Abstract
Introduction
The purpose of this study was to evaluate intraocular pressure (IOP) lowering and safety of XEN® stent in medically refractory, progressive, open-angle glaucoma (OAG).
Methods
Forty-seven eyes of 42 patients were treated with XEN® stent alone or combined with phacoemulsification.
Results
Mean IOP decreased from 22.34 ± 7.34 mmHg to 12.91 ± 4.21, 12.95 ± 4.36, 13.49 ± 3.91, and 13.36 ± 3.63 mmHg at 1, 3, 6, and 12 months (95% confidence interval [CI] [20.24, 24.44], [11.71, 14.12], [11.63, 14.27], [12.36, 14.62], and [12.10, 14.62]), respectively. Mean number of medications decreased from 2.96 ± 1.20 (95% CI [2.62, 3.30]) at baseline to 0.75 ± 1.27 (95% CI [0.31, 1.19]) at 1 year. At 1 year (n = 32), complete success was achieved in 68.8% (n = 22/32) (i.e., IOP reduction ≥ 20% and IOP < 18 mmHg without medication or any secondary glaucoma intervention). Qualified success was achieved in 90.6% (n = 29/32) (i.e., IOP reduction of ≥ 20% and IOP < 18 mmHg with and without medication or any secondary glaucoma intervention). Eleven eyes had not yet reached 12 months. Two patients (three eyes) died before 1 year; one patient (one eye) was lost to follow up. Adverse events: localized choroidal hemorrhage in one eye; hypotony (IOP < 6 mmHg) at day 1 in 10 eyes, with full resolution by 2 weeks. No persistent hypotony or maculopathy occurred. Stent erosion with removal occurred in two eyes. Fourteen eyes (29.8%) underwent needling. One patient required trabeculectomy.
Conclusions
XEN® stent is effective and relatively safe surgery for medically refractory, progressive, OAG out to 1 year. Intraocular pressure and medications were significantly reduced.
Keywords: Glaucoma, MIGS; Surgery; XEN® stent
Introduction
Glaucoma is the world’s leading cause of blindness [1]. The disease consists of a painless, progressive optic neuropathy leading to the death of optic nerve fibers and corresponding loss of visual field. Untreated or inadequately controlled glaucoma commonly results in severe vision loss, which has a tremendous socioeconomic impact [1]. Numerous clinical trials have shown that lowering intraocular pressure (IOP) halts glaucoma progression [2–4] and, in doing so, prevents vision loss and maintains quality of life.
Medication, laser trabeculoplasty, and trabeculectomy are all effective treatments for lowering IOP. First-line management is commonly either medication or laser. Rates of noncompliance with medication vary widely, from 5% to 80% [5]. Noncompliance is associated with both poor outcomes and high health care costs [6–10]. In addition, chronic use of topical glaucoma medications causes inflammation and alteration of the conjunctival surface [5].
Laser trabeculoplasty is used as either primary or add-on therapy. Laser cannot achieve IOP below episcleral venous pressure, and its effect wanes with time, at a failure rate of nearly 10%/year [11–13].
Glaucoma surgery is indicated in eyes in which IOP is refractory to laser or medical management, disease progression occurs despite such therapy, or medication side effects or intolerance preclude their use. Trabeculectomy and tube shunt surgery are the most common surgical procedures for glaucoma. Although tube shunt surgery has gained popularity, it has not replaced trabeculectomy as the gold standard for surgically lowering IOP. These procedures are both done ab externo and require significant disruption of conjunctiva and Tenon’s capsule, increasing the risk of scar formation and surgical failure [14, 15]. Standardization and regulation of aqueous outflow are difficult and are associated with a relatively high percentage of short- and long-term complications, including persistent hypotony, serous choroidal detachments, suprachoroidal hemorrhage, bleb leaks, infection, cataract, and hypotony maculopathy [14, 16–18].
Minimally invasive glaucoma surgery (MIGS) has become popular due to the desire for safer, quicker, less invasive yet effective surgical alternatives to trabeculectomy and tube shunt surgery. Compared with current approaches, MIGS procedures are characterized by minimal tissue disruption, ab interno insertion, shortened surgical time, and IOP lowering. Less surgery should translate to fewer sight-threatening complications [19]. With U.S. Food and Drug Administration (FDA) approval in November 2016, the XEN® gel stent became the first MIGS option available in the United States for treatment of refractory, progressive, open-angle glaucoma (OAG) and also did not require combination with cataract surgery. The stent procedure is an alternative to trabeculectomy for progressive, uncontrolled glaucoma. The stent is a 6-mm hydrophilic, noninflammatory, nondegrading porcine gelatin stent [20]. It is the world’s first ab interno MIGS approach that models standard trabeculectomy by shunting aqueous humor from the anterior chamber to the subconjunctival space through the obstructed trabecular meshwork. Both procedures create an external filtration bleb and rely on adjunct antifibrotic agents to enhance filtration success. However, insertion of the XEN® stent requires no conjunctival dissection, and filtration blebs are typically lower-lying and more diffuse than those seen with trabeculectomy [20–29].
The flow characteristics of the XEN® gel stent are based on the Hagen-Poiseuille equation, which defines the amount of resistance to laminar fluid flow through a cylindrical tube [20]. Thus, the rate of aqueous humor flow through the XEN® stent is determined by stent length and inner diameter. During product development, 45 μm was found to be the optimal diameter to prevent hypotony yet maximize aqueous outflow for long-term IOP control [22, 24–27].
