Abstract
Background:
Postoperative delirium is one of the most common complications in elderly surgical population. However, its long-term outcomes remain largely to be determined. We therefore conducted a prospective cohort study to determine the association between postoperative delirium and long-term decline in activities of daily living and postoperative mortality. The hypothesis in the present study was that postoperative delirium was associated with greater decline in activities of daily living and higher mortality within 24–36 months after anesthesia and surgery.
Methods:
The participants (≥ 65 years old) having the surgeries of (1) proximal femoral nail, (2) hip replacement or (3) open reduction and internal fixation under general anesthesia were enrolled. The Confusion Assessment Method algorithm was administered to diagnose delirium before and on the first, second and fourth days after the surgery. Activities of daily living were evaluated by using the Chinese version of Activities of Daily Living Scale (range: 14 to 56 points), and preoperative cognitive function was assessed by using the Chinese Mini-Mental State Examination (range: 0 to 30 points). The follow-up assessments, including activities of daily living and mortality, were conducted between 24 to 36 months after anesthesia and surgery.
Results:
Thirty-four (26%) of 130 participants (80 ± 6 years, 24% male) developed postoperative delirium during the hospitalization. There were 32% of the participants who were lost to follow-up, resulting in 88 participants who were finally included in the data analysis. The participants with postoperative delirium had a greater decline in activities of daily living (16 ± 15 versus 9 ± 15, P = 0.037) and higher 36-month mortality (8/28, 29% versus 7/75, 9%; P = 0.009) as compared to the participants without postoperative delirium.
Conclusions:
Postoperative delirium was associated with long-term detrimental outcomes, including greater decline in activities of daily living and a higher rate of postoperative mortality.
Keywords: Postoperative delirium, activities of daily living, anesthesia and surgery
Summary statement:
Postoperative delirium was associated with greater decline in activities of daily living and higher postoperative mortality.
Introduction
Postoperative delirium, one of the most common postoperative complications among elderly patients1,2, is associated with postoperative neurocognitive disorder, increased other postoperative complications, prolonged hospital stays, higher discharge rates to nursing homes and poor survival rates3–5. The U.S. healthcare costs attributable to delirium exceed $182 billion per year6,7.
Postoperative delirium is not always transient or reversible, and increasing evidences have demonstrated both short-term and long-term poor prognoses in surgical patients who have developed postoperative delirium8–10. Large cohort studies suggest that postoperative delirium is associated with a significant impairment in global cognitive function 12 months post-surgery8,9. Moreover, such cognitive impairment can persist up to 36 months10.
There have been studies to investigate the association between delirium and activities of daily living (ADL)11,12. Specifically, Marcantonio and his colleagues reported that postoperative delirium was independently associated with poorer ADL at one month after the surgery, but such association disappeared at six months post-surgery11. A recent study showed that postoperative delirium was associated with persistent ADL impairment after a major elective surgery13. However, controversy still exists regarding the causal relationship between delirium and postoperative mortality due to the high risk of confounding bias as evidenced by a recent systematic review14. Although most studies reported that postoperative delirium was associated with an increased risk of death15,16, a few other studies have indicated that the association was not apparent after adjusting for adequate confounders17,18. Therefore, the associations among postoperative delirium, the long-term ADL and mortality remain to be determined.
We therefore set up a prospective longitudinal study using a cohort of patients who had orthopedic surgery under general anesthesia. The objective of this study was to investigate the effects of postoperative delirium on the long-term decline in ADL and postoperative mortality. The primary hypothesis in the present study was that postoperative delirium was associated with greater ADL decline. The secondary hypothesis was that patients with postoperative delirium would have a higher rate of mortality within 24 to 36 months after anesthesia and surgery.
Methods
Study Population
The study protocol was approved by the Human Research Ethics Committee of Shanghai Tenth People’s Hospital and Tongji University in Shanghai, P. R. China [RES-2013015]. All participants signed the informed consent prior to being enrolled in the study.
Eligible participants were screened and enrolled exclusively at Shanghai Tenth People’s Hospital, a university-affiliated hospital with about 3 million outpatients and more than 40,000 surgeries every year, from August 2013 to August 2014. The follow-up assessments were carried out within 24 to 36 months after anesthesia and surgery. Participants were included if they met the following eligibility criteria: (1) 65 years old or older, (2) Chinese Mandarin as the native language, (3) scheduled to undergo orthopedic surgery, and (4) having the ability of verbal communication and writing skills and thus being able to provide informed consent13. Eligible surgical procedures included the surgeries of proximal femoral nail, hip replacement and open reduction and internal fixation. The exclusion criteria were: (1) preoperative delirium according to the Confusion Assessment Method (CAM) algorithm19, (2) prior diagnoses of neurologic diseases, e.g., Parkinson’s diseases, multiple sclerosis or stroke according to International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)20, (3) history of mental disorders, e.g., major depressive disorder and schizophrenia diagnosed according to Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV)21, or (4) unwillingness to participate in the study.
Preoperative interview
After the patients being admitted to the hospital, two trained research assistants (Z.S. and Y.W.) carried out the preoperative screening assessments in person one day before the scheduled surgery. The assessments included a review of the patient’s medical chart and an interview with the patient. Characteristics of the participants were collected, including age, sex, education, marital status and living conditions. Moreover, the age-adjusted Charlson comorbidity index (ACCI)22 was obtained through patient interviews or medical records reviews based on the validated Charlson comorbidity coding algorithms23, with higher scores indicating more comorbidities.
