Abstract
Study Design:
Systematic review (Level 4)
Objective:
To summarize the demographics, clinical presentations, and conditions associated with butterfly vertebrae.
Methods:
A systematic search was performed of multiple databases. A total of 279 articles were identified for screening. Case series or case reports of butterfly vertebrae with adequate clinical detail were complied.
Results:
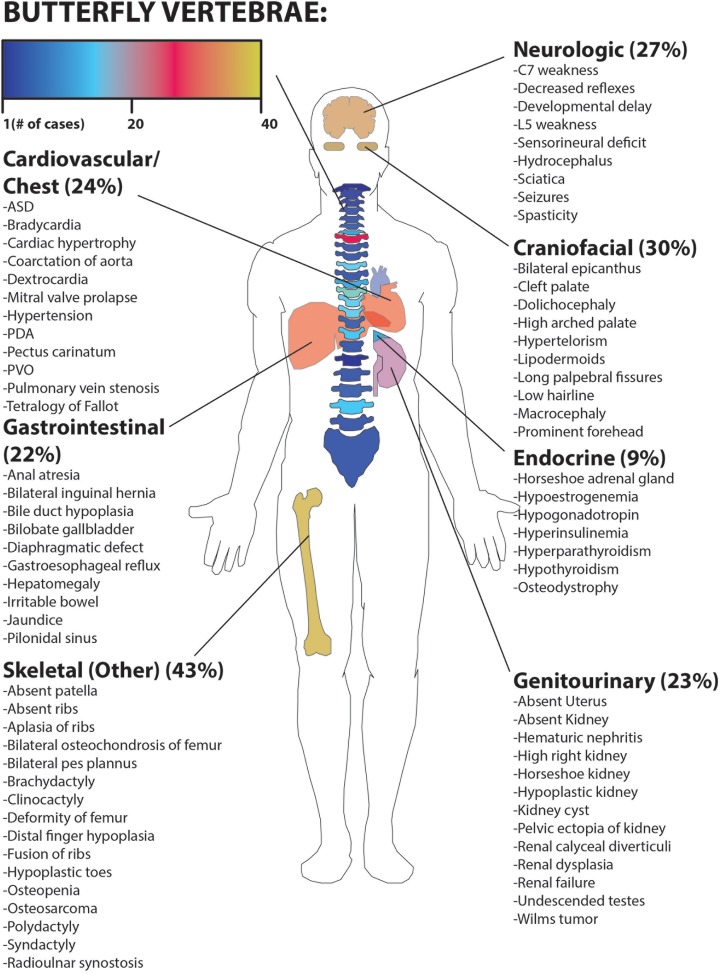
Eighty-two total articles (109 patients) were selected for final inclusion. Sixty-one percent of patients presented with a single butterfly vertebra, while 39% were multiple. The most common location for butterfly vertebrae was T1. Fifty-six percent of cases were associated with a syndrome, the most common being spondylocostal dysostosis. The presence of multiple butterfly vertebra was strongly associated with a syndrome or additional anomalies (P < .001). Overall, the most common presenting complaint was low back pain. Seventy percent of patients had associated spinal disease. Other organ systems affected included musculoskeletal (43%), craniofacial (30%), neurologic (27%), cardiovascular (24%), genitourinary (23%), gastrointestinal (22%), laboratory abnormality (16%), and endocrine (9%).
Conclusions:
This study is the largest collection of butterfly vertebrae cases to date. Butterfly vertebrae are associated with spinal deformity and multiple butterfly vertebrae may indicate a syndromic illness. Low back pain or disc herniation may occur with lumbar butterfly vertebrae however the etiology of this phenomena has not been rigorously explained. Many diseases and syndromes are associated with butterfly vertebrae.
Keywords: butterfly vertebrae, anterior rachischisis, sagittal cleft vertebrae, congenital spine, spinal malformation, Klippel-Feil syndrome, Alagille syndrome, spondylocostal dysostosis
Introduction
A butterfly vertebra (sagittal cleft vertebra or anterior rachischisis) is a sagittal defect in the vertebral body caused by failure of fusion of the 2 lateral chondrification centers during embryogenesis.1,2 The name is based on the appearance of the 2 hemivertebrae emerging as butterfly wings from the central cleft on x-ray.3 This malformation has been reported to be exceptionally rare in the literature.1,3-9
Several sources cite the association between butterfly vertebrae and congenital diseases such as Alagille syndrome, Jarcho-Levin syndrome, Crouzon syndrome, and Pfeiffer’s syndrome.9,10 Reports have also associated butterfly vertebrae with low back pain.1,7,9,11 Because of their rarity, they can easily be misclassified as other pathologic processes.12,13 The true incidence, as well as the full spectrum of related conditions, are unknown as many are only picked up incidentally.
The largest previous series of butterfly vertebrae was published by Cave3 in 1957, in which he reviewed 33 cases in the literature. However, detailed clinical data from these cases was not reported.3 Later, Kapetanakis et al11 reviewed the literature and reported on 11 cases published between 1990 and 2015. To our knowledge, a comprehensive analysis of all butterfly vertebrae cases has not been performed. The goal of this study was to assimilate all reports of butterfly vertebrae in the literature to formulate a review and glean new information about this rare malformation. We were specifically interested in the rate of associated abnormalities in other organ systems occurring through concurrent syndromes. Furthermore, we wished to determine the implications, if any, of discovering incidental butterfly vertebrae with regard to clinical workup.
Materials and Methods
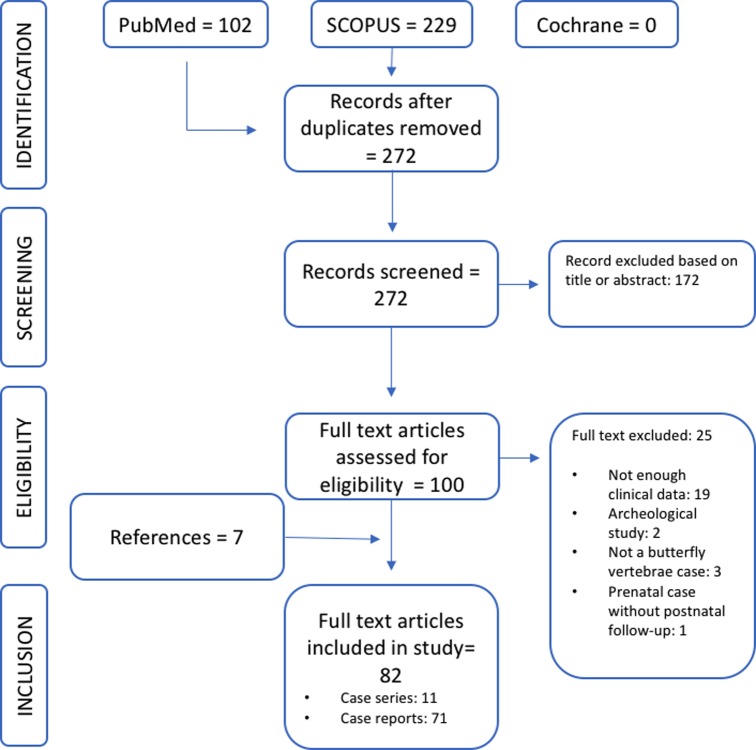
A systematic review was prepared according to the protocol set forth by the Cochrane Collaboration and Wright et al and reported according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines (Figure 1).14-16 In November 2017, an electronic search was performed on the Scopus and PubMed databases, as well as the Cochrane Library, to identify studies containing the following terms: “butterfly vertebrae,” or its common synonyms “sagittal cleft vertebrae” and “anterior rachischisis.” Two independent reviewers screened titles and abstracts from which full-length texts were selected. References contained in the selected texts were also reviewed for possible sources. Furthermore, major journals were hand-searched for recent publications that might not have been included in the initial search.
