Abstract
OBJECTIVES:
Shared care plans play an essential role in coordinating care across health care providers and settings for children with medical complexity (CMC). However, existing care plans often lack shared ownership, are out-of-date, and lack universal accessibility. In this study, we aimed to establish requirements for shared care plans to meet the information needs of caregivers and providers and to mitigate current information barriers when caring for CMC.
METHODS:
We followed a user-centered design methodology and conducted in-depth semistructured interviews with caregivers and providers of CMC who receive care at a tertiary care children’s hospital. We applied inductive, thematic analysis to identify salient themes. Analysis occurred concurrently with data collection; therefore, the interview guide was iteratively revised as new questions and themes emerged.
RESULTS:
Interviews were conducted with 17 caregivers and 22 providers. On the basis of participant perspectives, we identified 4 requirements for shared care plans that would help meet information needs and mitigate current information barriers when caring for CMC. These requirements included the following: (1) supporting the accessibility of care plans from multiple locations (eg, cloud-based) and from multiple devices, with alert and search features; (2) ensuring the organization is tailored to the specific user; (3) including collaborative functionality such as real-time, multiuser content management and secure messaging; and (4) storing care plans on a secure platform with caregiver-controlled permission settings.
CONCLUSIONS:
Although further studies are needed to understand the optimal design and implementation strategies, shared care plans that meet these specified requirements could mitigate perceived information barriers and improve care for CMC.
Care coordination is a critical function of high-quality health systems to meet the health service and information needs of patients and families.1–3 This function is particularly important for children with medical complexity (CMC), who on average receive care from 13 outpatient health care providers representing 6 distinct subspecialties.4 A central component of care coordination is a multidisciplinary shared care plan.5–7 A care plan is a single, comprehensive tool containing the child’s pertinent medical history, medication list, appointments, goals of care, and action items that is developed in partnership with families and providers.8 These care plans have the potential to strengthen family-provider relationships, enhance communication, and improve child health outcomes.8 Furthermore, as components of multifaceted interventions, care plans have been associated with high-quality care experiences and improved patient-reported outcomes in pediatric and adult populations.9
Care plans are typically in paper format and are created by using standardized templates, taking the form of loose sheets of paper, notebooks, binders, or documents scanned into the electronic medical record.8,10–12 Researchers in qualitative studies explored the use of care plans by CMC families, and providers highlighted several limitations in their design and implementation that impede routine use.10,11,13 These limitations include a lack of shared ownership, difficulty modifying them in real time, and a lack of universal accessibility from various devices. Cloud-based care plans (ie, care plans that are stored online and are available to users on demand via the Internet) may provide an efficient platform to support their adaptability and accessibility in real time.14–18 However, little is known in terms of how families and providers perceive information sharing in the cloud and how they would define a cloud-based platform. Furthermore, there is a paucity of evidence that demonstrates how families and providers would initiate, review, update, and share these care plans across settings to facilitate care coordination.17–21
To provide such evidence, we used user-centered design as an innovative approach, both to understand the optimal design and implementation strategies for shared care plans and to ensure that they are consistent with the needs, constraints, and previous experiences of relevant stakeholders.19,22–26 Through a user-centered design process, stakeholders are actively engaged in iterative cycles of developing new technologies by doing the following: (1) identifying their needs and establishing requirements for the technology, (2) developing designs, (3) building interactive versions of the designs, and (4) evaluating designs.27 In this study, we aimed to conduct the first step of the user-centered design process by understanding the needs of caregivers (parents or legal guardians) and health care providers who care for CMC and to establish requirements for shared care plans that would mitigate current barriers to meeting these information needs.
METHODS
Study Design and Population
Consistent with user-centered design methodology, we used pragmatic inquiry to meet the study objectives. Pragmatic inquiry involves eliciting perspectives of diverse stakeholders on the basis of real-world experiences to guide future interventions and action.28 Such an approach is commonly used as the first step in the user-centered design process to identify the needs and requirements of relevant stakeholders.
We recruited English-speaking caregivers and providers of CMC 0 to 18 years of age who were hospitalized at a tertiary care children’s hospital between March 2016 and November 2016. We identified CMC using a flag in the child’s medical record that is based on predefined criteria developed by the institution. Trained research staff approached eligible caregivers during the child’s hospitalization using a standardized recruitment protocol. We recruited providers (eg, emergency department [ED] providers, primary care providers [PCPs]) caring for CMC enrolled in the study using a standard e-mail template. We intentionally did not interview individuals with expertise in clinical informatics or information security at this stage because our aim in this study was to foster an open palate of ideas to meet caregiver and provider needs, rather than understand the feasibility of these ideas within current health information systems.
We used purposive sampling, a qualitative strategy to recruit eligible participants on the basis of their demographic characteristics to maximize participant diversity and the range of perspectives. As data analysis progressed, we also used theoretical sampling to recruit different types of providers (eg, subspecialists, nursing staff) as new questions or areas of exploration emerged from the study findings.29 We recruited and enrolled caregivers and providers until the research team deemed that a diverse array of perspectives was obtained, and well-defined themes emerged from the analysis.
