ABSTRACT
Background: Violence against women is a global public health problem. A better understanding of risk factors for intimate partner violence (IPV) exposure during pregnancy is important to develop interventions for supporting women being exposed to IPV.
Objective: The purpose of this study was to measure the prevalence of IPV during pregnancy and analyse how social support and various risk factors are associated with IPV.
Methods: A cross-sectional study conducted among 1309 pregnant women in Dong Anh district, Vietnam. Information about socio-economic conditions and previous exposure to IPV was collected when women attended antenatal care before the 24th gestational week. Information about social support information and exposure to IPV during pregnancy was collected in the 30th-34th gestational week. Multivariable regression was used to identify associations between IPV, social support and other potential risk factors.
Results: The prevalence of IPV exposure during pregnancy was 35.2% (Emotional violence: 32.2%; physical violence: 3.5% and sexual violence: 9.9%). There was a statistically significant association between previous IPV exposure, lack of social support and IPV exposure during pregnancy. After adjustment for socioeconomic characteristics, pregnant women who had previously been exposed to IPV were more likely to be exposed IPV at least one time (AOR = 6.3; 95% CI: 4.9–8.2) as well as multiple times (AOR = 6.0; 95% CI: 4.5–8.0). Similarly, pregnant women having a lack of social support had a higher likelihood of being exposed to IPV at least one time (AOR = 3.1; 95% CI: 2.4–3.9) or multiple times (AOR = 2.9; 95% CI: 2.2–3.8).
Conclusion: IPV is relatively high during pregnancy in Vietnam. Previous exposure to IPV and lack of social support is associated with increased risk of violence exposure among pregnant women in Vietnam.
SPECIAL ISSUE: Gender and Health Inequality
KEYWORDS: Intimate partner violence, pregnancy, prevalence, risk factors, social support
Background
Intimate partner violence (IPV) against women is a global public health crisis [1]. World Health Organization (WHO) reported that 35% of women worldwide experienced physical and/or sexual violence in 2013, of which the rate of IPV has been generally higher in low and middle-income countries in comparison with high-income countries [2,3]. IPV rates are considerably high among women who are young [4–7]; unemployed [4,6–8]; have a low educational level and low income [4,7,9]; and live in rural areas [4,5,8,9]. In addition, those being married to a partner who is unemployed have low education or abuse alcohol are also at increased risk of IPV [4,5,9]. Pregnant women are particularly vulnerable to IPV. Although it is controversial whether IPV increases during pregnancy or not [10], this serious issue significantly reduces the health of women and their new-born children, as well as increases risk of infant mortality [11–14]. In low- and middle-income countries, the prevalence of pregnancy-related IPV range from 2%-57% [4,15].
Social support is an important instrument to prevent the occurrence of IPV as well as its adverse effects on pregnant women [16–19]. Social support is a critical function of social relationships, referring that a person has friends, family or social organizations who help providing a broader focus and positive self-image if needed [20]. It includes emotional (empathy, love, trust), instrumental (being available if need), and informational (supportive advice and suggestions) perspectives [20,21]. Prior studies suggested that women with high level of social support had a lower risk of IPV [22,23]. However, most of the studies have been conducted in high-income countries and not looked into the effects of different types of social support on the occurrence of IPV.
In Vietnam, according to a WHO’s report in 2014, the rate of pregnant women accessing antenatal care (ANC) is high with 94% due to a substantial progress in developing the primary health-care sector [24]. Nonetheless, a national study on violence against women in 2010 showed that 58% of women suffered violence at least once in their life including emotional (54%), physical (32%) and sexual (10%) violence [25]. This survey also indicated that 5% of pregnant women experienced physical violence [25]. However, literature about the relationship between social support and IPV is still limited. Therefore, this study aimed to measure the prevalence of IPV during pregnancy and analyse how social support and various risk factors are associated with IPV. The findings will partly contribute to design contextualized interventions and policies in addressing the IPV and its negative effects among pregnant women in Vietnam.
Methods
Study design and setting
A cross-sectional study was implemented that was nested within a larger cohort study involving 1337 pregnant women in Dong Anh District, Hanoi, Vietnam. The purposes of cohort study were to identify the prevalence of IPV during pregnancy and to measure the associations between IPV and the risk of low birth weight and preterm birth among pregnant women.
Sampling procedure
Participants were pregnant women who were before 24 weeks of gestation (confirmed by ultrasound scanning) at Dong Anh District from May 2014 to August 2015. Data collection was conducted in three stages: (i) at enrolment or baseline (collecting socio-demographic and reproductive health information); (ii) at 30–34 weeks of pregnancy (collecting violence exposure information – before and during pregnancy, and social support); and (iii) at delivery (measuring birth weight and gestational age of the child). This study used data at stage (i) and (ii). There were 1.337 pregnant women enrolling in the study at stage (i) and 1309 (97.9%) completing surveys at stage (ii). The processing of data collection is presented in Figure 1.
