Abstract
Background and objective
As new migraine prevention treatments are developed, the onset of a preventive effect, how long it is maintained and whether patients initially non-responsive develop clinically meaningful responses with continued treatment can be assessed.
Methods
Analyses were conducted post-hoc of a double-blind, placebo-controlled, phase II-a study in patients with episodic migraine receiving galcanezumab 150 mg or placebo biweekly for 12 weeks (Lancet Neurol 13:885, 2014). The number of migraine headache days per week, and onset of efficacy measured as the first week galacanezumab separated from placebo were determined. Patients with ≥50%, ≥75% and 100% reduction in migraine headache days from baseline at months 1, 2 and 3 were calculated and defined as sustained responses. Non-responders (<50% response) at month 1 or 2 who then showed ≥50%, ≥75% and 100% response at later time-points were calculated.
Results
Patients were randomised to galcanezumab (n=107) or placebo (n=110). A significant (p=0.018) change of −0.89±0.11 (galcanezumab) vs −0.53±0.11 (placebo) migraine headache days indicated onset at week 1. Forty-seven per cent of galcanezumab and 25% of placebo patients responding at month 1 maintained response through months 2 and 3. Of non-responders at month 1, 27% on galcanezumab and 20% on placebo responded on months 2 and 3, and 50% of galcanezumab non-responders in months 1 and 2 responded on month 3, vs 24% on placebo.
Conclusions
The onset of efficacy of galcanezumab is within 1 week in a majority of patients, and patients receiving galcanezumab are twice more likely to maintain responses than placebo patients. Early non-responders may respond by month 2 or month 3.
Trial registration number
Keywords: LY2951742, calcitonin gene-related peptide, CGRP, galcanezumab, migraine, clinical trial
Background
Novel preventive treatments that are effective and well tolerated are highly desirable given the number of individuals who suffer from frequent migraine1 and the burden migraine causes.2 Few drugs are approved by regulatory authorities for migraine prevention; with the exception of the recently approved humanised monoclonal antibodies, none are migraine-specific,3 only a small fraction of patients receive preventive treatment,1 and they are associated with undesirable side effects and low adherence rates.4 Although the postmarketing side effects and adherence are not yet known for the monoclonal antibodies, they were well tolerated in clinical trials.
Advances in our understanding of the pathogenesis of migraine5 have unveiled several potential drug targets for both acute and preventive treatment.6 The neuropeptide calcitonin gene-related peptide (CGRP) is found throughout the trigeminovascular complex7 and in central brain regions.8–11 This neuropeptide is regarded as important in the pathophysiology of migraine.11 CGRP’s role in migraine has been supported by several experimental and clinical findings: during spontaneous migraine attacks, the jugular venous blood concentration of CGRP increases.12 Interictal blood concentrations are significantly elevated in patients with episodic and chronic migraine, suggesting that elevated CGRP levels are not simply symptomatic, but may even serve as a biomarker for disease activity.13 Intravenous infusion of recombinant human CGRP can trigger a migraine attack that is indistinguishable from a spontaneous attack,14 and raised CGRP serum concentrations can be reversed with triptan administration—an effect that coincides with migraine symptom relief.15 16 In addition, small-molecule CGRP receptor antagonists have been shown to be effective in the acute17–22 and preventive23 treatment of migraine headache in double-blind, randomised, placebo-controlled trials.
Challenges in small molecule development and understanding the important role of CGRP in migraine have led to the development of monoclonal antibodies against the CGRP pathway. One of these monoclonal antibodies against the CGRP pathway is galcanezumab, a humanised monoclonal antibody that potently and selectively binds to CGRP. In a phase II-a study, the primary analyses evaluated the safety and efficacy of galcanezumab for the preventive treatment of episodic migraine24; the results provided preliminary evidence that galcanezumab was effective and generally well tolerated for the prevention of episodic migraine. These data have been substantiated by subsequent studies that have shown efficacy of galcanezumab in migraine prevention.25–27
As evidence for the efficacy of galcanezumab and other CGRP pathway monoclonal antibodies for the prevention of migraine has become available, with galcanezumab, fremanezumab and erenumab having received approval from the Food and Drug Administration for this indication,28–32 questions that are important to patients and clinicians remain, such as how quickly a patient can expect relief, whether relief will be sustained over the course of treatment, and what proportion of the patient population can expect to see relief over the course of treatment, even if they fail to respond initially by having at least a 50% reduction in migraine headache days (MHDs) within the first month or first 2 months of treatment.
Here, we present post-hoc analyses from the phase II-a study data24 to explore how early efficacy of galcanezumab can be observed using weekly measures, in contrast to efficacy assessments made using monthly measures previously presented, to evaluate sustained response over the 3-month study period, and to determine whether a cumulative response occurs over time. These post-hoc data have been presented in abstract form previously.33 34
Methods
Post-hoc analyses were conducted using data from a randomised, double-blind, placebo-controlled, phase II-a study (beginning June 2012 and concluding September 2013) with patients at 35 centres in the USA randomly assigned (1:1) to galcanezumab (150 mg subcutaneous injection every 2 weeks) or placebo for 12 weeks. The study consisted of four phases: (1) a screening period to assess inclusion/exclusion criteria and discontinuation of any excluded medications; (2) a baseline period to record the frequency and symptoms of migraine headaches; (3) double-blind, placebo-controlled treatment period of 12 weeks (month 1, 2 or 3) with injection of study drug every 2 weeks; and (4) a post-treatment follow-up period of an additional 12 weeks for continued safety assessment (figure 1).24
Figure 1.