Data Collection
In-depth, semistructured interviews led by 1 of 3 research team members (A.D.D., E.A.J-F., and J.W.) were conducted either in the child’s hospital room, child’s home, a private hospital meeting room, provider’s office, or by telephone for participants who were not local at the time of the interview. Interviews lasted ~1 hour, were audio recorded, and transcribed. We used open-ended questions and probes to elicit caregiver and provider experiences with current health information processes and their perspectives on existing care plans and cloud-based care plans (Supplemental Information). Participants were also asked to draw designs of their recommendations for these care plans. We revised interview guides weekly as new themes and areas of inquiry emerged from the data analysis. Participants completed a demographic survey after the interview and were provided a $100 gift card.
All study procedures were approved by the Seattle Children’s Hospital Institutional Review Board.
Data Analysis
We used applied thematic analysis, a process that is used to identify the main ideas from participant responses, combine similar ideas into themes, and organize these themes into actionable strategies that may be useful for solving practical problems.30 To identify main ideas from interview transcripts, 3 authors (A.D.D., E.A.J-F., and J.W.) first read each transcript in its entirety to gain insights into broad concepts. Next, at least 1 of these authors reread each transcript, highlighted excerpts, and applied codes to each idea in the excerpt. Each transcript was then reviewed by at least 1 of the other authors, and additional codes were applied to each excerpt if needed. During weekly meetings throughout the data collection period, these 3 authors initially reviewed codes, resolved coding questions, and developed a codebook. As interviews, analysis, and codebook development progressed, weekly meetings were focused on combining codes into themes and organizing themes into categories. Data analysis was facilitated by using Dedoose version 7.0.23 qualitative software.31
RESULTS
Demographics
The study sample consisted of 17 caregivers and 22 providers. In Table 1, we outline demographic characteristics of the participants. Demographic characteristics of children are presented in Supplemental Table 5.
TABLE 1.
Caregiver and Provider Demographics
| Caregivers | Providers | |
|---|---|---|
| Age, y, No. (%)a | ||
| ≤35 | 7 (41) | 7 (32) |
| 36–45 | 6 (35) | 7 (32) |
| >45 | 4 (24) | 8 (36) |
| Female sex, No. (%)a | 16 (94) | 17 (77) |
| Race and/or ethnicity, No. (%)a | ||
| White | 14 (82) | — |
| Hispanic | 2 (12) | — |
| Caregiver education, No. (%)a | ||
| High school graduate or GED | 3 (18) | — |
| Some college or 2-y degree | 6 (35) | — |
| 4-y college degree | 4 (24) | — |
| >4 y college | 4 (24) | — |
| Type of provider, No. (%)a | ||
| Complex care provider | — | 2 (9) |
| PCP | — | 6 (27) |
| ED physician | — | 4 (18) |
| Inpatient pediatric resident | — | 1 (5) |
| Subspecialty physician | — | 3 (14) |
| ED nurse | — | 1 (5) |
| Inpatient floor nurse | — | 1 (5) |
| School nurse | — | 1 (5) |
| Home health nurse | — | 1 (5) |
| Care coordinator | — | 1 (5) |
| Case manager | — | 1 (5) |
| Clinic location of provider, No. (%)a | ||
| Main hospital | — | 13 (59) |
| Regional | — | 8 (36) |
| Out of state | — | 1 (5) |
| Provider y of practice, No. (%)a | ||
| 0–5 | — | 7 (32) |
| 6–10 | — | 5 (23) |
| 11–20 | — | 4 (18) |
| >20 | — | 6 (27) |
| Mean provider comfort level caring for CMC (range)b | — | 8.0 (3–10) |
| Provider uses EHR at main practice location,No. (%)a | — | 19 (86) |
| Provider has access to main hospital EHR, No. (%)a | — | 18 (82) |
| Provider comfort level using EHR, mean (range)b | — | 8.9 (6–10) |
| Participant owns a smartphone, No. (%)a | 16 (94) | 22 (100) |
| Participant comfort level with smartphone app usage, mean (range)b | 8.5 (2–10) | 8.3 (2–10) |
| Caregiver endorsed having a care plan for the child, No. (%)a | 8 (47) | — |
GED, general equivalency diploma. —, not applicable.
Sum may not equal 100% due to rounding or participant preferred not to answer survey item.
Response options were on a scale from 1 to 10, with higher ranking indicating a higher comfort level.
Overview of Study Findings
We organized the themes we identified into 3 main categories: (1) information needs when caring for CMC, (2) barriers to meeting these information needs in the current system, and (3) requirements for care plans to meet the information needs of all stakeholders and to mitigate barriers. Regarding information needs, caregivers and providers noted that information should be centralized, timely, consistent, and helpful when caring for CMC (Table 2). Participants also highlighted several barriers that currently exist to meeting these needs (Table 2). On the basis of these perceived needs and barriers, we identified 4 requirements for care plans that could help to meet needs and mitigate barriers: accessible, user-centered, collaborative, and secure. Each requirement is presented in more detail below, with illustrative quotes used to highlight similarities and differences in perceptions between caregivers and providers in Table 3.
TABLE 2.