Although the XEN® gel stent has been used and studied in countries outside the United States, data from within the United States are limited. We therefore undertook this study to evaluate the efficacy and safety of the stent both as a standalone filtration procedure and in combination with cataract surgery for patients with progressive OAG refractory to medical therapy. In studying this device, we hoped to better understand how to optimize success and identify potential issues with placement or postoperative management to assist glaucoma surgeons as XEN® stent use becomes more widespread.
Methods
Study Population
This was an investigator-initiated, prospective, noncomparative study of glaucoma patients referred within Park Nicollet Clinic, a multispecialty, non-university medical practice in St. Louis Park, Minnesota, USA. Eligible patients enrolled in the study were 21 years or older with severe-stage OAG that was uncontrolled, refractory to medical therapy, and requiring either trabeculectomy or tube shunt surgery to halt glaucoma progression. Uncontrolled, medically refractory OAG was defined as uncontrolled IOP, documented visual field progression, and/or increasing optic nerve damage despite maximum medical therapy (four or more topical IOP-lowering medications, or fewer in the case of tolerability or efficacy issues) and laser treatment, when possible. Patients with mild or moderate-stage OAG were not included in the study, as other MIGS devices were available for eyes with these stages of disease. Of the FDA-approved MIGS devices, the XEN® stent is the only one that utilizes the subconjunctival space and the only one that can achieve intraocular pressure lowering to the same level as standard trabeculectomy or tube shunt surgery. Unlike the other categories of MIGS, the FDA approved use of the XEN® stent with or without cataract surgery.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the HealthPartners Institute Institutional Review Boards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants in the study for both the procedure itself and inclusion in the study. The HealthPartners Institutional Review Board approved this study.
Preoperatively, eyes underwent a complete ophthalmic examination, including slit-lamp and funduscopic examinations, Goldmann applanation tonometry (two separate measurements, with resetting of the dial to 10 mmHg between readings), gonioscopy, corneal pachymetry, standardized automated perimetry, and optical coherence tomography analysis. Patients were required to have healthy, free, and mobile conjunctiva superiorly in the area of planned XEN® stent implantation and an open angle with a visible trabecular meshwork. Exclusion criteria included previous incisional glaucoma filtration or tube surgery, conjunctival pathology, aphakia, epithelial downgrowth, anterior chamber intraocular lens, presence of vitreous in the anterior chamber, and the following types of glaucoma: uveitic, neovascular, angle-closure, iridocorneal endothelial syndrome, and Axenfeld-Rieger syndrome.
At minimum, postoperative examinations were conducted at day 1, week 1, and months 1, 3, 6, and 12. Each visit included slit-lamp and posterior segment examinations, IOP by Goldmann applanation tonometry, and gonioscopy. Standardized automated perimetry was performed at 1 year at minimum. Endothelial cell counts were not measured pre- or postoperatively. Visual acuity, medications, and adverse events were also recorded.
Surgical Implantation
Surgeries were performed from March 2017 to May 2018 by a single surgeon (PK). All surgeries were performed under topical anesthesia. After prepping and draping the eye in sterile ophthalmic fashion, the superior nasal conjunctiva was marked 3 mm from the limbus in the planned exit point of the stent. Using a 30G needle, 0.1 ml of mitomycin-C (0.2 mg/ml) was injected posteriorly into Tenon’s capsule. Using cellulose sponges, the mitomycin-C was massaged over the area of anticipated stent placement, with efforts to keep it away from the limbus. Main and side port incisions were created. A combination of cohesive and dispersive viscoelastic was used to fill the anterior chamber. In patients with cataract surgery, preservative-free lidocaine was injected before the viscoelastic. Phacoemulsification and lens implantation were performed before XEN® stent placement. The angle was inspected before XEN® stent insertion with a disposable gonioprism (Katena, Denville, NJ, USA). After obtaining the XEN® stent inserter, the protective devices were removed and the inserter was checked to confirm that it contained a stent. The inserter was introduced into the eye through the main incision, and the needle was directed across the anterior chamber towards 12 o’clock. Countertraction was supplied by using a Vera hook (Katena) in the side port. The gonioprism was then reapplied to ensure that the inserter was positioned to engage the angle just anterior to the trabecular meshwork.
The inserter needle was then slowly pushed through the sclera until the needle was seen exiting into the subconjunctival space close to the preoperative markings and, ideally, above Tenon’s capsule. The needle was then rotated towards 12 o’clock. Engagement of the blue lever, which advances and releases the XEN® stent, occurred next, followed by slow advancement. Subsequent slow retraction of the inserter needle resulted in stent placement into the subconjunctival space. The injector was then removed from the eye. Stent positioning in the subconjunctival and anterior chamber stent was confirmed. Tissue or stent manipulation was rarely needed after insertion. Automated irrigation/aspiration was used to remove the viscoelastic from the eye. While doing so, the presence of a bleb superiorly was confirmed. The incisions were hydrated with a balanced salt solution and, where needed, sutured with 10-0 nylon.
Follow-Up Examinations and Postoperative Management
Glaucoma medications were continued until the day of surgery. A washout period was not included. After XEN® gel stent implantation, all glaucoma medications were stopped in the operative eye. Postoperative examinations were performed on day 1, week 1, and months 1, 3, 6, and 12. Additional postoperative visits were scheduled in between these time points, as dictated by the clinical findings. Topical antibiotics were used four times a day for 1 week. Topical steroids were used four times a day for 1 month, then tapered over 4 weeks. Restarting of glaucoma medications, bleb needling, 5-fluorouracil (5-FU) injections, or other interventions were done at the discretion of the surgeon.
