Abstract
Introduction
Although the interest is growing in topical low-dose atropine to control myopia in schoolchildren worldwide, its use in children of European ancestry remains controversial and solid evidence is sparse. The Oxford Centre for Evidence Based Medicine (OCEBM) classifies the evidence for this therapy as level I for East Asian populations, but only level IV in non-Asian populations.
Methods
Fifty-six children, aged a median of 11 years (range 6–17), were analysed after 12 months of topical treatment with 0.01% preservative-free atropine in both eyes at bedtime every day. Efficacy was assessed during treatment every 6 months. In a subset of 20 patients, treatment of the second eye was delayed by 1 day to enable a controlled safety assessment of side effects such as pupil dilation, hypoaccommodation, and near vision reduction.
Results
Prior to treatment, the mean myopic progression was estimated as 1.05 D/year; after 12 months of treatment with 0.01% atropine, it was 0.40 D/year (p < 0.0001). The only consistently measurable side effect was the induction of 1 mm pupil dilatation, which was only noticeable in comparison to the non-treated eye during the safety investigation.
Conclusions
Topical low-dose atropine appears to be safe and efficacious also in a cohort of European schoolchildren. These data should motivate researchers to conduct more randomised clinical trials.
Keywords: Atropine, Children, Low-dose, Myopia, Progression
Introduction
Myopia is the most common developmental eye disorder. In 2000, 23% of the world population were estimated myopic, and the worldwide prevalence is expected to increase to 50% by the year 2050 [1]. Recent European data on myopia prevalence published by the E3-consortium [2] indicate that 47% of 25–29-year-old individuals are myopic, based on non-cycloplegic measurements. Myopia is the major risk factor (after age) for developing degenerative eye diseases such as cataract, glaucoma, retinal detachment, and macular degeneration, and not just in severely myopic individuals [3]. It is one of the five ocular conditions identified as immediate priorities by the WHO’s Global Initiative for the elimination of avoidable blindness [4]. Myopia usually commences during primary school and progresses until a mean age of 16 years [5]. Therefore, controlling myopia in adolescents is essential, and can be considered an unmet medical need.
Topical atropine for myopia control has been known for over 100 years [6], but its use at standard concentrations is hampered by side effects. Not until 2012 did the positive outcome of the ATOM-2 trial in Singapore spark worldwide interest in low-dose atropine eye drops [7], which demonstrated that atropine 0.01% application produced a decrease in myopia progression from 1.20 to 0.49 Diopters (D) over 2 years without a rebound after cessation and only negligible side effects. The trial used a historical control group, but did not have a parallel control group. Further, it revealed no measurable effect on axial eye growth at this concentration. The more recent LAMP trial from Hong Kong demonstrated a dose-dependent effect of topical atropine at concentrations of 0.05, 0.025 and 0.01% compared to placebo [8]. In these four groups, the progression over 1 year was 0.27, 0.46, 0.59, and 0.81 D, respectively. The lowest concentration did not decrease axial eye growth significantly. Hence, up to now, only two randomised clinical trials from Asia qualify as adequately powered and present data favouring low-dose atropine. Two meta-analyses [9, 10] advocate the use of low-dose atropine eye drops for myopia control, but also recommend further clinical trials, especially in non-Asian populations. A very recent, seminal review addresses the lack of robust evidence outside East Asia justifying the unrestricted use of low-dose atropine as a means to control myopia [11].
Here, we report pilot data on the rate of myopia progression before and after treatment with atropine 0.01% in a single centre cohort of children from southwest Germany, collected in preparation for a larger randomised clinical trial. In a subset of our cohort, we systematically investigated the short-term rate and extent of side effects.
Methods
Population, Ethics and Legal Issues
The compilation of this cross-sectional, single centre, observational case series was approved by our institutional Ethics Committee (Institutional Review Board Approval University of Freiburg #287/16) and adhered to the tenets of the Declaration of Helsinki. Informed parental consent with regard to the therapy and data capture, as well as the off-label use of low-dose atropine, was obtained at the time of first presentation. This observational investigation was carried out within the clinical routine, and hence did not fall under the auspices of the German drug law.
