Abstract
Introduction:
The purpose of this study is to characterize violence-related disparities experienced by young blacks in the U.S. Reducing violence experienced by blacks, particularly youth, who are at substantially higher risk, is essential to improving the health of blacks in the U.S.
Methods:
Data from four independent data sets for youth and adults were analyzed to examine rates of homicide, assault, injury from a physical fight, bullying victimization, and missing school because of safety concerns for non-Hispanic blacks and whites aged 10–34 years between 2010 and 2015. Disparities in adverse childhood experiences (e.g., exposure to violence and household challenges) and physical/mental health outcomes in adulthood were examined. Data were analyzed in 2017.
Results:
Black adolescents and young adults are at higher risk for the most physically harmful forms of violence (e.g., homicides, fights with injuries, aggravated assaults) compared with whites. In addition, black adults reported exposure to a higher number of adverse childhood experiences than whites. These adverse childhood experiences were positively associated with increased odds of self-reported coronary heart disease, fair or poor physical health, experiencing frequent mental distress, heavy drinking, and current smoking.
Conclusions:
Disproportionate exposure to violence for blacks may contribute to disparities in physical injury and long-term mental and physical health. Understanding the violence experiences of this age group and the social contexts surrounding these experiences can help improve health for blacks in the U.S. Communities can benefit from the existing evidence about policies and programs that effectively reduce violence and its health and social consequences.
INTRODUCTION
In the report, A Nation Free of Disparities in Health and Healthcare, the HHS highlights the disproportionate burden of mortality experienced by some racial and ethnic groups, including black Americans.1 Homicide is a leading cause of death for black Americans of all ages.2 Non-Hispanic black Americans (hereafter “blacks”) consistently experience the highest homicide rates among racial/ethnic subgroups, with rates far exceeding non-Hispanic whites (hereafter “whites”).3,4 Young blacks are at particularly high risk for homicide. The homicide rate for blacks aged 10—34 years was 2.6 times higher than the rate for blacks aged 35 years and older in 2015.5 In addition to agerelated risks, disparities in homicide rates between blacks and whites have persisted over time. For example in 2000, for people aged 10—34 years, homicide rates were more than 11 times higher for blacks than whites (i.e., 35.9 per 100,000 for blacks and 3.1 per 100,000 for whites).5 In 2015, the homicide rate for blacks aged 10—34 years (37.5 per 100,000) was 13 times the rate for whites (2.9 per 100,000).5
Reasons for disparities in violence between blacks and whites are understood.6 Minority populations are disproportionately exposed to conditions such as concentrated poverty, racism, limited educational and occupational opportunities, and other aspects of social and economic disadvantage contributing to violence.7 These conditions provide context for disproportionate rates of homicide and nonfatal violence experienced by blacks, particularly among young males.8,9 These disparities are sustained, in part, due to the persistence of unfavorable social conditions,10 and because exposure to childhood trauma and adversity is associated with increased risk for victimization and perpetration of violence, both within one’s lifetime and across generations.11,12
Less established and understood is the contribution of violence exposure to racial and ethnic disparities in a range of mental and physical health problems. Aside from immediate physical consequences of violence, stress and trauma in the form of victimization have the potential to set individuals on negative health trajectories with lasting consequences.13 Violence exposure is associated with increased risk of mental health problems, risky health-related behaviors (e.g., alcohol abuse, sexual risk-taking), chronic disease (e.g., coronary heart disease, diabetes), delinquency, and premature mortality.14,15 Evidence for causal relationships between early exposure to violence, especially child maltreatment, and health outcomes is emerging.16,17 This literature suggests racial and ethnic disparities in violence may be linked to other prominent health disparities.
Violence also exacts enormous and disproportionate social and economic costs in minority communities.18 These include medical, educational, and justice system costs, reduced labor market productivity, decreased property values, and disruption of community services.19–22 Thus, preventing violence exposure and intervening when violence has occurred has implications for the health and prosperity of racial and ethnic minority communities.
The purpose of this study is to update the literature on racial disparities in violence between black and white youth using data sources capturing different severity levels in violent outcomes (e.g., homicide versus assault). This paper also seeks to extend understanding of the impact of these disparities by examining associations between disparities in childhood adversity (e.g., child maltreatment) and adult health conditions. The results provide a basis for discussing available evidence for prevention that may be important for reducing these disparities.
