Abstract
The authors present a series of 11 patients. All of them sustained an unstable dorsal fracture-dislocation of the proximal interphalangeal joint (PIPJ). These were managed with open reduction and internal fixation (ORIF) by use of an eight-hole, 1.3-mm oblique-angled strut plate, cut to shape to produce a four-hole plate, acting as a buttress plate. The operations were performed by orthopaedic surgeons with a special interest in hand surgery. Range of motion (ROM) and fixed flexion deformity (FFD) were measured postoperatively. Outcomes were assessed using the Quick Disabilities of the Arm, Shoulder and Hand (Quick-DASH) scoring system. Bony union, articular step-off, degenerative changes, persistent subluxation, or dislocation were confirmed by review of radiographs at latest follow-up. One patient developed a superficial infection and another developed complex regional pain syndrome. However, all patients were pain free at final follow-up. Radiographs at final follow-up confirmed bony union with no step-off, except for one patient who had a 1-mm step-off of the articular surface. Our attractive and novel technique of ORIF allows articular congruity to be restored anatomically with early active mobilization of the affected digit and early return to function.
Keywords: fracture, dislocation, proximal interphalangeal joint, internal fixation, buttress
Introduction
Dorsal fracture-dislocation of the proximal interphalangeal joint (PIPJ) may cause significant stiffness, loss of function, 1 and result in posttraumatic arthritis. 2 These fractures commonly occur when an axial load is applied to the fingertip causing hyperextension. 3
With any intra-articular fracture, the outcome is dependent on the amount of articular surface involved and the maintenance of a congruous joint during fracture healing. These principles apply to dorsal fracture-dislocation of the PIPJ, comparable in management to a partial articular volar Barton's fracture of the distal radius ( Fig. 1 ). The stability of the PIPJ is provided by the articular surface and surrounding soft tissue support. The soft tissue support comprises the collateral ligaments, volar plate, joint capsule, and flexor and extensor tendons.
Fig. 1.

Preoperative radiograph showing an unstable dorsal fracture-dislocation of the proximal interphalangeal joint.
Various techniques have been used to treat dorsal fracture-dislocation of the PIPJ. It is generally accepted that if there is less than 40% involvement of the joint surface, fracture is deemed to be stable and can be treated nonoperatively. If more than 40% of the articular surface is involved, fracture is considered unstable and requires surgical correction. 3 Many treatment methods have been described, including closed reduction and dorsal blocking splint 4 or percutaneous transarticular pinning. 1 Other methods include dynamic traction devices, 5 volar plate arthroplasty, 6 and various open reduction and internal fixation (ORIF) techniques using mini-screws 7 or cerclage wires. 8
There are several issues with fracture-dislocation of the PIPJ. First, the fracture fragments are often small and fixation can be difficult; second, prolonged periods of immobilization often lead to scarring and stiffness of the joint. The senior author advocated the use of a four-hole, 1.3-mm oblique-angled strut plate (Synthes Ltd., Welwyn Garden City, United Kingdom) as a buttress for dorsal fracture-dislocation of the PIPJ. This allowed for early active and passive joint mobilization.
There are several techniques of ORIF described in the literature with varying outcomes. 2 8 9 The authors report a series of 11 patients with unstable dorsal fracture-dislocation of the PIPJ who underwent ORIF using volar buttress plating.
Materials and Methods
This study was designed as a retrospective cohort study, with records of 11 consecutive patients with unstable dorsal fracture-dislocation of the PIPJ reviewed. All these patients were treated with a four-hole, 1.3-mm oblique-angled strut plate. Objective outcomes of active range of motion (ROM) were measured using a goniometer.
The authors measured subjective outcomes to treatment using a Quick Disabilities of the Arm, Shoulder and Hand (Quick-DASH) scoring system. Bony union, articular step-off, degenerative changes, persistent subluxation, or dislocation were confirmed by review of radiographs at latest follow-up.
Surgical Technique
All procedures were performed as a day case. Patients had a general anesthetic or regional block. A combination of both techniques were used in some patients. A zigzag Bruner incision was initially made at the level of the PIPJ ( Fig. 2A ). This approach provided excellent exposure to the volar structures. The skin flap was mobilized exposing the subcutaneous tissue and the flexor sheath ( Fig. 2B ). The digital neurovascular bundles were mobilized away from the flexor sheath structures. After the flexor sheath anatomy had been exposed adequately, the A3 pulley was vented by incising one of its lateral borders and superior and inferior borders. The A3 pulley was retracted and later repaired at the end of the operation.
