Abstract
Variability in individuals’ responses to interventions may contribute to small average treatment effects of childhood obesity prevention interventions. But, neither the causes of this individual variability nor the mechanism by which it influences behavior are clear. We used qualitative methods to characterize variability in students’ responses to participating in a childhood obesity prevention intervention and psychosocial characteristics related to the behavior change process. We interviewed 18 students participating in a school-based curriculum and policy behavior change intervention. Descriptive coding, summary, and case-ordered descriptive meta-matrices were used to group participants by their psychosocial responses to the intervention and associated behavior changes. Four psychosocial phenotypes of responses emerged: (a) Activated—successful behavior-changers with strong internal supports; (b) Inspired—motivated, but not fully successful behavior-changers with some internal supports, whose taste preferences and food environment overwhelmed their motivation; (c) Reinforced—already practiced target behaviors, were motivated, and had strong family support; and (d) Indifferent—uninterested in behavior change and only did target behaviors if family insisted. Our findings contribute to the field of behavioral medicine by suggesting the presence of specific subgroups of participants who respond differently to behavior change interventions and salient psychosocial characteristics that differentiate among these phenotypes. Future research should examine the utility of prospectively identifying psychosocial phenotypes for improving the tailoring of nutrition behavior change interventions.
Keywords: Childhood obesity prevention intervention, Psychosocial phenotyping, Qualitative research
Students who learned about healthy eating fell into four subgroups: Activated (made healthy changes), Inspired (wanted to change), Reinforced (kept healthy habits), and Indifferent (uninterested).
Implications
Practice: Phenotypes can be used to explain differences in responses to childhood obesity prevention interventions.
Policy: Policy-based solutions might be necessary to improve energy balance–related behavior among children who are motivated but do not have strong self-regulation skills.
Research: Future research should be aimed at validating, scaling, and applying phenotyping methods in health behavior change interventions.
INTRODUCTION
School-based childhood obesity prevention interventions, which typically focus on education and environmental change around energy balance–related behaviors (EBRBs), have been demonstrated to have positive, but small, effects [1–3]. Research that identifies how best to tailor future interventions is an important next step in childhood obesity prevention efforts [3]. Psychological, social, and environmental factors act as determinants (i.e., mediators or moderators) of EBRBs; therefore, they are intervention targets [4,5]. Rigorous intervention evaluations depend on average treatment effects [6], despite wide variability in individual responses to behavior change interventions [4, 7]. Niether the causes of this variability nor the mechanism by which it influences behavior are clear. Typifying differences in responses to a health behavior change intervention and identifying characteristics related to these differences will contribute to progress in this area.
Phenotyping, a method that emerged from genome-wide association studies and has been used clinically to identify patient characteristics that predict different responses to treatment [8, 9] is an apt analogy for characterizing the combination of psychological, social, and environmental factors mediating individuals’ EBRB change during an intervention. Researchers have developed phenotypes relating overeating behaviors to childhood obesity etiology [10] and have called for research identifying subgroups of children that share determinants of dietary behavior change [11], but phenotyping has not yet been used in the context of EBRB change.
We define psychosocial phenotypes of EBRB change as the combination of psychological and social characteristics that explain variations in behavioral response to an intervention. A prior study identified subgroups of youth by their psychosocial motivations for food choice [12], but psychosocial phenotypes that describe intervention response have not been identified. Qualitative methods, which have been called for to explain influences on EBRBs [13] and used to identify new approaches to improving childhood obesity prevention interventions [14], are particularly well suited for in-depth examinations of individual characteristics. Thus, we conducted a qualitative study to describe psychosocial phenotypes of EBRB change in response to a childhood obesity prevention intervention by characterizing individual variability in behavior change and related psychosocial characteristics among participating students.
METHODS
Food, health, and choices
This phenomenological [15] and social constructivist [16] study explored students’ experiences with adopting EBRBs during Food, Health, and Choices (FHC), a school-based childhood obesity prevention intervention designed for elementary schools in areas with high health inequality. FHC is based on social cognitive [17] and self-determination [18] theories and consists of a 23-lesson nutrition curriculum and a classroom nutrition and physical activity policy. FHC focuses on improving EBRBs: increasing physical activity and fruit and vegetable intake, and decreasing intake of sugar sweetened beverages, processed packaged snacks, fast food, and screentime via theoretically related psychosocial mediators. FHC was implemented in three forms: classroom curriculum, curriculum plus policy, and policy alone, during a cluster randomized controlled trial in 5th grade classes in 20 New York City public schools. On average, FHC participants were 10 years old and 51% were male. Most FHC participants were Hispanic (58%) or African-American (30%) and free/reduced price lunch eligible (86%).