METHODS
Study Sample
This study examined racial disparities in violent victimization across a range of violent behaviors, and health consequences associated with violence exposure during childhood by black youth and young adults aged 10–34 years.5,8 Rates of violence were stratified by sex, age, and race. Rate ratios (RRs) of population-based rates were calculated to show the magnitude of disparities between blacks and whites. Four independent, cross-sectional data sets were analyzed. Data were analyzed in years 2017–2018.
Measures
Data from the National Vital Statistics System (NVSS) for 2015 were analyzed to examine leading causes of death using the Web-based Injury Statistics Query and Reporting System (WISQARS). Death certificate data from NVSS and population estimates from the U.S. Census Bureau were used to calculate homicide rates by sex, race, and age using the Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (WONDER).5,23 RRs with 95% CIs were calculated to compare homicide rates by race.
Data from the National Crime Victimization Survey (NCVS) from 2010 to 2015 for non-Hispanic blacks (n=469) and non-His-panic whites (n=2,163) aged 12–34 years were used to calculate pooled rates of aggravated assault (i.e., attack or attempted attack with a weapon, regardless of whether an injury occurred, and an attack without a weapon when serious injury results) and simple assault (i.e., not causing a serious injury).24 NCVS is a self-report survey administered to individuals aged ≥12 years from a nationally representative sample of U.S. households. Sample data are weighted to be representative of people aged ≥12 years. Established procedures were used to calculate 95% CIs for each estimate.24
Data from the Youth Risk Behavior Surveillance System (YRBSS) for 2015 were used to calculate the prevalence of being physically injured in a fight, bullying on school property in the past year, and students’ reports of missing school in the past month because they felt too unsafe to go among 15,624 high schoolers. The YRBSS includes a nationally representative sample of U.S. high school students (grades nine to 12). Weighted prevalence estimates, 95% CIs, and pairwise comparisons of black and white students were generated using the Youth Online analysis tool.25
Data from NVSS, NCVS, and YRBSS were used to show RRs of black and white experiences of violence over time. RRs of homicide, aggravated assault, and missing school because of safety concerns were calculated for years 1995–2015.
Data from the Adverse Childhood Experiences (ACE) module of the Behavioral Risk Factor Surveillance System (BRFSS) 2011–2012 were analyzed to examine the average number of ACEs experienced and associations with health conditions. BRFSS is an annual, cross-sectional telephone survey of non-institution-alized adults aged ≥18 years.26–28 The ACE module consists of 11 items assessing exposure to eight adversities including child abuse (physical, emotional, and sexual) and household challenges (parental divorce/separation, domestic violence, substance abuse by a household member, a household member incarcerated, or living with a household member who attempted suicide, was depressed, or mentally ill) experienced prior to age 18 years. Analyses were conducted in R, version 3.3.2. Logistic regression models were used to test associations between ACEs and physical and mental health conditions, including having coronary heart disease, fair or poor physical health, frequent mental distress (i.e., experiencing >14 mentally unhealthy days during the past 30 days), heavy drinking (i.e., more than one or two drinks on average daily for females and males, respectively), and current smoking. Each model adjusted for age, sex, income, and education.
RESULTS
Analyses included participants aged 18—34 years from 14 states that administered this optional module (n=10,589). Analysis of NVSS data showed homicide was the leading cause of death for black males aged 10—34 years (n=5,396 deaths, 41.2% of all deaths in this age group). Homicide was the second leading cause of death for black females (n=579 deaths, 11.7% of all deaths). By contrast, among white males (n=1,213 deaths, 3.5% of all deaths) and females (n=544, 3.5% of all deaths), homicide was the fifth leading cause of death for those aged 10—34 years (data not shown in tables). The homicide rate for blacks was 12.9 times higher than the homicide rate for whites (Table 1). Differences in homicide rates were greatest when comparing black and white males; the RRs for those aged 10—17 and 18—34 years were 17.9 and 17.7, respectively.
Table 1.
