Abstract
Introduction
End of life and organ donation discussions come at a time of acute emotional unrest for grieving relatives. Their attitudes and eventual decisions regarding consent to organ donation are shaped by multiple factors during these stressful periods. At our tertiary centre intensive care unit, we anecdotally observed that the mode of organ donation affects family behaviour as to whether families stay until transfer to theatre for organ recovery, or leave after consenting for donation. We sought to ascertain if this observation was true and then to hypothesise reasons for why this may be the case.
Methods
Records of patients consented for deceased organ donation between 1 January 2015 and 31 December 2017 at the Nottingham University Hospitals NHS Trust were reviewed and analysed.
Results
After exclusion criteria were applied, 91 patient cases were included in the final analysis (donation after brainstem death (DBD), 36; donation after circulatory death (DCD), 55). Thirty-six per cent of DBD families stayed until the point of organ recovery compared to 80% of DCD families (p < 0.00001).
Discussion
We hypothesise that this family behaviour may be indicative of an acceptance in DBD of the patient's death, and therefore that the patient has moved beyond further harm. For this reason, the family may feel able to leave after consent for donation. A greater understanding of how family behaviours differ depending on the mode of organ donation may aid how these families are best cared for in the intensive care unit.
Keywords: Brain death, critical care, family behaviour, organ donation, tissue donors
Introduction
The events leading to patients becoming deceased organ donors are invariably abrupt, unanticipated and untimely for family members and this places an additional emotional burden. During end-of-life discussions, it is the responsibility of intensive care staff to approach grieving relatives and, working with a specialist nurse for organ donation, raise the subject of organ donation in a multi-disciplinary and appropriately timed manner.1–3 This can be a challenging prospect and requires a great deal of compassion, empathy and professional expertise to make this approach and fulfil the care needs of the bereaved family and the potential donor.
A UK quantitative analysis of 4703 family approaches to discuss organ donation found that patient ethnicity, knowledge of a patient's wish and involvement of a specialist nurse for organ donation were strongly associated with consent (p < 0.0001).4 Studies conducted during the 1990s demonstrated that family interactions with healthcare professionals at the time of the donation process markedly affected their eventual decisions regarding donation. The importance of comprehension of brain death, satisfaction with the level of care provided and the timing of practitioner approach all had substantial bearing on the eventual donation decision.5–7 Subsequent research has highlighted influencing factors such as families receiving clear information regarding prognosis and the donation process, being approached in an empathetic and supportive manner and being offered ample opportunity to broach any concerns with staff.8–10
In addition, the emotional turmoil experienced in the context of a relative's death has been demonstrated to markedly affect behaviour. Compelling UK evidence from Sque et al. describes how the emotional upheaval experienced by families when combined with a poor understanding of brain death, in the context of a ventilated ‘still breathing’ patient, provokes discord with the donation process and intensifies familial distress.11,12 This was subsequently found to negatively affect donation decisions. Other instinctive next of kin responses to family death include the inability to distinguish between the physical body and personal identity,13 as well as ‘death anxiety defences’ such as ‘feelings of immortality’ which are strengthened by grieving families observing their deceased relatives in a physiologically maintained state in intensive care.14 It is proposed that in some individuals and families, such factors engender further dissonance between the notions of ‘gift of life’ as supported by transplant policy and altruistic and societal norms, verse ‘sacrifice’ of the body, and the wish to protect the dead body.15 The latter perhaps acting as an anthropological higher mammalian norm.16
It is well established that a families' acknowledgement of their relative's death or impending loss and understanding of the end-of-life process is key to facilitate organ donation.17 The behaviours exhibited by families are therefore a reflection of their attitudes to donation and thus provide insight into decisions made. In our intensive care unit, we anecdotally observed a difference in family behaviour between consented, donors after brainstem death (DBD) and donors after circulatory death (DCD) patients. In DBD, patient families often did not stay on the ICU until the patient was moved to theatre for organ recovery, but in DCD they usually did.
We considered it important to consider whether variation in family behaviour truly exists between DBD and DCD. Any distinction observed could provide opportunities to tailor the structure of organ donation discussion in each group and thus optimise the support offered to families. Moreover, such data are necessary if they can provide avenues to improve consent rates to donation within the UK.
The aim of this service evaluation was to note how often families stay with the patients in DBD and DCD donor groups, until being transferred to theatre for organ recovery.
Methods
Nottingham University Hospitals NHS Trust provides specialist services for three to four million people across the East Midlands. The major trauma and neurosurgical intensive care unit based at the Queen's Medical Centre campus manages the majority of organ donation cases within the region.
Medical and nursing records were reviewed for all patients consented for deceased donation at NUH between 1 January 2015 and 31 December 2017. From these records, we observed if it was documented whether the patient's family stayed with their relative up to the point of being transferred to theatre for organ recovery, or withdrawal of life-sustaining treatment (WLST) in DCD. The Trust's Caldicott guardian was consulted for permission for the service evaluation to take place.
