Abstract
Pediatric trauma is one of the leading causes of morbidity and mortality in children in the USA. Every year, nearly 10 million children are evaluated in emergency departments (EDs) for traumatic injuries, resulting in 250,000 hospital admissions and, unfortunately, 10,000 deaths. Pediatric trauma care in hospitals is distributed across time and space and involves a large and fluid care team. Several clinical teams (including emergency medicine, surgery, anesthesiology, and pediatric critical care) converge to help support trauma care in the ED; this co-location in the ED can help to support communication, coordination and cooperation of team members. The most severe trauma cases often need surgery in the operating room (OR) and are admitted to the pediatric intensive care unit (PICU). Care transitions in pediatric trauma can result in loss of information or transfer of incorrect information, which can negatively affect the care a child will receive. In this study, we interviewed 18 clinicians and asked questions about communication and coordination during care transitions between the ED, operating room and PICU. After the interview was completed, clinicians completed a short questionnaire about patient safety during transitions. Results of our study show that, despite the fact that the many services and units involved in pediatric trauma cooperate well together during trauma cases, often important patient care information is lost when transitioning patients between units. To safely manage the transition of this fragile and complex population, we need to find ways to better manage the information flow during these transitions by, for instance, providing technological support for shared mental models.
Keywords: Pediatric trauma, teamwork, care transitions, patient safety
1. Introduction
Pediatric trauma is one of the leading causes of morbidity and mortality in children in the USA. Every year, nearly 10 million children are evaluated in emergency departments (EDs) for traumatic injuries, resulting in 250,000 hospital admissions and 10,000 deaths. Traffic accidents are by far the leading cause of death for children in the USA [1]. The nature of traumatic injuries creates situations characterized by incomplete or nonexistent information (e.g., non-identified patient) and, thus, ambiguity about the patient’s conditions and treatment [2]. One of the many aspects that make pediatric trauma care in hospitals so complex is the distribution across time, space, and the large and fluid care team that is involved in the care of the child. However, despite the wealth of research on care transitions, (1) most of the literature focuses on shift hand-offs;(2) there is relatively little literature on ED handoffs, and (3) there is less literature on (pediatric) trauma handoffs [3]. Trauma care is characterized by non-routine, non-standardized events. EDs are often described as stressful environments, with an increasing number of high acuity patients, resulting in high time pressure and workload [4,5]. Compared to other routine transitions, trauma transitions are often non-routine with sequences of activities that are less discrete and normalized; therefore, putting patients at high risk of coordination problems [3].
Prior to arriving to the ED, patients are triaged into trauma levels based on perceived injury severity and mechanism: level 1 trauma cases are most urgent with potential immediately life-threatening injuries while level 2 trauma cases are still critical but less likely to have life-threatening injuries. Other pediatric trauma cases may not meet leveling criteria but still require treatment. Pediatric trauma patients often present with multiple injuries, requiring multi-disciplinary care. Depending on the trauma level, several clinical teams (including emergency medicine, anesthesiology, surgery, and pediatric critical care) converge to help support trauma care in the ED. This co-location in the ED can help to support communication, coordination and collaboration of team members. Pediatric trauma patients often need surgery in the operating room (OR) or are admitted to the pediatric intensive care unit (PICU). These transitions can result in loss of information or transfer of incorrect information, which can negatively affect the patient’s care [6,7].
The number of roles involved in pediatric trauma care increases care complexity and can pose challenges to communication and coordination. The number of personnel involved in (pediatric) trauma cases and the potential number of transitions are impressive; more than 50 different roles can be involved and children may experience more than 20 transitions between different services and units before being discharged from the hospital [8–10].
2. Background: care transitions
Patient transitions from one service or unit to another may increase safety risks to the patient [11–14]. Information about the patient should be transferred from care providers (e.g. physicians and nurses) on the sending unit to the receiving unit. However, in reality, there are often gaps in the information flow, or information can be completely omitted. The transfer of information often happens during handoffs. Handoffs are defined as: “a transfer of care involving a transfer of information, responsibility, and authority between clinicians” [15,16]. Results of systematic reviews show that effective handoffs are necessary for successful patient care management activities such as communication and coordination, resulting in better quality of care and improved patient safety [2,16].
There are many types of care transitions, e.g., between shifts of healthcare professionals, hospital units, or care settings. In this study, we focus on inter-departmental care transitions (also known as inter-service handoffs), in particular transitions between the ED and OR, the OR and PICU, and the ED and the PICU. Compared to an intra-departmental transition, inter-departmental transitions carry a high risk because of transfer in at least three domains: provider, department, and physical location, which do not always occur simultaneously [17].
