Abstract
This study was a secondary analysis of LaFreniere and Newman (2016), a randomized controlled trial comparing two ecological momentary interventions (EMIs) for generalized anxiety disorder (GAD): The worry outcome journal (WOJ) and thought log (TL). We predicted that higher thought-related distress would be a mediator by which higher uncontrollability beliefs (UB) would hinder the efficacy of the WOJ, but not the TL. Fifty-one undergraduates who met GAD criteria underwent one of the EMIs for 10 days. WOJ users tracked worries, associated distress, interference, expected outcome probabilities, and whether their worries came true four times/day. TL users tracked general thoughts, associated distress, and interference four times/day. Bootstrapping path analysis was used to analyze moderated mediation models. Higher UB predicted higher thought-related distress for both EMIs. Higher UB also predicted reduced efficacy of the WOJ at post-trial and of both EMIs at 30-day follow-up. However, for WOJ users, when higher initial UB levels predicted higher thought-related distress early in treatment, participants reported greater levels of worry at post-trial and follow-up. In contrast, UB’s effect on the TL group at post-trial and follow-up was not mediated by early distress. Thought-related distress appears to be a mechanism by which UB impedes the WOJ intervention.
Keywords: generalized anxiety disorder, GAD, worry, distress, uncontrollability beliefs, contrast avoidance, worry outcome monitoring, ecological momentary interventions
1. The Impact of Uncontrollability Beliefs and Thought-Related Distress on Ecological Momentary Interventions for Generalized Anxiety Disorder: A Moderated Mediation Model
1.1. Higher Uncontrollability Beliefs May Hinder Efficacy
The impact of beliefs on experience has been an important theoretical factor since the beginning of cognitive therapy (Ellis, 1962). Without accounting for the influence of appraisal, behavior and emotion are imperfectly understood. The same is true for beliefs about cognition, or “meta-cognition.” These beliefs can influence the frequency and intensity of thoughts (van der Heiden, 2013; Wells, 1995) as well as the distress those thoughts can create (McEvoy, Erceg-Hurn, Anderson, Campbell, & Nathan, 2015). Meta-cognition is especially relevant for generalized anxiety disorder (GAD). Although primarily defined by worry, GAD is linked to meta-cognitive beliefs about worry as well (Wells, 2010).
One prominent meta-cognition in GAD is a lack of belief in one’s ability to control thought. Worry uncontrollability is itself a central criterion for GAD diagnosis (American Psychiatric Association, 2013). Furthermore, Wells’ (2010; 1995) metacognitive theory suggests that those with GAD believe that they cannot control the onset, frequency, and/or force of their worry, maintaining symptoms (Cartwright-Hatton & Wells, 1997). In both cross-sectional and experimental studies, uncontrollability beliefs (UB) differentiated those with GAD from subsyndromal worriers (Hirsch, Mathews, Lequertier, Perman, & Hayes, 2013; Ruscio & Borkovec, 2004; Wetherell, Le Roux, & Gatz, 2003), those with other anxiety disorders (Hoyer, Becker, & Roth, 2001; Wells & Carter, 2001), and non-anxious controls (Abel & Borkovec, 1995; Brown, 1997; Hoyer et al., 2001; Wells & Carter, 2001; Wetherell et al., 2003). In some studies, uncontrollability was found to be the only distinct phenomenon among persons with GAD compared to others (Craske, Rapee, Jackel, & Barlow, 1989; Ruscio & Borkovec, 2004). After controlling for excessiveness of worry, UB also explained additional variance in GAD severity, comorbid disorder amount and severity, and treatment use (Hallion & Ruscio, 2013). Moreover, in longitudinal studies, UB predicted daily worry above and beyond trait worry and intolerance of uncertainty (Thielsch, Andor, & Ehring, 2015) and changes in UB across treatment predicted concurrent changes in repetitive negative thinking (McEvoy et al., 2015). Despite recurrent theorization that these beliefs are critical factors that may maintain the disorder (Ruscio & Borkovec, 2004; Wells, 1999; Wells & King, 2006; Wells, 1995), no studies have included them as predictors of GAD symptom severity after treatment. The current study aimed to test whether UB predicted the outcome of a randomized controlled trial (RCT) comparing two ecological momentary interventions (EMIs), the Worry Outcome Journal (WOJ) and the Thought Log (TL).
In the WOJ condition of this RCT, clients recorded their worries, worry-associated distress and interference, and estimated probabilities of outcome when prompted. They then tracked and noted the actual outcomes of their worries. Yet in the TL condition, participants simply recorded any thoughts—worrisome or not—and rated the distress and interference created by those thoughts. TL users did not track worry outcomes. Both interventions reduced worry, yet the WOJ led to significantly greater reductions of worry than the TL after only ten days of use, as well as remission of over half of GAD cases (LaFreniere & Newman, 2016). Like most GAD treatments, both of these cognitive interventions were aimed at increasing worry control. Thus, greater beliefs that thought is uncontrollable could directly interfere with their efficacies. Yet specifically for the WOJ condition, UB could also reduce efficacy by increasing the distress brought on by worries.
1.2. UB May Increase Thought-Related Distress
Worry-related distress is a possible mechanism by which UB may impede the processes of the WOJ intervention, predicting worse outcome. Several authors propose that having stronger UB leads to experiencing stronger distress (Ruscio & Borkovec, 2004; Wells & Carter, 2001). Theory has suggested several reasons why this may be true. According to Wells (1999), the belief that one cannot control worry may facilitate "worry about worry", leading to higher distress. The construct of UB also includes the belief that lack of thought control is dangerous, which may make unrestrainable worry more upsetting. UB may also induce additional distress through feelings of helplessness when worry control feels fruitless (Heide & Borkovec, 1984; Seligman, 1975). If UB leads worriers to forgo attempts at controlling worry, they never disconfirm their UB. Thus, the cycle of UB, worry, and distress would continue, even in treatment.
1.3. Worry-Related Distress May Worsen WOJ Outcome
According to a variety of theoretical rationales, worry-related distress may interfere with optimal WOJ efficacy. If enough distress is present, the outcome tracking function of the WOJ may fuel continued worry, instead of refuting worry’s benefits. Higher worry-related distress from UB may enable a function of worry known as contrast avoidance. The contrast avoidance theory proposes that individuals with GAD worry to increase and sustain distress in order to lessen undesirable shifts toward negative emotion (Newman & Llera, 2011). It is the only worry theory that identifies worry distress as serving a function valued by clients—one that promotes worry. Worry’s capacity to lessen spikes in negative emotion by increasing distress has been supported experimentally (Llera & Newman, 2010) and in diary studies (Crouch, Lewis, Erickson, & Newman, 2017; Newman et al., in press). In addition, those with GAD (versus those without GAD) have reported a preference for using worry to cope with shifts in upsetting feelings by creating distress (Llera & Newman, 2014, 2017). Following from this theory, higher worry-created distress actually promotes worry, because it increases worry’s power to lessen emotional contrasts. Higher worry-related distress also leads to greater negative reinforcement of worry when worries do not come true. Thus, higher thought-related distress may be key to worry maintenance for those with higher UB, even when undergoing WOJ treatment. If worries are creating enough distress to prevent unwanted emotional contrasts—worry’s valued function—it may not matter whether WOJ tracking shows clients their worries are untrue and interfering. This may be particularly true for those with higher UB, who are less likely to attempt worry control than those with lower UB.