Pre-admission status of daily function was assessed by using the Chinese version of Activities of Daily Living Scale (ADLs)24, which included a Physical Self-Maintenance Scale (PSMS) and an Instrumental ADLs (IADLs). There is a total of 14 items. Specifically, PSMS is used to assess the fundamental skills typically needed to manage basic physical needs and consists of the following six tasks: transferring/ambulating, eating, dressing, grooming/personal hygiene, bathing, toileting/continence; IADLs is used to assess more complex activities related to independent living and contains the following eight tasks: taking public transportation, preparing food, housekeeping, taking medications, doing laundry, shopping, making phone calls and managing finances. For each item, the scoring is determined by a 4-point coding system: 1 = “can do it myself”, 2 = “have some difficulty doing but can still do it by myself”, 3 = “need help to do it”, 4 = “cannot do it at all”. The total score of ADLs ranges from 14 to 56 points and higher ADLs scores indicate lower activities of daily living. The participants with the ADLs score more than 22 points (the cutoff score) are defined as having impairment in activities of daily living25.
The Chinese Mini-Mental State Examination (CMMSE) was performed to assess for global cognitive function. There are 19 items and the maximum score of CMMSE is 30 points. The optimal cutoff points in dementia or abnormal cognitive function screening are stratified by education levels (17/18 for those illiterate, 20/21 for individuals with 1–6 years of education, and 24/25 for individuals with 7 or more years of education)26.
Anesthesia and surgery
All participants were scheduled to undergo orthopedic surgery, and had standardized perioperative care, including anesthesia and postoperative pain management, as described in our previous studies27. We did not determine the association between the depth of anesthesia and postoperative delirium as such association has been investigated in the previous studies28–30. In addition, by reviewing the patient’s anesthesia records, we were able to obtain the information of American Society of Anesthesiologists (ASA) classification, anesthesia types, estimated blood loss, the length of anesthesia administration and operation, as well as the length of hospitalization.
Postoperative delirium assessment
The assessments of delirium were performed as described in our previous studies27. Specifically, postoperative delirium was assessed once daily between 10:00 am and 4:00 pm on day 1, day 2, and day 4 post-surgery. The psychiatrists who performed the delirium assessments in the current study had good training and went through quality control procedures. The inter-rater reliability calculated from the intra-class correlation (ICC) coefficient was 0.96 [95% confidence interval (CI): 0.92–0.98)31.
The incidence of postoperative delirium was determined according to the CAM diagnostic algorithm, which was used to determine the presence or absence of delirium19. The algorithm consists of four clinical criteria: (1) acute onset and fluctuating course, (2) inattention, (3) disorganized thinking, and (4) altered level of consciousness. To define a patient as having delirium, both the first and the second criteria have to be present, as well as either the third or the fourth criteria is present. The CAM in the Chinese language has been proven to have good reliability and validity among the Chinese elderly population32. Patients with a positive diagnosis on postoperative day 1, day 2 or day 4 would be coded as “having postoperative delirium”.
Follow-up interview
The participants had follow-up interviews within 24 to 36 months after anesthesia and surgery. The following assessments were conducted in the form of face-to-face interviews or phone interviews if the participants were not available for the face-to-face interviews. The interviewers who performed the follow-up assessments were blinded to the diagnosis of postoperative delirium of the participants. During the interviews, activities of daily living were assessed with the Chinese version of ADLs. Moreover, we obtained information on participant’s status of death by consulting with their family members and reviewing their electronic medical records. In addition, the diagnosis of postoperative delirium was made only immediately on postoperative days during the hospitalization but not at the time of follow-up.
Statistical analysis
The study was powered to detect a difference in activities of daily living between the participants with and without postoperative delirium in an orthopedic surgery population, based on the incidence of postoperative delirium (26%) and the between-group differences in preoperative ADLs score [mean difference ± standard deviation (SD): 4 ± 6], obtained and analyzed from the data in our previous studies27. It was estimated that 96 participants would be required to detect a significant difference, at the 5% significance level with 80% power. Moreover, the previous studies demonstrated a recruitment rate of 63%27. Thus, we had planned to screen at least 153 patients undergoing orthopedic surgery in one year to be able to recruit 96 participants at the start of the studies.
The Kolmogorov-Smirnov test was used to test for the normality of all variables. The between-group differences were compared using a Student’s t-test for continuous variables (mean ± SD) or a Chi-square test for categorical variables [n (%)]. Mann-Whitney U test was used to compare the group difference in the ADLs score [median ± interquartile range (IQR)]. We estimated the overall mortality rate by using the Kaplan-Meier analysis and the differences were compared using log-rank tests. Cox regression analysis was carried out to determine the association between postoperative delirium and overall survival rate. Factors that showed a significant association with postoperative delirium in the univariate analyses were included as covariates in the Cox survival analysis model. Since the burden of comorbidities has been demonstrated to affect the postoperative short-term and long-term survival rates, it was further included in the model as a covariate. All analyses were performed using the SPSS version 20.0 (SPSS Inc., Chicago, IL) or Prism 6 software (La Jolla, CA), with P < 0.05 as the significance level.