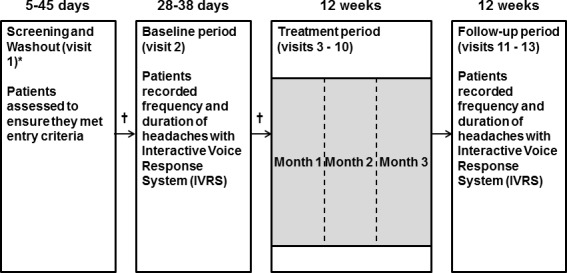
Study design. *Washout period of 30 days was included for patients to discontinue the use of migraine prevention medications. Patients who did not need a washout period were moved to the baseline period as soon as study eligibility was verified. †Eligible patients who met all the inclusion criteria and none of the exclusion criteria continued with the study.
Key inclusion criteria included men and women aged 18–65 years with at least 1-year history of migraine as defined by the International Classification of Headache Disorders (ICHD-II)35 and experiencing 4–14 MHDs per month. In addition, the patient must have discontinued any drug or other treatment to prevent migraine headaches for at least 30 days before visit 2 (baseline). Specific details of the study design, patient population, procedure and primary outcomes of this phase II-a study have been previously reported.24
An MHD was defined as a calendar day on which a headache lasting >30 min and that met the remaining criteria for migraine as defined by ICHD-II24 35 occurred. Probable migraine was also defined according to the standard ICHD-II definition as a headache of >30 min duration, with or without aura, fulfilling all but one of the criteria for migraine headache and not attributed to another disorder.35 Probable MHD was defined as a calendar day when a probable MHD occurred. Responders were defined as patients who had a ≥50% reduction in the number of MHD in a 28-day period during treatment.
Statistical analysis for onset of efficacy
The aim of this analysis was to determine the onset of efficacy of galcanezumab. To assess the onset of efficacy, daily diary data indicating whether the patient had a migraine headache (‘yes’ vs ‘no’) during the 12-week treatment period were aggregated into the number of MHD for each weekly interval. Onset of efficacy was defined as the first week in which galcanezumab was statistically superior to placebo in reducing MHD per week (p<0.05).
For derivation of weekly MHD, weekly baseline value was calculated as the number of MHD per 28-day period at baseline divided by 4. For postbaseline data, first biweekly injection schedules at weeks 0, 2, 4, 6, 8 and 10 were used to cut daily data into biweekly intervals. Then biweekly intervals are divided into two equal weekly intervals by identifying the midpoint. Change from baseline in weekly MHD was analysed with mixed model repeated measures analyses with fixed covariate of treatment, weeks, treatment-by-week interaction and baseline weekly number of MHD. Least squares means of weekly treatment differences were calculated based on the mixed model repeated measures analysis. An unstructured covariance structure was used to model the within-patient errors.
Statistical analysis for response outcomes
Here, analyses assessed the proportion of patients with ≥50%, ≥75% and 100% reduction in MHD from baseline at month 1 who sustained those response levels for months 2 and 3 (defined as ‘sustained response’). The difference for the proportion of patients meeting 50% sustained response between galcanezumab and placebo was analysed using a categorical, pseudo-likelihood-based, repeated measures analysis of binary outcome indicating whether patients met the ≥50% (or the ≥75% or the 100%) sustained response criteria (SAS GLIMMIX).
A patient was defined as a non-responder if the percentage improvement from baseline in MHD is <50% or the patient discontinued early from the treatment phase. Furthermore, to characterise subsequent response outcomes for non-responders at month 1, the proportions of patients with ≥50%, ≥75% and 100% response at months 2 and 3 were calculated and compared between treatment groups; for non-responders at months 1 and 2, the proportions of patients with ≥50%, ≥75% and 100% response at month 3 were calculated and compared between treatment groups with logistic regression. All statistical analyses—for both onset and response outcomes—were conducted using SAS V.9.2. All p values presented are nominal without multiplicity adjustment.
Results
Demographics and baseline disease characteristics
A total of 217 intent-to-treat (ITT) patients were randomised and received galcanezumab (n=107) or placebo (n=110) in the phase II-a study.24 Baseline demographics and disease state characteristics for galcanezumab and placebo groups, respectively, included an average age of 41±11 and 42±12 years; gender distribution of 88 (82%) and 96 (87%) women, and 19 (18%) and 14 (13%) men; mean number of MHD of 7±2 and 7±2 per 28 days during the baseline period; and MHD or probable MHD of 8±3 and 8±3 per 28 days during the baseline period. The post-hoc analyses for sustained response was performed with the modified ITT population, consisting of the ITT patients who have non-missing values at months 1, 2 and 3, and included 99 patients receiving galcanezumab and 105 patients on placebo. The baseline demographics and disease state characteristics for galcanezumab and placebo groups for patients classified as responders (≥50% reduction in MHD) and non-responders (<50% reduction in MHD) are presented in table 1. The mean number of MHD or probable MHD for galcanezumab and placebo groups for patients classified as responders (≥50% reduction in MHD) was 8±2 and 9±3, respectively, per 28 days during the baseline period, whereas the mean number of MHD or probable MHD for galcanezumab and placebo groups for patients classified as non-responders (<50% reduction in MHD) was 9±3 and 8±3, respectively, per 28 days during the baseline period (table 1).
