Abstract
The goal of chronic hepatitis B (CHB) therapy is to improve the patient prognosis through the sustained inhibition of viral replication. However, due to the uncertainty and potentially unlimited duration of the treatment course, nucleus(t)ide analogue (NA) resistance and safety, financial costs and patient compliance, different endpoints of antiviral treatment have been proposed in CHB prevention and treatment guidelines. Different treatment endpoints are closely associated with the safety of drug withdrawal and improvements in prognosis. Antiviral treatment suppresses HBV DNA replication, drug withdrawal leads to relapse, and long-term treatment causes drug safety and resistance issues. Although hepatitis B e antigen seroconversion based on HBV DNA inhibition is considered as “a satisfactory endpoint”, drug withdrawal still leads to high relapse rates. Hepatitis B surface antigen (HBsAg) clearance is the “ideal endpoint” in terms of the safety of drug withdrawal and improvements in prognosis. However, the HBsAg clearance rate is low using the conventional single drug treatment and fixed course regimens. Recently, the application of an “optimized antiviral treatment strategy” has improved the HBsAg clearance rate, and make an “ideal endpoint” possible. This article reviews the different antiviral treatment endpoints in terms of the safety of drug withdrawal, improvements in prognosis and relevant advances.
Keywords: Chronic hepatitis B, Antiviral treatment endpoint, Safety, Prognosis improvement, Hepatitis B surface antigen clearance
Core tip: Different antiviral treatment endpoints have different degrees of improvement in disease prognosis. Hepatitis B surface antigen (HBsAg) clearance has been recommended as an optimal endpoint of antiviral treatment by the latest chronic hepatitis B management guidelines. It can not only lead to safer drug withdrawal but also significantly improves prognosis. However, HBsAg clearance rate is low using the conventional single drug treatment and fixed course regimens. So individualized treatment strategies should be implemented according to the specific conditions of patients. This article reviews the different antiviral treatment endpoints in terms of the safety of drug withdrawal, improvements in prognosis and how to improve HBsAg clearance.
INTRODUCTION
Chronic hepatitis B (CHB) is the main cause of liver cirrhosis and hepatocellular carcinoma (HCC). The annual incidence of liver cirrhosis is 2%-10%[1], and the annual incidences of HCC are 0.5%-1% for patients without liver cirrhosis and 3%-6% for patients with liver cirrhosis[2-4]. The prognosis of patients has improved with the advent of effective antiviral treatment. Currently, the goal of CHB antiviral treatment is to alleviate liver inflammation and necrosis and reduce the incidences of liver cirrhosis, HCC, and other complications through maximal and long-term inhibition of HBV replication[5]. Covalently closed circular DNA (cccDNA) is a replication template of HBV. It can transcribe 3.5 kb, 2.4 kb, 2.1 kb and 0.7 kb mRNA, of which 3.5 kb is pre-genomic RNA (pgRNA), which can reverse transcribe into DNA. At present, antiviral drugs can not directly act on cccDNA, which makes it difficult to eradicate. Therefore, long-term or even indefinite drug maintenance therapy is needed. Considering issues of drug safety, financial costs and patients’ desire for drug withdrawal, the major guidelines in China and other countries have proposed different antiviral treatment endpoints based on these considerations[5-8]. However, currently, a large number of studies have confirmed that the safety of drug withdrawal and improvements in prognosis for different treatment endpoints are different.
Previous studies mainly focus on improving the hepatitis B e antigen (HBeAg) seroconversion rate based on HBV DNA inhibition to achieve drug withdrawal and reduce relapse. Guidelines, including Guidelines for the prevention and treatment of chronic hepatitis B: A 2015 update[5] by the Chinese Society of Hepatology and Chinese Society of Infectious Diseases, still propose to extend antiviral and consolidating treatments to reduce relapse after drug withdrawal. However, extending treatment fails to fundamentally solve the problem, and patients still have a high relapse rate after drug withdrawal. In a study by Chaung et al[9], 39 patients achieved HBeAg seroconversion after nucleos(t)ide analogue (NA) treatment and were subsequently treated with a consolidation treatment of 12 mo (1-55 mo). After drug withdrawal, 90% of the patients had viral relapses, among whom 38% had clinical relapses. The relapse rates were 100%, 80% and 89% for the patients with consolidation treatments < 6 mo, 6-11 mo and ≥ 12 mo, respectively; however, the differences were not statistically significant (P = 0.34). Additionally, Papatheodoridis et al[10] systemically evaluated a total of 1716 patients from 25 studies and did not find any difference in the relapse rate between patients receiving < 12 mo and > 12 mo of NA consolidation treatment after HBeAg seroconversion (P = 0.928). Therefore, the focus of antiviral treatment should be changed, and antiviral treatment endpoints should be reconsidered; the aim should not just be “providing timely help” - treating the relapse after drug withdrawal- but it should be “making things better”. Hepatitis B surface antigen (HBsAg) clearance, the ideal endpoint, should be considered for patients who have undergone effective long-term antiviral treatment.
CHB ANTIVIRAL TREATMENT ENDPOINTS AND SAFETY OF DRUG WITHDRAWAL
With the increasing understanding of CHB, the treatment guidelines have also been corrected and modified. In the 1960s-1970s, treatment focused on reducing transaminase because a normal transaminase level was thought to be a marker for disease recovery. In the early 1970s, the pathogenesis of HBV and CHB were studied in depth, and it was recognized that liver inflammation and injury are caused by immune mechanisms in patients with HBV. The continuous presence and replication of HBV are important reasons for persistent liver inflammation in HBV patients[11]. Therefore, the key to treatment is pathogen treatment, antiviral treatment. NA and interferon (IFN), including normal IFNs and pegylated IFNs (Peg-IFNs) are currently the two most commonly used antiviral drugs.
In 2009, the European Association for the Study of the Liver (EASL) first proposed 3 endpoints for antiviral treatment of CHB: The ideal endpoint was HBsAg clearance, a satisfactory endpoint was HBeAg seroconversion, and the next most desirable endpoint was persistent inhibition of HBV DNA replication[12]. At that time, persistent inhibition of HBV DNA replication and HBeAg seroconversion could be achieved easily through antiviral treatment; however, HBsAg clearance was unattainable. In recent years, with the continuous development of CHB antiviral treatment, antiviral treatment endpoints have also improved. Based on this, in Guidelines for the prevention and treatment of chronic hepatitis B: A 2015 update[5], high treatment requirements, including the pursuit of “clinical cure” for suitable patients with CHB, are proposed. The proposal of this treatment endpoint is closely associated with the safety of drug withdrawal and improvements in the prognosis of patients.