Figure 1.
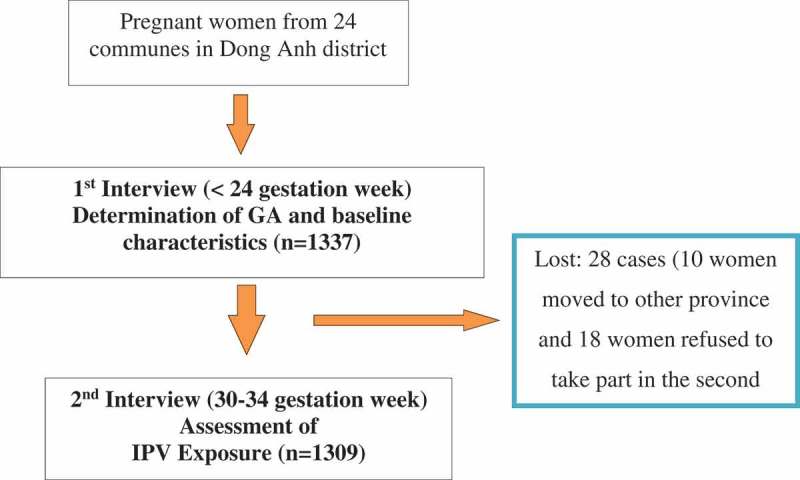
Follow-up chart.
Data collection and measurement
Six interviewers were selected among 24 staffs in the Dong Anh District Population Centre by the research group. They were aged 35–45, had a college degree and had experience in working with the community. The interviewers were trained about interview skills in two weeks. A questionnaire was developed based on the WHO questionnaire on health and violence against women, which was used in the National Study on Violence against Women in Vietnam in 2010 [25]. The questionnaire was piloted among 30 pregnant women living in study settings and revised before implementing data collection.
Dependent variable
Exposure to IPV during pregnancy: Our participants were asked about whether they experienced any specific violence by their husband during their current pregnancy, as well as the number of times of being exposed to different types of violence. Emotional violence referred to those being insulted, humiliated, intimidated or threatened to hurt her or someone she cared for. Meanwhile, physical violence was defined as being slapped, pushed, hit, kicked, chocked or threatened. Sexual violence referred to pregnant women who were physically forced to have sexual intercourse, and accepted due to fear of partner’s reaction, or were forced to do a sexual act which she found degrading or humiliating. Women were considered being exposed to IPV during pregnancy if they exposed to any form of IPV at least once.
Independent variables
Socioeconomic characteristics: Information about age, educational level (below high school/high school/above high school) and occupation (White-collar worker/Blue-collar worker/Farmer/Other (housewives, small business …)). was collected. The socioeconomic index was measured by asking: ‘Does your household have television, landline phone, mobile phone, refrigerator, computer or bank account ?’. The answers were coded in two categories: yes = 1; no = 0. After calculating the asset index of household, a quintile variable was defined and coded into three groups.
Previous exposure to IPV: To explore the history of IPV exposure, pregnant women were asked following question: ‘In the past 12 months before pregnancy, 1) Has your partner done things to scare or intimidate you on purpose?’; 2) ‘Has your partner threatened to hurt you or someone you care for?’; 3) ‘Has your partner hit you, slapped you, or thrown something at you that could hurt you’; and, 4) ‘Has your partner forced you or pressured you to have sexual intercourse when you did not want to’. Previous emotional IPV was determined if participants answered ‘Yes’ for question 1 and 2. Moreover, physical and sexual IPV were defined if the answers of question 3 and 4 were ‘Yes’, respectively. Women confirming any of the four questions were considered to have been exposed to previous IPV.
Social support
Social support was assessed using seven questions about emotional, instrumental and informational support [20]. Each question had five options to respond: always, most of the time, some of the time, rarely and never, ranking from 5 to 1.
Emotional support was measured via two questions: 1) ‘Do you have someone whom you know that you can always trust?’; and 2) ‘Do you have someone with whom you can share your thoughts and worries?’. Pregnant women had emotional support if the total score was 8 or more.
Instrumental support was evaluated using four questions: 1) ‘Do you have someone who cares for you by making sure you get enough to eat?’; 2) ‘Do you have someone who helps you with daily tasks (shopping, cooking, childcare, transportation, etc.)?’; 3) ‘Do you have someone in your family who takes a positive interest in your antenatal care visits?’; and 4) ‘Do you have someone who can help you financially if you need it?’. Participants had instrumental support if they had a total score of 16 or more.
