Abstract
Purpose
The prevalence of hypertension continues to increase worldwide, raising an urgent need for novel and efficient methods for controlling hypertension. As the Internet and smartphones become more popular, their multiple functions and large user base make mobile health (mHealth) technology a potential tool for hypertension management. We aim to evaluate the use of mHealth technology to improve blood pressure and self-management behavior in people with hypertension and prehypertension.
Intervention
The mHealth intervention measures include health education, behavior promotion, group chatting and long-term blood pressure monitoring hierarchically delivered via WeChat application among 242 participants. The frequency, intensity and content of the hierarchical intervention are determined based on the cardiovascular risk stratification of the intervention subjects.
Study design
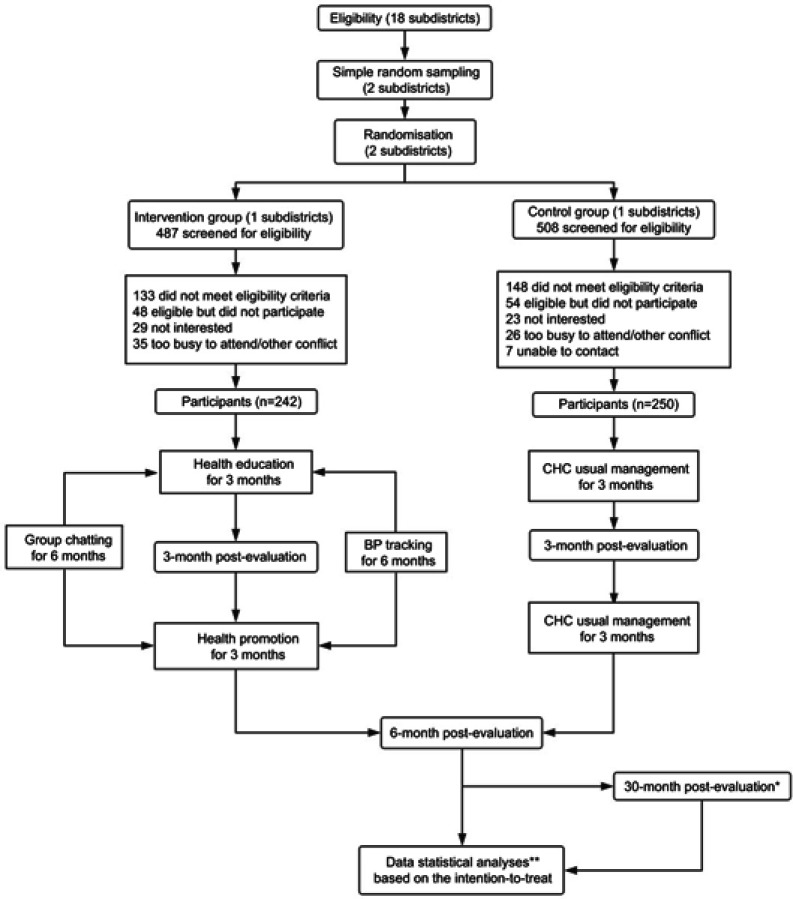
This cluster randomized controlled trial was carried out in two subdistricts in Guangzhou, China, among 492 smartphone users with hypertension or prehypertension, from August 2018 to September 2019. The intervention group received hierarchical intervention through WeChat for six months, while the control group received usual care in the community healthcare center during this period. Indicators are measured at three time points for each group, and a telephone follow-up is planned for two years after the intervention. The primary outcome is systolic blood pressure; secondary outcomes include BMI, CPAT score, improvements in behavior and diet, score of self-efficacy and self-management. Feasibility is evaluated by intervention participation. The cost-effectiveness is evaluated by ICER.
Conclusion
This study aims to evaluate the effect of the WeChat-based hierarchical management mode on improving blood pressure and self-management behavior in population with hypertension and prehypertension, based on health-related knowledge, self-efficacy and medication adherence. If successful, the management mode will serve as a feasible, economical and efficient hypertension management mode suitable for the community.
Clinical trial identifier: ChiCTR1900023002
Keywords: chronic disease, mHealth, self-management, self-efficacy, China
Introduction
Hypertension (HTN), the most common chronic disease and major risk factor for cardiovascular and cerebrovascular diseases, has become the main factor of the global disease burden.1 More than 1.5 billion people are expected to have hypertension in 2025 worldwide. In China, the prevalence of hypertension and prehypertension in adults were 25.2%2 and 33.6%,3 respectively, while the rates of awareness, treatment and control of hypertension were only 51.5%, 46.1%, and 16.9%, respectively.4 In recent years, the distribution of hypertension in China has presented an island distribution with rapidly developing cities and areas as “hot spots”. An unhealthy lifestyle, environmental pollution, occupation, public relations and other social pressures all contribute to incidence of hypertension.5 Since the 1980s, China has carried out a series of health education and promotion activities relying on community healthcare centers (CHC) in some cities, mainly for patients with chronic diseases.6 With the aging of the population, the shortage and unbalanced distribution of medical resources can no longer cope with the ever-increasing burden of chronic disease, further aggravating the great pressure of medical service supply.7 The traditional chronic disease management mode conducted face to face calls for high manpower and material cost, which is difficult to maintain and cover extensively.8 The question arises whether using modern technology in place of face-to-face interaction can attain favorable effects on hypertension management.
The rapid development of mobile Internet technology provides an opportunity for online medical services.9 Mobile health (mHealth) was put forward by Istepanian RSH in 200410 and uniformly defined by the WHO as “a support for medical and public health practices through mobile devices such as mobile phones, patient monitoring devices, PDA and other wireless devices”11 in 2011. It mainly includes voice, short message service (SMS) and third-party applications (App) and has profoundly changed people’s lifestyles and behaviors.12 By using mobile cloud computing technology to address big medical data on the Internet, mHealth can provide timely medical services and accurate information,13 which cannot be achieved by traditional medical modes. With its portability and multiple functions, mHealth is easily accepted by different socioeconomic groups and offers great potential for chronic disease management.14 In 2008, Green et al.15 successfully conducted a three-arm randomized controlled trial combining home blood pressure monitoring (HBPM), pharmacist-assisted care and network education. The study of Vargas G16 on the effect of SMS in hypertension management revealed that SMS works best in promoting two-way communication between doctors and patients. Logan AG et al.17 confirmed that a remote blood pressure (BP) monitoring App on a smartphone could improve the treatment compliance and BP of patients with hypertension.