NAs are currently the most widely used antiviral drugs. They are convenient to take and have significant inhibition effects on HBV DNA. However, long-term use can lead to drug resistance and side effects. A study showed that the resistance rate was as high as 70% following 5 years of lamivudine (LAM) treatment[6]. Long-term use of adefovir dipivoxil can damage renal function, and telbivudine can increase creatine kinase levels, leading to muscle pain. The NAs with high barriers to resistance, such as entecavir (ETV) and tenofovir disoproxil fumarate (TDF), have significantly reduced drug resistance. However, although patients who use ETV or TDF have good virologic responses, drug safety should also be considered. A study by Han et al[13] showed that long-term ETV or TDF treatment reduced the glomerular filtration rate and caused kidney damage. In particular, the study showed that TDF was 1.6 times more likely than ETV to cause kidney damage. Moreover, long-term TDF treatment also increased the risk of hypophosphataemia. Additionally, the long-term usage is required to maintain clinical efficacy, and drug withdrawal leads to relapse. Liem et al[14] showed that long-term application (the average duration of treatment was 8 years) ETV or TDF treatment maintain virologic suppression HBeAg negative CHB, after 48 wk of drug withdrawal, 2% of patients had HBsAg clearance, only 24% maintained a persistent response [negative HBeAg, HBV DNA < 2000 IU/mL and normal alanine aminotransferase (ALT)], and 74% had virologic relapse (HBV DNA > 2000 IU/mL). Among the patients with virologic relapse, 29% required retreatment (HBV DNA > 20000 IU/mL or accompanied with ALT > 5 ULN).
When patients with HBeAg-positive CHB have reached a satisfactory treatment endpoint after antiviral treatment, patient conditions are relatively stable. It is generally believed that drug treatment can be withdrawn from patients after a period of consolidation treatment. However, because the relapse rate after drug withdrawal is as high as 20%-40%[15] and the mechanism underlying relapse is still not clear, the updated guidelines suggest extending treatment to reduce relapse. The 2005 Chinese guidelines for CHB suggest that patients who have achieved HBeAg seroconversion through NA treatment should undergo 1 year of consolidation treatment[16]. The 2010 guidelines suggest that the total treatment should be at least 2 years[17]. The 2015 guidelines suggest extending consolidation treatment for at least 3 years and that the total treatment should last at least 4 years[5]. However, current studies are inconsistent about whether extended treatment can reduce relapse. Although the American Association for the Study of Liver Diseases does not suggest extending treatment, due to the high risk of relapse, it suggests close follow-up after drug withdrawal. It also proposes that HBsAg clearance is a better option, and the patients who have achieved HBeAg seroconversion can further seek HBsAg clearance[7]. The 2017 EASL guidelines[6] also have reinterpreted the previously (2009 and 2012)[12,18] proposed “satisfactory endpoint” and changed it to “valuable endpoint”, believing that HBeAg seroconversion is only partial HBV inhibition through the immune system. Because the safety of drug withdrawal is uncertain, HBsAg clearance is recommended as the optimal treatment endpoint for patients with HBeAg-positive or HBeAg-negative CHB.
It has become the consensus of all major guidelines in China and other countries that HBsAg clearance is the ideal treatment endpoint for CHB; this is referred to as a “clinical cure”[5] or “functional cure”[6]. However, currently, the HBsAg clearance rate is still very low. The annual spontaneous clearance rate does not exceed 1%[19], and the clearance rate for patients who have undergone 48 wk of NA or IFN single drug treatment is only 0%-3%[5,20]. Kim et al[21] reported that among 110 patients who achieved HBsAg clearance through NA treatment (with an annual clearance rate of 0.33%), the cumulative relapse rate was 11.7% within a 3-year follow-up and 2 patients had HCC. Similar to that study, in our study, 238 patients achieved HBsAg clearance after IFN treatment, and the cumulative relapse rate was 9.7%, with the majority being HBsAg reversion and/or HBV DNA reversion and only 1 patient showing clinical relapse. Additionally, liver cirrhosis or HCC was not found during the follow-up (unpublished data). Therefore, current studies have confirmed that compared to patients who achieved HBV DNA inhibition with or without simultaneous HBeAg seroconversion, HBsAg clearance not only leads to safer drug withdrawal and longer efficacy but also significantly improves long-term prognosis. Additionally, in the pursuit of HBsAg clearance, attention should also be paid to the HBeAg status. HBsAg disappearance does not necessarily indicate that HBeAg is absent. Different HBsAg response patterns could be observed during HBsAg clearance[22]. Only HBsAg clearance based on HBV DNA inhibition and HBeAg seroconversion was safe for drug withdrawal. The treatment goals and endpoints of CHB proposed by domestic and foreign guidelines are shown in Table 1.
Table 1.
Treatment goals and endpoints of chronic hepatitis B guidelines at home and abroad
| Guidelines | Time (yr) | Treatment goals |
Treatment endpoints |
|||
| persistent inhibition of HBV DNA | HBeAg seroconversion | HBsAg clearance | ||||
| European Association for the Study of the Liver (EASL) | 2009 | Improve quality of life and survival | Next most desirable endpoint | Satisfactory endpoint | Ideal endpoint | |
| 2012 | Improve quality of life and survival | Next most desirable endpoint | Satisfactory endpoint | Ideal endpoint | ||
| 2017 | Improve survival and quality of life, prevent mother to child transmission | Main endpoint | Valuable endpoint | Optimal endpoint | ||
| American Association for the Study of Liver Diseases (AASLD) | 2009 | Improve prognosis | - | - | - | |
| 2016 | Decrease the morbidity and mortality | - | Intermediate endpoint | Best predictor of sustained remission | ||
| 2018 | Reduce risk of progression to cirrhosis and liver-related complications | - | - | “Functional cure” or “Resolved CHB” | ||
| Chinese guidelines for the prevention and treatment of chronic hepatitis B | 2005 | Improve quality of life and survival | - | - | - | |
| 2010 | Improve quality of life and survival | - | - | - | ||
| 2015 | Improve quality of life and survival | Basic endpoint | Satisfactory endpoint | Ideal endpoint (“clinical cure”) | ||
HBeAg: Hepatitis B e antigen; HBsAg: Hepatitis B surface antigen.
