Abstract
Recent years have witnessed a rapid growth in our understanding of the pathogenic property of monoclonal proteins. It is evident that some of these small monoclonal proteins are capable of inducing end-organ damage as a result of their intrinsic physicochemical properties. Hence, an umbrella term, monoclonal gammopathy of clinical significance (MGCS), has been coined to include myriad conditions attributed to these pathogenic proteins. Because kidneys are the most commonly affected organ (but skin, peripheral nerves, and heart can also be involved), we discuss MGRS exclusively in this review. Mechanisms of renal damage may involve direct or indirect effects. Renal biopsy is mandatory and demonstration of monoclonal immunoglobulin in kidney, along with the corresponding immunoglobulin in serum or urine, is key to establish the diagnosis. Pitfalls exist at each diagnostic step, and a high degree of clinical suspicion is required to diagnose MGRS. Recognition of MGRS by hematologists and nephrologists is important, because timely clone-directed therapy improves renal outcomes. Autologous stem cell transplant may benefit selected patients.
Introduction
Recently, it was recognized that a small number of patients with a monoclonal gammopathy (MG) in the serum/urine do not meet the criteria for the diagnosis or treatment of symptomatic multiple myeloma (MM), Waldenstrom macroglobulinemia (WM), chronic lymphocytic leukemia (CLL), or other malignant non-Hodgkin lymphomas (NHLs) present with renal dysfunction and pathological findings on renal biopsy specimens.1-3 As a result, the term “monoclonal gammopathy of renal significance” (MGRS) was coined in 2012 to increase awareness among hematologists and nephrologists and to consider initiation of appropriate therapy.2 Although clone-directed therapy leads to improves renal outcome, not all patients with renal impairment and MG of undetermined significance (MGUS) have MGRS, and diagnosis of MGRS depends on the appropriate clinicopathological context.2 In this article, we review the definition, epidemiology, pathogenesis, and classification of MGRS. Current concepts in the understanding of MGRS diagnosis, management, and renal outcomes are also highlighted. Description of the 2 real-world cases of MGRS is provided in the supplemental Data.
MGRS: background
MG refers to the presence of monoclonal immunoglobulin in the serum/urine in its intact form or as fragments produced by an expanded clone of B cells, plasma cells, or lymphoplasmacytic cells. Whereas plasma cells secrete a range of monoclonal proteins, intact immunoglobulin (immunoglobulin G [IgG] > IgA > IgM > IgD > IgE), and free light chains, B cells and lymphoplasmacytic cells typically produce IgM > IgG.3,4 MGUS and smoldering MM (SMM) are plasma cell dyscrasias (PCDs) that are characterized by the absence of end-organ damage.1 The prevalence of MGUS in the general population is ∼0.7% and increases with age (3.2% in people older than 50 years, and 5.3% in those older than 70 years). The risk of progression to MM in MGUS is variable (0.5%-1.5% per year) depending on risk factors.5 Because end-organ damage is not a feature of MGUS, it is considered “benign,” and treatment of this entity with antimyeloma therapy is not recommended. Current consensus suggests monitoring of serum paraprotein level, serum free light chains (sFLCs), blood counts, and organ chemistry to look for end-organ damage.6
A small percentage of patients with renal impairment have a “nonmyeloma” MG at the time of initial presentation or one that is detected later during follow-up. In a further observation, a retrospective review of 5410 kidney biopsies showed that 2.5% had monoclonal Ig deposition. Typically, these patients had a small paraprotein in the serum/urine and were labeled as having MGUS, as per the International Myeloma Working Group diagnostic criteria.7 Therefore, MGUS in these patients could no longer be considered benign, and the hemato-nephrological term MGRS was introduced in 2012 to emphasize the importance of MG in the setting of renal disease. MGRS encompasses a group of renal disorders with a range of renal pathology findings in the presence of an MG. The size of the paraprotein and the associated B-cell clone (“small dangerous B-cell clone”) is typically small.8 Conventionally, renal damage in the setting of high tumor burden (symptomatic MM, WM malignant lymphoma, and CLL) is not considered MGRS.2 Recently, the International Kidney and Monoclonal Gammopathy Research Group (IKMG) updated the definition of MGRS to include all B-cell/plasma cell clonal proliferative disorders not requiring immediate treatment of the clonal disease: SMM, smoldering WM, low-grade CLL, and low-grade NHL (marginal zone lymphoma, mantle cell lymphoma, and mucosa-associated lymphoid tissue lymphoma).9 Nephrotoxic monoclonal proteins are implicated in the pathogenesis of MGRS directly or indirectly, as a result of their unique physicochemical properties rather than the tumor bulk per se.10 But caveats exist; patients with C3 glomerulopathy (C3G) and renal-limited atypical hemolytic uremic syndrome (referred to as thrombotic microangiopathy [TMA] in this article) with MG do not demonstrate monoclonal protein deposition in the kidney, and some patients with MGRS lack an identifiable monoclonal protein (discussed under "Diagnosing MGRS: a challenge").4,11,12
Epidemiology and clinical importance of MGRS
MGRS has been estimated from previous observations at 10% of cases of MGUS, with a prevalence of 0.32% and 0.53% in people older than 50 years and 70 years, respectively.5,13 Since its first formal description in 2012, published evidence describe the natural history of MGRS. Key findings from these studies are listed below.
Renal function declines in MGRS patients with a potential to progress to end-stage renal disease (ESRD). Renal diseases with MG (MGRS) have a worse renal survival (not requiring dialysis or becoming dialysis independent) compared with those without MGRS.14
Monoclonal proteins produced by B-cell/plasma cell clones mediate MGRS; clone-directed therapy using novel chemotherapeutic combinations results in improved renal survival.15 Treatment of the underlying hematological disorder in light chain amyloidosis (AL amyloidosis), monoclonal immunoglobulin deposition disease (MIDD), proliferative glomerulonephritis (GN) with monoclonal immunoglobulin deposition (PGNMID), and C3G has resulted in improved renal survival compared with no treatment or immunosuppressive medications.11,16-19
Recurrence after renal transplantation has been documented in MGRS patients in whom incomplete hematological remission was achieved before renal transplant, making complete hematological remission a prerequisite in MGRS when renal transplantation is contemplated.20-27
There is an urgent need to maintain awareness of MGRS in routine hematology, pathology, and nephrology practice, working in a multidisciplinary setting, to prevent end-stage renal damage and surveillance to monitor for progression to an overt hematological malignancy.
Classification of MGRS
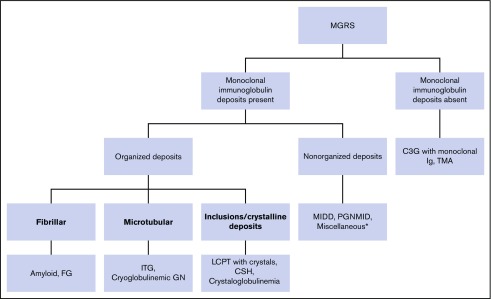
Renal parenchyma can be broadly divided into 3 structural and functional compartments: glomerulus, tubulointerstitium, and vasculature. Conceptually, monoclonal deposits in MGRS can affect any or all of these compartments. Therefore, 1 way of classifying MGRS is based on the dominant site of monoclonal deposition (Table 1). It is an arbitrary schema because most MGRS lesions involve >1 compartment within a single entity, and significant overlap exists.5 Another method of classification relies on the histological and ultrastructural findings (Figure 1).2,28 Both classifications are pertinent: although the former is clinically relevant because it helps to clarify the pathogenesis and clinical features of MGRS, the latter is relevant from a diagnostic standpoint. Nevertheless, both schemes are commonly used together in clinical practice for better clinicopathological correlation.
Table 1.
Classification of MGRS entities based on presence and site of deposition of monoclonal proteins in renal structures
| MGRS with monoclonal protein deposition in renal structures | ||
|---|---|---|
| Glomerular deposition | Tubulointerstitial deposition | Intrarenal vascular deposition |
| Amyloidosis (AL/AH/AHL) | LCPT with and without crystals | Amyloidosis |
| Monoclonal fibrillary glomerulopathy | CSH | Crystalglobulinemia |
| Immunotactoid glomerulopathy | Amyloidosis | MIDD |
| Cryoglobulinemic GN (types I and II) | MIDD | Cryoglobulinemic GN (types I and II) |
| MIDD (LCDD/HCDD/HLDD) | ||
| PGNMID | ||
| MPGN associated with monoclonal immunoglobulin | ||
| MN secondary to monoclonal immunoglobulin | ||
| MGRS without monoclonal protein deposition in renal structures | ||
|---|---|---|
| Glomerular involvement | Tubulointerstitial involvement | Intrarenal vascular involvement |
| C3GN | TMA | |
| TMA | POEMS syndrome | |
| POEMS syndrome | ||
AH, heavy chain amyloidosis; AHL, heavy and light chain amyloidosis; AL, light chain amyloidosis; C3GN, C3 glomerulonephritis; CSH, crystal-storing histiocytosis; HCDD, heavy chain deposition disease; HLDD, heavy and light chain deposition disease; LCDD, light chain deposition disease; LCPT, light chain proximal tubulopathy; MN, membranous nephropathy; POEMS, polyneuropathy organomegaly endocrinopathy monoclonal gammopathy, and skin changes.
Adapted from Ciocchini et al5 with permission.
Figure 1.
