Abstract
Background:
Transmasculine individuals have been largely ignored in HIV prevention research, and there is a lack of data regarding this population’s eligibility for and utilization of HIV pre-exposure prophylaxis (PrEP).
Setting:
National online survey conducted in the United States
Methods:
Between May and July 2017, we surveyed 1808 transmasculine individuals (ages 18-60; 30% people of color and/or Latinx), asking questions about sexual behavior and receipt of sexual health care, including PrEP. We examined the number of individuals who would meet eligibility criteria for PrEP, and then used log-linked Poisson regression with robust variance estimation to examine predictors of PrEP eligibility.
Results:
Almost one quarter of the sample (n = 439; 24.3%) met one or more criterion for PrEP eligibility. PrEP eligibility did not differ by age, race/ethnicity, education, or binary gender identity. PrEP eligibility was lower among heterosexual-identified and higher income participants, and was higher among participants who were in open relationships and reported substance use. Among PrEP-eligible individuals, 64.9% had received an HIV test in the past year, 33.9% had received PrEP information from a provider, and 10.9% (n = 48) had received a PrEP prescription. PrEP-eligible individuals who had received a PrEP prescription were more likely to have a binary gender identity, identify as gay, and be taking testosterone.
Conclusion:
A substantial proportion of transmasculine individuals meet PrEP eligibility criteria, but few are receiving adequate PrEP services. Enhanced efforts should be made by providers, programs, and systems to assess HIV-related risk in transmasculine patients and engage them in comprehensive sexual health care.
Keywords: HIV, Pre-exposure prophylaxis, transgender
INTRODUCTION
In recent years, increasing attention has been focused on the specific needs of transgender individuals, both in society at large and in efforts to improve sexual health 1,2. This important shift is reflected in research on HIV prevention. Within HIV research and prevention efforts, there has been a significant focus on understanding structural and systemic dynamics that might increase HIV vulnerability among transgender women1, who bear a disproportionate burden of infection 3.
However, transgender men and transmasculine individuals (i.e., individuals who were assigned female at birth and identify along the transmasculine spectrum) have been largely ignored in HIV and STI research2,3. The failure to include transgender men in past HIV prevention efforts is due, in part, to an assumption that transgender men have sex exclusively or primarily with cisgender women and are therefore not at risk for HIV4,5. Such assumptions fail to acknowledge the diversity of sexual attraction, behavior, and expression among transmasculine individuals. The limited research that has engaged transmasculine populations in conversations about their sexuality and sexual heath finds that many transgender men report attraction and sexual contact with cisgender men 6,7. The Trans PULSE Project conducted in Ontario, Canada in 2009-2010 found that an estimated 63.3% of trans men were gay, bisexual, and/or had sex with men7, and in an online study of HIV risk behavior among transgender people in the United States, 17.1% of transmasculine individuals reported having sex with men in the past 3 months6. Transgender men who had sex with men in this sample were more likely to have sex with multiple partners in the past three months, engage in sex work, or report substance use during sexual activity than those that did not have sex with men6. In a recent study, 33% of transmasculine youth reported male sexual partners, 28.6% reported transgender sexual partners, and approximately 15% reported condomless sex during substance use 8. An analysis of sexually transmitted infection (STI) surveillance data in Los Angeles found an STI positivity rate of 13% among gay and bisexual transgender men and 3% among transgender heterosexual men9.
These emerging data underscore the importance of engaging transmasculine individuals in conversations about their sexual health, as well as in HIV prevention services. Data indicate that a small, but increasing number of transmasculine individuals are HIV-positive. From 2009 to 2014, a review of national HIV surveillance from the Center for Disease Control found that 2351 transgender people were diagnosed with HIV, 361 of whom (15%) were transgender men 10. It is important to note that most of the transgender men who were diagnosed with HIV were Black/African American (211, 58%)10. However, data suggest that transmasculine individuals have inadequate access to HIV prevention services. At present, few interventions have been developed that aim to address the unique HIV prevention needs of transgender men 11. Barriers such as lack of access to sexual health care, health care provider stigma, and insufficient implementation of trans-inclusive policies may contribute to low rates of HIV and STI testing among transgender men1,12. And transmasculine individuals face significant barriers to pre-exposure prophylaxis (PrEP). In one study of PrEP use among transgender youth, only 8.2% of transgender youth recruited through Adolescent Medicine Trials Unit sites reported PrEP use and none of these were transgender men8. In a study of PrEP attitudes and beliefs among transgender men, participants reported challenges in speaking to their providers about sexual health and explained that providers often assumed they were not at risk for HIV.13
As increasing numbers of young people and adults are identifying with genders beyond the traditional gender binary14, patterns of sexual expression and behavior are shifting. It is crucial to reexamine assumptions about sexual behavior in order to ensure that those who need access to HIV prevention services are included in prevention efforts. Research on the sexual behavior and related HIV risk factors of transmasculine individuals may illuminate patterns of behavior and contribute to more comprehensive, equitable HIV prevention practices.