ANTIVIRAL TREATMENT ENDPOINTS AND PROGNOSIS IMPROVEMENT
Currently, large amounts of evidence-based medical data indicate that inhibiting HBV DNA replication through active antiviral therapy can improve the patient prognosis. The early REVEAL-HBV study[23] analyzed the incidence of HCC in patients with different HBV DNA loads. The study recruited 3653 patients infected with chronic HBV who did not undergo antiviral treatment. Patients were stratified according to baseline HBV DNA (copies/mL) levels (< 300, 300-9999, 10000-99999, 100000-999999 and ≥ 1 million), and the average follow-up period was 11.4 years. The results showed that higher HBV DNA levels were associated with higher annual incidences and cumulative incidences of HCC. Additionally, if the HBV DNA level was elevated or reduced during the follow-up compared to that at baseline, HCC incidence also increased (P = 0.01) or reduced (P < 0.01). Additionally, multivariable analysis showed that HBV DNA ≥ 10000 copies/mL was an independent predictive factor for HCC. Does the inhibition of HBV DNA replication through antiviral treatment reduce the incidence of HCC? A multi-centered, randomized, double-blinded and placebo-controlled study provided an excellent answer to this question. The 4006 study in which LAM treatment slowed disease progression[24] was the first to compare an antiviral treatment group and placebo group. The study recruited 651 patients with decompensated liver cirrhosis, and the average follow-up was 3 years. The results showed that compared to the placebo group, the antiviral treatment group exhibited significantly reduced disease progression rates (P < 0.001), Child-Pugh scores (P = 0.02), and incidences of HCC (P = 0.047). Since this study, the importance of antiviral treatment in improving patient prognosis has been established. Currently, TDF is a first line antiviral drug for CHB, and relevant studies have made similar conclusions. In a study of 641 CHB patients receiving TDF treatment, 348 patients underwent liver biopsy at baseline and 5 years after treatment. The results showed that liver histology was improved in 74% of patients with liver cirrhosis at baseline and that liver histology was not aggravated in 96% of patients without liver cirrhosis at baseline[25]. After 8 years of TDF treatment, 14 patients had HCC and the annual incidence of HCC was 0.37%. Compared with historical data, the incidence of HCC was significantly lower than that of non-antiviral patients[26].
HBeAg status affects patient prognosis. A study by Yang et al[27] recruited 2361 patients with CHB who did not receive antiviral treatment; the total follow-up period was 18154 patient years. This study found that HBeAg-positive status was a high-risk factor for HCC. The risk of HCC in patients with an HBsAg-positive HBeAg-positive status was 6.3 times higher than that of patients with an HBsAg-positive HBeAg-negative status. Studies have confirmed that HBeAg seroconversion through antiviral treatment significantly improves patient prognosis. An early study by van Zonneveld et al[28] recruited 165 patients with HBeAg-positive CHB and found that the prognosis was improved after only 16 wk of IFN treatment. The median follow-up period was 8.8 years, and 8 patients had HCC, among whom, 6 patients were non-responders. Multivariable analysis showed that compared to non-responders, HBeAg seroconversion could significantly extend patient survival [relative risk (RR) = 0.28, 95% confidence interval (CI): 0.10-0.78] and reduce HCC risk (RR = 0.084, 95%CI: 0.09-0.75). A study by Lin et al[29] recruited 466 patients with HBeAg-positive CHB, among whom 233 patients underwent IFN treatment (11-28 wk) and the remaining 233 patients did not receive any treatment. At 15 years of follow-up, compared to the control group, the IFN treatment group had a higher HBeAg seroconversion rate (P = 0.031) and lower incidences of liver cirrhosis and HCC (P = 0.041, P = 0.011). In a comparison of patients with and without HBeAg seroconversion, the former had lower risks of liver cirrhosis and HCC (P = 0.023, P = 0.003). As shown in the study, compared to the control group, the IFN treatment (independent of achieving HBeAg seroconversion) improved patient prognosis; patients with HBeAg seroconversion had an even better prognosis.
The above studies confirmed that HBV DNA inhibition and HBeAg seroconversion can both improve prognosis. However, long-term NA maintenance treatment is required for patients who only achieve HBV DNA inhibition. HBeAg seroconversion can not only improve prognosis but also lead to safe drug withdrawal in some patients; therefore, this endpoint is important to achieve in clinical practice. For patients who cannot achieve HBeAg seroconversion, long-term HBV DNA inhibition should be maintained to delay disease progression and await the development of new drugs, which is also an acceptable option. Additionally, different percentages of relapses were present in patients with HBeAg seroconversion, 20%-40% could revert to HBeAg-positive CHB and 10%-20% could revert to HBeAg-negative CHB. Even after converting to inactive HBsAg carriers (IHC), 20%-40% may revert to HBeAg-negative CHB[15], and HCC incidence and liver-related mortality in these patients were both higher than those for HBsAg-negative healthy controls (HR = 4.6, 95%CI: 2.3-8.3, HR = 2.1, 95%CI: 1.1-4.1)[30]. Therefore, HBsAg clearance should be the goal for the treatment of CHB.
Recent studies have found that the HBsAg levels in patients who have achieved HBV DNA inhibition and HBeAg seroconversion also affect prognosis. Tseng et al[31] studied 2688 CHB patients who did not receive antiviral treatment (2165 patients were HBeAg-negative, and 1068 patients had baseline HBV DNA < 2000 IU/mL), among whom 191 patients had HCC; the average follow-up was 14.7 years. The study showed that for patients who were HBeAg-negative and had baseline HBV DNA < 2000 IU/mL, HBsAg level is the decisive factor for HCC occurrence. The risk of HCC in patients with baseline HBsAg > 1000 IU/mL is 13.7 times that of patients with baseline HBsAg < 1000 IU/mL. If the HBsAg level increased during the follow-up, the HCC risk also increased. On the other hand, recent studies have shown that achieving HBsAg clearance not only improves liver tissue but also reduces the incidence of HCC. In a study of 92 patients with HBsAg clearance and a median follow-up of 126 mo, Yuen et al[32] found that after HBsAg clearance, the transaminase levels of patients were significantly improved. HBV DNA was not detected in the serum of 98% of patients. Among the 14 patients who underwent liver tissue biopsy, the liver histology was very close to that of normal liver tissue. In the study by Kim et al[21], among 110 CHB patients who achieved HBsAg clearance through NA treatment, with a total follow-up of 287 patient years, 2 patients had HCC, which was significantly lower than that of the matched patients without HBsAg clearance (HR = 0.09, P < 0.01). Additionally, even for patients with pre-existing liver cirrhosis, HBsAg clearance is associated with prognosis. A study by Fattovich et al[33] recruited 309 patients with decompensated liver cirrhosis confirmed by biopsy, with an average follow-up of 5.7 years, and found that 32 patients achieved HBsAg clearance, among whom 1 patient (3%) had HCC and died. Among the patients with persistent positive HBsAg, 11% had HCC, and 20% died. Compared to patients with persistent positive HBsAg, patients with HBsAg clearance had a lower risk of HCC (P = 0.013) and longer survival (P < 0.001).
However, it should be noted that HBsAg clearance does not indicate virus eradication[34,35]. Due to the presence of cccDNA, it is possible for HBV reactivation in patients treated with immunosuppressants, cytotoxic drugs and hormones[36-40]. Therefore, we refer to HBsAg clearance as a “clinical cure” or “functional cure”, which is the highest treatment endpoint that can be achieved by current treatment methods.