Classification of MGRS based on the ultrastructural findings of the monoclonal deposits. *Includes non-MGRS kidney diseases, such as anti-glomerular basement membrane (glomerular basement membrane (GBM) disease, membranous nephropathy, and Henoch-Schonlein purpura (HSP). These are presumed to be due to a monoclonal protein acting as an autoantibody (against antigen on glomerular basement membrane in anti-GBM disease and PLA2R in membranous nephropathy). Notably, a single subclass restriction (IgG1κ), absence of PLA2R staining, and associated proliferative changes on renal biopsy are indicative of MGRS in occasional cases of membranous nephropathy with monoclonal immunoglobulin.37 Rare cases of HSP with IgA nephropathy have been associated with monoclonal IgA or MM. These patients experience frequent relapses and a high recurrence rate postrenal transplantation.9 FG, fibrillary glomerulopathy; Ig, immunoglobulin; ITG, immunotactoid glomerulonephritis.
Pathogenesis of MGRS
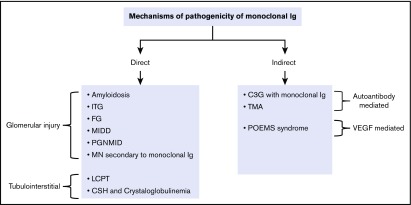
Renal involvement can be seen in high and low tumor cell burden, but the term MGRS is often restricted to the latter. This has been clarified in a recent IKMG consensus to include all levels of tumor burden, even when they do not automatically qualify for therapy.9 Unique physicochemical properties of the monoclonal protein, as well as host factors like tissue pH, interaction with the local environment, and tissue binding, contribute to the pathogenesis of MGRS.9 The mechanisms of renal injury in MGRS fall into 2 broad categories based on the demonstration of monoclonal protein in the kidneys: direct and indirect (Figure 2).29
Figure 2.
Mechanisms of MGRS pathogenicity. VEGF, vascular endothelial growth factor.
Direct mechanisms
Renal handling of monoclonal proteins is variable; light chains and truncated heavy chains are freely filtered across the glomerulus owing to their small molecular weight, but intact immunoglobulin molecules are entrapped in the glomerulus. Light chains are normally internalized by the proximal tubular cells via receptor-mediated endocytosis and degraded in the lysosomal system, resulting in very small amounts of free light chains in the urine. Therefore, renal injury resulting from the presence of intact immunoglobulin molecules is limited to the glomerulus, whereas light chains and truncated heavy chains can potentially affect all renal compartments. We further classify the direct mechanism according to the main site of injury: glomerular and tubulointerstitial.7,10,28-31
Glomerular injury.
Deposited light and truncated heavy chains/immunoglobulin molecules interact with the resident glomerular cells and activate signaling pathways that result in inflammation and tissue injury.10,32 This mechanism may explain the renal damage seen in amyloidosis and MIDD. Amyloidogenic light chains (VλVI) in AL amyloidosis change the properties of mesangial cells to a macrophage type that endocytose them. As a result of their intrinsically abnormal nature, light chains are partially digested, converted to fibrils after misfolding, and finally secreted extracellularly where they are deposited in association with other components (apolipoprotein, serum amyloid protein) as amyloid fibrils. Increased matrix metalloproteinases have also been implicated in mesangial matrix destruction.33,34 Light chains (VκIV) in LCDD convert mesangial cells into myofibroblasts, which, in turn, secrete excessive mesangial matrix and platelet-derived growth factor (PDGF), leading to a nodular glomerulosclerosis membranoproliferative appearance.35,36 A subset of membranous GN shows light chain restriction, usually κ on renal biopsy (Figure 1, “Miscellaneous” category).19,37 Mechanisms of glomerular injury in other MGRS lesions, such as PGNMID, ITG, FG, MPGN with monoclonal immunoglobulin, and cryoglobulinemic GN are poorly understood. Notably, the majority of FG cases demonstrate polyclonal glomerular immunoglobulin deposition. Only those cases with monotypic deposition (monoclonal FG; referred to as FG in this article) are considered MGRS.28
Tubulointerstitial injury.
Tubules and interstitium can be affected by either light chains (most often κ) produced in excess with an intact immunoglobulin or rarely, truncated heavy chains, which can be filtered across the glomerulus.7,38 When the resorptive capacity of the tubules is outweighed by excess light chains, they accumulate in proximal tubular epithelium and resist degradation by the lysosomal proteases because of the unique variable domain (Vκ1). Interference with lysosomal function leads to generation of reactive oxygen species, sustained inflammation, and tubular constipation. LCPT is a broad term referring to proximal tubular damage induced by light chains resulting in disrupted resorption capability, with or without Fanconi syndrome (FS) and acute tubular injury. Progressive renal failure can ensue.7 Two main morphological variants are described.
LCPT with inclusions: rhomboid, needle-shaped, or rectilinear eosinophilic inclusions (periodic acid–Schiff [PAS] negative) are found by light microscopy (LM). In all cases, κ restriction can be demonstrated by immunofluorescence, especially in pronase digestion–treated sections. This condition is commonly associated with FS.7,39,40
LCPT without inclusions: excessive vacuolar or droplet changes, tubule cell necrosis, detachment, and apical blebbing are common findings on LM. In contrast with LCPT with inclusions, λ light chains might be the cause in one third of the cases, and electron microscopy (EM) demonstrates cytoplasmic droplets and vacuoles, with no evidence of crystalloid inclusions. The frequency of this subtype is variable (13%- 77%).7,41,42
Indirect mechanisms
Monoclonal protein cannot be demonstrated in the kidney biopsy in certain MGRS entities, supporting an indirect role for monoclonal proteins in the pathogenesis.29 This view is strengthened by the observation that the clone-directed therapy results in improved renal outcome. Under this category, we would include 3 provisional MGRS entities: C3G, TMA, and POEMS syndrome.11,12,43 The first 2 entities result from MG behaving as an autoantibody.28
C3G and TMA.
C3G is a well-known entity that is characterized by dominant C3 renal deposits by IF and, often, a GN with a membranoproliferative pattern. C3 GN (C3GN) and TMA result from dysregulation of the alternative complement pathway. Recent reports described an unusually high prevalence of MG in C3GN and TMA patients compared with the age-matched general population (Table 2).11,12,44,45 Hypothetically, the monoclonal protein acts as an autoantibody against complement regulatory proteins, especially complement factor H, or as a stabilizer C3 convertase (C3 nephritic factor), resulting in sustained C3 activation. These mechanisms can coexist in the same patient.44,45
Table 2.
Incidence of detectable monoclonal protein, most commonly found MGs, and the reported hematological disorders associated with MGRS
| Type of monoclonal immunoglobulin deposition | Associated renal pathologies | Incidence of detectable MG | Most common type of paraprotein/MG | Associated hematological disorders |
|---|---|---|---|---|
| Intact immunoglobulin molecule/immunoglobulin molecule with truncated heavy chain* | ALH amyloidosis4,10,28,29* | 97%-100% | IgGλ | MM, CLL |
| LHCDD10,28,29,46,47* | SPEP/IFE: 80%-100% | IgGκ | MM (50%) | |
| UPEP/IFE: 80%-100% | ||||
| sFLC assay: 100% | ||||
| Cryoglobulinemic GN28,29,48,49 | Type 1: 76%-82.5% | Type I IgG/IgM with κ | Type 1: MM, WM, CLL, B-NHL, MGRS, HCL | |
| Type 2: 40%-49% | Type II IgMκ | Type 2: B-CLPD, LPL, MALToma, WM | ||
| PGNMID10,29,31,50 | 20%-30% | IgG3 | Rare (4.4%): MM, CLL, NHL | |
| ITG9,28,29,51 | 63%-71% | IgG1 | CLL (19%), LPL (13%), MM (13%) | |
| FG28,52-54 | 15%-17% | IgG | MM, CLL | |
| Light chains only | AL amyloidosis4,10,28,29 | 97%-100% | VλVI | MM, LPL, CLL |
| LCDD10,28,29,46,47 | SPEP/IFE: 25%-76% | VκIV | MM (39%-59%), MGRS (39%), LPL | |
| UPEP/IFE: 42%-90% | ||||
| sFLC assay: 100% | ||||
| LCPT9,28,29,41,55 | 93.4%-97% | VκI | MGRS (27%-46%), MM (14%-33%), SMM (15%-51%), NHL (4%), CLL (2%), WM (8%) | |
| CSH9,28,29,56 | 81.8%-90% | κ | MM, LPL, MGRS (rare) | |
| Heavy chains only | AH amyloidosis4,10,28,29* | 97%-100% | IgG | MM |
| HCDD10,28,29,46,47* | SPEP/IFE: 67%-100% | IgG1 | MM (29%) | |
| UPEP/IFE: 50%-100% | ||||
| sFLC assay: 100% | ||||
| No monoclonal protein xdemonstrable in kidneys | C3G (C3GN and DDD)28,29,45,57-60† | 33%-83% | IgGκ | MGRS (60%-77.8%), MM (4%-13.9%), SMM (5.6%-30%), CLL/lymphoma (5.6%-6%), type 1 cryoglobulinemia (2.8%) |
| TMA29,57† | 13.7% (>50 y, 21%; >60 y, 24%) | IgGκ | MGRS (75%), MM (5%), SMM (5%), POEMS (10%), T-cell lymphocytic leukemia (5%) | |
| Atypical | MN secondary to monoclonal immunoglobulin19,37 | 0%-21.4% | IgG1κ | CLL/SLL (17.8%-28.5%), MM (7.1%), SMZL (3%) |
B-CLPD, B-cell chronic lymphoproliferative disorder; B-NHL, B-cell NHL; DDD, dense deposition disease; HCL, hairy cell leukemia; IFE, immunofixation electrophoresis; LHCDD, light and heavy chain deposition disease; LPL, lymphoplasmacytic lymphoma; MALToma, mucosa-associated lymphoid tissue lymphoma; SLL, small lymphocytic lymphoma; SMZL, splenic marginal zone lymphoma; SPEP, serum protein electrophoresis; UPEP, urine protein electrophoresis.