Fig. 2.
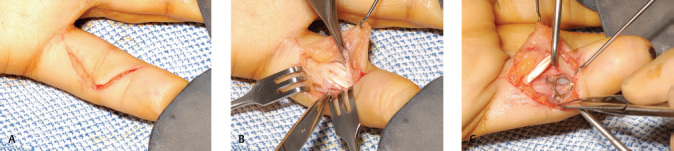
Bruner incision marking (A) , exposure of the flexor tendon sheath (B) , and insertion of a four-hole plate in situ intraoperatively (C) .
The flexor digitorum profundus (FDP) and flexor digitorum superficialis (FDS) tendons were retracted allowing the volar plate and fracture to be visualized. An image intensifier (II) was used to reduce fracture fragments. An eight-hole, 1.3-mm oblique-angled strut plate was cut to shape to produce a four-hole plate ( Fig. 2C ). This was then used to buttress the fracture. Proximal screws were placed initially to secure the fracture fragments. Once the fracture appeared satisfactorily reduced, distal screws were inserted. Care must be taken not to introduce the distal screws into the PIPJ. Intraoperative radiographs were taken with the II to assess for joint congruency and stability of fracture fixation. Postoperatively, patients were seen within 5 days by the hand therapist. For the initial 3 weeks, the affected digit was placed in a dorsal blocking splint of the PIPJ at 30-degree flexion and active ROM of the PIPJ was initiated. Passive ROM was initiated at 6 weeks postoperatively.
Results
There were nine men and two women who sustained dorsal fracture-dislocation of the PIPJ. The mean follow up was 17.3 months (range: 7–32 months), and the average age of patients was 35.6 years (range: 17–63 years). All patients were right handed. Four patients injured their fingers on the dominant hand. All, except for two patients, had their fractures treated within 72 hours of their injury. The two patients were referred from other district general hospitals after initial conservative treatment failed. These two patients had their operation 3 weeks after initial injury. Six of these patients fell on an outstretched hand and sustained this injury. Other causes included alleged assault (two patients), road traffic accident (one patient), during sporting activity—cricket (one patient), and a work-related injury (one patient). Five patients had flexor tenolysis, and their metal work removed once union was achieved to improve ROM. The active arc of motion (AAM) was defined as the range of movement from total active flexion (TAF) of the joint in question—the PIPJ for the purpose of this study—to the fixed flexion deformity (FFD) of that joint ( Fig. 3 ). The mean AAM of the metacarpal phalangeal joint (MCPJ) was 92.9 degrees (range: 50–125 degrees). The mean AAM of the operated PIPJ was 66.2 degrees (range: 20–100 degrees), and the distal interphalangeal joint (DIPJ) was 60.9 degrees (range: 15–95 degrees). The mean total active motion (TAM) was 220 degrees (range: 140–290 degrees). Seven out of 11 patients had an FFD of the PIPJ at their final clinical review. The mean FFD of the PIPJ was 14 degrees (range: 10–30 degrees). Table 1 documents the final ROM achieved in all joints of the affected digit in this patient cohort. Most patients scored very well on the Quick-DASH with an average of 13 (range: 0–36.4). Out of the 11 patients, 1 was operated on by a senior registrar under consultant supervision and 10 were operated on by consultants.
Fig. 3.

Range of motion of PIPJ of left ring finger from flexion (A) to extension at fixed flexion deformity (B, C) at 3 months follow-up following volar buttress plating of PIPJ.
Table 1. Final ROM of individual joints of the affected digit.