Patients excluded from the evaluation were those in which insufficient data were available and cases where clinical improvement occurred post donation consent. Total number of cases and percentage values were attributed to all groups and subset data.
Additionally, in order to further analyse our qualitative data, a chi squared statistical test was performed. The CHITEST function on Microsoft excel software was utilised to generate the final p-value in order to highlight significance.
Results
Between 1 January 2015 and 31 December 2017, 130 families gave initial consent for organ donation to proceed (DBD 42, DCD 88). The consent rate for DBD was 64%, for DCD 55%.
Thirty-nine patients were excluded from this total (DBD 2, DCD 37). Seventeen of the 39 were ineligible due to insufficient information regarding the family behaviour after consent. Two further patients' data were removed, as following initial consent to donation they improved clinically. Two were removed as the patient's families withdrew their consent further into the donation process, both of which were DCD. The remaining 18 excluded cases did not proceed to organ donation. Three of which were declined by Her Majesty's Coroner, 3 clinically deteriorated and 12 had no organs accepted.
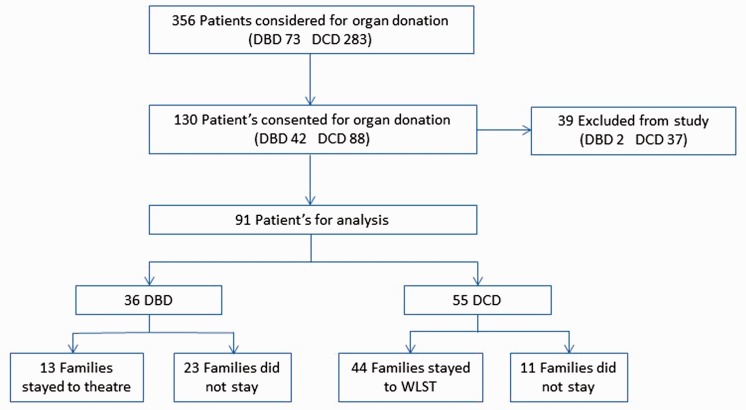
Ninety-one patient cases were therefore included in the analysis (DBD 36, DCD 55). In DBD, 13 families (36%) stayed until up to the point of transfer to theatre for organ recovery, and in DCD 44 (80%) stayed until WLST (p < 0.00001) (see Figure 1).
Figure 1.
Flow diagram illustrating patient inclusion breakdown.
DBD: donation after brainstem death; DCD: donation after circulatory death.
Discussion
It is evident that family behaviour differs markedly between DBD and DCD in our tertiary referral neuro and trauma hospital, with significantly fewer DCD families saying their goodbyes and leaving after giving consent for donation. In effect, this means DCD families stay approximately 12 or more hours longer than most DBD cases.
Variation between the two modes of organ donation is also evident from national statistics. Data from NHS Blood and Transplant illustrate discernibly lower consent rates for donation in DCD in comparison with DBD and a noticeably greater incidence of consent withdrawal further along the donation process.18 The latter is reflected in our data, with the two withdrawals of consent occurring in the DCD cohort. In DCD, the length of the donation process is more often quoted by families as a reason not to consent to donation for their relative.18
It is important to speculate about what this disparity in exhibited behaviour reveals about the attitudes of families to death and donation. It may be indicative of an acceptance in DBD of the patient's death, and therefore the patient has moved beyond further harm. For this reason, the family may feel able to leave compared to in DCD where the patient has not yet died and therefore the end has not yet occurred. Additionally, in DCD, there is much less guarantee that deceased donation will actually occur. Time to asystole greater than 3 h will lead to the national organ retrieval service standing down, this occurs in 45% of all DCD cases that do not proceed to solid organ donation.19 It is even possible that in DCD, families may hold out hope that the doctors are wrong and patient recovery is still feasible. But if this was so it seems unlikely, they would give consent for organ donation.
Despite active public engagement and improvement to many aspects in donor processes, organ demand still heavily outweighs provision in the UK. This is highlighted by the death of 457 potential organ recipients waiting for transplantation in the year between March 2016 and March 2017.18 Static consent rates remain the biggest obstacle affecting the recovery of more donor organs, with the UK exhibiting some of the highest percentage of donation refusals by family in Europe.20 It is well established that the way in which clinicians initiate organ donation discussions with families can markedly influence, both positively and negatively, decisions regarding consent to donation. Our postulated family variance in mind-set between DBD and DCD may indicate that a more individually tailored approach to donation discussion in each group is required.
A recent study from the USA highlighted harms that can occur to families when DCD does not proceed.21 Further work into exploring differences in family behaviours between the two modes of organ donation may assist intensive care staff in better understanding the needs of the bereaved proceeding with DCD and thus provide for them during such uniquely heart-rending situations. The UK, as the world leader in DCD, has a special obligation to lead on this area of research.