IMPROVING THE HBSAG CLEARANCE RATE BY OPTIMIZING ANTIVIRAL TREATMENT
Previous studies concluded that HBsAg level is a marker for determining the safety of drug withdrawal after patients achieve HBeAg seroconversion. It was generally believed that drugs can be withdrawn safely from patients with HBsAg < 1000 IU/mL[41-45]. Liu et al[46] systematically reviewed 11 studies comprising 1716 patients, aiming to determine the effects of HBsAg level on NA withdrawal in Asian CHB patients. The study found that among patients with HBsAg < 100 IU/mL, after more than 1 year of drug withdrawal and follow-up, 9.1%-19.6% of patients had virologic relapse (HBV DNA > 1000 IU/mL), and 15.4%-29.4% patients had clinical relapse (HBV DNA > 1000 IU/mL, ALT > 2ULN). The results indicated that although HBsAg is very low in patients undergoing NA treatment, the relapse rate after drug withdrawal is still high. However, if patients with low levels of HBsAg (e.g., HBsAg < 100 IU/mL) were treated properly, they could achieve HBsAg clearance. Therefore, the goal of antiviral treatment should not be limited to lack of relapse after drug withdrawal. HBsAg clearance is the most effective way to reduce relapse and improve prognosis.
Currently, NA and IFN are the two major antiviral drugs for CHB treatment. NA inhibits virus replication by acting on virus reverse transcription and can effectively reduce the HBV DNA load. However, NAs have no significant effect on HBsAg clearance[47]. A previous study showed that after 48 wk of antiviral treatment with NA, the HBsAg clearance rate of HBeAg-positive CHB was 0%-3%[48,49], and that of HBeAg-negative CHB was 0%[49], which was equivalent to the HBsAg spontaneous annual clearance rate[20,50]. IFN has both antiviral and immune regulatory functions. IFN not only prevent infection of new liver cells but also clear infected liver cells, which is beneficial for HBsAg clearance[47]. However, after 48 wk of antiviral treatment with Peg-IFN and 24 wk of follow-up, the HBsAg clearance rate of HBeAg-positive CHB was only 3%-4%[51], and that of HBeAg-negative CHB was 2.8%[52]. These above studies showed that independent of HBeAg-positive or -negative CHB status, treatments with a single drug or fixed course led to poor HBsAg clearance. Therefore, exploring and optimizing antiviral treatment is important for improving the HBsAg clearance rate.
In the PegBeLiver study[53], patients with HBeAg-negative CHB were treated with a single Peg-IFN with an extended course of 96 wk, and the HBsAg clearance rate was 5.8%. In a study by Marcellin et al[54], patients were treated with a “powerful combination” of TDF and Peg-IFN for 48 wk; follow-up at the 24th wk after drug withdrawal showed that the HBsAg clearance rate was 9.1%. In the ARES study[55], HBeAg-positive CHB patients were divided into two groups after 24 wk of ETV treatment. Patients were treated with Peg-IFN combined with ETV or ETV alone for another 24 wk. The results showed that the response rate in the Peg-IFN group increased more rapidly than that in the ETV group alone. A study by Cao et al[56] used the combination and extended treatment method and found that the HBsAg clearance rate was as high as 25.5% in patients with HBeAg-positive CHB and 28% in patients with HBeAg-negative CHB[57] at the 96th wk. These above studies indicate that extended treatment, combined treatment or extended treatment together with combined treatment can improve treatment effectiveness. However, treatment efficacy does not improve with an extended treatment course. Even patients who respond well to IFN are not able to tolerate the adverse effects of IFN. Recently, Chinese researchers have conducted studies on NA treated patients. In the OSST study[58], patients with HBeAg-positive CHB who had received ETV, with HBeAg < 100 IU/mL,HBV DNA ≤ 1000 copies/mL, were subjected to Peg-IFNα-2a or ETV treatments for 48 wk, and the HBsAg clearance rates were 8.5% and 0%, respectively. Further subgroup analysis showed that the HBsAg clearance rate was as high as 22.2% at the 48th wk of Peg-IFNα-2a treatment in patients with baseline HBeAg- negative and HBsAg < 1500 IU/mL and only 1.7% for patients with baseline HBsAg ≥ 1500 IU/mL. The New Switch study[59] is an open clinical study actively seeking HBsAg clearance, and the subjects are patients with HBeAg- positive who achieved HBV DNA inhibition and HBeAg seroconversion after NA treatment. The patients were divided into two Peg-IFN sequential treatments: One for 48 wk and the other for 96 wk. The results showed that the HBsAg clearance rates for the 48-wk group and 96-wk group were 14.4% and 20.7%, respectively, among which the HBsAg clearance rates of patients with baseline HBsAg < 1500 IU/mL and ≥ 1500 IU/mL were 26.5% vs 4.7% (48 wk) and 40.0% vs 3.8% (96 wk), respectively. These studies suggest that patients undergoing NA treatment can achieve high HBsAg clearance rates by combining IFN treatment. An extended treatment course leads to better effectiveness, and patients with baseline HBsAg < 1500 IU/mL are the “advantageous population” who achieves HBsAg clearance.
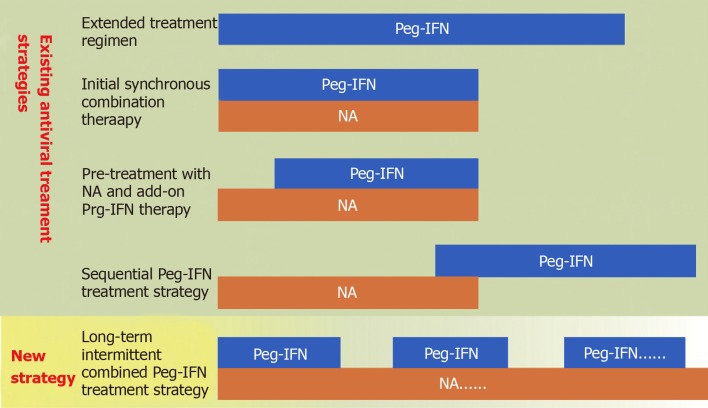
In our previous study of 107 patients with HBeAg-negative CHB, the patients underwent 96 wk of Peg-IFN combined with NA treatment and were followed up for 120 wk to assess effectiveness. We found that 31 patients (28.9%) achieved HBsAg clearance[60]. Further retrospective analysis of these patients showed that low levels of baseline HBsAg and the HBsAg level at the 48th wk were favourable predictors of HBsAg clearance. When the patients were divided according to nodal levels, the 96th wk HBsAg clearance rates of patients with HBsAg ≤ 1000 IU/mL, ≤ 100 IU/mL and ≤ 10 IU/mL at the end of the 48th wk were 36.1%, 52.8%, and 67.7%, respectively. When patients were divided according to interval levels, the 96th wk HBsAg clearance rates of patients with HBsAg levels at the 48th wk within 100 IU/mL< HBsAg ≤ 1000 IU/mL, 10 IU/m < HBsAg ≤ 100 IU/mL and HBsAg ≤ 10 IU/mL were 6.7%, 31.8%, and 67.7%, respectively[61]. Our results indicate that division by the “interval level” eliminates the population overlap caused by the division of the “nodal level” and more accurately predicts HBsAg clearance. Therefore, we believe that NA combined with Peg-IFN treatment in patients with HBsAg ≤ 100 IU/mL at the end of the 48th wk has a high possibility of HBsAg clearance at the 96th wk. This patient population have high chances of HBsAg clearance and are the “advantageous population” for HBsAg clearance. Therefore, on the basis of previous studies, we proposed a “targeted and indefinite course of treatment strategy” for patients with low HBsAg level, namely NA based treatment regimen plus IFN in stages. Through each stage of combined treatment, the promotion rate of the “advantageous population” is continuously increased, and the overall HBsAg clearance rate is finally improved. Different antiviral treatment regimens are summarized as follows (Figure 1).