In addition to facilitating greater contrast avoidance, higher distress may also make it more difficult for clients to attend to the favorable non-occurrence of their worry outcomes. Those with GAD have an attentional bias toward negativity (Bar-Haim, Lamy, Pergamin, Bakermans-Kranenburg, & van IJzendoorn, 2007), which may steer them away from noting or dwelling on positive outcomes. They are also significantly distracted by irrelevant threat content when trying to attend to other, non-threatening information (Mathews & MacLeod, 1985) and have difficulty controlling cognition to switch between information types (Tempesta et al., 2013). Higher distress may exacerbate threat biases, drawing attention away from non-outcomes.
Distress may also interfere with WOJ treatment by enhancing worry reinforcement. Cycles of negative reinforcement are thought to maintain worry. In these cycles, worry-created distress is relieved by the non-occurrence of unrealistic predicted outcomes. Borkovec, Hazlett-Stevens, and Diaz (1999) reported that 85% of GAD client worries did not come true. In fact, the WOJ trial itself found that 91.4% of GAD participant worries never actualized (LaFreniere & Newman, 2018). In addition, Newman et al. (in press) found that heightened negative affect in worry either 1) diminished the likelihood of experiencing increased negative emotion or 2) increased the probability of experiencing reduced negative emotion in the next hour. If the nonoccurrence of feared outcomes is especially reinforcing, tracking non-outcomes of worry may strengthen worry rather than highlighting its fruitlessness. This may be particularly true for those with less belief in their worry control. In summary, UB may predict lower reductions in worry during and after WOJ treatment through increasing thought-related distress early in therapy.
1.4. UB’s Distress Mediation May Be Moderated by EMI Type
Following from these rationales, one should expect differences in how thought-related distress functions in the WOJ and TL interventions. The WOJ tracked worries, their associated distress, and their outcomes. Yet the TL recorded any thoughts and their associated distress, but not outcomes. Given that the WOJ depends on outcomes, the above rationales suggest higher distress would lead to greater contrast avoidance when worries do come true, greater negative reinforcement of worry when they do not come true, and greater distraction from attending to non-outcomes of worry. Since these distress-dependent processes require outcome tracking, they are unrelated to the TL. Thus, by tracking outcomes, the WOJ’s effects should be more hindered by higher distress associated with UB than that of the TL. Stated differently, distress’ prediction of treatment success and mediation of UB’s impact should be moderated by treatment condition.
The current study contributes to the literature by highlighting new factors that may impede therapy. Furthermore, it provides a longitudinal test of the impact of UB and thought-related distress on treatment for the first time. In addition, it also seeks to address whether Well’s prediction that UB increases worry-related distress is accurate. In a secondary analysis of LaFreniere and Newman’s (2016) trial data, we employed bootstrapping path analysis (Preacher & Hayes, 2008) to test whether early thought-related distress as a mediator was moderated by condition (WOJ or TL). For the WOJ group, we hypothesized that those with GAD who reported higher UB pre-trial would have higher levels of worry at post-trial and follow-up due to higher levels of early thought-related distress. Yet for the TL, we hypothesized that mediation by thought-related distress would not occur, though UB would still predict outcome. This prediction was based on the rationale that thought-related distress would garner greater attention toward contrast avoidance and negative reinforcement in those who tracked worry outcomes, as opposed to the TL group, which did not track worries or outcomes. Accordingly, in between-group model comparisons we hypothesized that the path from distress to post-trial and follow-up worry and the residual direct effect of UB to post-trial and follow-up worry would differ between groups.
2. Method
The current study draws on data from LaFreniere and Newman’s (2016) randomized controlled trial comparison of the Worry Outcome Journal (WOJ) and the Thought Log (TL). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
2.1. Participants
Fifty-one undergraduate students, 43 females and 8 males, participated. Participants met full DSM-IV criteria for GAD as assessed by the Generalized Anxiety Disorder Questionnaire for DSM-IV (GAD-Q-IV; Newman et al., 2002), which are the same as DSM-5 (American Psychiatric Association, 2013). Inclusion criteria included speaking English and being over 18 years of age. We also required participants to complete 80% or more WOJ entries at a 2nd-day compliance check, which all did. Ethnicity was 76.5% White, 7.8% Asian, 5.9% Black, 3.9% Hispanic, 2% Middle Eastern, and 3.9% other. One participant dropped out due to discomfort with recording worries. She reported no harm, but was informed of therapy options nonetheless.
2.2. Self-Report Outcome Measures
The Penn State Worry Questionnaire (PSWQ).
(Meyer, Miller, Metzger, & Borkovec, 1990). The PSWQ served as the primary outcome measure. This 16-item self-report measure assesses the severity and frequency of worry. Responses are rated on a 5-point Likert scale ranging from “not at all typical” to “very typical.” Meyer et al. (1990) determined that the PSWQ has an internal consistency coefficient of .91 and high retest reliability (r = 0.92). It also exhibits sensitivity to psychotherapeutic change. Furthermore, the PSWQ discriminates persons with GAD from those who meet criteria for other anxiety disorders. (Brown, Antony, & Barlow, 1992; Meyer et al., 1990).
The Generalized Anxiety Disorder Questionnaire for DSM-IV
(GAD-Q-IV; Newman et al., 2002). The GAD-Q-IV was used both to select participants for the study. The GAD-Q-IV is a 9-item self-report measure designed to assess the degree of GAD symptoms as defined by the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; APA, 1994). The GAD-Q-IV is the only self-report measure that evaluates all DSM GAD symptoms (Rodebaugh, Holaway, & Heimberg, 2008). The measure can be scored based on diagnostic criteria, a function used to select the GAD sample (Moore, Anderson, Barnes, Haigh, & Fresco, 2013; Newman et al., 2002). Its internal consistency is robust (Cronbach’s alpha = .94; Newman et al., 2002) and it has shown sufficient retest reliability in clinical classification over a two week period (92% of the sample; Newman et al., 2002). It has also demonstrated convergent validity with measures of worry and discriminant validity against measures of social anxiety and panic disorder. Rates of kappa agreement between the GAD-Q-IV and the Anxiety Disorders Interview Schedule (ADIS) are good as well (κ = .67). PSWQ scores of undergraduates identified as having GAD with the GAD-Q-IV were also not significantly different from baseline PSWQ scores in a treatment seeking community sample (see Newman et al., 2002). Furthermore, in a primary care therapy-seeking sample, criterion scoring was the optimal strategy for identifying GAD (with a sensitivity of .89 and specificity of .82; Moore, Anderson, Barnes, Haigh, & Fresco, 2014).