Caregiver and Provider Information Needs and Barriers When Caring for CMC
| Information Needs | Description of Need | Perceived Barriers to Meeting Information Needs |
|---|---|---|
| Centralized | Information should be stored in a single, centralized location | Information stored in EHRs that are not accessible in all care settings Paper copies are not always available or “get lost in the shuffle” Information needs to be retrieved from multiple sources or locations Information that lives “outside the system” is difficult to retrieve and makes it difficult to know what events are occurring between health encounters “in the system” Time-consuming for 1 provider to generate and maintain a single, comprehensive, up-to-date care plan Burden of keeping information often falls on caregivers (“on-call historian”), which results in them having to share information repeatedly or worry about forgetting important information Limited tools to help families organize vast quantities of health information |
| Timely | Information should be available before health care encounters and easily retrievable | Information may not be available before the patient’s arrival Slow transfer of information between care settings (eg, fax) Time-consuming to “dig through charts” to find relevant information Critical information for emergency situations is difficult to find |
| Consistent | Information should be consistent across care team members and care settings to “get everyone on the same page” | Information is documented in multiple places leading to discrepancies Multiple existing versions of the care plan leading to inaccuracies Inadequate documentation of rationale for provider recommendations or changes to the plan of care |
| Helpful | Information should help familiarize care team members with the child and provide management guidance because CMC “do not follow the textbook” | Current care plans use “1-size-fits-all” and may have too much information or have missing information, depending on the care team member Content may not be organized in a manner that is helpful for guiding specific health care encounters (ED visit versus follow-up visit) Information is often not accessible by unfamiliar providers (lives in child’s primary EHR only) |
TABLE 3.
Illustrative Quotes From Caregivers and Providers Regarding Requirements for a Shared Care Plan
| Requirement | Caregivers | Providers |
|---|---|---|
| Accessible | ||
| Accessible where they need it | “I’ve got my laptop, my tablet, [and] my phone, depending on where I’m at. Especially if I’m at the doctor or if they can’t access [the care plan] for some reason, which they should be able to, then I can from the phone. Then I wouldn’t have to have everything memorized.” (Caregiver 13) | “While it needs to connect to our EHR, it also needs to be accessible for other caregivers. Outside hospitals also need to be able to access it because they will see a lot of our kids from Alaska or Montana. They’ll present to an outside emergency room and then get transferred to our hospital. We don’t want to delay their care and things that they could start working on just because they don’t have access to the care plan.” (Complex care provider, provider 11) |
| Accessible when they need it | “Having a Web-based option where it’s not only readily available but it doesn’t require the family to mention it to the provider so that they know it’s there. It would be great if there were some sort of alert or flag that could come up on a child’s record when he’s admitted to an emergency room. Whether it’s our local one or here. It says, ‘Alert, child has care plan. Click here.’ They don’t have to wait until the parent goes, ‘Oh yeah, by the way we have a care plan.’ Or stumble across it on encounter 63 of 2000.” (Caregiver 7) | “If I could have [access] when she was coming in, gone on the cloud and had a password, and read that discharge summary, I think I would have been more prepared when I saw her, to know what was going on with her” (PCP, provider 2) |
| Find information quickly within the care plan | “It would be nice to have things searchable. That’s another reason I started the blog [with his information], because I thought it would be easier to search for things if I need to try to remember something.” (Caregiver 2) | “Do I need to wade through to page 37 to find the seizure action plan? If I can type in something, enter, bam, it comes up right away, that would be useful. It would be very easy to come up with, ‘How do I take care of this thing right now?’” (Subspecialist, provider 12) |
| User-centered | ||
| “I don’t feel like anyone is going to take the time to read a 6-page document, so to serve both purposes [for ED providers versus inpatient providers], there would be a way to have a triage version up front for acute crisis or first meetings. Basically, if you have 5 min or if you have an hour” (Caregiver 4) | “It really depends [on] who it is for It would be important to have care plans for specific purposes…for the family, for the emergency room. The needs of the care plan really vary based on the audience.” (Care coordinator, provider 20) | |
| Collaborative | ||
| Team leader | “I would have to say 1 of his rehab doctors [should be the team leader] because that’s where he spent the most time. That was the most recent experience. They had their hands on him. I wouldn’t say his PCP because of my remote situation. In this instance, I would rather his rehab doctors to manage this piece of things. It would have to be a collaboration, of course.” (Caregiver 9) | “I like the idea of the [complex care team] because they’re a nice synthesizer of all these different problems and specialties. They have the 10 000-ft view of everything, whereas maybe the gastrointestinal specialists and the sleep doctor, maybe they don’t see the whole picture as well. The [complex care team] knows everything that’s going on with him, so I feel confident that they have the most up-to-date information, because they are in contact with this family so much.” (Inpatient pediatric resident, provider 1) |
| Contributors | “[My role is] to check and make sure that everything’s correct. [And] when I need to add something, to make sure that’s correct as well and up-to-date. I think it needs to be checked, I would say at least once a month or depending on your child’s health. If you’re having some problems, then check it as often as you can and make sure that it’s okay” (Caregiver 16) | “Maybe with cloud based, if the pulmonologist is changing the plan and we made it easy enough to change within the cloud-based system, they could go in and update it, and they wouldn’t have to update every section. They could just update their particular problem, which would mainly allow [the care plans] to be more up-to-date.” (Complex care provider, provider 11) |