The present study was designed to examine patterns of sexual behavior, specifically behavior that would make an individual eligible for PrEP, among a large-scale national sample of transmasculine individuals. We were interested in the prevalence of PrEP-eligible behaviors in this population, as well as in understanding their access to HIV prevention and PrEP-related care.
METHOD
Recruitment and Study Design
Between May and July 2017, we administered a 45-minute online survey (total of 157 questions) to transmasculine individuals using the Qualtrics web-based survey platform (Qualtrics, Provo, UT). The survey was developed by a transgender-lead, majority transgender-identified research team, and was part of a larger project to understand the range of sexual behaviors, identities, and sexual health needs of transmasculine individuals. The online survey was advertised on social media platforms (i.e., Facebook, Twitter, Tumblr) and via e-mail to transgender community leaders. Snowball sampling on social media and word of mouth were also critical to sample recruitment. During the three-month recruitment period, there were 519 shares by participants on Facebook, 479 retweets on Twitter, and 953 reblogs on Tumblr. The Facebook page for the project had 719 users.
To be eligible to complete the survey, participants had to be at least 18 years of age, assigned female sex at birth, and identify on the transmasculine spectrum. Participants were asked two questions to measure current gender identity; 1) “What sex were you assigned at birth-on your original birth certificate?; and 2) Which BEST describes your current gender identity? (varied response choices, including open-ended text box). Individuals were eligible if they were assigned female at birth and identified as something other than female/woman. Eligible participants had the option to enter raffle to win one of ten $100 Visa gift cards. All study procedures were approved by the Institutional Review Board of [removed for blinding].
Data and Measures
The larger study was focused on identifying barriers and facilitators to sexual health care among transmasculine individuals and development of tools and guidance to assist providers in engaging transmasculine patients in sexual health care. As such, the full survey instrument contained questions about gender identity, gender expression, gender affirmation, health care access and utilization, preferred language for body parts, sexual behavior, HIV testing, alcohol and drug use, community connectedness, and demographic information. The present research focused on items related to demographics, testosterone use as gender affirming health care, HIV testing, sexual behavior, STI history, PrEP use, and substance use.
Participants were asked to report on their sexual behavior in the past six months. In order to accurately capture the variety of sexual behaviors in which they engaged, participants were asked to indicate the genders of their sex partners, the specific types of sex acts that they performed (e.g., oral, anal or vaginal penetration), what was used for any penetrative sex (e.g., penis, fingers, toys), whether they performed these acts as the receptive or insertive partner, and whether any condom or barrier was used. It is important to note that participants were first asked what words or terminology they prefer when asked about their body parts and sex acts in a medical setting. When participants were asked about their sexual behavior, an algorithm was used to present survey questions using participants’ preferred language (e.g., some participants preferred the term “front hole” to “vaginal” sex). Since the majority of participants who reported vaginal penetration preferred the term “vaginal sex” (61%; n =850), we have chosen to use that term in presenting results below. For the present analysis, we created four composite variables to reflect recent sexual behavior that would connote PrEP eligibility based on Centers for Disease Control and Prevention (CDC) PrEP eligibility criteria15 (see Table 1). These behaviors included condomless receptive anal or vaginal sex involving penetration by a penis, with partners that were either cisgender men or transgender women. We also counted the number of cisgender male or transgender female partners reported by the participant in the past six months. In addition, participants were asked whether they had engaged in sex work in the past six months. Finally, to assess past history of STIs, participants were asked whether or not they had been diagnosed with a sexually transmitted infection in the past year.
Table 1.