Shows entities with truncated heavy chains.
Provisional MGRS entities.
POEMS syndrome.
Microangiopathic renal lesions seen in this syndrome are thought to be mediated by vascular endothelial growth factor released by the clonal plasma cells. An in-depth review of this feature is provided elsewhere.61
Clinical presentation
There is a wide spectrum of MGRS clinical presentations, with variable combinations of proteinuria, hematuria, renal insufficiency, hypertension, and hypocomplementemia. We find it useful to describe the constellation of these features as distinct syndromes for better clinical applicability (Table 3).29 Broadly, glomerular disorders present with nephrotic syndrome (NS) or nephritic-nephrotic syndrome (variable combinations of proteinuria, hematuria, hypertension, low complement levels, and renal insufficiency). Although the former presentation is common in amyloidosis and MIDD, the latter is more typical of proliferative glomerulopathies. Tubulointerstitial disorders (LCPT) usually present with tubular proteinuria, electrolyte abnormalities, with/without progressive renal insufficiency, and FS. FS is manifested by global proximal tubular dysfunction (ie, glycosuria, aminoaciduria, uricosuria, phosphaturia, and type 2 renal tubular acidosis). Acute renal failure is typical of TMA.28,29 Extrarenal manifestations may be superimposed on these entities (Table 4). Clinical presentation may vary within a particular entity, depending on the dominant site of injury. For example, amyloidosis may present with progressive renal insufficiency rather than NS if renal vasculature is the dominant site of amyloid deposition.28,29
Table 3.
Syndromic approach to the clinical presentation of MGRS
| Clinical syndrome/presentation | Associated MGRS entities |
|---|---|
| NS | Amyloidosis (glomerular), MIDD |
| Nephritic-nephrotic syndrome (proteinuria, hematuria, hypertension, low complement levels, and renal insufficiency) | PGNMID, ITG, FG, C3G with monoclonal immunoglobulin, cryoglobulinemic GN |
| Acute renal failure | TMA, MIDD, and crystalglobulinemia |
| Proteinuria/progressive renal insufficiency | LCPT (with/without FS), MIDD, amyloidosis (tubulointerstitial and vascular), CSH, TMA |
Adapted from Sethi et al29 with permission.
Table 4.
Summary of the reported end-organ manifestations in MGRS entities
| MGRS subtype | Organs affected/manifestations | References |
|---|---|---|
| Amyloidosis | Heart, liver, autonomic nerves, skin, gastrointestinal tract, pulmonary | 62 |
| MIDD | Liver, heart, peripheral nerves, lung, skin (seen in 35% of cases) | 28,63-65 |
| Cryoglobulinemic GN | Vasculitis, Raynaud’s phenomenon, purpura, livedo reticularis, arthralgia, peripheral neuropathy | 29,48,49 |
| C3G | Skin necrosis | 11 |
| LCPT with FS | Osteomalacia | 28 |
| Crystalglobulinemia | Skin rash, polyarthralgia, neuropathy | 29,66 |
| CSH | FS, spleen, lymph nodes, macrophage activation, cornea, lungs, thyroid, parotid gland, synovium, liver, brain, skin, subcutaneous fat | 9,55 |
| POEMS syndrome | Sensory motor polyneuropathy, organomegaly, endocrinopathy, skin | 61 |
Diagnosing MGRS: a challenge
Diagnosing MGRS remains challenging for hematologists, nephrologists, and renal pathologists. Often, patients have a delayed diagnosis, with the resultant renal function being significantly worse before clone-directed therapy is instituted. This underscores the importance of maintaining a low threshold for clinically suspecting MGRS. Clinical suspicion of MGRS arises when an MGRS-compatible lesion is identified on kidney biopsy or an MG is detected in a patient with renal impairment. Because not all patients with the latter have MGRS, recent IKMG suggestions for kidney biopsy may help hemato-nephrologists with clinical decision making.9 Correlation between MG and monoclonal deposit in the renal biopsy specimen is essential, because a discrepancy would argue against the diagnosis of MGRS.9 A renal pathologist should screen for monoclonal protein deposits in all of the compartments of a renal biopsy specimen. Accurate clinical information should be available because not all MGRS lesions demonstrate monoclonal protein deposition in kidney (for instance, C3G and TMA) and vice versa.3,12,44,45 To this end, we will discuss the step-wise diagnostic approach to MGRS, pitfalls in currently available tests, and challenges faced by clinicians while dealing with a suspected case of MGRS.
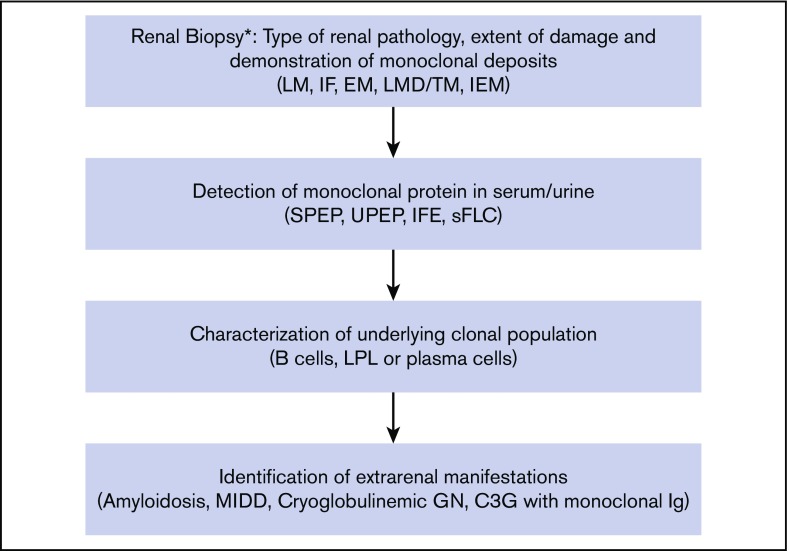
As shown in Figure 3, the diagnosis of MGRS has 4 elements: (1) renal biopsy for identification of the pattern of renal parenchymal damage and demonstration of monoclonal protein, if present, (2) identification of the corresponding monoclonal protein in the serum and/or urine, (3) demonstration of the underlying clonal population of cells secreting the monoclonal protein, and (4) characterization of extrarenal manifestations of the clonal disorder.3 The incidence and type of detectable monoclonal protein, as well as the associated hematological disorders with MGRS conditions, are summarized in Table 2.
Figure 3.
Proposed step-wise algorithm for the diagnosis of MGRS. *Renal biopsy advised if ≥1 of acute kidney injury (AKI) stage 3, estimated glomerular filtration rate (eGFR) < 60 mL/min per 1.73 m2 and >2 mL/min per 1.73 m2 per year decline, proteinuria and hematuria, albumin/creatinine ratio > 30 mg/mmol, and FS (hypouricemia).9 *Renal biopsy considered if ≥1 of AKI stage 1 or 2, eGFR < 60 mL/min per 1.73 m2 and <2 mL/min per 1.73 m2 per year decline, albumin/creatinine ratio 3 to 30 mg/mmol and eGFR > 60 mL/min per 1.73 m2, hematuria and eGFR < 60 mL/min per 1.73 m2, and evidence of light chain proteinuria.9 *Defer renal biopsy if stable eGFR, bland urinalysis, and no evidence of light chain proteinuria.9 In ∼40% of cases, monoclonal protein is not demonstrated in serum/urine. In such cases, renal biopsy should be considered in the diagnostic algorithm depending on the clinical suspicion.3 In cases of MGRS-compatible renal lesion with monoclonal immunoglobulin deposition, a diagnosis of MGRS should be considered and therapy instituted, because a monoclonal protein might not be demonstrated in some of these cases, despite a thorough evaluation (eg, PGNMID, FG). The latter situation could arise due to the extremely small amount of monoclonal protein that escapes detection by conventional methods or a result of pitfalls in the current diagnostic assays. IEM, immunoelectron microscopy; IF, immunofluorescence; LMD, laser microdissection; TM, tandem mass spectrometry. Adapted from Leung et al9 with permission.