The Meta-Cognitions Questionnaire
(MCQ; Cartwright-Hatton & Wells, 1997). The MCQ was used to capture baseline UB. The total measure uses a 65-item, 4-point response scale and is composed of five subscales. However, the interests of the current study were limited to the Uncontrollability of Thoughts and Corresponding Danger scale, hereafter referred to as UB. Cronbach’s alpha for this subscale is .89, its retest correlation is adequate (r = .89), and it has been shown to be distinct from all other MCQ factors (Cartwright-Hatton & Wells, 1997).
2.3. Procedure
An institutional review board approved this study. An online subject pool screening identified university students who met criteria for GAD based on criterion scoring of the GAD-Q-IV. Qualifying students were invited to participate in the study through a mass email. Those wishing to enroll were randomly assigned to either the WOJ or the TL.
Participants first presented at the research facility and completed the PSWQ, the GAD-Q-IV, and the MCQ. They then underwent a 30-minute training session wherein study personnel read from a script as participants followed along. Participants in both conditions were given a treatment rationale to replicate actual cognitive-behavioral clinical practice and to control for treatment expectancy. The rationale for the WOJ suggested that attending to worry costs (such as high distress and interference) alongside tracking the non-occurrence of outcomes may reduce worries and anxiety by showing worries are not worthwhile. The rationale for the TL condition suggested that research shows self-awareness of thoughts and behaviors can change thinking and action for the better, which may reduce worries and anxiety (see LaFreniere & Newman, 2016). For the WOJ group, the training then defined worry for participants, describing it as “a repetitive anxious thought that an event in the future will turn out badly … apprehensive expectation … repetitive and hard to control in your mind.” They were given several examples. Participants were also instructed that “a worry is not just a fleeting concern about the future,” but rather must “forecast a negative outcome.” They were then provided examples of thoughts that were not worries. They were asked to only record specific, concrete, testable worries that they could be sure either came true or did not come true within the 30 days of the study; they were given examples of both ideal and improper entries. WOJ users were also taught how to track outcomes. Next, both groups were taught how to complete journal ratings and how to use the online system. Lastly, they were given the chance to ask questions, as well as contact information for any later inquiries. The entire session script was included in the initial pages of each WOJ and TL for participants’ reference.
The next morning participants began making prompted entries using a commercial mass texting service. For ten days they recorded worries or thoughts in their paper journals when prompted randomly (four times/day within four timeframes: Morning 8:00 AM-12:00 PM, early afternoon 12:00-3:00 PM, late afternoon 3:00-6:00 PM, and evening 6:00-9:00 PM) by text message on their personal mobile phone. They were permitted to make additional entries at any time, but were required to record at least one at the prompted time. Recorded worries or thoughts must have occurred within the two hours prior to the prompt. For each recorded entry, they also noted the prompt time and date.
For WOJ-recorded worries, participants noted their specific, testable predictions about the future. Next, they rated the degree of distress caused on a scale of 1 (no distress) to 7 (severe distress) and their best estimate answering the question, “How much time did that worry take up since I first had the worry?” (these were considered the “costs” of worry). After completing these present-moment cost ratings, they gave two probability estimates with respect to the worry outcome. First, they rated how likely they felt that the feared outcome would occur, according to their “gut feelings or intuition.” Next, they rated how likely “a person would logically conclude the worried outcome would occur if they were thinking as realistically as possible.” They were strongly encouraged to record a worry immediately when prompted, but if they had not experienced a worry since the last prompt time, they were allowed to write “No worry.”
For TL users, upon prompting they wrote a single thought from the past two hours and rated any distress and thinking time associated with it. They were instructed to log “any kind of thought [they] would like, no matter what it is.” They then rated the distress associated with the thought from 1 to 7 and the percent of total thinking time spent on that thought since it began.
After a day’s worth of prompts, each night at 10:00 PM participants recorded the content of their paper records into an online survey via PsychData. For both groups this included first entering all content from their day’s recordings, then reviewing the entirety of their journals. They also recorded the percentage of thinking time spent on each specific worry or thought across the entire day. After reviewing their journals at the end of the nightly survey, only WOJ participants recorded if any worries led to an outcome and if so, if their feared outcome came true. They also rated if the outcome was “as bad as, worse than, or better than expected”. They could note these outcomes in their paper journals at any time, but outcomes were also recorded online at the nightly review.
After two days of recording and online entry, participants received a phone call to check compliance rates. They were asked the total number of paper and online entries made and were assessed for any study-related harm. They were required to complete at least 80% of their entries by this time or they were eliminated from the study. No participant had a compliance rate below 80%. Consequently, no one was removed from the study due to low compliance.
The day after the ten-day intervention period they completed the PSWQ, the GAD-Q-IV, and MCQ via PsychData. Participants then returned their paper records to the lab within three days. Twenty days after the final day of worry recording they were provided the entire content of their journals electronically. They were again asked to review each entry. For WOJ users, if any worries came true in the past 20 days, they wrote whether the worries turned out as bad as, worse than, or better than expected. They then completed the three outcome measures once again. Lastly, participants were compensated with course-specific research participation credit.
2.4. Planned Statistical Analyses
Statistical analyses utilized Mplus 7 software. The early thought distress variable was based on the average of each participant’s distress ratings across the first two days of the trial (the mean of eight ratings). This was meant to capture average thought-related distress prior to treatment’s effect, but after baseline assessment. We conducted a paired samples t-test comparing average worry distress on day one and average worry distress on day two to verify this lack of change. We also ran an independent samples t-test to test whether the average early level of distress for WOJ entries was higher than that for TL entries.
For the primary analyses we employed bootstrapping regression-based path analysis (Preacher & Hayes, 2008). 4.9% of values were missing overall with 11.8% missingness at follow-up, likely due to participant non-compliance. Consequently, we used Full-Information Maximum Likelihood (FIML) estimation with the MPlus ML estimator. We employed identical analyses for two models, one including post-trial worry as outcome and one including follow-up worry. These analyses examined whether treatment condition moderated a hypothesized mediation model where uncontrollability beliefs at baseline predicting PSWQ worry at post-trial or follow-up were each mediated by early thought-related distress. To test whether specific beta paths differed between groups, we ran a series of two-group models each with greater constraints, including our hypothesized model, and compared them using chi-square significance tests. Final models were selected based on best fit. This procedure was done for both the posttrial and follow-up worry models. We then directly compared the indirect effects of the aforementioned mediation models between the WOJ and TL groups using MPlus’ MODEL CONSTRAINT command, which provides a z-test with bootstrap confidence intervals (Muthén & Muthén, 2012). Lastly, we examined the significance of each path by group in the final models. We report unstandardized coefficients for path betas. Cohen’s d effect sizes were calculated by the formula d = B/(√(n)*SE). In the rare case that determination of significance by p-values contradicted that of bootstrap confidence intervals, we deferred to the conclusion of the confidence intervals—a more powerful test (Hayes, 2009).
3. Results
3.1. Descriptive Analyses
See Table 1 for means and standard deviations by condition on all variables. There were no between-group pretreatment differences in the UB scale (F(2, 49) = 0.654, p = .422, ηp2 = 0.013) nor the PSWQ (F(2, 49) = 0.225, P = .637, ηp2 = 0.005). Average thought-related distress on day one did not differ from average worry distress on day two in either sample (WOJ users: t(28) = 0.261, p = 0.796, d = .055; TL users: t(20) = 0.392, p = 0.700, d = .097).