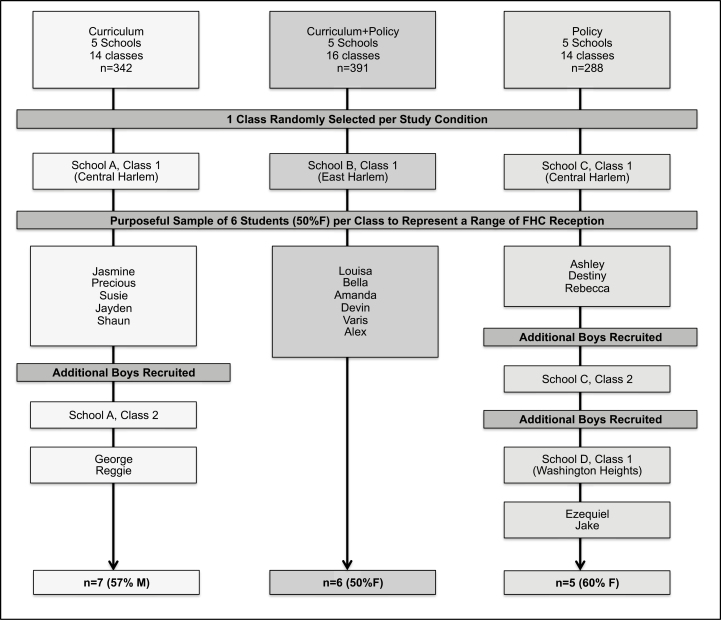
Participant recruitment
We recruited student participants from classes in each active study condition, using purposeful sampling [19] and engaging classroom teachers and FHC instructors to ensure participants represented a range of engagement in FHC (see Supplementary Material for the sampling diagram). Potential participants were told that participation would involve sharing about personal experiences with adopting EBRBs via interviews and photos they took with disposable cameras provided by the study team. Parental consent and assent were obtained from interested participants. Participants selected their pseudonyms and received a printed set of their photos as a thank you. Participants did not provide demographic information as part of the interview. The Teachers College and NYC Department of Education Institutional Review Boards approved the methods used in this study.
Interview protocol
The first author, who has training and experience in qualitative research, conducted two 30-minute photo elicitation interviews [20, 21] with participants (n = 18) in March–June 2013 using a semistructured interview guide (available online) adapted from Ref. [21] based on the team’s extensive experience working with children. Because it was impossible to member-check interview transcripts with students, the interviewer used paraphrasing and reflective techniques during the interviews to increase data trustworthiness [19]. Interviews were audio recorded and transcribed; coding was done with NVivo10 (QSR International, 2012).
Analysis
The first author wrote a case summary about each interviewee (available online) and descriptively coded the interviews [22]. The second author also coded early interviews and case summaries to ensure reproducibility [19]; discrepancies were resolved by consensus. From this process, a coding dictionary was developed based on constructs from health behavior theories [23], depicted in Table 1; the first author coded remaining interviews. Case-ordered descriptive meta-matrices [22] were used to examine individual variability in interviewees’ EBRBs. Iterative coding of the summaries and transcripts led us to a holistic judgment by two coders about the extent to which each interviewee adopted each EBRB, and whether the behavior change was related to FHC or other factors (i.e., did FHC prompt behavior change or did it occur prior to FHC?). Although interviewees were not explicitly asked when they adopted each EBRB, their discussions of the supports and barriers to adopting each behavior made this distinction clear (see Supplementary Material for the case summaries). Next, the interviewees’ psychosocial characteristics were described. Then, matrices examining behavior change and psychosocial characteristics were developed and interviewees were categorized into phenotypes. Finally, within- and between-group similarities and differences were identified and summarized.
Table 1.
