Abstract
Introduction
In resource-limited settings – with inequalities in access to and outcomes for trauma, surgical and critical care – intensive care registries are uncommon.
Aim
The Pakistan Society of Critical Care Medicine, Intensive Care Society (UK) and the Network for Improving Critical Care Systems and Training (NICST) aim to implement a clinician-led real-time national intensive care registry in Pakistan: the Pakistan Registry of Intensive CarE (PRICE).
Method
This was adapted from a successful clinician co-designed national registry in Sri Lanka; ICU information has been linked to real-time dashboards, providing clinicians and administrators individual patient and service delivery activity respectively.
Output
Commenced in August 2017, five ICU’s (three administrative regions – 104 beds) were recruited and have reported over 1100 critical care admissions to PRICE.
Impact and future
PRICE is being rolled out nationally in Pakistan and will provide continuous granular healthcare information necessary to empower clinicians to drive setting-specific priorities for service improvement and research.
Keywords: Intensive care, health system strengthening, intensive care registries, low and middle income countries
Intensive care registries
Intensive care registries in high-income countries (HICs) play an increasingly pivotal role in evaluating treatment outcomes, benchmarking services and providing opportunities for service forecasting.1,2 These high-quality continuous surveillance systems are ideally suited to capture the level of granular data needed to evaluate care processes and outcomes, and to inform strategies to improve care.1,2 However intensive care registries remain notably absent in the vast majority of the world’s healthcare systems.3 In South Asia, a region encompassing eight countries and a population of 1.87 billion (24.6% of the world's population), only Sri Lanka has a national intensive care registry.4,5
Investment in registries remains limited with ambiguity and concern over cost, sustainability and feasibility. Experiences from HICs have demonstrated that registries can be difficult to implement; requiring specialist and expensive information technology. In addition, implementation in low and low and middle income countries (LMICs) also needs to overcome low information availability and poor infrastructure.6 Scarce resources and high patient numbers often disconnect frontline staff from the potentially long-term benefits of such systems.7,8
In South Asia, improving sanitation, industrial urbanisation and increasing life expectancy have generated a shift in the region’s healthcare priorities: trauma care and curative services including surgical and cancer care are in growing demand. Whilst mortality is estimated to be higher in the region compared to HICs, the true burden of morbidity on recovery and on economic growth remains unquantified.7,8 As intensive care services become more accessible in the region, the lack of reliable, granular, setting-specific data hampers efforts to address inequalities in care and evaluate therapies such as respiratory support, fluid management and antibiotic use.9,10
A trend for change
Encouragingly, there are indications that intensive care registries are being implemented in non-HIC settings. Epimed, a privately funded registry in Brazil (an upper middle-income country) incorporates 598 ICU’s from 318 hospitals predominantly in the southeast region of the country.11 In Malaysia, another upper middle-income country, The National Audit on Adult Intensive Care Units (NAICU, formerly MRIC) similarly combines annual data on occupancy, with measures of ICU performance and national service provision.12 In Sri Lanka, National Intensive Care Surveillance supported by the Network for Intensive Care Systems and Training (NICST) in partnership with the Sri Lankan Ministry of Health includes virtually all 102 state adult (and most paediatric and neonatal) ICUs. This lower middle-income country national registry (as with Epimed in Brazil) provides real-time aggregate information on ICU occupancy and acuity. Focused on supporting quality improvement, these registries provide classical demographic and occupancy information, alongside detailed data regarding infectious episodes, adverse events and checklists aimed at improving adherence to best practice guidelines. In addition, the Sri Lankan registry informs a national 24 h bed availability system and has to date assisted in locating ICU beds for over 4800 patients.13 The registry output has also resulted in collaborative service evaluations, multicentre validations of prognostic models and international research projects.14–16
These grass roots initiatives, driven by frontline clinicians, demonstrate that electronic ICU registries providing real-time, continuous data are feasible in non-HICs. This paper describes the collaborative efforts to develop such a national critical care registry for Pakistan.
Aim
A clinician-led partnership of the Pakistan Society of Critical Care Medicine (PSCCM), Intensive Care Society (ICS, UK) and Network for Improving Critical care Systems and Training (NICST) aims to implement a national intensive care registry – Pakistan Registry of Intensive CarE (PRICE) – which has been adapted from the electronic registry methodology used in Sri Lanka.13,17 The collaboration aims to develop a critical care network linking South Asia and the UK, with a focus on system strengthening and increased availability of granular data needed for setting-specific, globally relevant research.