Needling and 5-FU Injections
Clinical exam findings determined if and when needling and 5-FU were to be done. Most commonly, eyes had elevated IOP with signs of decreasing bleb function (i.e., lack of microcysts, vascularization, and Tenon’s encapsulation, scarring in and around the external tip of the stent). Needling was performed under microscopic guidance in a minor procedure room. Betadine, antibiotic, and 2% lidocaine were topically applied. A solution of 2% lidocaine, 0.1 ml, was then injected subconjunctivally temporally, and cotton-tipped applicators were used to disperse the lidocaine to the location of the external stent. Under sterile conditions, an angled 27G needle was directed towards the external end of the stent and surrounding fibrosis. Using the tip of the needle, the fibrous adhesions surrounding the external end of the stent were lysed, and an attempt was made to raise the stent above the episcleral and scleral surface. On completion of the procedure, 0.1 ml of 5-FU (50 mg/ml) was injected temporally, and additional antibiotic drops were instilled. Subconjunctival injections of mitomycin could not be used due to institutional regulatory policies. Both topical antibiotic and steroid drops were prescribed four times a day. The antibiotic was stopped at 7 days and the steroid tapered over 4 weeks.
Outcome Measures
Measurements included IOP, medications, and complications. Degree of success was defined by World Glaucoma Association guidelines, which were also used for data presentation [30]. Complete success was defined as an IOP reduction of ≥ 20% and an IOP of < 18 mmHg without medication or any secondary glaucoma intervention. Qualified success was defined as an IOP reduction of ≥ 20% and an IOP < 18 mmHg with and without medication or any secondary glaucoma intervention. Eyes with follow-up that were in neither of these groups were deemed failures.
Statistical Analysis
Data analysis was performed using R 3.4.1 statistical software. The IOP was analyzed by calculating various descriptive statistics, including range, median, and mean. The standard deviation, standard error, and 95% CI were computed around the mean. The change in IOP from preoperative measurements to each of the subsequent time points was also examined. The resultant values were reported as both a numeral and a percentage. These analyses were replicated for various subsets of the data, including XEN® stent standalone procedures versus XEN® stent with cataract surgery. To visualize the data, the following plots were created: (1) combined graph showing mean IOP change, percentage change of mean IOP, and mean medication reduction values from baseline over time, and (2) scatterplots of preoperative and postoperative IOP for 6 months and 12 months.
The above descriptive statistics were also calculated for the raw observed medication use values and the change in medication from preoperative measurements at the study time points. These computations were carried out for the overall study group, the standalone XEN® stent eyes, and the combined XEN® stent and cataract surgery eyes. A Wilcoxon test was chosen to analyze our data. This nonparametric test was chosen over a t test because our data failed the normality assumption.
Results
Forty-seven eyes of 42 patients with medically refractory OAG with visual field and/or optic disc progression underwent XEN® stent insertion (as a standalone procedure or in combination with phacoemulsification) from April 2017 to May 2018. Demographic and baseline characteristics for the patients are displayed in Table 1. The mean age of the study population was 78.15 ± 8.55 years (54–91 years). All patients were white, except for one Asian patient. Regarding the different subtypes of glaucoma, most eyes had primary OAG (n = 32; 68.1%), with the remainder being pseudoexfoliative (n = 11; 23.4%) and low-tension glaucoma (n = 4; 8.5%). Glaucoma staging was severe in all 47 eyes (100%). Patient follow-up was available on 46 eyes at 1 week, 47 eyes at 1 month, 42 eyes at 3 months, 46 eyes at 6 months, and 32 eyes at 12 months. Eleven eyes have not yet reached the 12-month follow-up time point. Two patients (three eyes) died during the study period before reaching their 12-month visit. One patient (one eye) was lost to follow-up at 12 months.
Table 1.