Limitations in our evaluation were its retrospective nature and that we focussed narrowly on comparing the mode of organ donation versus the family decision to leave the patient after consent. We did not investigate demographic data on the age, sex, ethnicity, cause of death and other factors which may also influence family behaviour. Nor did we have any qualitative family discussions which could elucidate their reasons for leaving. Additionally, we did not record if families who said no to donation stayed or left, and this difference would be important for future comparison and reflection. We would encourage a multi-centre observation research trial, perhaps with some qualitative interviews of donor families, in this important area of deceased donation.
Summary
There is profound complexity surrounding end-of-life care with respect to deceased organ donation. Family consent to donation is known to be affected by a whole host of varying cultural, personal, religious, demographic and healthcare professional factors. The results of this evaluation highlight differences in the behaviour and attitude of DBD and DCD families, which could provide new insights. This is important to understand in more detail, so that the care of the patient and their bereaved family can remain the primary focus of all clinicians involved in the donation process.
Acknowledgements
This work was conducted at the Nottingham University Hospitals NHS Foundation Trust.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.General Medical Council (UK): treatment and care towards the end of life: good practice in decision making, www.gmc-uk.org/guidance/ethical_guidance/end_of_life_guidance.asp (2010, accessed 8 January 2018).
- 2.National Institute for Health and Clinical Excellence: organ donation for transplantation: improving donor identification and consent rates for deceased organ donation, www.nice.org.uk/guidance/cg135 (2011, accessed 8 January 2018).
- 3.NHS Blood & Transplant: approaching the families of potential organ donors. Best practice guidance, https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/1462/family_approach_best_practice_guide-1.pdf (2013, accessed 8 January 2018).
- 4.Hulme W, Allen J, Manara AR, et al. Factors influencing the family consent rate for organ donation in the UK. Anaesthesia 2016; 71: 1053–1063. [DOI] [PubMed] [Google Scholar]
- 5.Gortmaker SL, Beasley CL, Sheehy E, et al. Improving the request process to increase family consent for organ donation. J Transpl Coord 1998; 8: 210–217. [DOI] [PubMed] [Google Scholar]
- 6.DeJong W, Franz HG, Wolfe SM, et al. Requesting organ donation: an interview study of donor and non-donor families. Am J Crit Care 1998; 7: 13–23. [PubMed] [Google Scholar]
- 7.McNamara P, Beasley C. Determinants of familial consent to organ donation in the hospital setting. In: PI Cecka, JM Terasaki. (eds). Clinical transplants, Los Angeles, CA: UCLA Tissue Typing Laboratory, 1997, pp. 219–229. [PubMed] [Google Scholar]
- 8.Siminoff LA, Gordon N, Hewlett J, et al. Factors influencing families' consent for donation of solid organs for transplantation. JAMA 2001; 286: 71–77. [DOI] [PubMed] [Google Scholar]
- 9.Jacoby L, Breitkopf CR, Pease E. A qualitative examination of the needs of families faced with the option of organ donation. Dimens Crit Care Nurs 2005; 24: 183–189. [DOI] [PubMed] [Google Scholar]
- 10.Rodrigue JR, Cornell DL, Howard RJ. Organ donation decision: comparison of donor and nondonor families. Am J Transplant 2006; 6: 190–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sque M, Long T, Payne S. Organ donation: key factors influencing families' decision-making. Transplant Proc 2005; 37: 543–546. [DOI] [PubMed] [Google Scholar]
- 12.Sque M, Payne S, Macleod Clark J. Gift of life or sacrifice?: key discourses to understanding organ donor families' decision-making. Mortality 2006; 11: 117–132. [Google Scholar]
- 13.Haddow G. The phenomenology of death, embodiment and organ transplantation. Sociol Health Ill 2005; 27: 92–113. [DOI] [PubMed] [Google Scholar]
- 14.Sanner M. People's attitudes and reactions to organ donation. Mortality 2006; 11: 133–150. [Google Scholar]
- 15.Sque M, Long T, Payne S, et al. Why relatives do not donate organs for transplants: ‘sacrifice’ or ‘gift of life’?. J Adv Nursing 2008; 61: 134–144. [DOI] [PubMed] [Google Scholar]
- 16.King BJ. Animal behaviour: when animals mourn. Sci Am 2013; 309: 62–67. [DOI] [PubMed] [Google Scholar]
- 17.Vincent A, Logan L. Consent for organ donation. Br J Anaesth 2015; 108: 80–87. [DOI] [PubMed] [Google Scholar]
- 18.NHS Blood & Transplant: organ donation and transplantation; activity report 2016/17, https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/4657/activity_report_2016_17.pdf (accessed 13 February 2018).
- 19.NHS Blood & Transplant: potential donor audit 2016/2017. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/5985/annual-pda-report-2016-17.pdf (accessed 13 February 2018).
- 20.Farsides B. Respecting wishes and avoiding conflict: understanding the ethical basis for organ donation and retrieval. Br J Anaesth 2012; 108: 73–79. [DOI] [PubMed] [Google Scholar]
- 21.Taylor L, Buffington A, Scalea J, et al. Harms of unsuccessful donation after circulatory death: an exploratory study. Am J Transplant 2018; 18: 402–409. [DOI] [PMC free article] [PubMed] [Google Scholar]