Univariate and multivariate associations between demographic and behavioral factors and PrEP eligibility and PrEP use among a national sample of transmasculine individuals
| Characteristic | Total (n = 1808) | Eligible for PrEP (n = 439; 24.2%) | Not Eligible for PrEP (n = 1369; 75.7%) | Univariable PR (95% CI) | Multivariable PR (95% CI)b | PrEP Eligible, On PrEP (n = 48) |
|---|---|---|---|---|---|---|
| Demographics | N (%) | N (%) | ||||
| Age | ||||||
| 18-24 | 720 (39.8%) | 159 (22.1%) | 561 (77.9%) | 1 [Reference] | 3 (6.3%) | |
| 25-29 | 493 (27.3%) | 133 (27.0%) | 360 (73.0%) | 1.22 [1.00, 1.49] | 22 (45.8%) | |
| 30-44 | 492 (27.2%) | 130 (26.4%) | 362 (73.6%) | 1.20 [.98, 1.46] | 21 (43.8%) | |
| 45+ | 103 (5.7%) | 17 (16.5%) | 86 (83.5%) | .75 [.47, 1.18] | 2 (4.2%) | |
| Race | ||||||
| Non-Hispanic White | 1278 (70.7%) | 305 (23.9%) | 973 (76.1%) | 1 [Reference] | 36 (75.0%) | |
| African American/Black | 132 (7.3%) | 38 (28.8%) | 94 (71.2%) | 1.21 [.91, 1.61] | 2 (4.2%) | |
| Latinx/Hispanic | 171 (9.5%) | 48 (28.1%) | 123 (71.9%) | 1.18 [.91, 1.52] | 5 (10.4%) | |
| Asian/Pacific Islander | 83 (4.6%) | 16 (19.3%) | 67 (80.7%) | .81 [.52, 1.27] | 2 (4.2%) | |
| Multiracial | 144 (8.0%) | 32 (22.2%) | 112 (77.8%) | .93 [.68, 1.28] | 3 (6.3%) | |
| Income | ||||||
| < $24,999 | 778 (43.0%) | 220 (28.3%) | 558 (71.7%) | 1 [Reference] | 18 (37.5%) | |
| $25,000-$49,999 | 473 (26.2%) | 104 (22.0%) | 369 (78.0%) | .78* [.63, .95] | 0.70*** [0.58, 0.85] | 12 (25.0%) |
| $50,000+ | 557 (30.8%) | 115 (20.6%) | 442 (79.4%) | .73** [.60, .89] | 0.71*** [0.59, 0.85] | 18 (37.5%) |
| Education | ||||||
| High school or less | 277 (15.3%) | 60 (21.7%) | 217 (78.3%) | 1 [Reference] | 1 (2.1%) | |
| Some college/Associate’s degree | 647 (35.8%) | 169 (26.1%) | 478 (73.9%) | 1.21 [.93, 1.56] | 11 (22.9%) | |
| Bachelor’s degree | 515 (28.5%) | 129 (25.0%) | 386 (75.0%) | 1.16 [.88, 1.51] | 22 (45.8%) | |
| Master’s degree or higher | 369 (20.4%) | 81 (22.0%) | 288 (78.0%) | 1.01 [.75, 1.36] | 14 (29.2%) | |
| Gender Identity | ||||||
| Non-binary | 580 (32.1%) | 140 (24.1%) | 440 (75.9%) | 1 [Reference] | 9 (18.8%) | |
| Binary | 1228 (67.9%) | 299 (24.3%) | 929 (75.7%) | 1.01 [.85, 1.20] | 39 (81.3%) | |
| Sexual Orientation | ||||||
| Straight | 171 (9.5%) | 15 (8.8%) | 156 (91.2%) | 1 [Reference] | 0 (0.0%) | |
| Asexual/Demisexual | 142 (7.9%) | 10 (7.0%) | 132 (93.0%) | .93 [.43, 2.00] | .89 [.42, 1.89] | 1 (2.1%) |
| Gay/MSM | 259 (14.3%) | 89 (34.4%) | 170 (65.6%) | 3.97*** [2.48, 6.37] | 2.91*** [1.76, 4.82] | 21 (43.8%) |
| Bisexual | 229 (12.7%) | 60 (26.2%) | 169 (73.8%) | 3.03*** [1.85, 4.95] | 2.72*** [1.63, 4.55] | 5 (10.4%) |
| Queer | 688 (38.1%) | 173 (25.1%) | 515 (74.9%) | 2.91*** [1.84, 4.61] | 2.14**[1.31, 3.49] | 19 (39.6%) |
| Pansexual | 287 (15.9%) | 87 (30.3%) | 200 (69.7%) | 3.50*** [2.18, 5.63] | 2.87*** [1.73, 4.76] | 2 (4.2%) |
| Does not use label | 23 (1.3%) | 4 (17.4%) | 19 (82.6%) | 2.01 [.74, 5.43] | 2.16 [.84, 5.54] | 0 (0.0%) |
| Other label | 9 (0.5%) | 1 (11.1%) | 8 (88.9%) | 1.28 [.19, 8.58] | 1.12 [.23, 5.39] | 0 (0.0%) |
| Relationship Status | ||||||
| Single | 648 (35.8%) | 133 (20.5%) | 515 (79.5%) | 1 [Reference] | 20 (41.7%) | |
| Partnered/Monogamous | 828 (45.8%) | 175 (21.1%) | 653 (78.9%) | 1.03 [.84, 1.26] | 1.11 [.92, 1.34] | 10 (20.8%) |
| Aromantic/Platonic | 66 (3.7%) | 11 (16.7%) | 55 (83.3%) | .81 [.46, 1.42] | 1.34 [.80, 2.24] | 1 (2.1%) |
| Open/Polyamorous | 266 (14.7%) | 120 (45.1%) | 146 (54.9%) | 2.20*** [1.80, 2.69] | 1.69*** [1.39, 2.06] | 17 (35.4%) |