Results
Baseline characteristics
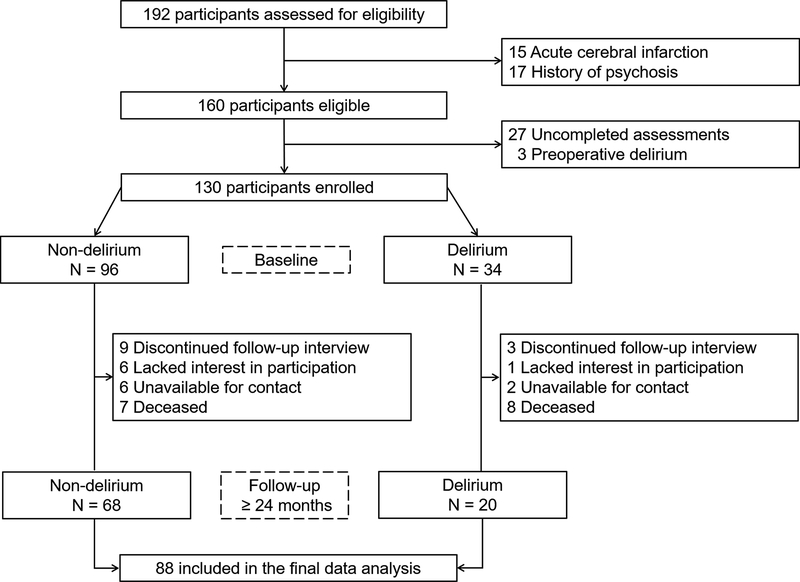
Figure 1 showed the enrollment, exclusions, and patients available for analysis among 192 participants. Six-two participants were excluded at baseline due to acute cerebral infarction (N = 15), psychosis history (N = 17), uncompleted assessments (N = 27), and the diagnosis of preoperative delirium (N = 3). Thus, a total of 130 participants (80 ± 6 years, 24% male) provided informed consent and were enrolled in this study. All participants had been scheduled to undergo orthopedic surgery, including proximal femoral nail (N = 67), hip replacement (N = 56) and open reduction and internal fixation surgeries (N = 7) under general anesthesia. The characteristics of these participants were presented in Table 1.
Figure 1.
Consort diagram shows the enrollment, exclusions, and participants available for analysis.
Table 1.
Baseline characteristics of study population.
| Variables (N=130) | Delirium (N=34) | Non-delirium (N=96) | P Value |
|---|---|---|---|
| Age (years), mean ± SD | 83 ± 5 | 79 ± 6 | 0.001 |
| Sex, male, n (%) | 9 (27%) | 22 (23%) | 0.676 |
| Marital status, n (%) | |||
| married | 21 (62%) | 74 (77%) | 0.058 |
| single | 11(32%) | 16 (17%) | |
| divorced/widowed | 2 (6%) | 6 (6%) | |
| Living condition, n (%) | |||
| living together | 20 (59%) | 73 (76%) | 0.056 |
| living alone | 14 (41%) | 23 (24%) | |
| Children, n (%) | |||
| having children | 29 (85%) | 89 (93%) | 0.289 |
| no children | 5 (15%) | 7 (7%) | |
| BMI (kg/m2), mean ± SD | 20 ± 6 | 22 ± 4 | 0.673 |
| Education (years), mean ± SD | 4 ± 5 | 5 ± 5 | 0.229 |
| ACCI (points), mean ± SD | 5 ± 1 | 5 ± 2 | 0.353 |
| CMMSE (points), mean ± SD | 18 ± 5 | 24 ± 5 | 0.001 |
| CRP (mg/L), mean ± SD | 29 ± 26 | 25 ± 21 | 0.245 |
| HGB (g/dL), mean ± SD | 10 ± 2 | 10 ± 2 | 0.123 |
| WBC (K/μL), mean ± SD | 8 ± 3 | 8 ± 3 | 0.598 |
| ASA class, n (%) | |||
| I | 1 (3%) | 1 (1%) | |
| II | 20 (59%) | 64 (67%) | 0.580 |
| III | 13 (38%) | 31 (32%) | |
| Anesthesia type, n (%) | |||
| propofol | 1 (3%) | 5 (5%) | |
| sevoflurane | 10 (29%) | 21 (22%) | 0.620 |
| propofol & sevoflurane | 23 (68%) | 70 (73%) | |
| Surgery type, n (%) | |||
| proximal femoral nail | 22 (65%) | 45 (47%) | |
| hip replacement | 10 (29%) | 46 (48%) | 0.160 |
| open reduction and internal fixation | 2 (6%) | 5 (5%) | |
| Length of anesthesia (min), mean ± SD | 128 ± 49 | 132 ± 50 | 0.729 |
| Length of operation (min), mean ± SD | 88 ± 46 | 100 ± 44 | 0.174 |
| Estimated blood loss (mL), mean ± SD | 329 ± 286 | 316 ± 264 | 0.814 |
| Length of hospitalization (day), mean ± SD | 20 ± 6 | 18 ± 5 | 0.127 |
BMI, Body Mass Index; SD, standard deviation; ACCI, age-adjusted Charlson comorbidity index; CMMSE, Chinese Mini-Mental State Examination; CRP, C-reactive protein; HGB, Hemoglobin; WBC, white blood cell; ASA, American Society of Anesthesiologists.
Thirty-four of the 130 participants (26%) developed postoperative delirium on day 1, day 2 or day 4 after anesthesia and surgery. The participants who developed postoperative delirium were older (83 ± 5 versus 79 ± 6, P = 0.001), and had more severe preoperative cognitive impairment than those without postoperative delirium (CMMSE score of 18 ± 5 versus 24 ± 5, P = 0.001).