Finally, one question was used to define informational support: ‘Do you have someone who helps you if you need to make difficult decisions?’. A score of 4 or more was used to identify having informational support.
The total score of seven questions was calculated (max score 35), and having social support was determined if the total score was 28 or more. The cut-off point was identified based on the median score among women who were not exposed to IPV during pregnancy, which was validated elsewhere [26,27].
Statistical analysis
Data (S1 File, S2 File) were cleaned and double data entry was implemented using EpiData version 3.1 by two researchers. STATA version 14 was used for statistical analysis. Descriptive statistics were used to summarize the prevalence of IPV and frequency of IPV episodes during pregnancy. The analysis compared pregnant women who reported having experienced ‘any IPV’ and ‘IPV repeatedly’ with those not suffering any violence during pregnancy. For the latter, we excluded those with only one exposure and kept women who had multiple exposures. To determine risk factors associated with IPV exposure during pregnancy, crude odds ratios (OR) with 95% confidence intervals were calculated. Multivariable logistic regression then was used for controlling potential confounding factors (women’s age, education, occupation, economic status, previous IPV and social support). Statistical significance was considered at p value of less than 0.05.
Ethical consideration
Our participants were informed about the study and written informed consents were then obtained. If they were less than 18 years old, the researcher explained to their parents about the study and the consent forms were signed by both women and their parents. After enrolment, participants were assigned different identification code (ID) and interviewers write the ID in each question sheet to instead of women’s identity. The title ‘Survey on Women’s Health and Life Experiences’ was used in research documents to not reveal that the study was about violence, which did not put respondents and interviewers at risk. The interviewers had to sign in ‘security agreement’ form as part of the employment contract. For those suffering IPV, after the entire cohort, we referred them to the appropriate social and psychological professional supports that were available in the community according to the guideline of World Health Organization [28]. The study was approved by the Ethical Committee of Hanoi Medical University, Vietnam (Decision 137/HMU IRB dated 29 November 2013).
Results
Among 1,337 pregnant women enrolling at baseline, 1309 (97.9%) attended the second interview at the gestational week 30th-34th. The mean age was 27 years (SD = 4.8), ranging from 17 to 47 years. There were 44% educated at high school level education or above and 33% employed. Among women who were lost to follow up, the mean age was 27.6 years (SD = 4.3), 54% were educated at high school level or above and 10.7% were employed.
Table 1 presents the prevalence of IPV during pregnancy, 35.2% had been exposed to IPV at least once, and of those exposed, 85.9% had been exposed repeated times. Prevalence and frequency of the different types of IPV were: emotional violence: 32.2% (84.3% had been exposed 2 times or more); physical violence: 3.5% (38.1% had been exposed 2 times or more) and; sexual violence: 9.9% (92.3% had been exposed 2 times or more).
Table 1.
The prevalence of IPV during pregnancy.
| n = 1309 | % | |
|---|---|---|
| Any IPV during pregnancy (n = 461) | ||
|
848 | 64.8 |
|
461 | 35.2 |
|
65 | 14.1 |
|
325 | 70.5 |
|
71 | 15.4 |
| Emotional IPV during pregnancy (n = 421) | ||
|
888 | 67.8 |
|
421 | 32.2 |
|
66 | 15.7 |
|
303 | 72.0 |
|
52 | 12.3 |
| Physical IPV during pregnancy (n = 46) | ||
|
1263 | 96.5 |
|
46 | 3.5 |
|
28 | 60.9 |
|
15 | 32.6 |
|
3 | 6.5 |
| Sexual IPV during pregnancy (n = 130) | ||
|
1179 | 90.1 |
|
130 | 9.9 |
|
10 | 7.7 |
|
89 | 68.5 |
|
31 | 23.8 |
Table 2 shows that in the univariate analysis, education level, occupation and economic status were found to be associated with IPV exposure. However, in multivariable regression, women who were workers and farmers were 1.9 (OR = 1.9; 95%CI: 1.4–2.7) and 2.4 times (OR = 2.4; 95%CI: 1.5–3.6) more likely to be exposed to IPV repeated times, respectively, which were higher compared to women being white-collar workers ư. In addition, those aged from 33 to 47 were less likely to suffer from repeated IPV (OR = 0.6; 95%CI = 0.4–0.9).
Table 2.