Violence Exposure for Non-Hispanic Blacks and Non-Hispanic Whites by Sex
| Male |
Female |
Total (male and female) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable | Black (95% Cl) | White (95% Cl) | Black to white RR | Black (95% Cl) | White (95% Cl) | Black to white RR | Black (95% Cl) | White (95% Cl) | Black to white RR |
| Homicide rate per 100,000 | |||||||||
| Ages 10–34 yearsa | 67.7 (65.9, 69.5) | 3.9 (3.7, 4.1) | 17.4* | 7.3 (6.7, 7.8) | 1.8 (1.7, 2.0) | 4.0* | 37.5 (36.5, 38.4) | 2.9 (2.7, 3.0) | 12.9* |
| Ages 10–17 yearsa | 16.1 (14.5,17.6) | 0.90(0.7,1.1) | 17.9* | 2.4 (1.8, 3.1) | 0.6 (0.5, 0.8) | 3.7* | 9.3 (8.5,10.2) | 0.8 (0.6, 0.9) | 11.6* |
| Ages 18–34 yearsa | 91.7 (89.2, 94.3) | 5.2 (4.9, 5.5) | 17.7* | 9.4 (8.6,10.3) | 2.3 (2.1, 2.5) | 4.1* | 50.3 (48.9, 51.6) | 3.8 (3.6, 4.0) | 13.2* |
| % Injured in a physical fightb | 5.8 (4.1, 8.0) | 2.8 (2.0, 3.8) | 2.1* | 3.4 (2.1, 5.6) | 0.9 (0.6,1.6) | 3.8* | 4.7 (3.5, 6.3) | 1.9 (1.4, 2.6) | 2.5* |
| Aggravated assault rate per 1,000, ages 12–34 yearsc |
6.8 (5.1, 8.5) | 6.3 (5.3, 7.2) | 1.1 | 7.6 (5.9, 9.4) | 3.8 (3.1, 4.5) | 2.0* | 7.2 (5.9, 8.6) | 5.1 (4.4, 5.7) | 1.4* |
| Simple assault rate per 1,000, ages 12–34 yearsc |
20.3 (16.2, 24.4) | 26.7 (23.7, 29.7) | 0.8* | 22.0 (17.9, 26.2) | 21.4(18.8, 24.1) | 1 | 21.2 (18.0, 24.5) | 24.1 (21.8, 26.4) | 0.9 |
| % Missed school due to safety concernsd | 6.9 (5.0, 9.4) | 2.9 (2.0, 4.1) | 2.4* | 6.4 (4.7, 8.5) | 5.4 (4.1, 7.1) | 1.2 | 6.8 (5.4, 8.5) | 4.2 (3.2, 5.4) | 1.6* |
| % Bullied on school propertye | 11.2 (8.4,14.9) | 18.1 (16.3, 20.0) | 0.6* | 15.1 (11.9,18.9) | 29.1 (26.5, 31.8) | 0.52* | 13.2 (10.7,16.3) | 23.5 (21.7,25.3) | 0.5* |
Note: Boldface indicates statistical significance
(p<0.05).
Data source: National Vital Statistics System, year 2015.
Data source: YRBSyear 2015, Percentage of high school students injured in a physical fight one or more times in the past 12 months. Injuries had to be treated by a doctor or nurse.
Data source: Bureau of Justice Statistics, National Crime Victimization Survey, 2010–2015, special tabulation.
Data source: YRBS, year 2015, Percentage of high school students missing school at least once in the past 30 days because they felt unsafe at school or on the way to or from school.
Data source: YRBS, year 2015, Percentage of high school students bullied on school property during the past 12 months.
RR, rate ratio; YRBS, Youth Behavior Surveillance System.
Data from NCVS indicated rates of aggravated assault were significantly higher for blacks aged 12—34 years (7.2 per 1,000 people) compared with whites (5.1 per 1,000, black to white RR=1.4). When examined by sex, rates of aggravated assault were significantly higher for black females (7.6 per 1,000 people) compared with white females (3.8 per 1,000 people, RR=2.0); however, there were no significant differences in aggravated assault for black males (6.8 per 1,000 people) compared with white males (6.3 per 1,000 people). No significant differences emerged in overall rates of simple assault for blacks and whites (Table 1).
YRBSS data showed involvement in a physical fight resulting in injury was significantly more common among black than white high school students (RR=2.5; Table 1). The prevalence of missing school because of safety concerns was also significantly higher in blacks as compared with whites, overall (RR=1.6), and in males (RR=2.4), but not in females. The prevalence of having been bullied on school property was significantly lower among blacks (RR=0.5).
Data from NVSS, NCVS, and YRBSS show that disparities in violence between blacks and whites have persisted over the past two decades (Figure 1). Although rates of aggravated assault and missing school because of safety concerns have become more similar for blacks and whites over the past 10 years, rates of homicide for blacks remain higher and the disparity in 2015 was the highest it has been since 2006.