Methodology
In partnership with clinician, academic and administrative stakeholders in Pakistan, ICUs from both government, and semi-government healthcare facilities have been recruited. Initial recruitment has focused on hospitals recognised for postgraduate training by the College of Physicians and Surgeons Pakistan (CPSP) enabling PRICE to build on a core group of accredited ICUs from each region.17
Registry design
Admission characteristics, diagnosis and basic physiology were captured daily for each patient admitted to the ICU, adapted from the NICST registry. Diagnoses were mapped to APACHE IV18 enabling risk adjustment, benchmarking and the potential for international comparison. Real-time information was displayed in dashboards,19 supporting clinicians with routine clinical care. De-identified information was displayed in dashboards, enabling administrators and researchers to evaluate trends in unit activity, severity of illness, bed occupancy and outcomes within their respective institution. Anonymised aggregate data were developed to provide centres (and the public) the opportunity to see their output in relation to their peers.
Implementation and stakeholder engagement
In partnership with frontline ICU healthcare teams, clinical stakeholders (doctors, nurses, technicians) were locally appointed as centre coordinators during site recruitment. Following face-to-face training, centre coordinators then led local implementation, supporting data collection and assisting colleagues with dashboard navigation. A cycle of adaptation, implementation and evaluation, (including user feedback and data completeness) was used to refine the data set and highlight the priorities in information requirement of frontline users.
Data entry and management
Centres contributed information voluntarily through a secure cloud-based mobile or desktop portal, co-designed by clinicians and researchers in Sri Lanka (NICST). To reduce the burden of data entry and enable real-time data visualisation, free-text fields were avoided and instead drop-down and check-box options were utilised. Weekly telephone follow-up, conducted through the nominated local coordinators was used to extract admission numbers from existing (paper-based) records within each ICU. Telephone follow-up combined validation of reporting with an opportunity for technical support and regular contact with local coordinators and clinicians. Information on completeness of reporting was displayed monthly through each participating centre’s own dashboard, guiding the participating ICUs towards greater data completeness.20
Pilot data
PRICE, founded in August 2017, has recruited five member ICU’s (Figure 1), with a combined capacity of 104 ventilated beds.
Figure 1.
ICU centres recruited to PRICE August 2017 to January 2018. (1) Pakistan Institute of Medical Sciences, Islamabad. (2) National Hospital and Medical Centre, Lahore. (3) Jinnah Hospital, Lahore. (4) National Institute of Cardiovascular Diseases, Karachi. (5) Civil Hospital Karachi.
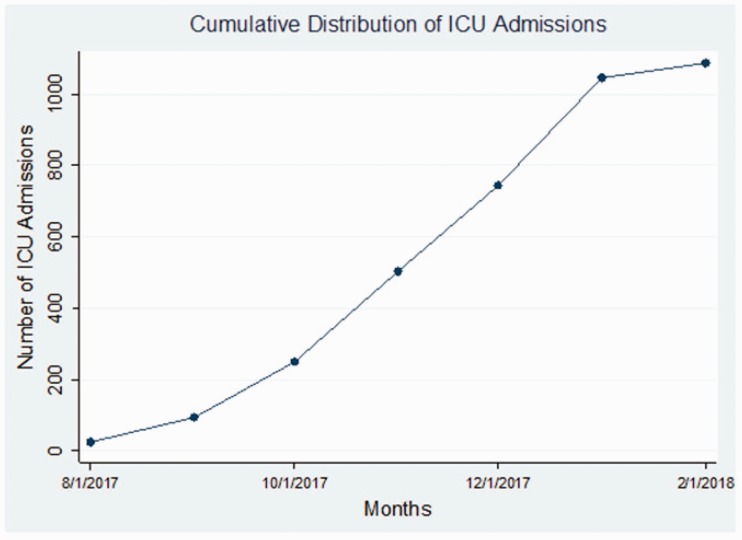
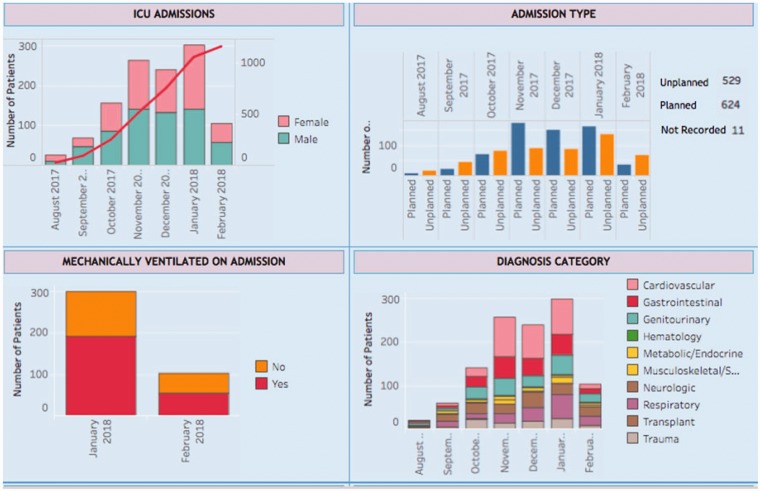
Recruited ICUs were from three cities: Karachi, Lahore and Islamabad, connecting three of the countries’ seven administrative regions. The network has reported 1100 admissions, of whom 494 (44.83%) were unplanned and 640 (58.1%) were male patients (Figure 2).