Table 1.
Descriptive information on measures at pre-assessment (Pre), post-assessment (Post), and follow-up and early thought-related distress
| Pre | Initial 2 Day Average |
Post | Follow- Up |
||
|---|---|---|---|---|---|
| M (SD) |
M (SD) |
M (SD) |
M (SD) |
||
| MCQ Uncontrollability Beliefs | WOJ | 45.758 (9.804) |
-- | 41.902 (9.585) |
39.592 (11.615) |
| Control | 48.000 (9.793) |
-- | 45.109 (8.790) |
44.379 (9.945) |
|
| Thought-Related Distress | WOJ | -- | 4.51 (1.49) |
-- | -- |
| Control | -- | 3.47 (1.91) |
-- | -- | |
| PSWQ | WOJ | 67.206 (6.450) |
-- | 60.417 (8.21) |
59.382 (10.710) |
| Control | 66.136 (9.657) |
-- | 64.080 (9.752) |
62.297 (11.309) |
3.2. Model Selection
Post-trial Model:
The first two-group post-trial model was fully saturated with all beta relationships unconstrained between groups. When all pathways were constrained to be equal between groups except for the hypothesized paths (thought-related distress predicting post-trial worry and the residual direct effect path of uncontrollability predicting post-trial worry), the model fit was very good (χ2(1) = 0.001, p = .970; CFI = 1.00; TLI = 1.25; RMSEA = 0.00). The latter model’s fit was not significantly different from that of the first (χ2diff = 0.001, p = .975). Thus, we were justified in conducting a comparison of the hypothesized model against a fully constrained model. When all beta relationships were constrained to be equal, the model fit was not significant (χ2(3) = 6.266, p = .099). A second model freeing the predictive path of distress had a significantly better fit than the fully-constrained model (χ2diff(2) = 6.265, pdiff = .044). This significant difference confirmed that the paths from distress to post-trial worry and uncontrollability to post-trial worry differed significantly between WOJ and TL users. Thus, a model constraining all paths except these paths was chosen as the final post-trial model.
Follow-up Model:
The first two-group follow-up model was fully saturated with all beta relationships unconstrained between groups. When all pathways were constrained to be equal between groups except the hypothesized paths (thought-related distress predicting follow-up worry and the residual direct effect path of uncontrollability predicting follow-up worry), the model fit was very good (χ2(1) = 0.001, p = .970; CFI = 1.00; TLI = 1.17; RMSEA = 0.00). The latter model’s fit was not significantly different from that of the first (χ2diff = 0.001, p = .975). Thus, we were justified in conducting a comparison of the hypothesized model against a fully constrained model. When all beta relationships were constrained to be equal the model fit was not significant (χ2(3) = 6.277, p = .099). A second model freeing the predictive path of distress had a significantly better fit than the fully-constrained model (χ2diff(2) = 6.276, pdiff = .043). This significant difference demonstrates that the paths from distress to follow-up worry and uncontrollability to follow-up worry differed significantly between WOJ and TL users. Thus, a model constraining all paths except these four paths was chosen as the final follow-up model.
3.3. Moderation of Indirect Effects Between Interventions
Post-trial Model:
Indirect effects of higher thought-related distress mediating the relationship between higher uncontrollability and higher post-trial symptoms were significantly different between WOJ and TL users (a1b1-a2b2 = −0.301, p = 0.024, bootstrap CI = [−0.628, −0.087], d = −0.317). According to a 95% bias-corrected bootstrap confidence interval, the indirect effect of uncontrollability beliefs on post-trial worry through higher distress in the WOJ group was statistically different from zero (ab = 0.188, p = .047, bootstrap CI = [0.033, 0.414], d = 0.367). Yet within the TL group, the indirect effect of this mediation path was not significant (ab = −0.112, p = .170, bootstrap CI = [−0.326, 0.011], d = −0.291). Whereas higher uncontrollability beliefs pre-trial and higher worry post-trial was mediated by higher levels of thought-related distress in the WOJ group, it was not mediated by distress for the TL group.
Follow-up Model:
The indirect effect of distress mediating the path from uncontrollability to follow-up worry was also significantly different between WOJ and TL users (a1b1-a2b2 = −0.308, p = .044, bootstrap CI = [−0.654, −0.042], d = −0.284). The indirect effect of this mediation path was significant in the WOJ group (ab = 0.317, p = .005, CI = [0.092, 0.538], d = 0.526), but was not significant in the TL group (ab = 0.009, p = .931, bootstrap CI = [−0.191, 0.227], d = 0.019). As predicted, the positive relationship between UB and follow-up worry was mediated by higher thought-related distress for the WOJ group, but not for the TL group.
3.4. Final Model Path Analyses
Post-trial Model:
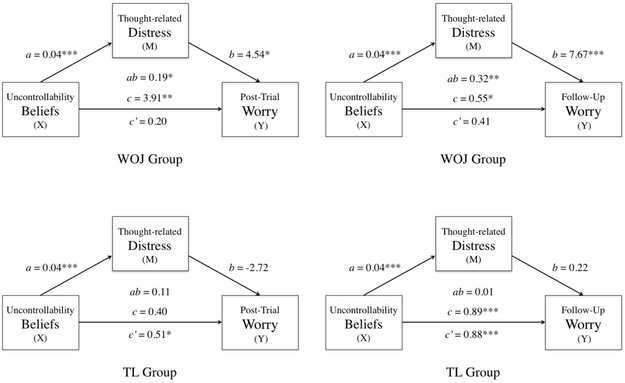
The coefficients (a, b, c, and c’) represent unstandardized regression coefficients for each respective model path (Figure 1). There was a significant total effect where higher uncontrollability beliefs pre-trial predicted higher worry post-trial for the WOJ group (c = 3.91, p = .004, bootstrap CI = [0.157, 0.695], d = 0.526). Yet in contrast to predictions, this same total effect was not significant at post-test for the TL group (c = 0.395, p = .091, bootstrap CI = [−0.125, 0.801], d = 0.360). Note that a significant total effect is not necessary for statistically significant, theoretically meaningful mediation effects (Hayes & Rockwood, 2017). Since the uncontrollability to distress path in the final model was constrained to be equal between groups, only one beta relationship is reported for the path from predictor to mediator. In both groups, higher pre-trial UB significantly predicted higher thought-related distress (a = 0.041, p < .001, bootstrap CI = [0.021, 0.062], d = 0.574). Lastly, as expected, higher thought-related distress significantly predicted higher post-trial worry in the WOJ group (b = 4.543, p = 0.042, bootstrap CI = [0.741, 9.626], d = 0.378), but did not in the TL group (b = −2.722, p = .147, bootstrap CI = [−6.900, 0.711], d = −0.310). Recall that the same pattern of significance emerged regarding indirect effects, supporting the hypothesized model.
Figure 1.