Renal biopsy
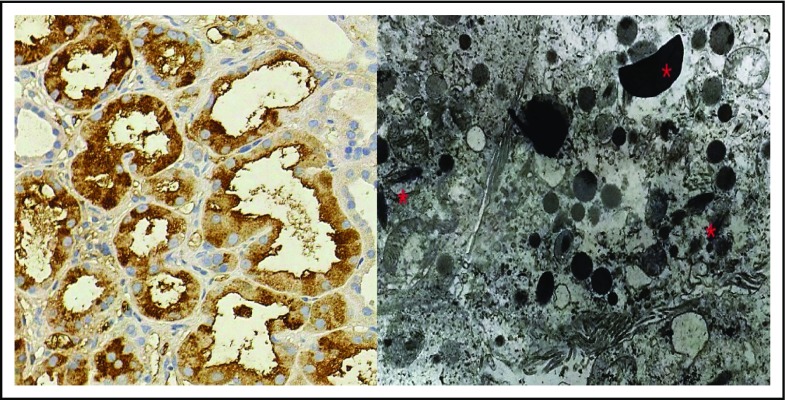
Renal biopsy is a relatively safe procedure in patients with MGRS and carries a similar risk for hemorrhagic complications (4.1%) as in patients without MGRS.67 Renal biopsy could potentially be avoided in certain cases of amyloidosis for which a biopsy from less-invasive sites (abdominal fat pad, gingival or rectal) has successfully demonstrated amyloid deposition.68 The biopsy specimen must be processed for LM, as well as for IF using antibodies for light chains, heavy chains, and intact immunoglobulin molecules. IgG subclass IF is essential in cases associated with intact monoclonal immunoglobulin or truncated heavy chain deposition (Table 2). Complement deposition (C3 with or without C1q) could be demonstrated in certain MGRS entities (PGNMID, ITG, C3GN, HCDD, light and heavy chain deposition disease, and cryoglobulinemic GN). The need for ancillary investigations like pronase digestion, EM, immunogold labeling, and laser microdissection, followed by liquid chromatography and mass spectrometry (LC-MS), is discussed further.9 Despite thorough work-up, IF may fail to identify some cases of amyloidosis as a result of the hidden antigen epitopes within the fibrillar structure.69 Conversely, false-positive IF may be seen in amyloidosis as a result of nonspecific tissue binding of circulating monoclonal proteins.70 IF can be negative in cases of LCPT and crystal-storing histiocytosis (CSH) as a result of the intracellular localization of monoclonal light chains. Tissue processing, including an antigen-retrieval step by pronase digestion, helps to detect intracellular light chains. Occasional cases of congophilic FG could be reliably distinguished from amyloidosis by DNAJB9 immunohistochemistry (IHC) staining and LC-MS.71,72 LC-MS is indispensable for amyloid subtyping and identification of IgD HCDD (associated with a negative IF).9 EM offers valuable supplementary information regarding the substructure of organized deposits (amyloid, fibrils, immunotactoids, cryoglobulins, and light chains) and their localization.56,73 It is especially important to appreciate that >1 pattern may exist in the same patient. As an example, 6% of patients with C3G may have TMA changes, and MIDD can present with amyloidosis.11,54 LM, IF, and EM findings of various MGRS lesions are summarized in Table 5. Figures 4-6 highlight the renal biopsy findings in LCPT, LCDD, and C3G, respectively (provided by M.S.).
Table 5.
Summary of the main pathological findings in MGRS
| Glomerular diseases | LM | IF/IHC | EM |
|---|---|---|---|
| Amyloidosis | Congo red+ mesangial expansion/nodules | AL: LC restriction (mostly λ) | Unbranched randomly distributed fibrils (8-12 nm diameter) |
| Hairbrush projections from glomerular basement membranes | AH: HC deposits (g1 or g4, or a) | ||
| Congo red+ deposits in interstitium and vessel walls (occasional) | AHL: LC and HC deposits | ||
| FG* | Congo red−, silver− mesangial expansion | Mesangial and capillary loop IgG, C3, κ and λ deposits | Unbranched, randomly distributed 15-20 nm diameter fibrils |
| Positivity for DNAJB9 on IHC | |||
| ITG | Membranous-like or MPGN-like changes | Coarse mesangial IgG (monoclonal in 60% of cases), C3 and occasional IgM deposits | Microtubules (20-60 nm diameter) |
| Congo red−, silver− mesangial expansion | |||
| Type I cryoglobulinemic GN | MPGN pattern | Monoclonal immunoglobulin (most frequently κ) of the same type as found in circulation, C3, C4 deposits | Paired microtubules (25-40 nm diameter) |
| Endocapillary proliferative pattern/exudation | |||
| PAS+ capillary pseudothrombi common | |||
| MIDD | Mesangial proliferation and Congo red−, silver+ mesangial matrix expansion/nodules | LCDD: mesangial and/or glomerular basement membrane monoclonal LC deposits | Powdery electron-dense deposits along inner aspect of glomerular basement membranes, mesangium, and outer aspect of tubular basement membranes |
| HCDD: κ and λ negative, staining for 1 of the immunoglobulins (most commonly IgG or IgM) | |||
| PGNMID | Endocapillary proliferative GN/MPGN | Monoclonal immunoglobulin or, more rarely, monoclonal LC deposits | Nonorganized mesangial, subendothelial, and subepithelial electron-dense deposits |
| Membranous GN with monoclonal immunoglobulin | Membranous changes (spikes, lucencies) | Monoclonal immunoglobulin deposits | Nonorganized subepithelial electron-dense deposits |
| C3G associated with monoclonal gammopathy | Endocapillary proliferative GN/MPGN | Granular, C3-dominant deposits | Nonorganized mesangial, subendothelial, and subepithelial electron-dense deposits |
| Dense osmiophilic transformation of basement membranes if DDD | |||
| TMA | Glomerular and/or arterial TMA | Pauci-immune pattern; occasional C3 trapping | Acute: subendothelial flocculent material |
| Chronic: new subendothelial basement membrane and/or subendothelial widening | |||
| Tubulointerstitial diseases | |||
| LCPT | Proximal tubular vacuolation/fragmentation | LC inclusions within tubular epithelium | Intralysosomal or free rhomboid-shaped crystals in proximal tubules |
| Intracytoplasmic inclusions, often crystalloid | |||
| Miscellaneous | |||
| CSH | Accumulated crystals within macrophages/histiocytes within glomerular or peritubular capillaries and in the mesangium | LC crystalloid inclusions within macrophages/histiocytes | Rhomboid and needle-shaped crystalloid inclusions and vacuoles within macrophages/histiocytes. |
HC, heavy chain; LC, light chain.
Occasional cases of FG could show congophilia (congophilic FG). These cases could be reliably distinguished from amyloid deposits by DNAJB9 immunostain or mass spectroscopy.72
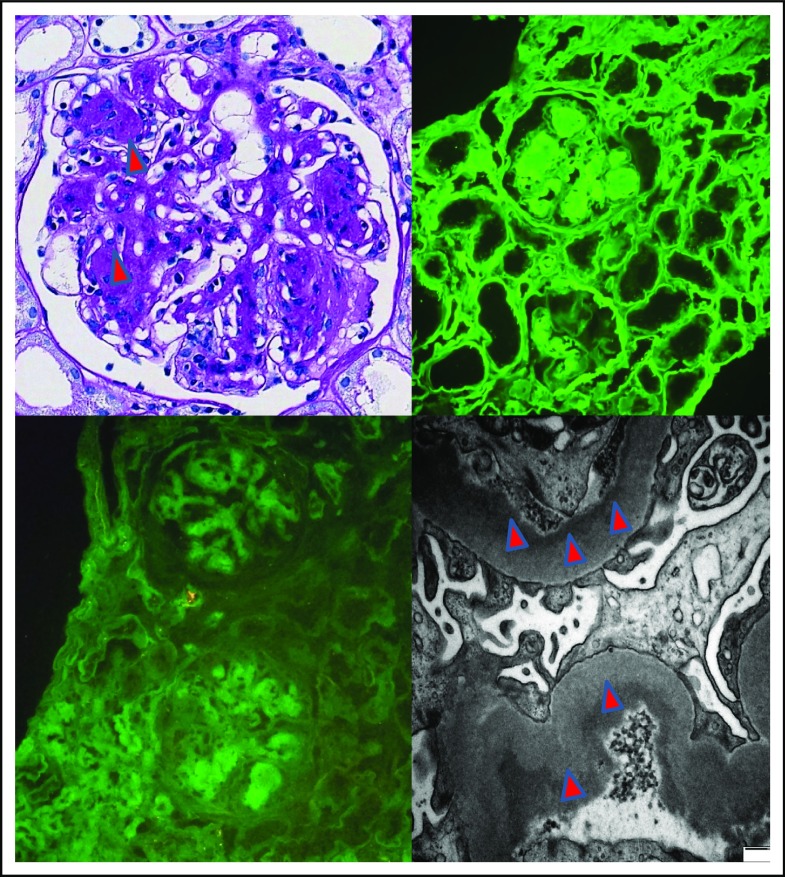
Figure 4.
Features of LCPT. IHC stained strongly positive for κ light chain in proximal tubules; λ (data not shown) was negative (original magnification ×400; DAB + Harris’s hematoxylin stain; left panel). TE microscopy image shows rhomboid crystal inclusions (*) in keeping with light chain proximal tubulopathy (original magnification ×4000; right panel).
Figure 5.
Features of an LCDD. Glomerulus with nodular mesangial expansion (arrowheads; original magnification ×400; PAS; upper left panel). IF showed strong positivity for κ light chain (upper right panel); compare with negative λ (lower left panel) in glomerular and tubular basement membranes and mesangial nodules, in keeping with a κ LCDD (original magnification ×200; fluorescein isothiocyanate). TE microscopy image shows powdery electron-dense deposits along basement membranes (arrowheads) in keeping with LCDD (original magnification ×6000, fluorescein isothiocyanate; lower right panel).