There were no significant differences in other characteristics between the participants with and without postoperative delirium. There were also no significant differences in the ASA class, anesthesia types (total intravenous anesthesia with propofol versus inhalational anesthesia with sevoflurane versus mixed with propofol and sevoflurane), surgery types, length of anesthesia and surgery, estimated blood loss, and the length of hospitalization between the participants with postoperative delirium and those without postoperative delirium.
Association between postoperative delirium and the long-term outcomes
During the period of follow-up, there were 42 participants (32%) who were lost to the follow-up due to the discontinuation of interviews (N = 12), no more interest in participating in the study (N = 8), and unavailability of contacts (N = 8). In addition, another 15 participants died during the follow-up period, which we confirmed through their family members and by reviewing their electronic medical records. Consequently, 88 participants completed the follow-up assessments and were finally included in the data analysis (Figure 1). The assessments in the follow-up studies included both face-to-face interviews (N = 47) and phone interviews (N = 41). There were no significant differences in regards to the incidence of postoperative delirium and the characteristics between the participants who remained in the study and those who dropped out from the study (Table 2).
Table 2.
Demographic and clinical characteristics between the participants who stayed in the studies and the participants who dropped from the studies.
| Variables (N=130) | Followed (N=88) | Dropped out (N=42) | P Value |
|---|---|---|---|
| Age (years), mean ± SD | 80 ± 7 | 81± 5 | 0.586 |
| Sex, male, n (%) | 19 (22%) | 12 (29%) | 0.382 |
| Marital status, n (%) | |||
| married | 64 (73%) | 31 (74%) | 0.450 |
| single | 20 (23%) | 7 (17%) | |
| divorced/widowed | 4 (4%) | 4 (9%) | |
| Living condition, n (%) | |||
| living together | 65 (74%) | 28 (67%) | 0.395 |
| living alone | 23 (26%) | 14 (33%) | |
| Children, n (%) | |||
| having children | 79 (90%) | 38 (90%) | 0.900 |
| no children | 9 (10%) | 4 (10%) | |
| BMI (kg/m2), mean ± SD | 23 ± 5 | 23 ± 3 | 0.902 |
| Education (years), mean ± SD | 5 ± 5 | 4 ± 5 | 0.272 |
| ACCI (points), mean ± SD | 5 ± 2 | 4 ± 5 | 0.939 |
| CMMSE (points), mean ± SD | 22 ± 5 | 22 ± 6 | 0.823 |
| CRP (mg/L), mean ± SD | 29 ± 24 | 20 ± 19 | 0.082 |
| HGB (g/dL), mean ± SD | 11 ± 2 | 11 ± 2 | 0.879 |
| WBC (K/μL), mean ± SD | 8 ± 3 | 8 ± 3 | 0.521 |
| ASA class, n (%) | |||
| I | 1 (1%) | 1 (2%) | |
| II | 55 (63%) | 29 (69%) | 0.613 |
| III | 32 (36%) | 12 (29%) | |
| Anesthesia type, n (%) | |||
| propofol | 3 (3%) | 3 (7%) | |
| sevoflurane | 22 (25%) | 9 (21%) | 0.620 |
| propofol & sevoflurane | 63 (72%) | 30 (72%) | |
| Surgery type, n (%) | |||
| proximal femoral nail | 47 (53%) | 20 (48%) | |
| hip replacement | 37 (42%) | 19 (45%) | 0.743 |
| open reduction and internal fixation | 4 (5%) | 3 (7%) | |
| Length of anesthesia (min), mean ± SD | 129 ± 46 | 134 ± 58 | 0.585 |
| Length of operation (min), mean ± SD | 93 ± 41 | 103 ± 51 | 0.231 |
| Estimated blood loss (mL), mean ± SD | 304 ± 241 | 351 ± 322 | 0.372 |
| Length of hospitalization (day), mean ± SD | 19 ± 6 | 19 ± 5 | 0.973 |
| Postoperative delirium, n (%) | 20 (23%) | 14 (33%) | 0.198 |
BMI, Body Mass Index; SD, standard deviation; ACCI, age-adjusted Charlson comorbidity index; CMMSE, Chinese Mini-Mental State Examination; CRP, C-reactive protein; HGB, Hemoglobin; WBC, white blood cell; ASA, American Society of Anesthesiologists.
Activities of daily living (ADL).
In this cohort, 18 of 34 (53%) participants with postoperative delirium had preoperative ADL impairment (more than the cutoff score of 22 points), while only 22 of 96 (23%) participants without postoperative delirium had ADL impairment before the surgery (P = 0.001; Chi-square test). Moreover, 24–36 months after anesthesia and surgery, the participants who developed postoperative delirium had a greater decline in ADL, as evidenced by the larger increase in ADLs scores as compared to the participants who did not develop postoperative delirium (median ± IQR: 16 ± 15 versus 9 ± 15, P = 0.037; Mann-Whitney U test). Specifically, the participants who had developed postoperative delirium after proximal femoral nail surgery (median ± IQR: 18 ± 15 versus 10 ± 12, P = 0.041; Mann-Whitney U test), but not after hip replacement surgery (median ± IQR: 12 ± 13 versus 7 ± 14, P = 0.283; Mann-Whitney U test), exhibited significant decline in ADL at the time of the follow-up evaluation. Since only one in four participants had developed postoperative delirium after open reduction and internal fixation surgery, we decided not to determine the association between postoperative delirium and ADL decline in these participants during the follow-up interviews (Table 3).