| Region | ||||||
| Northeast | 529 (29.3%) | 128 (24.2%) | 401 (75.8%) | 1 [Reference] | 20 (41.7%) | |
| Midwest | 330 (18.3%) | 79 (23.9%) | 251 (76.1%) | .99 [.78, 1.26] | 6 (20.8%) | |
| South | 458 (25.3%) | 108 (23.6%) | 350 (76.4%) | .98 [.78, 1.22] | 7 (14.6%) | |
| West | 491 (27.2%) | 124 (25.3%) | 367 (74.7%) | 1.04 [.84, 1.29] | 15 (31.3%) | |
| Currently taking Testosterone | ||||||
| No | 596 (33.0%) | 118 (19.8%) | 478 (80.2%) | 1 [Reference] | 3 (6.3%) | |
| Yes | 1212 (67.0%) | 321 (26.5%) | 891 (73.5%) | 1.34** [1.11, 1.61] | 1.05 [0.88, 1.26] | 45 (93.8%) |
| Last HIV Test (n = 1802)a | ||||||
| Within last year | 715 (39.7%) | 285 (39.9%) | 430 (60.1%) | 1 [Reference] | 47 (97.9%) | |
| > 1 year ago | 541 (30.0%) | 91 (16.8%) | 450 (83.2%) | .42*** [.34, .52] | 0.51*** [0.41, 0.62] | 1 (2.1%) |
| Never | 546 (30.3%) | 62 (11.4%) | 484 (88.6%) | .29*** [.22, .37] | 0.35*** [0.27, 0.45] | 0 (0.0%) |
| Substance Usec (n = 1805)a | ||||||
| Alcohol | 1389 (77.0%) | 360 (25.9%) | 1029 (74.1%) | 1.37** [1.10, 1.70] | 1.07 [0.87, 1.32] | 41 (85.4%) |
| Stimulantsd | 84 (4.7%) | 44 (52.3%) | 40 (47.6%) | 2.28*** [1.83, 2.85] | 1.53** [1.19, 1.97] | 4 (8.3%) |
| Poppers | 67 (3.7%) | 44 (65.6%) | 23 (34.3%) | 2.89*** [2.38, 3.51] | 1.79*** [1.45, 2.20] | 18 (37.5%) |
| Prescription Drugse | 201 (11.1%) | 71 (35.3%) | 130 (64.7%) | 1.54*** [1.25, 1.90] | 1.10 [0.89, 1.34] | 8 (16.7%) |
Total n for variables with missing data displayed in characteristics column.
Total n for the multivariate regression is 1799 due to missing data for last HIV test and substance use.
Any use in the past 3 months.
Includes cocaine, crystal meth, and ecstasy.
Refers to recreational use
To assess sexual health care, participants were asked whether they had seen a provider in the past year, the last time they had received an HIV test, whether or not a provider had provided them with information about PrEP, and whether they were currently taking PrEP. Finally, participants were asked if they were currently receiving testosterone injections from a provider.
Sample and Analysis
There were 2,404 individuals who attempted the survey with 2,386 meeting eligibility criteria (8 were assigned male sex at birth, 4 were under 18, and 6 declined to give consent). Sixty participants (2.5%) completed less than 20% of the survey and were excluded from further analysis. Participants were excluded from the current analysis if they lived outside the United States (n = 207), reported being HIV-positive (n = 7), or failed to complete the sexual behavior questions that were the focus of the present study (n = 304), leaving a final analytic sample of 1808.
We began by examining the number of individuals in the sample who would meet eligibility criteria for PrEP, then describing the behaviors that comprise this eligibility, and calculating percentages eligible and ineligible across a variety of demographics and other predictors. We then compared PrEP eligible and ineligible individuals across various predictors using unadjusted prevalence ratios produced by log-linked Poisson regression models with robust variance estimation16(also known as modified Poisson regression)17. Predictors with a univariable p-value of 0.05 or lower were included in a multivariable modified Poisson regression model, estimating adjusted prevalence ratios. Finally, we developed a PrEP access cascade for PrEP eligible transmasculine individuals, designed to reflect their likelihood of receiving HIV testing, PrEP information, and PrEP prescription, as needed.