Table 1.
Demographics and baseline disease characteristics for responders versus non-responders to galcanezumab
| Responders (≥50% reduction) |
Non-responders | |||
| Baseline parameters | Galcanezumab (n=46) |
Placebo (n=26) |
Galcanezumab (n=53) |
Placebo (n=79) |
| Age, years* | 42±12 | 37±12 | 41±11 | 44±11 |
| Gender, female, n (%) | 38 (83) | 23 (88) | 44 (83) | 69 (87) |
| Number of MHD* | 6±2 | 7±2 | 7±3 | 7±3 |
| Number of MHD or probable MHD* | 8±2 | 9±3 | 9±3 | 8±3 |
*Values presented as mean±SD.
MHD, migraine headache days.
Onset of efficacy
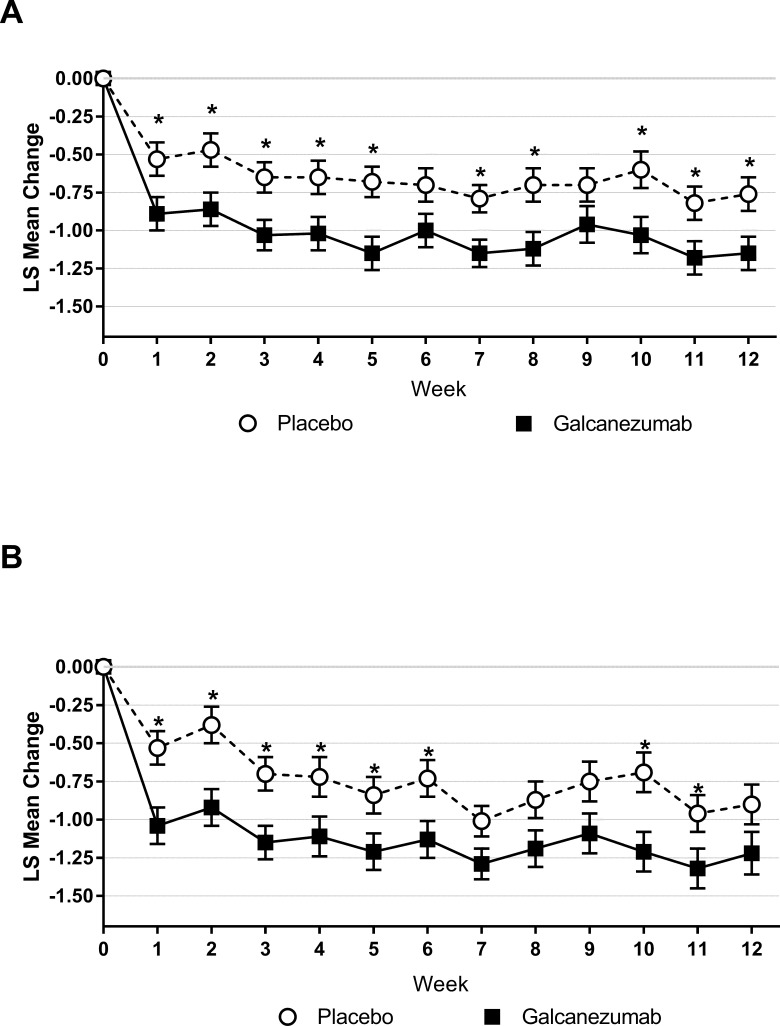
Analyses of mean change in weekly MHD from baseline showed that onset of efficacy of galcanezumab started at week 1 after the first injection as demonstrated by a statistically significant reduction in mean change in weekly MHD from baseline of −0.89±0.11 (galcanezumab) vs −0.53±0.11 (placebo) at week 1 (p=0.018); there was no statistically significant treatment-by-week interaction. A higher proportion of galcanezumab-treated patients (compared with placebo-treated patients) responded at week 1, with 62% of galcanezumab-treated patients having a ≥50% reduction in the number of weekly MHD compared with 42% of patients on placebo. This difference between galcanezumab-treated patients and placebo-treated patients for ≥50% reduction in the number of weekly MHD at week 1 was statistically significant (p<0.05). The mean reduction in weekly MHD in the galcanezumab-treated group remained statistically significantly greater (p<0.05) compared with the placebo-treated group at all weeks1–5 7 8 10–12 except for week 6 and week 9 (figure 2A).
Figure 2.
(A) Change from baseline in weekly MHD±SE. (B) Change from baseline in weekly MHD or probable MHD±SE. *P<0.05. LS, least square; MHD, migraine headache days.