Table 3.
Comparison of activities of daily living between participants with and without postoperative delirium.
| Overall (N=88) | Delirium (N=20) | Non-delirium (N=68) | P Value |
|---|---|---|---|
| Baseline ADLs (points), median ± IQR | 22 ± 11 | 15 ± 5 | 0.005 |
| Follow-up ADLs (points), median ± IQR | 40 ± 23 | 27 ± 17 | 0.002 |
| ADL declinea (points), median ± IQR | 16 ± 15 | 9 ± 15 | 0.037 |
| Proximal femoral nail (n=47) | Delirium (n=13) | Non-delirium (n=34) | P Value |
| Baseline ADLs (points), median ± IQR | 23 ± 10 | 15 ± 4 | 0.002 |
| Follow-up ADLs (points), median ± IQR | 43 ± 21 | 28 ± 16 | 0.001 |
| ADL declinea (points), median ± IQR | 18 ± 15 | 10 ± 12 | 0.041 |
| Hip replacement (n=37) | Delirium (n=6) | Non-delirium (n=31) | P Value |
| Baseline ADLs (points), median ± IQR | 20 ± 14 | 16 ± 7 | 0.432 |
| Follow-up ADLs (points), median ± IQR | 33 ± 24 | 27 ± 19 | 0.147 |
| ADL declinea (points), median ± IQR | 12 ± 13 | 7 ± 14 | 0.283 |
| Open reduction and internal fixation (n=4) | Delirium (n=1) | Non-delirium (n=3) | N/Ab |
ADL decline was calculated by using follow-up ADLs score minus baseline ADLs score, which indicated the decline of activities of daily living. The larger ADLs change score indicates the greater ADL decline.
There was only one in four participants who had developed postoperative delirium after open reduction and internal fixation surgery at the time of follow-up evaluation. Thus, we did not determine the association between postoperative delirium and the decline of ADL in these participants.
Statistically significant results are highlighted in bold. ADL, activities of daily living; IQR, interquartile range; N/A, not applicable.
Mortality.
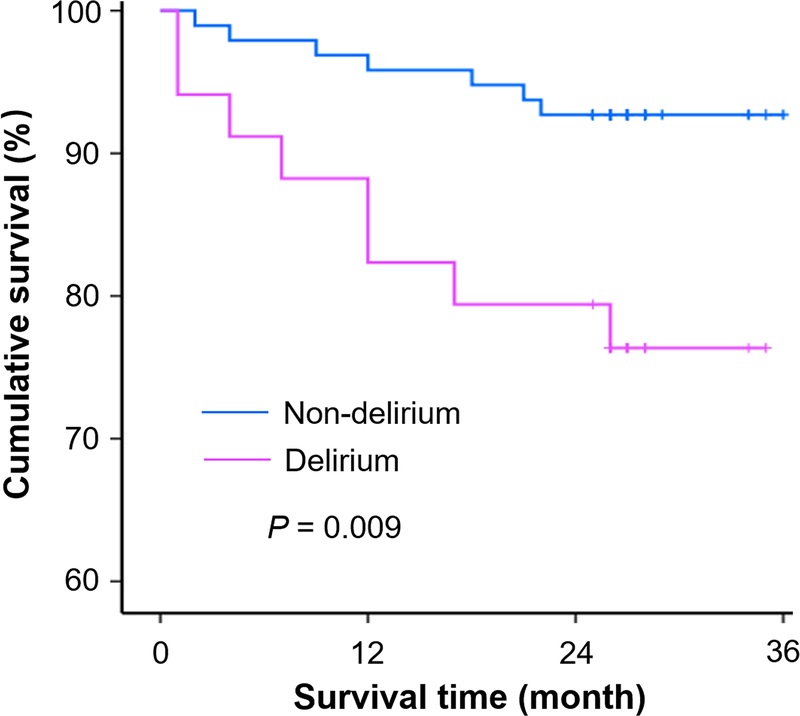
The mortality rate of patients with and without postoperative delirium within 24–36 months after anesthesia and surgery was calculated using Kaplan-Meyer analysis. In the current cohort, participants who developed postoperative delirium had a higher mortality rate (8/28, 29%) as compared to the participants who did not develop postoperative delirium (7/75, 9%; P = 0.009; log-rank test; Figure 2).
Figure 2. Cumulative survival rates according to the presence of postoperative delirium.
The postoperative morality rates within 24–36 months of the followed participants after orthopedic surgery were calculated by using the Kaplan-Meyer analysis. Specifically, the 36-month mortality rate of participants with postoperative delirium (8/28, 29%) was significantly higher than that of participants without postoperative delirium (7/75, 9%) at the follow-up (P = 0.009, log-rank test). Symbols (+) indicate the censored data.
Univariable and multivariable analyses of overall survival were calculated by using Cox regression models. Postoperative delirium was associated with a lower survival rate (unadjusted hazard ratio = 0.28, 95% CI of 0.10–0.78, P = 0.015). After the adjustment of preoperative cognitive function (determined by CMMSE score) and the age-adjusted comorbidities (determined by ACCI score), we found that postoperative delirium was still independently associated with poor long-term survival rate (adjusted hazard ratio = 0.22, 95% CI of 0.07–0.67, P = 0.007). These results suggested that participants with postoperative delirium had an increased risk of mortality in the long-term after anesthesia and surgery.