RESULTS
Demographics of the sample are presented in Table 1. The sample ranged in age from 18 to 69, and came from all over the country, with 29.3% from the Northeast, 18.3% from the Midwest, 25.3% from the South, and 27.2% from the West. Almost 30% of the sample (n = 530) identified as a person of color and/or Latinx. The sample was fairly well distributed in terms of income and education, with 51.1% having less than a bachelor’s degree and 43% reporting making less than $25,000 per year. Almost two thirds of the sample (n = 1228; 67.9%) reported a binary gender identity, and most participants identified as queer (38.1%), pansexual (15.9%), or gay (14.3%). There were 1212 participants (67.0%) who reported currently taking testosterone for gender affirmation.
PrEP Eligibility
Table 2 presents the frequencies of engaging in PrEP-eligible behavior among the 1808 participants in the sample. Almost one quarter of the sample (n = 439, 24.3%) met one or more criterion for PrEP eligibility. There were 330 participants (18.3%) who reported condomless receptive anal or vaginal sex with a cisgender male or transgender female partner in the past six months. Of these, 129 participants (7.1% of the total sample) reported having condomless receptive anal sex, with 107 reporting condomless receptive anal sex with a cisgender male partner and 28 participants reporting condomless receptive anal sex with a transgender woman. There were 290 participants (16.0% of the total sample) who reported having condomless receptive vaginal sex, with 226 participants reporting condomless receptive vaginal sex with a cisgender male partner and 79 reporting condomless receptive vaginal sex with a transgender woman. STI diagnosis in the past year was reported by 5.5% of participants (n = 99) and 3.4% (n = 62) reported engaging in sex work in the past six months. Less than one percent of the sample (n = 5) reported heroin use in the past three months. Finally, 5.7% (n = 103) reported having sex with five or more cisgender male or transgender female sex partners in the past six months.
Table 2.
Frequencies of PrEP Eligibility Criteria.
| N = 1808 | # | % |
|---|---|---|
| Any Condomless receptive anal or vaginal sex a | 330 | 18.3% |
| Condomless receptive anal sexa | 129 | 7.1% |
| Condomless receptive vaginal sexa | 290 | 16.0% |
| STI historyb | 99 | 5.5% |
| Sex worka | 62 | 3.4% |
| Heroin usec | 5 | 0.3% |
| 5 or more cismale/transwomen sexual partnersa | 103 | 5.7% |
| PrEP eligible (i.e., one or more of the above) | 439 | 24.3% |
In the past 6 months, receptive sex involving a natal penis
In past year
In past 3 months
Predictors of PrEP Eligibility
Table 1 compares demographic and behavioral factors among individuals in the sample who met criteria for PrEP eligibility based on their behavior in the past six months (n = 439, 24.2%) and those who did not (n = 1369; 75.7%). PrEP eligibility did not differ by age, race/ethnicity, education, or binary gender identity. Higher income individuals, i.e., those making more than $25,000 per year and those making more than $50,000, had lower prevalence of being eligible for PrEP compared to those making less than $25,000 per year (PR = .78, 95% CI .63-.95 and PR = .73, 95% CI .60-.89, respectively). PrEP eligibility was significantly associated with sexual identity, such that individuals who identified as gay or MSM (PR = 3.97, 95% CI 2.48-6.37), bisexual (PR = 3.03, 95% 1.85-4.95), queer (PR = 2.91, 95% CI 1.84-4.61), or pansexual (PR = 3.50, 95% CI 2.18-5.63) had higher prevalance of PrEP eligibility, compared to those who identified as straight.
There was no difference between individuals in monogamous partnerships and single individuals in their prevalence of PrEP eligibility. Those in open or polyamorous relationships had higher prevalence of PrEP eligibility compared to single individuals (PR = 2.20, 95% CI 1.80-2.69). Prevalence of PrEP eligibility was significantly higher among participants who were taking testosterone (PR = 1.34, 95% CI = 1.11-1.61). Prevalence of PrEP eligibility was significantly lower among those who reported HIV testing less recently. We compared prevalence of PrEP eligibility between participants who reported each type of substance use to those who did not. Prevalence of PrEP eligibility was higher among those who reported each type of substance use, with prevalence being highest among those who reported poppers (PR = 2.89, 95% CI 2.38-3.51).
We conducted a multivariable analysis, including all factors that were significant in univariable modified Poisson regression models. These results are presented in the last column of Table 2. All variables that were significant in univariable testing were retained as independent predictors in the multivariable model, with the exception of being on testosterone and consumption of alcohol or prescription drugs in the past 3 months.