Conceptual diagram of post-trial (left) and follow-up (right) mediation models for both WOJ (top) and TL users (bottom). Regression coefficients: a = effect of X on M, b = effect of M on Y, ab = indirect effect, c’ = direct effect of X on Y (with M included in the model), c = total effect of X on Y (with M not included in the model). *p < .05; **p<.01; ***p<.001.
The residual direct effect path from uncontrollability to worry was also freed. For the WOJ group, the residual direct effect of uncontrollability predicting post-trial worry was not significant (c’ = 0.204, p = .186, bootstrap CI = [−0.099, 0.508], d = 0.246). Traditionally, a significant total effect, significant indirect effect, and non-significant residual direct effect, as found in the WOJ group, suggests complete mediation. The residual direct effect of post-trial worry regressed on uncontrollability was also not significant for the TL group, according to its bootstrap confidence interval (c’ = 0.508, p = .042, bootstrap CI = [−0.056, 0.928], d = 0.433).
Follow-up Model:
As hypothesized, there was a significant total effect where higher uncontrollability beliefs at baseline predicted higher worry at follow-up for both the WOJ (c = 0.545,p = .052, bootstrap CI = [0.122, 1.120], d = 0.361) and TL group (c = 0.887, p < .001, bootstrap CI = [0.429, 1.239], d = 0.941). Again, the constrained path where higher pre-trial uncontrollability predicted higher distress was significant in both groups (a = 0.041, p < .001, bootstrap CI = [0.021, 0.062], d = 0.574). Also as hypothesized, distress significantly predicted follow-up worry for WOJ users (b = 7.669 , p = .001, bootstrap CI = [1.815, 12.128], d = 0.598), but not for TL users (b = 0.216, p = .930, bootstrap CI = [−4.536, 5.259], d = 0.019). For the WOJ group, the residual direct effect of UB predicting follow-up worry was not significant (c’ = 0.228, p = .409, bootstrap CI = [−0.269, 0.750], d = 0.153). Yet this path was significant for the TL group (c’ = 0.878, p < .001, bootstrap CI = [0.365, 1.341], d = 0.755). See Figure 1.
4. Discussion
Although many studies have established a link between worry uncontrollability beliefs (UB) and GAD, none have examined the means by which such beliefs may interfere with treatment. The metacognitive model of worry proposes that uncontrollability beliefs facilitate thought-related distress and symptom severity. The contrast avoidance theory of worry marks thought-induced distress as a crucial factor in GAD maintenance, promoting symptoms. However, such distress has not been examined in the context of treatment outcome. The current study used moderated mediation analysis via bootstrapping on data from a randomized controlled trial of two ecological momentary interventions (EMIs). We predicted that the Worry Outcome Journal (WOJ) condition would show an association between higher uncontrollability beliefs (UB) at baseline and higher worry at post-trial and follow-up. We also predicted these paths would be mediated by greater thought-related distress early in the trial. Yet we expected that such mediation would not occur in a basic thought monitoring conditioning (TL), since the TL did not focus on worry and did not track worry outcomes. These hypotheses were fully supported. In the WOJ group, higher uncontrollability of worry at baseline predicted higher levels of worry both immediately after treatment and at 30-day follow-up. The mechanism of this hindering effect was higher levels of thought-related distress early in treatment. In contrast, although uncontrollability beliefs did predict outcome at follow-up for the TL group, its effect at post-trial and follow-up was not mediated by thought-related distress.
Those with higher uncontrollability beliefs may respond less well to worry outcome monitoring and other GAD interventions. As the metacognitive model would suggest, higher uncontrollability beliefs prospectively predicted greater distress and worse follow-up outcome for both WOJ and TL users. These results replicate and extend previous findings regarding the positive relation between uncontrollability and thought-related distress. They support Wells’ prediction that higher UB is associated with higher worry distress. It is possible that uncontrollability beliefs arise when a person begins worrying, amplifying the distress created by the initial worry. This phenomenon may be especially true when those with GAD wish to cut their worry short—a desire one would expect from those engaging in a worry intervention. When a person believes that worry is interfering and that efforts to stop it will be useless, a primary worry may trigger secondary meta-worries to intensify distress (Wells, 1999). This dilemma may eventually lead to a further distressing experience of learned helplessness (Seligman, 1975). When clients experience distressing worries and believe that nothing can be done about them, they may forgo the opportunity to disconfirm their beliefs. Even if clients do attempt control, they may opt for thought control strategies that only increase distress and have no effect (or even an enhancing effect) on their worry. Coles and Heimberg (2005) found that those with GAD reported significantly higher levels of self-punishment strategies to manage thoughts compared to non-anxious controls. These punishment strategies included getting angry with oneself, self-insults, internal verbal reprimands, and inflicting pain to stop thoughts. Such strategies may also increase or sustain the initial distress of the worry with which they are frustrated.
Higher uncontrollability was only a marginally significant predictor of worse treatment outcome for TL users at post-trial, in contrast to hypotheses. This weaker path may have arisen because the treatment effect was significantly stronger for the WOJ than the TL at post-trial in general, but less different between EMIs at follow-up (LaFreniere & Newman, 2016). For TL users, worry scores may not have changed enough from pre- to post-trial for UB to interfere. As for how UB may have hindered therapy, our mediation analyses offer an explanation.
In the WOJ group, thought-related distress early in treatment (and likely prior to treatment’s influence) explained the relationship between uncontrollability and outcome. We theorized that the up-regulation of such distress in the context of tracking worry outcomes serves clients by enhancing contrast avoidance—the softening of unsavory shifts toward negative emotions (Newman & Llera, 2011). When those with high uncontrollability beliefs receive a greater increase in distress from each worry, the maintenance of that distress helps participants evade unwanted drops in affect when their worries come true. This process affords clients a perceived benefit of worrying that is not targeted by outcome monitoring. The WOJ is meant to demonstrate to clients that their worry is of little worth in light of its high level of interference and low likelihood of worries coming true. Yet if GAD clients profit meaningfully from increased contrast avoidance, outcome monitoring may not convince them to lessen their worry. For these clients, worry would be worth its drawbacks. Our results suggest that the WOJ could be improved by adding elements that may target contrast avoidance. Since higher UB and higher distress are associated with worse treatment outcomes, lowering UB and thought-related distress may be one way to make this improvement. One possible improvement to the WOJ could be asking clients to rate their level of control over each worry, or identify times where they could control their thoughts in their nightly recordings. They may receive evidence that their thoughts were not as uncontrollable as they once believed, especially across the course of treatment. The desire to maintain worry-related distress to avoid negative contrasts might be targeted through monitoring of the specific costs of maintaining distress via worry beyond cognitive interference. For example, the WOJ could include monitoring of fatigue, difficulty concentrating, and disrupted sleep, in addition to showing that feared outcomes rarely happen. These changes may help GAD clients realize that costs of creating and maintaining distress outweigh any benefits. Moreover, greater distress from worry may even prevent those with GAD from attending to the outcomes the WOJ means to highlight. Greater distress provokes greater hypervigilance toward threat and away from non-threatening outcomes, as is typical in GAD (Bar-Haim et al., 2007). Higher state levels of anxiety—such as those induced by worries and captured by distress ratings—cause higher levels of threat-biased attention in those with GAD (Broadbent & Broadbent, 1988). Positive events disconfirming worry then stay out of awareness, or leave its focus quickly. Such a process directly counters the intentions of the WOJ.