Discussion
This prospective study demonstrated that postoperative delirium was associated with greater decline in activities of daily living and higher postoperative mortality within 24 to 36 months after anesthesia and surgery.
It has been reported that the prevalence of preoperative delirium in elderly patients with hip fractures was 4–6%33,34. The prevalence of preoperative delirium in the present study was 2% (3/133), which could be partially due to the strict exclusion of participants. Specifically, the participants with acute cerebral infarction (N = 15) or history of psychosis (N = 17) have been excluded from the studies and did not receive the assessment of preoperative delirium. In addition, another 27 participants were excluded because they had refused to complete the assessment of preoperative delirium. The prevalence of preoperative delirium could have been different if these participants had not been excluded.
The observed incidence of postoperative delirium in current study was 26%, which was comparable with that obtained in other studies for non-cardiac surgeries13,35–37with a range from 9% to 28%38, thus demonstrating the validity of our assessment of postoperative delirium. However, Bitsch and his co-workers reported an average incidence of postoperative delirium being 35% in their studies39. Moreover, the incidence was higher in the intensive care unit patients with critical illness (19%−82%), and in patients who received emergent hip fracture repair surgery (41%)2,11. The exact reasons for such differences are not clear at the present time. It might be related to the different healthcare environment and settings, predisposing conditions and types of surgery.
Previous studies have reported that postoperative delirium was associated with cognitive impairment upon discharge and decline in ADL during 1–3 months after hip surgery11,40. However, the associations between postoperative delirium and the long-term (e.g., more than 24 months) ADL and mortality have not been investigated. The current study showed that the participants who had postoperative delirium experienced a greater decline in ADL and exhibited higher mortality within 24 to 36 months after anesthesia and surgery.
Activities of daily living or ADL, an important component of assessment for major surgery41, have been widely used as an index for the measurement of postoperative recovery as demonstrated in previous studies24,25. It has been found that patients who developed postoperative delirium had poorer recovery within six months after the surgery as compared to those did not develop it11,12,15,40. The current study found that all of the participants showed declined ADL (increase of ADLs scores) after anesthesia and surgery. Specifically, the participants who developed postoperative delirium had a greater decline in ADL 24 to 36 months after anesthesia and surgery as compared to those who did not develop it. Furthermore, participants undergoing the surgery of proximal femoral nail demonstrated greater decline in ADL than the participants having hip replacement during the time of follow-up interviews, which was likely due to the different age distributions (82 ± 6 versus 78 ± 7, P = 0.040) and surgical indications (e.g., femoral intertrochanteric fracture). Collectively, these findings suggested that the occurrence of postoperative delirium among the elderly surgical population could worsen the long-term ADL.
The current study reported that patients who had postoperative delirium would have a higher mortality rate even after controlling for age-adjusted Charlson comorbidities and preoperative cognitive status. Consistently, most studies supported that patients who developed delirium were at an increased risk of death14, and that delirium was associated with 6-month15, 12-month16 and 5-year42 postoperative mortality. These results suggest that efforts should be implemented in the elderly population at high risk of developing postoperative delirium following orthopedic surgery. Note that there were potential confounders during the follow-up 24–36 months post-surgery, which could influence the outcomes of the current studies. The future studies to determine such influence are warranted.
Limitations
The current studies have several limitations. First, the sample size was relatively small. However, the 88 participants in the follow-up studies were sufficient to illustrate the association between postoperative delirium and long-term decline in ADL. The current studies have mainly established a system and generated a hypothesis for the future larger scale studies. Note, the retention rates (20/34, 59% versus 68/96, 71%; P = 0.601) and the total follow-up time (28 ± 3 months versus 27 ± 3 months; P = 0.724) were comparable between the participants with and without postoperative delirium. Second, the need for informed consent in the studies could limit the participation into a group that has less risk of developing postoperative delirium, declined ADL or death. Third, we didn’t assess whether the participants had postoperative delirium daily until the discharge, which may lead to missing the detection of postoperative delirium. However, ample evidences have suggested that most of postoperative delirium occurred within the first three days after anesthesia and surgery9,43. Moreover, we purposely didn’t evaluate the postoperative delirium diagnosed after 7 days to avoid the influence of postoperative neurocognitive disorder, another common postoperative complication among elderly patients, on the activities of daily living and postoperative mortality44. Finally, we did not evaluate the association between postoperative delirium and pre- or postoperative cognitive function. However, such a relationship has been well established in previous studies8–10.
In conclusion, the current studies showed that postoperative delirium was associated with the combination of a greater decline in activities of daily living and a higher mortality rate within 24–36 months after anesthesia and surgery. These findings highlight the need to prevent postoperative delirium whenever possible, particularly among geriatric patients who are vulnerable to developing preoperative and postoperative neurocognitive disorder.
Funding statement:
This work was supported by the National Natural Science Foundation of China (81720108012, 81571034) and Shanghai Natural Science Foundation (16410724500) to Y.S.; National Institute on Aging grants (R01AG030618, K24AG035075, P01AG031720) to E.R.M; and the International Exchange Program for Graduate Students, Tongji University (2017020012) to Z.S.
Footnotes
Clinical trial number and registry URL: Not applicable
Prior Presentations: Not applicable
Conflicts of Interest: None.