Figure 2.
Cumulative admission episodes to PRICE, August 2017 to January 2018.
The most common specialities were general surgery 174 (15.8%), cardiac surgery 278 (25.3%) and neuro-trauma 144(13.1%). Mechanical ventilation on ICU admission was required in 666 (60.48%) cases.
Dashboards enabled users to highlight specific trends and sort the aggregate information by week, month or by admission characteristics (e.g. planned versus unplanned, or operative versus non operative) depending on their requirements (Figure 3).
Figure 3.
PRICE – clinician co-designed real-time dashboards.
Challenges
Data security and appropriate data management are universal considerations in electronic health systems and registries. Following the international standards set by existing registries, data are stored in secure servers, and access is curated.21 Contributing sites have full access to all data submitted from their ICU but do not have access to raw data submitted by other contributing units.
Technical support for the registry, data management and storage is currently provided by the NICST team based in Sri Lanka. The collaboration is working with local experts and existing health-related registries in Pakistan to build capacity (funding and human resources) for local management.
Impact and future
Output from the registry is already supporting ongoing international research collaborations in ventilation practices in LMIC’s.15 The registry will also enable identification of specific risk factors for mortality in critically ill patients within the region. PRICE will provide an opportunity for routine, continuous capture of granular healthcare information necessary to empower clinicians driving setting-specific priorities for service improvement and research in intensive care. Improving access to and delivery of surgical care and evaluation of measures in quality of life for patients following intensive care admission have been identified as priorities.
Implementation will next focus on recruitment of all centres recognised by CPSP for postgraduate training and expansion to the administrative regions of Khyber Pakhtunkhwa, Balochistan, Gilgit Baltistan and Azad Kashmir.
Contemporaneous to the expansion of PRICE, a national cross-sectional survey, adapted from NICST, is being undertaken in collaboration with the Pakistan Society of Critical Care Medicine (PSCCM).22 This survey will provide the first detailed profile of state and private intensive care facilities in Pakistan including infrastructure, human resources and staff training.22
The collaboration will strengthen critical care networks internationally by linking South Asia and the UK, and by providing real-time epidemiology (e.g. sepsis, respiratory infections and febrile illness) the registry network will provide a springboard for future globally relevant research.10 PRICE will further contribute to the ongoing work by South Asian collaborations including South East Asia Research in Critical care Health [SEARCH]* (founded in 2015) which under the umbrella of South Asian Association for Regional Cooperation (SAARC) aims to improve collaborative research and development of healthcare in the region.
Acknowledgements
The authors would like to acknowledge Mr Asif Umer, National Hospital and Medical Centre, Lahore; Dr Muhammad Liaqat, Jinnah Hospital, Lahore; Dr Amin Khawaja, National Institute of Cardiovascular Diseases, Karachi; Dr Muneeb Ali, Pakistan Institute of Medical Sciences, Islamabad; Dr Safia Zafar Siddiqui, Civil Hospital, Karachi; Mr PGI Udayanga, Ms GDD Priyadarshani, Ms AWBWS Wijesiriwardana, Mr Ahamed Imdad Rafaideen, Network for Improving Critical care Systems and Training (www.nicst.com); South Asian Association for regional cooperation (http://www.saarc-sec.org/).