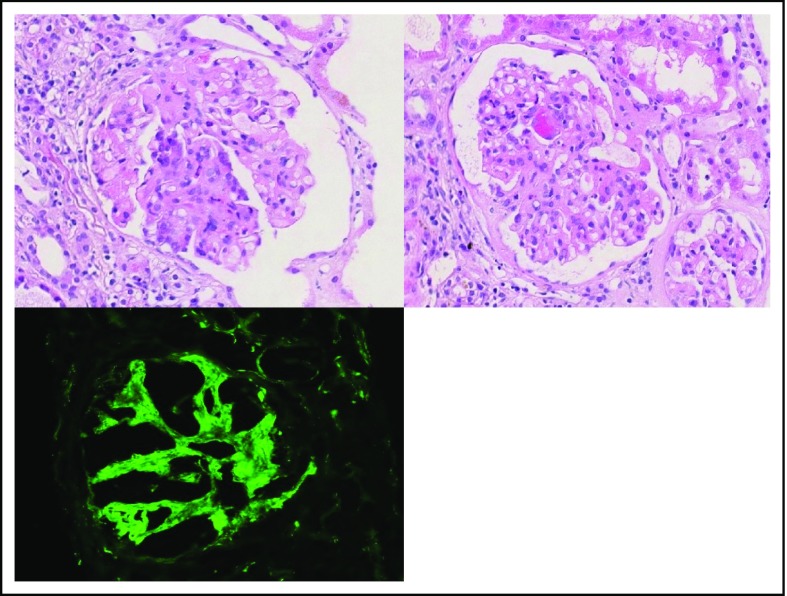
Figure 6.
Features of a C3GN in the setting of MGRS. Glomerulus with segmental endocapillary hypercellularity (original magnification ×400; hematoxylin & eosin stain; upper left panel). Glomerulus with segmental capillary tuft fibrinoid necrosis (original magnification ×400; hematoxylin & eosin stain; right panel). IF showed C3-dominant deposits in the mesangium and capillary loops, in keeping with a C3-dominant GN (original magnification ×400; fluorescein isothiocyanate; lower left panel).
Identification of paraprotein
The next step is to identify monoclonal protein in the serum and urine of patients suspected to have MGRS. Correlation between tissue and serum monoclonal protein is important, because ∼10% patients with hereditary amyloidosis were misdiagnosed as having AL amyloidosis based on serum MG in 1 series.74 Notably, paraprotein is typically small in these patients and is often undetectable by the available methods.28 This scenario is variable, depending upon the type of MGRS.3 Paraprotein is identified by serum and urine electrophoresis with a detection limit of 0.3 to 0.5 g/dL and 0.7 g/dL in the γ and α/β regions, respectively.75 Because only free light chains are filtered across the glomerulus, urine electrophoresis is the least sensitive test to identify an MG, but it is valuable in distinguishing cast nephropathy from AL amyloidosis/MIDD, because it shows dominant light chains in the former condition and selective albuminuria in the latter 2 conditions.76,77 Serum/urine immunofixation electrophoresis characterizes the type of MG and is more sensitive than electrophoresis (detection limit of 0.1 g/dL).4,78 Immunoblotting (not widely available) is highly sensitive for detecting small amounts of monoclonal immunoglobulin, characterization of heavy chain subclass, and identification of first constant domain deletion of heavy chain.30 Measurement of sFLCs using polyclonal antibodies for light chain epitopes (Freelite, Birmingham, United Kingdom) is the most sensitive method for the detection of MG. It is based on the concept that even plasma cells secreting an intact immunoglobulin secrete an excess of light chains in the serum. Due to the catabolism of free light chains by the proximal tubular cells, urine Freelite assay is an insensitive method. The normal range for sFLCs (κ/λ ratio) has been defined as 0.26 to 1.65 in a normal renal function setting. Any perturbation of this ratio could indicate monoclonality, although the “renal range” of sFLCs has been defined as 0.37 to 3.17. Renal impairment causes an increase in free κ and λ chains in the serum (κ > λ) and resulting dependence on the reticuloendothelial system for the elimination of light chains.4,78,79 sFLCs are pivotal for response assessment in AL amyloidosis and MIDD.65,80 Newer methods for sFLC measurement have been developed, including a monoclonal antibody–based assay, N latex nephelometric assay, and Luminex assay, but none are standardized, and Freelite continues to be used most commonly.4 Intriguingly, a serum IF is more sensitive than sFLCs in cases of PCDs producing an intact immunoglobulin molecule, such as PGNMID.81 Time-of-flight mass spectrometry and urinary exosomes are the newer techniques with a higher sensitivity than sFLCs for the detection of low levels of a paraprotein characteristic of MGRS.82-84 Table 2 highlights the incidence of a positive MG in patients with MGRS. The use of different methods might explain the variability in the detection of MG.
Clonal identification
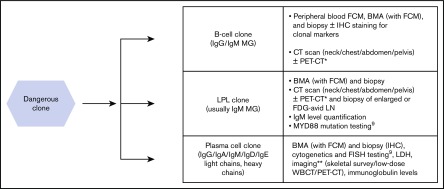
After establishing the presence of an MG and its correlating monoclonal protein in the renal biopsy, the diagnostic approach should characterize the underlying clonal population of cells and should be based on the type of paraprotein. Because a lymphoplasmacytic clone typically produces IgM, relevant tissue (bone marrow/lymph node) must be obtained after cross-sectional imaging (eg, computed tomography scan). Clonal characterization is extremely important from a therapeutic perspective, because a B-cell/lymphoplasmacytic clone typically requires incorporation of anti-CD20 antibody (rituximab) in the treatment regimen, and a plasma cell clone is managed along the lines of PCD/MM.3 Figure 7 elaborates the structured approach to clonal identification in a case of MGRS and gives a battery of investigations that may be performed.9 Use of appropriate investigation for clonal identification requires an individualized approach.
Figure 7.
Diagnostic work-up for clonal identification in MGRS. *Imaging could help identify lymphadenopathy in low-grade, low-stage lymphoma.9 **Imaging could be performed to identify plasmacytoma, bone lesions in a suspected case of MM, and when bone marrow aspiration (BMA) and biopsy fails to detect the plasma cell clone.9 Note: despite a similar work-up, a distinction between B-cell and LPL clone is helpful, both for a precise diagnosis, and for wider therapeutic options available for LPL (both rituximab- and bortezomib-based therapies). MYD88 mutation is positive in about 90% cases of LPL/WM.9 A positive result would therefore be supportive, but an absence would not rule out the diagnosis. Considering a low proliferative rate of low-grade B-cell lymphoproliferative disorders, and LPL, positron emission tomography–computed tomography (PET-CT) may have a lower degree of sensitivity compared to high-grade NHL. However, PET-CT could be useful in such cases given the avoidance of iodinated contrast, and a potential for directed biopsy from an area of increased metabolic uptake to enhance the diagnostic yield.3 FCM, flow cytometry; FDG-avid LN, fluorodeoxyglucose avid lymph nodes; FISH, fluorescent in situ hybridization; LDH, lactate dehydrogenase; WBCT, whole-body computed tomography.
Extrarenal manifestations
Identification of the extrarenal involvement secondary to the MG is critical from a therapeutic and prognostic perspective. Cardiac involvement in AL amyloidosis is considered a high-risk feature and confers a poor prognosis requiring urgent initiation of chemotherapy to reduce the burden of amyloidogenic free light chains.2,28,64,85 Autologous stem cell transplant (ASCT) may be suitable for selected patients with Mayo stage I/II cardiac amyloidosis but is contraindicated in stage III patients owing to extremely high transplant-related mortality.86,87 Table 4 summarizes the MGRS conditions associated with extrarenal involvement. Organ-directed testing (2-dimensional echocardiogram, troponin level, N-terminal pro-B–type natriuretic peptide level, cardiac magnetic resonance imaging for cardiac, nerve conduction studies for paranasal sinuses, skin biopsy for cutaneous, endoscopy and biopsy for gastrointestinal involvement) should be used based on the history and clinical examination findings.62,87
Treatment and outcome
Treatment of MGRS is directed at the underlying B-cell or plasma cell clones. Historically, reluctance among clinicians to treat MGRS was due to toxicity concerns, including secondary malignancies with the use of alkylating agents in a condition that was considered relatively benign.2 Therefore, therapy in MGRS aims at improving renal survival (reduction in proteinuria or serum creatinine or delayed/no need for dialysis or independence from dialysis) and reducing the recurrence after renal transplantation.2,3 Studies have shown that the renal survival of patients with MGRS has improved, and achievement of hematological response with treatment correlates with a renal response.2,64 Treatment is based on a combination of chemotherapeutic agents used to treat PCD or NHL optimizing for safety in the setting of renal failure, as well as extrarenal involvement (especially cardiac). The following guiding principles apply while treating MGRS.
Baseline glomerular filtration rate is prognostic for predicting renal outcome, as shown in PGNMID, MIDD, and amyloidosis. Therefore, prompt initiation of therapy is recommended before irreversible renal damage occurs.22,46,88,89
Early initiation of chemotherapy is indicated in the presence of chronic kidney disease (CKD) stage 1-3 to reduce the production of monoclonal immunoglobulin and achieve a deep hematological response. Response may be consolidated with ASCT to achieve deeper and sustained hematological and renal remissions.90
For patients with CKD stage 4 or ESRD, chemotherapy is indicated only if they are planned for a renal transplant or if coexisting extrarenal involvement is present (especially cardiac, liver, or pulmonary). Achieving a complete hematological response prior to renal transplant is necessary to avoid the risk of recurrence of MGRS in the renal allograft and ensuing graft failure. ASCT may be used in this setting before proceeding with a renal transplant. For patients with extrarenal involvement, therapy may improve the function of the extrarenal organ.90
Response assessment in MGRS is challenging. In patients who have a detectable MG, paraprotein may be followed up for hematological response assessment based on the International Myeloma Working Group criteria used for amyloidosis. In cases lacking a detectable baseline paraprotein, patients may be followed up using proteinuria and renal function (creatinine). Renal response in MGRS could be assessed using the organ-response criteria for amyloidosis.3,80
Appropriate dose reduction is required for certain drugs in the setting of renal failure.3
Because amyloidosis and POEMS syndrome have been reviewed extensively,61,62 we have reviewed the literature regarding the treatment outcomes of other MGRS entities. Most of the studies in MGRS involve isolated case reports or small case series. No formal guidelines exist regarding the treatment of MGRS. However, expert opinion/consensus-based treatment decisions can guide clinical practice (Table 6).90 In the next section, we discuss the outcomes of LCDD and C3G and summarize the most recent available data on renal outcomes for all MGRS entities in supplemental Table 1.11,12,19,20,22,24-26,41,51,52,58,64,89,91-93
Table 6.