Furthermore, higher levels of distress allow for greater relief when worries do not come true. Greater relief implies a greater negative reinforcement value for non-aversive outcomes, maintaining chronic worry despite treatment. It appears quite common that worries do not come true for those with GAD (Borkovec et al., 1999; LaFreniere & Newman, 2018). This nonoccurrence of feared outcomes suggests frequent opportunity for negative reinforcement to promote worry—a process that may be especially powerful when worry distress is high.
Whereas uncontrollability beliefs significantly predicted higher early thought-related distress for both EMIs, thought-related distress only served as a mediator for the WOJ group. Why? Distress is theorized to facilitate greater contrast avoidance utility for participants when worry predictions are true, greater negative reinforcement when predictions are false, and less attention to favorable non-outcomes. Yet the TL intervention makes no effort to direct participants to such non-outcomes. Thus, it should be less influenced by distress than the WOJ. It is possible that the monitoring of worry outcomes was a “double-edged sword”: It led to a stronger treatment effect on average for the WOJ, but did not benefit those with higher thought-related distress as much as those with lower distress. Note that the early distress ratings of our models were also taken before treatment could have an impact, as confirmed by our descriptive analyses comparing ratings from day one and day two. Accordingly, these findings are only relevant to typical distress very early in treatment and not its response to treatment over time.
Lowering early thought-related distress may be an important mechanism for successful therapy. Fortunately, there are several ways treatment can meet with goal with cognitive-behavioral techniques that are already well-established. First, clinicians should routinely assess clients’ UB and work to demonstrate that thought management is possible, as is common in CBT for GAD. Worry distress (and thus contrast avoidance, attentional bias, and worry reinforcement) may then be reduced, improving therapy. Specifically, the WOJ may be enhanced by having clients continually rate their actual ability to control worries, eventually showing that they can in fact conquer them with some effort. Beyond worry outcome monitoring, techniques from Wells’ empirically-supported metacognitive therapy (van der Heiden, 2012) were specifically designed to target uncontrollability beliefs and may be useful. In addition, distress induced by each worry may be targeted by having clients conduct relaxation techniques immediately prior to worrying; this may reduce the distress their worry creates long-term through counterconditioning. Clinicians could also devote session time to CBT worry control exercises, first inducing worries and then guiding clients through purposeful means of distracting from it or restructuring it. Moreover, adding stimulus control (designating a single time and place for all client worrying) might also increase belief in one’s worry control ability. Afterwards clinicians could draw the client’s attention to their successful ability to manage worry, disconfirming high UB. This reduction may then lessen each worry’s distress response and cut off the full power of contrast avoidance.
We cannot and do not claim that the negative impact of uncontrollability beliefs on treatment was above and beyond an effect of pathological worry severity at baseline. Our measure of worry uncontrollability beliefs (MCQ UB) includes both the conviction that worry cannot be stopped and beliefs that lack of worry control is consuming and interfering (Cartwright-Hatton & Wells, 1997). Each of these aspects of UB are important aspects of pathological worry in the PSWQ and the diagnosis of GAD. In fact, uncontrollability beliefs were highly correlated (collinear) with PSWQ scores at baseline, as would be expected (r = .64). Thus, controlling for pathological worry at baseline would bias results and likely nullify key parts of uncontrollability beliefs as a predictor, or vice versa. Many statisticians have argued (and empirically demonstrated) that it is not appropriate to control for highly collinear covariates; doing so significantly biases results (larger standard errors, inaccurate model parameterization, decreased power, etc.) and makes interpretations ambiguous (e.g., Graham, 2003). Therefore, rather than suggesting that uncontrollability beliefs are entirely distinct from GAD, our results simply highlight UB’s potential importance within the diagnosis and treatment of GAD.
The current study supports the importance of perceived worry uncontrollability in both the GAD diagnosis and its treatment with longitudinal analysis. Prior to the publication of DSM-5, debate arose concerning the validity of uncontrollability as a criterion for GAD. Despite cross-sectional studies that attempted to show that uncontrollability distinguishes those with GAD from those without (Abel & Borkovec, 1995; Hallion & Ruscio, 2013; Hoyer et al., 2001; Ruscio & Borkovec, 2004; Wells & Carter, 2001; Wetherell et al., 2003), some opposed its criterion status. The opposition argued that uncontrollability is merely a dimensional difference across worriers—one not impactful enough to warrant its requirement for diagnosis (Andrews & Hobbs, 2010; Andrews et al., 2010). In contrast to this notion, the current longitudinal study further supports the idea that uncontrollability beliefs are quite meaningful to GAD: They significantly influence treatment outcome. Our findings offer further evidence that uncontrollability is best kept in the DSM definition. At the very least, it should continue to receive attention in therapy.
The negative effect of uncontrollability beliefs and thought-related distress found here may be present in other cognitive-behavioral treatments as well. Future studies should assess uncontrollability beliefs and distress in GAD treatments of all types and determine whether they are predictors of outcome or influencing factors in process. Furthermore, it would likely be beneficial for researchers to test directly if stronger contrast avoidance tendencies among treatment populations impact therapy. As in the WOJ, many treatments may be missing a chance to address this crucial component of GAD and bring greater well-being for more clients.
It is also of note that this study made predictions based on two models of GAD and how they may work together: The metacognitive model (uncontrollability beliefs are associated with worry distress) and the contrast avoidance model (distress buffers contrasts, impeding treatment effects on worry). To fully understand GAD and improve treatment, future GAD studies may benefit from integrating models of worry function in this way. There are currently many different models, all with evidence (Newman & Llera, 2011). It is perhaps time to see how these models may coincide with one another to create the complex and multi-faceted construct that is GAD.
As with any study, the current project could have been improved. Regarding limitations, the current trial was quite short at only ten days. It would be important to replicate our effects within a trial timeframe that resembles the length of actual clinical practice. The length of follow-up also had a short duration. Though the mediation model used here showed an effect of UB and worry distress twenty days after treatment’s end, longer follow-up times could give a clearer sense of the time range of UB’s effects. The sample size was also small, and participants were largely young and White. An ideal test of UB’s impact should include more participants with a diversity mirroring that seen in real world practice. Unfortunately, we were not able to assess contrast avoidance effects directly in the current study. An improved mediation model would assess the strength of each person’s distress in lessening emotional shifts as a mediator. This would likely require an EMA design recording negative affect both before and concurrent to a negative event. As noted in our discussion of clinical implications, the treatment itself may have been improved by targeting UB and contrast avoidance in some way, perhaps by having clients monitor their worry control ability and detailed costs. Future studies are advised to test such possible improvements not only to the WOJ, but to other interventions as well.