Figure 1.
Study selection based on PRISMA (Preferred Reporting for Systematic Reviews and Meta-Analyses) guidelines.
Studies that contained individual or case series of patients having single or multiple butterfly vertebrae, either in isolation or part of a constellation of anomalies, were included if they contained the following clinical details: age (at final exam or follow up), sex, location, and number of butterfly vertebrae. Several studies with relevant clinical data that were missing a single part of the above information were included in our analysis only for those data sets to which they were applicable.
Articles were excluded if they did not involve butterfly vertebrae, did not present discrete cases of butterfly vertebrae, pertained primarily to archeological studies or veterinary studies, involved prenatal patients without postnatal follow up, were in languages not translatable by the researchers, or the article could not be located despite exhaustive archive review (typically due to age of the article). Studies were also excluded if they lacked sufficient clinical data to be included for analysis (greater than 2 of the above inclusion points).
Following the selection of articles, clinical cases were aggregated for analysis,17 and the following variables were considered for extraction: age, sex, location of butterfly vertebrae in the spine, number of butterfly vertebrae, presenting complaint, concomitant syndrome or systemic illness, other spinal abnormality excluding butterfly vertebrae, abnormal laboratory findings, and finally abnormalities of the genitourinary, cardiac, endocrine, neurologic, craniofacial, or musculoskeletal systems. Systems abnormalities were collected and sorted into these groups based on the valid positive associated findings as reported by the authors of the case. A patient was considered to have “a normal system” if it was not specifically identified in the article. For simplicity, we use the term “syndrome” to indicate any syndrome, sequence, association, or other condition affecting multiple organ systems.
Article quality was appraised based on complete review of the imaging and clinical information presented in the text. A bias review was deemed unnecessary as these studies were case reports and case series.
Statistics
Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software (version 24.0, IBM Corp, Armonk, NY, USA). The chi-square test was used to test the association between multiple versus single butterfly vertebrae and the presence or absence of a syndrome or other systemic illness.
Results
The Scopus search yielded 229 citations while PubMed yielded 102, for a total of 331 articles. A search of the Cochrane library yielded 0 results. After duplicates were removed there were 272 citations in total. From these 172 citations were excluded based on analysis of the abstract or title for the following reasons: was not a case of butterfly vertebrae (125 citations), the article was not available (15 citations), was a prenatal article (14 citations), was an archeological study (10 citations), was a veterinary study (7 articles), or could not be translated (1 citation). 100 articles were included for full review from this group with an additional 7 added based on review of references (107 articles). From this group, another 25 articles were excluded for the following reasons: not enough clinical data (19 articles), was not a case of butterfly vertebrae (3 articles), was an archeological study (2 articles), was a prenatal case without postnatal follow-up (1 article). After careful review of abstracts and full articles, a total of 82 articles (109 cases of butterfly vertebrae) were included for final review (Figure 1). Of the 109 cases included, 11 were categorized as lacking a single data point, and thus grouped separately (5 cases lacked specific vertebral location of the butterfly vertebrae, 6 lacked the sex of the patient) (Table 1). Therefore, these cases were not included in the calculation of average sex and location of butterfly vertebrae.
Table 1.
List of Included Cases.
| Author | Year | Age (Years) | Sex | Single or Multiple | Location | Syndrome | Spine | GU | Cardiac | GI | Endo | Neuro | Lab | MSK | CF |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Frederick | 1945 | 38 | M | Single | L3 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Frederick | 1945 | 23 | M | Single | T7 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Franciosi | 1951 | 28 | M | Multiple | L3, L4 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Cave | 1957 | 32 | F | Single | T7 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Lagarde | 1960 | 20 | F | Multiple | L3, L4 | None | (+) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Lagarde | 1960 | 26 | F | Single | T12 | None | (+) | (–) | (+) | (–) | (–) | (–) | (–) | (–) | (–) |
| Schwartz | 1960 | 28 | M | Single | T7 | Calyceal diverticuli | (–) | (+) | (+) | (–) | (–) | (–) | (+) | (+) | (–) |
| Schwartz | 1960 | 18 | M | Single | T11 | Calyceal diverticuli | (–) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Colquhoun | 1968 | 12 | F | Single | T9 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Colquhoun | 1968 | 46 | M | Single | T7 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Colquhoun | 1968 | 56 | F | Single | T11 | None | (+) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Colquhoun | 1968 | 46 | F | Single | T11 | None | (+) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Tamagawa | 1972 | 25 | F | Single | T7 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Mitchell | 1981 | 0.42 | F | Multiple | T8 | 4q21 Interstitial deletion | (+) | (–) | (+) | (+) | (–) | (+) | (+) | (+) | (+) |
