Abstract
Elevated rates of burnout and post-traumatic stress have been found in staff working in critical care settings, but the aspect of moral distress has been harder to quantify until a recent revision of a scale previously designed for nurses, was adapted for use with a range of health professionals, including physicians. In this cross-sectional survey, n = 171 nurses and physicians working in intensive care in the United Kingdom completed the Moral Distress Scale-Revised in relation to their experiences at work. Mean (SD) Moral Distress Scale-Revised score was 70.2 (39.6). Significant associations were found with female gender (female 74.1 (40.2) vs. male 55.5 (33.8), p = 0.010); depression (r = 0.165, p = 0.035) and with intention to leave job (considering leaving 85.5 (42.4) vs. not considering leaving 67.2 (38.6), p = 0.040). These results highlight the importance of considering the moral impact of work-related issues when addressing staff wellbeing in critical care settings.
Keywords: Moral Distress Scale-Revised, staff stress, depression, ethics, futility
Technological advances in critical care medicine have led to dramatic improvements in patient survival but have also been associated with a number of unforeseen negative consequences for staff, beyond the inevitable challenges inherent in keeping up with such a fast-moving, highly technical specialty. Paradoxically, given that technology is supposed to make life easier, there is evidence that health workers are increasingly overloaded by the clerical burden related to electronic record keeping and feel guilty about the time it requires them to be away from the bedside.1 Also, the increased survival of intensive care patients has sometimes come at a significant cost to the quality of that survival, particularly in paediatric settings.2 These factors have led to staff feeling demoralised and at times questioning why they do what they do. Furthermore, this anxiety has recently been amplified by the intense public scrutiny of their clinical decision-making afforded by 24/7 social media,3 to which they are unable to respond directly for reasons of patient confidentiality.
Growing appreciation of the stress critical care staff are under has led to calls for more research in this area4 and there are a number of well-validated tools available to measure the symptoms of burnout and post-traumatic stress that staff experience,5–7 but distress related to more existential concerns about meaning and purpose8 is harder to quantify.
Jameton9 first used the term ‘moral distress’ in 1984 to identify this aspect of work-related distress, defining it as ‘when one knows the right thing to do, but institutional constraints make it nearly impossible to pursue the right course of action’,9 differentiating it from having an ‘ethical dilemma’, where the best treatment option is unclear or ‘emotional distress’, which does not necessarily have a moral component. Specifically, moral distress involves ‘a perceived violation of one’s core values and duties’.10 This original concept has been further elaborated by observations that it may build up cumulatively with repeated exposure which leaves behind a ‘moral residue’,11 which is then added to, over time, by subsequent similar events, in what has been described as ‘the crescendo effect’.10 The UK literature on moral distress is limited but recent studies have shown that medical students are able to habituate to it, to some degree, if they are able to see that coping with a morally distressing situation contributes to their learning12 and that critical care nurses feel conflicted, among other things, about the discrepancy between the way they talk about patients in the course of their work and the way they feel they ought to talk about patients.13
In relation to the quantification of moral distress, a scale developed in 2001 to measure it in adult critical care nurses14 has recently been shortened and adapted to cover a wider range of potentially distressing situations and for use with a range of health professionals15 and is now known as the Moral Distress Scale-Revised (MDS-R).16 It has been validated in a number of different staff groups both in intensive care and general hospital settings.17–20
The main aim of this study was to add to the literature by using this scale to establish levels of moral distress in a sample of physicians and nurses working in adult ICU settings in the United Kingdom. Secondary aims were to examine associations between MDS-R scores and socio-demographic factors, scores on a brief mental health screening instrument and intention to leave the job. It was hypothesised that staff would report moral distress associated with their work to varying degrees, with nurses17,20–22 and those with more experience of working on ICU17,23 reporting higher levels than others. It was also expected that intention to leave the job would be correlated with total moral distress scores.16,17,19,22
Method
Ethics approval was obtained from the Joint Research and Enterprise Office for the hospital and university. External ethical approval was not required. The anonymous survey was cross-sectional and took place over two four-week periods in October 2015 (General Intensive Care Unit) and 2016 (Neuro-Intensive Care Unit and Cardiothoracic Intensive Care Unit). Informed consent was assumed by the completion and return of the surveys, which were provided in both electronic and paper form and took less than 10 min to complete. Participants were also provided with an information sheet about the purpose of the study and details of local support services.