We would also like to note that the current study’s statistical analyses describe relationships in between-person variation. We theorize that those with greater uncontrollability beliefs than others are likely to have both higher worry-related distress than others and worse treatment outcome than others. Yet we also theorize about within-person processes in our conceptualization. For example, we propose that variation in uncontrollability beliefs over time within a person with GAD likely predicts variation in worry-related distress within that person, which, in turn, prevents emotional contrasts to a greater degree, interfering with his or her treatment response. Despite its common use in psychology, we recognize that between-person analyses are a limitation when attempting to address theorized within-person processes (Molenaar, 2004).
Nonetheless, results of this study demonstrated that faith in one’s capacity to control worry and the distress it provokes can make a significant difference in clients’ response to treatment. There may be other unseen factors that reduce the power of therapies, especially if we remain unaware of their influence. When we overlook these impeding elements, we miss out on the crucial goal and merit of all our treatments—further alleviating the distress of those looking for a better, healthier life.
Glossary
- GAD
Generalized Anxiety Disorder
- UB
Uncontrollability Beliefs
- WOJ
Worry Outcome Journal
- TL
Thought Log
Footnotes
Declarations of interest: None
Contributor Information
Lucas S. LaFreniere, Department of Psychology, The Pennsylvania State University
Michelle G. Newman, Department of Psychology, The Pennsylvania State University
5. References
- Abel JL, & Borkovec TD (1995). Generalizability of DSM-III-R generalized anxiety disorders to proposed DSM-IV criteria and cross-validation of proposed changes. Journal of Anxiety Disorders, 9, 303–315. doi: 10.1016/0887-6185(95)00011-C [DOI] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, D.C.: American Psychiatric Association. [Google Scholar]
- American Psychiatric Association, A. P. A. (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM-5; 5th ed.). Arlington, Virginia: American Psychiatric Association. doi: 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Andrews G, & Hobbs MJ (2010). The effect of the draft DSM-5 criteria for GAD on prevalence and severity. Australian and New Zealand Journal of Psychiatry, 44, 784–790. doi: 10.3109/00048671003781798 [DOI] [PubMed] [Google Scholar]
- Andrews G, Hobbs MJ, Borkovec TD, Beesdo K, Craske MG, Heimberg RG, Rapee RM, Ruscio AM, & Stanley MA (2010). Generalized worry disorder: A review of DSM-IV generalized anxiety disorder and options for DSM-V. Depression and Anxiety, 27, 134–147. doi: 10.1002/da.20658 [DOI] [PubMed] [Google Scholar]
- Bar-Haim Y, Lamy D, Pergamin L, Bakermans-Kranenburg MJ, & van IJzendoorn MH (2007). Threat-related attentional bias in anxious and nonanxious individuals: A meta-analytic study. Psychological Bulletin, 133, 1–24. doi: 10.1037/0033-2909.133.1.1 [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Hazlett-Stevens H, & Diaz ML (1999). The role of positive beliefs about worry in generalized anxiety disorder and its treatment. Clinical Psychology & Psychotherapy, 6, 126–138. doi: [DOI] [Google Scholar]
- Broadbent D, & Broadbent M (1988). Anxiety and attentional bias: State and trait. Cognition & Emotion, 2, 165–183. doi: 10.1080/02699938808410922 [DOI] [Google Scholar]
- Brown TA (1997). The nature of generalized anxiety disorder and pathological worry: Current evidence and conceptual models. Canadian Journal of Psychiatry, 42, 817–825. [DOI] [PubMed] [Google Scholar]
- Brown TA, Antony MM, & Barlow DH (1992). Psychometric properties of the Penn State Worry Questionnaire in a clinical anxiety disorders sample. Behaviour Research and Therapy, 30, 33–37. doi: 10.1016/0005-7967(92)90093-V [DOI] [PubMed] [Google Scholar]
- Cartwright-Hatton S, & Wells A (1997). Beliefs about worry and intrusions: The Meta-Cognitions Questionnaire and its correlates. Journal of Anxiety Disorders, 11, 279–296. doi: 10.1016/S0887-6185(97)00011-X [DOI] [PubMed] [Google Scholar]
- Coles ME, & Heimberg RG (2005). Thought Control Strategies in Generalized Anxiety Disorder. Cognitive Therapy and Research, 29, 47–56. doi: 10.1007/s10608-005-1647-x [DOI] [Google Scholar]
- Craske MG, Rapee RM, Jackel L, & Barlow DH (1989). Qualitative dimensions of worry in DSM-III-R generalized anxiety disorder subjects and nonanxious controls. Behaviour Research and Therapy, 27, 397–402. doi: 10.1016/0005-7967(89)90010-7 [DOI] [PubMed] [Google Scholar]
- Crouch TA, Lewis JA, Erickson TM, & Newman MG (2017). Prospective investigation of the contrast avoidance model of generalized anxiety and worry. Behavior Therapy, 48, 544–556. doi: 10.1016/j.beth.2016.10.001 [DOI] [PubMed] [Google Scholar]
- Ellis A (1962). Reason and emotion in psychotherapy. New York: Lyle Stuart. [Google Scholar]
- Graham MH (2003). Confronting multicollinearity in ecological multiple regression. Ecology, 84, 2809–2815. doi: 10.1890/02-3114 [DOI] [Google Scholar]
- Hallion LS, & Ruscio AM (2013). Should uncontrollable worry be removed from the definition of GAD? A test of incremental validity. Journal of Abnormal Psychology, 122, 369–375. doi: 10.1037/a0031731 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millenium. Communication Monographs, 76, 408–420. doi: 10.1080/03637750903310360 [DOI] [Google Scholar]
- Hayes AF, & Rockwood NJ (2017). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy, 98, 39–57. doi: 10.1016/j.brat.2016.11.001 [DOI] [PubMed] [Google Scholar]
- Heide FJ, & Borkovec TD (1984). Relaxation-induced anxiety: Mechanisms and theoretical implications. Behaviour Research and Therapy, 22, 1–12. doi: 10.1016/0005-7967(84)90027-5 [DOI] [PubMed] [Google Scholar]
- Hirsch CR, Mathews A, Lequertier B, Perman G, & Hayes S (2013). Characteristics of worry in generalized anxiety disorder. Journal of Behavior Therapy and Experimental Psychiatry, 44, 388–395. doi: 10.1016/j.jbtep.2013.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoyer J, Becker ES, & Roth WT (2001). Characteristics of worry in GAD patients, social phobics and controls. Depression and Anxiety, 13, 89–96. doi: 10.1002/da.1021 [DOI] [PubMed] [Google Scholar]
- LaFreniere LS, & Newman MG (2016). A brief ecological momentary intervention for generalized anxiety disorder: A randomized controlled trial of the Worry Outcome Journal. Depression & Anxiety, 33, 829–839. doi: 10.1002/da.22507 [DOI] [PubMed] [Google Scholar]