The literature has identified several issues with information transfer during handoffs: omission, lack of data, delayed information, inaccuracies, poorly organized data and information overload [2,18–20]. For example, results of a study by Horwitz et al. [17] examined the transition of adults from ED to inpatient care and found that nearly a third (29%) of survey respondents reported that a patient of theirs experienced a near miss or an adverse advent after a transition. Bigham et al. [21] showed that 26% of handoffs in 23 pediatric hospitals were linked to a handoff-related care failure before the implementation of a standardized hand-off, which decreased these failures to 8%. The study also showed that ED to inpatient (IP) handoffs had some of the highest failures (37% before implementation). The standardized handoff tool reduced ED to IP unit handoff failures to 13% [21]. However, little is known about transitions in pediatric trauma care and factors associated with information flow problems.
The goal of this study is to understand the different transitions and barriers to the flow of information in pediatric trauma. If we better understand the transitions and barriers to the information flow, we can design health information technology that supports the transitions. Eventually, better supported care transitions should lead to fewer missed injuries, reduced delay in care, increased patient and family involvement, lower clinician frustration and more satisfaction.
3. Methods
3.1. Setting and sample
This study took place in an academic hospital in the Midwestern USA. The participating hospital is an American College of Surgeons certified level 1 pediatric and adult trauma center [22,23], with an 87-bed children’s hospital, 8 pediatric operating rooms and a 21-bed PICU. The pediatric ED receives about 300 pediatric trauma patients per year. On average, about 40 of those patients are level 1 (highest acuity) patients and more than 250 are level 2 patients. The average length of stay (LOS) for level 1 patients is 8 days (median: 3.5 days, range: 1 to 102 days); the average LOS for level 2 patients is 2 days (median: 1 day, range: 1 to 46 days). Healthcare professionals, i.e. nurses, physicians and other support staff, in the ED, OR and PICU were involved in the study; physicians, i.e. attendings, fellows and residents, are on the emergency medicine, surgery, anesthesia or pediatric critical care services. At the hospital, pediatric trauma care is initiated in the ED where a specialized pediatric trauma team cares for the patient. After care is provided in the ED, the patient may be transferred to another unit or discharged. The majority (60%) of pediatric level 1 patients are transferred to the PICU, 19% to the OR, 14% to the floor, 7% are discharged and 3% are deceased. Of the level 2 pediatric patients, 4% are transferred to the OR, 9% to the PICU, 48% to the floor and 42% are discharged from the ED. We conducted interviews on transitions of care between the ED and OR, OR and PICU, and ED and PICU with 18 people (see Table 1). Fourteen of the interviewees were female. On average, the respondents (including the residents) had more than six years of experience in health care.
Table 1.
Interviewee and survey respondent characteristics
| # | Service/Unit | Job Title | Transitions | Duration |
|---|---|---|---|---|
| 1 | ED | ED RN | ED->OR, ED->PICU | 0:56 |
| 2 | ED | ED RN | ED->OR, ED->PICU | 1:06 |
| 3 | ED | Coordinator | ED->OR, ED->PICU | 0:37 |
| 4 | ED | Child life specialist | ED->OR, ED->PICU | 0:55 |
| 5 | ED | Resident | ED->OR, ED->PICU | 0:54 |
| 6 | Anesthesia | Attending | ED->OR, OR->PICU | 0:51 |
| 7 | Anesthesia | Resident | ED->OR, OR->PICU | 0:50 |
| 8 | Anesthesia | Certified Nurse Anesthetist | ED->OR, OR->PICU | 0:57 |
| 9 | OR | OR nurse manager | ED->OR, OR->PICU | 0:44 |
| 10 | OR | Care team leader | ED->OR, OR->PICU | 0:44 |
| 11 | OR | Circulating RN | ED->OR, OR->PICU | 0:54 |
| 12 | OR | Director of surgical services | ED->OR, OR->PICU | 1:02 |
| 13 | Surgery | Resident | ED->OR, OR->PICU | 0:53 |
| 14 | Surgery | Resident | ED->OR, OR->PICU | 0:58 |
| 15 | PICU | PICU RN/ care team leader | ED->PICU, OR->PICU | 1:04 |
| 16 | PICU | Care team leader | ED->PICU, OR->PICU | 0:45 |
| 17 | PICU | Fellow | ED->PICU, OR->PICU | 0:49 |
| 18 | PICU | Fellow | ED->PICU, OR->PICU | 0:29 |
| Total | 14:44 |
3.2. Procedure
We first conducted four one-hour interviews with research team members (pediatric ED attending physician, pediatric surgery attending physician, PICU attending physician, and pediatric trauma manager) about teamwork and care transitions in pediatric trauma to get a better understanding of the process and refine the interview guide. The four initial interviews were excluded from data analysis. After these four initial interviews, we used purposeful sampling to identify clinicians who are knowledgeable about the pediatric trauma care process. We contacted potential participants with a description of the project via email and participation was voluntary. Once participants agreed to be interviewed, we scheduled a meeting at the hospital for about an hour, most of the time at the beginning or end of their shift. We used a semi-structured interview guide to ask about pediatric trauma care transition processes between the ED, OR and PICU, including communication and coordination. At the end of the interview, clinicians filled out a short questionnaire about patient safety during transitions (response rate: 100%). The study protocol was reviewed and approved by the University of Wisconsin-Madison Internal Review Board (IRB).