Figure 1. Black to white rate ratios of violence experiences by year, 1995—2015.
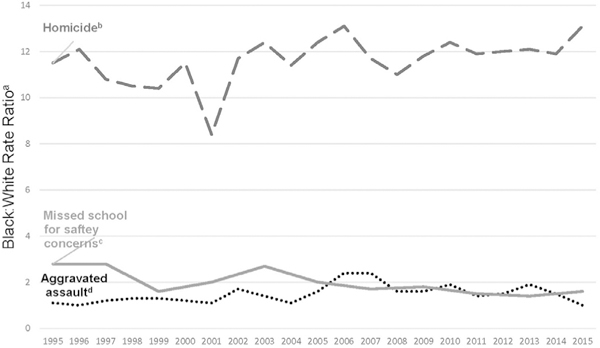
a Comparison between the annual rates of violence between non-Hispanic blacks and non-Hispanic whites. For example, in 1995, blacks aged 10—34 years experienced homicide rates almost 12 times greater than whites aged 10—34 years. b Data source: National Vital Statistics System, non-Hispanic black and non-Hispanic whites aged 10—34, years 1995—2015. Comparison of rates of homicide per 100,000. c Data Source: Youth Risk Behavior Surveillance System, 1995—2015 (biennial data), percentage of non-Hispanic black and non-Hispanic white high school students missing school at least once in the past 30 days because they felt unsafe at school or on the way to or from school. d Data source: Bureau of Justice Statistics, National Crime Victimization Survey, 1995—2015, special tabulation. Comparison of rates (per 1,000) of aggravated assault for non-Hispanic blacks and non-Hispanic whites aged 12—34 years.
Data from BRFSS showed blacks (mean 2.16, 95% CI=1.97, 2.35) reported significantly higher levels of ACE exposure compared with whites (mean 1.82, 95% CI=1.76, 1.88; Table 2). The number of ACEs experienced was positively associated with self-rated fair to poor health, frequent mental distress, heavy drinking, and smoking for blacks and whites. ACEs were significantly associated with increased odds of reporting coronary heart disease among blacks (AOR=1.45, 95% CI=1.02, 2.08), but not whites (AOR=1.03, 95% CI=0.83, 1.28).
Table 2.
Relationships Between ACE Score and Health Conditions, 2011—2012
| Variable | Black, non-Hispanic | White, non-Hispanic |
|---|---|---|
| ACE score,a mean (95% CI) | 2.16 (1.97, 2.35) | 1.82 (1.76, 1.88) |
| Coronary heart disease, AOR (95% CI)b | 1.45 (1.02, 2.08) | 1.03 (0.83, 1.28) |
| Fair/poor health, AOR (95% CI)b | 1.16 (1.02, 1.33) | 1.23 (1.16, 1.30) |
| Frequent mental distress, AOR (95% CI)b | 1.38 (1.19, 1.60) | 1.29 (1.24, 1.36) |
| Heavy drinking, AOR (95% CI)b | 1.29 (1.08, 1.54) | 1.08 (1.03,1.13) |
| Smokingstatus, AOR (95% CI)b | 1.22 (1.09, 1.36) | 1.23 (1.19, 1.28) |
Note: Stratified by race/ethnicity among adult respondents aged 18—34 years. AOR indicates, for example, for each ACE reported, the model predicts a 45% increase in the odds of reporting coronary heart disease among blacks.
Mean number of ACEs reported.
All models statistically adjusted forage, sex, household income, and educational attainment. ACE score ranges from 0 to 8.
ACE, adverse childhood experiences.
DISCUSSION
These results indicate that young blacks, compared with young whites, continue to be at disproportionately high risk for several forms of violence, and this disparate risk has persisted over the past two decades. Moreover, this gap between violence experiences of young blacks and whites is widest for outcomes with the greatest immediate risks to physical health, including homicide, physical fights with injuries, and aggravated assault. In contrast to forms of violence with more severe proximate risks to physical health, estimates for simple assault and bullying victimization were either not significantly higher for blacks as compared with whites or were higher for whites. Homicide rates have consistently been at least ten times higher for blacks aged 10—34 years compared with whites in the same age group between 1995 and 2015. The only exception to this pattern occurred in 2001 when the gap between black and white homicides narrowed to approximately eight homicides experienced by blacks for every one homicide experienced by whites. This change was likely a result of increased homicide deaths among whites for this year due to the 9/11 terrorist attacks.