Measures
The questionnaire comprised a section on socio-demographic and occupational information (e.g. marital status, gender, length of time qualified) and two standardised measures – the MDS-R and the Patient Health Questionnaire-4 (PHQ-4).
The MDS-R16 is a revision of the Moral Distress Scale14 which comprised 38 items and was designed for use with adult critical care nurses. The updated version, MDS-R, was adapted to include a wider range of potentially distressing situations and shortened to 21 items. It was also made available in a number of different versions, such that it could be completed by a range of health professionals, working in adult or paediatric healthcare settings.
It contains items relating to a range of situations which would be expected, from the literature in this field, to engender a sense of moral distress. These include six items about end of life care; five items on limited staffing and resources; four items about communication between staff and with families; four items on the way decisions are made and two items relating to the witnessing of unethical behaviour. Respondents are asked to rate each item in terms of how frequently they have come across the situation in their work and again, in terms of how disturbing they would find the situation. Responses are scored on a Likert scale from 0 to 4 for both frequency and intensity of disturbance. Composite scores for each item are then generated by multiplying the relevant frequency and intensity scores and these are summed to provide an overall composite moral distress score ranging from 0 to 336. The MDS-R also contains a final section consisting of a series of short questions exploring the respondent’s attitude to the idea of leaving their position as a result of moral distress.
The scale has been shown to have good content validity16 and reliability (Cronbach’s alpha 0.84 to 0.90) across a number of different samples.18–20 It has also been used in a number of different hospital settings.19,24 Questionnaires were included in the analyses in this study as long as there were no more than three missing data points on the MDS-R20 and where missing data were included in the calculation of the total composite score, they were scored conservatively as equivalent to zero.
The PHQ-4 is a validated four-item screening measure for rating psychological distress over the previous two weeks.25 It has good psychometric properties26 and was developed by combining the PHQ-2 and the GAD-2, which are brief screens for the core criteria of depressive disorders and generalised anxiety disorder, respectively, and have been shown to be excellent population screening tools.27,28
Responses for each of the four items are scored using a Likert scale: 0 = ‘not at all’ to 3 = ‘nearly every day’. Subscale scores are obtained by summing scores for questions 1 and 2 for depression, and questions 3 and 4 for anxiety, resulting in total scores that range from 0 to 6 for each subscale. A score of ≥3 on the relevant subscale is regarded as suggestive of depression or anxiety and worthy of further assessment, although not definitively diagnostic.
Statistical analysis
Statistical analyses were carried out using the IBM Statistical Package for the Social Sciences (SPSS) version 25. Descriptive data are given in the form of mean (SD) and percentages. As the distribution of MDS-R scores was negatively skewed (i.e. non normal), non-parametric statistics were employed: Mann–Whitney U and Kruskal–Wallis H tests for between-group comparisons, Spearman’s rho to establish correlations between continuous variables and Fisher’s exact test for categorical group comparisons. Linear regression analysis was performed to ascertain the degree to which any socio-demographic variables which emerged as significantly associated with moral distress explained variance in the total MDS-R score. A p value of 0.05 was applied to determine statistical significance throughout.
Results
In all, 190/408 (47% response rate) questionnaires were returned; 157 on paper and 33 online. Nineteen surveys contained too many missing responses for a composite moral distress score to be calculated, resulting in a final sample of n = 171 for the main analyses. The sample characteristics of this group are provided in Table 1.
Table 1.