3.3. Data collection and analysis
Interviews.
An interview guide was developed to collect data on the different transitions, and barriers and facilitators to these transitions. Participants were asked to describe a pediatric trauma case transition, including the start and the end of the transition, the people who participate in the transitions, what information was provided by the interviewee during the transition, what information s/he received, what technologies and tools were used, who accompanies the patient when she leaves, who is with the patient during the transfer, who is with the patient when they arrive at the receiving unit/service, etc. In addition, questions were asked about what is being done to prepare for the transitions, and any follow-up that occurs. Participants were also asked to provide an example of a pediatric trauma transition from ED to OR (or OR to PICU, or ED to PICU) that went well and an example of a transition that went poorly. All questions were asked for both level 1 and level 2 patients. The interview guide can be found here: https://cqpi.wiscweb.wisc.edu/wp-content/uploads/sites/599/2016/08/Pediatric-Trauma-Transitions-Interview-Guide.pdf. All interviews were audio-recorded, transcribed, and then uploaded to a qualitative data analysis software (Dedoose®). The interviews lasted between 30 minutes and little more than an hour (average duration: 51 minutes). In total, the 18 interviews lasted nearly 15 hours. One interview was conducted with two interviewees (interviewees #9 and #10 in Table 1). The interview data analysis in Dedoose® focused on text that indicated problems with information flow in the transitions. The interviews contained 22 excerpts with these problems. The analysis process identified four themes for barriers to information flow: (1) information is not available, (2) information is available but not transferred, (3) information is transferred but there is information loss during the transfer, and (4) incorrect information is transferred.
Survey.
Clinicians filled out a short version of the AHRQ Hospital Survey on Patient Safety Culture (HSPC) [24] about patient safety during transitions. HSPC contains 11 questions about care transitions and communication, coordination and cooperation. Three questions about hospital management and patient safety were not used in this project. Two of the remaining 8 questions asked about shift changes; the wording in these questions was changed to transitions between units. The survey can be found here: http://cqpi.wisc.edu/wp-uploads/2018/05/AHRQ-Patient-Safety-Survey-in-Peds-Trauma-Transition-Interviews.pdf. Survey data were entered in SPSS©. Frequencies and percentages were calculated for the individual items.
4. Results
4.1. Survey
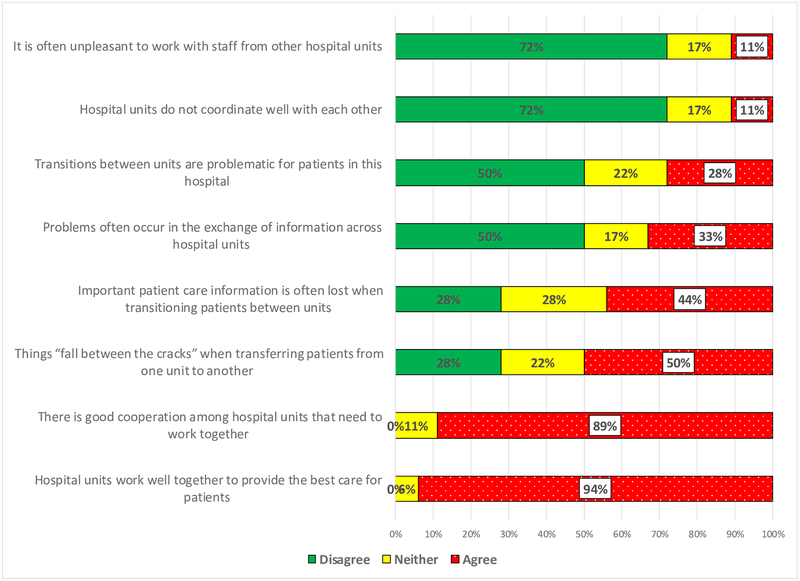
Results of the survey show that, despite many services and units involved in pediatric trauma cooperating well together during trauma cases (94% of respondent agree with that statement, see Figure 1), “Important patient care information is often lost when transitioning patients between units” (44% of respondents agree) and “Things ‘fall between the cracks’ when transferring patients from one unit to another” (50% of respondents agree).