Analyses of mean change in weekly migraine or probable MHD from baseline showed that the onset of efficacy of galcanezumab also started at week 1 after the first injection as demonstrated by a statistically significant reduction in mean change in weekly MHD or probable MHD from baseline at week 1 (p=0.002); no statistically significant treatment-by-week interaction was observed. The mean change in weekly migraine or probable MHD from baseline in the galcanezumab-treated group was statistically significantly greater (p<0.05) compared with the placebo-treated group at most weeks (figure 2B).
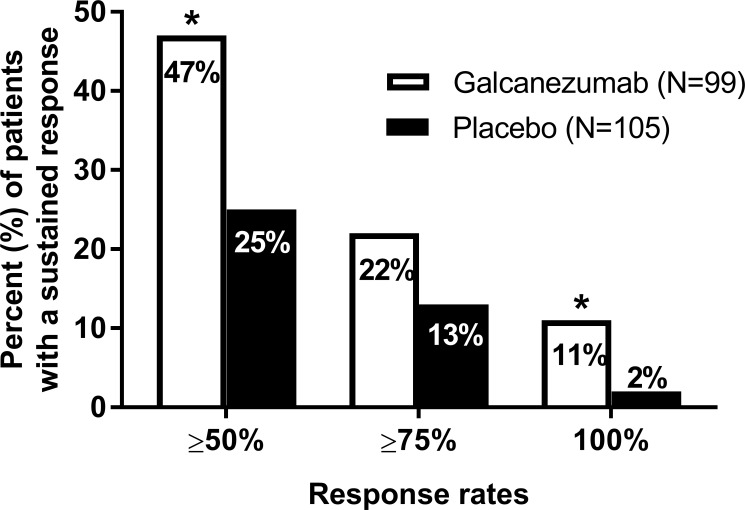
Sustained response
The proportions of galcanezumab-treated versus placebo-treated patients meeting ≥50%, ≥75% and 100% sustained response at months 1, 2 and 3 are noted in figure 3. Forty-seven per cent of galcanezumab-treated patients (n=99) vs 25% of patients on placebo (n=105) (p<0.001) responded (ie, ≥50% response rates) at months 1, 2 and 3. There was no significant difference between galcanezumab-treated versus placebo-treated patients, 22% and 13%, respectively, who met ≥75% response at months 1, 2 and 3 (figure 3). The 11% of galcanezumab-treated patients was statistically significantly greater (p<0.05) than the 2% of placebo-treated patients who met 100% response at months 1, 2 and 3 (figure 3). Among patients who were ≥50% responders at month 1, 27% of galcanezumab-treated vs 45% of placebo-treated patients either did not sustain a ≥50% response at month 2 or 3, or discontinued early.
Figure 3.
Sustained response† of galcanezumab-treated (n=99) versus placebo-treated (n=105) patients for months 1, 2 and 3. *P<0.05. †Sustained response is defined as the proportion of patients with ≥50%, ≥75% and ≥100% reduction in migraine headache days from baseline at month 1 and who sustained those same response levels through months 2 and 3.
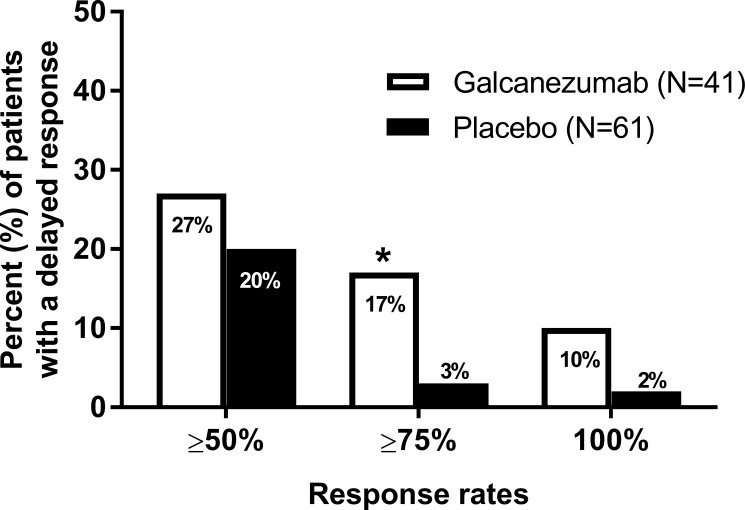
Subsequent response in initial non-responders
Subsequent response outcomes for non-responders at month 1 and non-responders at months 1 and 2 are reported in figures 4 and 5, respectively. Among month 1 non-responders (ie, patients who did not have at least a 50% reduction in MHD at month 1), 27% (galcanezumab; n=41) vs 20% (placebo; n=61) of patients responded at both months 2 and 3 (figure 4). Seventeen per cent of galcanezumab-treated vs 3% of placebo-treated (p<0.05) patients experienced at least a 75% reduction in MHD at months 2 and 3, and 10% of galcanezumab-treated vs 2% of placebo-treated patients experienced 100% reduction in MHD at months 2 and 3; only the ≥75% response rate was statistically significantly different (figure 4).
Figure 4.
Proportion of galcanezumab-treated (n=41) versus placebo-treated (n=61) patients not meeting ≥50% response (ie, ≥50% improvement from baseline in migraine headache days) at month 1 but meeting ≥50%, ≥75% and 100% response at months 2 and 3. *P<0.05.