References
- 1.Inouye SK: Delirium in older persons. N Engl J Med 2006; 354: 1157–65 [DOI] [PubMed] [Google Scholar]
- 2.Inouye SK, Westendorp RGJ, Saczynski JS: Delirium in elderly people. Lancet 2014; 383: 911–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moskowitz EE, Overbey DM, Jones TS, Jones EL, Arcomano TR, Moore JT, Robinson TN: Post-operative delirium is associated with increased 5-year mortality. Am J Surg 2017; 214: 1036–38 [DOI] [PubMed] [Google Scholar]
- 4.Sprung J, Roberts RO, Weingarten TN, Nunes Cavalcante A, Knopman DS, Petersen RC, Hanson AC, Schroeder DR, Warner DO: Postoperative delirium in elderly patients is associated with subsequent cognitive impairment. Brit J Anaesth 2017; 119: 316–23 [DOI] [PubMed] [Google Scholar]
- 5.Witlox J, Eurelings LS, de Jonghe JF, Kalisvaart KJ, Eikelenboom P, van Gool WA: Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA 2010; 304: 443–51 [DOI] [PubMed] [Google Scholar]
- 6.Leslie DL, Marcantonio ER, Zhang Y, Leo-Summers L, Inouye SK: One-year health care costs associated with delirium in the elderly population. Arch Intern Med 2008; 168: 27–32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leslie DL, Inouye SK: The importance of delirium: economic and societal costs. J Am Geriatr Soc 2011; 59 Suppl 2: S241–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, Brummel NE, Hughes CG, Vasilevskis EE, Shintani AK, Moons KG, Geevarghese SK, Canonico A, Hopkins RO, Bernard GR, Dittus RS, Ely EW, the B-ICUSI: Long-term cognitive impairment after critical illness. N Engl J Med 2013; 369: 1306–16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, Jones RN: Cognitive trajectories after postoperative delirium. N Engl J Med 2012; 367: 30–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Inouye SK, Marcantonio ER, Kosar CM, Tommet D, Schmitt EM, Travison TG, Saczynski JS, Ngo LH, Alsop DC, Jones RN: The short-term and long-term relationship between delirium and cognitive trajectory in older surgical patients. Alzheimers Dement 2016; 12: 766–75 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marcantonio ER, Flacker JM, Michaels M, Resnick NM: Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc 2000; 48: 618–24 [DOI] [PubMed] [Google Scholar]
- 12.Marcantonio E, Ta T, Duthie E, Resnick NM: Delirium severity and psychomotor types: their relationship with outcomes after hip fracture repair. J Am Geriatr Soc 2002; 50: 850–7 [DOI] [PubMed] [Google Scholar]
- 13.Hshieh TT, Saczynski J, Gou RY, Marcantonio E, Jones RN, Schmitt E, Cooper Z, Ayres D, Wright J, Travison TG, Inouye SK: Trajectory of functional recovery after postoperative delirium in elective surgery. Ann Surg 2017; 265: 647–53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamilton GM, Wheeler K, Di Michele J, Lalu MM, McIsaac DI: A systematic review and meta-analysis examining the impact of incident postoperative delirium on mortality. Anesthesiology 2017; 127: 78–88 [DOI] [PubMed] [Google Scholar]
- 15.Mosk CA, Mus M, Vroemen JP, van der Ploeg T, Vos DI, Elmans LH, van der Laan L: Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging 2017; 12: 421–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dubljanin-Raspopovic E, Markovic Denic L, Marinkovic J, Grajic M, Tomanovic Vujadinovic S, Bumbasirevic M: Use of early indicators in rehabilitation process to predict one-year mortality in elderly hip fracture patients. Hip Int 2012; 22: 661–7 [DOI] [PubMed] [Google Scholar]
- 17.Gottschalk A, Hubbs J, Vikani AR, Gottschalk LB, Sieber FE: The impact of incident postoperative delirium on survival of elderly patients after surgery for hip fracture repair. Anesth Analg 2015; 121: 1336–43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furlaneto ME, Garcez-Leme LE: Impact of delirium on mortality and cognitive and functional performance among elderly people with femoral fractures. Clinics (Sao Paulo) 2007; 62: 545–52 [DOI] [PubMed] [Google Scholar]
- 19.Inouye SK, van Dyck CH, Alessi CA, Balkin S, Siegal AP, Horwitz RI: Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 1990; 113: 941–8 [DOI] [PubMed] [Google Scholar]
- 20.WHO: ICD-10-version: 2016. http://apps.who.int/classifications/icd10/browse/2016/en.