Association between socio-economic characteristics and IPV during pregnancy.
| IPV exposure, any vs. no exposure |
IPV exposure, repeated times vs. no exposure |
||||||
|---|---|---|---|---|---|---|---|
| Total n (%) |
IPV exposure n (%) (n = 461) |
Crude OR (95% CI) |
AOR (95% CI) |
IPV exposure n (%) (n = 396) |
Crude OR (95% CI) |
AOR (95% CI) |
|
| Age groups | |||||||
|
1122 (85.7) | 406 (88.1) | 1 | 1 | 349 (88.1) | 1 | 1 |
|
187 (14.3) | 55 (11.9) | 0.7 (0.5–1.0) | 0.6 (0.4–0.9) | 47 (11.9) | 0.7 (0.5–1.0) | 0.6 (0.4–0.9) |
| Education level | |||||||
|
256 (19.6) | 104 (22.6) | 1 | 1 | 84 (21.2) | 1 | 1 |
|
482 (36.8) | 175 (38.0) | 0.8 (0.6–1.1) | 0.9(0.6–1.2) | 156 (39.4) | 0.9 (0.7–1.3) | 0.9 (0.7–1.3) |
|
571 (43.6) | 182 (39.5) | 0.7 (0.5–0.9) | 0.9 (0.6–1.3) | 156 (39.4) | 0.7 (0.5–0.9) | 0.9 (0.7–1.4) |
| Occupation | |||||||
|
425 (32.5) | 109 (32.5) | 1 | 1 | 89 (22.5) | 1 | 1 |
|
354 (27) | 139 (30.2) | 1.9 (1.4–2.6) | 1.8 (1.3–2.5) | 122 (30.8) | 2.0 (1.5–2.8) | 1.9 (1.4–2.7) |
|
170 (13) | 74 (16.1) | 2.2 (1.5–3.3) | 2.2 (1.4–3.3) | 64 (16.2) | 2.4 (1.6–3.5) | 2.4 (1.5–3.6) |
|
360 (27.5) | 139 (30.2) | 1.8 (1.3–2.5) | 1.8 (1.3–2.4) | 121 (30.5) | 1.9 (1.4–2.7) | 1.9 (1.4–2.7) |
| Economic status | |||||||
|
456 (34.8) | 183 (39.7) | 1 | 1 | 155 (39.1) | 1 | 1 |
|
657 (50.2) | 218 (47.3) | 0.7 (0.6–0.9) | 0.8 (0.6–1.1) | 192 (48.5) | 0.8 (0.6–1) | 0.9 (0.6–1.1) |
|
196 (15) | 60 (13.0) | 0.7 (0.5–0.9) | 0.8 (0.5–1.2) | 49 (12.4) | 0.6 (0.4–0.9) | 0.8 (0.5–1.1) |
Table 3 indicates that after adjusting to age, education, occupation, and economic status, pregnant women being exposed to emotional, physical and sexual IPV previously, as well as not receiving emotional, instrumental and informational support had significantly high likelihood of being exposed to IPV during pregnancy. Experiencing previous emotional IPV had the largest effect on predicting multiple IPV during pregnancy (OR = 6.6; 95%CI = 5.1–8.7) compared to other factors. In addition, Crude OR and Adjusted OR in this table did not change significantly, showing stable relationships between previously experiencing IPV, social support and suffering IPV during pregnancy.
Table 3.
Associate between act of previous violence and social support and IPV during pregnancy.
| IPV exposure, any vs. no exposure |
IPV exposure, repeated times vs. no exposure |
||||||
|---|---|---|---|---|---|---|---|
| Total n (%) |
IPV exposured n (%) (n = 461) |
Crude OR (95% CI) |
AOR* (95% CI) |
IPV exposure n (%) (n = 396) |
Crude OR (95% CI) |
AOR* (95% CI) |
|
| Previous emotional IPV | |||||||
|
738 (56.4) | 130 (28.2) | 1 | 1 | 110 (27.8) | 1 | 1 |
|
571 (43.6) | 331 (71.8) | 6.5 (4.9–8.5) | 6.5 (5.0–8.5) | 286 (72.2) | 6.6 (4.9–8.8) | 6.6 (5.1–8.7) |
| Previous physical IPV | |||||||
|
1160 (88.6) | 364 (79.0) | 1 | 1 | 312 (78.8) | 1 | 1 |
|
149 (11.4) | 97 (21.0) | 4.1 (2.8–5.9) | 4.0 (2.8–5.8) | 84 (21.2) | 4.1 (2.8–6) | 4.1 (2.8–6) |
| Previous sexual IPV | |||||||
|
1200 (91.7) | 393 (85.3) | 1 | 1 | 339 (85.6) | 1 | 1 |
|
109 (8.3) | 68 (14.8) | 3.4 (2.3–5.1) | 3.1 (2.1–4.7) | 57 (14.4) | 3.3 (2.2–5.1) | 2.9 (1.9–4.5) |
| Emotional support | |||||||
|
1010 (77.2) | 308 (66.8) | 1 | 1 | 311 (78.5) | 1 | 1 |
|
299 (22.8) | 153 (33.2) | 2.4 (1.8–3.1) | 2.2 (1.7–2.9) | 85 (21.5) | 2.5 (1.9–3.3) | 2.2 (1.7–3.0) |
| Instrumental support | |||||||
|
759 (58) | 199 (43.2) | 1 | 1 | 173 (43.7) | 1 | 1 |
|
550 (42) | 262 (56.8) | 2.6 (2.0–3.3) | 2.5 (2.0–3.2) | 223 (56.3) | 2.5 (2–3.2) | 2.4 (1.9–3.1) |
| Informational support | |||||||
|
933 (71.3) | 286 (62.0) | 1 | 1 | 248 (62.6) | 1 | 1 |
|
376 (28.7) | 175 (38.0) | 1.8 (1.4–2.3) | 2.2 (1.3–3.7) | 148 (37.4) | 1.9 (1.5–2.5) | 1.8 (1.4–2.3) |
*Adjusted for women’s age, education, occupation, economic status.