Between June 2014 and December 2017, we started 56 children on bilateral topical therapy with 0.01% atropine at bedtime. Inclusion criteria were an age between 6 and 17 years and a myopic progression ≥ 0.5 D during the year prior to inclusion. Iris colour was classified as light or dark [12]. Our exclusion criteria were non-European ancestry, myopia acquired before primary school, any organic eye disease, strabismus, prematurity and pre-treatment with atropine. Two children were excluded from analysis during follow-up because they used multifocal contact lenses concurrently; one child was lost to follow-up at the 12-months visit.
Refraction
Progression in the year prior to therapy was assessed by relying on the current refraction compared to their previous prescription or information provided by the family ophthalmologist or optician. We performed non-cycloplegic automated refraction (RM-8900, Topcon, Tokyo, Japan) followed by subjective refraction whenever possible. Five children who could not comply with this method due to their age received cycloplegic retinoscopy (Beta 200 retinoscope, Heine, Herrsching, Germany). Follow-up examinations for refractive error and visual acuity were performed every 6 months. Each patient’s follow-up refraction was measured as it had been done before. As axial eye length could not be determined prior to treatment and was not documented systematically during treatment, we have no such data to report.
Treatment
All children were advised to spend about 2 h per day outdoors and to wear their full optical correction. New glasses were prescribed whenever an undercorrection of ≥ 0.5 D was detected. 0.01% custom-made atropine was provided by a pharmacy (Berg Apotheke, Tecklenburg, Germany) as single-dose vials without preservatives. Children were given one drop into each eye at bedtime every day.
Side Effects
At each visit we checked for any potential side effects like glare, reading difficulties, or an enlarged pupil. Answers were classified as “no problem”, “problem, but only mentioned on demand” and “problem and described by patient himself”. Compliance was assessed by history and parental report.
A subset of 20 families agreed to start the therapy in one eye only and to present the next day for an assessment of near vision, accommodation, and pupil size at 08:00, 10:00 and 12:00 a.m. by an orthoptist blinded to the trial. This enabled us to exploit the untreated fellow eye for intraindividual control. Allocation of the treated eye was randomised. From the day thereafter, both eyes were treated with atropine. Pupil size was measured with the cross lines of the eye-piece of a manual Goldmann perimeter (Haag-Streit, Bern, Switzerland) at 10 cd/m2. Near visual acuity was tested with Landolt single optotypes (C test for near and distance vision, according to Haase/Hohmann, Oculus, Wetzlar, Germany) in 30 cm with the distance refraction. Accommodation was estimated via dynamic retinoscopy averaging three measurements: The patients were instructed to read optotypes while being examined with the retinoscope (Beta 200 retinoscope, Heine, Herrsching, Germany), as that was brought continuously closer to the eye. The near point of accommodation was defined as the distance at which the fundus red flickering reflex changed to a “with movement”.
Data Analysis
All refraction data are presented as the spherical equivalent in D derived from sphere and cylinder. Data were analysed using the R system (R Foundation for Statistical Computing, Vienna, Austria). Continuous data are presented via mean and standard deviation. Categorial data are aggregated via percentages. To analyse the primary endpoint, we performed linear regression analysis. We plotted the spherical equivalents over time for each patient separately. We extracted the slope of myopia progression before treatment, after treatment until 6 months later and, where possible, after treatment until 1 year later. We used the paired t test to compare the slope before treatment to the slope after treatment until 6 months and/or until 12 months. It was further used to compare younger with older children as well as children with light and dark coloured irides. Data were considered significant at p < 0.05.
Results
Demographics
The mean age was 11 years (range 6–17 years, median 10.5 years). 36 (64%) of the children were female and 20 (36%) male. 41% of the irides were light-coloured and 59% dark. All children were of European ancestry. Mean refraction at the beginning of the treatment was − 3.85 ± 1.88 D (median − 3.63 D). In the year prior to treatment, the mean progression per year was 1.05 ± 0.37 D (median 1.00 D).