Figure 1.
Pattern of different antiviral treatment regimens. IFN: Interferon; NA: Nucleos(t)ide analogue.
Of course, the concept of an “advantageous population” is not contradictory to the “advantageous population” mentioned above. The “advantageous population” from the above study is based on treating CHB patients with NA, and the “advantageous population” from our study is the patients who would benefit from extended treatment at the end of 48-week Peg-IFN treatment. Additionally, the HBsAg level is the predictive indicator for treatment efficacy. We should also ensure safety during the treatment to seek HBsAg clearance.
CONCLUSION
In summary, different antiviral treatment endpoints have different degrees of improvement in disease prognosis, and currently, HBsAg clearance is the ultimate goal of antiviral treatment. HBsAg clearance not only leads to biochemical, virologic and liver histological improvements but also reduces the risk of HCC. However, it is difficult to obtain a high HBsAg clearance rate with the existing single drug (NA or IFN) and fixed course of treatment, while the “advantageous population” in different studies can obtain a relatively higher HBsAg clearance rate. Therefore, in the pursuit of “clinical cure”, individualized treatment strategies should be implemented according to the specific conditions of patients, in which both effectiveness evaluation and safety monitoring should be carried out.
Footnotes
Conflict-of-interest statement: The authors have no conflicts of interest to declare.
Manuscript source: Invited manuscript
Peer-review started: March 11, 2019
First decision: April 16, 2019
Article in press: June 27, 2019
Specialty type: Medicine, Research and Experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Razek AA, Yoshioka K, Tuna N S-Editor: Dou Y L-Editor: A E-Editor: Wu YXJ
Contributor Information
Ya-Li Wu, International Medical Department, Beijing Youan Hospital, Capital Medical University, Beijing 100069, China.
Cheng-Li Shen, Division of Surgical Oncology, James Cancer Hospital, The Ohio State University Wexner Medical Center, Columbus, OH 43210, United States.
Xin-Yue Chen, International Medical Department, Beijing Youan Hospital, Capital Medical University, Beijing 100069, China. chen1204doc@ccmu.edu.cn.
References
- 1.Fattovich G, Bortolotti F, Donato F. Natural history of chronic hepatitis B: special emphasis on disease progression and prognostic factors. J Hepatol. 2008;48:335–352. doi: 10.1016/j.jhep.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 2.Chu CM, Liaw YF. Hepatitis B virus-related cirrhosis: natural history and treatment. Semin Liver Dis. 2006;26:142–152. doi: 10.1055/s-2006-939752. [DOI] [PubMed] [Google Scholar]
- 3.Chen YC, Chu CM, Yeh CT, Liaw YF. Natural course following the onset of cirrhosis in patients with chronic hepatitis B: a long-term follow-up study. Hepatol Int. 2007;1:267–273. doi: 10.1007/s12072-007-5001-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hsu YS, Chien RN, Yeh CT, Sheen IS, Chiou HY, Chu CM, Liaw YF. Long-term outcome after spontaneous HBeAg seroconversion in patients with chronic hepatitis B. Hepatology. 2002;35:1522–1527. doi: 10.1053/jhep.2002.33638. [DOI] [PubMed] [Google Scholar]
- 5.Chinese Society of Hepatology, Chinese Medical Association. Chinese Society of Infectious Diseases, Chinese Medical Association, Hou JL, lai W. [The guideline of prevention and treatment for chronic hepatitis B: a 2015 update] Zhonghua Gan Zang Bing Za Zhi. 2015;23:888–905. doi: 10.3760/cma.j.issn.1007-3418.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.European Association for the Study of the Liver. European Association for the Study of the Liver. EASL 2017 Clinical Practice Guidelines on the management of hepatitis B virus infection. J Hepatol. 2017;67:370–398. doi: 10.1016/j.jhep.2017.03.021. [DOI] [PubMed] [Google Scholar]
- 7.Terrault NA, Bzowej NH, Chang KM, Hwang JP, Jonas MM, Murad MH American Association for the Study of Liver Diseases. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63:261–283. doi: 10.1002/hep.28156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sarin SK, Kumar M, Lau GK, Abbas Z, Chan HL, Chen CJ, Chen DS, Chen HL, Chen PJ, Chien RN, Dokmeci AK, Gane E, Hou JL, Jafri W, Jia J, Kim JH, Lai CL, Lee HC, Lim SG, Liu CJ, Locarnini S, Al Mahtab M, Mohamed R, Omata M, Park J, Piratvisuth T, Sharma BC, Sollano J, Wang FS, Wei L, Yuen MF, Zheng SS, Kao JH. Asian-Pacific clinical practice guidelines on the management of hepatitis B: a 2015 update. Hepatol Int. 2016;10:1–98. doi: 10.1007/s12072-015-9675-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chaung KT, Ha NB, Trinh HN, Garcia RT, Nguyen HA, Nguyen KK, Garcia G, Ahmed A, Keeffe EB, Nguyen MH. High frequency of recurrent viremia after hepatitis B e antigen seroconversion and consolidation therapy. J Clin Gastroenterol. 2012;46:865–870. doi: 10.1097/MCG.0b013e31825ceed9. [DOI] [PubMed] [Google Scholar]
- 10.Papatheodoridis G, Vlachogiannakos I, Cholongitas E, Wursthorn K, Thomadakis C, Touloumi G, Petersen J. Discontinuation of oral antivirals in chronic hepatitis B: A systematic review. Hepatology. 2016;63:1481–1492. doi: 10.1002/hep.28438. [DOI] [PubMed] [Google Scholar]
- 11.Ye WX, Zhong ZY, Wang J. Tianjin: Tianjin science and technology press; 1996. Viral hepatitis and drug induced liver injury; pp. 794–795. [Google Scholar]