| Patient | AAM MCPJ | AAM PIPJ | AAM DIPJ | TAM |
|---|---|---|---|---|
| Abbreviations: AAM, active arc of motion; DIPJ, distal interphalangeal joint; MCPJ, metacarpal phalangeal joint; PIPJ, proximal interphalangeal joint; ROM, range of motion. | ||||
| 1 | 120 | 60 | 35 | 215 |
| 2 | 82 | 88 | 90 | 260 |
| 3 | 50 | 70 | 35 | 155 |
| 4 | 100 | 100 | 90 | 290 |
| 5 | 90 | 65 | 60 | 215 |
| 6 | 95 | 70 | 90 | 255 |
| 7 | 110 | 90 | 50 | 250 |
| 8 | 125 | 20 | 15 | 160 |
| 9 | 95 | 45 | 95 | 235 |
| 10 | 65 | 60 | 15 | 140 |
| 11 | 90 | 60 | 95 | 245 |
One patient developed a superficial infection after undergoing flexor tenolysis and metal-work removal 4 months after initial ORIF. The authors suspect that this complication was due to poor compliance with postoperative rehabilitation and poor wound hygiene. Although his infection improved after the patient was treated with oral antibiotics, his TAM remained poor. One patient developed complex regional pain syndrome. Her TAM remained poor even after she underwent flexor tenolysis and metal-work removal. All patients were pain free at final follow-up. Radiographs at final follow-up confirmed bony union and no step-off, as shown in an example 3-month postoperative radiograph ( Fig. 4 ), except for one patient who had a 1-mm step-off of the articular surface. However, this patient remained asymptomatic and continued to have a good TAM. No radiographic evidence of degenerative changes was seen in this study group. None of this cohort of patients experienced any flexor of extensor tendon rupture or attrition. All patients who were employed before their injury returned to employment when seen at final follow-up.
Fig. 4.

Three-month postoperative radiograph—lateral (A) and anteroposterior (B) —showing fracture union with four-hole plate and screws in situ.
Discussion
Dorsal fracture-dislocation of the PIPJ remains one of the most challenging problems encountered by hand surgeons, with a high incidence toward loss of function. 8 The main aims of treatment of such fracture-dislocations are to determine whether the fracture can be stably reduced with a congruent joint and the congruency maintained during postoperative rehabilitation. Such fractures involving less than 40% of the articular surface are generally stable and can be conservatively managed with a dorsal blocking splint with moderate flexion. 4 6 McElfresh et al reported satisfactory results with this technique with 17 patients regaining 90 degrees of PIPJ motion with a limited follow-up. 4 Unfortunately, most of these fractures are unstable, and conservative measures such as dorsal blocking splint has a limited role.
Newington et al reported satisfactory outcomes, using a Kirschner wire (K-wire) spanning across a reduced and flexed PIPJ for such fracture-dislocations. 1 Some surgeons prefer an alternative technique of K-wire stabilization where the wire is passed dorsally to the flexed PIPJ through the central slip, into the head of the proximal phalanx. 10 These techniques prevent early active mobilization of the affected digit with concerns that the central slip may become scarred and damaged. Pin site infection is also a possible risk.
In patients with unstable fracture-dislocation of the PIPJ, more definitive form of treatment is required. External fixation and traction devices can allow early active motion of the PIPJ, but reduction in fracture fragments can be hampered if there is significant degree of comminution. Suzuki et al used the pins and rubber bands traction system and reported an active ROM of the affected PIPJ as 82.5 degrees. 5 Unfortunately, their case series had only four patients with PIPJ fracture-dislocation, and hence it was difficult to conclude the outcome of this treatment option. 5 The possible complications of this reduction included pin site infection, loss of reduction due to loss of elasticity of rubber bands, and overdistraction of the PIPJ leading to postoperative stiffness. Application and maintenance of this device can also be cumbersome.
Volar plate advancement arthroplasty offers resurfacing of the irregular or deficient volar articular surface, while simultaneously providing volar restrain to maintain reduction. 11 Although this technique may look attractive, in the authors’ experience, the re-dislocation rate is high if more than 40% of the articular surface is involved. The rates of postoperative dislocation varied in studies that used volar plate advancement arthroplasty. Eaton and Malerich reported one dislocation in 24 patients. 6 The current literature suggests that this result is not reproducible.
Hastings and Carroll reported a 31% risk of postoperative subluxation or dislocation. 11 Deitch et al performed a retrospective study on dorsal fracture-dislocation of the PIPJ treated by volar plate arthroplasty or ORIF. 12 This study found that 13% of patients with volar plate arthroplasty developed re-dislocation when compared with 9% of patients who underwent ORIF. 12
Although the technique used in this series to approach the PIPJ from the volar aspect is well documented in the literature, this attractive and novel technique of ORIF allowed articular congruity to be restored anatomically. The four-hole, 1.3-mm oblique-angled strut plate acted as a buttress and prevented any displacement of even comminuted volar fragments. This technique is similar to buttress plating of volar Barton's fracture in the distal radius. Gentle active mobilization can be commenced as soon as the initial postoperative edema settles. Hamilton et al performed ORIF of these fractures using mini-screws and documented a mean AAM of 70 degrees, 7 with functional outcomes similar to this study.