Efficacy
After the 6 months of therapy, 51 (91%) children attended their first scheduled follow-up visit. During that time period, the mean change in refraction was − 0.22 ± 0.48 D. 54 (93%) patients attended their scheduled 12-month follow-up visit. Over this entire year, the rate of progression was − 0.40 ± 0.49 D. The difference in progression before and after 12 months’ treatment was statistically highly significant (p < 0.0001). Progression was greater before and during treatment in the 6–11 years age group than in the children aged 12–17 years (Fig. 1a). We observed no difference between light and dark-coloured eyes (Fig. 1b).
Fig. 1.
Box-whisker-plots (Tukey) illustrating myopic progression in the year prior to treatment and after 6 and 12 months of treatment with 0.01% topical atropine, stratified for age (a) and iris colour (b)
Safety
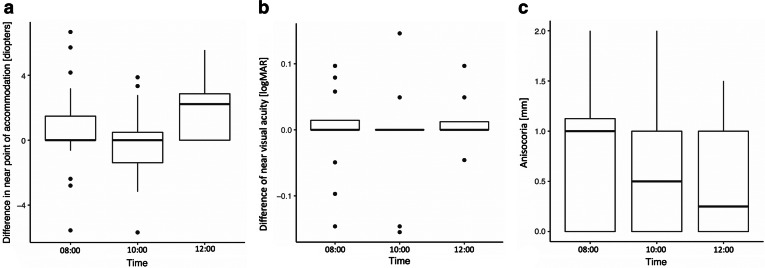
Our subgroup analysis revealed minor but still measurable side effects. No difference in the near point of accommodation was evident at 8:00 (n = 20) and 10:00 a.m. (n = 18). At 12:00 a.m. (n = 12), we noted a minor, but insignificant median reduction of 2.0 D (Fig. 2a). Near visual acuity was unaffected in relation to the untreated fellow eye at each of the three measurements (Fig. 2b). Those minor reductions in accommodation therefore had no functional consequences for near vision. Pupil size was the only parameter that revealed a consistent effect from 0.01% atropine: it induced anisocoria of 1 mm at 8:00 a.m., decreasing to 0.5 mm at 10:00 a.m. and 12:00 a.m. (Fig. 2c). We observed no side effects such as conjunctival redness or other changes in the ocular surface. No patient complained of glare, reading difficulties, or other symptoms related to the therapy.
Fig. 2.
Box-whisker-plots (Tukey) showing a the interocular difference in the accommodative response, b the interocular difference in visual acuity and c the amount of anisocoria at 08:00 h, 10:00 h and 12:00 h after unilateral application of 0.01% atropine on the evening before
Discussion
Our data show a significant effect of low-dose atropine on myopia progression in school children aged between 6 and 17 years. After treatment with atropine 0.01%, we documented a mean progression of myopia of 0.40 D/year as opposed to 1.05 D/year before treatment. We observed neither clinically relevant nor statistically significant side effects on visual acuity, near accommodation, pupil size or the ocular surface.
The effect of atropine 0.01% on progression we observed concurs with the aforementioned randomised controlled trials from Asia, i.e. ATOM-2 [7] and LAMP [8] as well as two meta-analyses [9, 10]. Two non-randomised studies report data from European cohorts. First, Polling et al. described the efficacy and safety of atropine 0.5% in a Dutch cohort with 23% Asian individuals under longitudinal observation [13]. Similar to our cohort, their progression was − 1.0 D/year prior to treatment. During 12 months of treatment, progression was 0.1 D/year. The concentration of 0.5%, however, was accompanied by a rather high rate of side effects (72% photophobia, 38% reading problems) leading to a high rate of therapy cessation. Remarkably, the therapy effect was stronger in teenagers than in younger children. In our analysis, we likewise observed a non-significant correlation between age and effect size of therapy, most likely due to decreasing progression with increasing age. Second, Diaz-Llopis et al. compared 100 Spanish children aged 9–12 years on atropine 0.01% with a control group left untreated [14]. Progression was − 0.14 D/year in the atropine group and − 0.65 D/year in the control group. Side effects were reported in 2%.