- 21.American-Psychiatric-Association: Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Washington, DC: American Psychiatric Association; 1997 [Google Scholar]
- 22.Charlson M, Szatrowski TP, Peterson J, Gold J: Validation of a combined comorbidity index. J Clin Epidemiol 1994; 47: 1245–51 [DOI] [PubMed] [Google Scholar]
- 23.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–83 [DOI] [PubMed] [Google Scholar]
- 24.Chen P, Yu ES, Zhang M, Liu WT, Hill R, Katzman R: ADL dependence and medical conditions in Chinese older persons: a population-based survey in Shanghai, China. J Am Geriatr Soc 1995; 43: 378–83 [DOI] [PubMed] [Google Scholar]
- 25.Lawton MP, Brody EM: Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 1969; 9: 179–86 [PubMed] [Google Scholar]
- 26.Katzman R, Zhang MY, Ouang Ya Q, Wang ZY, Liu WT, Yu E, Wong SC, Salmon DP, Grant I: A Chinese version of the Mini-Mental State Examination; impact of illiteracy in a Shanghai dementia survey. J Clin Epidemiol 1988; 41: 971–78 [DOI] [PubMed] [Google Scholar]
- 27.Shi Z, Wu Y, Li C, Fu S, Li G, Zhu Y, Swain CA, Marcantonio ER, Xie Z, Shen Y: Using the Chinese version of Memorial Delirium Assessment Scale to describe postoperative delirium after hip surgery. Front Aging Neurosci 2014; 6: 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sieber FE, Zakriya KJ, Gottschalk A, Blute MR, Lee HB, Rosenberg PB, Mears SC: Sedation depth during spinal anesthesia and the development of postoperative delirium in elderly patients undergoing hip fracture repair. Mayo Clin Proc 2010; 85: 18–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan MT, Cheng BC, Lee TM, Gin T: BIS-guided anesthesia decreases postoperative delirium and cognitive decline. J Neurosurg Anesthesiol 2013; 25: 33–42 [DOI] [PubMed] [Google Scholar]
- 30.Luk TT, Jia B, Pang EY, Lau VN, Lam CK, Chu MH, Han R, Chan MT: Depth of anesthesia and postoperative delirium. Curr Anesthesiol Rep 2015; 5: 1–9 [Google Scholar]
- 31.Wu Y, Shi Z, Wang M, Cao J, Zhu Y, Shen Y: Chinese version of the Memorial Delirium Assessment Scale (MDAS): Clinical validity and reliability in old postoperative patients. Chinese Mental Health Journal 2014; 28: 937–41 [Google Scholar]
- 32.Leung J, Leung V, Leung CM, Pan PC: Clinical utility and validation of two instruments (the Confusion Assessment Method Algorithm and the Chinese version of Nursing Delirium Screening Scale) to detect delirium in geriatric inpatients. Gen Hosp Psychiatry 2008; 30: 171–6 [DOI] [PubMed] [Google Scholar]
- 33.Brauer C, Morrison R, Silberzweig SB, Siu AL: The cause of delirium in patients with hip fracture. Arch Intern Med 2000; 160: 1856–60 [DOI] [PubMed] [Google Scholar]
- 34.Kagansky N, Rimon E, Naor S, Dvornikov E, Cojocaru L, Levy S: Low incidence of delirium in very old patients after surgery for hip fractures. Am J Geriat Psychiat 2004; 12: 306–14 [PubMed] [Google Scholar]
- 35.Xie Z, Swain CA, Ward SA, Zheng H, Dong Y, Sunder N, Burke DW, Escobar D, Zhang Y, Marcantonio ER: Preoperative cerebrospinal fluid beta-Amyloid/Tau ratio and postoperative delirium. Ann Clin Transl Neurol 2014; 1: 319–28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guo Y, Jia P, Zhang J, Wang X, Jiang H, Jiang W: Prevalence and risk factors of postoperative delirium in elderly hip fracture patients. J Int Med Res 2016; 44: 317–27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, Li Y, Wang L, Liu Y, Yin P, Liu J, Yu S, Tan F, Barber RM, Coates MM, Dicker D, Fraser M, Gonzalez-Medina D, Hamavid H, Hao Y, Hu G, Jiang G, Kan H, Lopez AD, Phillips MR, She J, Vos T, Wan X, Xu G, Yan LL, Yu C, Zhao Y, Zheng Y, Zou X, Naghavi M, Wang Y, Murray CJ, Yang G, Liang X: Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet 2016; 387: 251–72 [DOI] [PubMed] [Google Scholar]
- 38.Bruce AJ, Ritchie CW, Blizard R, Lai R, Raven P: The incidence of delirium associated with orthopedic surgery: a meta-analytic review. Int Psychogeriatr 2007; 19: 197–214 [DOI] [PubMed] [Google Scholar]
- 39.Bitsch M, Foss N, Kristensen B, Kehlet H: Pathogenesis of and management strategies for postoperative delirium after hip fracture: A review. Acta Orthop Scand 2004; 75: 378–89 [DOI] [PubMed] [Google Scholar]
- 40.Rudolph JL, Inouye SK, Jones RN, Yang FM, Fong TG, Levkoff SE, Marcantonio ER: Delirium: an independent predictor of functional decline after cardiac surgery. J Am Geriatr Soc 2010; 58: 643–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wijeysundera DN, Pearse RM, Shulman MA, Abbott TEF, Torres E, Ambosta A, Croal BL, Granton JT, Thorpe KE, Grocott MPW, Farrington C, Myles PS, Cuthbertson BH; METS study investigators: Assessment of functional capacity before major non-cardiac surgery: an international, prospective cohort study. Lancet 2018; 391: 2631–40 [DOI] [PubMed] [Google Scholar]
- 42.Lundstrom M, Edlund A, Bucht G, Karlsson S, Gustafson Y: Dementia after delirium in patients with femoral neck fractures. J Am Geriatr Soc 2003; 51: 1002–6 [DOI] [PubMed] [Google Scholar]
- 43.Lee H, Oh SY, Yu JH, Kim J, Yoon S, Ryu HG: Risk factors of postoperative delirium in the intensive care unit after liver transplantation. World J Surg 2018; 42: 2992–99 [DOI] [PubMed] [Google Scholar]
- 44.Dokkedal U, Hansen TG, Rasmussen LS, Mengel-From J, Christensen K: Cognitive functioning after surgery in middle-aged and elderly Danish twins. Anesthesiology 2016; 124: 312–21 [DOI] [PMC free article] [PubMed] [Google Scholar]