Interview Coding Dictionary
| Code | Definition | Example(s) |
|---|---|---|
| Motivations | ||
| Experiential attitude | Feelings about behavior, including preferences, ambivalence | “Sometimes when you’re eating, you want something sweet in your mouth” “The cookie I really like and the apple, but the apple was much more healthier than the cookie…” “I felt angry because, you know the company that makes all those sodas? I feel as if they’re really greedy and selfish” |
| Instrumental attitude | Cognitive beliefs about outcomes of behavior, including perceived risk, personal experiences | “My cholesterol is high for a girl my age” “Well, unhealthy snacks or drinks can lead to diabetes” “When I was in third grade I was fat” |
| Responsibility | Beliefs about obligation to share knowledge with others, including role modeling | “Because he drinks it every day he’s getting a lot of sugar that he doesn’t need. I told him that if he continues, later on he might catch a disease such as diabetes” “I would like to give an example to my little cousins that it is better to be healthy and active than eating all of this” |
| Injunctive social norms | Beliefs about how others think one should behave + motivation to comply, including social support | “She tells me to eat a lotta fruits and vegetables because it’s good for you” “And the reason I like it is because in the end, everyone says good job Varis, yay, good for you” “Because after lunch, we always Take A Dance Break and they encourage us to dance more” |
| Descriptive social norms | Perceptions about what others are doing, including observational learning, peer comparison | “I also see people eating junk food. It compels me to eat junk food too” “My sister is really crazy for sweets” “Makes me feel great because I’m not, I’m not [drinking Arizona and] going to be fat” |
| Perceived control | Beliefs about ability to surmount difficulties in adopting behavior; power/situational control, including Disinhibition, “addiction” | “But some of them are hard for me because I’m totally addicted to it” “It’s like once you eat it, you can’t stop. You just want more and more and more and more” |
| Self-efficacy | Confidence in ability to take action | “My mom taught me and she made it once and I started to, it started being a habit for me so I start doing it here” |
| Self-identity | How one perceives one’s salient characteristics | “And sometimes I would get bored and I would look at kids outside and like, why can’t I do that; why am I so lazy?” |
| Capabilities | ||
| Knowledge | Factual statement (regardless of correctness) | “Fruits have vitamins” “I know too much oil means too much fat and that’s unhealthy” |
| Skills | Label-reading, dancing, food preparation | “Um this is the pie that sometimes I just put it in the oven and I like heat it up because it tastes good, it’s easy to heat up and it has vegetables in it” |
| Self-regulation | Self-control via self-monitoring, goal setting, self-assessment, planning, recovery. Includes strategies, e.g. Avoidance, moderation, reminders, substitution, decision fatigue | “I’m like, okay, I have a half an hour left before I go to sleep. Why not watch a little bit of TV. That’s it” “Like let’s say you are done with school and you have nothing else to do, you just eat a little bit of food or a snack so you can eat it and then you can take your mind off of all that thinking” |
| Habit | Repeated behaviors | “I always drink water instead of juice” |
| Environment | ||
| Neighborhood environment | Includes stores, park, outside of school PA programs | “It’s at the supermarket coming from school” “There’s a rack of chips, and then, there’s juices in the cooler; and it’s just hard to not get a pack of chips or juice” |
| Information environment | Advertising, messaging, informational visuals in school, on screen, in print | “Because like on the commercial that I saw yesterday, it was a famous person drinkin’ somethin’ healthy, and I was thinkin’ maybe the famous person are encouragin’ kids to drink that stuff more” |
| School environment | Includes cafeteria, school food, including policies/rules | “Like in the lunch room, there’s a salad bar” |
| Home environment | Includes types of food available | “At home my mom usually makes home cooked food” |
Definitions adapted from Ref. [5, 23].