These results indicate that disparities in childhood violence exposure are associated with health conditions in adulthood for which blacks also face disproportionately high risk.2,16 Specifically, a significant link between ACEs and coronary heart disease emerged for blacks, but not for whites. This finding is especially concerning because respondents in this part of the analyses were very young (18—34 years). Future research should examine disproportionate exposure to ACEs and violence experienced by blacks relative to whites, as these exposures may contribute to disparities not only in death and injury but also in mental health and chronic disease observed across the lifespan.2,4 This analysis is cross-sectional and descriptive in nature and cannot establish causality. However, previous literature has shown evidence for causal relationships between ACEs and later health outcomes.16 Further longitudinal and retrospective studies would clarify associations between experiences of violence and physical and mental health outcomes.
Although not a focus of the current study, additional research is needed to examine disparities in forms of violence that have received substantial attention in recent years, such as police use of force,29 as well as forms of violence experienced across the lifespan such as child and elder abuse. It is also important to acknowledge the substantial heterogeneity among blacks in the U.S. (e.g., income, ethnicity). Examining variation in violence disparities within subgroups of those identifying as black is another important topic for future research.
Results of the current study are consistent with prior research showing black youth shoulder a disproportionate burden of many types of violence experiences.30 A new aspect of these results is that the disproportionate impact of violence on young blacks seems to be confined to forms of violence having the greatest immediate negative consequences on physical health, such as homicide and aggravated assault. Considering racial disparities in violence, it is important to emphasize that race/ethnicity is not a risk factor for violence; rather, violence is associated with socioeconomic risk factors that are disproportionately clustered among some racial and ethnic groups.6 Therefore, it is important for prevention efforts to consider societal conditions disproportionately experienced by blacks, including concentrated poverty, residential segregation, and other forms of racism that limit opportunities to grow up in healthy, violence-free environments. Addressing these conditions is critical to limiting violence exposure.10 An important question is whether socioeconomic factors have similar impacts on forms of violence with the most immediate negative consequences versus those forms with less immediate impact.
The body of research on racial and ethnic disparities in violence points to a number of violence and disparity reduction strategies. The field of violence prevention has generated a substantial body of information to help communities reduce violence through application of the best available evidence for prevention.31 Drawing on this literature, the authors suggest five key strategies whose combined effectiveness should be rigorously evaluated in racial and ethnic minority communities.
It is important to create economic, physical, and social conditions that protect against violence and promote life opportunities for black youth. For example, lower family income is associated with a range of negative health consequences, including violence.32 Approaches to strengthen household financial security include tax credits for families with children, safe and affordable housing, paid parental leave, livable wages, and economic support for developmentally appropriate childcare.32 These types of approaches are likely to be beneficial to racial and ethnic groups disproportionately impacted by concentrated poverty and other forms of economic disadvantage.
Another strategy to reduce opportunities for violence and increase positive social interaction includes enhancing physical characteristics of communities. For example, Business Improvement Districts, which entail business owners providing funds to supplement public services to enhance security and beautification of exterior areas, have been linked to reductions in various forms of violence, including violence likely to result in serious injury.33 Community strategies for creating and improving green spaces (e.g., planting trees and community gardens, remediating vacant lots) have also been linked to reductions in violence.34,35 Furthermore, street outreach programs, which train staff to mediate conflicts and promote social norms that protect against violence, may reduce violence and youths’ acceptability of violence when implemented well.36 These findings support previous research showing that increased collective efficacy (e.g., neighborhood contexts of trust and solidarity that facilitate residents’ willingness to intervene to prevent violence) is inversely related to community violence,37 and suggest that community approaches can benefit youth living in urban neighborhoods.