| HIT system | “The [doctor] updates what medication he’s on, what dosage he’s on, and they change something so that goes into the system, and it goes to part of the hospital that updates the care plan. They get an alert, and then updates have to be made within a certain time frame.” (Caregiver 5) | “I’d like to not have to have a whole lot of awareness of [the care plans] because what I’m doing as part of my clinical routine care and my discussion with parents is automatically populating into it. That is the most ideal basis. On a more realistic basis, I would say I’d like to be able to enter in the information I need to and have it alert the people who it potentially touches every time I’ve made an update. Likewise, if somebody else makes an update that touches something to do with seizures, it pings me to let me know” (Subspecialist, provider 12) |
| Messaging system | “It would be good for the [home dietician] and [hospital dietician] to be able to communicate that back and forth about the best feeding plan. That would probably be easier, too, because I know that different providers don’t talk with certain in-home people. There’s a communication barrier there. It would be easy to see the changes that a doctor made and why, so that everybody can see what’s been changed, why, [and] what the plan is, so that they have an understanding, too.” (Caregiver 11) | “The way I envision it is that the communication is all in 1 place so other team members could see the communications that they wanted to, or you could include other team members in the communications. That way you’re not reinventing the wheel by trying to communicate different ways with different people or cc’ing people in e-mails.” (PCP, provider 5) |
| Secure | ||
| Balance between access versus security | “Who’s going to be accessing it, when, and for what purpose? Is there some piece that is public domain? And if I know that information, I can find this person quickly, and the rest of it is password protected.” (Caregiver 1) |
“Obviously it needs to be HIPAA compliant and password protected, but it can’t be 10 clicks away. You can’t have to go to a new Web site that you have to update your login every 2 months.” (ED provider, provider 10) |
| Control over permission settings | “I would probably like it to be similar to how Facebook does their privacy, where you can say, ‘I want everybody at [hospital 1] to be able to access this.’ Or ‘I only want [child’s] direct care providers to access this.’ Or ‘I only want [child’s] immediate medical team for this admission to access this.’ Then give the families those options.” (Caregiver 7) | “The ideal piece of EHRs is that parents can go in and say school nurse A can look at my kid’s record, but school teacher B cannot…it’s about [the patient]. They should control who has access.” (School nurse, provider 17) |
Requirement 1: Accessible
Caregiver number 6 said: “If there’s a way to tie it all in with the computer system, where a parent could say, ‘He’s got a care plan. He’s got a special pre-op protocol that needs to be followed.’ They could go, ‘Look. You’ve got a red flag here.’ Quick. Boom. It pops up”
A key requirement for care plans is ensuring quick accessibility wherever and whenever users (ie, caregivers or providers) need it. For where they need it, participants were open to accessing a care plan in the cloud because this would provide a single version of the care plan that was available in a centralized location regardless of where the child was receiving care (ie, a “universal porta” They suggested that a cloud-based care plan should be affiliated with a hospital system (as opposed to a personal cloud-based health record) to enhance trustworthiness of information within the care plan. Hospital providers (inpatient or ED) strongly recommended that any care plan should be linked through the hospital electronic health record (EHR) to find information in a timely manner; however, the document does not need to “live” within the EHR. Participants also request that care plans be electronically accessible on multiple devices (eg, computer, smartphone). This would mitigate barriers of paper copies “getting lost in the shuffle.” For example, caregivers could share the care plan through an app on their smartphone to avoid the frustration of repetitively sharing their child’s health history. In addition, caregivers noted that care plans must have download and print capabilities in case an Internet connection was unavailable or for users without smartphones.
For when they need it, providers recommended that care plans be available before any health care encounter, so they would have time to familiarize themselves with the child’s unique care needs to efficiently guide the encounter. This feature would alleviate the burden on caregivers to be the “on-call historian.” Participants suggested that electronic alert features could help meet this goal. For example, outpatient follow-up providers could receive an alert when a discharge summary is available to prepare for the follow-up visit. Participants also noted users should have customizable alert settings to avoid “alert fatigue.”
Participants emphasized that information they would like to share or find “in the moment” must be easily retrievable within the care plan. This requirement would alleviate the burden on caregivers to remember all of their child’s health information and prevent providers from having to “dig through” multiple folders or documents. Participants requested a robust search function to help meet this goal. This would give users the “10 000 ft view” (eg, problem list) and allow them to quickly find details regarding a particular event, action plan, or medication change without having to open multiple programs, tabs, screens, or notes.
Requirement 2: User-centered
In the very front, executive summary, boom. That’s right here, and all this other stuff is behind the scenes. If somebody needs that, which they do, it’s just not me, they can have all that stuff. But what I need, when its emergent, is right here in front of me…the three things I got to worry about…this kid is different from a normal kid because of this, this, and this. –ED provider 3
Participants noted that care plans should contain content relevant to their particular role, and the content should be organized in a manner that addresses the user’s specific needs. This requirement would enable users to quickly retrieve the information they need to efficiently care for the child. The formatting adaptability of an electronic care plan would meet this requirement, in which the interface would differ on the basis of the user’s role, although the back-end data infrastructure would remain the same. In Fig 1, we present 2 examples of content a caregiver and provider would prefer to have in a care plan and how they would organize it. The content in Fig 1 was representative of the main areas discussed by the majority of participants. Participants also discussed how they would prioritize different types of content given time constraints and how they would use layers via hyperlinks or tabs to access lower priority content.