Figure 1:
Perceptions of care transitions (N=18)
4.2. Interviews
Results of the qualitative analyses of the interview data identified four themes: (1) information not available or accessible, (2) information is available but not transferred, (3) transferred information is incomplete, and (4) transferred information is not accurate or incorrect; see Table 2.
Table 2:
Problems with information transfer during pediatric trauma transitions
| Problem with information flow | Description | ED-OR | OR- PICU | ED- PICU |
|---|---|---|---|---|
| 1 Information not transferred because the information is not available or not accessible | Sending party does not have the information and can therefore not transfer information to receiving party, or sending party does have information, but information is not (yet) recorded or not accessible and can therefore not be transferred to receiving party | 6 | 2 | 3 |
| 2 Information is not transferred because of omission | Information is available, but information does not get transferred from the sending to receiving party | 1 | 1 | 1 |
| 3 Information transfer is incomplete or loss of information during transfer | Information is available but during transfer from sender to receiver, information gets lost | 1 | 3 | 3 |
| 4 Inaccurate information transferred | Correct information is available, but during transition from sender to receiver, information becomes inaccurate | 0 | 0 | 1 |
| Total | 8 | 6 | 8 |
Note: The numbers in the table refer to the number of excerpts
Information is not available or not accessible.
Information that is not available or not accessible can be a problem for pediatric trauma. For example, because the patient may be unconscious or the parents have not arrived to the ED yet, information about the patient may not be available. [“A lot of times you don’t know a history on the patient, or what you know is very limited, so vital signs, the history of the event, so, you know, is this a car accident or a burn or whatever, the lines, what you’ve given as far as medications, blood, fluids, anything that basically is going to have an impact on the next couple of hours, any trends that they’ve had” -ED nurse]. Trauma cases, and especially level 1 cases, can be life-threatening situations and significant effort is spent on stabilizing the patient. During initial patient care in the ED, the care team may focus on the main, high priority injury(ies) and may miss other low(er) priority injuries (or injuries were noticed but not recorded). Time pressure due to the critical nature of the patient can contribute to missed injuries, i.e., information is not available. Information may not be available nor accessible for a transition from ED to OR due to lack of necessary resources. For example, staffing considerations (e.g., overcrowding, multiple trauma cases, high acuity cases) may impact the allocation of a dedicated resource to documentation. While one nurse is usually assigned to document patient care, in severe cases, this nurse may need to assist with the patient, and therefore cannot document. [“With some patients though, they’re sick enough that that nurse can’t chart. They have to jump in and hang blood or, you know, so in theory, there’s always a nurse charting and a nurse doing, but sometimes you need two or three nurses” ED Nurse]. Sometimes there is not enough time to enter all available information in the EHR (information overflow), which can be aggravated by EHR usability issues. For example, information may be available, but not recorded due to distraction, and is ‘lost’. [“And a lot of times it’s like the critical information, you get a distraction, and then it goes from your memory. But like I said, my experience has been the very severe cases”, ED Nurse].
Information is available but is not transferred.
Sometimes, the information is available, but is not transferred. In some situations, the receiving unit is not notified about a patient’s transfer before their arrival on the unit. This is sometimes caused by an adult ED team taking care of the pediatric patient and not being familiar with procedures for pediatric patients [“… But the trauma team that takes care of the patient in the ED is the adult trauma team. And then they, oftentimes the kid doesn’t need surgery, so they’ll just admit them directly to the PICU or to the floor, and then they become a pediatric general surgery patient, but we’re not always told that the patient even exists”, Anesthesia intern]. The receiving unit then does not receive information about the patient. [“…It’s like I didn’t even realize this patient was on the unit. The surgeon is nowhere to be found, and the anesthesiologist has started a case, went home… And so in that scenario, it’s really just a lot of loss of things, a lot of loss of information that was, you know, they never passed on or maybe never documented or and then wasn’t verbally passed onto our team. So that’s kind of the worst”, PICU Fellow].
Incomplete information or loss of information.