Table 4 shows that pregnant women who had previously been exposed to IPV were more likely to be exposed IPV at least one time (AOR = 6.3; 95% CI: 4.9–8.2) as well as multiple times (AOR = 6.0; 95% CI: 4.5–8.0). Similarly, pregnant women having a lack of social support had a higher likelihood of being exposed to IPV at least one time (AOR = 3.1; 95% CI: 2.4–3.9) or multiple times (AOR = 2.9; 95% CI: 2.2–3.8).
Table 4.
Multiple logistic regressions between previous IPV/social support and IPV during pregnancy.
| IPV exposure, any vs. no exposure |
IPV exposure, repeated times vs. no exposure |
||||||
|---|---|---|---|---|---|---|---|
| Total n (%) |
IPV exposure n (%) |
Crude OR (95% CI) |
AOR* (95% CI) |
IPV exposure n (%) |
Crude OR (95% CI) |
AOR* (95% CI) |
|
| Previous IPV | |||||||
|
702 (53.6) | 119 (25.8) | 1 | 1 | 100 (25.2) | 1 | 1 |
|
607 (46.4) | 342 (74.2) | 6.3 (4.8–8.4) | 6.3 (4.9–8.2) | 296 (74.8) | 6.5 (4.8–8.7) | 6.0 (4.5–8.0) |
| Social support | |||||||
|
732 (55.9) | 173 (37.5) | 1 | 1 | 143 (36.1) | 1 | 1 |
|
577 (44.1) | 288 (62.5) | 3.2 (2.5–4.1) | 3.1 (2.4–3.9) | 253 (63.9) | 3.4 (2.6–4.4) | 2.9 (2.2–3.8) |
*Adjusted for women’s age, education, occupation, economic status
Discussion
Prevalence of IPV
In our study, more than one-third of pregnant women had been exposed to IPV during pregnancy with 32.2% women reporting exposure to emotional, 3.5% to physical and 10% to sexual violence. These findings were different from a previous work that the prevalence of emotional, physical and sexual violence was 28.4%, 13.8%, and 8.0%, respectively [9]. Our physical and sexual violence rates also differed from those in other countries such as China (11.9% ad 9.1%, respectively), and Japan (2.3% and 1%, correspondingly) [6,8]; and much lower compared to Thailand, where 54% of pregnant women were exposed to emotional violence, 27% to physical violence and 19% to sexual violence [29]. These dissimilarities might be explained by the use of different measures and definitions of violence [5,9,30,31]. In this study, we used the WHO questionnaire for measuring IPV among women, while the Chinese study used the revised conflict tactics scale and the Japanese study used an IPV screening tool (VAWS) [6,8]. In addition, the disparity may be due to the willingness of women to disclose the IPV exposure, which relies on the culture, the fear of retaliation and the availability of support [5,32,33]. In Vietnam, particularly in rural areas, the perceived social norm is that women were responsible for the marital harmony while men had a role as primary income earners (i.e. ‘pillars’ in the family) [34]. Therefore, domestic violence might be treated as private issues and could not be disclosed for a ‘Happy’ family [35–37].
Risk factor of IPV
Our current study shows in multivariable regression that being blue-collar workers or farmers were risk factors of being exposed to IPV repeatedly, while those having higher age were less likely to suffer multiple IPV. This is consistent with two recent meta-analyses [4,9] and studies in other settings such as India, Bangladesh, Nepal, Japan, and Egypt [6,7,38]. In Vietnam, while white-collar workers were related to high education and income, those being blue-collar workers or farmers were more likely to have low education [39]. A possible explanation behind the found linkage between these social vulnerabilities (young, manual jobs such as blue-collar workers and farmers) and IPV is that those women had more difficult access to information about women’s rights. This situation may foster higher levels of gender inequality and greater acceptance of norms that support violence against women [4,9].