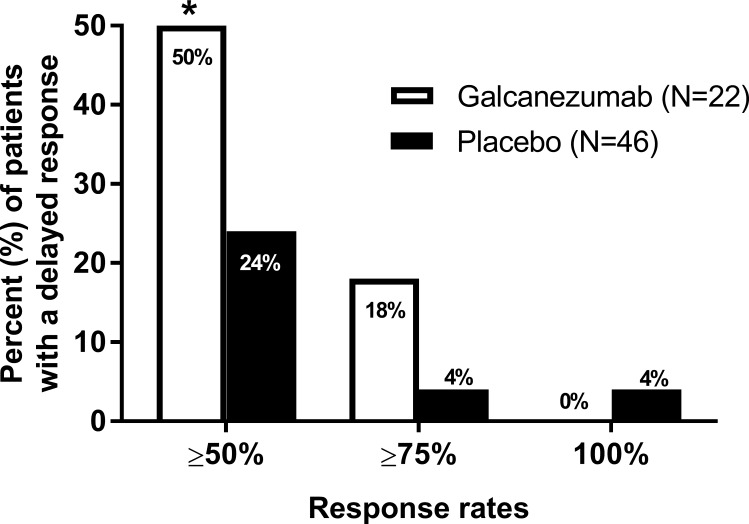
Figure 5.
Proportion of galcanezumab-treated (n=22) versus placebo-treated (n=46) patients not meeting ≥50% response (ie, ≥50% improvement from baseline in migraine headache days) at months 1 and 2 but meeting ≥50%, ≥75% and 100% response at month 3. *P<0.05.
Of the patients who did not respond (ie, have ≥50% reduction in MHD) at months 1 and 2, 50% of those who were treated with galcanezumab (n=22) vs 24% of those who were treated with placebo (n=46) (p≤0.05) subsequently experienced at least a 50% reduction in MHD at month 3, 18% of galcanezumab-treated patients vs 4% of those treated with placebo experienced at least a 75% reduction in MHD at month 3, whereas no galcanezumab-treated patients and 4% of placebo-treated patients experienced 100% reduction in MHD at month 3; only the ≥50% response rate was statistically significantly different (figure 5).
Discussion
This post-hoc analysis suggests the onset of efficacy of galcanezumab appears to begin within 1 week after the first dose in a substantial number of patients, and once improvement is achieved it is sustained during the 3-month treatment period in a substantial proportion of patients. In addition, 47% of patients who responded to galcanezumab at month 1 continued to respond at months 2 and 3. Importantly, there is also a response in a proportion of patients that may occur at months 2 and 3 despite the lack of a response 1 month after initiation of treatment. Further, response may still occur in a subset of patients at month 3 despite the lack of a response 1 or 2 months after initiation of treatment.
Little is known about the onset of efficacy, sustained response and response over time despite an initial non-response in migraine prevention trials. Rapid onset of efficacy is considered to be important for patient compliance, adherence to treatment, and therefore favourable long-term clinical outcomes,36 although any promise for onset needs to be tempered against the consequences of disappointment. Given that these are important questions for both the patient and the physician, these types of analyses could usefully be carried out more frequently in migraine preventive studies. Unlike with acute therapies, there is also a paucity of research evaluating the most important attributes of preventive medications among patients. In one study conducted on patients in Brazil and the USA, overall efficacy and the speed of onset in particular were considered by the majority of patients to be the most important attributes of preventive medications.37 However, the importance of a sustained response was not addressed in that study. In a study in a headache specialty practice, issues such as being involved in care decisions, knowledge of side effects and being prescribed treatments with published efficacy ranked highly.38 Our data are supported by similar onset of action analyses in the CGRP monoclonal antibody class that support separation of active treatment from placebo by 1 week39 40 or indeed earlier.41 The rapidity of onset of effect reinforces the importance of CGRP in the pathophysiology of migraine, its role in the genesis of headache in people with migraine and the rapid target engagement of the antibodies.
Limitations
Non-planned analyses have important limitations, particularly where the parent studies were not designed to evaluate the time frame of the analyses, here weekly efficacy outcomes. Due to the nature of post-hoc analyses, no multiplicity adjustment was conducted; thus, the results need to be interpreted under the consideration that false positives may occur. More comprehensive data are needed to confirm the findings in these post-hoc analyses. The evaluation of mean changes in migraine frequency over the course of a week in a population of patients may not accurately reflect overall changes in migraine frequency for an individual patient. Migraine frequency is variable, and weekly assessment of migraine frequency is probably not as stable as monthly assessment of migraine frequency. In particular, calculations for weekly change in MHD in patients who have migraine frequency at the lower end of the range (eg, 4 MHDs/month) may have a greater risk for inaccurate frequency interpolations than those with higher frequency MHD. Moreover, by definition episodic migraine frequency limits the frequency of MHD and thus the granularity of measurement of changes in that frequency. Chronic migraine is more suitable with its greater frequency to explore onset of action questions in migraine prevention. In addition, for the non-responders at month 1 or at months 1 and 2, only a subset of the randomised patients are included in the analyses; therefore, statistical comparison between treatment groups is limited due to potential selection bias.