The sending unit may have information but fails to transfer it adequately to the receiving unit, for example because the people involved in the information exchange have changed, e.g., over shift change. The clinical team on the receiving unit may have specific questions; if they try to contact the physician or nurse from the sending unit after shift change, the individual who cared for the patient may no longer be available. The same issue may happen with shift change in the receiving unit. [“And that’s a pretty detailed report we would give to the floor nurse or the ICU nurse. The only hard thing about it is that sometimes, depending on how long the patient is going to be in the OR, it may be a change of shift before that patient gets up to the unit. So then it’s like kind of playing telephone with having to make sure they all get the right information, if they have to pass the information to a next nurse”, ED Nurse]. Several interviewees mentioned information loss when the information is exchanged only through written documentation. Verbal communication often contains more details than written communication, and the opportunity for questions and feedback is missing from non-verbal, written communication. [“…I think just the words that you use to describe them are different, verbally versus just on paper. You could, and then it’s a conversation, right, and you could ask questions. So when you get, have a chance to have a conversation with someone, it’s just, there’s just that much more information that gets passed on. There’s less likely things get missed… So there’s just a lot of things that aren’t communicated just by the written word. To a lesser extent, the same can happen when the information is exchanged over the phone, and not face-to-face” PICU Fellow]. Information may also be lost when information is only transferred from one role in the sending unit (e.g. nurse) to the same role (nurse) in the receiving unit rather than communication between all roles and team members. Information that is important to the other roles in the care team (e.g. physician, physical therapist) may not be shared.
Inaccurate information.
One interviewee made comments about incorrect or inaccurate information during a transfer. One example is when the patient has received a preliminary diagnosis in the ED, but that diagnosis needs to be confirmed by diagnostic tests, e.g., imaging and labs. If the patient is transferred with a preliminary diagnosis before test results have been received, the results may arrive to the ED but not communicated to the receiving unit, resulting in a failure to confirm/reject the preliminary diagnosis or additional, unnecessary testing. Another example is information that is incorrectly entered in the electronic system. For example, a bed may have been assigned to a patient, but upon arrival in the receiving unit, the bed is already taken by another patient. [“It might just be whoever, coordinators or something might have put the wrong thing in or, so it physically won’t let us go any further if a patient is already in that bed in the PICU. So again, I just call and say, hey, I’ve got a, you know, bed 48 down but it says it’s occupied, and they’ll go, oh, yeah, they should go in here”, ED Coordinator].
5. Conclusion and Discussion
5.1. Conclusion
Pediatric trauma care transitions are complex, involve very vulnerable patients and several different hospital services, units and clinicians. To safely manage the transition of this fragile and complex patient population, we need to better manage the information flow during these transitions. Results of our study confirm the potential information loss during pediatric trauma transitions. Although the many services and units involved in pediatric trauma work well together during trauma cases, important patient care information can get lost when transitioning patients between units and services and “Things ‘fall between the cracks’ when transferring patients from one unit to another”. Results of our interview analysis show that during the transitions, information may not be available or accessible, incomplete, or inaccurate. It is not always possible to strictly separate these four categories from each other. They are not independent and what happens in an early stage can have an effect on later stages of the care process. For example, a level 1 pediatric trauma patient gets to the ED and the ED physician suspects a certain medical condition and orders laboratory tests to confirm the preliminary diagnosis. However, before the test results are available, the patient (with the preliminary diagnosis) has been transferred to the OR and then to the PICU. The tests are ordered in the ED and therefore the results are sent to the ED. Sometimes this information is forwarded to the next service(s), but sometimes it is not. The preliminary diagnosis, even if the test results would have changed this diagnosis, may remain the same during the patient trajectory in the different units and services. Information problems in the transitions between the ED and OR or PICU often involve situations where the information is not (yet) available or accessible. In trauma cases, the information may not be available and in pediatric trauma cases, the child often cannot provide information. The potentially limited time and personnel resources in the ED during a trauma case, and the fact that the diagnostic process has not been completed yet compound to the problem. Finally, the often hectic and stressful nature of a trauma case means that a standardized handoff between ED and OR may not be possible. Results show further that information loss occurs in the transitions between OR and PICU and ED and PICU. Our results confirm the study by Zakrison et al. [25] that showed that in nearly 25% of patients, injuries were missed in the transition from ED to PICU, and in 48% of patients, information discrepancies occurred. Interestingly, the transition from OR to PICU is a team handoff that may reduce information loss. Some studies have demonstrated the benefits of team handoffs [26], but there are also some negative consequences. First, team handoffs require effort and coordination. Second, when team handoffs are not well organized, and for example, the physician and nurse handoff take place at the same time, participants can have problems focusing. Research is needed to further explore advantages and disadvantages of team handoffs, as well as develop other solutions for better managing the information flow during care transitions.