Sample characteristics (n = 171).
| Variable | n (%) / mean (SD) | n |
|---|---|---|
| Profession: | ||
| Physician | 26 (15%) | |
| Nurse | 145 (85%) | 171 |
| Intensive care unit: | ||
| General (18-bed) | 74 (43%) | |
| Neuro-intensive (14-bed) | 50 (29%) | |
| Cardiothoracic (18-bed) | 46 (27%) | 170 |
| Age (years) | 36.4 (9.2) | 163 |
| Female | 132 (77%) | 168 |
| Married/cohabiting | 101 (59%) | 169 |
| Live alone | 27 (16%) | 168 |
| Children living at home | 59 (35%) | 168 |
| Full-time worker | 144 (84%) | 166 |
| Years qualified | 11.5 (8.6) | 163 |
Prevalence of distress
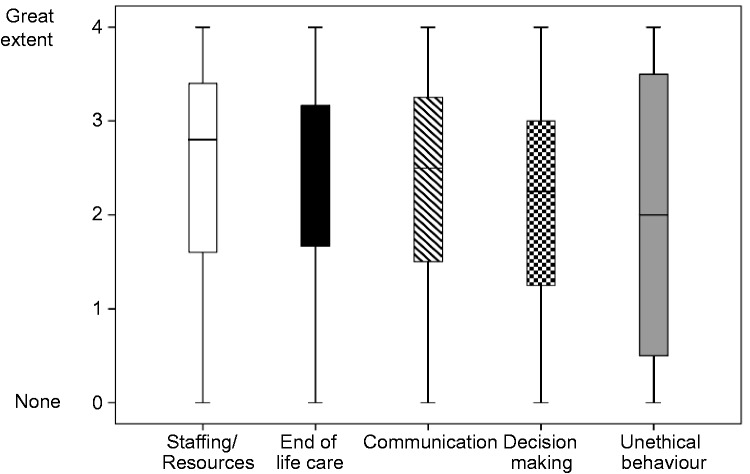
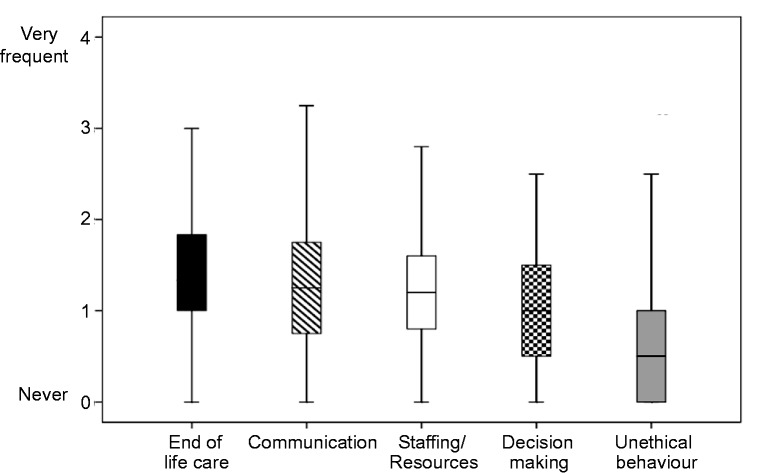
MDS-R total composite scores ranged from 0 to 182, with a mean (SD) of 70.2 (39.6), and no significant differences between units (General 76.7 (44.1), Cardiothoracic 62.8 (32.0), Neuro-intensive 68.5 (37.9); Kruskal–Wallis H = 2.514, p = 0.285). The reliability of responses was good (Cronbach’s alpha = 0.87). In general, staff reported the highest intensity ratings for the items relating to scarce resources and issues arising in the context of end of life care (Figure 1), but in practice the causes of moral distress cited with the highest frequency related to end of life care and communication problems, with unethical behaviour rarely reported as a problem (Figure 2). The two professional groups rated the same three situations as most distressing overall (Table 2) and all of these related to the provision of end of life care in situations of futility.