Inverse relationships between violence and prosocial involvement underscore the importance of providing safe, stable, and nurturing relationships for youth as a means to reduce violence. Connecting youth to caring adults through mentoring and after-school programs reduces violence by promoting prosocial behavior, helping youth to develop healthy life goals, and providing supervision.21 A cost—benefit analysis in the state of Washington showed that connecting youth to caring adults through school-based mentoring yielded between $15 and $24 in return for every $1 of cost.28,36 A well-developed body of research shows nurturing and supportive relationships between caregivers and children significantly lowers risk of violence.21,32 Parenting skill and family relationship programs promote caregivers’ knowledge about age-appropriate child development, strategies for enhancing communication and behavioral monitoring, and management in childhood and adolescence.21,32
In the current study, rates of physical fighting in school and missing school because of safety concerns were higher for black students compared with white students. In a study examining links between prosocial school engagement and reductions in violence, approximately 36% of black middle and high school students reported involvement in physical fights; however, participants were less likely to be involved in violence if they were involved in prosocial activities.38 In a randomized trial of prevention programs for black youth, participation in a culturally sensitive social and emotional skill building program was linked to significant reductions in violent behavior for boys.39 School-based programs that strengthen youth’s skills (e.g., communication and conflict resolution) have shown reductions in violence across age groups and regardless of the SES and race/ethnicity of the students served.21,40
An additional focus area for violence reduction is intervening to lessen the harms of exposure to violence. In instances when violence has occurred, and symptoms such as behavior problems, post-traumatic stress, and anxiety are present, symptoms can be treated successfully with evidence-based treatment programs.21,32 Therapeutic interventions are linked to decreases in victimization and perpetration of violent crime.21 Evidenced-based interventions include individual and family therapies,41 and hospital-based brief interventions42 designed to manage trauma-related stress, build adaptive coping, and enhance problem-solving skills. It is important for these types of services to be made readily available, accessible, and affordable in minority communities.
Limitations
There are several challenges with data used to document racial disparities in violence. Self-report data were used in several of the data systems analyzed for this study, and are vulnerable to misreporting of experiences with violence. There was also variation in the timeliness of available data. NVSS and YRBSS data are available for 2015. NCVS data, while available for 2015, required data to be pooled across 2010—2015 to produce reliable estimates. The ACEs module from BRFSS was generated using data from 2011 to 2012. Given the significance of this public health problem, efforts to improve the availability of timely data are needed.
CONCLUSIONS
The data presented show violence experienced by young blacks in the U.S. is a public health problem with farreaching effects. Preventing violence exposure is strategic for addressing disparities in a range of health problems in this population. For young blacks, disparities in violence exposure can mean immediate and long-term decreased health-related quality of life. For society, these disparities translate into higher healthcare costs, loss of vibrant and productive communities, and social inequity.1,43 Continuing to identify barriers to health and well-being and ways to increase life opportunities may help to reduce violence exposure for youth and young adults most at risk. Preventing exposure to violence is inextricably woven into overall health. To reduce health disparities experienced by black communities, identifying and reducing disparities in violence is essential.
ACKNOWLEDGMENTS
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention or the Bureau of Justice Statistics.
We would like to acknowledge Barbara Oudekerk for verifying the National Crime Victims Survey data.
No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.HHS. HHS action plan to reduce racial and ethnic health disparities: a nation free of disparities in health and health care. www.minority-health.hhs.gov/assets/pdf/hhs/HHS_Plan_complete.pdf. Published 2011. Accessed May 10,2018.