In 2011, Tencent Inc. launched a free smart terminal application called WeChat (Wei Xin), which offers instant messaging and social networking. People can use it to send text and voice messages, make free calls, and subscribe to public accounts (also known as We-Media) to obtain recent and multifarious information. A unique function called Moments encourages users to post photos and text, share articles and music, and comment on and “like” others’ posts.18 Since its introduction, WeChat has attracted increasing numbers of loyal users and become the most popular social networking site in China, boasting over 600 million active users worldwide.19 As of 2017, WeChat accounted for 86.07% of the social software used by senior citizens in China.20 By 2018, its monthly active users had exceeded 1 billion, and daily active users reached 902 million.21 WeChat has initiated a new era of mobile Internet communication as a new lifestyle.22
A wide variety of information, including health knowledge that is of great concern to middle-aged and elderly people, rapidly disseminates among massive users through WeChat, which Forbes calls one of the most powerful applications in the world.23 Zhang et al.24 surveyed 1,636 people from 32 provinces and cities in China and found that 71.4% of them received health education through the Internet, among which 29.5% searched for health information on the Baidu website and WeChat, and 32.33% read health-related articles on WeChat regularly. On WeChat, the primary sources of health information were Moments (70.54%), public accounts (53.36%), and group chats (31.17%). Some scholars have carried out studies on the effect of WeChat-based chronic disease management. Zhang et al.25 found that the attributional intervention mode based on WeChat could improve patients’ self-management ability and BP control rate after 6 months. Dong et al.26 carried out health education on individuals with diabetes via the Wechat platform in conjunction with conventional diabetes treatment, which obviously improved the glycemic control and diabetes self-care skills of the patients. He et al.27 applied WeChat to improve weight loss behavior among an occupational population and found that the more actively the male participants used WeChat, the more weight they lost.
However, the existing studies with small sample size (generally dozens) do not include people with prehypertension and lack the interventions of health behavior promotion, resulting in poor generalization and representativeness of the conclusions. Research on the intervention participation that may have a direct impact on the change in outcome indicators is also missing. Therefore, we carried out a study with people with different cardiovascular risks using remote mHealth intervention measures, aiming to improve BP and self-management behavior in patients with hypertension and reduce the risk of people with prehypertension developing hypertension.
Methods
Study design
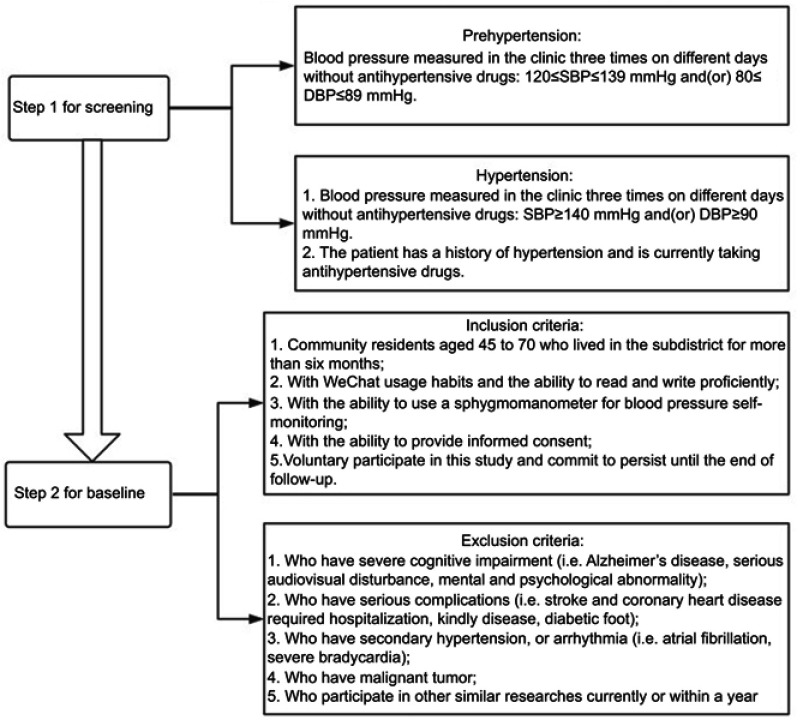
This study is a cluster randomized controlled trial conducted in two subdistricts (Baiyun Subdistrict and Dadong Subdistrict) in Guangzhou between 2018 and 2019. Interventions were allocated at the community rather than the individual level to minimize contamination among participants within the same community. Yuexiu District, a highly developed region with less population migration in Guangzhou, was selected as the research site. The pseudorandom number method (random seed =005) was used to select Baiyun Subdistrict and Dadong Subdistrict as the research communities from 18 subdistricts. Then, Baiyun Subdistrict was allocated randomly as the intervention group and Dadong Subdistrict as the control group (random seed =2018). The randomization was performed via SPSS 25.0 (IBM Corp, Armonk, NY, United States) by an independent statistician. Baiyun Subdistrict covers an area of 3.25 square kilometers and has a permanent resident population of 51,674, while Dadong Subdistrict covers an area of 1 square kilometer and has a permanent resident population of 85,987.28 The gender ratio (male: female) in both communities is close to 0.988:1, 29.7% of whom are aged 50 and above. In the CHC of each subdistrict, smartphone users were screened for eligibility based on a combination of screening criteria detailed in Figure 1.
Figure 1.
The eligibility criteria at screening and baseline.
Subjects and recruitment
The inclusion criteria, a combination of age, BP, drug intake and smartphone usage, were designed to ensure that qualified objects were selected for the study. The exclusion criteria were: (1) severe cognitive impairment (ie, Alzheimer’s disease, mental and psychological abnormality); (2) severe clinical complications requiring hospitalization, kidney disease or diabetic foot; (3) secondary hypertension or arrhythmia; (4) malignant tumors; and (5) had participated in other similar studies within the last year. The eligibility criteria at screening and baseline are shown in Figure 1.