RESULTS
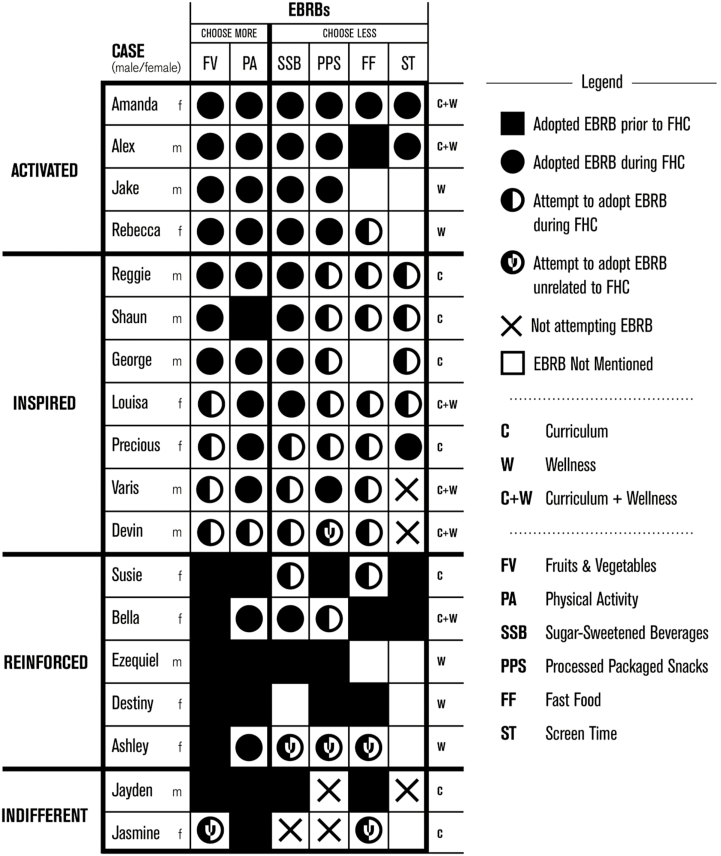
Interviewees were classified into four emergent phenotypes of psychosocial response to the intervention: (a) Activated (n = 4)—at least four EBRBs fully adopted during FHC; (b) Inspired (n = 7)—fewer than four EBRBs successfully adopted, but motivation from FHC indicated; (c) Reinforced (n = 5)—more EBRBs adopted prior to FHC than during FHC, but motivation from FHC indicated; and (d) Indifferent (n = 2)—regardless of EBRBs reported, no motivation from FHC indicated. Phenotypes are depicted in Fig. 1 and summarized below. Interviewees with different phenotypes exhibited not only different behaviors in response to the intervention, but also different psychosocial characteristics. Preference was an exception. Across all phenotypes, interviewees reported the influence of taste preferences and the allure of “junk food.” Although several interviewees liked fruit and vegetables, many shared photos of and discussed preferences for salty snacks, sweets, and fast food, using words like “addicted” and “hooked” to describe their affinity for them. Likewise, many also mentioned being “addicted” to screentime.
Fig 1.
Behavioral phenotypes of food health and choices (FHC) participants. Activated = at least four FHC energy balance–related behaviors (EBRBs) fully adopted during FHC; Inspired = fewer than four FHC EBRBs successfully adopted, but motivation from FHC indicated; Reinforced = more FHC EBRBs adopted prior to FHC than during FHC, but motivation from FHC indicated; Indifferent = regardless of the FHC EBRBs reported, no motivation from FHC indicated.
Activated interviewees reported mostly internal motivators, capabilities, and supports. Although they discussed the lure of junk foods, they also liked (or tolerated) fruit and vegetables. As Alex described, “At dinner I used to love desserts with processed snacks but I told my mother, ‘Mom, instead of making soup with ordinary chicken and that’s it, why don’t you add a little green beans, a little broccoli; a recipe that tastes good.’ Well, I started eating more fruit and vegetables in my foods and it wasn’t hard for me because it actually tastes good.” Positive and negative outcome expectations and perceived risk seemed to propel them to success in adopting the EBRBs. For example, Rebecca, who was concerned about her cholesterol being “too high for a girl of my age,” mentioned diabetes and heart attacks as negative outcomes of eating excessive candy as she pondered, “What if that actually happens and all of that would affect your family...let’s start being more healthier.” These interviewees did not come from families with strong rules about EBRBs. Instead, they relied heavily on their own self-regulatory skills, including self-evaluation, goal setting, planning, substitution, self-talk, and avoidance. For example, Amanda described how, “basically every Sunday I just make a schedule or a list saying that on Monday I’m gonna take this [healthy snack]...next I’m gonna take that...So, I just make a schedule…like time, but it’s mostly referring to what kinds of food I’ll take or what kinds of beverages I’ll take” and photographed a water bottle she drank and refilled at school. They also seemed to feel a responsibility to share what they learned with others. As Jake described his reasons for wanting to teach his family about FHC, “because they are always eating junk food and I want to help them a little bit.”