| De Graaf | 1982 | 39 | M | Single | L5 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Dastur | 1985 | 13 | M | Single | L2 | Goldenhar | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (+) |
| Garcia-Cruz | 1985 | 16 | M | Multiple | T2-T9 | 20p12.2 deletion | (+) | (–) | (+) | (–) | (+) | (+) | (–) | (+) | (+) |
| Schlitt | 1989 | 42 | F | Single | C4 | Klippel-Feil | (+) | (–) | (+) | (–) | (+) | (+) | (+) | (–) | (–) |
| Rose | 1991 | 0.13 | M | Multiple | T4, T6 | Deletion of 4(q21q25) | (–) | (+) | (+) | (–) | (–) | (+) | (–) | (+) | (+) |
| Mahajan | 1992 | 24 | F | Single | T11 | Mullerian agenesis | (+) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Garcia | 1993 | 58 | F | Single | T11 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Garcia | 1993 | 61 | F | Single | T11 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| McCall | 1994 | 7.67 | M | Multiple | Not reported | Jarcho-Levin, spondylocostal dysostosis | (+) | (–) | (+) | (+) | (–) | (–) | (–) | (+) | (+) |
| Maillefert | 1995 | 34 | M | Multiple | T8, T10 | Alagille | (–) | (–) | (–) | (+) | (–) | (–) | (+) | (–) | (+) |
| Delgado | 1996 | 41 | M | Single | L3 | None | (+) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Herman | 1996 | 0.06 | F | Single | T7 | I-cell disease (neonatal type II mucolipidosis) | (–) | (–) | (–) | (–) | (+) | (–) | (+) | (+) | (–) |
| Funke | 2001 | 31 | M | Single | T8 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Sonel | 2001 | 37 | M | Single | L3 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Brasili | 2002 | 36 | F | Multiple | L5, S1 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Przkora | 2002 | 14 | F | Multiple | T1, T4, T7, T8, T10, T11, L3 | Alagille | (+) | (–) | (+) | (+) | (+) | (–) | (–) | (+) | (–) |
| Chan | 2003 | 1.15 | M | Multiple | T1-T5 | Klippel-Feil | (+) | (+) | (–) | (–) | (–) | (+) | (–) | (+) | (–) |
| Ryan | 2003 | 39 | F | Multiple | T6, T8 | Alagille | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Anderson | 2003 | 7 | N/A | Single | C3 | Pfeiffer’s | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Rahimi-Movaghar | 2004 | 15 | M | Multiple | T2-T6 | Klippel-Feil | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (+) | (+) |
| Satpathy | 2004 | 13 | F | Single | L1 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Dejardin | 2004 | 6 | F | Single | Lumbar, not specified | None | (–) | (+) | (+) | (–) | (–) | (+) | (–) | (–) | (+) |
| Anderson | 2005 | 0.17 | M | Single | C6 | Goldenhar | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (+) |
| Anderson | 2005 | 8 | M | Single | T4 | Goldenhar | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (+) |
| Anderson | 2005 | 1 | M | Single | C4 | Goldenhar | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (+) |
| Vázquez-López | 2005 | 0.65 | F | Multiple | T3-T5, L3 | Jarcho-Levin, spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Ahn | 2005 | 12 | F | Multiple | Multiple, thoracic not specified | Delta phalanges plus | (+) | (–) | (+) | (–) | (–) | (+) | (–) | (+) | (+) |
| Atar | 2006 | 2 | M | Single | T9 | Kabuki | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (+) |
| Takikawa | 2006 | 4 | M | Multiple | C6, C7 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 2 | F | Multiple | C6, C7 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 4 | F | Multiple | L5, S1 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 3 | M | Multiple | L5, S1-S3 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 5.5 | M | Multiple | C6, C7, T1-T3, L4, L5, S1, S2 | Spondylocostal dysostosis | (+) | (–) | (–) | (+) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 0.17 | F | Single | T11 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (+) |
| Takikawa | 2006 | 6.5 | F | Multiple | C6, C7 | Spondylocostal dysostosis | (+) | (–) | (+) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 18 | F | Multiple | C6, C7 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (+) |
| Takikawa | 2006 | 18 | F | Multiple | C5, C7 | Spondylocostal dysostosis | (+) | (+) | (+) | (–) | (–) | (+) | (–) | (+) | (–) |
| Takikawa | 2006 | 17 | F | Multiple | C5, C7, T4 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 13 | F | Multiple | T6-T8 | Spondylocostal dysostosis | (+) | (–) | (–) | (+) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 0.75 | M | Multiple | C6, C7, L2, S1, S2 | Spondylocostal dysostosis | (+) | (–) | (–) | (+) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 5 | M | Multiple | C5, C6, L2 C7, S1, S2 | Spondylocostal dysostosis | (+) | (+) | (–) | (+) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 3 | M | Multiple | C6, C7 | Spondylocostal dysostosis | (+) | (+) | (+) | (+) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 2 | M | Multiple | T6, T9, T10, T12 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 9.5 | M | Multiple | T4, T5 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Takikawa | 2006 | 2 | F | Multiple | T7, T9 | Spondylocostal dysostosis | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Zeglam | 2006 | 2.5 | F | Single | T12 | None | (+) | (–) | (+) | (–) | (–) | (+) | (–) | (+) | (–) |
| Zeglam | 2006 | 54 | M | Single | L4 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Pasku | 2007 | 25 | F | Single | C2 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Rossi | 2007 | 7 | F | Single | T8 | Lathosterolosis | (–) | (+) | (–) | (+) | (–) | (+) | (+) | (+) | (+) |
| Robert | 2007 | 5 | M | Multiple | Nonspecific thoracic and lumbar | Alagille | (–) | (+) | (+) | (+) | (+) | (+) | (+) | (+) | (+) |
| Küpeli | 2008 | 0.17 | F | Multiple | T3, T8 | Wilms’ tumor | (+) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Patinharayil | 2008 | 46 | F | Single | T6 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Wang | 2008 | 2 | N/A | Single | T6 | Alagille | (–) | (+) | (+) | (+) | (–) | (–) | (+) | (–) | (+) |