Figure 1.
Main causes of moral distress on the Moral Distress Scale-Revised by mean item score for level of intensity of disturbance (n = 171).
Note: Data spread is indicated by box and whisker plots, illustrating median, interquartile range and range of scores, excluding outliers.
Figure 2.
Main causes of moral distress on the Moral Distress Scale-Revised by mean item score for frequency (n = 171).
Note: Data spread is indicated by box and whisker plots, illustrating median, interquartile range and range of scores, excluding outliers.
Table 2.
Top five ranking items on the Moral Distress Scale-Revised (MDS-R) for physicians and nurses.
| Item no. | Distressing situation | Physicians
(n = 26) |
Nurses (n = 145) |
||
|---|---|---|---|---|---|
| Mean (SD) composite scorea | Rank | Mean (SD) composite scorea | Rank | ||
| 3. Follow the family’s wishes to continue life support even though I believe it is not in the best interest of the patient | 5.73 (5.01) | 1 | 6.52 (4.16) | 1 | |
| 4. Initiate extensive life-saving actions when I think they only prolong death | 5.04 (4.08) | 2 | 6.13 (4.32) | 2 | |
| 7. Continue to participate in care for a hopelessly ill person who is being sustained on a ventilator, when no one will make a decision to withdraw support | 4.58 (3.72) | 3 | 5.98 (4.69) | 3 | |
| 2. Witness healthcare providers giving ‘false hope’ to a patient or family | 4.04 (3.78) | 4 | 3.91 (3.64) | (8) | |
| 20. Watch patient care suffer because of lack of continuity | 3.46 (4.10) | 5 | 4.09 (4.46) | (7) | |
| 21. Work with levels of nursing or other care provider staffing that I consider unsafe | 3.12 (3.57) | (8) | 5.61 (4.68) | 4 | |
| 17. Work with nurses or other healthcare providers who are not as competent as the patient care requires | 2.77 (2.96) | (11) | 5.31 (4.68) | 5 | |
MDS-R composite score (range 0–16) = frequency score (range 0–4) × intensity score (range 0–4)
Mean item scores relating to the intensity of disturbance associated with the MDS-R items ranged from 1.71 out of a possible total of 4 for item 14 ‘Increase the dose of sedatives for an unconscious patient that I believe could hasten the patient’s death’ to 2.89 for item 21 ‘Work with levels of nursing or other care provider staffing that I consider unsafe’. Mean item scores relating to the frequency with which the situations described in the questionnaire were actually encountered in practice were lower, ranging between 0.46 and 2.09 out of a possible total of 4. The majority of items were rated as occurring infrequently with only two items rated at a mean above 2 for frequency (‘sometimes’/’frequently’). These were item 3 ‘Follow the family’s wishes to continue life support even though I believe it is not in the best interest of the patient’ and item 4 ‘Initiate extensive life-saving actions when I think they only prolong death’.
As regards the intention to quit, 12/171 (7%) reported they had left a previous job for this reason; 44/171 (26%) had considered leaving one in the past and 28/170 (16%) were currently considering leaving because of their feelings of moral distress.
The mental health screening tool PHQ-4 identified 26/163 (16%) of staff as reporting clinically significant levels of anxiety and 13/164 (8%) reporting clinically significant levels of depression. These levels are consistent with community norms.29
Associations with moral distress
Initial analyses of the relationship between socio-demographic variables and MDS-R scores indicated significant associations with nursing profession, female gender and length of time since qualification (see Table 3). However, a linear regression model incorporating the three socio-demographic explanatory variables, although statistically significant (F = 3.103, adjusted R2 = 0.037, p = 0.028), explained less than 4% of the variance in scores and found gender to be the only significant predictor (standardised beta = 0.174, p = 0.037). This suggests that socio-demographic factors are not strongly predictive of moral distress and that the difference initially found between professional groups was most likely accounted for by the higher proportion of female responders in the nursing group as compared with the physician group (85% vs. 44%).