The recruitment was carried out at the CHC and lasted for three months. A convenience sampling method was used for the community residents who came to the clinic. If a patient met the criteria listed in Figure 1, he was invited to complete a panel of tests (Table 1) to collect the baseline data. Approximately 500 people were screened for eligibility in each subdistrict, and a total of 492 were eligible to participate in the study over 6 months. They would receive either mHealth hypertension intervention or the usual care in the two subdistricts. All participants had established resident health records at the CHC with community physicians before entering the study.
Table 1.
Summary of study measures at baseline and the end of follow-up
| Measurement | Method | Contents |
|---|---|---|
| Questionnaire | self-administered |
|
| Physiquea | examined by the investigators |
|
| Office blood pressure | examined by the investigators |
|
Notes: aPhysique: All measurements are accurate to one decimal place.
Abbreviations: BP, blood pressure; HPSMBRS, Hypertension Patients Self-Management Behavior Rating Scale; IPAQ-S-C, the Chinese version of short International Physical Activity Questionnaire; HSES, Hypertension Self-Efficacy Scale; CPAT, the compliance in patient with antihypertensive therapy.
Sample size calculation
The change in systolic blood pressure (SBP) after 6 months of intervention or usual care is the main outcome evaluation index, and the sample size of the intervention group is the same as that of the control group. According to previous research, the standard deviations of the intervention group and control group are 15.6 mmHg and 12.2 mmHg, respectively, the allowable error is 7.1 mmHg, and the intraclass correlation coefficient (ICC) is 0.01. On this assumption, a sample size of 152 individuals in each group had to obtain a minimum of 7.1 mmHg difference in SBP change between groups with a power of 90% and a significance level of 5%. As a mobile phone-based intervention study, a slightly higher dropout rate of 35% was expected; thus, 234 individuals in each group needed to be tested in the trial, resulting in a total of 468, which was rounded to a total of 480 individuals across 2 clusters (240 per cluster). All sample size and power calculations were performed using the PASS software (Power Analysis and Sample Size, Version 11, NCSS, Georgia).
Control group
The control group participants in Dadong Subdistrict received the usual education and health promotion, including hypertension knowledge lectures and health brochures in the CHC. They were required to regularly monitor BP, heart rate and uncomfortable symptoms of hypertension at home. Patients with hypertension stages 1, 2 and 3 were followed up once every 3 months, every 2 months and every month, respectively. At each follow-up, the community physician recorded their daily home blood pressure (HBP) in the resident health records and gave personalized advice.
Intervention group
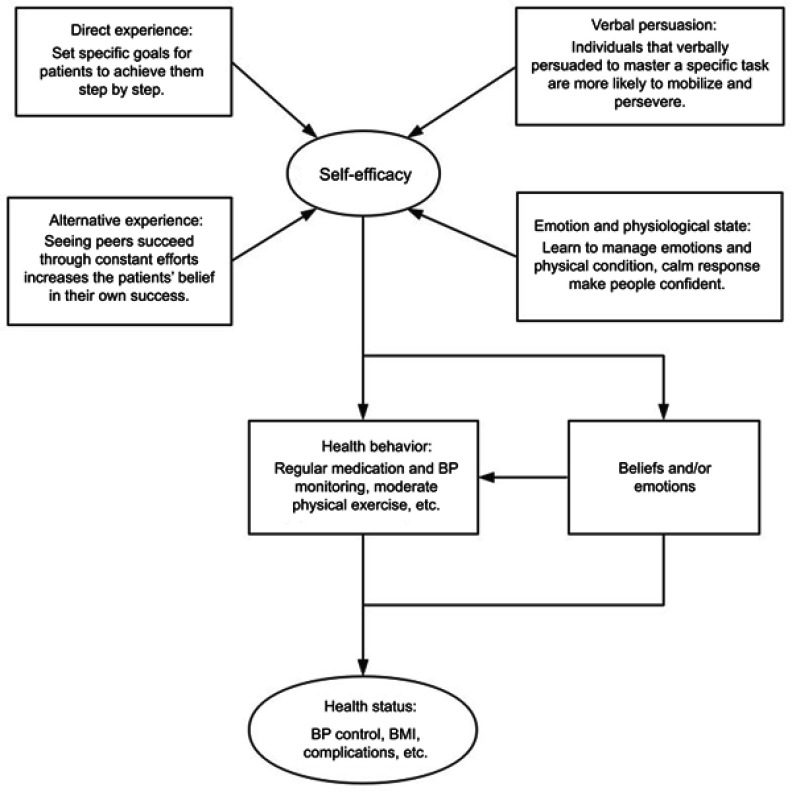
Theoretical basis: the self-efficacy theory
Self-efficacy was proposed by Bandura in 1977 and refers to the individual’s subjective judgment of his ability to perform a specific behavior.29 Self-efficacy is positively correlated to the self-management behaviors (P<0.05).30 The contents of self-management specifically include self-confidence, three self-management tasks and five basic self-management skills, among which self-confidence refers to self-efficacy. Based on the self-efficacy theory, patients can be given various kinds of positive health interventions to improve their level of self-efficacy, which is conducive to the formation of their self-management behavior. After learning related knowledge, skills, confidence and communication skills, patients can solve various physical and emotional problems brought by diseases in daily life mainly by themselves. The study of Warsi et al.31 revealed that self-management can effectively reduce the BP level of patients with hypertension.
The effective ways to improve self-efficacy in disease management include direct experience, alternative experience, verbal persuasion and regulation of emotions and physiological state,29 ultimately improving patients’ health and quality of life through behavioral improvement and emotional control. This study is based on the self-efficacy theory and uses WeChat to guide participants to implement effective self-management and form a healthy lifestyle. The framework of self-efficacy theory is shown in Figure 2.
Figure 2.
The framework of self-efficacy theory in the study.