- LaFreniere LS, & Newman MG (2018). Studying smartphone treatment mechanisms with ecological momentary assessment (EMA): Percentage of untrue worries in a generalized anxiety disorder intervention. Paper presented at the Association for Behavioral and Cognitive Therapies Convention 2018, Washington, D.C. [Google Scholar]
- Llera SJ, & Newman MG (2010). Effects of worry on physiological and subjective reactivity to emotional stimuli in generalized anxiety disorder and nonanxious control participants. Emotion, 10, 640–650. doi: 10.1037/a0019351 [DOI] [PubMed] [Google Scholar]
- Llera SJ, & Newman MG (2014). Rethinking the role of worry in generalized anxiety disorder: Evidence supporting a model of Emotional Contrast Avoidance. Behavior Therapy, 45, 283–299. doi: 10.1016/j.beth.2013.12.011 [DOI] [PubMed] [Google Scholar]
- Llera SJ, & Newman MG (2017). Development and validation of two measures of emotional contrast avoidance: The Contrast Avoidance Questionnaires. Journal of Anxiety Disorders, 49, 114–127. doi: 10.1016/j.janxdis.2017.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathews A, & MacLeod C (1985). Selective processing of threat cues in anxiety states. Behaviour Research and Therapy, 23, 563–569. doi: 10.1016/0005-7967(85)90104-4 [DOI] [PubMed] [Google Scholar]
- McEvoy PM, Erceg-Hurn DM, Anderson RA, Campbell BN, & Nathan PR (2015). Mechanisms of change during group metacognitive therapy for repetitive negative thinking in primary and non-primary generalized anxiety disorder. Journal of Anxiety Disorders, 35, 19–26. doi: 10.1016/j.janxdis.2015.07.003 [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, & Borkovec TD (1990). Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy, 28, 487–495. doi: 10.1016/0005-7967(90)90135-6 [DOI] [PubMed] [Google Scholar]
- Molenaar P (2004). A manifesto on psychology as idiographic science: Bringing the person back into scientific psychology, this time forever. Measurement Interdisciplinary Research and Perspectives, 2, 201–218. doi: 10.1207/s15366359mea0204_1 [DOI] [Google Scholar]
- Moore MT, Anderson NL, Barnes JM, Haigh EAP, & Fresco DM (2014). Using the GAD-Q-IV to identify generalized anxiety disorder in psychiatric treatment seeking and primary care medical samples. Journal of Anxiety Disorders, 28, 25–30. doi: 10.1016/j.janxdis.2013.10.009 [DOI] [PubMed] [Google Scholar]
- Moore MT, Anderson NL, Barnes JM, Haigh EA, & Fresco DM (2013). Using the GAD-Q-IV to identify generalized anxiety disorder in psychiatric treatment seeking and primary care medical samples. Journal of Anxiety Disorders, 28, 25–30. doi: 10.1016/j.janxdis.2013.10.009 [DOI] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus User's Guide (7th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Przeworski A, Erickson T, & Cashman-McGrath L (2002). Preliminary reliability and validity of the Generalized Anxiety Disorder Questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy, 33, 215–233. doi: 10.1016/S0005-7894(02)80026-0 [DOI] [Google Scholar]
- Newman MG, Jacobson NC, Zainal NH, Shin KE, Szkodny LE, & Sliwinski MJ (in press). The effects of worry in daily life: An ecological momentary assessment study supporting the tenets of the contrast avoidance model. Clinical Psychological Science. doi: 10.1177/2167702619827019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, & Llera SJ (2011). A novel theory of experiential avoidance in generalized anxiety disorder: A review and synthesis of research supporting a Contrast Avoidance Model of worry. Clinical Psychology Review, 31, 371–382. doi: 10.1016/j.cpr.2011.01.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods, 40, 879–891. doi: 10.3758/BRM.40.3.879 [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Holaway RM, & Heimberg RG (2008). The factor structure and dimensional scoring of the Generalized Anxiety Disorder Questionnaire for DSM-IV. Assessment, 15, 343–350. doi: 10.1177/1073191107312547 [DOI] [PubMed] [Google Scholar]
- Ruscio AM, & Borkovec TD (2004). Experience and appraisal of worry among high worriers with and without generalized anxiety disorder. Behaviour Research and Therapy, 42, 1469–1482. doi: 10.1016/j.brat.2003.10.007 [DOI] [PubMed] [Google Scholar]
- Seligman ME (1975). Helplessness: On depression, development and death. New York: Freeman. [Google Scholar]
- Tempesta D, Mazza M, Serroni N, Moschetta FS, Di Giannantonio M, Ferrara M, & De Berardis D (2013). Neuropsychological functioning in young subjects with generalized anxiety disorder with and without pharmacotherapy. Progress in Neuropsychopharmacology and Biological Psychiatry, 45, 236–241. doi: 10.1016/j.pnpbp.2013.06.006 [DOI] [PubMed] [Google Scholar]
- Thielsch C, Andor T, & Ehring T (2015). Do metacognitions and intolerance of uncertainty predict worry in everyday life? An ecological momentary assessment study. Behavior Therapy, 46, 532–543. doi: 10.1016/j.beth.2015.05.001 [DOI] [PubMed] [Google Scholar]
- van der Heiden C (2012). Randomized controlled trial on the effecdtiveness of metacognitive therapy and intolerance-of-uncertainty therapy for generalized anxiety disorder. Behavior Research and Therapy, 50, 100–109. doi: 10.1016/j.brat.2011.12.005 [DOI] [PubMed] [Google Scholar]
- van der Heiden C (2013). Metacognitions in generalized anxiety disorder: Theoretical and practical perspectives. Expert Review of Neurotherapeutics, 13, 135–141. doi: 10.1586/ern.12.161 [DOI] [PubMed] [Google Scholar]
- Wells A (2010). Metacognitive thoery and therapy for worry and generalized anxiety disorder: Review and status. Journal of Experimental Psychopathology, 1, 133–145. doi: 10.5127/jep.007910 [DOI] [Google Scholar]
- Wells A (1999). A cognitive model of generalized anxiety disorder. Behavior Modification, 23, 526–555. doi: 10.1177/0145445599234002 [DOI] [PubMed] [Google Scholar]
- Wells A, & King P (2006). Metacognitive therapy for generalized anxiety disorder: An open trial. Journal of Behavior Therapy and Experimental Psychiatry, 37, 206–212. doi: 10.1016/j.jbtep.2005.07.002 [DOI] [PubMed] [Google Scholar]
- Wells A (1995). Meta-cognition and worry: A cognitive model of generalized anxiety disorder. Behavioural and Cognitive Psychotherapy, 23, 301–320. doi: 10.1017/S1352465800015836 [DOI] [Google Scholar]
- Wells A, & Carter K (2001). Further tests of a cognitive model of generalized anxiety disorder: Metacognitions and worry in GAD, panic disorder, social phobia, depression, and nonpatients. Behavior therapy, 32, 85–102. doi: 10.1016/S0005-7894(01)80045-9 [DOI] [Google Scholar]
- Wetherell JL, Le Roux H, & Gatz M (2003). DSM-IV criteria for generalized anxiety disorder in older adults: distinguishing the worried from the well. Psychology and Aging, 18, 622–627. doi: 10.1037/0882-7974.18.3.622 [DOI] [PubMed] [Google Scholar]