Consensus opinions for the treatment of selected MGRS conditions
| MGRS entity | Current consensus/recommendation |
|---|---|
| MIDD | CKD stage I-III: bortezomib-based therapy, followed by ASCT (in the absence of extrarenal manifestations and good performance status) |
| CKD stage IV-V: eligible for renal transplant, bortezomib-based therapy followed by ASCT; not eligible for renal transplant, bortezomib-based therapy only (to protect extrarenal organs, heart) | |
| PGNMID | CKD stage I-II with proteinuria < 1 g/d and nonprogressive disease: symptomatic treatment |
| CKD stage I-II with proteinuria > 1 g/d or progressive disease and CKD stage III-IV: chemotherapy* with or without ASCT | |
| CKD stage V: eligible for renal transplant, chemotherapy followed by ASCT; not eligible for renal transplant, symptomatic management; no identifiable MG: no consensus, may benefit from chemotherapy prior to renal transplant | |
| ITG | CLL-type regimens incorporating bendamustine/corticosteroids/cyclophosphamide with rituximab For cases not associated with CLL, bortezomib-based regimens |
| Type 1 cryoglobulinemic GN | Treatment indication: symptomatic/progressive systemic disease (renal), depends on underlying clone |
| Plasma cell: antimyeloma drugs (ASCT may be considered) | |
| LPL clone: treat along lines of WM (rituximab backbone) | |
| B-cell clone: rituximab-based therapy | |
| Type 2 cryoglobulinemic GN | HCV+ |
| Minimally symptomatic: antiviral therapy | |
| Symptomatic vasculitis: rituximab/high-dose dexamethasone (+ antiviral therapy) | |
| Rapidly progressive renal disease: TPE + definitive therapy as for symptomatic vasculitis (above) | |
| HCV− | |
| Minimally symptomatic: observation | |
| Symptomatic vasculitis: rituximab | |
| WM/B-cell NHL: rituximab-based regimens (according to the underlying condition) | |
| LCPT with FS | CKD stage I-III: chemotherapy based on bortezomib/cyclophosphamide/thalidomide/bendamustine, ASCT may be considered for nonresponding patients |
| CKD stage IV-V: eligible for renal transplant, bortezomib-based therapy followed by ASCT; not eligible for renal transplant, symptomatic management |
HCV, hepatitis C virus; TPE, therapeutic plasma exchange.
Adapted from Fermand et al.90
For PGNMID cases, choice of chemotherapy should be clone directed. For plasma cell clone, bortezomib-based regimens, like cyclophosphamide/bortezomib/dexamethasone; for B-cell clone, rituximab-based regimens may be used. Because clone is detected in only ∼30% of cases of PGNMID, an empirical therapy directed at the hypothesized clone may be used.92
LCDD and C3G
The 1-year and 5-year overall survival (OS) in LCDD patients was found to be 89% and 70%, respectively, in contrast with corresponding renal survival rates of 67% and 37%.94 In a large series on LCDD, ASCT and proteasome inhibitor–based treatments were significantly associated with a hematological response compared with other therapies. Achievement of a complete hematological remission was associated with a renal response. Five-year OS and 5-year renal survival were 67% and 57%, respectively.89 Sayed et al reported the median renal survival and OS of LCDD patients to be 5.4 years and 14 years, respectively.64 Of the 7 patients in that cohort whose underlying clonal disorder was in hematological remission and who received a renal allograft, none had disease recurrence after a median of 9.7 years.64 Retrospective data from monoclonal immunoglobulin–associated C3G illustrated that the renal response and median renal survival were higher in patients who achieved a hematological response after chemotherapy.11 Zand et al reviewed the outcome of patients after renal transplant for ESRD due to C3G and noted a recurrence rate of 66.7% after a median of 28 months; half of these patients also had a graft failure.24
Conclusions
MGRS is an umbrella term that encompasses renal damage mediated directly or indirectly by monoclonal protein. Awareness of MGRS among clinicians and renal pathologists is critical to suspect, investigate, and diagnose it in a timely fashion. Early clone-directed treatment based on expert consensus is crucial to improve the renal survival of these patients. Studies with a larger sample size are needed for the formulation of treatment and follow-up guidelines.
Supplementary Material
The full-text version of this article contains a data supplement.
Authorship
Contribution: A.J. wrote the manuscript; K.R. and J.K. conceptualized, edited, and supervised the manuscript; M.S. wrote the renal pathology portion of the manuscript and provided histopathology images; R.H. contributed to the clinical nephrology aspect of the manuscript; A.K. provided the details about the 2 cases of MGRS that are described in the supplemental Data; and all authors reviewed and approved the draft individually.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Karthik Ramasamy, Level 2, Cancer and Hematology Centre, Churchill Hospital, Oxford OX3 7LE, United Kingdom; e-mail: kramasamy@nhs.net.
References
- 1.Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538-e548. [DOI] [PubMed] [Google Scholar]
- 2.Leung N, Bridoux F, Hutchison CA, et al. ; International Kidney and Monoclonal Gammopathy Research Group . Monoclonal gammopathy of renal significance: when MGUS is no longer undetermined or insignificant. Blood. 2012;120(22):4292-4295. [DOI] [PubMed] [Google Scholar]
- 3.Hogan JJ, Weiss BM. Bridging the divide: an onco-nephrologic approach to the monoclonal gammopathies of renal significance. Clin J Am Soc Nephrol. 2016;11(9):1681-1691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leung N, Barnidge DR, Hutchison CA. Laboratory testing in monoclonal gammopathy of renal significance (MGRS). Clin Chem Lab Med. 2016;54(6):929-937. [DOI] [PubMed] [Google Scholar]
- 5.Ciocchini M, Arbelbide J, Musso CG. Monoclonal gammopathy of renal significance (MGRS): the characteristics and significance of a new meta-entity. Int Urol Nephrol. 2017;49(12):2171-2175. [DOI] [PubMed] [Google Scholar]
- 6.Go RS, Rajkumar SV. How I manage monoclonal gammopathy of undetermined significance. Blood. 2018;131(2):163-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herrera GA. Proximal tubulopathies associated with monoclonal light chains: the spectrum of clinicopathologic manifestations and molecular pathogenesis. Arch Pathol Lab Med. 2014;138(10):1365-1380. [DOI] [PubMed] [Google Scholar]
- 8.Merlini G, Stone MJ. Dangerous small B-cell clones. Blood. 2006;108(8):2520-2530. [DOI] [PubMed] [Google Scholar]
- 9.Leung N, Bridoux F, Batuman V, et al. The evaluation of monoclonal gammopathy of renal significance: a consensus report of the International Kidney and Monoclonal Gammopathy Research Group. Nat Rev Nephrol. 2019;15(1):45-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doshi M, Lahoti A, Danesh FR, Batuman V, Sanders PW; American Society of Nephrology Onco-Nephrology Forum . Paraprotein-related kidney disease: kidney injury from paraproteins-what determines the site of injury? Clin J Am Soc Nephrol. 2016;11(12):2288-2294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chauvet S, Frémeaux-Bacchi V, Petitprez F, et al. Treatment of B-cell disorder improves renal outcome of patients with monoclonal gammopathy-associated C3 glomerulopathy. Blood. 2017;129(11):1437-1447. [DOI] [PubMed] [Google Scholar]
- 12.Ravindran A, Go RS, Fervenza FC, Sethi S. Thrombotic microangiopathy associated with monoclonal gammopathy. Kidney Int. 2017;91(3):691-698. [DOI] [PubMed] [Google Scholar]
- 13.Steiner N, Göbel G, Suchecki P, Prokop W, Neuwirt H, Gunsilius E. Monoclonal gammopathy of renal significance (MGRS) increases the risk for progression to multiple myeloma: an observational study of 2935 MGUS patients. Oncotarget. 2017;9(2):2344-2356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shaik M, Al-Janadi A. Long term survival of monoclonal gammopathy of renal significance (MGRS): an analysis of Nhanes III. Blood. 2014;124:4849. [Google Scholar]
- 15.Fermand JP, Bridoux F, Dispenzieri A, et al. Monoclonal gammopathy of clinical significance: a novel concept with therapeutic implications. Blood. 2018;132(14):1478-1485. [DOI] [PubMed] [Google Scholar]
- 16.Leung N, Dispenzieri A, Fervenza FC, et al. Renal response after high-dose melphalan and stem cell transplantation is a favorable marker in patients with primary systemic amyloidosis. Am J Kidney Dis. 2005;46(2):270-277. [DOI] [PubMed] [Google Scholar]
- 17.Lorenz EC, Gertz MA, Fervenza FC, et al. Long-term outcome of autologous stem cell transplantation in light chain deposition disease. Nephrol Dial Transplant. 2008;23(6):2052-2057. [DOI] [PubMed] [Google Scholar]