The baseline grouping
At the baseline survey, the subjects learned the purpose and process of the study and how to fill out an electronic questionnaire and measure BP correctly. Then, they were divided into three groups (prehypertension group, low-intermediate risk group and high-risk group) by cardiovascular risk stratification (Table 2) and requested to subscribe to corresponding WeChat We-Media accounts, which were set up by researchers to publish relevant intervention articles. The three We-Media accounts were named “Anti-hypertension Talents”, “Anti-hypertension Guards”, “Anti-hypertension Doers”, which corresponded to subscribers of the three groups: the prehypertension group, low-intermediate risk patients and high-risk patients. For every 30 individuals in the same cardiovascular risk, a WeChat intervention group was established in the order of inclusion.
Table 2.
Cardiovascular risk stratification of hypertension patients
| Risk factors and medical history | Hypertension Stage 1 SBP 140~159/DBP 90~99 |
Hypertension Stage 2 SBP 160~179/DBP 100~109 |
Hypertension Stage 3 SBP≥180/DBP≥110 |
|---|---|---|---|
| None | Low risk | Intermediate risk | High risk |
| 1~2 risk factorsa | Intermediate risk | Intermediate risk | High risk |
| ≥3 risk factors or complicationsb | High risk | High risk | High risk |
Notes: aRisk factors: male >55 years old, female >65 years old; smoking; dyslipidemia; family history of early onset of cardiovascular disease; obesity (BMI ≥28 kg/m2). bComplications: cerebrovascular disease, heart disease, kidney disease, peripheral vascular disease, retinopathy, diabetes.
The hierarchical intervention measures
The intervention lasted for six months, including health education for the first three months and health behavior promotion for the last three months, while group chat and BP monitoring continued throughout the intervention. The content of health education and the task of behavior promotion were mainly based on Chinese guidelines for the management of hypertension revised for 2018 (the Guidelines).32 The frequency, intensity and content of the intervention measures were determined according to the cardiovascular risk stratification of the subjects. The higher the cardiovascular risk stratification was, the higher the frequency of intervention. The key points of intervention for patients with hypertension are disease management and complication prevention. For people with prehypertension, intervention mainly focuses on how to prevent hypertension (Table 3).
Table 3.
Content of mHealth intervention based on WeChat
| Intervention | Duration | Forms | Frequency | Contents |
|---|---|---|---|---|
| Health education | 3 months | deliver articles of health knowledge to participants via WeChat We-Media accounts |
|
|
| Health promotion | 3 months | offer targeted health advices to participants; implement the punch-in system for fixed goals |
|
|
| Group chatting | 6 months | encourage communication and disease management experience sharing in WeChat groups |
|
|
| Tracking on BP | 6 months | self-report HBPM and regular feedback |
|
|
Abbreviations: BP, blood pressure; HBPM, home blood pressure monitoring; SBP, systolic blood pressure; DBP, diastolic blood pressure.
At the stage of health education, people read health knowledge articles delivered by WeChat in accordance with their cardiovascular risk stratification. To test the degree of knowledge acquisition, a QR code of a relevant quiz was attached at the end of each article. Those earning perfect scores were awarded verbal encouragement. In contrast, if someone did not read the article or finish the quiz within a week, the researchers would contact them privately to find out why not and keep a record. The researchers recorded the article reading frequencies, quiz scores, knowledge contest scores, and times of noncompliance for each participant throughout the whole stage.
In the health promotion phase, participants were required to implement specific behavior proposals consistent with their cardiovascular risk and “punch in” regularly by a short electronic questionnaire (Table 3). With learning and practice constantly strengthened, the difficulty perception of participants in performing a healthy behavior would be reduced. Verbal encouragement was given to those who responded actively and achieved goals. Those who failed to complete fixed goals for two consecutive times or dropped out were contacted privately to determine the reason. The researchers recorded the total punch-in frequencies and adherence to goals for all participants.
Different WeChat groups for participants with different cardiovascular risks were established at the beginning of the intervention. The group chats were initiated by researchers, and people could freely share their disease management experience and physical condition throughout the whole process to increase the execution of health management under the perception of social pressure. The frequencies of group chatting were in accordance with cardiovascular risk stratification (Table 3). Each chat lasted for nearly an hour. Participants could also consult the researchers privately via WeChat and receive a response within 24 hrs.
Blood pressure was tracked throughout the intervention. At the time of inclusion, everyone was asked to self-report BP three times a week, and the report frequency was reduced to once a week if their BP was well controlled. If someone’s BP was not well controlled for two consecutive weeks, the researchers would send an early warning signal to remind him to seek medical advice in time and track his results. The goals for BP were based on Guidelines. The researchers wrote a BP assessment report, which was reviewed by cardiologists, as feedback to participants every month and gave them professional health advice based on the recent data tracked by WeChat.
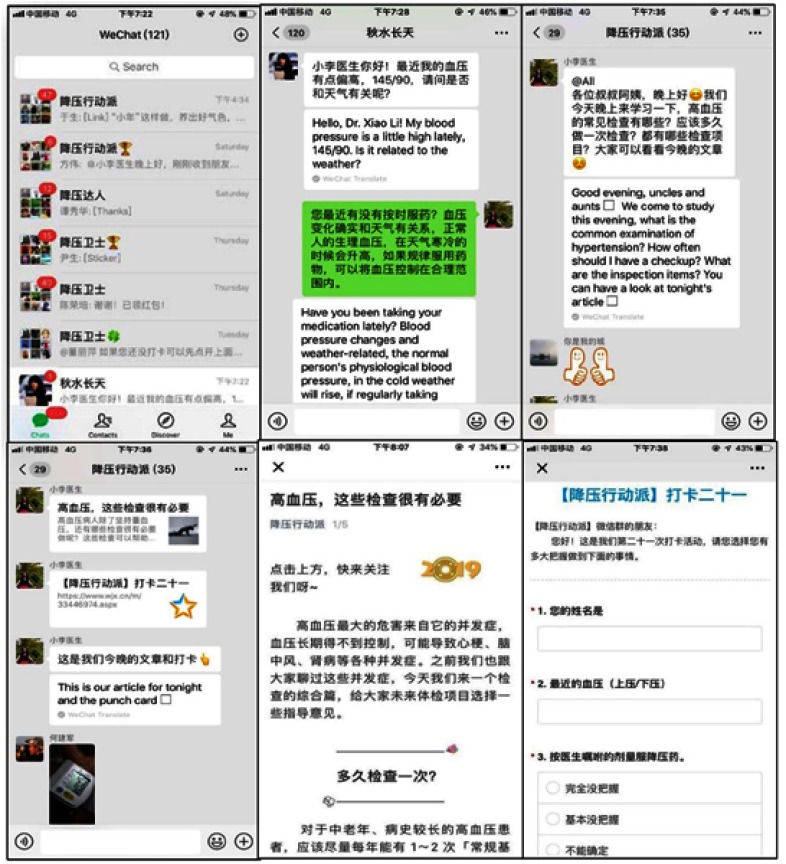
WeChat screenshots are shown in Figure 3, and the entire study process is shown in Figure 4.