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Harrison DA, Brady AR, Rowan K. Case mix, outcome and length of stay for admissions to adult, general critical care units in England, Wales and Northern Ireland: the Intensive Care National Audit & Research Centre Case Mix Programme Database. Crit Care 2004; 8: R99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van de Klundert N, Holman R, Dongelmans DA, et al. Data resource profile: the Dutch National Intensive Care Evaluation (NICE) registry of admissions to adult intensive care units. Int J Epidemiol 2015; 44: 1850–1850h. [DOI] [PubMed] [Google Scholar]
- 3.Haniffa R, Lubell Y, Cooper BS, et al. Impact of a structured ICU training programme in resource-limited settings in Asia. PLoS ONE 2017; 12: e0173483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haniffa R, De Silva AP, Beane A, et al. To: The Epimed Monitor ICU Database®: a cloud-based national registry for adult intensive care unit patients in BrazilPara: Epimed Monitor ICU Database®. Rev Bras Ter Intensiva 2018; 30: 251–252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Beane A, Athapattu PL, Dondorp AM, et al. Commentary: challenges and priorities for pediatric critical care clinician–researchers in low- and middle-income countries. Front Pediatr 2018; 6: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Riviello ED, Letchford S, Achieng L, et al. Critical care in resource-poor settings: lessons learned and future directions. Crit Care Med 2011; 39: 860–867. [DOI] [PubMed] [Google Scholar]
- 7.El-Jardali F, Makhoul J, Jamal D, et al. Eliciting policymakers’ and stakeholders’ opinions to help shape health system research priorities in the Middle East and North Africa region. Health Policy Plan 2009; 25: 15–27. [DOI] [PubMed] [Google Scholar]
- 8.Swaminathan S, Qureshi H, Jahan MU, et al. Health research priorities and gaps in South Asia. BMJ 2017; 357: j1510. [DOI] [PubMed] [Google Scholar]
- 9.Biccard BM, Madiba TE, Kluyts HL, et al. Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet 2018; 391: 1589–1598. [DOI] [PubMed] [Google Scholar]
- 10.Dare AJ, Onajin-Obembe B, Makasa EM. A snapshot of surgical outcomes and needs in Africa. Lancet 2018; 391: 1553–1554. [DOI] [PubMed] [Google Scholar]
- 11.Zampieri FG, Soares M, Borges LP, et al. The Epimed Monitor ICU Database®: a cloud-based national registry for adult intensive care unit patients in Brazil. Braz J Intensive Care 2017; 29: 418–426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Malaysian Registry of Intensive Care, http://mric.org.my/about-mric/ (accessed February 2018).
- 13.National Intensive Care Surveillance, Ministry of Health, Sri Lanka. Critical Care Bed System for Sri Lanka, www.scribd.com/document/211611539/CRITICAL-CARE-BED-SYSTEM-FOR-SRI-LANKA (2013, accessed February 2018).
- 14.Rudd KE, Seymour CW, Aluisio AR, et al. Association of the Quick Sequential (Sepsis-Related) Organ Failure Assessment (qSOFA) score with excess hospital mortality in adults with suspected infection in low- and middle-income countries. JAMA 2018; 319: 2202–2211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pisani L, Algera AG, Neto AS, et al. PRactice of VENTilation in Middle–Income Countries (PRoVENT–iMIC) – rationale and protocol for a prospective international multicentre. BMJ Open 2018; 8: e020841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Haniffa R, Mukaka M, Munasinghe SB, et al. Simplified prognostic model for critically ill patients in resource limited settings in South Asia. Crit Care 2017; 21: 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.College of Physicians and Surgeons of Pakistan, www.cpsp.edu.pk/ (accessed February 2018).
- 18.Zimmerman JE, Kramer AA, McNair DS, et al. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today’s critically ill patients. Crit Care Med 2006; 34: 1297–1310. [DOI] [PubMed] [Google Scholar]
- 19.Haniffa R, Beane A, De Silva AP, et al. Re: emerging and re-emerging infectious disease threats in South Asia: status, vulnerability, preparedness, and outlook. BMJ 2017; 357: j1447. [DOI] [PubMed] [Google Scholar]
- 20.De Silva AP, Harischandra PL, Beane A, et al. A data platform to improve rabies prevention, Sri Lanka. Bull World Health Org 2017; 95: 646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.ANZICS. Privacy and security assessment, www.anzics.com.au/ (2017, accessed February 2018).
- 22.Haniffa R, De Silva AP, Iddagoda S, et al. A cross-sectional survey of critical care services in Sri Lanka: a lower middle-income country. J Crit Care 2014; 29: 764–768. [DOI] [PubMed] [Google Scholar]