- 2.Cunningham TJ, Croft JB, Liu Y, Lu H, Eke PI, Giles WH. Vital signs: racial disparities in age-specific mortality among blacks or African Americans—United States, 1999—2015. MMWR Morb Mortal Wkly Rep. 2017;66(17)444–456. 10.15585/mmwr.mm6617e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Peterson RD, Krivo LJ, Hagan J. The Many Colors of Crime: Inequalities of Race, Ethnicity, and Crime in America. New York, NY: NYU Press, 2006. [Google Scholar]
- 4.Pathak E Mortality among black men in the USA. J Racial Ethn Health Disparities. 2018;5(1):50–61. 10.1007/s40615-017-0341-5. [DOI] [PubMed] [Google Scholar]
- 5.CDC. Web-based Injury Statistics Query and Reporting System (WIS-QARS). Atlanta, GA: HHS; 2017. www.cdc.gov/injury/wisqars/index.html. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sampson RJ, Morenoff JD, Raudenbush S. Social anatomy of racial and ethnic disparities in violence. Am J Public Health. 2005;95(2):224–232. 10.2105/AJPH.2004.037705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilson WJ. The Truly Disadvantaged: The Inner City, the Underclass, and Public Policy. Chicago, IL: University of Chicago Press; 2012. 10.7208/chicago/9780226924656.001.0001. [DOI] [Google Scholar]
- 8.Sumner SA, Mercy JA, Dahlberg LL, Hillis SD, Klevens J, Houry D. Violence in the United States: status, challenges, and opportunities. JAMA. 2015;314(5):478–488. 10.1001/jama.2015.8371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McCall PL, Land KC, Parker KF. An empirical assessment of what we know about structural covariates of homicide rates: a return to a classic 20 years later. Homicide Stud. 2010;14(3):219–243. 10.1177/1088767910371166. [DOI] [Google Scholar]
- 10.Bell C Violence: Contagion, Group Marginalization, and Resilience or Protective Factors: A Workshop of the Institute of Medicine. Washington, DC: National Academy of Science, 2012. [Google Scholar]
- 11.Lansford JE, Miller-Johnson S, Berlin LJ, Dodge KA, Bates JE, Pettit GS. Early physical abuse and later violent delinquency: a prospective longitudinal study. Child Maltreat. 2007;12(3):233–245. 10.1177/1077559507301841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Widom CS, Wilson HW. How victims become offenders In: Bottoms BL, Najdowski CJ, Goodman GS, eds. Children as Victims, Witnesses, and Offenders: Psychological Science and the Law. New York, NY: Guilford Press; 2009:255–274. [Google Scholar]
- 13.Moffitt TE. Childhood exposure to violence and lifelong health: clinical intervention science and stress-biology research join forces. Dev Psychopathol. 2013;25(4 pt 2):1619–1634. 10.1017/S0954579413000801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gilbert LK, Breiding MJ, Merrick MT, et al. Childhood adversity and adult chronic disease: an update from ten states and the District of Columbia, 2010. Am J Prev Med. 2015;48(3):345–349. 10.1016/j.amepre.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 15.Fagan AA, Novak A. Adverse childhood experiences and adolescent delinquency in a high-risk sample: a comparison of white and black youth. Youth Violence Juv Justice. In press. Online October 15, 2017. 10.1177/1541204017735568. [DOI] [Google Scholar]
- 16.Norman RE, Byambaa M, De R, Butchart A, Scott J, Vos T. The longterm health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med. 2012;9 (11):e1001349 10.1371/journal.pmed.1001349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Theall KP, Shirtcliff EA, Dismukes AR, Wallace M, Drury SS. Association between neighborhood violence and biological stress in children. JAMA Pediatr. 2017;171(1):53–60. 10.1001/jamapediatrics.2016.2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Oliver W The public health and social consequences of black male violence. J Afr Am Men. 2000;5(2):71–92. 10.1007/s12111-000-1008-5. [DOI] [Google Scholar]
- 19.Mercy JA, Butchart A, Farrington D, Cerda M. Youth Violence. Geneva, Switzerland: WHO, 2002. [Google Scholar]
- 20.Corso PS, Mercy JA, Simon TR, Finkelstein EA, Miller TR. Medical costs and productivity losses due to interpersonal and self-directed violence in the United States. Am J Prev Med. 2007;32(6):474–482. 10.1016/j.amepre.2007.02.010. [DOI] [PubMed] [Google Scholar]
- 21.David-Ferdon C, Vivolo-Kantor AM, Dahlberg LL, Marshall KJ, Rainford N, Hall JE. A Comprehensive Technical Package for the Prevention of Youth Violence and Associated Risk Behaviors. Atlanta, GA: National Center for Injury Prevention and Control, CDC; 2016. 10.15620/cdc.43085. [DOI] [Google Scholar]
- 22.Lee BA, Firebaugh G, Iceland J, et al. Neighborhood income composition by household race and income, 1990—2009. Ann Am Acad Pol Soc Sci. 2015;660(1):78–97. 10.1177/0002716215576104. [DOI] [Google Scholar]
- 23.CDC, National Center for Health Statistics. Underlying cause of death 1999–2015 on CDC WONDER Online Database, released 2016, Data are from the multiple cause of death files, 2015. https://wonder.cdc.gov/. Accessed May 10, 2018.