Inspired interviewees were motivated by health-related outcome expectations, but taste preferences for and the availability of junk food seemed to overtake outcome expectations. For example, Devin pointed out “unhealthy snacks or drinks can lead to diabetes,” but later said, “when it’s really hot… I really like sugary beverages, not really healthy drinks.” Inspired interviewees who reported self-regulation skills tended to mention substitution and moderation rather than self-evaluation, planning, or avoidance. A common substitution was juice or a smoothie instead of soda or sweetened tea. Inspired interviewees relied more on external motivations. For example, Louisa was frustrated that “I really like candy but I get so mad that I can’t eat it” because it would ruin her braces and get her in trouble with her mom. They were more attuned to the social environment; peers, norms, and rules were important influences. Precious photographed her cousin exercising at home, explaining that her example encouraged Precious to do more physical activity, “since she came and lived in my house, and she’s very flexible, and she never watched TV a lot, all she do is just play around the house…exercising; exercise before going to bed, exercise before eating, exercise before doing anything, she was exercising, so I started doing the same thing....” Many Inspired interviewees relied on social support at home to help them adopt EBRBs; some specifically asked family members for support. Reggie reported feeling “happy because I did something good for myself” when he ate salad; his mom provided support by buying him fruit. However, Inspired students also found their homes to be a barrier to EBRBs, mentioning family norms of television, processed snacks, and sugary beverages. For example, Varis reported that he strongly preferred juice to water and was willing to lie to his mom, telling her he was drinking water when it was juice his uncle brought home. Some Inspired interviewees also shared what they learned with others. As Louisa described, “…My mom usually buys me bottles of Gatorade and I am trying to change that, I am telling her to buy me bottles of water…I have been telling my mom to do what I tell her that has to do with healthier stuff and she has been doing good…now, she only drinks those healthy fruit drinks and homemade smoothies and water.”
Fig 2.
Flow diagram of interview study purposeful sampling. FHC = Food, health, and choices childhood obesity prevention intervention. Student names listed are pseudonyms. One class in each of the three active study conditions was randomly selected, and six students from these three classes were chosen in consultation with classroom teachers to represent a range of engagement and participation in FHC. In the class from the policy alone condition, only three students received parent consent for the interview. The researchers decided that it would be more useful to interview additional students at a school where the policy was more fully implemented; two students from the second school were interviewed. Two additional students from a second class receiving curriculum were also interviewed.
Table 2.
Food, health, and choices interview questions and constructs of interest
| Constructs | Interview questions |
|---|---|
| Interview 1 | |
| Intervention reception | 1. Imagine a new student was starting in your class today and you are assigned by your teacher to help catch them up with Food, Health & Choices. Your instructor is coming tomorrow. What would you be sure to tell them? a. What other topics do you think would be important for the new student to know about? b. What experiences have you and the other students in your class had during Food, Health & Choices that would be helpful for the new student to hear about? |
| Intervention reception | 2. [Set out index cards with the FHC EBRBs written on them] Which of these goal behaviors do you remember learning about during Food, Health, and choices? |
| EBRB change supports and barriers | 3. Which goal behaviors have you tried to do yourself? a. What made it easier? Possible prompts: Are there people/places/personality traits that made it easier? b. What made it more challenging? Possible prompts: Are there people/places/personality traits that made it more challenging? |
| EBRB change supports and barriers | 4.Which goal behaviors do you think you have made automatic or a habit? a. How do you know? b. What makes it easy? c. What makes it challenging? |
| Behavioral intention supports and barriers | 5. Which goal behaviors do you plan to try? a. What will help you try out these behaviors? b. What will make it challenging? |
| Interview 2 | |
| EBRB change supports and barriers | 1. [Set out prints of student’s photos] Look through the photos you took and choose the one you are most eager to tell me about…What do you want to tell me about the photo you have chosen? a. What do you see in this picture? b. What is happening in this picture? c. Why did you choose this picture? d. When was this photo taken? e. Is this a typical purchase/meal/snack for you? f. How does this picture make you feel? Repeat questions for additional photos as student chooses |
| Supports and barriers | 2. Now that you’ve looked back at all the photographs you took, what do you think is the most important thing you learned about things that help make your Food, Health, and Choices goals easier/more challenging? |
FHC food, health, and choices obesity prevention intervention; EBRB energy balance–related behaviour.