5.2. Discussion
Several “mechanisms” are proposed to improve care transitions, including the transfer of information, and prevent information loss, such as a better organization of the process, organizational change and health information technology (IT) support.
Organized handoff to support the (individual) handoff.
Several tools have been developed to support care transitions such standardized tools (e.g. SBAR), mnemonics (memory aids), checklist, handoff tools (for example I-pass) and other health IT tools. Some of these tools have been successful in improving information transfer during transitions. However, most of the literature focuses on inpatient transitions and not on transitions from the ED to inpatient units. More research is needed to study handoffs between ED and hospital services/units, and how these handoffs can be improved.
Organizational change to support the transitions.
Organizational changes have been implemented to support care transitions. Certified level 1 trauma centers require personnel from different services and units to be present during level 1 and 2 trauma cases in the ED. When attending physicians and sometimes nurses from surgery, anesthesiology, OR and the PICU are present during a trauma case in the ED, the need for a handoff is greatly reduced: the receiving unit/service already has the information needed to take care of the patient. While this organizational intervention may have benefits, there are also some drawbacks. First, it requires resources in time and personnel. Second, during a trauma case, the large number of people impede identifying individual roles, including what information they need and/or possess. The trauma team response does not necessarily impact the OR to PICU transition, and so different ways of organizing that handoff have been developed, e.g., team handoff. Research should evaluate the impact of this team organization of care transition.
Information technology to support the transitions.
Health information technology can help in addressing information loss. Several studies have shown that health IT can support handoffs [27,28]. For example, I-pass is an evidence-based package of interventions that has been shown to reduce communication problems during handoffs [29,30].
Some solutions to address information flow problems in care transitions have been successful. The care transition literature shows that, in general, well-designed interventions that consider the whole work system are more effective than single, narrow interventions [31]. However, it may be difficult to apply some of these solutions to trauma care. The high-speed environment of trauma care with non-routine work processes does not always allow for successful application of these standardized solutions. Our larger study aims to better understand the communication and information transfer issues, and formulate design requirements for a health IT tool that can support the clinicians in these fast-paced, sometimes life-threatening situations by increasing situation awareness and supporting teamwork.
5.3. Study limitations
The study took place in one academic hospital, which makes it difficult to generalize results to other hospitals. Further, we only examined transitions from ED to OR, OR to PICU and ED to PICU, but not other transitions such as the transitions from ED, OR or PICU to hospital medical units. During the interviews, we asked clinicians about pediatric trauma transitions, and barriers and facilitators to transitioning pediatric trauma patients from one service/unit to another, but not specifically about problems with information flow. This resulted in a limited number of excerpts for analysis. Future studies should specifically focus on the transfer of information during transitions, to better understand all of the different types of information that is missing, incomplete or inaccurate. Finally, survey results are based on only 18 respondents, which also makes it difficult to generalize the results. A strength of the study is that we interviewed a wide range of roles involved in the pediatric trauma transition processes, providing us with a fairly complete description of care transitions and associated challenges of information flow.
Acknowledgments
Funding for this research was provided by the Agency for Healthcare Research and Quality (AHRQ) [Grant No. R01 HS023837]. The project described was supported by the Clinical and Translational Science Award (CTSA) program, through the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS), [Grant UL1TR002373]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the funding agencies. We thank the study participants, as our research would not be possible without them.