Table 3.
Socio-demographic associations with Moral Distress Scale-Revised (MDS-R) composite scores.
| Categorical variables | MDS-R composite |
|||
|---|---|---|---|---|
| N | Mean (SD) |
p a | ||
| Yes | No | |||
| Nurse profession (v physician) | 171 | 72.5 (39.4) | 57.4 (36.7) | 0.040 |
| Female gender | 168 | 74.1 (40.2) | 55.5 (33.8) | 0.010 |
| Married/living with partner | 169 | 70.2 (41.6) | 71.1 (36.8) | 0.706 |
| Lives alone | 168 | 67.4 (41.6) | 71.3 (39.5) | 0.517 |
| Children living at home | 168 | 71.4 (42.0) | 69.6 (38.2) | 0.855 |
| Full-time worker | 166 | 69.0 (40.4) | 76.9 (34.0) | 0.255 |
| Continuous variables |
n
|
Correlation coefficient |
p b | |
| Age | 165 | 0.099 | 0.209 | |
| Years qualified | 165 | 0.180 | 0.021 | |
Mann–Whitney U test.
Spearman’s rho test. Significant results are indicated in bold.
Moral distress scores were, however, associated with the participant currently considering leaving their job (85.5 (42.4) vs. 67.2 (38.6), p = 0.04); with them having left or considered leaving a job for this reason in the past (86.9 (43.9) vs. 62.1 (34.7) p < 0.001) and with a higher depression score on the PHQ-4 (r = 0.165, p = 0.035), but not with a higher anxiety score (r = 0.122, p = 0.122).
Discussion
The mean MDS-R score of 70.2 in this sample was comparable with those for adult ICU professionals reported in the international literature, which range from 57 to 9216–19 but was lower than that reported recently in a sample of 206 staff working in a paediatric ICU setting20 where the mean MDS-R score was 102. Further investigation is warranted as to whether this finding is representative of other paediatric ICU staff groups as it may be that there are moral issues particularly relevant to the care of critically ill children. The recent dramatic reduction in child mortality has been associated with a significant increase in the numbers of children surviving with serious disabilities, leading one editorial to suggest that moral distress in paediatric and neonatal intensive care settings is ‘inevitable’.2
The expected associations with past and present intention to leave the job were confirmed, lending further support to the argument that employers would be wise to address moral distress in their staff if they wish to retain them.30 However, in this sample, neither profession or length of service were significantly related to moral distress, after controlling for female gender. Although a number of studies have found higher moral distress scores in nurses, and have speculated that this might be because they spend more time at the bedside or have less say in clinical decision making,19 they have not always controlled for gender in their analyses and there are examples of other studies that also found higher levels of moral distress in female staff31,32 reflecting a tendency for women to report higher rates of symptoms more generally.33
The lack of a clear relationship with age or length of service did not support the notion that moral distress is cumulative. However, given the association across the literature with intention to quit, it is possible that staff with the highest moral distress in these occupations self-select out of the workforce, leaving behind staff with lower moral distress. This might explain why, in addition to studies which found an association with higher moral distress, there are examples of studies which found experience was associated with lower moral distress.22 Nevertheless, the finding that rates of mental health problems in this sample were not significantly elevated or strongly related to moral distress is consistent with the idea that moral distress is conceptually different, as has also been found with burnout, which is more prevalent in this population than anxiety or depression.7
As in previous studies, the nature of the situations engendering the highest levels of moral distress was similar across profession and often concerned aggressive treatment in situations where care was felt to be futile. This illustrates the impact on staff of the strain of the new ethical dilemmas that have arisen as a direct result of recent technological advances in this field of medicine, which often involve balancing the wish to preserve life with the obligation to consider the impact on quality of life and on the limited resources available. Interestingly, and consistent with other studies, there was less evidence of moral distress in relation to withholding potential treatment.16,21
There are a number of limitations to this study. The response rate was moderate although comparable to or better than that of other studies in this field.17,19,24 Also the fact that the survey was anonymous meant that it was not possible to determine how representative the sample was of the total staff group. Finally, the fact that it was cross-sectional and based on one site meant that it was not possible to infer causality from the associations found or draw conclusions about their wider generalisability.