Reinforced interviewees already followed EBRBs and reported that preferences and outcome expectations motivated them to do so. Destiny talked about how she ate fruits as snacks at home because they are sweet and will “not give you obesity” and Ezequiel described his personal experiences with being overweight, “I was obese when I was 8 years old and I [don’t] want to gain the weight back.” Reinforced interviewees emphasized shorter term negative outcomes of junk food consumption, like Ashley, who pointed out “sodas and stuff, it stains your teeth and it’s not good.” Although Reinforced interviewees tended to do the EBRBs, they were not immune to junk food preferences. For example, Susie reported that she was trying to choose smaller fast food sizes and avoid McDonald’s, but found it difficult because the fries were “irresistible.” Reinforced students used some self-regulation skills, including avoidance and substitution, but external supports seemed more important. Reinforced interviewees’ families supported EBRBs. Bella described how “[My mom is] always right there. So she makes…our dinner. She tries to put vegetables in it…we always have fruit on the table.” They also mentioned supportive school environments, including lunchtime salad bars. Ashley described how the “[lunch staff] give us a fruit like an orange, a banana or apple to add in with our food for lunch.” Reinforced students mentioned environmental issues, including omnipresent delis and fast food advertising, but they did not seem to overwhelm this group.
Indifferent interviewees were not motivated by FHC, but engaged in some EBRBs. Like other interviewees, they were motivated by preferences. As Jayden put it, “I like to work out.” Jasmine brought candy to lunch “‘cause it’s good” and did not hesitate to say she preferred candy to fruit or vegetables. Indifferent interviewees’ primary motivators and supports were external. For example, social norms at recess encouraged Jasmine to engage in physical activity despite her distaste for it, “…when we go outside in school, we’re always running in the tracks, we’re running to see who’s the fastest.” Jayden talked about his mom making him vegetables and not allowing him to have fast food too frequently and photographed a bag of oranges she bought for their home. Jasmine recounted, “When I go to the restaurant with my mother and my sister and when it’s time to order they tell me not to pick the fast food, they tell me to pick healthy stuff.” Indifferent interviewees reported few barriers.
DISCUSSION
In this qualitative examination of a childhood obesity prevention intervention, we used students’ rich descriptions of the behavior change process to characterize individual variability into four psychosocial phenotypes of behavior change in response to FHC. Interviewees in the Activated, Inspired, Reinforced, and Indifferent phenotypes had different behavioral responses and psychosocial characteristics related to their behavioral responses. Our findings contribute to the field of behavioral medicine by suggesting the presence of specific subgroups of participants who respond differently to childhood obesity prevention behavior change interventions, as well as salient psychosocial characteristics that differentiate among these phenotypes.
Psychosocial characteristics that differentiated the highly successful Activated phenotype were perceived risk and self-regulation. In the general population, fear has been demonstrated to be a mediator of behavior change [24], but perceived risk has been dismissed as unlikely to influence children and adolescents [25]. Given the high prevalence of type 2 diabetes, obesity, and other diet-related diseases in interviewees’ families and neighborhoods, as well as the ubiquity of these conditions in the media, familiarity with these diseases may make them relevant, even to children. The importance of self-regulation in EBRBs has also been examined, though not in elementary students. In a cross-sectional study of diverse 9th grade students, self-control, a construct like self-regulation, was related to EBRBs [26]. Likewise, self-regulation was related to physical activity among adolescents in a systematic review of mediation analyses [4].
Family support was one area that was perceived quite differently across the four phenotypes. EBRBs, specifically screentime, have been observed to be an incidental happening related to family norms and home environment [4]. We found that Activated interviewees focused on internal rather than family support; Inspired interviewees experienced inconsistent family support and this lack of support made acting on their motivations challenging; Reinforced interviewees relied on family to motivate and support them in doing EBRBs; and Indifferent interviews only did EBRBs because their families insisted.