| Wang | 2008 | 5 | N/A | Multiple | T3, T4 | Alagille | (–) | (–) | (+) | (+) | (–) | (–) | (+) | (–) | (+) |
| Wang | 2008 | 3 | N/A | Multiple | T4,T6-T10 | Alagille | (–) | (–) | (+) | (+) | (–) | (–) | (+) | (–) | (+) |
| Wang | 2008 | 4 | N/A | Multiple | T4, T7, T9 | Alagille | (–) | (–) | (–) | (+) | (–) | (–) | (+) | (–) | (+) |
| Wang | 2008 | 2 | N/A | Multiple | T4-T9 | Alagille | (–) | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (+) |
| Ekim | 2010 | 32 | M | Single | L2 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Qian | 2010 | 26 | M | Single | L4 | Ankylosing spondylitis | (+) | (–) | (–) | (–) | (–) | (–) | (+) | (–) | (–) |
| Qian | 2010 | 40 | M | Single | L5 | Ankylosing spondylitis | (+) | (–) | (–) | (–) | (–) | (–) | (+) | (–) | (–) |
| Tuncel | 2010 | 27 | M | Single | L2 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Boulet | 2011 | 35 | M | Single | S1 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Cho | 2011 | 56 | F | Single | L4 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Choi | 2011 | 46 | M | Single | C1 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Choi | 2011 | 5 | M | Single | C4 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Cui | 2011 | 13 | F | Single | L6 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Massobrio | 2011 | 5 | M | Multiple | T7-T11 | Alagille | (–) | (–) | (–) | (+) | (–) | (–) | (–) | (+) | (+) |
| Jarzabek | 2012 | 24 | F | Multiple | T9-T11 | Kallman | (+) | (–) | (–) | (–) | (+) | (+) | (–) | (+) | (+) |
| Jarzabek | 2012 | 28 | M | Single | L2 | Kallman | (+) | (+) | (–) | (–) | (–) | (+) | (–) | (–) | (+) |
| Kilgore | 2012 | 33 | M | Single | T8 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Zarate | 2012 | 0.75 | F | N/A | N/A | Kabuki | (–) | (+) | (+) | (+) | (+) | (+) | (+) | (+) | (+) |
| Ditkofsky | 2013 | 51 | F | Single | T9 | None | (+) | (–) | (–) | (+) | (+) | (+) | (–) | (+) | (–) |
| Zuo | 2013 | 24 | F | Single | L4 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Patra | 2013 | 10 | F | Single | C2 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Aygün | 2014 | 0.06 | M | Single | T8 | Fryns | (–) | (+) | (+) | (+) | (–) | (–) | (–) | (+) | (+) |
| Canitez | 2014 | 0.33 | F | Single | T7 | Lung agenesis | (–) | (+) | (–) | (–) | (–) | (–) | (–) | (+) | (+) |
| Ekiz | 2014 | 40 | M | Single | L4 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Frost | 2014 | 54 | M | Single | T8 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Sandal | 2014 | 0.67 | M | Multiple | T9, T11 | VACTERL | (–) | (+) | (+) | (+) | (–) | (–) | (–) | (+) | (–) |
| Youssef | 2014 | 0.5 | M | Single | T12 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Cheng | 2015 | 50 | F | Multiple | T10, L2, L4 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Diehl | 2015 | 3 | F | Multiple | T5, T7 | Micro duplication of 22q11.21 | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (+) | (–) |
| Hawkes | 2015 | 1 | F | Multiple | T9, T10 | Myhre | (+) | (–) | (+) | (–) | (–) | (+) | (–) | (+) | (+) |
| Hopkins | 2015 | 21 | M | Single | L4 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Karargyris | 2015 | 40 | F | Single | L4 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Ozaras | 2015 | 38 | M | Multiple | T9, L3 | Behçet’s disease | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Sifuentes | 2015 | 62 | F | Single | T10 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Esen | 2016 | 5.5 | F | Single | T12 | None | (–) | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Esen | 2016 | 56 | M | Single | L4 | None | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Guo | 2016 | 4 | M | Single | T1 | None | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Kapetanakis | 2016 | 40 | F | Single | S1 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (–) |
| Karaca | 2016 | 42 | F | Single | T1 | Klippel-Feil | (+) | (–) | (–) | (–) | (–) | (–) | (–) | (–) | (–) |
| Slouma | 2016 | 55 | F | Multiple | T9-T12, L3 | None | (–) | (–) | (–) | (+) | (–) | (–) | (–) | (–) | (–) |
| Deepak | 2017 | 14 | M | Single | C3 | None | (+) | (–) | (–) | (–) | (–) | (+) | (–) | (–) | (+) |
| Hannoush | 2017 | 1 | M | Multiple | T4, T6, T8 | Alagille | (–) | (+) | (+) | (+) | (–) | (–) | (+) | (–) | (+) |
Abbreviations: M, male; F, female; GU, genitourinary; Cardiac, cardiovascular/chest; GI, gastrointestinal; Endo, endocrine; Neuro, neurologic; Lab, laboratory values; MSK, musculoskeletal/other; CF, craniofacial; N/A, not available; VACTERL, vertebral defects, anal atresia, cardiac defects, tracheoesophageal fistula, renal anomalies, and limb abnormalities.
Clinical Characteristics
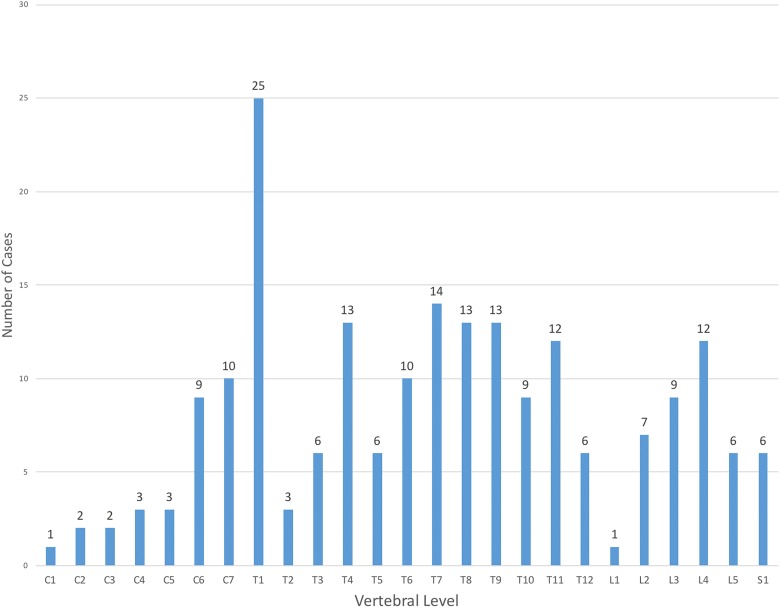
The average age of patients in this group was 20.5 years. Fifty-one of 103 cases were female (50%). Sixty-three cases were single vertebrae (61%), while 41 of 104 cases were multiple (39%). The most common location was T1 (25 cases), followed by T7 (14 cases) (Figure 2).
Figure 2.
Prevalence of butterfly vertebrae at vertebral levels.
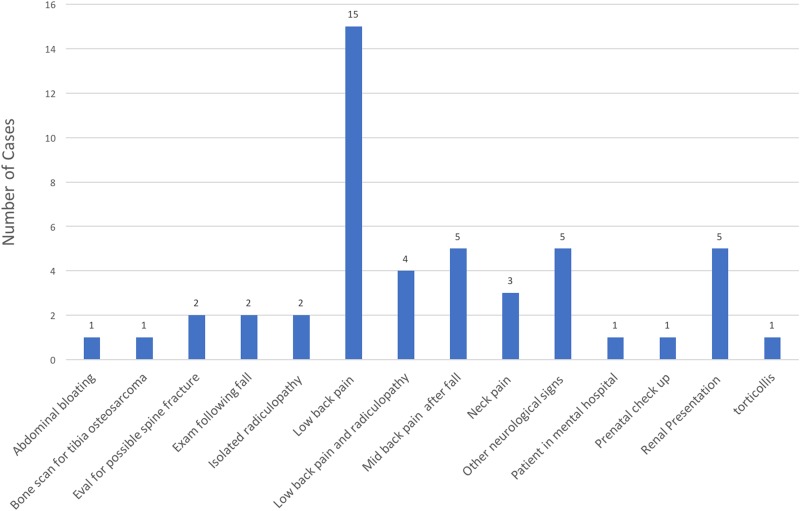
The most common presenting complaint was low back pain (23%, 25/109 cases), followed by neck pain (0.05%, 5/109) and jaundice (0.05%, 5/109). When examining only nonsyndromic cases, low back pain was still the most common presenting complaint (30%, 14/48 patients), followed by mid back pain (10%, 5/48 patients). Of note 5/48 cases (10%) were reports of butterfly vertebrae being mistaken for either fracture or tumor. See Figure 3 for most common presenting complaints.
Figure 3.
Most common presenting complaints in nonsyndromic cases.