These findings add to a body of literature on this newly revised measure and confirm its applicability in another country. The development of a measure such as this is helpful not only in terms of helping health professionals and institutions better understand the causes of work-related distress, but also in relation to the evaluation of interventions designed to address this aspect of working in these demanding healthcare settings. The literature on intervention to reduce moral distress is small but growing.34 In a recent editorial on this topic, Perni 35 has stressed the need for more open discussion about ‘the disconnect between our ideals and the realities of medical practice’ and Hamric and Blackhall21 have observed that successful interventions tend to share common attributes in that they improve communication between members of staff and with patients and families, thereby enabling people to understand the perspectives of others better. In an example, one such intervention, which used the MDS-R as an outcome measure, the ‘PEACE communication rounds’ were not only shown to be associated with a reduction in staff members’ moral distress scores but also with a shorter length of stay for patients.36 Several studies have identified that conflict in relation to the recognition of futility is associated with poor communication about prognosis and end of life planning and that conversely, efforts to reach agreement about care strategies make acceptance of the prognosis by families more likely.37,38 Recently, there has been a move towards ensuring that there is more discussion and documentation of treatment escalation plans in relation to the management of frail, co-morbid patients where CPR or escalation to ICU may be both futile and traumatic.39,40 These developments may be associated with a reduction in moral distress in ICU staff. Other organisational strategies, which might usefully be considered, include the increased provision of mentoring, which is now recognised as a valuable asset across the whole lifespan of a career,41 and the development of an institution-wide Moral Distress Consultation Service.42
In conclusion, it is likely that some degree of moral distress is inevitable in this work and indeed some discomfort of this kind may be a sign that staff are retaining the ability to think critically about what they are doing. However, if this form of work-related stress builds to a level where a staff member’s emotional wellbeing is seriously compromised, it is likely to have an impact on the quality of care of patients, as well as on unit morale and staff turnover. Interventions designed to help staff to make sense of the more difficult aspects of their experiences at work together and find a way to work through them, are therefore to be welcomed and a measure such as the MDS-R provides a potentially useful tool with which to evaluate their impact.
Acknowledgments
We are grateful to Dr Hamric for permission to use the MDS-R and would like to thank all the members of staff who took part in this study.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Shanafelt TD, Dyrbye LN, Sinsky C, et al. Relationship between clerical burden and characteristics of the electronic environment with physician burnout and professional satisfaction. Mayo Clin Proc 2016; 91: 836–848. [DOI] [PubMed] [Google Scholar]
- 2.Field D, Deeming J, Smith LK. Moral distress: an inevitable part of neonatal and paediatric intensive care? Arch Dis Child 2016; 101: 686–688. [DOI] [PubMed] [Google Scholar]
- 3.Hawryluck L, and Brindley PG. Psychological burnout and critical care medicine: big threat, big opportunity. Intens Care Med. Epub ahead of print 20 January 2018. DOI: 10.1007/s00134-018-5063-6. [DOI] [PubMed]