Despite these limitations, the results for responders and non-responders suggest a sustained and cumulative benefit over time in subgroups of patients treated with galcanezumab. These types of data will be essential to build evidence-based clinical guidelines for treatment initiation and duration of a treatment trial with this new class of treatment. Future studies should prospectively examine the earliest onset of a significant treatment effect, as well as sustained and delayed response outcomes as they are important treatment outcomes for patients and helpful in guiding clinical decision making for physicians.
Conclusions
These post-hoc analyses attempt to begin to address clinically important questions about the onset of efficacy, sustained response and probability of a delayed response in patients with migraine, and suggest that galcanezumab has an onset of action 1 week after treatment is started. In a proportion of patients who respond within 1 month, the response is sustained over the subsequent 2 months. In those patients who had less than robust response to galcanezumab in the first month or first 2 months of treatment, a subsequent response in a relevant proportion of patients may be possible.
Acknowledgments
The authors would like to thank Michael H Ossipov, PhD, for writing, formatting and editing assistance with this manuscript.
Footnotes
Contributors: PJG contributed to the conception and interpretation of data of the work, drafting of the manuscript, and critical revision for important intellectual content. DWD contributed to the conception of the work, analysis and interpretation of data, and critical revision of the manuscript for important intellectual content. JMM contributed to the conception of the work, interpretation of data and critical revision of the manuscript for important intellectual content. MBF contributed to the conception and design of the work, interpretation and analysis of data, drafting of the manuscript, and critical revision for important intellectual content. TMO contributed to the conception of the work, interpretation of data and critical revision of the manuscript for important intellectual content. QZ contributed to the conception and design of the work, analysis and interpretation of data, drafting of the manuscript, and critical revision of the manuscript for important intellectual content. VS contributed to the conception of the work, interpretation of data and critical revision of the manuscript for important intellectual content. SKA contributed to the interpretation of data and critical revision of the manuscript for important intellectual content.
Funding: This work was supported by Eli Lilly and Company, Indianapolis, Indiana, USA
Competing interests: The studies included in the analyses were sponsored and/or supported by Eli Lilly and Company. VS, MBF, JMM, TMO and SKA are full-time employees of Eli Lilly and Company and/or one of its subsidiaries, and are stockholders. QZ was an employee of Eli Lilly and Company at the time the manuscript was written and is presently an employee of Sanofi and is an Eli Lilly and Company stockholder. PJG reports grants and personal fees from Amgen and Eli Lilly and Company; personal fees from Alder BioPharmaceuticals, Allergan, Autonomic Technologies, Dr Reddy’s Laboratories, Biohaven Pharmaceuticals, Electrocore, eNeura, Novartis, Impel Neuropharma, Mundipharma, Teva Pharmaceuticals and Trigemina; and personal fees from MedicoLegal work, UptoDate, Oxford University Press, Massachusetts Medical Society and Wolters Kluwer; and a patent magnetic stimulation for headache assigned to eNeura without fee. Within the last 12 months, DWD reports personal fees from Amgen, lder, Allergan, Autonomic Technologies, Biohaven, Eli Lilly, eNeura, Foresight Capital, Neurolief, Zosano, WL Gore, Vedanta Associates, Promius Pharma, Nocira, Novartis, Electrocore, Teva, Ipsen, Impel, Satsuma, Charleston Laboratories and Theranica; compensation for activities related to data safety monitoring committee from Axsome; compensation related to CME content development: HealthLogiX, Medicom Worldwide, MedLogix Communications, MedNet, Miller Medical Communications, PeerView Operation Services America, WebMD/Medscape, American Academy of Neurology, American Headache Society, PeerView Institute for Medical Education, Chameleon Communications, Academy for Continued Healthcare Learning, Universal Meeting Management, Haymarket Medical Education, Global Scientific Communications, UpToDate and Meeting LogiX; royalties from editorial or book publishing: Oxford University Press, Cambridge University Press, Wiley-Blackwell, Sage and Wolters Kluwer Health; consulting use agreement through employer: Neuro Assessment Systems and Myndshft; holds equity in Aural Analytics, Healint, Theranica, Second Opinion/Mobile Health and Epien; and board of directors position: King-Devick Technologies and Ontologics.
Patient consent for publication: Not required.
