inpatient unit without ever visiting the McMaster ED. Therefore, our results may underestimate the number of repeat visits for patients who present to other hospitals.
Conclusions
In this study we found that approximately one in five patients presenting to the ED for a mental health concern had a repeat visit within six months, consistent with previous studies. This study provides support for some previously identified risk factors for repeat visits such as older age, female sex, and inpatient psychiatric admission, and offers new information on others, including anxiety disorder discharge diagnosis, overnight presentation to the ED, and interactions between patient sex and diagnosis. Future observational studies that do not rely on administrative data may provide a more robust assessment of pediatric patients presenting to the ED for mental health concerns and help to clarify reasons for repeat visit and identify targets for intervention.
Acknowledgements / Conflicts of Interest
Tea Rosic received support from the Richard and Mary Pelling Scholarship in Psychiatry. The funding body had no role in the study design, data analysis, or publication of results. The authors thank Elviera Janzen for her help with data access. The authors have no financial relationships to disclose.
References
- Berry A, Brousseau D, Brotanek JM, Tomany-Korman S, Flores G. Why do parents bring children to the emergency department for nonurgent conditions? A qualitative study Ambulatory Pediatrics. 2008;8(6):360–7. doi: 10.1016/j.ambp.2008.07.001. [DOI] [PubMed] [Google Scholar]
- Boyer L, Henry JM, Samuelian JC, Belzeaux R, Auquier P, Lancon C, Da Fonseca D. Mental disorders among children and adolescents admitted to a French psychiatric emergency service. Emergency Medicine International. 2013;2013 doi: 10.1155/2013/651530. 651530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI) Care for children and youth with mental disorders. 2015. Accessed from: https://secure.cihi.ca/free_products/CIHI%20CYMH%20Final%20for%20pubs_EN_web.pdf.
- Canadian Institute for Health Information (CIHI) Care for children and youth with mental disorders, 2018 update. 2018. Accessed from: https://www.cihi.ca/en/child-and-youth-mental-health-in-canada-infographic.
- Cloutier P, Thibedeau N, Barrowman N, Gray C, Kennedy A, Leon SL, Cappelli M. Predictors of Repeated Visits to a Pediatric Emergency Department Crisis Intervention Program. Canadian Journal of Emergency Medicine. 2017;19(2):122–130. doi: 10.1017/cem.2016.357. [DOI] [PubMed] [Google Scholar]
- Comeau J, Georgiades K, Duncan L, Wang L, Boyle MH 2014 Ontario Child Health Study Team. Changes in the prevalence of child mental disorders and perceived need for professional help between 1983 and 2014: Evidence from the Ontario Child Health Study. Canadian Journal of Psychiatry. 2019;64(4):256–264. doi: 10.1177/0706743719830035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frosch E, dosReis S, Maloney K. Connections to outpatient mental health care of youths with repeat emergency department visits for psychiatric crises. Psychiatric Services. 2011;62(6):646–649. doi: 10.1176/ps.62.6.pss6206_0646. [DOI] [PubMed] [Google Scholar]
- Gill PJ, Saunders N, Gandhi S, Gonzalez A, Kurdyak P, Guttmann A. Emergency department as a first contact for mental health problems in children and youth. Journal of the American Academy of Child and Adolescent Psychiatry. 2017;56(6):475–482. doi: 10.1016/j.jaac.2017.03.012. [DOI] [PubMed] [Google Scholar]
- Goldstein AB, Frosch E, Davarya S, Leaf PJ. Factors associated with a six-month return to emergency services among child and adolescent psychiatric patients. Psychiatric Services. 2007;58(11):1489–1492. doi: 10.1176/ps.2007.58.11.1489. [DOI] [PubMed] [Google Scholar]