- 4.Moss M, Good VS, Gozal D, et al. An official critical care societies collaborative statement – burnout syndrome in critical care health-care professionals: a call for action. Chest 2016; 150: 17–26. [DOI] [PubMed] [Google Scholar]
- 5.Embriaco N, Papazian L, Kentish-Barnes N, et al. Burnout syndrome among critical care healthcare workers. Curr Opin Crit Care 2007; 13: 482–488. [DOI] [PubMed] [Google Scholar]
- 6.Mealer ML, Shelton A, Berg B, et al. Increased prevalence of post-traumatic stress disorder symptoms in critical care nurses. Am J Respir Crit Care Med 2007; 175: 693–697. [DOI] [PubMed] [Google Scholar]
- 7.Colville GA, Smith JG, Brierley J, et al. Coping with staff burnout and work-related posttraumatic stress in intensive care. Pediatr Crit Care Med 2017; 18: e267–e273. [DOI] [PubMed] [Google Scholar]
- 8.Kompanje EJO. Burnout, boreout and compassion fatigue on the ICU: it is not about work stress, but about lack of existential significance and professional performance. Intens Care Med 44: 690–691. [DOI] [PubMed]
- 9.Jameton A. Nursing practice: the ethical issues, Englewood Cliffs, NJ: Prentice-Hall, 1984. [Google Scholar]
- 10.Epstein EG, Hamric AB. Moral distress, moral residue, and the crescendo effect. J Clin Ethics 2009; 20: 330–342. [PubMed] [Google Scholar]
- 11.Webster GC, Baylis FE. Moral Residue. In: Rubin SB, Zoloth L. (eds). Margin of error: the ethics of mistakes in the practice of medicine, Hagerstown, MD: University Publishing Group, 2000, pp. 217–230. [Google Scholar]
- 12.Monrouxe LV, Rees CE, Dennis I, et al. Professionalism dilemmas, moral distress and the healthcare student: insights from two online UK-wide questionnaire studies. BMJ Open 2015; 5: e007518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McLean C, Coombs M, Gobbi M. Talking about persons – thinking about patients: an ethnographic study in critical care. Int J Nurs Stud 2016; 54: 122–131. [DOI] [PubMed] [Google Scholar]
- 14.Corley MC, Elswick RK, Gorman M, et al. Development and evaluation of a Moral Distress Scale. J Adv Nurs 2001; 33: 250–256. [DOI] [PubMed] [Google Scholar]
- 15.Mealer M, Moss M. Moral distress in ICU nurses. Intens Care Med 2016; 42: 1615–1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hamric AB, Borchers CT, Epstein EG. Development and testing of an instrument to measure moral distress in healthcare professionals. AJOB Prim Res 2012; 3: 1–9.26137345 [Google Scholar]
- 17.Dodek PM, Wong H, Norena M, et al. Moral distress in intensive care unit professionals is associated with profession, age, and years of experience. J Crit Care 2016; 3: 178–182. [DOI] [PubMed] [Google Scholar]
- 18.Karanikola MNK, Albarran JW, Drigo E, et al. Moral distress, autonomy and nurse-physician collaboration among intensive care unit nurses in Italy. J Nurs Manag 2014; 22: 472–484. [DOI] [PubMed] [Google Scholar]
- 19.Whitehead PB, Herbertson RK, Hamric AB, et al. Moral distress among healthcare professionals: report of an institution-wide survey. J Nurs Scholarsh 2015; 47: 117–125. [DOI] [PubMed] [Google Scholar]
- 20.Larson CP, Dryden-Palmer KD, Gibbons C, et al. Moral distress in PICU and Neonatal ICU practitioners: a cross-sectional evaluation. Pediat Crit Care Med 2017; 18: e318–e326. [DOI] [PubMed] [Google Scholar]
- 21.Hamric AB, Blackhall LJ. Nurse-physician perspectives on the care of dying patients in intensive care units: collaboration, moral distress, and ethical climate. Crit Care Med 2007; 35: 422–429. [DOI] [PubMed] [Google Scholar]