Ethics approval: The study was approved by the appropriate institutional review board for each study site.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Lipton RB, Bigal ME, Diamond M, et al. Migraine prevalence, disease burden, and the need for preventive therapy. Neurology 2007;68:343–9. 10.1212/01.wnl.0000252808.97649.21 [DOI] [PubMed] [Google Scholar]
- 2. Disease GBD, Injury I, Global PC, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of Disease Study 2016. Lancet 2017;390:1211–59. 10.1016/S0140-6736(17)32154-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goadsby PJ, Sprenger T. Current practice and future directions in the management of migraine: acute and preventive. Lancet Neurology 2010;9:285–98. [DOI] [PubMed] [Google Scholar]
- 4. Hepp Z, Dodick DW, Varon SF, et al. Adherence to oral migraine-preventive medications among patients with chronic migraine. Cephalalgia 2015;35:478–88. 10.1177/0333102414547138 [DOI] [PubMed] [Google Scholar]
- 5. Goadsby PJ, Holland PR, Martins-Oliveira M, et al. Pathophysiology of migraine: a disorder of sensory processing. Physiol Rev 2017;97:553–622. 10.1152/physrev.00034.2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ong JJY, Wei DY-T, Goadsby PJ. Recent advances in pharmacotherapy for migraine prevention: From pathophysiology to new drugs. Drugs 2018;78:411–37. 10.1007/s40265-018-0865-y [DOI] [PubMed] [Google Scholar]
- 7. Eftekhari S, Edvinsson L. Calcitonin gene-related peptide (CGRP) and its receptor components in human and rat spinal trigeminal nucleus and spinal cord at C1-level. BMC Neurosci 2011;12 10.1186/1471-2202-12-112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Lennerz JK, Rühle V, Ceppa EP, et al. Calcitonin receptor-like receptor (CLR), receptor activity-modifying protein 1 (RAMP1), and calcitonin gene-related peptide (CGRP) immunoreactivity in the rat trigeminovascular system: differences between peripheral and central CGRP receptor distribution. J Comp Neurol 2008;507:1277–99. 10.1002/cne.21607 [DOI] [PubMed] [Google Scholar]
- 9. Summ O, Charbit AR, Andreou AP, et al. Modulation of nocioceptive transmission with calcitonin gene-related peptide receptor antagonists in the thalamus. Brain 2010;133:2540–8. 10.1093/brain/awq224 [DOI] [PubMed] [Google Scholar]
- 10. Pozo-Rosich P, Storer RJ, Charbit AR, et al. Periaqueductal gray calcitonin gene-related peptide modulates trigeminovascular neurons. Cephalalgia 2015;35:1298–307. 10.1177/0333102415576723 [DOI] [PubMed] [Google Scholar]
- 11. Ho TW, Edvinsson L, Goadsby PJ. CGRP and its receptors provide new insights into migraine pathophysiology. Nat Rev Neurol 2010;6:573–82. 10.1038/nrneurol.2010.127 [DOI] [PubMed] [Google Scholar]
- 12. Goadsby PJ, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol 1990;28:183–7. 10.1002/ana.410280213 [DOI] [PubMed] [Google Scholar]
- 13. Cernuda-Morollón E, Larrosa D, Ramón C, et al. Interictal increase of CGRP levels in peripheral blood as a biomarker for chronic migraine. Neurology 2013;81:1191–6. 10.1212/WNL.0b013e3182a6cb72 [DOI] [PubMed] [Google Scholar]
- 14. Lassen LH, Haderslev PA, Jacobsen VB, et al. CGRP may play a causative role in migraine. Cephalalgia 2002;22:54–61. 10.1046/j.1468-2982.2002.00310.x [DOI] [PubMed] [Google Scholar]
- 15. Goadsby PJ, Edvinsson L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol 1993;33:48–56. 10.1002/ana.410330109 [DOI] [PubMed] [Google Scholar]
- 16. Juhasz G, Zsombok T, Jakab B, et al. Sumatriptan causes parallel decrease in plasma calcitonin gene-related peptide (CGRP) concentration and migraine headache during nitroglycerin induced migraine attack. Cephalalgia 2005;25:179–83. 10.1111/j.1468-2982.2005.00836.x [DOI] [PubMed] [Google Scholar]
- 17. Olesen J, Diener H-C, Husstedt IW, et al. Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N Engl J Med 2004;350:1104–10. 10.1056/NEJMoa030505 [DOI] [PubMed] [Google Scholar]
- 18. Ho TW, Ferrari MD, Dodick DW, et al. Efficacy and tolerability of MK-0974 (telcagepant), a new oral antagonist of calcitonin gene-related peptide receptor, compared with zolmitriptan for acute migraine: a randomised, placebo-controlled, parallel-treatment trial. Lancet 2008;372:2115–23. 10.1016/S0140-6736(08)61626-8 [DOI] [PubMed] [Google Scholar]
- 19. Marcus R, Goadsby PJ, Dodick D, et al. BMS-927711 for the acute treatment of migraine: a double-blind, randomized, placebo controlled, dose-ranging trial. Cephalalgia 2014;34:114–25. 10.1177/0333102413500727 [DOI] [PubMed] [Google Scholar]
- 20. Diener H-C, Barbanti P, Dahlöf C, et al. BI 44370 TA, an oral CGRP antagonist for the treatment of acute migraine attacks: results from a phase II study. Cephalalgia 2011;31:573–84. 10.1177/0333102410388435 [DOI] [PubMed] [Google Scholar]
- 21. Hewitt DJ, Aurora SK, Dodick DW, et al. Randomized controlled trial of the CGRP receptor antagonist MK-3207 in the acute treatment of migraine. Cephalalgia 2011;31:712–22. 10.1177/0333102411398399 [DOI] [PubMed] [Google Scholar]