Demographics and baseline characteristics of the total population (n = 42)
| Parameter | Total: 47 eyes of 42 patients |
|---|---|
| Age (years) | |
| Mean ± SD | 78.15 ± 8.55 |
| Range | 54–91 |
| Sex, n (%) | |
| Female | 28 (66.7%) |
| Male | 14 (33.3%) |
| Study eye, n (%) | |
| Right | 20 (42.6) |
| Left | 27 (57.4) |
| Ethnicity, n (%) | |
| White | 41 (97.6%) |
| Asian | 1 (2.4%) |
| Hispanic or Latino | 0 |
| Black/African American | 0 |
| Glaucoma type, n (%) | |
| POAG | 32 (68.1) |
| Pseudoexfoliative | 11 (23.4) |
| Low tension | 4 (8.5) |
| Previous glaucoma procedures | |
| Selective laser trabeculoplasty, n (%) | 20 (42.6) |
| iStent, n (%) | 1 (2.1) |
| Endocyclophotocoagulation, n (%) | 1 (2.1) |
| Filtration or tube surgery, n (%) | 0 |
| IOP at baseline | |
| Mean ± SD | 22.34 (7.34) |
| Range | 11.00–36.00 |
| Mean medications at baseline, n (SD) | 2.96 (1.20) |
| Total number, n (%) | |
| None | 1 (2.1) |
| One | 3 (6.4) |
| Two | 10 (21.3) |
| Three | 22 (46.8) |
| Four | 7 (14.9) |
| Five or more | 4 (8.5) |
| XEN® stent and cataract surgery, n (%) | 27 (57.4) |
| XEN® stent as standalone, n (%) | 20 (42.6) |
| Phakic, n (% of 20) | 7 (35) |
Pseudophakic, n (% of 20) 13 (65)
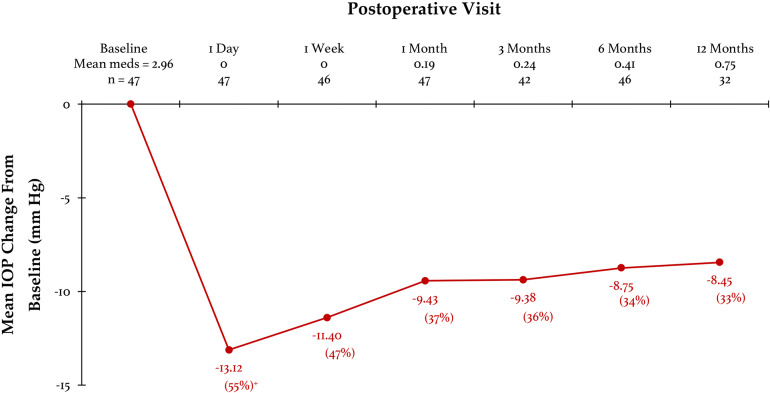
After XEN® stent implantation, the mean change in IOP (Fig. 1) was −13.12 ± 8.42 mmHg, −11.40 ± 8.24, −9.43 ± 8.02 mmHg, −9.38 ± 7.77, −8.75 ± 7.16, and −8.45 ± 7.33 mmHg at 1 day, 1 week, and 1, 3, 6, and 12 months, respectively (95% CI [10.71, 15.52], [9.02, 13.78], [7.13, 11.72], [7.03, 11.73], [6.68, 10.82], and [5.91, 10.99]). Percentage change in IOP from baseline for all eyes (Fig. 1) was 55% ± 27%, 47% ± 27%, 37% ± 26%, 36% ± 27%, 34% ± 24%, and 33% ± 24% at 1 day, 1 week, and 1, 3, 6, and 12 months, respectively (95% CI [47%, 62%], [39%, 54%], [29%, 44%], [28%, 45%], [27%, 41%], and [25%, 41%]). Scatterplots for preoperative and postoperative IOP are shown for 6-month (Fig. 2) and 12-month (Fig. 3) data. On each plot, the line shows the best fit.
Fig. 1.
Mean intraocular pressure (IOP) change and mean medication reduction from baseline for the overall population at each visit after XEN® stent placement. +Percentage change in mean intraocular pressure (IOP) from baseline shown in parentheses
Fig. 2.
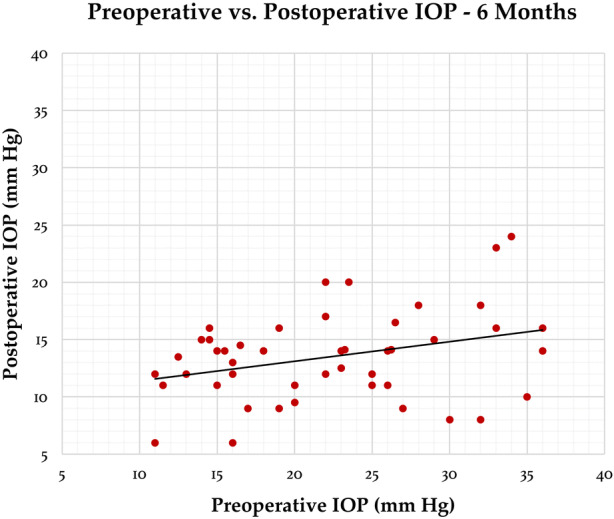
Scatterplot of preoperative and postoperative intraocular pressure (IOP) at 6 months. Line shows best fit
Fig. 3.
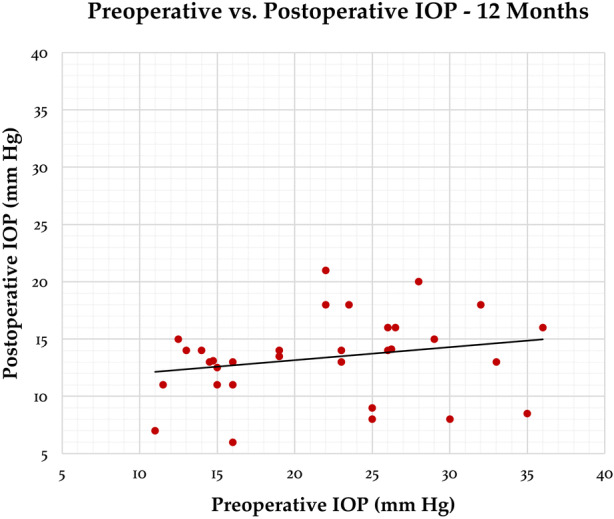
Scatterplot of preoperative and postoperative intraocular pressure (IOP) at 12 months. Line shows best fit
IOP data for standalone XEN® stent versus combined XEN® stent with cataract surgery are shown in Table 2. The small number of eyes in each group prevented meaningful statistical interpretation between groups.
Table 2.