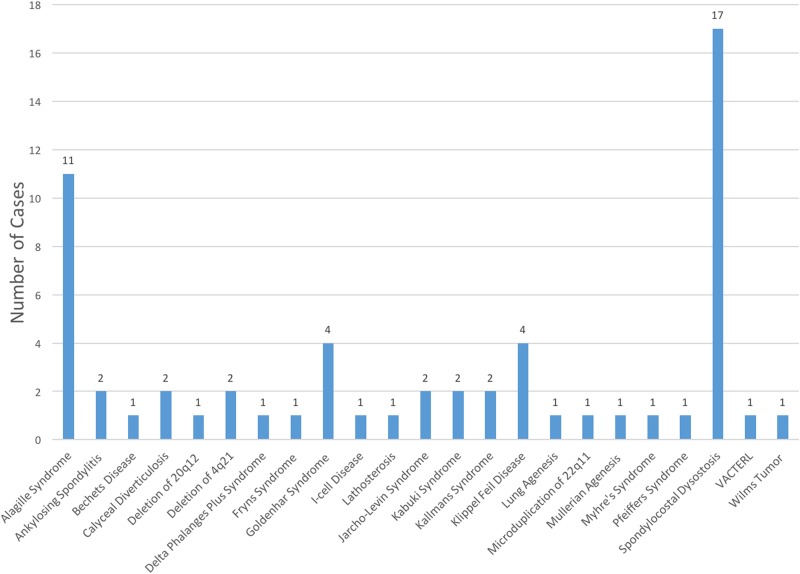
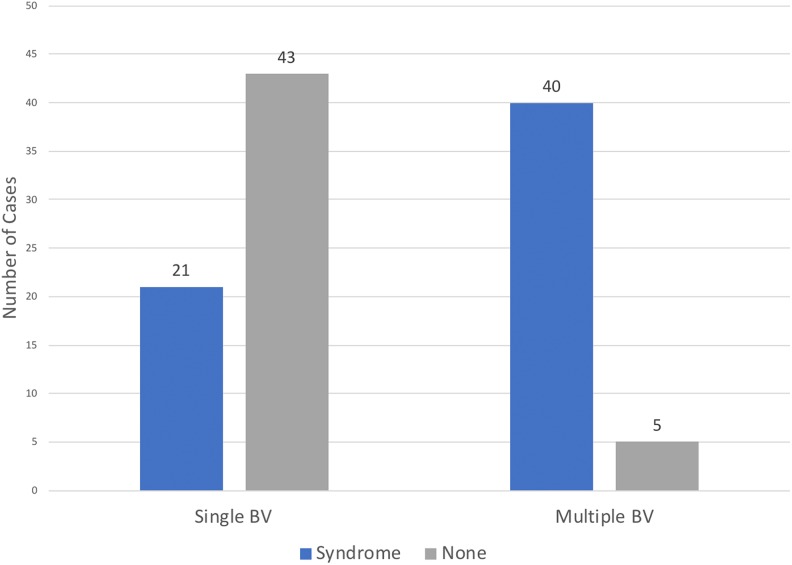
Of the 109 cases, 48 patients did not have an associated syndrome (44%), while 61 patients did have an associated syndrome (56%). The most common of these syndromes was spondylocostal dysostosis with 17 cases (28%) followed by Alagille syndrome with 11 cases (18%) (Figure 4). The presence of multiple butterfly vertebrae (>1) was associated with the presence of a syndrome (40/45 cases, 90%), while single butterfly vertebrae were more likely to occur alone (43/64 cases, 67%): χ2(1, n = 108) = 34.7, P < .001, ϕ coefficient = −0.57 (Figure 5).
Figure 4.
Summary of all syndromes that were associated with butterfly vertebrae.
Figure 5.
Breakdown of occurrences of single and multiple butterfly vertebrae either in isolation or as part of a syndrome. Multiple butterfly vertebrae were associated with the presence of a syndrome: (P < .001).
Associated Conditions
The most common associated organ system affected was “Other spinal deformity or disease,” which included any structural abnormality of the spine outside the butterfly vertebrae. There were 76 of 109 patients affected in this category (70%) with scoliosis as the most common finding. Other findings included failure of formation and segmentation, block vertebrae, kyphosis, spina bifida, disc herniation, spondylolisthesis, vertebral body abnormality, syringomyelia, and myelomeningocele. There was no significant association between “other spinal deformity” and the presence of single or multiple butterfly vertebrae: χ2(1, n = 108) = 0.11, P = .96, ϕ = −0.01.
The next most common associated organ system affected was “Other skeletal deformity or disease” with 46 of 109 patients affected (43%). The most common finding was rib fusion or abnormality. Other abnormalities included short stature, clinodactyly, syndactyly, polydactyly, brachydactyly, thumb hypoplasia, short dysplastic femurs, and radioulnar synostosis.
Craniofacial dysmorphism was present in 32 of 109 cases (30%) and all were associated with a syndrome of some type. Issues varied by syndrome, but included things such as mandibular malformation, cleft palate, and hypertelorism.
A neurologic abnormality was present in 30 of 109 cases (27%)—the most common findings being weakness, sensory loss, and spasticity. Other rarer findings included cerebral atrophy, occipital meningocele, bowel and bladder difficulty, seizures, and developmental delay.
The cardiovascular system was affected in 25 of 109 cases (24%), the most common finding being pulmonary vein stenosis. Other cardiac abnormalities included patent ductus arteriosis, patent foramen ovale, coarctation of the aorta, mitral valve prolapse, dextrocardia, and cardiac hypertrophy.
The genitourinary system was affected in 25 of 109 cases (23%), with undescended testes being the most common finding, followed by a horseshoe kidney. Other common findings in this area were renal calculi, renal failure, absent, dysplastic, or hypoplastic kidneys.
The gastrointestinal system was involved in 24 of 109 cases (22%), the most common findings being biliary atresia/hypoplasia and jaundice; both of which are common findings in Alagille syndrome. Other findings included diaphragm defects, hepatomegaly, inguinal hernia, and anal atresia.
Laboratory values were abnormal in 17 of 109 of cases (16%), the most common abnormality being increased bilirubin and liver enzymes; again, related to Alagille syndrome.
Finally, the endocrine system was involved in 10 of 109 cases (9%), with thyroid abnormalities being the most common finding. A complete overview of associated conditions can be found in Figure 6.
Figure 6.
Summary of associated organ systems affected and specific problems.
Discussion
Butterfly vertebrae were first described in a 55-year-old man in 1850 by Rokitansky.5 The oldest case ever reported was in an archeological specimen in Sharuna, Egypt in the L3 vertebrae dated to 2150 bc.18 Since this time there have been many articles on butterfly vertebrae, mostly as incidental reports. We performed this study to synthesize all information available regarding this rare malformation, and to summarize its associations. This study represents the largest collection of butterfly vertebrae to date.