- 22. Voss T, Lipton RB, Dodick DW, et al. A phase IIb randomized, double-blind, placebo-controlled trial of ubrogepant for the acute treatment of migraine. Cephalalgia 2016;36:887–98. 10.1177/0333102416653233 [DOI] [PubMed] [Google Scholar]
- 23. Ho TW, Connor KM, Zhang Y, et al. Randomized controlled trial of the CGRP receptor antagonist telcagepant for migraine prevention. Neurology 2014;83:958–66. 10.1212/WNL.0000000000000771 [DOI] [PubMed] [Google Scholar]
- 24. Dodick DW, Goadsby PJ, Spierings ELH, et al. Safety and efficacy of LY2951742, a monoclonal antibody to calcitonin gene-related peptide, for the prevention of migraine: a phase 2, randomised, double-blind, placebo-controlled study. Lancet Neurol 2014;13:885–92. 10.1016/S1474-4422(14)70128-0 [DOI] [PubMed] [Google Scholar]
- 25. Skljarevski V, Matharu M, Millen BA, et al. Efficacy and safety of galcanezumab for the prevention of episodic migraine: results of the EVOLVE-2 phase 3 randomized controlled clinical trial. Cephalalgia 2018;38:1442–54. 10.1177/0333102418779543 [DOI] [PubMed] [Google Scholar]
- 26. Oakes TMM, Skljarevski V, Zhang Q, et al. Safety of galcanezumab in patients with episodic migraine: a randomized placebo-controlled dose-ranging phase 2B study. Cephalalgia 2018;38:1015–25. 10.1177/0333102417747230 [DOI] [PubMed] [Google Scholar]
- 27. Stauffer VL, Dodick DW, Zhang Q, et al. Evaluation of Galcanezumab for the prevention of episodic migraine: the EVOLVE-1 randomized clinical trial. JAMA Neurol 2018;75:1080–8. 10.1001/jamaneurol.2018.1212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Goadsby PJ, Reuter U, Hallström Y, et al. A controlled trial of erenumab for episodic migraine. N Engl J Med 2017;377:2123–32. 10.1056/NEJMoa1705848 [DOI] [PubMed] [Google Scholar]
- 29. Dodick DW, Ashina M, Brandes JL, et al. Arise: a phase 3 randomized trial of erenumab for episodic migraine. Cephalalgia 2018;38:1026–37. 10.1177/0333102418759786 [DOI] [PubMed] [Google Scholar]
- 30. Dodick DW, Silberstein SD, Bigal ME, et al. Effect of Fremanezumab compared with placebo for prevention of episodic migraine: a randomized clinical trial. JAMA 2018;319:1999–2008. 10.1001/jama.2018.4853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Dodick D, Goadsby P, Silberstein S, et al. Randomized, double-blind, placebo-controlled trial of ALD403, an anti-CGRP peptide antibody in the prevention of chronic migraine. (S52.003). Neurology 2017;88. [Google Scholar]
- 32. Dodick DW, Goadsby PJ, Silberstein SD, et al. Randomized, double-blind, placebo-controlled, phase II trial of ALD403, an anti-CGRP peptide antibody in the prevention of frequent episodic migraine. Lancet Neurology 2014;13(16 Supplement):1100–7. [DOI] [PubMed] [Google Scholar]
- 33. Dodick DW, Goadsby PJ, Ferguson M, et al. Sustained responseresponse outcomesoutcomes from a phasephase 2a2A, randomizedrandomized, doubledouble-blind, placeboplacebo-controlled studystudy of ly2951742, a monoclonalmonoclonal antibodyantibody to calcitonincalcitonin genegene-related peptidepeptide, for the preventionprevention of migrainemigraine: AA post-hoc analysis. Headache 2015;55(Suppl 3). [Google Scholar]
- 34. Goadsby PJ, Dodick D, Martinez J, et al. Onset of efficacy of LY2951742 in migraine prevention: post-hoc analysis of phase 2A, randomized, double-blind, placebo-controlled study data of a calcitonin gene-related peptide monoclonal antibody. Cephalalgia 2015;35. [Google Scholar]
- 35. Headache Classification Subcommittee of the International Headache Society The International Classification of headache disorders: 2nd edition. Cephalalgia 2004;24 9–160. [DOI] [PubMed] [Google Scholar]
- 36. Hepp Z, Bloudek LM, Varon SF. Systematic review of migraine prophylaxis adherence and persistence. J Manag Care Pharm 2014;20:22–33. 10.18553/jmcp.2014.20.1.22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Peres MFP, Silberstein S, Moreira F, et al. Patients' preference for migraine preventive therapy. Headache 2007;47:540–5. 10.1111/j.1526-4610.2007.00757.x [DOI] [PubMed] [Google Scholar]
- 38. Rozen TD. Migraine prevention: What patients want from medication and their Physicians (a headache specialty clinic perspective). Headache 2006;46:750–3. 10.1111/j.1526-4610.2006.00429.x [DOI] [PubMed] [Google Scholar]
- 39. Bigal ME, Dodick DW, Krymchantowski AV, et al. TEV-48125 for the preventive treatment of chronic migraine: Efficacy at early time points. Neurology 2016;87:41–8. 10.1212/WNL.0000000000002801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Schwedt TJ, Alam A, Reed ML, et al. Factors associated with acute medication overuse in people with migraine: results from The 2017 migraine in America symptoms and Treatment (mast) study. J Headache Pain 2018;19:38–46. 10.1186/s10194-018-0865-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Smith J, Dodick DW, Goadsby PJ, et al. ALD403 (eptinezumab) elicits meaningful reductions in migraine activity 24 hours after a single intravenous administration. Headache 2017;57(Suppl 3):179–80.28128460 [Google Scholar]