Our result demonstrates that previous IPV exposure was a strong risk factor for IPV during pregnancy, which was consistent with other previous studies [4,9]. Indeed, repeated IPV exposure is common among Vietnamese women and being pregnant does not protect women against violence [25]. Since the women were asked about IPV that had occurred during the past 12 months, we assumed that the abusive acts previously and during current pregnancy were enacted by the same partner. To stop the vicious cycle of repeated IPV exposure and prevent the negative impact of IPV among pregnant women, it is of major importance to start implementing IPV screening programs in relation to antenatal care. Globally, screening IPV, receiving counselling from, and building trusting relationships with health-care providers or other social workers would decline the occurrence of IPV during pregnancy and improve knowledge and capacities to cope with IPV among pregnant women [40,41].
Social support
Social support was found to be a protective factor against IPV during pregnancy. This result is consistent with a study from Spain, which reported that women who were supported socially had a lower probability of IPV compared to those not being supported socially [22]. In literature, social support could maintain a positive self-esteem and self-concept [20], which might change women’s attitudes toward IPV and reduce risk of IPV [30]. It also reduced IPV-related eating disorders [17] and stress during pregnancy [16,42], assisting in preventing adverse effects of IPV on pregnant women’s mental health. However, it is cautious that the nature of cross-sectional design in these studies and our study as well does not allow determining the causal relationship between IPV and social support; thus, further longitudinal and experimental studies should be warranted to fill this knowledge gap.
Limitation of the study
Our study has some important limitations that should be considered. First, it relies on a cross-sectional design; therefore, it is not possible to conclude the causal relationship between social support and IPV. Second, selection bias may occur since the study only included women attending antenatal care. However, the vast majority of women in the study setting attended the service, implying the representative of our sample to the pregnant women living in Dong Anh district. Third, because violence is a sensitive topic, it may be difficult to obtain valid information about IPV exposure. To overcome this drawback, the research assistants, who performed the interviews, developed a good relation with the women and the interviews were performed rather as conversations than strict questionnaire-based interviews. To create an atmosphere of confidentiality and empathy, the research assistants were further encouraged to share their own experiences with the women they interviewed. Finally, 28 pregnant women who were lost to follow-up might have different IPV and social support characteristics compared to those participating in the follow-up study, which could affect the results. Other limitation, when minors participated in the study, they required the consent of a guardian as their mother or father. It was maybe a social desirability bias. In Vietnam, the law stipulates that minors are people under 18 years old. When they participated in community studies, they required the consent of a guardian as their mother or father. In our study, to avoid the risk of being involved in the study, we changed the research name to “research on women’s health and life experiences“. In our study, there were 02 participants who were 17 years old. We have explained the purpose of the study to the mother who was their guardian and they agreed to sign the consent form. The information of interview was coded and without disclosure to anyone including their guardian.
Conclusion
IPV is relatively high during pregnancy in Vietnam. Previous exposure to IPV and lack of social support is associated with increased risk of violence exposure among pregnant women in Vietnam.
Biography
All authors designed the study, developed the questionnaires and supervised the data collection. Thanh carried out the data analysis and wrote the first draft of the manuscript. Vibeke supervised the data analysis and interpretation of the findings. Vibeke reviewed the article critically for important intellectual content. All authors commented on manuscript drafts. All authors read and approved the final manuscript.
Responsible Editor
Isabel Goicolea, Umeå University, Sweden
Funding Statement
We would like to thank DANIDA (the Danish International Development Agency) for supporting the study. The funders had no role in study design, data collection and analysis, manuscript preparation or decision to publish.
Acknowledgments
This research was conducted under the auspices of the larger research project The Impact of Violence on Reproductive Health in Tanzania and Vietnam (PAVE). We are extremely grateful to the pregnant women who took part in this study, the research assistants and health staffs in Dong Anh district.
Disclosure statement
No potential conflict of interest was reported by the authors.
Ethics and consent
The study was approved by the Ethical Committee of Hanoi Medical University, Vietnam (Decision 137/HMU IRB dated 29 November 2013).
Paper context
Violence against women is a global problem. IPV during pregnancy does not only affect the women’s health but also imposes adverse health effect on the new-born children. A better understanding of risk factors for IPV exposure during pregnancy is important to develop interventions to support women. In this study (conducted among 1309 pregnant women), we show that there was a statistically significant association between previous IPV exposure, lack of social support and IPV exposure in pregnancy.
Supplementary material
Supplemental data for this article can be accessed here.