FIGURE 1.
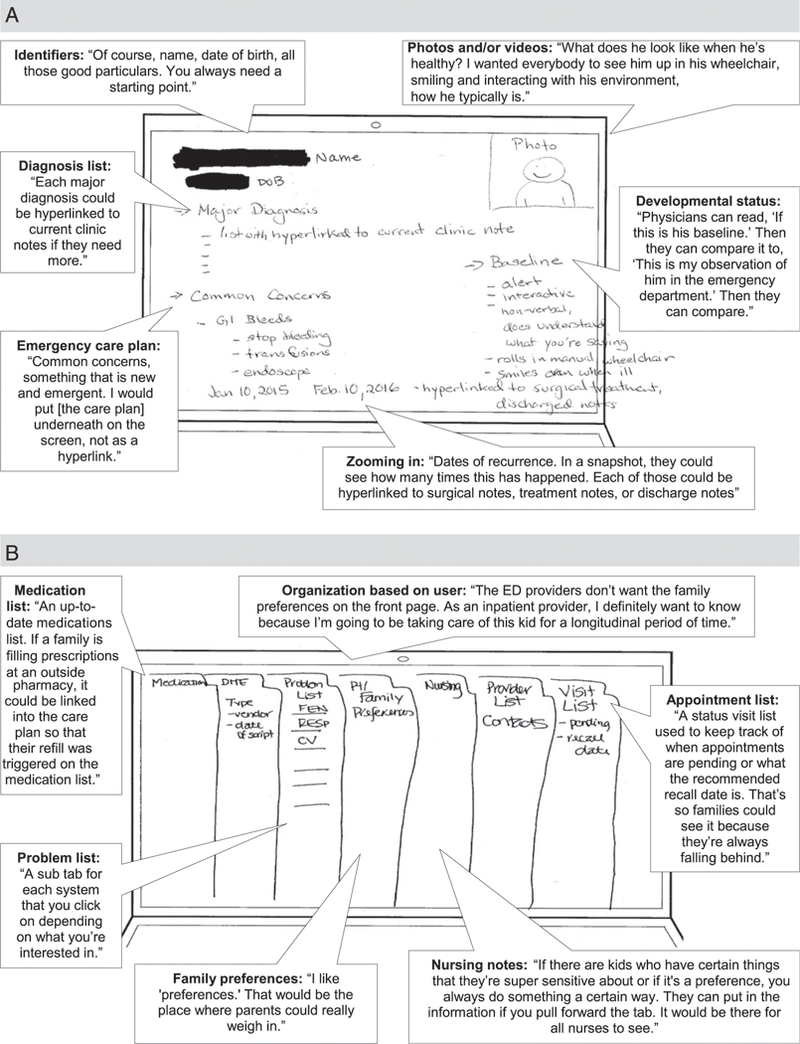
Cloud-based shared care plan design examples. A, Caregiver 7. B, Complex care provider 19. CV, cardiovascular; DOB, date of birth; Feb, February; FEN, fluids, electrolytes, and nutrition; Jan, January; RESP, respiratory.
Requirement 3: Collaborative
If there was truly a shared, live, active care plan, and all of the docs involved in his care could contribute to a running care plan, that would be amazing. But it needs to be easy for everyone to use because it takes time to do this kind of updating, time to document what conversations happened and have it be accurate so that it’s useful. –Primary care provider 6
We identified collaboration among care team members as a key requirement to generate and maintain information within a care plan. Collaboration was perceived to promote trustworthiness of the care plan because multiple care team members could provide content related to their area of expertise and review the content for accuracy. Participants emphasized that care plans stored in the cloud would make a collaborative model feasible because multiple care team members could share the responsibility of routinely updating the care plan in real time. Role clarity among care team members and effective communication were identified as 2 key features of a collaborative model for care plans.
To meet the need of having consistent information across care team members and settings, we identified 3 key roles: a team leader, contributors, and the health information technology (HIT) system (Table 4). For “team leader,” respondents expressed different opinions about which care team member(s) should fulfill this role. However, there was a general consensus that the team leader(s) should have expertise in complex care, understand the 10 000 ft view, and have frequent interactions with the child. The team leader(s) should be clearly identified at all times, and selecting the team leader should be a shared decision between caregivers and providers based on the individual or team that best meets these characteristics. For the role of contributors, caregivers and providers were unified in their perspective of which care team members should fulfill this role because these would be individuals who “own” specific aspects of the child’s care (eg, subspecialists, care coordinators, caregivers, etc). Participants also highlighted that the HIT system serves an important role in maintaining an updated and accurate care plan through seamless data transfer functionality (eg, auto-population) and user reminders to review or update information.
TABLE 4.