- 24.Truman JL, Morgan RE. Criminal Victimization, 2015. Washington, DC: Bureau of Justice Statistics, 2016. [Google Scholar]
- 25.CDC. Youth risk behavior surveillance system—United States, 2013. MMWR Morb Mortal Wkly Rep. 2014;63(4):1–168. www.cdc.gov/mmwr/pdf/ss/ss6304.pdf.24402465 [Google Scholar]
- 26.CDC. Behavioral Risk Factor Surveillance System, 2011. Atlanta, GA: CDC. [Google Scholar]
- 27.CDC. Behavioral Risk Factor Surveillance System, 2012. Atlanta, GA: CDC. [Google Scholar]
- 28.Ford DC, Merrick MT, Parks SE, et al. Examination of the factorial structure of adverse childhood experiences and recommendations for three subscale scores. Psychol Violence. 2014;4(4):432 10.1037/a0037723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeGue S, Fowler KA, Calkins C. Deaths due to use of lethal force by law enforcement: findings from the National Violent Death Reporting System, 17 U.S. states, 2009—2012. Am J Prev Med. 2016;51(5):S173–S187. 10.1016/j.amepre.2016.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Antunes MJL, Ahlin EM. Youth exposure to violence in the community: towards a theoretical framework for explaining risk and protective factors. Aggress Violent Behav. 2017;34:166–177. 10.1016/j.avb.2017.01.015. [DOI] [Google Scholar]
- 31.CDC. Technical packages for violence prevention: using evidence-based strategies in youth violence prevention efforts. www.cdc.gov/violenceprevention/pub/technical-packages.html. Accessed April 12, 2018.
- 32.Fortson B, Klevens J, Merrick MT, Gilbert LK, Alexander SP. Preventing Child Abuse and Neglect: A Technical Package for Policy, Norm, and Programmatic Activities. Atlanta, GA: National Center for Injury Prevention and Control, CDC, 2016. [Google Scholar]
- 33.MacDonald J, Golinelli D, Stokes RJ, Bluthenthal R. The effect of business improvement districts on the incidence of violent crimes. Inj Prev. 2010;16(5):327–332. 10.1136/ip.2009.024943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Branas CC, Kondo MC, Murphy SM, South EC, Polsky D, MacDonald JM. Urban blight remediation as a cost-beneficial solution to firearm violence. Am J Public Health. 2016;106(12):2158–2164. 10.2105/AJPH.2016.303434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bogar S, Beyer KM. Green space, violence, and crime: a systematic review. Trauma Violence Abus. 2016;17(2):160–171. 10.1177/1524838015576412. [DOI] [PubMed] [Google Scholar]
- 36.Milam AJ, Buggs SA, Furr-Holden CDM, Leaf PJ, Bradshaw CP, Webster D. Changes in attitudes toward guns and shootings following implementation of the Baltimore Safe Streets intervention. J Urban Health. 2016;93(4):609–626. 10.1007/s11524-016-0060-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sampson RJ, Raudenbush SW, Earls F. Neighborhoods and violent crime: a multilevel study of collective efficacy. Science. 1997;277 (5328):918–924. 10.1126/science.277.5328.918. [DOI] [PubMed] [Google Scholar]
- 38.McDade RS, King KA, Vidourek RA, Merianos AL. Impact of prosocial behavioral involvement on school violence perpetration among African American middle school and high school students. J Immigr Minor Health. 2018;20(1):7–13. 10.1007/s10903-016-0544-6. [DOI] [PubMed] [Google Scholar]
- 39.Flay BR, Graumlich S, Segawa E, Burns JL, Holliday MY. Effects of 2 prevention programs on high-risk behaviors among African American youth: a randomized trial. Arch Pediatr Adolesc Med. 2004;158 (4):377–384. 10.1001/archpedi.158.4.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hahn R, Fuqua-Whitley D, Wethington H, et al. Effectiveness of universal school-based programs to prevent violent and aggressive behavior: a systematic review. Am J Prev Med. 2007;33(2):S114–S129. 10.1016/j.amepre.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 41.Cary CE, McMillen JC. The data behind the dissemination: a systematic review of trauma-focused cognitive behavioral therapy for use with children and youth. Child Youth Serv Rev. 2012;34(4):748–757. https://doi.org/10.1016Aj.childyouth.2012.01.003. [Google Scholar]
- 42.Fein JA, Mollen CJ, Greene MB. The assault-injured youth and the emergency medical system: what can we do. Clin Pediatr Emerg Med. 2013;14(1):47–55. https://doi.org/10.1016Aj.cpem.2013.01.004. [Google Scholar]
- 43.National Research Council and Institute of Medicine. Panel on Understanding Cross-National Health Differences Among High-Income Countries, Woolf SH, Laudan A, eds. Committee on Population, Division of Behavioral and Social Sciences and Education, and Board on Population Health and Public Health Practice, Institute of Medicine. U.S. Health in International Perspective: Shorter Lives, Poorer Health. Washington, DC: The National Academies Press, 2013. [PubMed] [Google Scholar]