Footnotes
Conflict of Interest:
The authors have no conflict of interest
References
- 1.Center for Disease Control (CDC) (2015) Ten Leading Causes of Death and Injury. CDC; https://www.cdc.gov/injury/images/lc-charts/leading_causes_of_death_age_group_2015_1050w740h.gif. Accessed January 25 2018 [Google Scholar]
- 2.Apker J, Mallak LA, Gibson SC (2007) Communicating in the “gray zone”: perceptions about emergency physician hospitalist handoffs and patient safety. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 14 (10):884–894. doi: 10.1197/j.aem.2007.06.037 [DOI] [PubMed] [Google Scholar]
- 3.Catchpole KR, Gangi A, Blocker RC, Ley EJ, Blaha J, Gewertz BL, Wiegmann DA (2013) Flow disruptions in trauma care handoffs. The Journal of surgical research 184 (1):586–591. doi: 10.1016/j.jss.2013.02.038 [DOI] [PubMed] [Google Scholar]
- 4.Estryn-Behar M, Doppia MA, Guetarni K, Fry C, Machet G, Pelloux P, Aune I, Muster D, Lassauniere JM, Prudhomme C (2011) Emergency physicians accumulate more stress factors than other physicians-results from the French SESMAT study. Emergency medicine journal : EMJ 28 (5):397–410. doi: 10.1136/emj.2009.082594 [DOI] [PubMed] [Google Scholar]
- 5.Johnston A, Abraham L, Greenslade J, Thom O, Carlstrom E, Wallis M, Crilly J (2016) Review article: Staff perception of the emergency department working environment: Integrative review of the literature. Emergency medicine Australasia : EMA 28 (1):7–26. doi: 10.1111/1742-6723.12522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kitch BT, Cooper JB, Zapol WM, Marder JE, Karson A, Hutter M, Campbell EG (2008) Handoffs causing patient harm: a survey of medical and surgical house staff. Jt Comm J Qual Patient Saf 34 (10):563–570 [DOI] [PubMed] [Google Scholar]
- 7.Dojmi Di Delupis F, Pisanelli P, Di Luccio G, Kennedy M, Tellini S, Nenci N, Guerrini E, Pini R, Franco Gensini G (2014) Communication during handover in the pre-hospital/hospital interface in Italy: from evaluation to implementation of multidisciplinary training through high-fidelity simulation. Internal and Emergency Medicine 9 (5):575–582. doi: 10.1007/s11739-013-1040-9 [DOI] [PubMed] [Google Scholar]
- 8.Wooldridge AR, Carayon P, Hoonakker P, Hose B-Z, Ross J, Kohler J, Brazelton T, Eithun B, Kelly M, Dean S, Rusy D, Gurses A (2017) Understanding Team Complexity in Pediatric Trauma Care. Paper presented at the Human Factors and Ergonomics in Healthcare Conference, New Orleans, LO, March 5–8, 2017 [Google Scholar]
- 9.Durojaiye AB, McGeorge NM, Puett LL, Stewart D, Fackler JC, Hoonakker PLT, Lehmann HP, Gurses AP (2018) Mapping the flow of pediatric trauma patients using process mining on trauma registry data. Applied Clinical Informatics 09 (03):654–666. doi: 10.1055/s-0038-1668089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wooldridge AR, Carayon P, Hoonakker PLT, Hose B-Z, Ross JC, Kohler JE, Brazelton TB, Eithun BL, Kelly MM, Dean SM, Rusy DA, Durojaiye A, Gurses AP (2018. Published online) Complexity of the Pediatric Trauma Care Process: Implications for Multi-Level Awareness. Cognition, Technology and Work. doi: 10.1007/s10111-018-0520-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Academy of Pediatrics Committee on Pediatric Emergency Medicine (2016) Handoffs: Transitions of Care for Children in the Emergency Department. Pediatrics 138 (5):1–12. doi: 10.1542/peds.2016-2680 [DOI] [PubMed] [Google Scholar]
- 12.Gandhi TK (2005) Fumbled handoffs: one dropped ball after another. Ann Intern Med 142 (5):352–358 [DOI] [PubMed] [Google Scholar]
- 13.Calleja P, Aitken LM, Cooke ML (2011) Information transfer for multi-trauma patients on discharge from the emergency department: mixed-method narrative review. Journal of advanced nursing 67 (1):4–18. doi: 10.1111/j.1365-2648.2010.05494.x [DOI] [PubMed] [Google Scholar]
- 14.Commission Joint (2012) Joint Commission Center for Transforming Healthcare releases targeted solutions tool for hand-off communications. Joint Commission perspectives Joint Commission on Accreditation of Healthcare Organizations 32 (8):1, 3 [PubMed] [Google Scholar]
- 15.Arora VM, Johnson JK, Meltzer DO, Humphrey HJ (2008) A theoretical framework and competency-based approach to improving handoffs. Qual Saf Health Care 17 (1):11–14. doi: 10.1136/qshc.2006.018952 [DOI] [PubMed] [Google Scholar]