Like other qualitative studies, the findings from these interviews are not intended to be generalizable. Rather, the in-depth analysis of fewer cases was designed to be hypothesis generating. Furthermore, assessment of a student’s behavior by interpreting the whole of his or her interview responses may have yielded a more accurate assessment than multiple-choice survey responses. Students who chose not to participate or whose parents refused permission for them to be interviewed may have had different experiences with FHC; however, purposeful sampling [19] was chosen to minimize this bias. The small sample size may have precluded the identification of even more precise phenotypes; however, the absence of new descriptive codes in the coding of the final three interviews suggested that saturation [19] had been reached. Small within-phenotype numbers, particularly in the Indifferent phenotype, may have hidden other similarities or differences among the groups. Finally, that the interviewer was an FHC instructor may have encouraged more socially desirable responses, but using photo elicitation shifted the power dynamic from a typical teacher–child relationship and gave control over the topics discussed, especially in the second interview, to the interviewee. We also emphasized the value of interviewees’ opinions over “correct” answers. Interviewees recounted stories of deceiving their parents, troublemaking, their fears about diabetes, and their dislike for spinach, broccoli, and other vegetables; some even demonstrated dance moves. This suggests that interviewees were comfortable sharing their experiences with the interviewer. Importantly, our ability to make claims about the influence of FHC on behavior change and psychosocial characteristics was limited because participants were only interviewed at the conclusion of the intervention. Therefore, the psychosocial phenotypes were retrospectively constructed and we could not study the degree to which phenotypes predicted differences in intervention response. Future research should examine the reproducibility of psychosocial phenotyping of behavior change and prospectively identify psychosocial phenotypes to assess their influence on intervention results.
Our findings suggest implications for practice, policy, and research. Although further research is necessary to determine the generalizability of our results, the influence of home environment on three of the phenotypes we identified speaks to the importance of family education as a complement to school-based childhood obesity prevention [27]. Policy-based solutions, such as regulating snacks and drinks marketed to children or limiting fast food outlets in a neighborhood, might be helpful for children who were motivated to change their behavior but whose self-regulation skills were overcome by junk food preferences and ubiquity (i.e., Inspired phenotype). As a major goal of phenotyping is to better tailor interventions [9,10], a potentially fruitful next step would be to develop scalable, computational approaches to psychosocial phenotyping to identify phenotypes prior to intervention and identify mechanisms by which intervention activities and behavior change strategies [5] or techniques [28] work for participants with different psychosocial phenotypes.
Acknowledgements
The authors would like to acknowledge Scott Perez-Fox of Starship Designs (www.strshp.com); Heewon Lee Gray, Randi Wolf, Beth Tipton, and David Seres for suggestions during the study and manuscript preparation; the FHC research team; and FHC schools, teachers, and students. This study was funded by United States Department of Agriculture AFRI NIFA grant #2010-85215-20661. Dr. Burgermaster is currently supported by a National Institutes of Health training grant (LM007079); this study was conducted as part of her doctoral dissertation at Teachers College Columbia University.
Authors’ Contributions M.B., I.C., P.K. designed the study; M.B. collected data; M.B., I.C., L.M. analyzed and interpreted the data; M.B. drafted the article; I.C., P.K., L.M. critically revised the article; M.B., I.C., P.K., L.M. approved the final version to be published.
Compliance With Ethical Standards
Conflict of interest Drs. Burgermaster, Contento, Koch, and Mamykina declare that they have no conflict of interest.
Primary Data The authors state that the findings reported have not been previously published and that the manuscript is not being simultaneously submitted elsewhere; that the data reported in this manuscript were presented as a poster at the 2015 Society for Nutrition Education and Behavior conference; and that they have full control of all primary data and that they agree to allow the journal to review their data if requested.
Ethical Approval This article does not contain any studies with animals performed by any of the authors.
Informed Consent Both assent and parental informed consent was obtained from all individual participants included in the study; the Teachers College Columbia University and New York City Department of Education Institutional Review Boards both approved the methods used in this study.