There is very little information in the hand surgery literature regarding long-term patient satisfaction and outcomes following ORIF of dorsal fracture-dislocation of the PIPJ. Though this study is limited by its retrospective design, it emphasizes the importance of restoring anatomical congruity of the PIPJ to achieve good postoperative clinical and radiologic outcomes. In this study, the incidence of metal-work removal and flexor tenolysis was high (5 out of 11 patients—45%). This procedure was necessary to improve the ROM in the affected digit. We conclude the importance of informing patients prior to their initial operation regarding metal-work removal and flexor tenolysis.
The main limitation of this study is the small sample size. Hence, further studies should prospectively compare this technique results with others. Despite all the limitations, the authors believe that this technique yields a good functional outcome. This case series showed comparable objective and subjective outcomes with other techniques reported in the literature.
Footnotes
Conflict of Interest None declared.
References
- 1.Newington D P, Davis T R, Barton N J. The treatment of dorsal fracture-dislocation of the proximal interphalangeal joint by closed reduction and Kirschner wire fixation: a 16-year follow up. J Hand Surg [Br] 2001;26(06):537–540. doi: 10.1054/jhsb.2001.0698. [DOI] [PubMed] [Google Scholar]
- 2.Aladin A, Davis T R. Dorsal fracture-dislocation of the proximal interphalangeal joint: a comparative study of percutaneous Kirschner wire fixation versus open reduction and internal fixation. J Hand Surg [Br] 2005;30(02):120–128. doi: 10.1016/j.jhsb.2004.10.011. [DOI] [PubMed] [Google Scholar]
- 3.Glickel S Z, Barron O A, Eaton R G. 4th ed. New York, NY: Churchill Livingstone; 1999. Dislocations and ligament injuries in the digits; pp. 772–808. [Google Scholar]
- 4.McElfresh E C, Dobyns J H, O'Brien E T. Management of fracture-dislocation of the proximal interphalangeal joints by extension-block splinting. J Bone Joint Surg Am. 1972;54(08):1705–1711. [PubMed] [Google Scholar]
- 5.Suzuki Y, Matsunaga T, Sato S, Yokoi T. The pins and rubbers traction system for treatment of comminuted intraarticular fractures and fracture-dislocations in the hand. J Hand Surg [Br] 1994;19(01):98–107. doi: 10.1016/0266-7681(94)90059-0. [DOI] [PubMed] [Google Scholar]
- 6.Eaton R G, Malerich M M. Volar plate arthroplasty of the proximal interphalangeal joint: a review of ten years’ experience. J Hand Surg Am. 1980;5(03):260–268. doi: 10.1016/s0363-5023(80)80011-6. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton S C, Stern P J, Fassler P R, Kiefhaber T R. Mini-screw fixation for the treatment of proximal interphalangeal joint dorsal fracture-dislocations. J Hand Surg Am. 2006;31(08):1349–1354. doi: 10.1016/j.jhsa.2006.07.011. [DOI] [PubMed] [Google Scholar]
- 8.Weiss A P.Cerclage fixation for fracture dislocation of the proximal interphalangeal joint. Clin Orthop Relat Res 1996;(327):21–28. [DOI] [PubMed]
- 9.Lubahn J D. Dorsal fracture dislocations of the proximal interphalangeal joint. Hand Clin. 1988;4(01):15–24. [PubMed] [Google Scholar]
- 10.Inoue G, Tamura Y. Treatment of fracture-dislocation of the proximal interphalangeal joint using extension-block Kirschner wire. Ann Chir Main Memb Super. 1991;10(06):564–568. doi: 10.1016/s0753-9053(05)80329-1. [DOI] [PubMed] [Google Scholar]
- 11.Hastings H, II, Carroll C., IV Treatment of closed articular fractures of the metacarpophalangeal and proximal interphalangeal joints. Hand Clin. 1988;4(03):503–527. [PubMed] [Google Scholar]
- 12.Deitch M A, Kiefhaber T R, Comisar B R, Stern P J. Dorsal fracture dislocations of the proximal interphalangeal joint: surgical complications and long-term results. J Hand Surg Am. 1999;24(05):914–923. doi: 10.1053/jhsu.1999.0914. [DOI] [PubMed] [Google Scholar]