Figure 3.
The WeChat app screenshots.
Notes: From left to night top to bottom, the screenshots of WeChat app are Notifications. Health consultation, group chat (1), group chat (2), health articles delivered by We-Media Accounts, and the punch-in questionnaire respectively.
Figure 4.
Flowchart of the study procedures.
Notes: *30-month post-evaluabon: the evaluation of long-term effects of intervention, mainly assessed by the complication incidence (for patients with hypertension) and incidence of hypertension (for population with prehypertenson). **Data statistical analyses: including the economic evaluation.
Abbreviation: BP, blood pressure.
Data collection
At baseline, the subjects were administered a questionnaire and underwent physical examinations including BP, waist and abdominal circumference, height and weight in the CHC (Table 1). The questionnaire included sociodemographic details, hypertension-related health status, hypertension knowledge, medication adherence, self-efficacy and self-management behaviors. In addition to the benchmark survey, two other evaluation time points included an interim evaluation (at the end of the health education stage) and an evaluation at the end of intervention (at the end of the health promotion stage). The measurements of each evaluation are consistent with the baseline. To assess the long-term effects of the intervention, all subjects will be followed up by telephone two years after the end of the intervention to collect the complication incidence (for patients with hypertension) and incidence of hypertension (for those with prehypertension).
In the intervention group, daily BP and health-related behavior were assessed with short electronic questionnaires sent by WeChat. To assess the feasibility of the project, program adherence is measured by participants’ test scores after reading health education articles and their punch-in frequencies in health promotion activities. For the control group, daily BP were collected from resident health records. Finally, the database was established using EpiData Version 3.1 (EpiData Association, Odense, Denmark), and all questionnaires were coded and double entered by two independent professional data-entry staff.
Outcome measures
Primary outcome
The change of SBP after 6 months of intervention or usual care will be taken as the primary outcome, which is calculated by monthly average SBP of subjects. Over the course of the study, BP is measured strictly in accordance with the Guidelines using calibrated electronic sphygmomanometers (HEM-8713; Omron Corporation, Kyoto, Japan).
Secondary outcomes
Hypertension Self-Efficacy Scale (HSES)
This scare is composed of four subscales, namely, daily life, health behavior, medication and self-management, with 15 items in total. It is a scale translated by professionals from the authoritative American scale and is suitable for Chinese people.33 The Likert scale is used to score the project. Patients choose a score based on their confidence in performing certain activities, as the higher the score is, the better the self-efficacy. The questionnaire has been demonstrated to have good structural validity (explaining 79.77% of variance), content validity (r=0.916), and internal consistency (Cronbach’s α=0.852), indicating the feasibility and acceptability of measuring hypertension self-efficacy.34
Hypertension Patients Self-Management Behavior Rating Scale (HPSMBRS)
The hypertension self-management behaviors are measured by the Hypertension Patients Self-Management Behavior Rating Scale (HPSMBRS) designed by Zhao Qiuli and Liu Xiao in 2012. It has six management dimensions (medication, condition monitoring, diet, exercise, work and rest, emotion) and consists of 33 entries. Cronbach’s α coefficients for the subscale and the total scale were 0.757–0.911 and 0.914, respectively.35 This accepted and specialized questionnaire has been widely used to evaluate the self-management of patients with hypertension.36
Medication adherence
The compliance of patient with antihypertensive therapy (CPAT) refers to the degree to which patients with hypertension implement the doctor’s advice.37 Morisky et al.38 reported that four small problems could be used to determine the CPAT of the research object, ie, (1) Have you ever forgotten to take medication? (2) Do you sometimes pay no attention to taking medication? (3) Have you ever stopped taking medication when your symptoms improved? (4) Have you ever stopped taking medication when you felt worse? The answer to these four questions is called the CPAT score. The answer “yes” is scored as 0 and the answer “no” as 1. The cumulative score is 4 for a high CPAT, 2–3 for a medium CPAT, and 0–1 for a low CPAT. To assess the medication adherence before and after the mHealth intervention, this study adopted the Chinese version of the CPAT score translated by Dai Junming,39 which has been validated with a Cronbach’s α coefficient of 0.749 in a previous study.40
Physical activity
The subjects’ daily physical activity and exercise were recorded using the Chinese version of the short International Physical Activity Questionnaire (IPAQ-S-C). The IPAQ-S was developed to measure health-related physical activity (PA) in populations and has been tested extensively in many international population-based prevalence studies.41 There are 7 items on the scale, including moderate and severe physical activity and sitting time. Patients are required to review their physical activity status in the past 7 days and complete the questionnaire according to their subjective feelings. The ICCs ranged from 0.51 to 0.80, and the relative validity ranged from 0.44 to 0.58 for IPAQ-S-C.42
Intervention participation
The evaluation indicators of intervention participation include article reading frequency, test score, punch-in frequency and scores of achieving behavioral goals, which were obtained from the statistical data of the WeChat We-media account and Wenjuanxing System. At the time of each intervention, if 60% of all the participants read health education articles or finished the promotion task (namely, punch-in), we consider the intervention participation degree to be passed; if the above percentage reaches 80% or more, the participation degree is great. For each subject, if the test score or punch-in score reaches 60 points, we consider the intervention measures effective; if it reaches more than 80 points, the effect of the intervention is great.