Key Roles and Responsibilities of a Collaborative Model for a Cloud-Based Shared Care Plan
| Key Roles | Characteristics of Individuals and/or System to Fulfill Role | Responsibilities |
|---|---|---|
| Team leader | A single individual or team Medical expertise caring for CMC (knowledgeable about the range of child’s medical conditions) Has a 10 000-ft view of the child (understands how 1 change may impact child as a whole) Sees the child most often |
Review all sections of the care plan and clarify conflicting, redundant, or confusing content with section “owner” on a routine basis Find contributors to fill gaps in the care plan Maintain an active problem list |
| Contributors | Has the most current information about a particular section of the care plan (eg, tracheostomy settings, care coordination, family history) Includes caregivers and other family members | Review and update sections of the care plan that pertain to their area of expertise after all encounters with child Caregivers should review the care plan to ensure it is feasible to implement and reflects actual care Caregivers should update child’s family social, or developmental history on a routine basis |
| HIT system | Cloud-based platform to enable multiuser updates in real time Robust HIPAA-compliant data infrastructure Copy and paste functionality to transfer editable content from provider notes Capability to set permissions at the user level (eg, edit content, view only, share, download) |
Autopopulate relevant content from the EHR to various sections of the care plan Auto-sign off when changes are made with person, date and time stamp Trigger users to update the care plan at specified intervals Grant access to sections of the care plan depending on user’s permission level |
A collaborative model for care plans also requires seamless communication between care team members. Therefore, participants recommended that any care plan should contain a secure messaging system to enable care team members to ask questions, clarify the rationale behind decisions, or resolve conflicting information within the care plan. This could serve as a “mini virtual care conference” in real time, which caregivers highlighted would help team members “get on the same page” about their child’s evolving care plan. This would also decrease the burden on caregivers to constantly relay information between providers and allow interprovider conversations to occur at convenient times. For example, PCPs could receive a message from the inpatient team about a discharged patient, rather than a receiving a call in between scheduled patient visits. However, some participants noted that a messaging system should not replace discussions for urgent matters or for complex issues that need to occur by telephone. Finally, a conversation log would provide a historical record if similar questions or clarifications surfaced in the future.
Requirement 4: Secure
They obviously want security, but ultimately what they want is good care for their child, and if one had to be sacrificed, I think they would sacrifice security versus the care and care coordination. –Subspecialist, provider 14
The last requirement we identified for care plans was storing them on a secure electronic platform with strict permission controls. Participants discussed the balance between maximizing security and ease of access, with most respondents preferring easier access to information rather than a time-intensive login process. Some trusted that any platform developed by the health care system would have sufficient security (eg, Health Insurance Portability and Accountability Act [HIPAA] compliance), assuming the development of electronic care plans would follow similar security protocols as current EHRs. Participants prioritized emergency care information accessibility over security because this information should be readily available to emergency providers (eg, first responders, school nurses, ED providers). Finally, participants felt having a tracking system of when and where users are accessing care plans would be important to enhance accountability.
Participants felt that caregivers should control permission settings in terms of who can view and modify the care plan. Access could be granted to teams or institutions in which all providers within that team and/or institution would have access to the care plan. However, this should include an exception feature if caregivers want to exclude specific providers. Caregivers also noted that permission controls should be specific to different sections of the care plan based on the user’s relationship with the child. Additionally, different permission settings could be set for the user’s ability to edit, comment, view, download, or share information.
DISCUSSION
In this study, we describe how electronic care plans that are stored in the cloud may meet the information needs of caregivers and providers who care for CMC and mitigate perceived information barriers that exist in our current health information systems. Using a user-centered design approach, we identified 4 care plan requirements (accessible, user-centered, collaborative, and secure) that can be met with a cloud-based solution. We synthesized caregiver and provider recommendations into concrete actionable design features and implementation strategies that may be tested in future phases of the user-centered design process.
With the findings in this study, we introduce the idea of a cloud-based solution to mitigate barriers relating to lack of universal accessibility and information inconsistency across multiple users and settings. These barriers have been noted in studies in which researchers have examined the information needs of CMC, which suggest that a centralized, electronic care plan may be beneficial.10,11,13,32 Given that most people are now connected to the Internet via mobile phones, cloud-based care plans would enable users to access, share, and update care plans instantaneously as needed.33 In a few studies, researchers have explored the idea of Web-based care plans for specific pediatric populations and within specific care settings.18,19,21 We add to this existing body of work by explicitly detailing requirements for cloud-based care plans, such as having access via mobile devices, personal computers, and through links in the EHR. Given functional limitations of existing EHRs, cloud-based care plans may need to live outside of the EHR. It is suggested in our findings that health care providers would be willing to access an external platform if the benefits of accessing it (eg, content in a user-tailored format, efficient sharing of information across care team members) outweigh the time required to access it (ie, simplified login process). We also add to the existing body of work by identifying key roles for maintenance of a collaborative care plan.
With this study, we generated ideas regarding how cloud-based, electronic care plans would ideally be designed and implemented on the basis of the information needs of caregivers and providers. However, we recognize that many constraints and challenges will need to be overcome when translating their ideas into practice, which can be explored through future phases of the user-centered design process. For example, usability testing will help to identify whether team leaders are willing to take on the responsibility of overseeing the care plan and which sections of the care plan contributors are realistically willing to update. Involvement of a clinical informaticist in the design process will help to clarify which information can be auto-populated from other sources, and security experts can help to guide the optimal balance between accessibility and privacy. User-centered design methods allow for iterative cycles of development and testing. Within these cycles, stakeholder needs, requirements, and constraints are continually revisited; designs are revised on the basis of usability testing; and implementation strategies are modified until these care plans are proven to be effective tools for coordinating care and improving patient-and family-centered outcomes.