Figure 1 presents a PrEP access cascade for the transmasculine individuals in our sample who met PrEP eligibility criteria (n = 439). Of these PrEP eligible individuals, 82.2% (n = 361) reported that they had seen a health care provider in the past year. Of those who had seen a health care provider, 78.7% (64.9% of all those eligible) had been given an HIV test in the past year. Of those who had received an HIV test, 44.9% (33.9% of all those eligible) reported having received PrEP information from their provider. And of those who received PrEP information, 32.3% received a PrEP prescription. As such, only 10.9% (n = 48) of the PrEP-eligible transmasculine individuals in this sample reported being on PrEP. The demographics of 48 individuals who were PrEP eligible and reported being on PrEP are presented in the last column of Table 1. Compared to all PrEP eligible individuals, individuals who received PrEP were less likely to be between the ages of 18 and 24 (χ2(3) = 21.31, p <.001), and were more likely to have at least a college degree (χ2(3) = 17.01, p < .01), but did not differ significantly by race/ethnicity or income. PrEP-eligible individuals who had received a PrEP prescription were more likely to have a binary gender identity (χ2(1) = 4.28, p < .05, identify as gay (χ2(7) = 24.19, p < .01), and be single (χ2(3) = 8.52, p < .05). Finally, over 93.8% of those who had reported being on PrEP were currently taking testosterone, compared to 67% of the total sample (χ2(1) = 11.67, p < .01). There were an additional 11 individuals in the sample who reported being on PrEP despite not meeting CDC-defined eligibility criteria.
Figure 1.
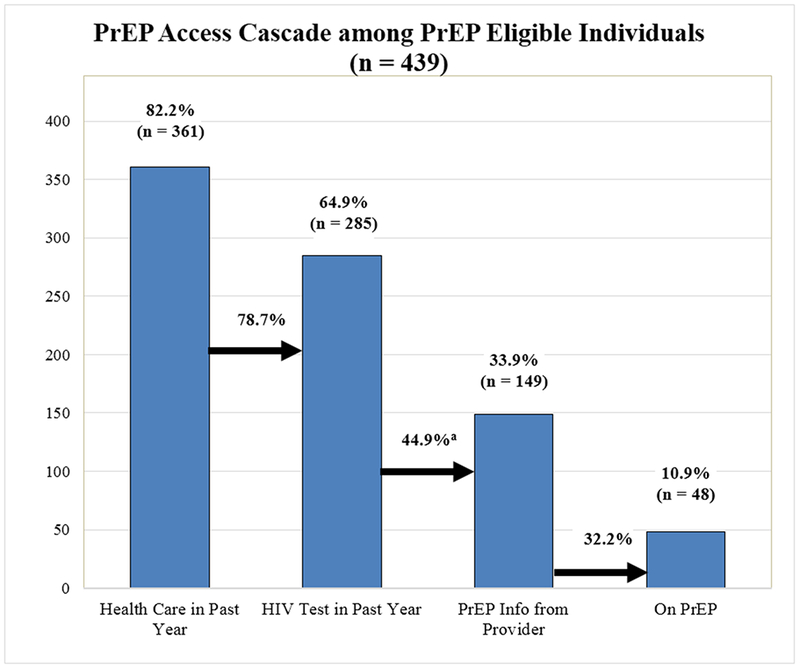
PrEP Access Cascade Among PrEP Eligible Transmasculine Individuals.
aTwenty-one of the 149 people who reported receiving PrEP information from a provider, but did not report having an HIV test in the past year. These people are included in the calculated percentage for the overall cascade (i.e., 33.9% = 149/439), but are excluded from the calculated relative percentage of those who had an HIV test in the past year (i.e., 44.9% = 128/285).
DISCUSSION
In this national sample of transmasculine individuals, almost one quarter (24.3%; n = 439) had engaged in sexual behaviors that would make them eligible for PrEP, but less than 3% (n = 48) had actually been prescribed PrEP. We created a cascade to examine PrEP access among PrEP eligible transmasculine participants, suggesting that high percentages of PrEP eligible individuals see a health care provider and receive an HIV test (64.9%), but only a third (33.9%, n = 149) of PrEP eligible patients actually received PrEP information from their doctor, and only 10.9% of those eligible for PrEP actually received a prescription.