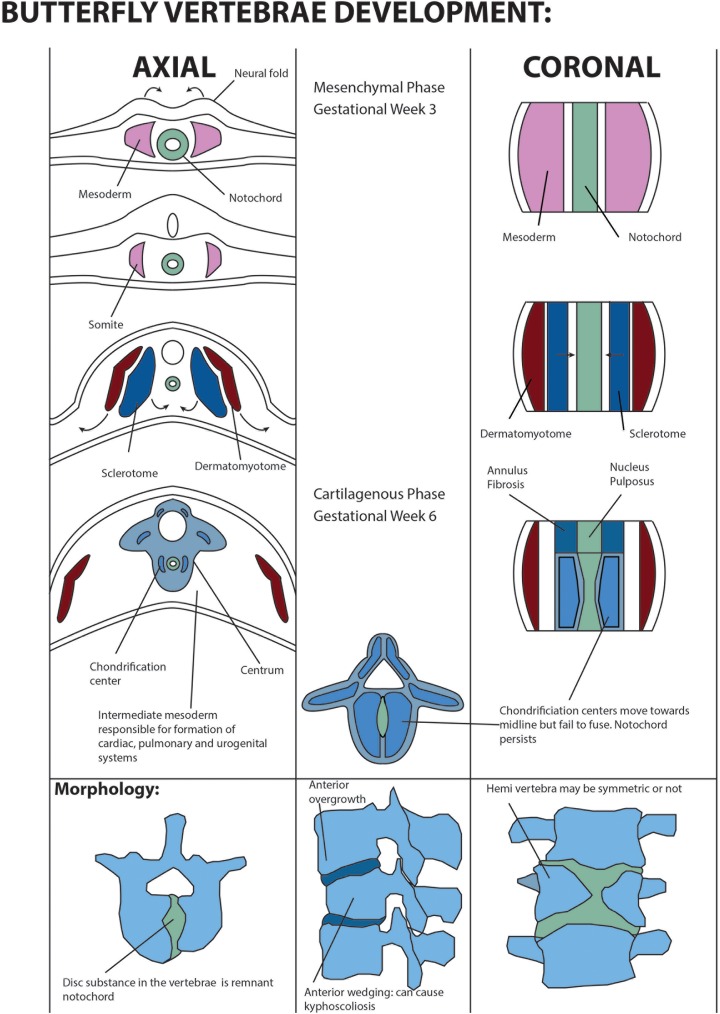
Butterfly vertebrae occur as an aberration in the normal embryological development of the vertebral body. Ordinarily, the first stage of development of the spine is neurulation with the formation of the notochord at day 7 during gastrulation.19 This is followed by the migration of endodermal cells and formation of the lateral mesoderm. Somatization of the mesoderm proceeds with the formation of 44 pairs of somites—blocks of tissue on either side of the neural tube.20 The mesoderm is also responsible for the formation of cardiac, pulmonary, and renal tissue—hence the high association of vertebral anomalies with disturbances of other major organ systems.19 In this study, the associated abnormalities in the cardiac, neurological, genitourinary systems were 30%, 27%, 23% respectively. Somites then differentiate into sclerotomes, which progress to form the spine and other aspects of the skeleton, while dermomyotomes form muscle. The close association between the development of the spine and the appendicular skeleton explains the high rate of butterfly vertebrae occurring with other skeletal defects. In this study, we noted that 43% of patients with a butterfly vertebra had another associated musculoskeletal abnormality. The sclerotomes then flank the notochord in the fourth week.20 Two anterior sclerotomes undergo chondrification and fuse to become the cartilage vertebral body at week 6 while the third part becomes the posterior arch.21 The notochord is obliterated at the level of the vertebral body but persists at the disc level to become the nucleus pulposus.8,19 Ossification typically beings around week 12.
Spinal malformations occur generally under the headings of failure of formation, failure of segmentation, and neural tube defects.19 Butterfly vertebrae have been postulated to develop secondary to failure of formation. One theory is that during somatogenesis, the two lateral chondral centers simultaneously fail to fuse secondary to persistence of the notochord.2,8,22-24 (Figure 7). Hemivertebrae form through a similar process where a single chondrification center fails to migrate medially, and thus butterfly vertebrae can be thought of as adjacent hemivertebrae.2,19
Figure 7.
Development and morphology of butterfly vertebrae. Axial: development of the embryonic spine. Following formation of the notochord, the lateral mesoderm differentiates into somites, which form the dermatomyotome and the sclerotome. The sclerotome undergoes chondrification to form the vertebral body. Coronal: shows differentiation of the mesoderm into the dermatomyotome and the sclerotome. The notochord forms the nucleus pulposus.
The geometry of butterfly vertebra is variable but tends to be deficient anteriorly, causing a wedge shape and focal kyphosis.25 The 2 halves are typically equal but can be asymmetric, with an intact posterior arch and pedicles.5,26 In some cases, they may be connected by an isthmus of bone.5 They are typically cold on bone scintigraphy.27 This structural abnormality has been proposed to alter the biomechanics of the spine and result in disc herniation (Figure 7).1,8,10 In this study, structural abnormality of the spine was the most common associated condition (70%), with scoliosis being the most common finding. Other common findings were other failure of formation and segmentation.
The thoracolumbar spine has been implicated as the most common location for the formation of butterfly vertebrae.2,6,9 McMaster et al26 noted in their large series of 15 single butterfly vertebrae that the most common location was T11 at the thoracolumbar region.26 This is in contrast to our findings, which showed T1 as the most common location. However, this finding was likely due to the high number of patients with spondylocostal dysostosis included in this report, which presents with upper thoracic and cervical abnormalities.
It is important to understand the radiographic features of butterfly vertebrae (see Figure 8 for a case example) to distinguish them from other pathological processes (fracture, metastasis infection, syringomyelia, and Charcot’s disease).3,25 In this series, 10% of nonsyndromic patients were misdiagnosed as having a compression fracture. Close examination of the adjacent vertebrae will show features of long-standing deformity such as exaggerated elongation anterior margins to occupy the defect, and a normal intervertebral disc.25 In addition, butterfly vertebrae typically cause less kyphosis than would be expected from the significant anterior wedging (Figure 7).3
Figure 8.

Multiplpanar reformatted computed tomographic image of a S1 butterfly vertebrae with associated sacral dysmorphism and pseudoarticulation on the left.
Multiple previous reports have linked butterfly vertebrae with low back pain,1,7,9,11 the treatment of which is generally conservative. In this series, low back pain was the most common presenting complaint occurring in 23% of all cases and 30% of nonsyndromic cases. Nonetheless, it must be noted that the association between butterfly vertebrae and low back pain remains unproven as low back pain is a common presenting complaint in the spine patient population. The etiology of low back pain in a patient with butterfly vertebrae may be unrelated to the structural abnormality and thus requires further research. However, the treatment of low back pain in most instances was generally conservative, with one case report of progressive kyphosis which required instrumentation.26 Butterfly vertebrae may also be associated with symptomatic disc herniation, which requires decompression.4,8,11
Based on our findings, evaluation of the other organ systems should be performed in the presence of a butterfly vertebra, especially if they are multiple. In this study, there was a high association between the presence of multiple butterfly vertebrae and a syndromic presentation. 89% of cases which had >1 butterfly vertebrae were associated with the presence of a syndrome. However, a significant number of single butterfly vertebrae cases also presented as part of a syndrome (32% of cases). Specific evaluation of the cardiac and genitourinary systems with ultrasound would be a practical and noninvasive modality to evaluate for any other malformations. Although there was a high incidence of neurologic abnormality in these cases, the description of these findings were reported based on symptoms as opposed to structural problems, and perhaps were unrelated directly to the butterfly vertebrae. Thus, the neurological system lacked a clear and cohesive group of associated findings due to lack of detailed information provided in the reports. Genetic testing should be considered in butterfly vertebrae patients who also have other skeletal or organ malformations. In this series, butterfly vertebrae were found to be associated with numerous syndromes surpassing those commonly cited in the literature (Table 2).
Table 2.