- 12.European Association For The Study Of The Liver. EASL Clinical Practice Guidelines: management of chronic hepatitis B. J Hepatol. 2009;50:227–242. doi: 10.1016/j.jhep.2008.10.001. [DOI] [PubMed] [Google Scholar]
- 13.Han Y, Zeng A, Liao H, Liu Y, Chen Y, Ding H. The efficacy and safety comparison between tenofovir and entecavir in treatment of chronic hepatitis B and HBV related cirrhosis: A systematic review and Meta-analysis. Int Immunopharmacol. 2017;42:168–175. doi: 10.1016/j.intimp.2016.11.022. [DOI] [PubMed] [Google Scholar]
- 14.Liem KS, Fung SK, Wong D, Yim CK, Noureldin S, Huang FF, Shah H, Feld JJ, Hansen BE, Janssen H. Limited Sustained Response and Lack of HBsAg Decline after Stopping Long-Term Nucleos(t) Ide Analogue Therapy in Hbeag Negative Patients with Chronic Hepatitis B: Results of a Prospective, Randomized, Open-Label Phase IV Trial. Proceedings of the 69th American Association for the Study of Liver Diseases; 2018 Nov 9-13; San Francisco, USA, Hepatology 2018; 28 suppl 1: P165A [Google Scholar]
- 15.McMahon BJ. The natural history of chronic hepatitis B virus infection. Hepatology. 2009;49:S45–S55. doi: 10.1002/hep.22898. [DOI] [PubMed] [Google Scholar]
- 16.Chinese Society of Hepatology, Chinese Medical Association. The guideline of prevention and treatment for chronic hepatitis B (2005 version) Zhonghua Ganzangbing Zazhi. 2005;13:881–891. [PubMed] [Google Scholar]
- 17.Chinese Society of Hepatology and Chinese Society of Infectious Diseases, Chinese Medical Association. The guideline of prevention and treatment for chronic hepatitis B (2010 version) Zhonghua Liu Xing Bing Xue Za Zhi. 2011;32:405–415. [PubMed] [Google Scholar]
- 18.European Association For The Study Of The Liver. EASL clinical practice guidelines: Management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–185. doi: 10.1016/j.jhep.2012.02.010. [DOI] [PubMed] [Google Scholar]
- 19.Zhou K, Contag C, Whitaker E, Terrault N. Spontaneous loss of surface antigen among adults living with chronic hepatitis B virus infection: a systematic review and pooled meta-analyses. Lancet Gastroenterol Hepatol. 2019;4:227–238. doi: 10.1016/S2468-1253(18)30308-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu Y, Hou J, Omata M, Wang Y, Li L. Loss of HBsAg and antiviral treatment: from basics to clinical significance. Hepatol Int. 2014;8:39–54. doi: 10.1007/s12072-013-9495-3. [DOI] [PubMed] [Google Scholar]
- 21.Kim GA, Lim YS, An J, Lee D, Shim JH, Kim KM, Lee HC, Chung YH, Lee YS, Suh DJ. HBsAg seroclearance after nucleoside analogue therapy in patients with chronic hepatitis B: clinical outcomes and durability. Gut. 2014;63:1325–1332. doi: 10.1136/gutjnl-2013-305517. [DOI] [PubMed] [Google Scholar]
- 22.Chen X, Cao Z, Liu Y, Zhang H, Zhang Y, Ma L, Jin Y, Yu H, Ma B, Zheng Y, Wu H. Potent hepatitis B surface antigen response to treatment of hepatitis-B-e-antigen-positive chronic hepatitis B with α-interferon plus a nucleos(t)ide analog. J Gastroenterol Hepatol. 2012;27:481–486. doi: 10.1111/j.1440-1746.2011.06970.x. [DOI] [PubMed] [Google Scholar]
- 23.Chen CJ, Yang HI, Su J, Jen CL, You SL, Lu SN, Huang GT, Iloeje UH REVEAL-HBV Study Group. Risk of hepatocellular carcinoma across a biological gradient of serum hepatitis B virus DNA level. JAMA. 2006;295:65–73. doi: 10.1001/jama.295.1.65. [DOI] [PubMed] [Google Scholar]
- 24.Liaw YF, Sung JJ, Chow WC, Farrell G, Lee CZ, Yuen H, Tanwandee T, Tao QM, Shue K, Keene ON, Dixon JS, Gray DF, Sabbat J Cirrhosis Asian Lamivudine Multicentre Study Group. Lamivudine for patients with chronic hepatitis B and advanced liver disease. N Engl J Med. 2004;351:1521–1531. doi: 10.1056/NEJMoa033364. [DOI] [PubMed] [Google Scholar]
- 25.Marcellin P, Gane E, Buti M, Afdhal N, Sievert W, Jacobson IM, Washington MK, Germanidis G, Flaherty JF, Aguilar Schall R, Bornstein JD, Kitrinos KM, Subramanian GM, McHutchison JG, Heathcote EJ. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: a 5-year open-label follow-up study. Lancet. 2013;381:468–475. doi: 10.1016/S0140-6736(12)61425-1. [DOI] [PubMed] [Google Scholar]
- 26.Kim WR, Loomba R, Berg T, Aguilar Schall RE, Yee LJ, Dinh PV, Flaherty JF, Martins EB, Therneau TM, Jacobson I, Fung S, Gurel S, Buti M, Marcellin P. Impact of long-term tenofovir disoproxil fumarate on incidence of hepatocellular carcinoma in patients with chronic hepatitis B. Cancer. 2015;121:3631–3638. doi: 10.1002/cncr.29537. [DOI] [PubMed] [Google Scholar]
- 27.Yang HI, Lu SN, Liaw YF, You SL, Sun CA, Wang LY, Hsiao CK, Chen PJ, Chen DS, Chen CJ Taiwan Community-Based Cancer Screening Project Group. Hepatitis B e antigen and the risk of hepatocellular carcinoma. N Engl J Med. 2002;347:168–174. doi: 10.1056/NEJMoa013215. [DOI] [PubMed] [Google Scholar]
- 28.van Zonneveld M, Honkoop P, Hansen BE, Niesters HG, Darwish Murad S, de Man RA, Schalm SW, Janssen HL. Long-term follow-up of alpha-interferon treatment of patients with chronic hepatitis B. Hepatology. 2004;39:804–810. doi: 10.1002/hep.20128. [DOI] [PubMed] [Google Scholar]
- 29.Lin SM, Yu ML, Lee CM, Chien RN, Sheen IS, Chu CM, Liaw YF. Interferon therapy in HBeAg positive chronic hepatitis reduces progression to cirrhosis and hepatocellular carcinoma. J Hepatol. 2007;46:45–52. doi: 10.1016/j.jhep.2006.08.021. [DOI] [PubMed] [Google Scholar]
- 30.Chen JD, Yang HI, Iloeje UH, You SL, Lu SN, Wang LY, Su J, Sun CA, Liaw YF, Chen CJ Risk Evaluation of Viral Load Elevation and Associated Liver Disease/Cancer in HBV (REVEAL-HBV) Study Group. Carriers of inactive hepatitis B virus are still at risk for hepatocellular carcinoma and liver-related death. Gastroenterology. 2010;138:1747–1754. doi: 10.1053/j.gastro.2010.01.042. [DOI] [PubMed] [Google Scholar]