The data from this national sample stand in contrast with some prevalent assumptions about transmasculine individuals and their sexual behavior and health. In our sample, transmasculine individuals had sexual partners of various genders and identified with sexual orientations across the spectrum. A substantial proportion of the sample reported receptive sex with cisgender male or transgender female partners, and over 18% of the sample reported condomless receptive sex in the past six months. These data indicate the importance of providing comprehensive sexual health care to transmasculine individuals, which includes HIV prevention, STI prevention, and reproductive health care. More work is needed in the development of sexual history and other assessment tools that are relevant and affirming to individuals regardless of their gender identity. Although the majority of participants reported that they preferred to be asked about “vaginal sex,” a substantial number (22.7%, n = 315) reported preferring the term “front hole sex,” and another 17.6% (n = 244) reported preferring different terms (e.g., “front opening sex,” “intercourse that could result in a child”). It is critical for providers to ask transgender patients about their preferred language when conducting a sexual history. Increased provider education is necessary to support culturally competent conversations about sexual health with their transgender patients.
Some of the factors associated with PrEP eligibility in this sample may be useful in guiding conversations about sexual health and focusing assessment. Not surprisingly, sexual identity was a strong predictor of PrEP eligibility, as was being in an open or polyamorous relationship. Over 34% of transmasculine individuals who identified as gay met PrEP eligibility criteria, and over 45% of those in open/polyamorous relationships were PrEP eligible. These data are consistent with recent examinations of PrEP eligibility among transmasculine individuals, albeit with much smaller samples.21 It is also important to note that 21% of transmasculine individuals who reported being in a monogamous relationship met eligibly criteria for PrEP. Similar to data indicating that a larger proportion of cisgender gay men are exposed to HIV from their main (or monogamous partner)18,19, transmasculine individuals may need to be engaged in HIV prevention efforts regardless of their relationship status. These types of questions may not be included in standard sexual histories, as providers are often taught to stick to more “objective” behavioral questions about number and gender of sexual partners20. These data suggest that including more open-ended questions about identity and relationship status may aid in the assessment of sexual health.
Although only a small percentage of the sample reported substance use other than alcohol, substance use emerged as an extremely important predictor of PrEP eligibility. Over 50% of stimulant users and over 65% of poppers users met PrEP eligibility criteria. These data are consistent with other recent analyses of the association between substance use and PrEP eligibility among sexual and gender minority individuals21. Substance use is not always integrated into sexual history assessments; these data suggest that discussions about substance use are a vital part of PrEP eligibility conversations for transmasculine individuals.
It is important to note that being on testosterone was a significant positive predictor of PrEP eligibility in univariable testing, but was not retained in the multivariable model. These data suggest that it is important for providers to engage transmasculine individuals in conversations around PrEP regardless of whether or not they are taking testosterone. It is encouraging to note that participants who had not had an HIV test in the past year had significantly lower prevalence of PrEP eligibility. These data suggest that individuals who are engaging in sexual risk behavior are more likely to seek out or receive testing. However, it is possible that individuals who were less likely to test for HIV were also less likely to test for STIs, and their PrEP eligibility might be underestimated due to undiagnosed infections. As our PrEP access cascade suggests, increasing rates of testing among transmasculine individual is important, as is ensuring that testing is supplemented by PrEP education and prescription, where warranted.
A major strength of this study is the fact that it is a large-scale, national sample of transgender individuals that is relatively demographically diverse. We believe that our success in recruitment was due in large part to the efforts of our transgender-lead research team, who designed a survey instrument that many participants described as “affirming” and led to wide distribution and sharing within transmasculine social networks across the country. At the same time, this sample is a convenience sample of individuals who completed a self-report survey on the internet. We performed extensive data checks for quality, but any internet-based survey study is limited in its potential generalizability. Future research should be conducted to review and potentially replicate these findings with other samples of transmasculine individuals, especially those that contain higher percentages of individuals of color.
Despite these limitations, our results suggest that a substantial proportion of transmasculine individuals meet eligibility criteria for PrEP and are in need of additional PrEP education and access. More research is needed into the unique sexual health needs of transmasculine patients, and into the development of provider guidelines for best working with this population. Enhanced efforts should be made by providers, programs, and systems to assess HIV-related risk in transmasculine patients and engage them in comprehensive sexual health care.
ACKNOWLEDGEMENTS
This research was supported by Grant R01AA022067-04S1 from the National Institute of Alcohol Abuse and Alcoholism (S.A. Golub, PI). The authors gratefully acknowledge the contributions of Charles Solidum, Brandyn Gallagher, and all the individuals who gave their time and energy to participate in this study.
Source of Funding: This research was funded by Grant R01AA022067-04S1 from the National Institute of Alcohol Abuse and Alcoholism (S.A. Golub, PI).