Incidence of hypertension
This index is mainly collected in the prehypertensive population. Two years after the end of the intervention, the number of people who develop from prehypertension to hypertension will be counted to calculate the incidence of hypertension. Then, the incidence will be compared between the intervention group and the control group to evaluate the effect of the intervention. The calculation formula is as follows:
Other outcome indexes
Other secondary outcomes include the following: 1) physiological index: diastolic blood pressure (DBP) and body mass index (BMI). 2) Index of health behaviors: the frequencies of BP monitoring, smoking and alcohol drinking; the intake of salt, oil, vegetables and fruit. 3) Index of safety: the incidence of complication. Height and weight are measured to calculate BMI, health behavior indicators are assessed through the questionnaire, and the incidence of complication can be obtained from the telephone follow-up two years later.
Cost and effect outcomes
The costs include individual medical expenses and WeChat intervention costs. The former refers to the average monthly cost of drugs, hospitalization costs, and check-up costs, all of which are available through electronic prescription systems and resident health records in the CHC. The costs of WeChat intervention include the development and maintenance costs of We-Media accounts and the labor costs needed for the surveys, and both can be obtained from the expenditure records of the research funds. On the other hand, the effect outcomes refer to the percentage drop of SBP, the change in medication compliance and the control rate of hypertension, which can be collected by questionnaire. The formula is as follows:
Statistical analysis
To obtain a real assessment of the intervention effect, the difference-in-differences (DID) model of longitudinal data will be used to combine “difference before and after” with “difference or not”, adding other covariates that may affect the outcome measures to control influencing factors in the intervention group and the control group. Considering the correlation between BP-values over time in individuals, mixed models will be used to analyze time effect and influencing factors. The covariates at the individual level include demographic factors, such as gender and age, and the covariates at the time level are behavioral factors (ie, salt and vegetable intake, physical activity and medication compliance). Since this study has only two clusters, which may lead to an increase in type 1 error, the Satterthwaite method43 will be used in this model to obtain an approximation of the degree of freedom, which is estimated according to the residual variances at different levels of each variable. As reported by Leyrat et al.,44 the Satterthwaite correction performs well in terms of the type I error rate, especially in some scenarios with low ICC and a high coefficient of variation. Finally, to explore the influencing factors of intervention involvement as well as the correlation between intervention participation and outcome, single-factor analysis and multifactor regression analysis will be conducted on the data of the intervention group. For multiple comparisons, Bonferroni adjustment will be used. During the process of data analyses, the intention-to-treat (ITT) analyses will be performed. Analyses will be performed with SPSS 25.0 and R 3.6.0 software, and a two-tailed P-value<0.05 is considered statistically significant.
Economic evaluation
Cost-effectiveness analysis of the intervention group vs the control group will be undertaken. At the end of the intervention, changes in BP and CPAT as well as the control rate of hypertension will be calculated, and differences in costs between the two groups will be analyzed. The analysis is carried out from the perspective of the national health service; thus, indirect costs, such as the charge for loss of working time, are not taken into account. The direct cost per patient will be calculated based on the utilization of healthcare resources, while the direct cost to the intervention group will also include the development costs of WeChat intervention technology and the labor cost of the intervention. The results will be summarized as incremental cost-effectiveness ratios (ICERs), which are calculated by dividing the mean difference in total costs between the study groups by the mean difference in effects. The nonparametric bootstrapping methods will be used to estimate 95% confidence intervals around cost and effect differences as well as the uncertainty surrounding the ICERs.45 A deterministic sensitivity analysis of the results will also be performed in multi-ways. All analyses will be consistent with accepted economic evaluation methods.46
Ethics
This study protocol conformed to the ethical guidelines of the 2008 Declaration of Helsinki and was approved by the ethics committee of the School of Public Health, Sun Yat-sen University (2017008). All participants wrote informed consent prior to administering the survey. At baseline investigation, all participants were also given a plain process statement of the study.
Trial status
All volunteer recruitment has been completed. At present, we have completed the WeChat intervention in the health education stage of the intervention group, and the behavioral promotion stage is under way. The first result of this cluster randomized controlled trial is expected to be submitted for publication at the end of 2019.
Discussion
Different from many studies focusing on young and middle-aged patients in hospitals, this study takes the natural population in the community as the research object and mainly focuses on the elderly, who are prone to hypertension in the community, which has better practical significance. China has a huge number of people with prehypertension, but the current chronic disease management mainly focuses on patients with hypertension. Participants may benefit from this study because the hierarchical intervention includes management of prehypertension to prevent the development of hypertension, thus bringing forward the intervention time points. For patients with hypertension, it is possible to urge them to form a healthy lifestyle by improving their knowledge, self-efficacy and medication adherence, which may be related to the improvement of health outcomes. By early detection, early diagnosis, and early treatment, hypertension complications can be prevented. Considering that the drug intake information of all subjects could not be collected by WeChat in a timely and uniform fashion, this study will collect the CPAT scores at three fixed time points and compare them between the two groups to more accurately evaluate the change in medication adherence. The study does not involve physical intervention or direct changes in patients’ drug regimens, so the increased risk to patients is minimal.
It took time and required manpower and technological development costs to build up and promote this intervention mode in the early days. With the rapid development of artificial intelligence technology, repetitive and mechanical tasks can be performed uniformly through machines by specific programs; thus, doctors only need to develop personalized intervention strategies for patients at network terminals and address emergencies. The development of technology is a fixed cost, and the more people use it, the smaller the cost becomes. A doctor can manage many patients at the same time online, thus greatly reducing the labor cost. In addition, the continuous popularization of mobile Internet technology reduces the corresponding use cost to the public. In general, this study can provide a beneficial experience for the combination of hypertension prevention and mobile medical treatment and offer a new, convenient, economical and effective hypertension hierarchical management model for the community to reduce the burden of the local medical and health system.
Limitations
The study is not free from limitations. First, with mHealth intervention, a potential risk is that patients will be less likely to return to treatment when needed. WeChat intervention may give wrong diagnosis and guidance, especially for patients who may delay regular follow-up due to good feedback in the WeChat group. However, this risk is moderate. Both researchers are professionals in the field of public health with rich medical knowledge, and they maintain close contact with clinicians to obtain correct guidance and timely correction. To avoid the potential risk of patient information disclosure, a unique code is assigned to each participant throughout the study. Only key researchers have access to the final identification database.