References
- [1].Garcia-Moreno C, Jansen HAFM, Ellsberg M, et al. Prevalence of intimate partner violence: findings from the WHO multi-country study on women’s health and domestic violence. Lancet. 2006;368:1260–8. [DOI] [PubMed] [Google Scholar]
- [2].World Health Organization Global status report on violence prevention. Geneva: World Health Organization; 2014. [Google Scholar]
- [3].Garcia-Moreno C, Pallitto C, Devries K, et al. Global and regional estimates of violence against women: prevalence and health effects of intimate partner violence and non-partner sexual violence. Geneva (Switzerland): World Health Organization; 2013. [Google Scholar]
- [4].Shamu S, Abrahams N, Temmerman M, et al. A systematic review of African studies on intimate partner violence against pregnant women: prevalence and risk factors. PLoS ONE. 2011;6:e17591 Epub 2011/ 03/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Capaldi DM, Knoble NB, Shortt JW, et al. A systematic review of risk factors for intimate partner violence. Partner Abuse. 2012;3:231–280. Epub 2012/ 07/04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kita S, Yaeko K, Porter SE.. Prevalence and risk factors of intimate partner violence among pregnant women in Japan. Health Care Women Int. 2014;35:442–457. Epub 2013/ 12/20. [DOI] [PubMed] [Google Scholar]
- [7].Ibrahim Z, Fau - Sayed Ahmed WA, Sayed Ahmed W, et al. Intimate partner violence among Egyptian pregnant women: incidence, risk factors, and adverse maternal and fetal outcomes. Clin Exp Obstet Gynecol. 2015;42:212–219. [PubMed] [Google Scholar]
- [8].Chan KL, Brownridge DA, Tiwari A, et al. Associating pregnancy with partner violence against Chinese women. J Interpers Violence. 2011;26:1478–1500. Epub 2010/ 05/25. [DOI] [PubMed] [Google Scholar]
- [9].James L, Brody D, Hamilton Z. Risk factors for domestic violence during pregnancy: a meta-analytic review. Violence Vict. 2013;28:359–380. Epub 2013/ 07/19. [DOI] [PubMed] [Google Scholar]
- [10].Jasinski JL. Pregnancy and domestic violence: a review of the literature. Trauma Violence Abuse. 2004;5:47–64. Epub 2004/ 03/10. [DOI] [PubMed] [Google Scholar]
- [11].RE AL B, Bhutta Z, Caulfield LE, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–260. [DOI] [PubMed] [Google Scholar]
- [12].Abadi MN, Ghazinour M, Nygren L, et al. Birth weight, domestic violence, coping, social support, and mental health of young Iranian mothers in Tehran. J Nerv Ment Dis. 2013;201:602–608. Epub 2013/ 07/03. [DOI] [PubMed] [Google Scholar]
- [13].Chai J, Fink G, Kaaya S, et al. Association between intimate partner violence and poor child growth: results from 42 demographic and health surveys. Bull World Health Organ. 2016;94:331–339. Epub 2016/ 05/06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Hoang TN, Van TN, Gammeltoft T, et al. Association between intimate partner violence during pregnancy and adverse pregnancy outcomes in Vietnam: a prospective cohort study. PLoS One. 2016;11:e0162844 Epub 2016/ 09/16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].KM KS D, Johnson H, Stöckl H, et al. Intimate partner violence during pregnancy: analysis of prevalence data from 19 countries. Reprod Health Matters. 2010;18:158–170. [DOI] [PubMed] [Google Scholar]
- [16].Iranzad I, Bani S, Hasanpour S, et al. Perceived social support and stress among pregnant women at health centers of Iran - Tabriz. J Caring Sci. 2014;3:287–295. Epub 2015/ 02/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Schirk DK, Lehman EB, Perry AN, et al. The impact of social support on the risk of eating disorders in women exposed to intimate partner violence. Int J Women’s Health. 2015;7:919–931. Epub 2015/ 12/10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Norbeck JS, DeJoseph JF, Smith RT. A randomized trial of an empirically-derived social support intervention to prevent low birthweight among African American women. Soc Sci Med. 1996;43:947–954. Epub 1996/ 09/01. [DOI] [PubMed] [Google Scholar]
- [19].Hetherington E, Doktorchik C, Premji SS, et al. Preterm birth and social support during pregnancy: a systematic review and meta-analysis. Paediatr Perinat Epidemiol. 2015;29:523–535. Epub 2015/ 09/04. [DOI] [PubMed] [Google Scholar]
- [20].Weber ML. She stands alone: A review of the recent literature on women and social support. Canada: Prairie Women’s Health centre of Excellence; 1998. [Google Scholar]
- [21].House JS. Work stress and social support. Canada: Addison-Wesley Publicing Company; 1981. [Google Scholar]
- [22].Plazaola-Castano J, Ruiz-Perez I, Montero-Pinar MI. The protective role of social support and intimate partner violence. Gac Sanit. 2008;22:527–533. Epub 2008/ 12/17. [DOI] [PubMed] [Google Scholar]