REFERENCES
- 1.Poteat T, Malik M, Scheim A, Elliott A. HIV prevention among transgender populations: Knowledge gaps and evidence for action. Current HIV/AIDS Reports. 2017;14(4):141–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reisner SL, Murchison GR. A global research synthesis of HIV and STI biobehavioural risks in female-to-male transgender adults. Global public health. 2016;11(7-8):866–887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poteat T, Scheim A, Xavier J, Reisner S, Baral S. Global epidemiology of HIV infection and related syndemics affecting transgender people. Journal of acquired immune deficiency syndromes (1999). 2016;72(Suppl 3):S210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kenagy GP, Hsieh C-M. The risk less known: Female-to-male transgender persons’ vulnerability to HIV infection. AIDS care. 2005;17(2):195–207. [DOI] [PubMed] [Google Scholar]
- 5.McFarland W, Wilson EC, Raymond HF. HIV Prevalence, Sexual Partners, Sexual Behavior and HIV Acquisition Risk Among Trans Men, San Francisco, 2014. AIDS Behav. 2017;21(12):3346–3352. [DOI] [PubMed] [Google Scholar]
- 6.Feldman J, Romine RS, Bockting WO. HIV risk behaviors in the US transgender population: prevalence and predictors in a large internet sample. Journal of homosexuality. 2014;61(11):1558–1588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bauer GR, Redman N, Bradley K, Scheim AI. Sexual health of trans men who are gay, bisexual, or who have sex with men: results from Ontario, Canada. International Journal of Transgenderism. 2013;14(2):66–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reisner SL, Jadwin-Cakmak L, Hughto JMW, Martinez M, Salomon L, Harper GW. Characterizing the HIV Prevention and Care Continua in a Sample of Transgender Youth in the US. AIDS and behavior. 2017;21(12):3312–3327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shover CL, DeVost MA, Beymer MR, Gorbach PM, Flynn RP, Bolan RK. Using Sexual Orientation and Gender Identity to Monitor Disparities in HIV, Sexually Transmitted Infections, and Viral Hepatitis. American journal of public health. 2018;108(S4):S277–S283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clark H, Babu AS, Wiewel EW, Opoku J, Crepaz N. Diagnosed HIV infection in transgender adults and adolescents: results from the National HIV Surveillance System, 2009-2014. AIDS and Behavior. 2017;21(9):2774–2783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reisner SL, Hughto JMW, Pardee DJ, Kuhns L, Garofalo R, Mimiaga MJ. LifeSkills for men (LS4M): pilot evaluation of a gender-affirmative HIV and STI prevention intervention for young adult transgender men who have sex with men. Journal of Urban Health. 2016;93(1):189–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Scheim AI, Santos GM, Arreola S, et al. Inequities in access to HIV prevention services for transgender men: results of a global survey of men who have sex with men. Journal of the International AIDS Society. 2016;19:20779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rowniak S, Ong-Flaherty C, Selix N, Kowell N. Attitudes, Beliefs, and Barriers to PrEP Among Trans Men. AIDS Educ Prev. 2017;29(4):302–314. [DOI] [PubMed] [Google Scholar]
- 14.Rider GN, McMorris BJ, Gower AL, Coleman E, Eisenberg ME. Health and care utilization of transgender and gender nonconforming youth: A population-based study. Pediatrics. 2018:e20171683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Service UPH. Preexposure prophylaxis for the prevention of HIV infection in the United States—2014: a clinical practice guideline. Washington, DC: US Public Health Service; 2014. [Google Scholar]
- 16.Barros AJ, Hirakata VN. Alternatives for logistic regression in cross-sectional studies: an empirical comparison of models that directly estimate the prevalence ratio. BMC medical research methodology. 2003;3(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zou G A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159(7):702–706. [DOI] [PubMed] [Google Scholar]
- 18.Sullivan PS, Salazar L, Buchbinder S, Sanchez TH. Estimating the proportion of HIV transmissions from main sex partners among men who have sex with men in five US cities. Aids. 2009;23(9):1153–1162. [DOI] [PubMed] [Google Scholar]
- 19.Goodreau SM, Carnegie NB, Vittinghoff E, et al. What drives the US and Peruvian HIV epidemics in men who have sex with men (MSM)? PloS one. 2012;7(11):e50522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fiereck K Cultural Conundrums: The Ethics of Epidemiology and the Problems of Population in Implementing Pre - Exposure Prophylaxis. Developing world bioethics. 2015;15(1):27–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Shover CL, Javanbakht M, Shoptaw S, et al. HIV Preexposure Prophylaxis Initiation at a Large Community Clinic: Differences Between Eligibility, Awareness, and Uptake. American journal of public health. 2018;108(10):1408–1417. [DOI] [PMC free article] [PubMed] [Google Scholar]