- 18.Bridoux F, Hugue V, Coldefy O, et al. Fibrillary glomerulonephritis and immunotactoid (microtubular) glomerulopathy are associated with distinct immunologic features. Kidney Int. 2002;62(5):1764-1775. [DOI] [PubMed] [Google Scholar]
- 19.Guiard E, Karras A, Plaisier E, et al. Patterns of noncryoglobulinemic glomerulonephritis with monoclonal Ig deposits: correlation with IgG subclass and response to rituximab. Clin J Am Soc Nephrol. 2011;6(7):1609-1616. [DOI] [PubMed] [Google Scholar]
- 20.Czarnecki PG, Lager DJ, Leung N, Dispenzieri A, Cosio FG, Fervenza FC. Long-term outcome of kidney transplantation in patients with fibrillary glomerulonephritis or monoclonal gammopathy with fibrillary deposits. Kidney Int. 2009;75(4):420-427. [DOI] [PubMed] [Google Scholar]
- 21.Leung N, Lager DJ, Gertz MA, Wilson K, Kanakiriya S, Fervenza FC. Long-term outcome of renal transplantation in light-chain deposition disease. Am J Kidney Dis. 2004;43(1):147-153. [DOI] [PubMed] [Google Scholar]
- 22.Nasr SH, Sethi S, Cornell LD, et al. Proliferative glomerulonephritis with monoclonal IgG deposits recurs in the allograft. Clin J Am Soc Nephrol. 2011;6(1):122-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pinney JH, Lachmann HJ, Sattianayagam PT, et al. Renal transplantation in systemic amyloidosis-importance of amyloid fibril type and precursor protein abundance. Am J Transplant. 2013;13(2):433-441. [DOI] [PubMed] [Google Scholar]
- 24.Zand L, Lorenz EC, Cosio FG, et al. Clinical findings, pathology, and outcomes of C3GN after kidney transplantation. J Am Soc Nephrol. 2014;25(5):1110-1117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lorenz EC, Sethi S, Leung N, Dispenzieri A, Fervenza FC, Cosio FG. Recurrent membranoproliferative glomerulonephritis after kidney transplantation. Kidney Int. 2010;77(8):721-728. [DOI] [PubMed] [Google Scholar]
- 26.Said SM, Cosio FG, Valeri AM, et al. Proliferative glomerulonephritis with monoclonal immunoglobulin G deposits is associated with high rate of early recurrence in the allograft. Kidney Int. 2018;94(1):159-169. [DOI] [PubMed] [Google Scholar]
- 27.Angel-Korman A, Stern L, Sarosiek S, et al. Long-term outcome of kidney transplantation in AL amyloidosis. Kidney Int. 2019;95(2):405-411. [DOI] [PubMed] [Google Scholar]
- 28.Bridoux F, Leung N, Hutchison CA, et al. ; International Kidney and Monoclonal Gammopathy Research Group . Diagnosis of monoclonal gammopathy of renal significance. Kidney Int. 2015;87(4):698-711. [DOI] [PubMed] [Google Scholar]
- 29.Sethi S, Rajkumar SV, D’Agati VD. The complexity and heterogeneity of monoclonal immunoglobulin-associated renal diseases. J Am Soc Nephrol. 2018;29(7):1810-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bridoux F, Javaugue V, Bender S, et al. Unravelling the immunopathological mechanisms of heavy chain deposition disease with implications for clinical management. Kidney Int. 2017;91(2):423-434. [DOI] [PubMed] [Google Scholar]
- 31.Leung N, Drosou ME, Nasr SH. Dysproteinemias and glomerular disease. Clin J Am Soc Nephrol. 2018;13(1):128-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Teng J, Russell WJ, Gu X, Cardelli J, Jones ML, Herrera GA. Different types of glomerulopathic light chains interact with mesangial cells using a common receptor but exhibit different intracellular trafficking patterns [published correction appears in Lab Invest. 2004;84(9):1219]. Lab Invest. 2004;84(4):440-451. [DOI] [PubMed] [Google Scholar]
- 33.Keeling J, Teng J, Herrera GA. AL-amyloidosis and light-chain deposition disease light chains induce divergent phenotypic transformations of human mesangial cells. Lab Invest. 2004;84(10):1322-1338. [DOI] [PubMed] [Google Scholar]
- 34.Charitaki E, Kastritis E, Petraki C, et al. Glomerular expression of matrix metalloproteinases in AL-amyloidosis and association with renal function at the time of kidney biopsy. Clin Nephrol. 2016;85(1):44-54. [DOI] [PubMed] [Google Scholar]
- 35.Herrera GA. Renal manifestations of plasma cell dyscrasias: an appraisal from the patients’ bedside to the research laboratory. Ann Diagn Pathol. 2000;4(3):174-200. [DOI] [PubMed] [Google Scholar]
- 36.Herrera GA, Shultz JJ, Soong SJ, Sanders PW. Growth factors in monoclonal light-chain--related renal diseases. Hum Pathol. 1994;25(9):883-892. [DOI] [PubMed] [Google Scholar]
- 37.Best Rocha A, Larsen CP. Membranous glomerulopathy with light chain-restricted deposits: a clinicopathological analysis of 28 cases. Kidney Int Rep. 2017;2(6):1141-1148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ugai T, Tsuda K, Sugihara H, et al. Renal Fanconi syndrome associated with monoclonal κ free light chain in a patient with Waldenström macroglobulinemia. Br J Haematol. 2013;162(1):1. [DOI] [PubMed] [Google Scholar]
- 39.Nasr SH, Valeri AM, Sethi S, et al. Clinicopathologic correlations in multiple myeloma: a case series of 190 patients with kidney biopsies. Am J Kidney Dis. 2012;59(6):786-794. [DOI] [PubMed] [Google Scholar]
- 40.Herrera GA. The contributions of electron microscopy to the understanding and diagnosis of plasma cell dyscrasia-related renal lesions. Med Electron Microsc. 2001;34(1):1-18. [DOI] [PubMed] [Google Scholar]
- 41.Stokes MB, Valeri AM, Herlitz L, et al. Light chain proximal tubulopathy: clinical and pathologic characteristics in the modern treatment era. J Am Soc Nephrol. 2016;27(5):1555-1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Larsen CP, Bell JM, Harris AA, Messias NC, Wang YH, Walker PD. The morphologic spectrum and clinical significance of light chain proximal tubulopathy with and without crystal formation. Mod Pathol. 2011;24(11):1462-1469. [DOI] [PubMed] [Google Scholar]
- 43.Sanada S, Ookawara S, Karube H, et al. Marked recovery of severe renal lesions in POEMS syndrome with high-dose melphalan therapy supported by autologous blood stem cell transplantation. Am J Kidney Dis. 2006;47(4):672-679. [DOI] [PubMed] [Google Scholar]
- 44.Lin M, Haas M. Paraprotein-associated thrombotic microangiopathy: expanding the spectrum of renal disease related to plasma cell dyscrasias. Kidney Int. 2017;91(3):532-534. [DOI] [PubMed] [Google Scholar]
- 45.Ciocchini M, Musso CG. Which should be the correct treatment for monoclonal gammopathy of renal significance with complement alternative pathway dysregulation (C3 glomerulopathy and atypical hemolytic uremic syndrome): clone-directed or anticomplement therapy? Int Urol Nephrol. 2018;50(7):1365-1366. [DOI] [PubMed] [Google Scholar]
- 46.Nasr SH, Valeri AM, Cornell LD, et al. Renal monoclonal immunoglobulin deposition disease: a report of 64 patients from a single institution. Clin J Am Soc Nephrol. 2012;7(2):231-239. [DOI] [PubMed] [Google Scholar]
- 47.Lin J, Markowitz GS, Valeri AM, et al. Renal monoclonal immunoglobulin deposition disease: the disease spectrum. J Am Soc Nephrol. 2001;12(7):1482-1492. [DOI] [PubMed] [Google Scholar]
- 48.Sidana S, Rajkumar SV, Dispenzieri A, et al. Clinical presentation and outcomes of patients with type 1 monoclonal cryoglobulinemia. Am J Hematol. 2017;92(7):668-673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bryce AH, Kyle RA, Dispenzieri A, Gertz MA. Natural history and therapy of 66 patients with mixed cryoglobulinemia. Am J Hematol. 2006;81(7):511-518. [DOI] [PubMed] [Google Scholar]
- 50.Gowda KK, Nada R, Ramachandran R, et al. Proliferative glomerulonephritis with monoclonal immunoglobulin deposition disease: the utility of routine staining with immunoglobulin light chains. Indian J Nephrol. 2015;25(6):344-348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Nasr SH, Fidler ME, Cornell LD, et al. Immunotactoid glomerulopathy: clinicopathologic and proteomic study. Nephrol Dial Transplant. 2012;27(11):4137-4146. [DOI] [PubMed] [Google Scholar]
- 52.Nasr SH, Valeri AM, Cornell LD, et al. Fibrillary glomerulonephritis: a report of 66 cases from a single institution. Clin J Am Soc Nephrol. 2011;6(4):775-784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Rosenstock JL, Markowitz GS, Valeri AM, Sacchi G, Appel GB, D’Agati VD. Fibrillary and immunotactoid glomerulonephritis: distinct entities with different clinical and pathologic features. Kidney Int. 2003;63(4):1450-1461. [DOI] [PubMed] [Google Scholar]
- 54.Motwani SS, Herlitz L, Monga D, Jhaveri KD, Lam AQ; American Society of Nephrology Onco-Nephrology Forum . Paraprotein-related kidney disease: glomerular diseases associated with paraproteinemias. Clin J Am Soc Nephrol. 2016;11(12):2260-2272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lebeau A, Zeindl-Eberhart E, Müller EC, et al. Generalized crystal-storing histiocytosis associated with monoclonal gammopathy: molecular analysis of a disorder with rapid clinical course and review of the literature. Blood. 2002;100(5):1817-1827. [PubMed] [Google Scholar]