Several investigations focussed primarily on the side effects of low-dose atropine. Cooper et al. compared three different doses of topical atropine in mostly emmetropic US-American adolescents and reported 0.02% as the threshold dose without relevant side effects [15]. Nishiyama et al. investigated the same parameters in Japanese myopes aged 6–12 years and detected accommodation reduced by 1.5 D and pupil dilation of 0.7 mm using atropine 0.01% [16]. Loughman and Flitcroft observed pupil dilation of 1.2 mm and an insignificant reduction in accommodation in Irish young adults induced by atropine 0.01% [17]. Kaymak et al. investigated short-term side effects in young adults revealing a pupil dilation similar in extent and duration to our data on atropine 0.01% and 0.005%, but almost no dilation in conjunction with 0.001% atropine [18]. The ATOM-2 trial reported pupil dilation of 1 mm, a small reduction in accommodation by 2 D and minimally reduced distance visual acuity of 0.02 logMAR [7]. In the LAMP trial, pupil size increased by 0.5 mm and near visual acuity remained unaffected [8]. Taken together, our data fall well in line with previous reports regarding side effects.
Our investigation has some shortcomings limiting the evidence mainly with regard to efficacy. The data were collected out of a paediatric ophthalmology clinic and not in a randomised, controlled fashion, measures that would have fallen under the auspices of our national medicines law. Further, the sample itself is not large. Second, our data must be interpreted as revealing the cumulative effect of a pharmacological therapy and the advice to increase outdoor-time. Retrospective separation of proportionate efficacy is not possible. Furthermore, we had no access to axial eye length data with which to compare the treatment phase to the pre-treatment period. A shortcoming in our safety assessment is also the difficulty masking the treated eye. As their anisocoria was usually obvious, and bias cannot be excluded even though we split the investigators into two groups. Finally, part of the refractive data are based on non-cycloplegic measurements.
Conclusion
In summary, we observed significantly less progression during treatment with topical atropine 0.01% as compared to the year prior to treatment, based on uncontrolled medical-history data. Though a retrospective separation of the proportionate efficacies of lifestyle recommendations and atropine is impossible, we assume that a certain amount of alleviating myopic progression is based on the pharmaceutical treatment. This is likely given the evidence from other trials using low dose atropine, and the general lack of effect of time outdoors on progression. Since we observed no clinically relevant side effects during our observation, we consider atropine 0.01% a viable and safe option for controlling myopic progression. It undoubtedly warrants further randomised, controlled trials—especially in non-Asian populations [19].
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Medical Writing, Editorial, and Other Assistance
Editorial assistance in the preparation of this article was provided by Dr. C. Cürten at Albert-Ludwigs-Universität Freiburg Medizinische Fakultät administration.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Conflict of Interest
Lutz Joachimsen, Daniel Böhringer, Nikolai J Gross, Michael Reich, Julia Stifter, Thomas Reinhard and Wolf A Lagrèze have nothing to disclose.
Compliance with Ethics Guidelines
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (Institutional Review Board Approval University of Freiburg #287/16) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Enhanced digital features
To view enhanced digital features for this article go to 10.6084/m9.figshare.8224469.