- 22.Abbasi M, Nejadsarvari N, Kiani M, et al. Moral distress in physicians practicing in hospitals affiliated to medical sciences universities. Iran Red Crescent Med J 2014; 16: e18797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shoorideh FA, Ashktorab T, Yaghmaei F, et al. Relationship between ICU nurses’ moral distress with burnout and anticipated turnover. Nurs Ethics 2015; 22: 64–76. [DOI] [PubMed] [Google Scholar]
- 24.Dyo M, Kalowes P, Devries J. Moral distress and intention to leave: a comparison of adult and paediatric nurses by hospital setting. Intens Crit Care Nurs 2016; 36: 42–48. [DOI] [PubMed] [Google Scholar]
- 25.Kroenke K, Spitzer RL, Williams JBW, et al. An ultra-brief screening scale for anxiety and depression: the PHQ-4. Psychosomatics 2009; 50: 613–621. [DOI] [PubMed] [Google Scholar]
- 26.Löwe B, Wahl I, Rose M, et al. A 4-item measure of depression and anxiety: validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. J Affect Disord 2010; 122: 86–95. [DOI] [PubMed] [Google Scholar]
- 27.Kroenke K, Spitzer RL, Williams JBW, et al. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007; 146: 317–325. [DOI] [PubMed] [Google Scholar]
- 28.Kroenke K, Spitzer RL, Williams JBW. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care 2003; 41: 1284–1292. [DOI] [PubMed] [Google Scholar]
- 29.Mental Health Foundation. Mental health statistics: the most common mental health problems, www.mentalhealth.org.uk/statistics/mental-health-statistics-mostcommon-mental-health-problems (accessed 4 March 2018).
- 30.Pendry PS. Moral distress: recognizing it to retain nurses. Nurs Econ 2007; 25: 217–212. [PubMed] [Google Scholar]
- 31.O’Connell CB. Gender and the experience of moral distress in critical care nurses. Nurs Ethics 2015; 22: 32–42. [DOI] [PubMed] [Google Scholar]
- 32.Førde R, Aasland OG. Moral distress among Norwegian doctors. J Med Ethics 2008; 34: 521–525. [DOI] [PubMed] [Google Scholar]
- 33.Green CA, Pope CR. Gender, psychosocial factors and the use of medical services: a longitudinal analysis. Soc Sci Med 1999; 48: 1363–1372. [DOI] [PubMed] [Google Scholar]
- 34.Musto LC, Rodney PA, Vanderheide R. Toward interventions to address moral distress: navigating structure and agency. Nurs Ethics 2015; 22: 91–102. [DOI] [PubMed] [Google Scholar]
- 35.Perni S. Moral distress: a call to action. AMA J Ethics 2017; 19: 533–536. [Google Scholar]
- 36.Wocial L, Ackerman V, Leland B, et al. Communication Excellence (PEACE) rounds: decreasing moral distress and patient length of stay in the PICU. HEC Forum 2017; 29: 75–91. [DOI] [PubMed] [Google Scholar]
- 37.Ryan C, Dawson D, Ball J, et al. Nurses' perceptions of aids and obstacles to the provision of optimal end of life care in ICU. ICMx 2016; 4(Suppl 1): 27. [Google Scholar]
- 38.Borowske D. Straddling the fence: ICU nurses advocating for hospice care. Crit Care Nurs Clin North Am 2012; 24: 105–116. [DOI] [PubMed] [Google Scholar]
- 39.Obolensky L, Clark T, Matthew G, et al. A patient and relative centred evaluation of treatment escalation plans: a replacement for the do-not-resuscitate process. J Med Ethics 2010; 37: 518–520. [DOI] [PubMed] [Google Scholar]
- 40.Shermon E, Munglani L, Oram S, et al. Reducing DNACPR complaints to zero: designing and implementing a treatment escalation plan using quality improvement methodology. BMJ Open Qual 2017; 6: e000011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Disch J. Rethinking mentoring. Crit Care Med 2018; 46: 437–441. [DOI] [PubMed] [Google Scholar]
- 42.Hamric AB, Epstein EG. A health system-wide Moral Distress Consultation Service: development and evaluation. HEC Forum 2017; 29: 127–143. [DOI] [PubMed] [Google Scholar]