This study has some limitations. First, we interviewed only 1 individual within many of the provider categories, thus limiting our ability to develop an in-depth understanding of particular needs and requirements of different provider groups. However, such a strategy satisfied our goal to explore common themes across a diverse set of providers. In future phases of the user-centered design process, it will be beneficial to gain in-depth insights from individual provider groups and ensure all stakeholders involved in caring for CMC are well represented (eg, surgical subspecialists). Second, the caregivers we interviewed were all English speaking, predominantly white, and reported high comfort levels with technology. Future studies should explore the perspectives of caregivers with diverse racial and/or ethnic backgrounds, limited English proficiency, and low self-reported technology capabilities to understand their unique information needs and requirements for care plans. Third, we did not explore the perspectives of patients with medical complexity directly; therefore, researchers in future studies should explore these patients’ roles with respect to accessing and updating content in their care plans. Finally, we did not conduct observations of how information is currently shared or retrieved and how care plans are currently used. Observations will be essential in future phases of the user-centered design process to discover additional needs and requirements for shared care plans, given existing work-arounds that caregivers and providers use.
CONCLUSIONS
Cloud-based, electronic care plans have the potential to mitigate many of the barriers that exist in our current health information systems. These care plans should be accessible wherever and whenever the information is needed, user-centered in terms of content and formatting, collaborative, and secure with strict permission controls. Future research is needed to test various design and implementation strategies to meet these stated requirements among diverse groups of stakeholders in real-world settings. Care plans that meet these requirements have the potential to promote efficiency, enhance communication, facilitate coordinated care, and improve health outcomes for CMC.
Supplementary Material
Acknowledgments
FUNDING: Supported by a Patient-Centered Outcomes Research Mentored Clinical Investigator Award from the Agency of Healthcare Research and Quality under award K08HS024299 (Dr Desai).
Footnotes
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
Dr Desai conceptualized and designed the study, collected data, participated in data analysis, and drafted the initial manuscript;Ms Jacob-Files and Ms Wignall collected data and participated in data analysis; Ms Wang participated in data analysis; Drs Pratt, Mangione-Smith, and Britto participated in the design of the study; and all authors reviewed and revised the manuscript, approved the final manuscript as submitted, and agree to be accountable for all aspects of the work
REFERENCES
- 1.Institute of Medicine. Priority Areas for National Action: Transforming Health Care Quality. Washington, DC: The National Academies Press; 2003. Available at: https://www.nap.edu/read/10593/chapter/1. Accessed October 4, 2017 [PubMed] [Google Scholar]
- 2.National Quality Forum. Priority setting for healthcare performance measurement: addressing performance measure gaps in care coordination. 2014. Available at: www.qualityforum.org/Publications/2014/08/Priority_Setting_for_Healthcare_Performance_Measurement_Addressing_Performance_Measure_Gaps_in_Care_Coordination.aspx. Accessed October 4, 2017
- 3.Bodenheimer T Coordinating care-a perilous journey through the health care system. N Engl J Med. 2008;358(10): 1064–1071 [DOI] [PubMed] [Google Scholar]
- 4.Cohen E, Berry JG, Camacho X, Anderson G, Wodchis W, Guttmann A. Patterns and costs of health care use of children with medical complexity. Pediatrics. 2012; 130(6). Available at: www.pediatrics.org/cgi/content/full/130/6/e1463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Berry JG, Agrawal RK, Cohen E, Kuo DZ. The landscape of medical care for children with medical complexity. 2013. Available at: https://www.childrenshospitals.org/issues-and-advocacy/children-with-medical-omplexity/issue-briefs-and-reports/the-landscape-of-medical-care-for-children-with-medical-complexity. Accessed October 4, 2017
- 6.Antonelli RC, McAllister JW, Popp J. Making care coordination a critical component of the pediatric health system: a multidisciplinary framework. 2009. Available at: mailto:www.lpfch.org/sites/default/files/care_coordination_a_multidisciplinary_framework.pdf. Accessed October 4, 2017
- 7.American Academy of Pediatrics Council on Children With Disabilities. Care coordination in the medical home: integrating health and related systems of care for children with special health care needs. Pediatrics. 2005;116(5): 1238–1244 [DOI] [PubMed] [Google Scholar]
- 8.McAllister JW. Achieving a shared plan of care with children and youth with special health care needs. 2014. Available at: mailto:https://www.lpfch.org/publication/achieving-shared-plan-care-children-and-youth-special-health-care-needs. Accessed October 4, 2017
- 9.Lion KC, Mangione-Smith R, Britto MT. Individualized plans of care to improve outcomes among children and adults with chronic illness: a systematic review. Care Manag J 2014;15(1):11–25 [DOI] [PubMed] [Google Scholar]