Mean IOP in eyes receiving XEN® stent as a standalone procedure (n = 20) versus XEN® stent with cataract surgery (n = 27)
| IOP (mmHg) | ||||
|---|---|---|---|---|
| XEN® stent standalone | 95% confidence interval | XEN® stent with cataract surgery | 95% confidence interval | |
| Baseline (mean ± SD) | 24.18 ± 8.18 (n = 20) | (20.59, 27.76) | 20.98 ± 6.47 (n = 27) | (18.54, 23.42) |
| 1 week post-op (mean ± SD) | 8.83 ± 4.13 (n = 20) | (7.01, 10.64) | 12.79 ± 5.39 (n = 26) | (10.72, 14.86) |
| 1 month post-op (mean ± SD) | 11.83 ± 3.65 (n = 20) | (10.23, 13.42) | 13.72 ± 4.48 (n = 27) | (12.03, 15.41) |
| 3 months post-op (mean ± SD) | 13.37 ± 5.11 (n = 19) | (11.07, 15.67) | 12.61 ± 3.70 (n = 23) | (11.09, 14.12) |
| 6 months post-op (mean ± SD) | 13.53 ± 4.89 (n = 19) | (11.33, 15.73) | 13.46 ± 3.14 (n = 27) | (12.28, 14.65) |
| 1 year post-op (mean ± SD) | 13.04 ± 4.50 (n = 14) | (10.68, 15.39) | 13.61 ± 2.90 (n = 18) | (12.27, 14.95) |
The mean number of medications at baseline and change after surgery at each time point for the total population are shown in Fig. 1. At baseline, 97.9% of eyes (n = 46) were receiving at least one glaucoma medication. Side effects or ineffectiveness limited the number of glaucoma medications in some eyes. A statistically significant reduction in medications occurred, from 2.96 ± 1.20 (95% CI [2.62, 3.30]) at baseline to 0.75 ± 1.27 (95% CI [0.31, 1.19]) at 1 year.
At 6 months (n = 46), complete success was achieved in 82.6% (n = 38/46), qualified success in 97.8% (n = 45/46), and failure in 2.2% (n = 1/46). For eyes with 1-year follow-up (n = 32), complete success was achieved in 68.8% (n = 22/32), qualified success in 90.6% (n = 29/32), and failure in 9.4% (n = 3/32). Eleven eyes had not yet reached 12-month follow-up. Two patients (three eyes) died before reaching 1-year follow-up, and one patient (one eye) was lost to follow-up.
Adverse Events
Intraoperatively, one eye (2.1%) had a small, nonexpulsive choroidal hemorrhage that self-resorbed without issue. At 1 month, two stents (4.3%) in different patients were noted to have eroded through the conjunctiva, which necessitated immediate stent removal. A detailed review of both eyes was conducted. In each eye, XEN® stent insertion was uneventful, with desired placement above Tenon’s capsule and underneath the conjunctiva. Mitomycin dosing and tissue manipulation were per study protocol. In the early postoperative period, each eye had a single-digit IOP, diffuse bleb, slightly shallow anterior chamber, and shallow serous choroidals. At postoperative day 1, the external portion of the stent was clearly visible; it was straight rather than angulated. However, in each eye, the midsection of the stent bowed anteriorly and pressed against the outer wall of the conjunctival filtration bleb. This appearance persisted throughout the entire month, despite choroidal resolution and anterior chamber deepening. With the thinness of the conjunctiva overlying the stent and concern that manipulation might create a buttonhole, neither stent was repositioned or redirected. Medications followed study protocol. Erosion was noted unexpectedly at the routine 1-month visit. Each eye was white and quiet. Neither patient reported any symptoms or new issues. Intraoperative stent removal was uneventful. In each eye, a second stent was inserted in a new location, away from the erosion. The second stents functioned less optimally than the first, but neither eroded. Fortunately, neither eye developed infection or vision loss from the erosion.
Hypotony (IOP < 6 mmHg) was seen in 10 eyes (21.3%) at day 1, with resolution in all eyes by 2 weeks. No hypotony, maculopathy, hyphema, endophthalmitis, anterior chamber flattening, cystoid macular edema, or perceived mitomycin-related complications occurred. One eye (2.1%) required trabeculectomy. No eyes showed significant loss in visual acuity due to either the procedure or adverse events.
Fourteen of 47 eyes (29.8%) required needling and 5-FU injection 1–3 months postoperatively. Needling was considered part of procedure management and not an adverse event, in agreement with another study [26]. Our 29.8% needling rate is similar to that of previous studies by Hengerer et al. (27.7%) [26], Galal et al. (30.7%) [25], and Grover et al. (32.3%) [28]. Our rate was lower than that reported by Fea et al. (50%) [31], Sheybani et al. (47%) [22], Schlenker et al. (43.2%) [29], and Mansouri et al. (37%) [27]. Our study differed from Grover et al. [28], who inserted the XEN® stent without conjunctiva disruption, but applied mitomycin with a sponge after opening the conjunctiva.
Optimal time for needling with trabeculectomy varies widely, depending on surgical technique, surgeon preference, and patient population [32, 33]. As with trabeculectomy, the reported average time of needling after XEN® stent insertion also varied with Mansouri et al. (4.5 months) [27] and Hengerer et al. [26] (1 week–3 months). In our study, needling was performed at 1–3 months, with improvement in IOP and bleb function in 10 of 14 eyes (71.4%). A second needling was performed in one eye without benefit.
No eyes showed significant loss in visual acuity due to either the procedure or adverse events. No observable corneal decompensation or other anterior segment issues related to the procedure were noted during the study. Endothelial cell counts were not included in this study.