- Grafstein E, Bullard MJ, Warren D, Unger B CTAS National Working Group. Revision of the Canadian Emergency Department Information System (CEDIS) presenting complaint list version 1.1. Canadian Journal of Emergency Medicine. 2008;10(2):151–73. doi: 10.1017/s1481803500009878. [DOI] [PubMed] [Google Scholar]
- Greenfield B, Larson C, Hechtman L, Rousseau C, Platt R. A rapid-response outpatient model for reducing hospitalization rates among suicidal adolescents. Psychiatric Services. 2002;53(12):1574–9. doi: 10.1176/appi.ps.53.12.1574. [DOI] [PubMed] [Google Scholar]
- Leon SL, Cloutier P, Polihronis C, Zemek R, Newton AS, Cappelli M. Child and Adolescent Mental Health Repeat Visits to the Emergency Department: A Systematic Review. Hospital Pediatrics. 2017;7(3):177–186. doi: 10.1542/hpeds.2016-0120. [DOI] [PubMed] [Google Scholar]
- Mapelli E, Black T, Doan Q. Trends in Pediatric Emergency Department Utilization for Mental Health-Related Visits. Journal of Pediatrics. 2015;167(4):905–910. doi: 10.1016/j.jpeds.2015.07.004. [DOI] [PubMed] [Google Scholar]
- McMartin SE, Kingsbury M, Dykxhoorn J, Colman I. Time trends in symptoms of mental illness in children and adolescents in Canada. Canadian Medical Association Journal. 2014;186(18):E672–E678. doi: 10.1503/cmaj.140064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton AS, Ali S, Johnson DW, Haines C, Rosychuk RJ, Keaschuk RA, Klassen TP. A 4-year review of pediatric mental health emergencies in Alberta. Canadian Journal of Emergency Medicine. 2009;11(5):447–454. doi: 10.1017/s1481803500011647. [DOI] [PubMed] [Google Scholar]
- Newton AS, Ali S, Johnson DW, Haines C, Rosychuck RJ, Keaschuk RA, Klassen TP. Who comes back? Characteristics and predictors of return to emergency department services for pediatric mental health care Academic Emergency Medicine. 2010;17(2):177–186. doi: 10.1111/j.1553-2712.2009.00633.x. [DOI] [PubMed] [Google Scholar]
- Newton A, Rosychuk RJ, Niu X, Radomski AD, McGrath PJ. Predicting time to emergency department return for anxiety disorders and acute stress reactions in children and adolescents: a cohort study. Social Psychiatry and Psychiatric Epidemiology. 2015;50:1199–1206. doi: 10.1007/s00127-015-1073-7. [DOI] [PubMed] [Google Scholar]
- Nicholls SG, Quach P, von Elm E, Guttmann A, Moher D, Petersen I, Benchimol EI. The REporting of Studies Conducted Using Observational Routinely-Collected Health Data (RECORD) Statement: Methods for Arriving at Consensus and Developing Reporting Guidelines. PLoS One. 2015;10(5):e0125620. doi: 10.1371/journal.pone.0125620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. Journal of Clinical Epidemiology. 1996;49(12):1373–1379. doi: 10.1016/s0895-4356(96)00236-3. [DOI] [PubMed] [Google Scholar]
- Raven MC, Lowe RA, Maselli J, Hsia RY. Comparison of Presenting Complaint vs Discharge Diagnosis for Identifying “Nonemergency” Emergency Department Visits. Journal of the American Medical Association. 2013;309(11):1145–1153. doi: 10.1001/jama.2013.1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rengasamy M, Sparks G. Reduction of postdischarge sucididal behavior among adolescents through a telephone-based intervention. Psychiatric Services. 2019 doi: 10.1176/appi.ps.201800421. appips201800421. [DOI] [PubMed] [Google Scholar]
- Sobolewski B, Richey L, Kowatch RA, Grupp-Phelan J. Mental health follow-up among adolescents with suicidal behaviors after emergency department discharge. Archives of Suicide Research. 2013;17(4):323–334. doi: 10.1080/13811118.2013.801807. [DOI] [PubMed] [Google Scholar]
- StataCorp. Stata Statistical Software: Release 15. College Station TX: StataCorp LLC; 2017. [Google Scholar]
- Yu AY, Rosychuk RJ, Newton AS. Clinical acuity of repeat pediatric mental health presentations to the emergency department. Journal of the Canadian Academy of Child and Adolescent Psychiatry. 2011;20(3):208–213. [PMC free article] [PubMed] [Google Scholar]