- 31.Tseng TC, Liu CJ, Yang HC, Su TH, Wang CC, Chen CL, Kuo SF, Liu CH, Chen PJ, Chen DS, Kao JH. High levels of hepatitis B surface antigen increase risk of hepatocellular carcinoma in patients with low HBV load. Gastroenterology. 2012;142:1140–1149.e3; quiz e13-4. doi: 10.1053/j.gastro.2012.02.007. [DOI] [PubMed] [Google Scholar]
- 32.Yuen MF, Wong DK, Sablon E, Tse E, Ng IO, Yuan HJ, Siu CW, Sander TJ, Bourne EJ, Hall JG, Condreay LD, Lai CL. HBsAg seroclearance in chronic hepatitis B in the Chinese: virological, histological, and clinical aspects. Hepatology. 2004;39:1694–1701. doi: 10.1002/hep.20240. [DOI] [PubMed] [Google Scholar]
- 33.Fattovich G, Giustina G, Sanchez-Tapias J, Quero C, Mas A, Olivotto PG, Solinas A, Almasio P, Hadziyannis S, Degos F, de Moura MC, Krogsgaard K, Pantalena M, Realdi G, Corrocher R, Schalm SW. Delayed clearance of serum HBsAg in compensated cirrhosis B: relation to interferon alpha therapy and disease prognosis. European Concerted Action on Viral Hepatitis (EUROHEP) Am J Gastroenterol. 1998;93:896–900. doi: 10.1111/j.1572-0241.1998.00272.x. [DOI] [PubMed] [Google Scholar]
- 34.Durantel D. New treatments to reach functional cure: Virological approaches. Best Pract Res Clin Gastroenterol. 2017;31:329–336. doi: 10.1016/j.bpg.2017.05.002. [DOI] [PubMed] [Google Scholar]
- 35.Brahmania M, Feld J, Arif A, Janssen HL. New therapeutic agents for chronic hepatitis B. Lancet Infect Dis. 2016;16:e10–e21. doi: 10.1016/S1473-3099(15)00436-3. [DOI] [PubMed] [Google Scholar]
- 36.Hsu C, Tsou HH, Lin SJ, Wang MC, Yao M, Hwang WL, Kao WY, Chiu CF, Lin SF, Lin J, Chang CS, Tien HF, Liu TW, Chen PJ, Cheng AL Taiwan Cooperative Oncology Group. Chemotherapy-induced hepatitis B reactivation in lymphoma patients with resolved HBV infection: a prospective study. Hepatology. 2014;59:2092–2100. doi: 10.1002/hep.26718. [DOI] [PubMed] [Google Scholar]
- 37.Huang YH, Hsiao LT, Hong YC, Chiou TJ, Yu YB, Gau JP, Liu CY, Yang MH, Tzeng CH, Lee PC, Lin HC, Lee SD. Randomized controlled trial of entecavir prophylaxis for rituximab-associated hepatitis B virus reactivation in patients with lymphoma and resolved hepatitis B. J Clin Oncol. 2013;31:2765–2772. doi: 10.1200/JCO.2012.48.5938. [DOI] [PubMed] [Google Scholar]
- 38.Seto WK, Chan TS, Hwang YY, Wong DK, Fung J, Liu KS, Gill H, Lam YF, Lie AK, Lai CL, Kwong YL, Yuen MF. Hepatitis B reactivation in patients with previous hepatitis B virus exposure undergoing rituximab-containing chemotherapy for lymphoma: a prospective study. J Clin Oncol. 2014;32:3736–3743. doi: 10.1200/JCO.2014.56.7081. [DOI] [PubMed] [Google Scholar]
- 39.Loomba R, Liang TJ. Hepatitis B Reactivation Associated With Immune Suppressive and Biological Modifier Therapies: Current Concepts, Management Strategies, and Future Directions. Gastroenterology. 2017;152:1297–1309. doi: 10.1053/j.gastro.2017.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Moghoofei M, Mostafaei S, Ashraf-Ganjouei A, Kavosi H, Mahmoudi M. HBV reactivation in rheumatic diseases patients under therapy: A meta-analysis. Microb Pathog. 2018;114:436–443. doi: 10.1016/j.micpath.2017.12.014. [DOI] [PubMed] [Google Scholar]
- 41.Yao CC, Lee CM, Hung CH, Wang JH, Hu TH, Lu SN, Changchien CS, Hsu MC, Chen CH. Combining age and HBsAg level predicts post-treatment durability of nucleos(t)ide analogue-induced HBeAg seroconversion. J Gastroenterol Hepatol. 2015;30:918–924. doi: 10.1111/jgh.12874. [DOI] [PubMed] [Google Scholar]
- 42.Qiu YW, Huang LH, Yang WL, Wang Z, Zhang B, Li YG, Su TT, Zhou HY, Xu W, Wang XD, Dai YP, Gan JH. Hepatitis B surface antigen quantification at hepatitis B e antigen seroconversion predicts virological relapse after the cessation of entecavir treatment in hepatitis B e antigen-positive patients. Int J Infect Dis. 2016;43:43–48. doi: 10.1016/j.ijid.2015.10.019. [DOI] [PubMed] [Google Scholar]
- 43.Cai W, Xie Q, An B, Wang H, Zhou X, Zhao G, Guo Q, Gu R, Bao S. On-treatment serum HBsAg level is predictive of sustained off-treatment virologic response to telbivudine in HBeAg-positive chronic hepatitis B patients. J Clin Virol. 2010;48:22–26. doi: 10.1016/j.jcv.2010.02.014. [DOI] [PubMed] [Google Scholar]
- 44.Chi H, Li Z, Hansen BE, Yu T, Zhang X, Sun J, Hou J, Janssen HLA, Peng J. Serum Level of Antibodies Against Hepatitis B Core Protein Is Associated With Clinical Relapse After Discontinuation of Nucleos(t)ide Analogue Therapy. Clin Gastroenterol Hepatol. 2019;17:182–191.e1. doi: 10.1016/j.cgh.2018.05.047. [DOI] [PubMed] [Google Scholar]
- 45.Chen CH, Lu SN, Hung CH, Wang JH, Hu TH, Changchien CS, Lee CM. The role of hepatitis B surface antigen quantification in predicting HBsAg loss and HBV relapse after discontinuation of lamivudine treatment. J Hepatol. 2014;61:515–522. doi: 10.1016/j.jhep.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 46.Liu J, Li T, Zhang L, Xu A. The Role of Hepatitis B Surface Antigen in Nucleos(t)ide Analogues Cessation among Asian Chronic Hepatitis B Patients: A Systematic Review. Hepatology. 2018 doi: 10.1002/hep.30474. [DOI] [PubMed] [Google Scholar]
- 47.Reijnders JG, Rijckborst V, Sonneveld MJ, Scherbeijn SM, Boucher CA, Hansen BE, Janssen HL. Kinetics of hepatitis B surface antigen differ between treatment with peginterferon and entecavir. J Hepatol. 2011;54:449–454. doi: 10.1016/j.jhep.2010.07.046. [DOI] [PubMed] [Google Scholar]