Discussion
Our prospective, noncomparative study found XEN® gel stent surgery in eyes with and without concomitant cataract surgery to be both efficacious and relatively safe. The results of this study based on reduction in IOP and medication use compare favorably with published studies on the XEN® gel stent. In a study with standalone XEN® stent insertion, Grover et al. reported that 75.4% of patients obtained ≥ 20% IOP lowering on similar or fewer medications at 12 months [28]. In 49 eyes, Sheybani et al. reported 36.4% IOP reduction after 1 year, and 89% achieved ≥ 20% IOP lowering [22]. In a study of 149 eyes, 62.1% of patients achieved ≥ 20% IOP lowering, with a 71.1% success rate when defined by an IOP < 16 mmHg (with or without medication) [27]. Galal et al. reported, on average, 23% IOP reduction at 1 year and ≥ 20% IOP lowering without medication in 42% of eyes [25]. Schlenker et al. found a 75% survival rate at about 10 months for complete success at an IOP ≤ 21 mmHg [29]. At 1 year, Fea et al. found a 31.62% reduction in IOP and 82.88% decrease in medication versus baseline [31]. Widder et al. reported a primary success rate (no revision) of 66% and overall success (limited to one revision) of 90% [34]. Hohberger et al. reported a much lower complete success rate (defined as IOP < 18 mmHg at any time point within 6 months of follow-up without local antiglaucomatous therapy or further surgical interventions), with 46.9% in single XEN® gel stents and 53.3% in the combined XEN® stent and cataract surgery group [35].
In our study, the safety profile was favorable overall. The postoperative complications that may occur with trabeculectomy or tube shunt surgery, such as chronic hypotony, flat anterior chamber, hyphema, hypotony maculopathy, kissing choroidal detachments, and bleb dysesthesia, were not seen in this study. One intraoperative, nonexpulsive choroidal hemorrhage occurred, but caused no loss of vision. The two stent erosions (4.3%) resulted in no endophthalmitis or vision loss, but their occurrence stresses the importance of closely monitoring eyes which have a XEN® stent. From previous studies, conjunctival erosion is an infrequent event [24–29, 34, 36]. The issues that did occur that might place eyes at higher risk for erosion include failure to elevate the bleb above the implant, a too-short implant length in the subconjunctival space, and the movement of the upper eyelid over the conjunctiva and implant. These factors did not seem to be the case in our two patients. Each eye had a nicely elevated filtration bleb. However, the midsection of the stent in each eye was bowed, with slight pressure on the conjunctival wall of the filtration bleb. This observation was also mentioned by Widder et al. [34]. Patients with this clinical finding after XEN® stent surgery need to be monitored closely or have surgical revision [33]. Although our experience is limited to two eyes, the positioning did not correct or change over time; therefore, we recommend that eyes with this postoperative finding undergo early revision to avoid conjunctival erosion and the potentially vision-threatening complication of endophthalmitis.
The overall risk of erosion over time is unclear. The design of the XEN® stent makes it much less likely than tube shunts to erode. The XEN® stent is 100 times more flexible than the silicone tube shunt. In addition, the XEN® stent has a much smaller outer diameter than a tube shunt. Theoretically, these features reduce stress on surrounding tissues, with a resulting lower likelihood of erosion and migration. However, with ideal XEN® stent placement above Tenon’s capsule and just underneath the conjunctiva, the risk of erosion may be heightened. This issue is especially important to monitor, because older patients with glaucoma have thin conjunctiva and little Tenon’s capsule; topical glaucoma medications alter the conjunctival surface, and the use of antifibrotic agents inhibit healing during and after surgery. Although no erosions were seen in eyes without a filtering bleb, this may be a problem in the future. Given the many factors involved in this issue, future study is warranted.
Limitations
The study has several limitations. It was a prospective study, but it was also a noncomparative analysis with no control group. In addition, the number of eyes is small. No medication washout was done at baseline; therefore, the unmedicated IOP is unknown. A randomized controlled study with a larger sample size and medication washout may yield different results.
Because all but one patient was white, this study cannot speak to the effectiveness or potential issues with XEN® stent use in other ethnic populations such as African Americans and Hispanics. Neither can this study draw any conclusions about XEN® stent effectiveness based on age.
XEN® stent insertion is relatively straightforward, but as with any surgical procedure, there is a learning curve. As we became more experienced, the stent functioned more favorably when positioned above Tenon’s capsule. Eyes with stent placement more intra-Tenon’s capsule tended towards higher IOPs and a higher incidence of needling. Later eyes may have benefited from more ideal stent positioning. Needling techniques and timing differ among glaucoma surgeons, making it difficult to reach standardized conclusions about this procedure. In this study, needling occurred when clinical exam results suggested restricted aqueous flow. Because no needling took place after 3 months, it is unclear whether this procedure would be beneficial at later stages. Because post-needling antifibrotic medication was limited to 5-FU injections, we cannot comment on the effect of subconjunctival mitomycin-C injections on filtration enhancement.
Despite these study constraints, there is limited long-term data on the use of the XEN® gel stent in the United States due to its relatively recent approval by the FDA. Thus, in spite of its limitations, we hope that this study broadens awareness and knowledge of this new treatment. In 12 months, the procedure has shown effective IOP lowering, a significant reduction in glaucoma medications, and a relatively good safety profile. However, the potential for conjunctival erosion exists, and with the significant needling rate, surgeons performing the procedure need to be comfortable with and knowledgeable about bleb management. In summary, the data from this study support the XEN® gel stent as an effective, relatively safe, and less invasive surgical filtration procedure for patients with medically uncontrolled glaucoma, either as a standalone procedure or combined with cataract surgery.