References
- 1.Holden BA, Fricke TR, Wilson DA, Jong M, Naidoo KS, Sankaridurg P, Wong TY, Naduvilath TJ, Resnikoff S. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123:1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 2.Williams KM, Verhoeven VJM, Cumberland P, Bertelsen G, Wolfram C, Buitendijk GHS, et al. Prevalence of refractive error in Europe: the European Eye Epidemiology (E(3)) Consortium. Eur J Epidemiol. 2015;30:305–315. doi: 10.1007/s10654-015-0010-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622–660. doi: 10.1016/j.preteyeres.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Pararajasegaram R. VISION 2020-the right to sight: from strategies to action. Am J Ophthalmol. 1999;128:359–360. doi: 10.1016/s0002-9394(99)00251-2. [DOI] [PubMed] [Google Scholar]
- 5.COMET Group Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET) Invest Ophthalmol Vis Sci. 2013;54:7871–7884. doi: 10.1167/iovs.13-12403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Derby H. On the atropine treatment of acquired and progressive myopia. Trans Am Ophthalmol Soc. 1874;2:139–154. [PMC free article] [PubMed] [Google Scholar]
- 7.Chia A, Chua WH, Cheung YB, Wong WL, Lingham A, Fong A, Tan D. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2) Ophthalmology. 2012;119:347–354. doi: 10.1016/j.ophtha.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Yam JC, Jiang Y, Tang SM, Law AKP, Chan JJ, Wong E, Ko ST, Young AL, Tham CC, Chen LJ, Pang CP. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126:113–124. doi: 10.1016/j.ophtha.2018.05.029. [DOI] [PubMed] [Google Scholar]
- 9.Huang J, Wen D, Wang Q, McAlinden C, Flitcroft I, Chen H, Bao F, Zhao Y, Hu L, Li X, Gao R, Lu W, Du Y, Jinag Z, Yu A, Lian H, Jiang Q, Yu Y, Qu J. Efficacy comparison of 16 interventions for myopia control in children: a network meta-analysis. Ophthalmology. 2016;123:697–708. doi: 10.1016/j.ophtha.2015.11.010. [DOI] [PubMed] [Google Scholar]
- 10.Gong Q, Janowski M, Luo M, Wei H, Chen B, Yang G, Liu L. Efficacy and adverse effects of atropine in childhood myopia: a meta-analysis. JAMA Ophthalmol. 2017;135:624–630. doi: 10.1001/jamaophthalmol.2017.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brennan NA, Cheng X. Commonly held beliefs about myopia that lack a robust evidence base. Eye Contact Lens. 2018 doi: 10.1097/icl.0000000000000566. [DOI] [PubMed] [Google Scholar]
- 12.Grigore M, Avram A. Iris colour classification scales—then and now. Rom J Ophthalmol. 2015;59:29–33. [PMC free article] [PubMed] [Google Scholar]
- 13.Polling JR, Kok RGW, Tideman JWL, Meskat B, Klaver CCW. Effectiveness study of atropine for progressive myopia in Europeans. Eye. 2016;30:998–1004. doi: 10.1038/eye.2016.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Diaz-Llopis M, Pinazo-Durán MD. Superdiluted atropine at 0.01% reduces progression in children and adolescents. A 5 year study of safety and effectiveness. Arch Soc Esp Oftalmol. 2018;93:182–185. doi: 10.1016/j.oftal.2017.12.015. [DOI] [PubMed] [Google Scholar]
- 15.Cooper J, Eisenberg N, Schulman E, Wang FM. Maximum atropine dose without clinical signs or symptoms. Optom Vis Sci. 2013;90:1467–1472. doi: 10.1097/OPX.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 16.Nishiyama Y, Moriyama M, Fukamachi M, Uchida A, Miyaushiro H, Kurata A, Tokoro T, Ohno-Matsui K. Side effects of low dose atropine. Nippon Ganka Gakkai Zasshi. 2015;119:812–816. [PubMed] [Google Scholar]
- 17.Loughman J, Flitcroft DI. The acceptability and visual impact of 0.01% atropine in a Caucasian population. Br J Ophthalmol. 2016;100:1525–1529. doi: 10.1136/bjophthalmol-2015-307861. [DOI] [PubMed] [Google Scholar]
- 18.Kaymak H, Fricke A, Mauritz Y, Löwinger A, Klabe K, Breyer D, Lagenbucher A, Seitz B, Schaeffel F. Short-term effects of low-concentration atropine eye drops on pupil size and accommodation in young adult subjects. Graefes Arch Clin Exp Ophthalmol. 2018;256:2211–2217. doi: 10.1007/s00417-018-4112-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lagrèze WA, Schaeffel F. Preventing myopia. Dtsch Arztebl Int. 2017;114:575–580. doi: 10.3238/arztebl.2017.0575. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.