- 48.Chang TT, Gish RG, de Man R, Gadano A, Sollano J, Chao YC, Lok AS, Han KH, Goodman Z, Zhu J, Cross A, DeHertogh D, Wilber R, Colonno R, Apelian D BEHoLD AI463022 Study Group. A comparison of entecavir and lamivudine for HBeAg-positive chronic hepatitis B. N Engl J Med. 2006;354:1001–1010. doi: 10.1056/NEJMoa051285. [DOI] [PubMed] [Google Scholar]
- 49.Marcellin P, Heathcote EJ, Buti M, Gane E, de Man RA, Krastev Z, Germanidis G, Lee SS, Flisiak R, Kaita K, Manns M, Kotzev I, Tchernev K, Buggisch P, Weilert F, Kurdas OO, Shiffman ML, Trinh H, Washington MK, Sorbel J, Anderson J, Snow-Lampart A, Mondou E, Quinn J, Rousseau F. Tenofovir disoproxil fumarate versus adefovir dipivoxil for chronic hepatitis B. N Engl J Med. 2008;359:2442–2455. doi: 10.1056/NEJMoa0802878. [DOI] [PubMed] [Google Scholar]
- 50.Chu CM, Liaw YF. HBsAg seroclearance in asymptomatic carriers of high endemic areas: appreciably high rates during a long-term follow-up. Hepatology. 2007;45:1187–1192. doi: 10.1002/hep.21612. [DOI] [PubMed] [Google Scholar]
- 51.Lau GK, Piratvisuth T, Luo KX, Marcellin P, Thongsawat S, Cooksley G, Gane E, Fried MW, Chow WC, Paik SW, Chang WY, Berg T, Flisiak R, McCloud P, Pluck N Peginterferon Alfa-2a HBeAg-Positive Chronic Hepatitis B Study Group. Peginterferon Alfa-2a, lamivudine, and the combination for HBeAg-positive chronic hepatitis B. N Engl J Med. 2005;352:2682–2695. doi: 10.1056/NEJMoa043470. [DOI] [PubMed] [Google Scholar]
- 52.Marcellin P, Lau GK, Bonino F, Farci P, Hadziyannis S, Jin R, Lu ZM, Piratvisuth T, Germanidis G, Yurdaydin C, Diago M, Gurel S, Lai MY, Button P, Pluck N Peginterferon Alfa-2a HBeAg-Negative Chronic Hepatitis B Study Group. Peginterferon alfa-2a alone, lamivudine alone, and the two in combination in patients with HBeAg-negative chronic hepatitis B. N Engl J Med. 2004;351:1206–1217. doi: 10.1056/NEJMoa040431. [DOI] [PubMed] [Google Scholar]
- 53.Lampertico P, Viganò M, Di Costanzo GG, Sagnelli E, Fasano M, Di Marco V, Boninsegna S, Farci P, Fargion S, Giuberti T, Iannacone C, Regep L, Massetto B, Facchetti F, Colombo M PegBeLiver Study Group. Randomised study comparing 48 and 96 weeks peginterferon α-2a therapy in genotype D HBeAg-negative chronic hepatitis B. Gut. 2013;62:290–298. doi: 10.1136/gutjnl-2011-301430. [DOI] [PubMed] [Google Scholar]
- 54.Marcellin P, Ahn SH, Ma X, Caruntu FA, Tak WY, Elkashab M, Chuang WL, Lim SG, Tabak F, Mehta R, Petersen J, Foster GR, Lou L, Martins EB, Dinh P, Lin L, Corsa A, Charuworn P, Subramanian GM, Reiser H, Reesink HW, Fung S, Strasser SI, Trinh H, Buti M, Gaeta GB, Hui AJ, Papatheodoridis G, Flisiak R, Chan HL Study 149 Investigators. Combination of Tenofovir Disoproxil Fumarate and Peginterferon α-2a Increases Loss of Hepatitis B Surface Antigen in Patients With Chronic Hepatitis B. Gastroenterology. 2016;150:134–144.e10. doi: 10.1053/j.gastro.2015.09.043. [DOI] [PubMed] [Google Scholar]
- 55.Brouwer WP, Xie Q, Sonneveld MJ, Zhang N, Zhang Q, Tabak F, Streinu-Cercel A, Wang JY, Idilman R, Reesink HW, Diculescu M, Simon K, Voiculescu M, Akdogan M, Mazur W, Reijnders JG, Verhey E, Hansen BE, Janssen HL ARES Study Group. Adding pegylated interferon to entecavir for hepatitis B e antigen-positive chronic hepatitis B: A multicenter randomized trial (ARES study) Hepatology. 2015;61:1512–1522. doi: 10.1002/hep.27586. [DOI] [PubMed] [Google Scholar]
- 56.Cao ZH, Liu YL, Ma LN, Lu JF, Jin Y, He ZM, Chen XY. Efficacy of pegylated interferon-2a combined with lamivudine or adefovir in the treatment of chronic hepatitis B with positive hepatitis B e antigen for 96 weeks. Chin J Infect Dis. 2016;34:422–424. [Google Scholar]
- 57.Cao ZH, Ma LN, Liu YL, Jin Y, He ZM, Lu JF, Zhang YH, Chen XY. [Efficacy and safety of peginterferon alfa-2a (40 kd) plus adefovir for 96 weeks in HBeAg-negative chronic hepatitis B patients] Zhonghua Gan Zang Bing Za Zhi. 2013;21:498–501. doi: 10.3760/cma.j.issn.1007-3418.2013.07.006. [DOI] [PubMed] [Google Scholar]
- 58.Ning Q, Han M, Sun Y, Jiang J, Tan D, Hou J, Tang H, Sheng J, Zhao M. Switching from entecavir to PegIFN alfa-2a in patients with HBeAg-positive chronic hepatitis B: a randomised open-label trial (OSST trial) J Hepatol. 2014;61:777–784. doi: 10.1016/j.jhep.2014.05.044. [DOI] [PubMed] [Google Scholar]
- 59.Hu P, Shang J, Zhang W, Gong G, Li Y, Chen X, Jiang J, Xie Q, Dou X, Sun Y, Li Y, Liu Y, Liu G, Mao D, Chi X, Tang H, Li X, Xie Y, Chen X, Jiang J, Zhao P, Hou J, Gao Z, Fan H, Ding J, Zhang D, Ren H. HBsAg Loss with Peg-interferon Alfa-2a in Hepatitis B Patients with Partial Response to Nucleos(t)ide Analog: New Switch Study. J Clin Transl Hepatol. 2018;6:25–34. doi: 10.14218/JCTH.2017.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Yan YJ, Lu JF, Cao ZH, Jin Y, He ZM, Geng N, Ren S, Liu YL, Cheng XY. Treatment of HBeAg negative chronic hepatitis B: 96 weeks of Peg-interferon alpha-2a and nucleoside/nucleotide analogues combined therapy versus single drug monotherapy. Zhongguo Bing Du Bing Za Zhi. 2017;7:337–342. [Google Scholar]
- 61.Yan YJ, Wang XX, Cao ZH, Lu JF, Jin Y, He ZM, Geng N, Ren S, Ma LN, Chen XY. [Low-levels of HBsAg quantification at 48-week in HBeAg-negative chronic hepatitis B patients are the advantageous population for HBsAg clearance] Zhonghua Gan Zang Bing Za Zhi. 2018;26:813–818. doi: 10.3760/cma.j.issn.1007-3418.2018.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]