Acknowledgements
The authors sincerely thank all participants for their involvement in this study.
Funding
No funding or sponsorship was received for this study or publication of this article. The article processing charges were funded by the authors.
Editorial assistance
Editorial assistance and statistics support were supplied and funded by Park Nicollet Clinic and HealthPartners Institute (Mary Van Beusekom, MS, ELS, MWC of HeathPartners Institute).
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship of this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Andrew G. Kalina, Paul H. Kalina, and Morgan M. Brown have nothing to disclose.
Compliance with Ethics Guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the HealthPartners Institute Institutional Review Boards and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all participants in the study for both the procedure itself and inclusion in the study. The HealthPartners Institutional Review Board approved this study.
Data availability
The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Enhanced digital features
To view enhanced digital features for this article go to 10.6084/m9.figshare.8209919.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–267. doi: 10.1136/bjo.2005.081224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kass MA, Heuer DK, Higginbotham EJ, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701–713. doi: 10.1001/archopht.120.6.701. [DOI] [PubMed] [Google Scholar]
- 3.Heijl A, Leske MC, Bengtsson B, et al. Reduction of intraocular pressure and glaucoma progression. Arch Ophthalmol. 2002;120(10):1268–1279. doi: 10.1001/archopht.120.10.1268. [DOI] [PubMed] [Google Scholar]
- 4.Lichter PR, Musch DC, Gillespie BW, et al. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology. 2001;108(11):1943–1953. doi: 10.1016/S0161-6420(01)00873-9. [DOI] [PubMed] [Google Scholar]
- 5.Pisella PJ, Pouliquen P, Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthalmol. 2002;86(4):418–423. doi: 10.1136/bjo.86.4.418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Olthoff CM, Schouten JS, van de Borne BW, et al. Noncompliance with ocular hypotensive treatment in patients with glaucoma or ocular hypertension an evidence-based review. Ophthalmology. 2005;112(16):953–961. doi: 10.1016/j.ophtha.2004.12.035. [DOI] [PubMed] [Google Scholar]
- 7.Goldshtein I, Shalev V, Zigman N, et al. The Maccabi Glaucoma Study: treatment patterns and persistence with glaucoma therapy in a large Israeli health maintenance organization. J Glaucoma. 2016;25(4):e386–e391. doi: 10.1097/IJG.0000000000000380. [DOI] [PubMed] [Google Scholar]
- 8.Sleath B, Blalock S, Covert D, et al. The relationship between glaucoma medication adherence, eye drop technique, and visual field defect severity. Ophthalmology. 2011;118(12):2398–2402. doi: 10.1016/j.ophtha.2011.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prager AJ, Liebmann JM, Cioffi GA, et al. Self-reported function, health resource use, and total health care costs among medicare beneficiaries with glaucoma. JAMA Ophthalmol. 2016;134(4):357–365. doi: 10.1001/jamaophthalmol.2015.5479. [DOI] [PubMed] [Google Scholar]
- 10.Töteberg-Harms M, Berlin MS, Meier-Gibbons F. Increasing healthcare costs: can we influence the costs of glaucoma care? Curr Opin Ophthalmol. 2017;28(2):127–132. doi: 10.1097/ICU.0000000000000343. [DOI] [PubMed] [Google Scholar]
- 11.Odberg T, Sandvik L. The medium and long-term efficacy of primary argon laser trabeculoplasty in avoiding topical medication in open angle glaucoma. Acta Ophthalmol Scand. 1999;77(2):176–181. doi: 10.1034/j.1600-0420.1999.770212.x. [DOI] [PubMed] [Google Scholar]
- 12.Shingleton BJ, Richter CU, Dharma SK, et al. Long-term efficacy of argon laser trabeculoplasty: a 10-year follow-up study. Ophthalmology. 1993;100(9):1324–1329. doi: 10.1016/S0161-6420(93)31480-6. [DOI] [PubMed] [Google Scholar]
- 13.Shingleton BJ, Richter CU, Bellows AR, et al. Long-term efficacy of argon laser trabeculoplasty. Ophthalmology. 1987;94(12):1513–1518. doi: 10.1016/S0161-6420(87)33253-1. [DOI] [PubMed] [Google Scholar]
- 14.Gedde SJ, Schiffman JC, Feuer WJ, et al. Treatment outcomes in the tube versus trabeculectomy (TVT) study after five years of follow-up. Am J Ophthalmol. 2012;153(5):789–803.e2. doi: 10.1016/ajo.2011.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Skuta GL, Parish RK., Jr Wound healing in glaucoma filtering surgery. Surv Ophthalmol. 1987;32(3):149–170. doi: 10.1016/0039-6257(87)90091-9. [DOI] [PubMed] [Google Scholar]
- 16.Watson PG, Jakeman C, Ozturk M, et al. The complications of trabeculectomy (a 20-year follow-up) Eye (Lond). 1990;4(Pt 3):425–438. doi: 10.1038/eye.1900.54. [DOI] [PubMed] [Google Scholar]