- 10.Adams S, Cohen E, Mahant S, Friedman JN, Macculloch R, Nicholas DB. Exploring the usefulness of comprehensive care plans for children with medical complexity (CMC): a qualitative study. BMC Pediatr. 2013;13:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berry JG, Goldmann DA, Mandl KD, et al. Health information management and perceptions of the quality of care for children with tracheotomy: a qualitative study. BMC Health Serv Res. 2011;11:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stewart D, Law M, Burke-Gaffney J, et al. Keeping it together: an information KIT for parents of children and youth with special needs. Child Care Health Dev. 2006;32(4):493–500 [DOI] [PubMed] [Google Scholar]
- 13.Quigley L, Lacombe-Duncan A, Adams S, Hepburn CM, Cohen E. A qualitative analysis of information sharing for children with medical complexity within and across health care organizations. BMC Health Serv Res. 2014;14:283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Council on Clinical Information Technology. Health information technology and the medical home. Pediatrics. 2011;127(5):978–982 [DOI] [PubMed] [Google Scholar]
- 15.Schneider JH, Marcus E, Del Beccaro MA, et al. ; Council on Clinical Information Technology. Policy statement-using personal health records to improve the quality of health care for children. Pediatrics. 2009;124(1):403–409 [DOI] [PubMed] [Google Scholar]
- 16.Klasnja P, Pratt W. Healthcare in the pocket: mapping the space of mobile-phone health interventions. J Biomed Inform. 2012;45(1):184–198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shaw KN, Krug SE, Ackerman AD, et al. ; American Academy of Pediatrics; Committee on Pediatric Emergency Medicine; Council on Clinical Information Technology; American College of Emergency Physicians; Pediatric Emergency Medicine Committee. Policy statement-emergency information forms and emergency preparedness for children with special health care needs. Pediatrics. 2010;125(4):829–837 [DOI] [PubMed] [Google Scholar]
- 18.Pyles LA, Hines C, Patock M, et al. Development of a Web-based database to manage American College of Emergency Physicians/American Academy of Pediatrics Emergency Information Forms. Acad Emerg Med. 2005;12(3):257–261 [DOI] [PubMed] [Google Scholar]
- 19.Bjerkan J, Hedlund M, Helleso R. Patients’ contribution to the development of a Web-based plan for integrated care - a participatory design study. Inform Health Soc Care. 2015; 40(2):167–184 [DOI] [PubMed] [Google Scholar]
- 20.Kim KK, Bell J, Reed S, et al. A novel personal health network for patient-centered chemotherapy care coordination. In: 2014 International Conference on Collaboration Technologies and Systems (CTS); May 19–23, 2014; Minneapolis, MN 449–456 [Google Scholar]
- 21.Rocha RA, Romeo AN, Norlin C. Core features of a parent-controlled pediatric medical home record. Stud Health Technol Inform. 2007;129(pt 2):997–1001 [PubMed] [Google Scholar]
- 22.Muller M, Druin A. Participatory design: The third space in HCI. Handbook of HCI; 2002. Available at: https://www.researchgate.net/publication/228398475_Participatory_Design_The_Third_Space_in_HCI. Accessed April 27, 2018 [Google Scholar]
- 23.Saleem N, Jones DR, Van Tran H, Moses B. Forming design teams to develop healthcare information systems. Hosp Top. 2006;84(1):22–30 [DOI] [PubMed] [Google Scholar]
- 24.Ruland CM, Starren J, Vatne TM. Participatory design with children in the development of a support system for patient-centered care in pediatric oncology. J Biomed Inform. 2008;41(4): 624–635 [DOI] [PubMed] [Google Scholar]
- 25.Pollack AH, Miller A, Mishra SR, Pratt W. PD-atricians: leveraging physicians and participatory design to develop novel clinical information tools. AMIA Annu Symp Proc. 2017;2016:1030–1039 [PMC free article] [PubMed] [Google Scholar]
- 26.Kinzie MB, Cohn WF, Julian MF, Knaus WA. A user-centered model for Web site design: needs assessment, user interface design, and rapid prototyping. J Am Med Inform Assoc. 2002;9(4): 320–330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Preece J, Rogers Y, Sharp H. Interaction Design: Beyond Human-Computer Interaction. Hoboken, NJ: John Wiley & Sons; 2002 [Google Scholar]
- 28.Denzin NK, Lincoln YS. The SAGE Handbook of Qualitative Research. 4th ed. Thousand Oaks, CA: Sage Publications; 2011 [Google Scholar]
- 29.Morse JM. Critical analysis of strategies for determining rigor in qualitative inquiry. Qual Health Res. 2015;25(9): 1212–1222 [DOI] [PubMed] [Google Scholar]
- 30.Guest G Introduction to applied thematic analysis In: Guest G, MacQueen KM, Namey EE, eds. Applied Thematic Analysis. Thousand Oaks, CA: SAGE Publications Ltd; 2012:3–20 [Google Scholar]
- 31.Dedoose [computer program]. Version 7.0.23 Web application for managing, analyzing, and presenting qualitative and mixed method research data. Los Angeles, CA: SocioCultural Research Consultants, LLC; 2014. Available at: www.dedoose.com. Accessed October 4, 2017 [Google Scholar]
- 32.Ranade-Kharkar P, Weir C, Norlin C, et al. Information needs of physicians, care coordinators, and families to support care coordination of children and youth with special health care needs (CYSHCN). J Am Med Inform Assoc. 2017; 24(5):933–941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Patel SN, Kientz JA, Hayes GR, Bhat S, Abowd GD. Farther than you may think: an empirical investigation of the proximity of users to their mobile phones In: Dourish P, Friday A, eds. UbiComp 2006: Ubiquitous Computing. Berlin, Germany: Springer; 2006:123–140 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