- 56.Vignon M, Javaugue V, Alexander MP, et al. Current anti-myeloma therapies in renal manifestations of monoclonal light chain-associated Fanconi syndrome: a retrospective series of 49 patients. Leukemia. 2017;31(1):123-129. [DOI] [PubMed] [Google Scholar]
- 57.Ravindran A, Fervenza FC, Smith RJH, Sethi S. C3 glomerulopathy associated with monoclonal Ig is a distinct subtype [published correction appears in Kidney Int. 2018;94(5):1025]. Kidney Int. 2018;94(1):178-186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lloyd IE, Gallan A, Huston HK, et al. C3 glomerulopathy in adults: a distinct patient subset showing frequent association with monoclonal gammopathy and poor renal outcome. Clin Kidney J. 2016;9(6):794-799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zand L, Kattah A, Fervenza FC, et al. C3 glomerulonephritis associated with monoclonal gammopathy: a case series. Am J Kidney Dis. 2013;62(3):506-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sethi S, Sukov WR, Zhang Y, et al. Dense deposit disease associated with monoclonal gammopathy of undetermined significance. Am J Kidney Dis. 2010;56(5):977-982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dispenzieri A. POEMS syndrome: 2017 update on diagnosis, risk stratification, and management. Am J Hematol. 2017;92(8):814-829. [DOI] [PubMed] [Google Scholar]
- 62.Wechalekar AD, Gillmore JD, Hawkins PN. Systemic amyloidosis. Lancet. 2016;387(10038):2641-2654. [DOI] [PubMed] [Google Scholar]
- 63.Pozzi C, D’Amico M, Fogazzi GB, et al. Light chain deposition disease with renal involvement: clinical characteristics and prognostic factors. Am J Kidney Dis. 2003;42(6):1154-1163. [DOI] [PubMed] [Google Scholar]
- 64.Sayed RH, Wechalekar AD, Gilbertson JA, et al. Natural history and outcome of light chain deposition disease. Blood. 2015;126(26):2805-2810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Joly F, Cohen C, Javaugue V, et al. Randall-type monoclonal immunoglobulin deposition disease: novel insights from a nationwide cohort study. Blood. 2019;133(6):576-587. [DOI] [PubMed] [Google Scholar]
- 66.Gupta V, El Ters M, Kashani K, Leung N, Nasr SH. Crystalglobulin-induced nephropathy. J Am Soc Nephrol. 2015;26(3):525-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fish R, Pinney J, Jain P, et al. The incidence of major hemorrhagic complications after renal biopsies in patients with monoclonal gammopathies. Clin J Am Soc Nephrol. 2010;5(11):1977-1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Merlini G, Wechalekar AD, Palladini G. Systemic light chain amyloidosis: an update for treating physicians. Blood. 2013;121(26):5124-5130. [DOI] [PubMed] [Google Scholar]
- 69.Novak L, Cook WJ, Herrera GA, Sanders PW. AL-amyloidosis is underdiagnosed in renal biopsies. Nephrol Dial Transplant. 2004;19(12):3050-3053. [DOI] [PubMed] [Google Scholar]
- 70.Herrera GA, Turbat-Herrera EA. Ultrastructural immunolabeling in the diagnosis of monoclonal light-and heavy-chain-related renal diseases. Ultrastruct Pathol. 2010;34(3):161-173. [DOI] [PubMed] [Google Scholar]
- 71.Nasr SH, Vrana JA, Dasari S, et al. DNAJB9 is a specific immunohistochemical marker marker for fibrillary glomerulonephritis. Kidney Int Rep. 2017;3(1):56-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Alexander MP, Dasari S, Vrana JA, et al. Congophilic fibrillary glomerulonephritis: a case series. Am J Kidney Dis. 2018;72(3):325-336. [DOI] [PubMed] [Google Scholar]
- 73.Nasr SH, Galgano SJ, Markowitz GS, Stokes MB, D’Agati VD. Immunofluorescence on pronase-digested paraffin sections: a valuable salvage technique for renal biopsies. Kidney Int. 2006;70(12):2148-2151. [DOI] [PubMed] [Google Scholar]
- 74.Lachmann HJ, Booth DR, Booth SE, et al. Misdiagnosis of hereditary amyloidosis as AL (primary) amyloidosis. N Engl J Med. 2002;346(23):1786-1791. [DOI] [PubMed] [Google Scholar]
- 75.Gay-Bellile C, Bengoufa D, Houze P, et al. Automated multicapillary electrophoresis for analysis of human serum proteins. Clin Chem. 2003;49(11):1909-1915. [DOI] [PubMed] [Google Scholar]
- 76.Drayson M, Begum G, Basu S, et al. Effects of paraprotein heavy and light chain types and free light chain load on survival in myeloma: an analysis of patients receiving conventional-dose chemotherapy in Medical Research Council UK multiple myeloma trials. Blood. 2006;108(6):2013-2019. [DOI] [PubMed] [Google Scholar]
- 77.Leung N, Gertz M, Kyle RA, et al. Urinary albumin excretion patterns of patients with cast nephropathy and other monoclonal gammopathy-related kidney diseases. Clin J Am Soc Nephrol. 2012;7(12):1964-1968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dispenzieri A, Kyle R, Merlini G, et al. ; International Myeloma Working Group . International Myeloma Working Group guidelines for serum-free light chain analysis in multiple myeloma and related disorders. Leukemia. 2009;23(2):215-224. [DOI] [PubMed] [Google Scholar]
- 79.Hutchison CA, Harding S, Hewins P, et al. Quantitative assessment of serum and urinary polyclonal free light chains in patients with chronic kidney disease. Clin J Am Soc Nephrol. 2008;3(6):1684-1690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Palladini G, Dispenzieri A, Gertz MA, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30(36):4541-4549. [DOI] [PubMed] [Google Scholar]
- 81.Bhutani G, Nasr SH, Said SM, et al. Hematologic characteristics of proliferative glomerulonephritides with nonorganized monoclonal immunoglobulin deposits. Mayo Clin Proc. 2015;90(5):587-596. [DOI] [PubMed] [Google Scholar]
- 82.Barnidge DR, Dasari S, Botz CM, et al. Using mass spectrometry to monitor monoclonal immunoglobulins in patients with a monoclonal gammopathy. J Proteome Res. 2014;13(3):1419-1427. [DOI] [PubMed] [Google Scholar]
- 83.Hoorn EJ, Pisitkun T, Zietse R, et al. Prospects for urinary proteomics: exosomes as a source of urinary biomarkers. Nephrology (Carlton). 2005;10(3):283-290. [DOI] [PubMed] [Google Scholar]
- 84.Ramirez-Alvarado M, Ward CJ, Huang BQ, et al. Differences in immunoglobulin light chain species found in urinary exosomes in light chain amyloidosis (Al). PLoS One. 2012;7(6):e38061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kyle RA, Gertz MA, Greipp PR, et al. A trial of three regimens for primary amyloidosis: colchicine alone, melphalan and prednisone, and melphalan, prednisone, and colchicine. N Engl J Med. 1997;336(17):1202-1207. [DOI] [PubMed] [Google Scholar]
- 86.Venner CP, Lane T, Foard D, et al. Cyclophosphamide, bortezomib, and dexamethasone therapy in AL amyloidosis is associated with high clonal response rates and prolonged progression-free survival. Blood. 2012;119(19):4387-4390. [DOI] [PubMed] [Google Scholar]
- 87.Merlini G. AL amyloidosis: from molecular mechanisms to targeted therapies. Hematology Am Soc Hematol Educ Program. 2017;2017:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Pinney JH, Lachmann HJ, Bansi L, et al. Outcome in renal Al amyloidosis after chemotherapy. J Clin Oncol. 2011;29(6):674-681. [DOI] [PubMed] [Google Scholar]
- 89.Kourelis TV, Nasr SH, Dispenzieri A, et al. Outcomes of patients with renal monoclonal immunoglobulin deposition disease. Am J Hematol. 2016;91(11):1123-1128. [DOI] [PubMed] [Google Scholar]
- 90.Fermand JP, Bridoux F, Kyle RA, et al. ; International Kidney and Monoclonal Gammopathy Research Group . How I treat monoclonal gammopathy of renal significance (MGRS). Blood. 2013;122(22):3583-3590. [DOI] [PubMed] [Google Scholar]
- 91.Nasr SH, Satoskar A, Markowitz GS, et al. Proliferative glomerulonephritis with monoclonal IgG deposits. J Am Soc Nephrol. 2009;20(9):2055-2064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Gumber R, Cohen JB, Palmer MB, et al. A clone-directed approach may improve diagnosis and treatment of proliferative glomerulonephritis with monoclonal immunoglobulin deposits. Kidney Int. 2018;94(1):199-205. [DOI] [PubMed] [Google Scholar]
- 93.Mallett A, Tang W, Hart G, et al. end-stage kidney disease due to fibrillary glomerulonephritis and immunotactoid glomerulopathy - outcomes in 66 consecutive ANZDATA Registry cases. Am J Nephrol. 2015;42(3):177-184. [DOI] [PubMed] [Google Scholar]
- 94.Heilman RL, Velosa JA, Holley KE, Offord KP, Kyle RA. Long-term follow-up and response to chemotherapy in patients with light-chain deposition disease. Am J Kidney Dis. 1992;20(1):34-41. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.