Syndromes Associated With Butterfly Vertebrae.
| Syndrome | Description |
|---|---|
| Alagille syndrome | An autosomal dominant disease characterized by a lack of the interlobular bile ducts, facial dysmorphism, pulmonary stenosis, posterior embryotoxon, and butterfly vertebrae (also known as arteriohepatic dysplasia).28 It may be asymptomatic and should be suspected in cases of butterfly vertebrae.28 In a case series of 92 patients with Alagille syndrome, butterfly vertebrae were present in 51% of patients.29 |
| Ankylosing spondylitis | A chronic inflammatory arthritis typically affecting the sacroiliac joints.30 |
| Behçet’s disease | A systemic vasculitis associated with oral and genital ulcers as well as arthritis.31,32 |
| Crouzon syndrome | A craniosynostosis syndrome associated with ocular proptosis and shallow orbits, as well as butterfly vertebrae. Anderson et al33 published the largest series reporting the spinal findings for this syndrome. In this series, 5 of 44 had evidence of cervical butterfly vertebrae.33 These results were not included in our current study as there was not enough patient data resolution to combine it with other cases. |
| Fryns syndrome | An autosomal recessive condition consisting of congenital diaphragmatic defect, abnormal facies, small thorax with widely spaced nipples, limb hypoplasia, hernia, and pulmonary hypoplasia.34 |
| Goldenhar syndrome | A sporadic genetic disease that consists of a spectrum of auriculovertebral malformations including eye, ear, and vertebral anomalies. It is hypothesized to result from embryological disturbance of the ectoderm.35 |
| Lathosterolosis | A defect in cholesterol synthesis that presents with multiple malformations, mental retardation, and liver pathology.36 |
| Jarcho-Levin syndrome/spondylocostal dysostosis | A spectrum of congenital malformations of the ribs and vertebrae with associated short stature.37-39 |
| Kabuki syndrome | A condition of unknown etiology with facial malformations that mimic the makeup worn in the Japanese Kabuki theater, mental retardation, and abnormal dentition.40 |
| Kallman syndrome | A mutation in the FGFR-1 gene characterized by hypogonadotropic hypogonadism and anosmia.41 |
| Klippel-Feil syndrome | Congenital cervical synostosis of 2 or more vertebrae resulting from a mutation of the SGM1 gene causing fusion of cervical vertebrae. Clinical signs include low hairline, short neck, and limited range of motion of neck.42 |
| Lung agenesis or pulmonary agenesis | A rare anomaly which may be associated with a number of other visceral systems abnormalities.43 |
| Myhre syndrome | An autosomal dominant condition characterized by facial dysmorphism, short stature, muscle pseudohypertrophy, joint stiffness, and thickened skin.44 |
| MURCS | Mullerian duct agenesis, renal agenesis, cervicothoracic somite dysplasia.45 |
| Pfeiffer syndrome | A mutation of the type 1 and type 2 fibroblastic growth hormone causing craniosynostosis with broad thumbs and toes.46 |
| VACTERL | Vertebral defects, anorectal malformations, cardiac defects, tracheoesophageal fistula with esophageal atresia, renal malformations, and limb defects.47 |
| Other | 22q11 micro duplications similar to DiGeorge syndrome,48 20p12 insertional deletion, 4q21 deletion |
One of the weaknesses of this study is that the incidence of pathological findings associated with butterfly vertebrae may actually be higher than we report. In our review, system categories were marked as “not affected” if there was no specific mention in the case report of an abnormality which may actually have been present in the patient but was not reported by the authors. In addition, because of the review nature of this study, our report cannot demonstrate any causality with regard to low back pain, or neurological symptoms occurring with butterfly vertebrae.
In conclusion, this study represents the largest summary and synthesis of butterfly vertebrae cases to date. Isolated butterfly vertebrae may be associated with back pain, disc herniation, and spinal deformity. The presence of multiple butterfly vertebrae should raise suspicion for a greater systemic illness of syndrome and prompt diagnostic workup by the clinician. Knowledge of butterfly vertebra are important not only to prevent misdiagnosis but also to ensure proper treatment of patients for suspected genetic abnormality.
Acknowledgments
Thank you to Caitlynn Smith, BS, Rachel Swafford, MPH, and Kimberly Davis, BS for technical and administrative support for this research.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Yoshihiro Katsuura, MD  https://orcid.org/0000-0001-7886-4720
https://orcid.org/0000-0001-7886-4720
References
- 1. Ekim A. Butterfly vertebra anomaly: a case report. J Back Musculoskelet Rehabil. 2010;23:161–164. [DOI] [PubMed] [Google Scholar]
- 2. Müller F, O’Rahilly R, Benson DR. The early origin of vertebral anomalies, as illustrated by a “butterfly vertebra.” J Anat. 1986;149:157–169. [PMC free article] [PubMed] [Google Scholar]
- 3. Cave P. Butterfly vertebra. Br J Radiol. 1958;31:503–506. [DOI] [PubMed] [Google Scholar]
- 4. Boulet C, Schiettecatte A, De Mey J, De Maeseneer M. Case report: imaging findings in a “butterfly” vertebra. Acta Neurol Belg. 2011;111:344–348. [PubMed] [Google Scholar]
- 5. Fischer F, Vandemark R. Sagittal cleft (butterfly) vertebrae. J Bone Joint Surg Am. 1945;27:695–698. [Google Scholar]
- 6. Sifuentes Giraldo WA, Gallego Rivera JI, Vázquez Díaz M. Butterfly vertebra. Reumatol Clin. 2015;11:52–53. [DOI] [PubMed] [Google Scholar]
- 7. Zuo K, Asenjo JF, Colmegna I. Butterfly vertebra. Arthritis Rheum. 2013;65:196. [DOI] [PubMed] [Google Scholar]
- 8. Cho HL, Kim JS, Paeng SS, Lee SH. Butterfly vertebra with lumbar intervertebral disc herniation. J Neurosurg Spine. 2011;15:567–570. [DOI] [PubMed] [Google Scholar]
- 9. Patinharayil G, Han CW, Marthya A, Meethall KC, Surendran S, Rudrappa GH. Butterfly vertebra: an uncommon congenital spinal anomaly. Spine (Phila Pa 1976). 2008;33:E926–E928. [DOI] [PubMed] [Google Scholar]
- 10. Delgado A, Mokri B, Miller GM. Butterfly vertebra. J Neuroimaging. 1996;6:56–58. [DOI] [PubMed] [Google Scholar]
- 11. Kapetanakis S, Giovannopoulou E, Nastoulis E, Demetriou T, Butterfly vertebra. A case report and a short review of the literature. Folia Morphol (Warsz). 2016;75:117–121. [DOI] [PubMed] [Google Scholar]
- 12. Frost C, Mesfin A. Butterfly vertebra mimicking a compression fracture. Spine J. 2014;14:2509–2510. [DOI] [PubMed] [Google Scholar]