- 17.Nouri-Mahdavi K, Brigatti L, Weitzman M, et al. Outcomes of trabeculectomy for primary open-angle glaucoma. Ophthalmology. 1995;102(12):1760–1769. doi: 10.1016/S0161-6420(95)30796-8. [DOI] [PubMed] [Google Scholar]
- 18.Jampel HD, Musch DC, Gillespie BW, et al. Perioperative complications of trabeculectomy in the Collaborative Initial Glaucoma Treatment Study (CIGTS) Am J Ophthalmol. 2005;140(1):16–22. doi: 10.1016/j.ajo.2005.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Chaudhary A, Salinas L, Guidotti J, et al. XEN Gel Implant: a new surgical approach in glaucoma. Expert Rev Med Devices. 2018;15(1):47–59. doi: 10.1080/17434440.2018.1419060. [DOI] [PubMed] [Google Scholar]
- 20.Lewis RA. Ab interno approach to the subconjunctival space using a collagen glaucoma stent. J Cataract Refract Surg. 2014;40(8):1301–1306. doi: 10.1016/j.jcrs.2014.01.032. [DOI] [PubMed] [Google Scholar]
- 21.Vera VI, Horvath C. XEN gel stent: the solution designed by AqueSys. In: Samples JR, Ahmed IIK, editors. Surgical innovations in glaucoma. Springer Science + Business Media: New York; 2014. pp. 189–198. [Google Scholar]
- 22.Sheybani A, Reitsamer H, Ahmed II. Fluid dynamics of a novel micro-fistula implant for the surgical treatment of glaucoma. Investig Ophthalmol Vis Sci. 2015;56(8):4789–4795. doi: 10.1167/iovs.15.16625. [DOI] [PubMed] [Google Scholar]
- 23.Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clin Ophthalmol. 2016;10:189–206. doi: 10.2147/opth.s580490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.De Gregorio A, Pedrotti E, Russo L, et al. Minimally invasive combined glaucoma and cataract surgery: clinical results of the smallest ab interno gel stent. Int Ophthalmol. 2018;38(3):1129–1134. doi: 10.1007/s10792-017-0571-x. [DOI] [PubMed] [Google Scholar]
- 25.Galal A, Bilgic A, Eltanamly R, et al. XEN glaucoma implant with mitomycin C 1-year follow-up: result and complications. J Ophthalmol. 2017;2017:5457246. doi: 10.1155/2017/5457246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hengerer FH, Kohnen T, Mueller M, et al. Ab interno gel implant for the treatment of glaucoma patients with or without prior glaucoma surgery: 1-year results. J Glaucoma. 2017;26(12):1130–1136. doi: 10.1097/IJG.0000000000000803. [DOI] [PubMed] [Google Scholar]
- 27.Mansouri K, Guidotti J, Rao H, et al. Prospective evaluation of standalone XEN gel implant and combined phacoemulsification-XEN gel implant surgery: 1-year results. J Glaucoma. 2018;27(2):140–147. doi: 10.1097/IJG.0000000000000858. [DOI] [PubMed] [Google Scholar]
- 28.Grover DS, Flynn WJ, Bashford KP, et al. Performance and safety of a new ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36. doi: 10.1016/j.ajo.2017.07.023. [DOI] [PubMed] [Google Scholar]
- 29.Schlenker MB, Gulamhusein H, Conrad-Hengerer I, et al. Efficacy, safety, and risk factors for failure of standalone ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124(11):1579–1588. doi: 10.1016/j.ophtha.2017.05.004. [DOI] [PubMed] [Google Scholar]
- 30.Shaaraway TM, Sherwood MB, Grehn F, eds. World Glaucoma Association. Guidelines on design and reporting of glaucoma surgical trials. https://wga.one/wga/guidelines-on-design-reporting-glaucoma-trials/. Accessed 15 May 2019.
- 31.Fea AM, Spinetta R, Cannizzo PML, et al. Evaluation of bleb morphology and reduction in IOP and glaucoma medication following implantation of a novel gel stent. J Ophthalmol. 2017;2017:9364910. doi: 10.1155/2017/9364910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laspas P, Culmann PD, Grus FH, et al. Revision of encapsulated blebs after trabeculectomy: long-term comparison of standard bleb needling and modified needling procedure combined with transconjunctival scleral flap sutures. PloS One. 2017;12(5):e0178099. doi: 10.1371/journal.pone.0178099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rotchford AP, King AJ. Needling revision of trabeculectomies bleb morphology and long-term survival. Ophthalmology. 2008;115(7):1148–1153.e4. doi: 10.1016/j.ophtha.2007.10.023. [DOI] [PubMed] [Google Scholar]
- 34.Widder RA, Dietlein TS, Dinslage S, et al. The XEN45 gel stent as a minimally invasive procedure in glaucoma surgery: success rates, risk profile, and rates of re-surgery after 261 surgeries. Graefes Arch Clin Exp Ophthalmol. 2018;256(4):765–771. doi: 10.1007/s00417-018-3899-7. [DOI] [PubMed] [Google Scholar]
- 35.Hohberger B, Ulrich-Christoph W-L, Lämmer R. MIGS: therapeutic success of combined XEN gel stent implantation with cataract surgery. Graefes Arch Clin Exp Ophthalmol. 2018;256(3):621–625. doi: 10.1007/s00417-017-3895-3. [DOI] [PubMed] [Google Scholar]
- 36.Weinreb RN, Ahmed IIK, Berdahl J, et al. XEN 45: the next generation of MIGS. January/February 2018. Supplement to Glaucoma Today. 2018;16(1):1–16.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.