- 16.Abraham J, Kannampallil T, Patel VL (2014) A systematic review of the literature on the evaluation of handoff tools: implications for research and practice. J Am Med Inform Assoc 21 (1):154–162. doi: 10.1136/amiajnl-2012-001351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horwitz LI, Meredith T, Schuur JD, Shah NR, Kulkarni RG, Jenq GY (2009) Dropping the Baton: A Qualitative Analysis of Failures During the Transition From Emergency Department to Inpatient Care. Annals of Emergency Medicine 53 (6):701–710.e704. doi: 10.1016/j.annemergmed.2008.05.007 [DOI] [PubMed] [Google Scholar]
- 18.Arora VM, Johnson JK, Lovinger D, Humphrey HJ, Meltzer DO (2005) Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 14 (6):401–407. doi: 10.1136/qshc.2005.015107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sharma A, Lo V, Lapointe-Shaw L, Soong C, Wu PE, Wu RC (2017) A time-motion study of residents and medical students performing patient discharges from general internal medicine wards: a disjointed, interrupted process. Internal and Emergency Medicine 12 (6):789–798. doi: 10.1007/s11739-017-1654-4 [DOI] [PubMed] [Google Scholar]
- 20.Beach C, Croskerry P, Shapiro M (2003) Profiles in patient safety: emergency care transitions. Academic emergency medicine : official journal of the Society for Academic Emergency Medicine 10 (4):364–367 [DOI] [PubMed] [Google Scholar]
- 21.Bigham MT, Logsdon TR, Manicone PE, Landrigan CP, Hayes LW, Randall KH, Grover P, Collins SB, Ramirez DE, O’Guin CD, Williams CI, Warnick RJ, Sharek PJ (2014) Decreasing Handoff-Related Care Failures in Children’s Hospitals. Pediatrics. doi: 10.1542/peds.2013-1844 [DOI] [PubMed] [Google Scholar]
- 22.Notrica DM, Brown D, Garcia-Filion P (2011) Development of a pediatric Level 1 trauma center at a freestanding children’s hospital: staff attitudes and perceptions before and after trauma designation. Journal of pediatric surgery 46 (9):1764–1770 [DOI] [PubMed] [Google Scholar]
- 23.Acosta CD, Delgado MK, Gisondi MA, Raghunathan A, D’Souza PrA, Gilbert G, Spain DA, Christensen P, Wang NE (2010) Characteristics of pediatric trauma transfers to a level I trauma center: implications for developing a regionalized pediatric trauma system in California. Academic emergency medicine 17 (12):1364–1373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sorra J, Gray L, Streagle S, Famolaro T, Yount N, Behm J, (2016) AHRQ Hospital Survey on Patient Safety Culture: User’s Guide. Agency for Healthcare Research and Quality (AHRQ), Rockville, MD [Google Scholar]
- 25.Zakrison TL, Rosenbloom B, McFarlan A, Jovicic A, Soklaridis S, Allen C, Schulman C, Namias N, Rizoli S (2016) Lost information during the handover of critically injured trauma patients: a mixed-methods study. BMJ quality & safety 25 (12):929–936. doi: 10.1136/bmjqs-2014-003903 [DOI] [PubMed] [Google Scholar]
- 26.Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM (2011) Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatric critical care medicine : a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies 12 (3):304–308. doi: 10.1097/PCC.0b013e3181fe25a1 [DOI] [PubMed] [Google Scholar]
- 27.Bernstein J, MacCourt DC, Jacob DM, Mehta S (2010) Utilizing Information Technology to Mitigate the Handoff Risks Caused by Resident Work Hour Restrictions. Clinical Orthopaedics and Related Research 468 (10):2627–2632. doi: 10.1007/s11999-010-1376-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sanchez LD, Chiu DT, Nathanson L, Horng S, Wolfe RE, Zeidel ML, Boyd K, Tibbles C, Calder S, Dufresne J, Yang JJ (2017) A Model for Electronic Handoff Between the Emergency Department and Inpatient Units. The Journal of Emergency Medicine 53 (1):142–150. doi: 10.1016/j.jemermed.2017.03.027 [DOI] [PubMed] [Google Scholar]
- 29.Starmer AJ, Landrigan CP (2015) Changes in medical errors with a handoff program. N Engl J Med 372 (5):490–491. doi: 10.1056/NEJMc1414788 [DOI] [PubMed] [Google Scholar]
- 30.Joint Commission (2017) Inadequate hand-off communication. Sentinel Alert Event (58):1–6 [PubMed] [Google Scholar]
- 31.Keebler JR, Lazzara EH, Patzer BS, Palmer EM, Plummer JP, Smith DC, Lew V, Fouquet S, Chan YR, Riss R (2016) Meta-Analyses of the Effects of Standardized Handoff Protocols on Patient, Provider, and Organizational Outcomes. Human factors 58 (8):1187–1205. doi: 10.1177/0018720816672309 [DOI] [PubMed] [Google Scholar]