- 13. Satpathy A, Sloan R, Bhoora IG. Compression fracture or butterfly vertebra: diagnostic importance in a trauma setting. Ann R Coll Surg Engl. 2004;86:W41–W43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wright RW, Brand RA, Dunn W, Spindler KP. How to write a systematic review. Clin Orthop Relat Res. 2007;455:23–29. [DOI] [PubMed] [Google Scholar]
- 15. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Moher D, Shamseer L, Clarke M. et al. ; PRISMA-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) 2015 Statement. Syst Rev. 2015;4:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jackson D, Daly J, Saltman DC. Aggregating case reports: a way for the future of evidence-based health care? Clin Case Rep. 2014;2:23–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Isidro A, Diez I, Malgosa A. Oldest sagittal cleft vertebra. Spine J. 2014;14:3056–3057. [DOI] [PubMed] [Google Scholar]
- 19. Kaplan KM, Spivak JM, Bendo JA. Embryology of the spine and associated congenital abnormalities. Spine J. 2005;5:564–576. [DOI] [PubMed] [Google Scholar]
- 20. Sadler TW, Langman J. Langman’s Medical Embryology. 12th ed Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012. [Google Scholar]
- 21. Bono CM, Bhalla A, Garfin SR. Development of the spine In: Garfin SR, Eismont FJ, Bell GR, Bono CM, Fischgrund JS, eds. Rothman-Simeone and Herkowitz’s The Spine. 7th ed Philadelphia, PA: Elsevier; 2018:3–15. [Google Scholar]
- 22. de Graaf RJ, Matricali B, Hamburger HL. Butterfly vertebra. Clin Neurol Neurosurg. 1982;84:163–169. [DOI] [PubMed] [Google Scholar]
- 23. Schlitt M, Dempsey PJ, Robinson RK. Cervical butterfly-block vertebra. A case report. Clin Imaging. 1989;13:167–170. [DOI] [PubMed] [Google Scholar]
- 24. Sonel B, Yalçin P, Oztürk EA, Bökesoy I. Butterfly vertebra: a case report. Clin Imaging. 2001;25:206–208. [DOI] [PubMed] [Google Scholar]
- 25. Colquhoun J. Butterfly vertebra or sagittal cleft vertebra. Am J Orthop Surg. 1968;10:44–50. [PubMed] [Google Scholar]
- 26. McMaster MJ, Singh H. Natural history of congenital kyphosis and kyphoscoliosis. A study of one hundred and twelve patients. J Bone Joint Surg Am. 1999;81:1367–1383. [DOI] [PubMed] [Google Scholar]
- 27. Tuncel M, Topbasi Z, Kiratli PO. Butterfly vertebra: a diagnostic pitfall on bone scintigraphy. Clin Nucl Med. 2010;35:293–294. [DOI] [PubMed] [Google Scholar]
- 28. Maillefert JF, Saggio D, Hillon P, Tavernier C. Butterfly vertebra: look for Alagille’s syndrome. Rev Rhum Engl Ed. 1995;62:537–538. [PubMed] [Google Scholar]
- 29. Emerick KM, Rand EB, Goldmuntz E, Krantz ID, Spinner NB, Piccoli DA. Features of Alagille syndrome in 92 patients: frequency and relation to prognosis. Hepatology. 1999;29:822–829. [DOI] [PubMed] [Google Scholar]
- 30. Qian B, Qiu Y, Wang B. et al. Unusual association of ankylosing spondylitis with congenital spinal deformity. Spine (Phila Pa 1976). 2010;35:E1512–E1515. [DOI] [PubMed] [Google Scholar]
- 31. Scheer JK, Osorio JA, Smith JS. et al. ; International Spine Study Group. Development of validated computer-based preoperative predictive model for proximal junction failure (PJF) or clinically significant PJK with 86% accuracy based on 510 ASD patients with 2-year follow-up. Spine (Phila Pa 1976). 2016;41:E1328–E1335. [DOI] [PubMed] [Google Scholar]
- 32. Ozaras N, Gumussu K, Demir SE, Rezvani A. Differential diagnosis of multiple vertebral compression: butterfly vertebrae. J Phys Ther Sci. 2015;27:3601–3603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Anderson PJ, Hall C, Evans RD, Harkness WJ, Hayward RD, Jones BM. The cervical spine in Crouzon syndrome. Spine (Phila Pa 1976). 1997;22:402–405. [DOI] [PubMed] [Google Scholar]
- 34. Aygün MS, Sekmenli T, Çiftçi I, Gökmen Z, Tolu İ, Mutlu-Aygün F. Atypical Fryns syndrome: clinical, radiological and pathological findings. Turk J Pediatr. 2014;56:107–110. [PubMed] [Google Scholar]
- 35. Anderson PJ, David DJ. Spinal anomalies in Goldenhar syndrome. Cleft Palate Craniofac J. 2005;42:477–480. [DOI] [PubMed] [Google Scholar]
- 36. Rossi M, D’Armiento M, Parisi I. et al. Clinical phenotype of lathosterolosis. Am J Med Genet A. 2007;143:2371–2381. [DOI] [PubMed] [Google Scholar]
- 37. Takikawa K, Haga N, Maruyama T. et al. Spine and rib abnormalities and stature in spondylocostal dysostosis. Spine (Phila Pa 1976). 2006;31:E192–E197. [DOI] [PubMed] [Google Scholar]
- 38. Vázquez-López ME, López-Conde MI, Somoza-Rubio C, Pérez-Pacín R, Morales-Redondo R, González-Gay MA. Anomalies of vertebrae and ribs: Jarcho Levin syndrome. Description of a case and literature review. Joint Bone Spine. 2005;72:275–277. [DOI] [PubMed] [Google Scholar]
- 39. McCall CP, Hudgins L, Cloutier M, Greenstein RM, Cassidy SB. Jarcho-Levin syndrome: unusual survival in a classical case. Am J Med Genet. 1994;49:328–332. [DOI] [PubMed] [Google Scholar]
- 40. Atar M, Lee W, O’Donnell D. Kabuki syndrome: oral and general features seen in a 2-year-old Chinese boy. Int J Paediatr Dent. 2006;16:222–226. [DOI] [PubMed] [Google Scholar]
- 41. Jarzabek K, Wolczynski S, Lesniewicz R, Plessis G, Kottler ML. Evidence that FGFR1 loss-of-function mutations may cause variable skeletal malformations in patients with Kallmann syndrome. Adv Med Sci. 2012;57:314–321. [DOI] [PubMed] [Google Scholar]
- 42. Chan PC, Hsieh WS, Peng SSF. Klippel-Feil syndrome plus atretic meningocele in one identical twin and anencephaly in the other. J Formos Med Assoc. 2003;102:506–509. [PubMed] [Google Scholar]
- 43. Kaya O, Gulek B, Yilmaz C. et al. Adult presentation of symptomatic left lung agenesis. Radiol Case Rep. 2017;12:25–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Hawkes L, Kini U. Myhre syndrome with facial paralysis and branch pulmonary stenosis: Clin Dysmorphol. 2015;24:84–85. [DOI] [PubMed] [Google Scholar]
- 45. Mahajan P, Kher A, Khungar A, Bhat M, Sanklecha M, Bharucha BA. MURCS association—a review of 7 cases. J Postgrad Med. 1992;38:109–111. [PubMed] [Google Scholar]
- 46. Anderson PJ, Hall CM, Evans RD, Jones BM, Harkness W, Hayward RD. Cervical spine in Pfeiffer’s syndrome. J Craniofac Surg. 1996;7:275–279. [DOI] [PubMed] [Google Scholar]
- 47. Sandal G, Aslan N, Duman L, Ormeci AR. VACTERL association with a rare vertebral anomaly (butterfly vertebra) in a case of monochorionic twin. Genet Couns. 2014;25:231–235. [PubMed] [Google Scholar]
- 48. Diehl A, Mu W, Batista D, Gunay-Aygun M. An atypical 0.73 MB microduplication of 22q11.21 and a novel SALL4 missense mutation associated with thumb agenesis and radioulnar synostosis. Am J Med Genet A. 2015;167:1644–1649. [DOI] [PubMed] [Google Scholar]