References
- 1. Silveira JAC, Taddei JAAC, Guerra PH, Nobre MRC. The effect of participation in school-based nutrition education interventions on body mass index: a meta-analysis of randomized controlled community trials. Prev Med. 2013;56(3–4): 237–243. [DOI] [PubMed] [Google Scholar]
- 2. Sobol-Goldberg S, Rabinowitz J, Gross R. School-based obesity prevention programs: a meta-analysis of randomized controlled trials. Obesity (Silver Spring). 2013;21(12):2422–2428. [DOI] [PubMed] [Google Scholar]
- 3. Wang Y, Wu Y, Wilson RF, et al. . Childhood obesity Prevention Programs: Comparative Effectiveness Review and Meta-analysis. Comparative Effectiveness Reviews, No. 115. Rockville, MD: Agency for Healthcare Research and Quality; 2013. [PubMed] [Google Scholar]
- 4. van Stralen MM, Yildirim M, te Velde SJ, Brug J, van Mechelen W, Chinapaw MJ; ENERGY-consortium What works in school-based energy balance behaviour interventions and what does not? a systematic review of mediating mechanisms. Int J Obes (Lond). 2011;35(10):1251–1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Contento IR. Nutrition Education: Linking Research Theory and Practice. Burlington: MA: Jones & Bartlett Learning; 2016. [PubMed] [Google Scholar]
- 6. Shadish WR, Cook TD, Campbell DT.. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Boston, MA: Houghton, Mifflin and Company; 2002. [Google Scholar]
- 7. McBride CM, Bryan AD, Bray MS, Swan GE, Green ED. Health behavior change: can genomics improve behavioral adherence?Am J of Public Health. 2012;102(3):401–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ziegler A, Koch A, Krockenberger K, Grosshennig A. Personalized medicine using DNA biomarkers: a review. Hum Genet. 2012;131(10):1627–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Frey LJ, Bernstam EV, Denny JC. Precision medicine informatics. J Am Med Inform Assoc. 2016;23(4):668–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Boutelle KN, Peterson CB, Crosby RD, Rydell SA, Zucker N, Harnack L. Overeating phenotypes in overweight and obese children. Appetite. 2014;76:95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Contento IR. Improving the diets and eating patterns of children and adolescents: how can nutrition education help?Adolesc Med State Art Rev. 2012;23(3):471–492. [PubMed] [Google Scholar]
- 12. Contento IR, Michela JL, Goldberg CJ. Food choice among adolescents: population segmentation by motivations. J Nutr Educ. 1988;20(6):289–98. [Google Scholar]
- 13. Baranowski T, Anderson C, Carmack C. Mediating variable framework in physical activity interventions. how are we doing? how might we do better?Am J Prev Med. 1998;15(4):266–297. [DOI] [PubMed] [Google Scholar]
- 14. Greaney ML, Hardwick CK, Spadano-Gasbarro JL, et al. . Implementing a multicomponent school-based obesity prevention intervention: a qualitative study. J Nutr Educ Behav. 2014;46(6):576–582. [DOI] [PubMed] [Google Scholar]
- 15. Rossman GB, Rallis SF.. Learning in the Field: An Introduction to Qualitative Research. Los Angeles, CA: Sage; 2003. [Google Scholar]
- 16. Freeman M, Mathison S.. Researching Children’s Experiences. New York, NY: Guilford Press; 2009. [Google Scholar]
- 17. Bandura A. Social cognitive theory: an agentic perspective. Annu Rev Psychol. 2001;52:1–26. [DOI] [PubMed] [Google Scholar]
- 18. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78. [DOI] [PubMed] [Google Scholar]
- 19. Patton M. Qualitative Research and Evaluation Methods. 3rd ed Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 20. Harper D. Talking about pictures: a case for photo elicitation. Vis Stud. 2002;17(1):13–26. [Google Scholar]
- 21. Johnson CM, Sharkey JR, Dean WR, Alex McIntosh W, Kubena KS. It’s who I am and what we eat. Mothers’ food-related identities in family food choice. Appetite. 2011;57(1):220–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Miles MB, Huberman AM.. Qualitative Data Analysis: An Expanded Sourcebook. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- 23. Glanz K, Rimer BK, Viswanath K.. Health Behavior and Health Education: Theory, Research, and Practice. Hoboken, NJ: John Wiley & Sons; 2008. [Google Scholar]
- 24. Witte K, Allen M. A meta-analysis of fear appeals: implications for effective public health campaigns. Health Educ Behav. 2000;27(5):591–615. [DOI] [PubMed] [Google Scholar]
- 25. Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health behavioral change models helpful in guiding prevention of weight gain efforts?Obes Res. 2003;11Suppl:23S–43S. [DOI] [PubMed] [Google Scholar]
- 26. Wills TA, Isasi CR, Mendoza D, Ainette MG. Self-control constructs related to measures of dietary intake and physical activity in adolescents. J Adolesc Health. 2007;41(6):551–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Briggs M, Fleischhacker S, Mueller CG; American Dietetic Association; School Nutrition Association; Society for Nutrition Education Position of the American Dietetic Association, School Nutrition Association, and Society for Nutrition Education: comprehensive school nutrition services. J Nutr Educ Behav. 2010;42(6):360–371. [DOI] [PubMed] [Google Scholar]
- 28. Michie S, Richardson M, Johnston M, et al. . The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95. [DOI] [PubMed] [Google Scholar]