The third limitation of the study is that it is a random grouping not of individuals but of the whole community. Due to the mobility of the population, the interaction between different communities can lead to contamination problems. There is natural geographical isolation between the two selected communities that reduces the population flow between them to some extent. However, the imbalance between the intervention group and the control group at the baseline level may affect the accuracy of the study results. This problem can be solved to some extent by using the DID model, which can control the unbalanced factors at the baseline (such as demographic and sociological factors) as covariates and take differential operation when fitting the model. Finally, for the limitation of research funds and manpower, there are only two clusters in the study, which may lead to an increase in the type I error in the mixed model. Because the two clusters are the same size and the ICC is 0.01, the Satterthwaite correction is used to obtain an approximation of the degree of freedom to control the type I error rate.44 When calculating the sample size, the type II error was controlled within 10%, which could appropriately improve the power of the test to some extent. More clusters with a reasonable number of participants will be included to implement the randomization of a larger number of clusters and maintain an appropriate type I error in future studies.
Conclusion
This study aims to evaluate the effect of the WeChat-based hierarchical management mode on improving blood pressure and self-management behavior in community patients with hypertension and prehypertension. For residents with prehypertension, the incidence of hypertension will be reduced by moving preventive interventions ahead of the onset of disease, and the medical and socioeconomic benefits will be greater. For patients with hypertension, the effect of WeChat management mode is based not only on health-related knowledge but also on self-efficacy and medication adherence. If successful, this management mode will serve as a feasible, economical and efficient hypertension management mode that is suitable for the community.
Acknowledgments
We are grateful to the community healthcare centers of Baiyun Subdistrict and Dadong Subdistrict for assisting us with field investigation. We also appreciate Yan Yan, an undergraduate from the school of public health of Sun Yat-sen University, for her great help in the volunteer recruitment.
Author contributions
TL, WWD, XWL and AHL contributed to the conceptualization of idea and preparation of original draft. TL, WWD and XWL was responsible for the design and improvement of methodology. TL edited the English language. WWD was responsible for the critical review. AHL was responsible for the supervision and project administration. All authors contributed to data analysis, drafting or revising the article, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors have no conflicts of interest in the subject or materials discussed in this paper.
References
- 1.Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2224–2260. doi: 10.1016/S0140-6736(12)61766-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Health Commission of the People’s Republic of China. Report on the Status of Nutrition and Chronic Diseases of Chinese Residents (2015). Beijing: People's Medical Publishing House; 2015. [Google Scholar]
- 3.Chen WW, Gao RL, Liu LS, et al. Summary of Cardiovascular disease report in China 2017. Chin Circ J. 2017;6:521–530. [Google Scholar]
- 4.Lu Y, Lu J, Wang X, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1·7 million adults in a population-based screening study (China PEACE million persons project). Lancet. 2017;390(10112):2549–2558. doi: 10.1016/S0140-6736(17)32478-9 [DOI] [PubMed] [Google Scholar]
- 5.Wang Z, Chen Z, Zhang L, et al. Status of hypertension in China: results from the China Hypertension survey, 2012–2015. Circulation. 2018;137(22):2344–2356. doi: 10.1161/CIRCULATIONAHA.117.032380 [DOI] [PubMed] [Google Scholar]
- 6.Zhang LL. Effect of Community-based Self-management Program among Hypertension Patient. China: Chinese Center for Disease Control and Prevention; 2010. [Google Scholar]
- 7.World Health Organization. Towards the development of an mHealth strategy: a literature review. Available from: http://www.who.int/goe/mobile_health/mHealthReview_Aug09.pdf. Accessed July 22, 2019.
- 8.Burke LE, Ma J, Azar KM, et al. Current science on consumer use of mobile health for cardiovascular disease prevention. Circulation. 2015;132(12):1157–1213. doi: 10.1161/CIR.0000000000000232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Demiris G, Afrin LB, Speedie S, et al. Patient-centered applications: use of information technology to promote disease management and wellness. A white paper by the AMIA knowledge in motion working group. J Am Med Inform Assoc. 2008;15(1):8–13. doi: 10.1197/jamia.M2492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Istepanian RSH, Jovanov E, Zhang YT. Guest editorial introduction to the special section on M-Health: beyond seamless mobility and global wireless health-care connectivity. IEEE Trans Inf Technol Biomed. 2004;8(4):405–414. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Global observatory for eHealth series-Volume 3: mHealth: new horizons for health through mobile technologies. Available from: www.who.int/goe/publications/ehealth_series_vol3/en/. Accessed July 22, 2019.
- 12.Sun DL, Li RL. The application of mobile medicine in the prevention and control of chronic diseases. Chin J Tissue Eng Res. 2016;20(40):6074–6080. [Google Scholar]
- 13.Wang H, Liu F. The construction and development of mobile medical treatment. Comput Syst Appl. 2015;24(12):18–24. [Google Scholar]
- 14.Muralidharan S, Mohan V, Anjana RM, et al. Mobile health technology (mDiab) for the prevention of type 2 diabetes: protocol for a randomized controlled trial. JMIR Res Protoc. 2017;6(12):e242. doi: 10.2196/resprot.8644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Green BB, Cook AJ, Ralston JD, et al. Effectiveness of home blood pressure monitoring, web communication, and pharmacist care on hypertension control: a randomized controlled trial. JAMA. 2008;299(24):2857–2867. doi: 10.1001/jama.299.24.2857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vargas G, Cajita MI, Whitehouse E, Han H-R. Use of short messaging service for hypertension management: a systematic review. J Cardiovasc Nurs. 2017;32(3):260–270. doi: 10.1097/JCN.0000000000000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Logan AG, Irvine MJ, McIsaac WJ, et al. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. Hypertension. 2012;60(1):51–57. doi: 10.1161/HYPERTENSIONAHA.111.188409 [DOI] [PubMed] [Google Scholar]
- 18.Hou J, Ndasauka Y, Pan X, et al. Weibo or WeChat? Assessing preference for social networking sites and role of personality traits and psychological factors. Front Psychol. 2018;9:545. doi: 10.3389/fpsyg.2018.00545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.CNNIC (2015). China Internet Network Information Center the Thirty-Sixth Statistics Report of China Internet Development. Available from: http://www.cnnic.net.cn/hlwfzyj/hlwxzbg/hlwtjbg/201507/P020150723549500667087.pdf
- 20. Zhu D, He Y, Tian F. Social life within HERE: how SNS empowers different generations in China Beijing: Social Sciences Academic Press (China); 2018.