- [23].Branch KA. The role of social support in the use of intimate partner violence: an exploration of the role of social support in heterosexual women’s use of non-lethal intimate partner violence. Saarbrücken, Germany: VDM Verlag Dr Muller Aktiengesellschaft; 2008. [Google Scholar]
- [24].World Health Organization Sucess factors for women’s and children’s health: policy and programme highlights from 10 fast-track countries. Geneva, Switzerland: World Health Organization; 2014. [Google Scholar]
- [25].Henrica AFMJ, Vung ND, Anh HT, et al. Results from the national study on domestic violence against women in Vietnam. Vietnam: Ministry of Health; 2010. [Google Scholar]
- [26].Sarason IG, Levine HM, Basham RB, et al. Assessing social support: the social support questionnaire. J Pers Soc Psychol. 1983;44:127–139. [Google Scholar]
- [27].Coker AL, Smith PH, Thompson MP, et al. Social support protects against the negative effects of partner violence on mental health. J Womens Health Gend Based Med. 2002;11:465–476. Epub 2002/ 08/08. [DOI] [PubMed] [Google Scholar]
- [28].World Health Organization Responding to intimate partner violence and sexual violence against women: WHO clinical and policy guidelines. Italia: World Health Organization; 2013. [PubMed] [Google Scholar]
- [29].Saito A, Creedy D, Cooke M, et al. Effect of intimate partner violence on antenatal functional health status of childbearing women in Northeastern Thailand. Health Care Women Int. 2013;34:757–774. Epub 2013/ 06/25. [DOI] [PubMed] [Google Scholar]
- [30].Trinh OT, Oh J, Choi S, et al. Changes and socioeconomic factors associated with attitudes towards domestic violence among Vietnamese women aged 15–49: findings from the multiple indicator cluster surveys, 2006–2011. Glob Health Action. 2016;9:29577 Epub 2016/ 03/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Yount KM, VanderEnde K, Zureick-Brown S, et al. Measuring attitudes about women’s recourse after exposure to intimate partner violence: the ATT-RECOURSE scale. J Interpers Violence. 2014;29:1579–1605. Epub 2013/ 12/26. [DOI] [PubMed] [Google Scholar]
- [32].Krug EG, Mercy JA, Dahlberg LL, et al. The world report on violence and health. Lancet. 2002;360:1083–1088. Epub 2002/ 10/18. [DOI] [PubMed] [Google Scholar]
- [33].Valladares E, Pena R, Persson LA, et al. Violence against pregnant women: prevalence and characteristics. A population-based study in Nicaragua. BJOG. 2005;112:1243–1248. Epub 2005/ 08/17. [DOI] [PubMed] [Google Scholar]
- [34].Nhị TT, Hạnh NTT, Gammeltoft TM. Emotional violence and maternal mental health: a qualitative study among women in northern Vietnam BMC Women’s Health. 2018;18:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Vung ND, Ostergren PO, Krantz G. Intimate partner violence against women in rural Vietnam – different socio-demographic factors are associated with different forms of violence: need for new intervention guidelines? BMC Public Health. 2008;8:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kwiatkowski L. Domestic violence and the “Happy Family” in Northern Vietnam. Anthropol Now. 2011;3:20–28. [Google Scholar]
- [37].Schuler SR, Lenzi R, Hoang T-A, et al. Recourse seeking and intervention in the context of intimate partner violence in Vietnam: aqualitative study. J Family Issues. 2016;37:1151–1173. [Google Scholar]
- [38].Anand E, Unisa S, Singh J. Intimate partner violence and unintended pregnancy among adolescent and young adult married women in south Asia. J Biosoc Sci. 2017;49:206–221. Epub 2016/ 06/22. [DOI] [PubMed] [Google Scholar]
- [39].Tran T, Tran A, Pham T, et al. Local governance and occupational choice among young people: first evidence from Vietnam. Hanoi, Vietnam: University of Economics and Buisness, Vietnam National University, Hanoi; 2017. [Google Scholar]
- [40].Nelson HD, Bougatsos C, Blazina I. Screening women for intimate partner violence: a systematic review to update the U.S. preventive services task force recommendation. Ann Intern Med. 2012;156:796–808. [DOI] [PubMed] [Google Scholar]
- [41].Van Parys AS, Verhamme A, Temmerman M, Verstraelen H. Intimate partner violence and pregnancy: a systematic review of interventions. PLoS One. 2014;9:e85084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Shishehgar S, Mahmoodi A, Dolatian M, et al. The relationship of social support and quality of life with the level of stress in pregnant women using the PATH model. Iran Red Crescent Med J. 2013;15:560–565. Epub 2014/ 01/08. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