- 21.Statista. Number of monthly active WeChat users from 1st quarter 2012 to 1st quarter 2019 (in millions). Available from: http://www.statista.com/statistics/255778/number-of-active-wechat-messenger-accounts/. Accessed July 22, 2019.
- 22.Tong H. Research on WeChat according to communication study and its influence. Chongqing Social Sci. 2013;9:61–66. [Google Scholar]
- 23.Zhu R, Xu X, Zhao Y, et al. Decreasing the use of edible oils in China using WeChat and theories of behavior change: study protocol for a randomized controlled trial. Trials. 2018;19(1):610–631. doi: 10.1186/s13063-018-2972-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang X, Wen D, Liang J, Lei J. How the public uses social media wechat to obtain health information in China: a survey study. BMC Med Inform Decis Mak. 2017;17(Suppl 2):66. doi: 10.1186/s12911-017-0470-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang Q, Ding FM, Bao JL, et al. Influence of attribution intervention based on WeChat on self-management level of hypertension patients in community. China Medl Herald. 2017;28:162–165. [Google Scholar]
- 26.Dong Y, Wang P, Dai Z, et al. Increased self-care activities and glycemic control rate in relation to health education via Wechat among diabetes patients: a randomized clinical trial. Medicine (Baltimore). 2018;97(50):e13632. doi: 10.1097/MD.0000000000013632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.He C, Wu S, Zhao Y, et al. Social media-promoted weight loss among an occupational population: cohort study using a Wechat mobile phone app-based campaign. J Med Internet Res. 2017;19(10):e357. doi: 10.2196/jmir.7861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yuexiu yearbook editorial department. Yuexiu Yearbook (2017). China: Guangdong Economic Press; 2017. [Google Scholar]
- 29.Bandura A. Self-efficacy: The Exercise of Control. Richmond: Worth Publishers; 1997. [Google Scholar]
- 30.Hu XL, You GY, Li JP. Study on correlation between self-management and self-efficacy of young and middle-aged hypertension patients in community. Chin Nurs Res. 2012;26(16):1523–1525. [Google Scholar]
- 31.Warsi A, Wang PS, LaValley MP, Avorn J, Solomon DH. Self-management education programs in chronic disease: a systematic review and methodological critique of the literature. Arch Intern Med. 2004;164(8):1641–1649. doi: 10.1001/archinte.164.15.1641 [DOI] [PubMed] [Google Scholar]
- 32.Revision Committee for Chinese guidelines for the management of hypertension. Chinese guidelines for the management of hypertension revised for 2018. Prev Treat Cardio-Cerebral-Vascular Dis. 2019;19(1):1–45. [Google Scholar]
- 33.Chen J. Analysis and Intervention of Knowledge, Belief, Behavior in Elderly Patients with Primary Hypertension in Haizhu District of Guangzhou. China: Southern Medical University; 2011. [Google Scholar]
- 34.Ding W, Li T, Su Q, Yuan M, Lin A. Integrating factors associated with hypertensive patients’ self-management using structural equation model: a cross-sectional study in Guangdong, China. Patient Prefer Adherence. 2018;12:2169–2178. doi: 10.2147/PPA.S180314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zhao QL, Liu X. Reliability and validity of the Hypertension Patients Self-Management Behavior Rating Scale (HPSMBRS). Chin Nurs Manage. 2012;12(11):26–31. [Google Scholar]
- 36.Cheng X. The Predictors of Self-Management Behavior in Patients with Hypertension Based on Health Ecological Model. China: Shandong University; 2014. [Google Scholar]
- 37.Bittar N. Maintaining long-term control of blood pressure: the role of improved compliance. Clin Cardiol. 1995;18(6 Suppl 3):III 12–16. doi: 10.1002/clc.4960181504 [DOI] [PubMed] [Google Scholar]
- 38.Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care. 1986;24(1):67. doi: 10.1097/00005650-198601000-00007 [DOI] [PubMed] [Google Scholar]
- 39.Dai J, Fu H, Shen Y. Study on compliance of medication for essential hypertension. Chin J Prev Contr Chron Non-Commun Dis. 2000;8(3):143–145. [Google Scholar]
- 40.Xu W, Wang Q, Liang W. Reliability and validity of Morisky questionnaire in measurement of the compliance with hypertensive medications. Chin J Prev Contr Chron Non-Commun Dis. 2007;15(5):424–426. [Google Scholar]
- 41.Hagströmer M, Oja P, Sjöström M. The International Physical Activity Questionnaire (IPAQ): a study of concurrent and construct validity. Public Health Nutr. 2006;9(6):755–762. [DOI] [PubMed] [Google Scholar]
- 42.Hu B, Lin LF, Zhuang MQ, et al. Reliability and relative validity of three physical activity questionnaires in Taizhou population of China: the Taizhou longitudinal study. Public Health. 2015;129(9):1211–1217. doi: 10.1016/j.puhe.2015.03.024 [DOI] [PubMed] [Google Scholar]
- 43.Satterthwaite FE. An approximate distribution of estimates of variance components. Biometrics. 1946;2:110–114. doi: 10.2307/3002019 [DOI] [PubMed] [Google Scholar]
- 44.Leyrat C, Morgan KE, Leurent B, Kahan BC. Cluster randomized trials with a small number of clusters: which analyses should be used? Int J Epidemiol. 2018;47(1):321–331. doi: 10.1093/ije/dyx169 [DOI] [PubMed] [Google Scholar]
- 45.Bosmans JE, van der Laan DM, Yang Y, et al. The cost-effectiveness of an intervention program to enhance adherence to antihypertensive medication in comparison with usual care in community pharmacies. Front Pharmacol. 2019;10:210. doi: 10.3389/fphar.2019.00210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Briggs A, Claxton K, Sculpher M. Decision Modelling for Health Economic Evaluation. New York: Oxford University Press; 2006. [Google Scholar]